Overview
In the demanding world of healthcare, providers often grapple with emotional challenges stemming from administrative burdens. It’s crucial to recognize how these pressures can impact patient care. This article focuses on enhancing documentation skills through the use of SOAP medical examples, highlighting their significance in clinical practice.
Effective SOAP notes are not just a formality; they are a lifeline for better communication. They reduce errors and streamline patient care, transforming how healthcare professionals interact with their patients. Evidence supports that organized records can enhance treatment outcomes and efficiency in healthcare settings.
Imagine the relief of knowing that your documentation can lead to clearer communication and improved patient care. By embracing SOAP notes, healthcare providers can foster a more efficient environment, ultimately benefiting both themselves and their patients.
Let’s take a moment to reflect: How often do you feel overwhelmed by paperwork? By prioritizing effective documentation, we can alleviate some of that burden. We encourage you to engage with these practices and witness the positive impact they can have on your daily routine and patient interactions.
Introduction
In the complex world of healthcare documentation, the SOAP note format emerges as a vital tool for fostering effective communication and enhancing patient care. Many providers face the dual pressures of managing administrative tasks and engaging with patients. By mastering SOAP notes, healthcare professionals can significantly improve their documentation skills and elevate the quality of care they provide. Yet, with the ever-changing demands of the medical field, how can providers ensure their notes not only comply with regulatory standards but also reflect the unique experiences of their patients? This article explores seven insightful examples of SOAP notes that highlight best practices, offering valuable insights that empower providers to streamline their documentation processes and ultimately promote better patient outcomes.
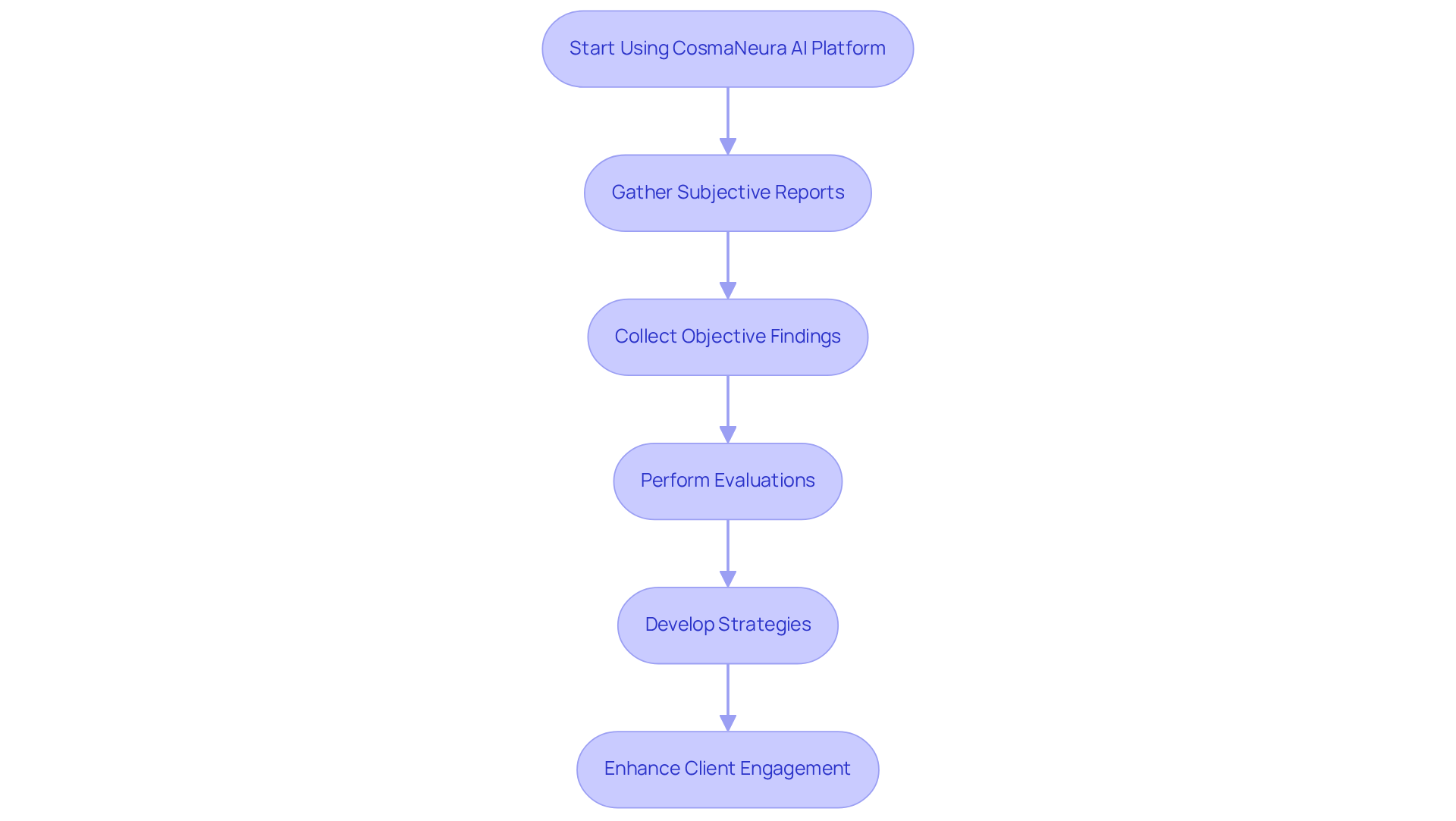
CosmaNeura: Streamline SOAP Note Documentation with AI-Powered Efficiency
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from the time they spend with patients. CosmaNeura's AI platform offers a transformative solution to this challenge, enabling the creation of soap medical example notes with remarkable speed and accuracy. By utilizing advanced algorithms, the platform efficiently gathers subjective reports, objective findings, evaluations, and strategies, significantly simplifying the record-keeping process.
Imagine the relief of saving precious time while improving the quality of care. This automation allows healthcare providers to focus on what truly matters—client engagement—rather than being bogged down by paperwork. Moreover, the incorporation of AI serves as a soap medical example that ensures compliance with best practices in record-keeping, making it an , particularly those committed to Catholic principles.
As AI continues to revolutionize healthcare, its role in enhancing record efficiency is becoming increasingly vital. By 2025, it is anticipated that a significant portion of healthcare providers will rely on AI solutions to improve their workflows and interactions with individuals. Embrace this opportunity to enhance your practice and provide the compassionate care your patients deserve.
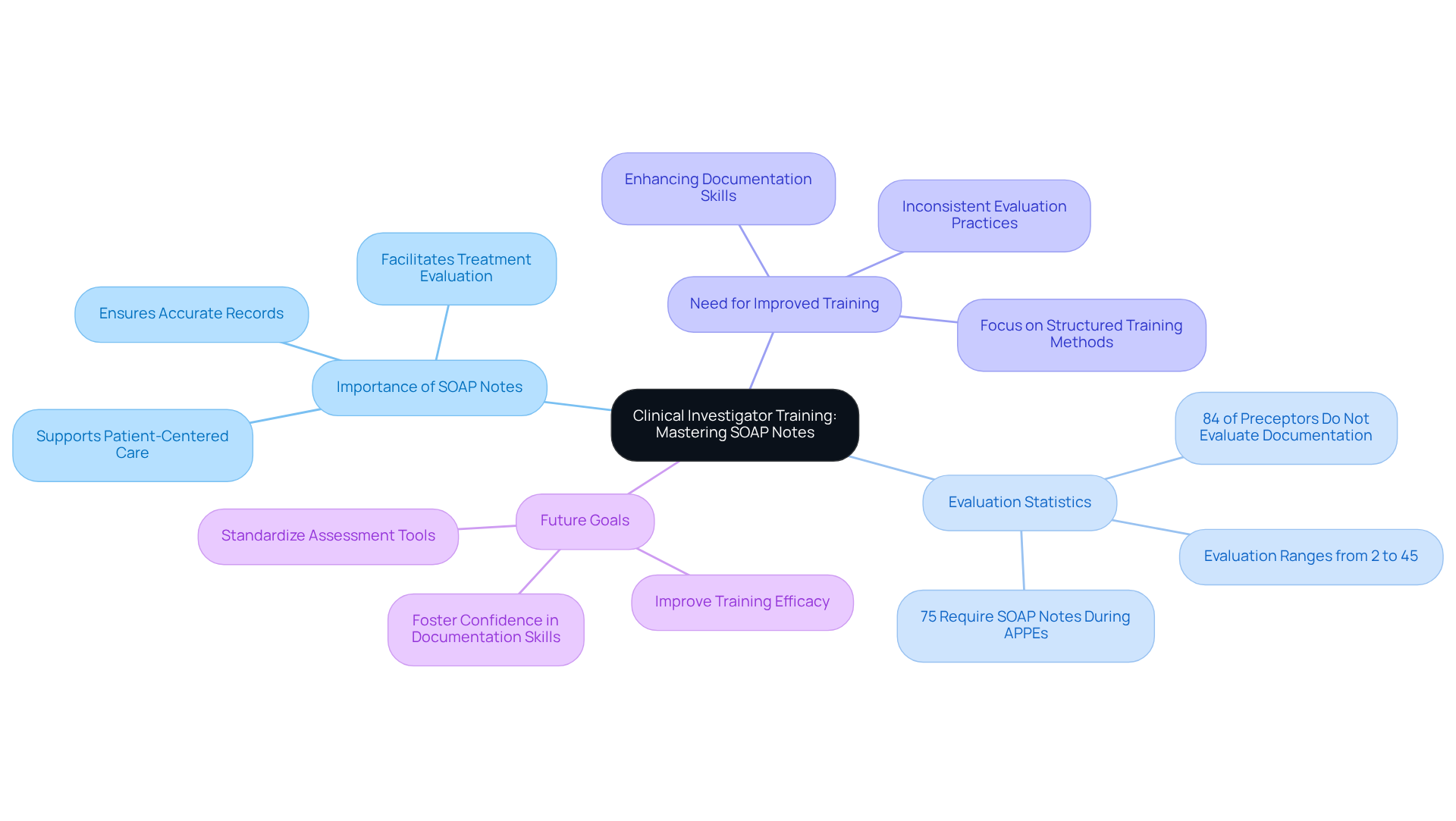
Clinical Investigator Training Course: Mastering SOAP Notes for Clinical Trials
Clinical Investigator Training Courses underscore the importance of mastering the SOAP medical example notes, which are a crucial skill for ensuring accurate and compliant records in clinical trials. Have you ever felt overwhelmed by the intricacies of patient documentation? Participants are guided on how to effectively capture patient data, including both subjective experiences and objective findings, which are essential for evaluating treatment efficacy.
These training programs often incorporate practical exercises and real-world examples, allowing investigators to refine their documentation skills while adhering to regulatory standards. However, it's concerning to note that the proportion of preceptors who officially evaluate clinical summaries varies significantly among schools, ranging from 2% to 45%. This inconsistency highlights a pressing need for improved training efficacy and evaluation criteria across institutions.
Moreover, a staggering 84% of preceptors do not officially evaluate clinical documentation. This statistic emphasizes the critical need for organized training methods that truly support our healthcare providers. Specialists like Philip Pastides have observed that while half of the preceptors perceive students as ready to compose clinical documentation, many students struggle with the evaluation segment.
By focusing on enhancing clinical record abilities, clinical researchers can significantly elevate the quality of their records. This improvement not only aids in more efficient and ethical clinical studies but also fosters a supportive environment for all involved. Together, we can work towards a future where every healthcare provider feels equipped and .
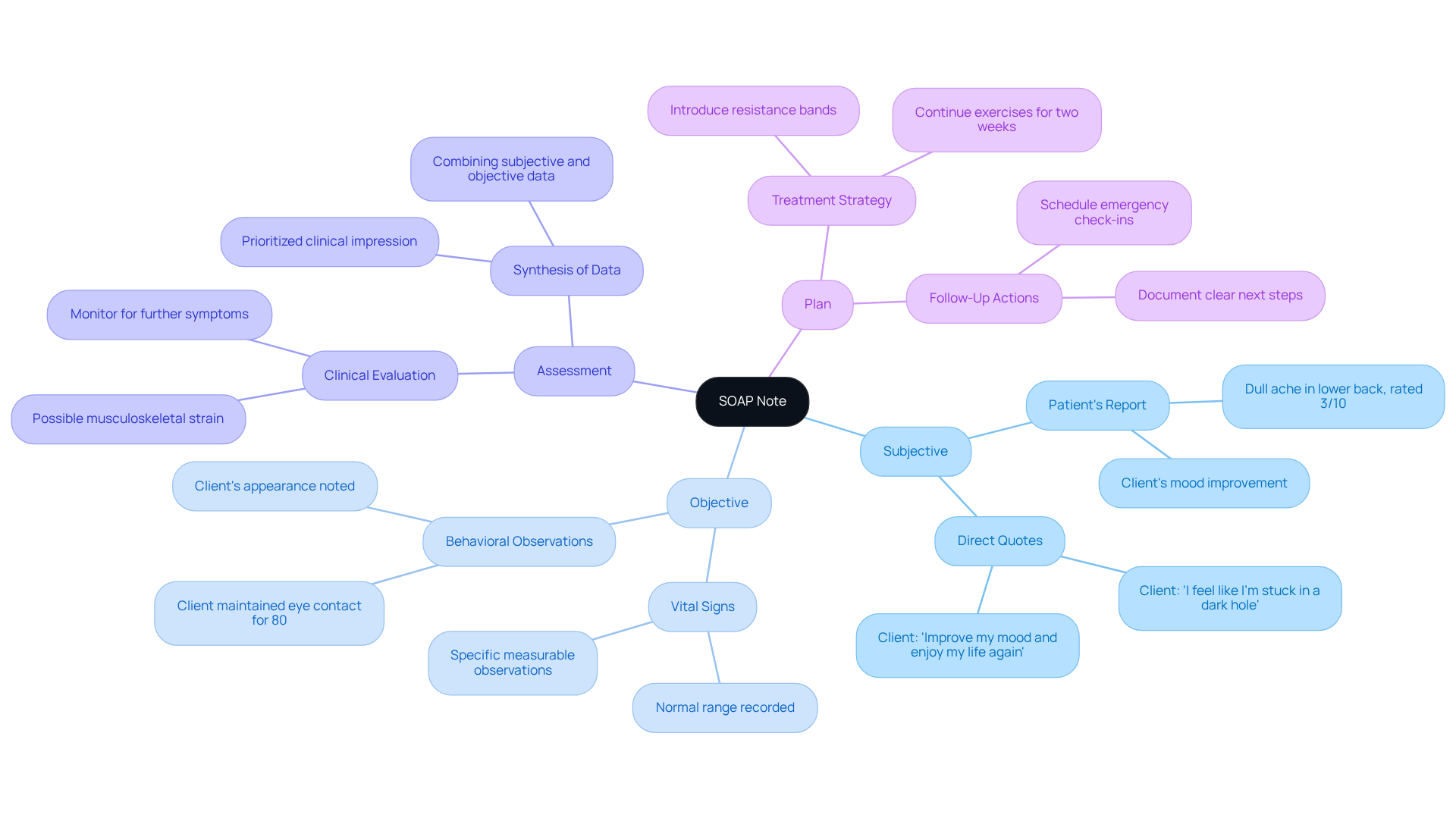
Medical SOAP Note Example: Templates and Best Practices for Effective Documentation
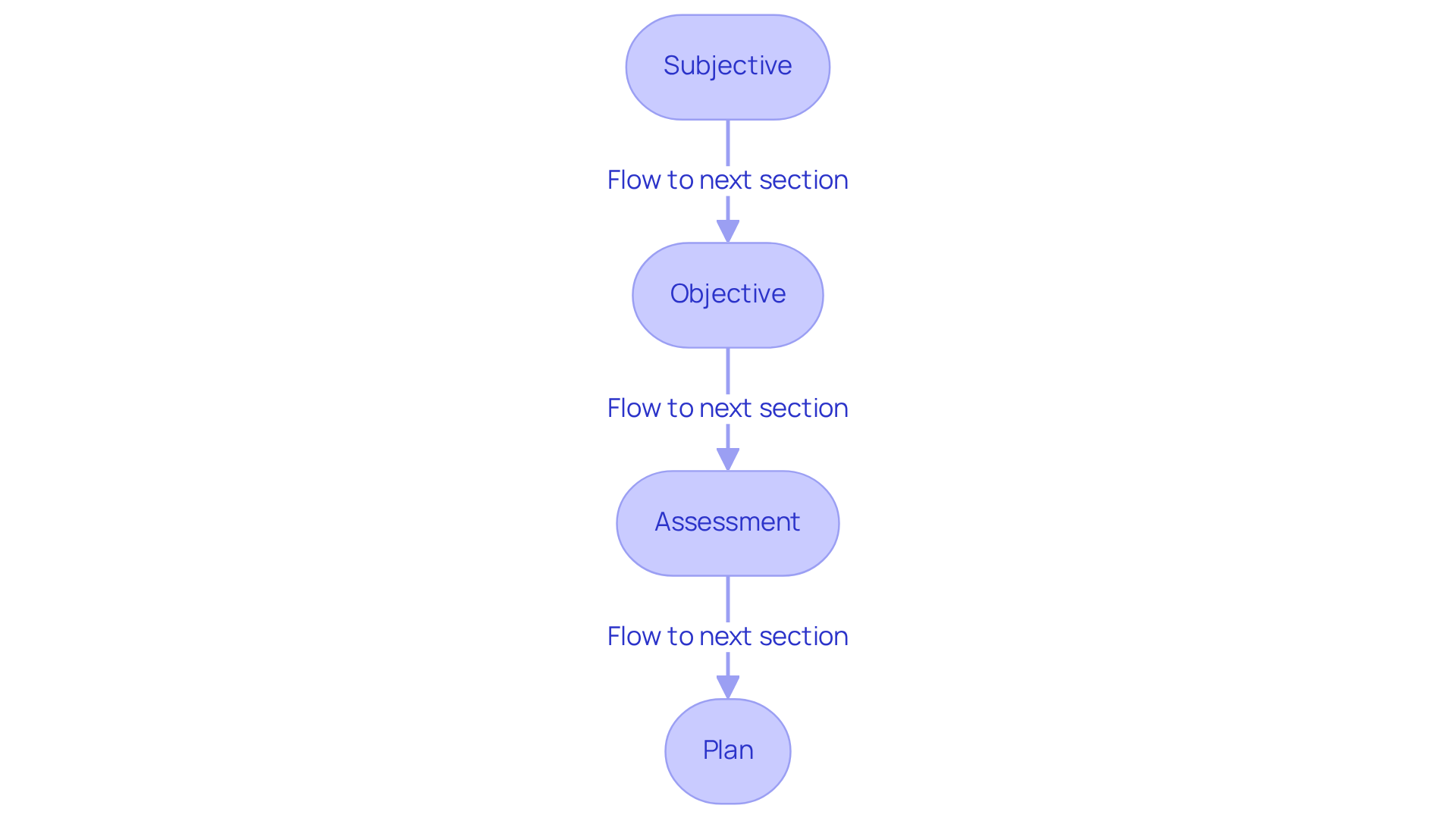
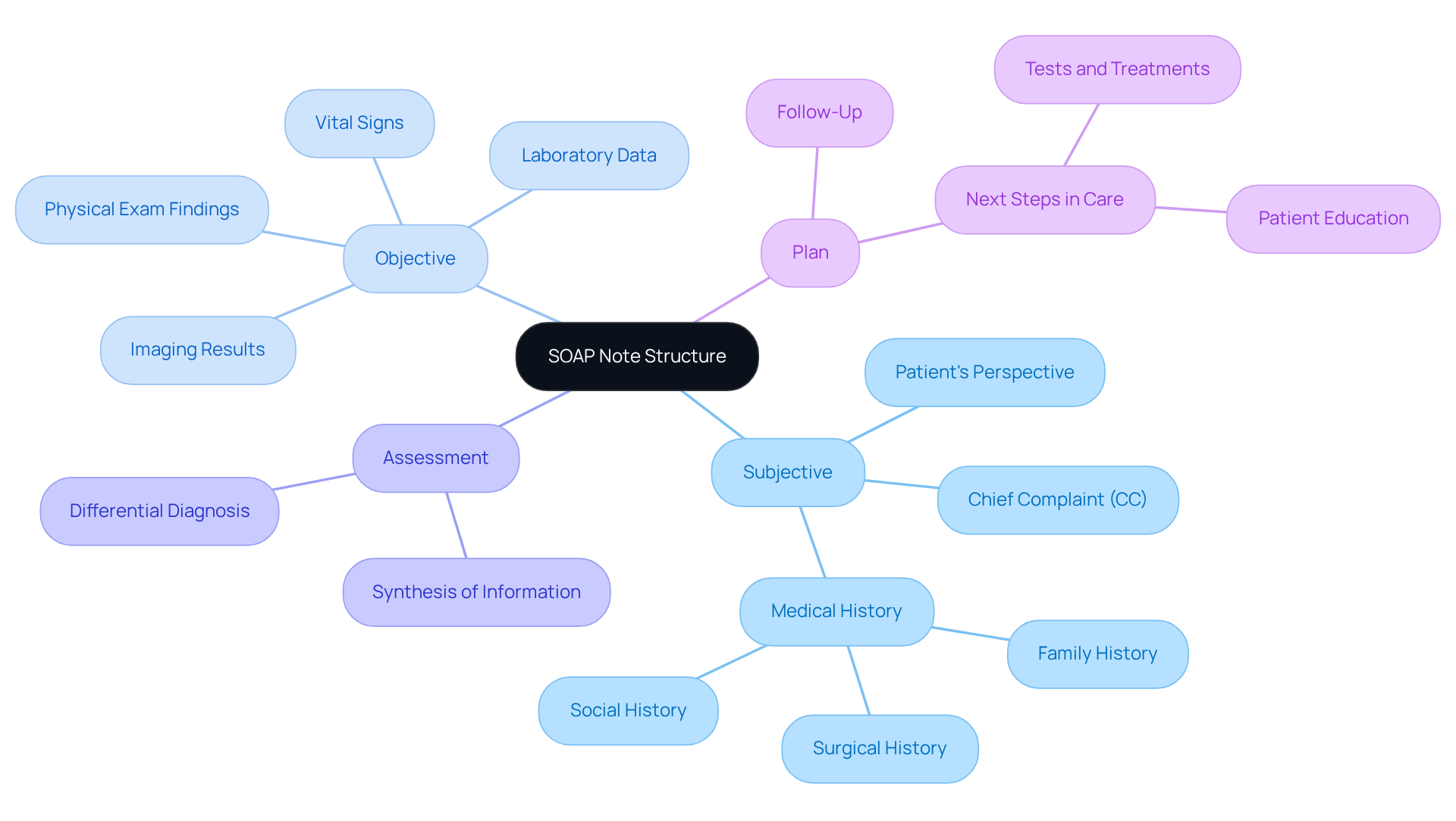
Effective documentation is essential in healthcare, and it relies on well-organized templates that consist of four fundamental sections: Subjective, Objective, Assessment, and Plan. For example, a standard clinical documentation begins with the patient's primary concern in the Subjective section, followed by quantifiable information like vital signs in the Objective section. The Assessment section provides a clinical evaluation, while the Plan outlines a detailed treatment strategy.
The methods for developing documentation highlight the importance of clear and concise language. Avoiding jargon can significantly improve readability, making it easier for healthcare providers to communicate effectively. This clarity not only aids in collaboration but also ensures that all pertinent information is accurately captured. Research shows that organized records can reduce medical errors by up to 40%, ultimately enhancing treatment outcomes and ensuring continuity of care. Additionally, methods that employ organized clinical records have demonstrated a 75% increase in record-keeping speed, further boosting efficiency.
To illustrate effective documentation, consider a SOAP note example:
- Subjective: Patient reports a 'dull ache' in the lower back, rated 3/10, an improvement from 6/10 last week.
- Objective: Vital signs recorded; individual exhibits normal range.
- Assessment: Possible musculoskeletal strain; monitor for further symptoms.
- Plan: Continue current exercises for two weeks, then introduce resistance bands.
Dr. Claire Dave emphasizes that the objective section must include specific, measurable observations to ensure clarity and adherence to record-keeping standards. By following these best practices and utilizing organized templates, healthcare providers can enhance their documentation skills. This ultimately leads to better care and , fostering a supportive environment for both patients and providers.
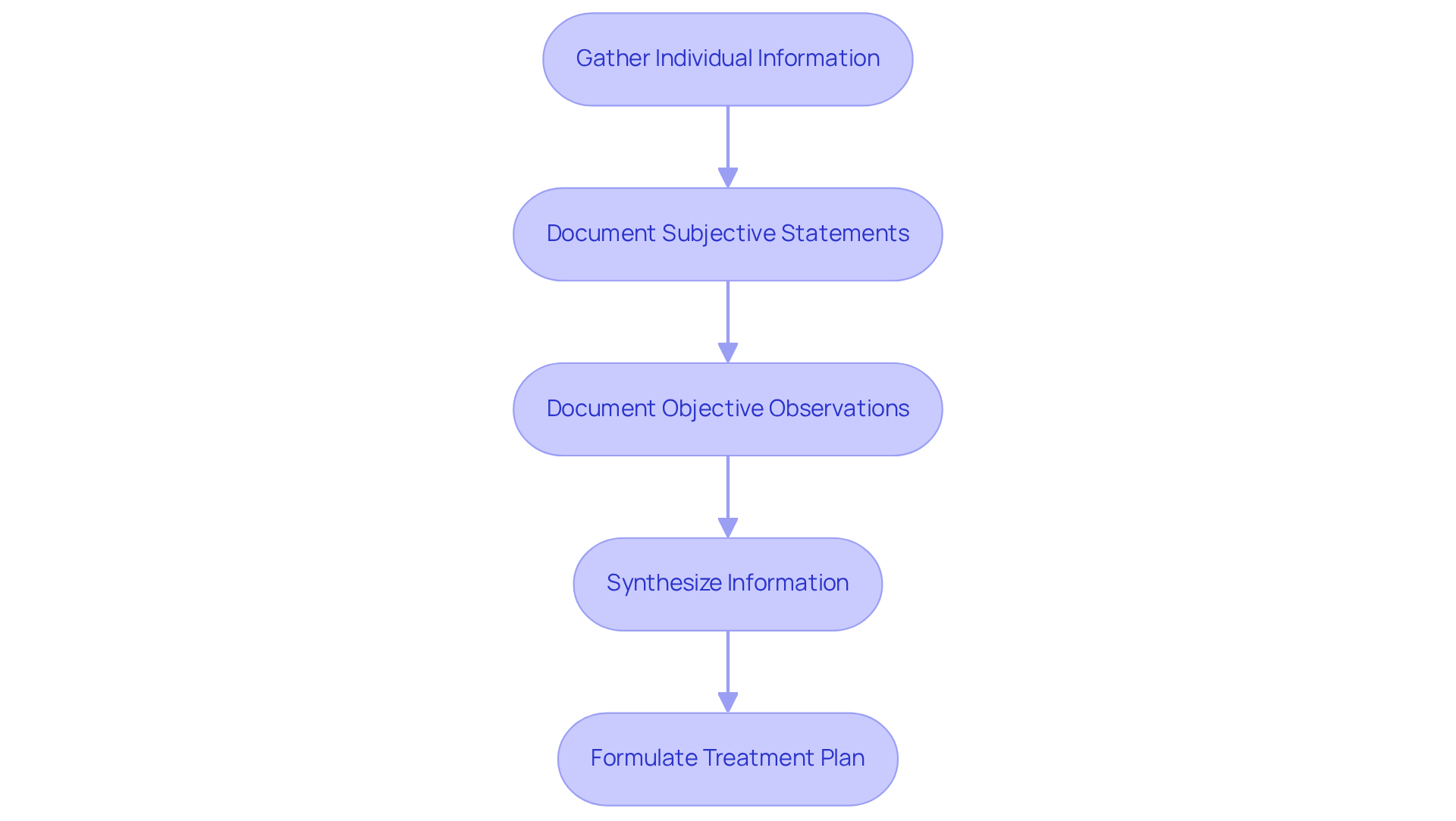
WikiHow: Step-by-Step Guide to Writing Effective SOAP Notes
For healthcare providers, writing [effective SOAP medical example notes](https://cosmaneura.com/about) can often feel overwhelming. By embracing a systematic approach, you can alleviate some of these emotional burdens. Start by gathering all relevant individual information before the appointment; this ensures you have a comprehensive understanding of the person's history and concerns. During the session, take care to accurately document the individual's subjective statements, capturing their feelings and experiences. Follow this with objective observations, including measurable data such as vital signs and physical examination findings.
After the visit, take a moment to synthesize the collected information. This will help you formulate a clear and actionable treatment plan. By adopting this structured methodology, you not only facilitate meticulous documentation but also create a SOAP medical example that significantly enhances communication among healthcare providers, promoting continuity of care. Have you considered how standardized medical terminology can improve clarity in your notes? This practice can enhance outcomes for individuals and ensure adherence to regulatory standards.
Effective documentation serves as a crucial communication tool. It reflects your professional judgment and fosters a collaborative healthcare environment. Remember, your efforts in are not just administrative tasks; they are vital components of patient support and care continuity. Embrace this process, and you can make a meaningful difference in the lives of those you serve.
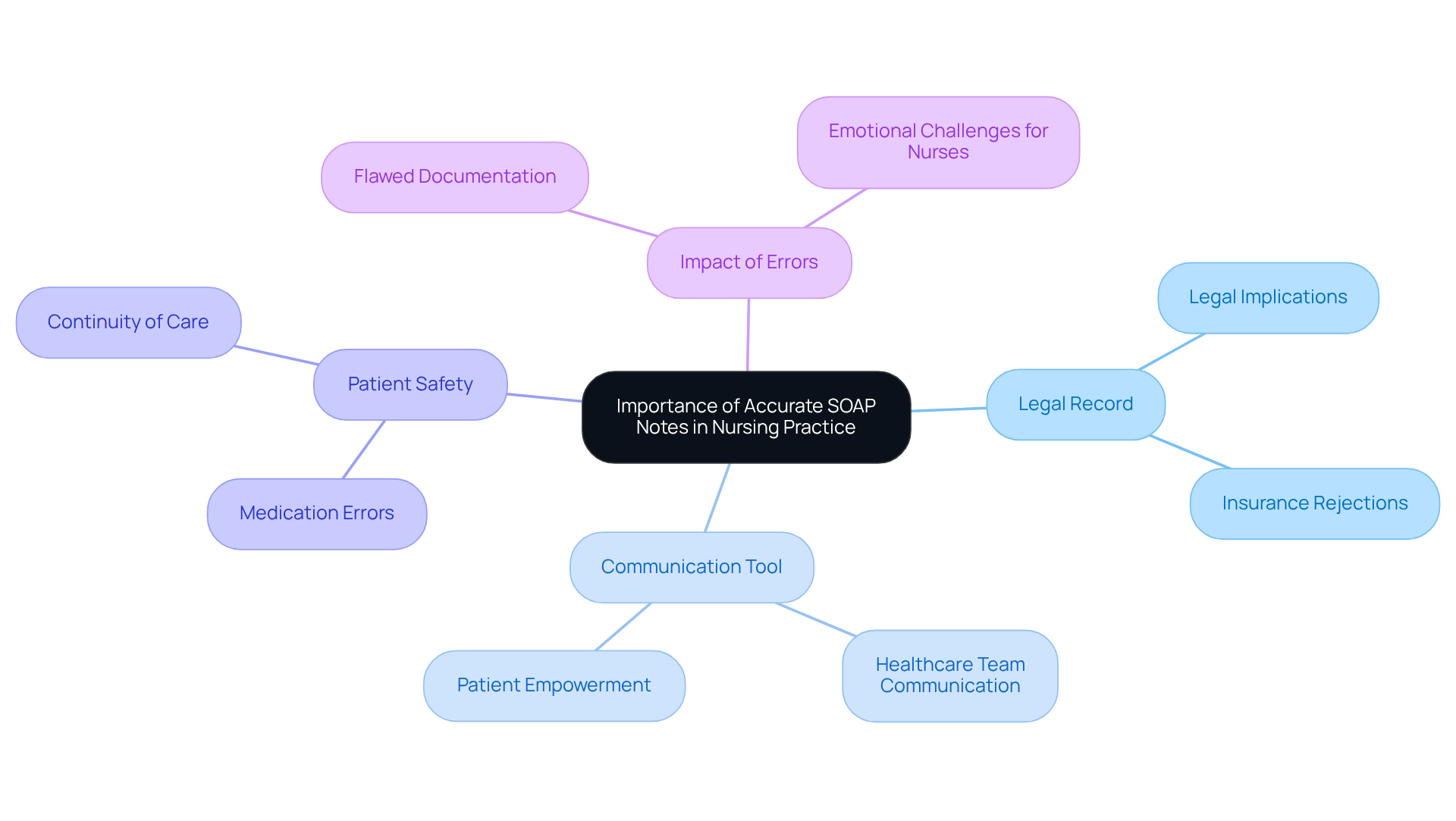
Herzing University: Importance of Accurate SOAP Notes in Nursing Practice
In nursing practice, precise SOAP notes are not just a formality; they are a lifeline. These notes serve as a legal record of interactions and are an essential communication tool among healthcare providers. When records are insufficient or erroneous, misunderstandings can arise, jeopardizing individual safety. Have you ever considered that nearly 10% of patients in hospital settings experience medication errors, often stemming from inadequate record-keeping?
Nurses are trained to meticulously document clinical findings, individual responses, and any changes in condition. This dedication ensures that all is readily available for ongoing care. By prioritizing thorough documentation, nurses not only enhance safety for those receiving care but also protect themselves legally. In fact, erroneous or insufficient entries were a primary reason for insurance rejections in 2025.
Imagine the peace of mind that comes from knowing that your careful documentation can significantly improve the quality of care. By fostering better communication within the healthcare team, we can create a safer environment for everyone involved. Let’s commit to embracing precise and comprehensive records—it's a small step that leads to profound benefits for our patients and ourselves.
Immigration Justice: Sample SOAP Notes for Legal Documentation
In the realm of immigration justice, the notes—representing Subjective, Objective, Assessment, and Plan—serve as vital tools for legal documentation. They ensure that every relevant piece of individual information is meticulously recorded. Have you considered the emotional challenges that individuals face regarding their immigration status? A soap medical example might reflect their subjective experiences, capturing the emotional and psychological hurdles they endure.
The objective section would detail specific findings from medical examinations, including vital signs like temperature, heart rate, and blood pressure, along with any pertinent diagnostic results. This not only enhances comprehensive care for individuals but also strengthens legal claims. By providing clear, organized records, we create references that can be invaluable in legal situations.
Accurate patient records are paramount; they can significantly influence the outcomes of immigration cases. It is essential for healthcare providers to advocate effectively for their patients. As Bertrand Meyer wisely noted, "Incorrect records are often worse than no records," underscoring the critical importance of precise record-keeping in both clinical and legal contexts.
Let’s reflect on how we can improve our documentation practices. By prioritizing accurate records, we not only support our patients but also empower ourselves to navigate the complexities of immigration justice with confidence.
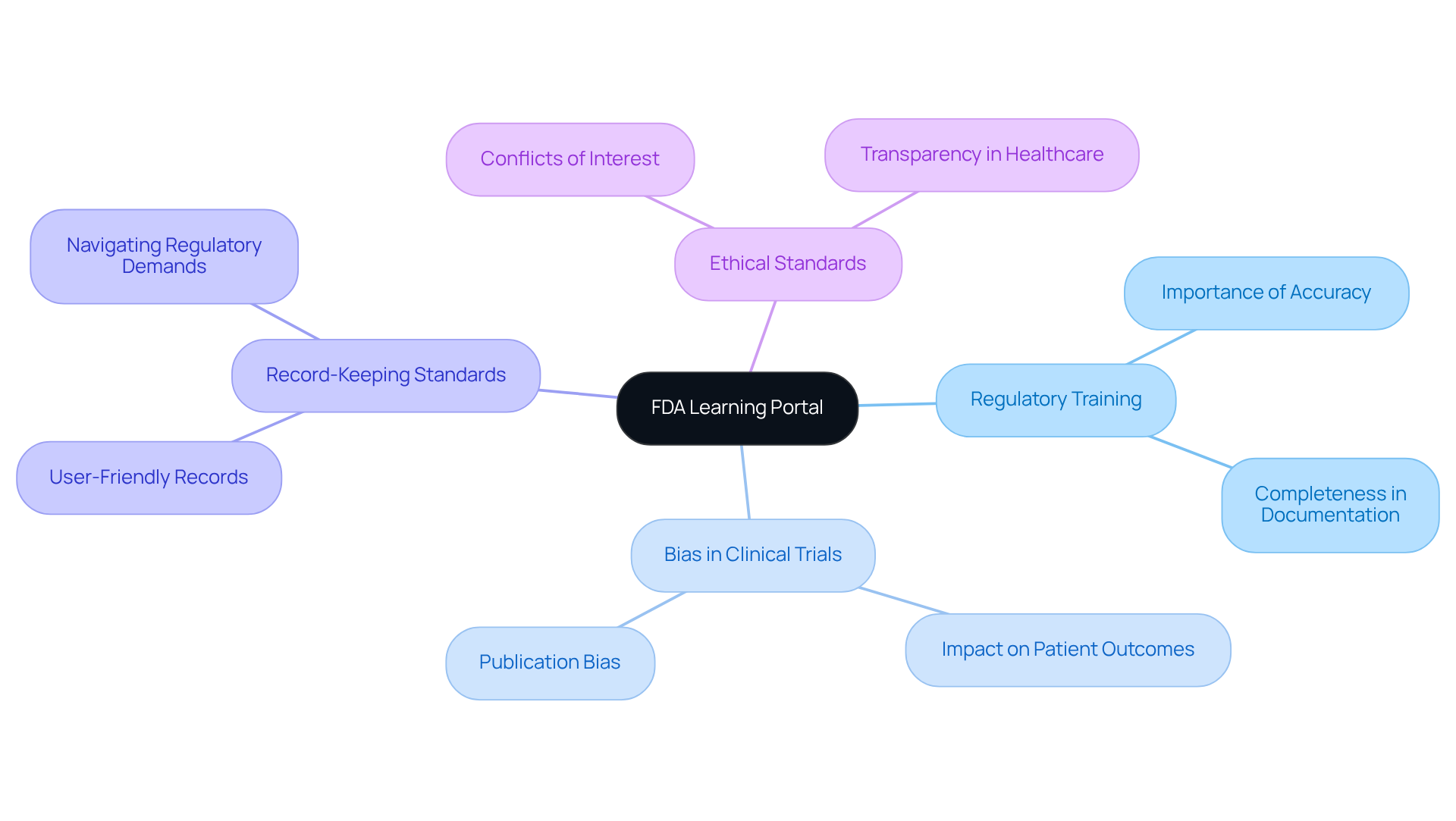
FDA Learning Portal: Regulatory Training for SOAP Note Compliance
The FDA Learning Portal offers crucial regulatory training designed to support healthcare providers in ensuring that their SOAP medical example notes align with industry standards. This training highlights the essential components of record-keeping that are vital for both clinical trials and patient care, emphasizing the importance of accuracy and completeness.
Have you ever considered how bias can affect patient outcomes? As Marcia Angell pointed out, "A review of seventy-four clinical trials of antidepressants... found that thirty-seven of thirty-eight positive studies were published. But of the thirty-six negative studies, thirty-three were either not published or published in a form that conveyed a positive outcome." This underscores the need for healthcare providers to master to mitigate biases and uphold integrity in clinical research.
Moreover, records should be user-friendly and tailored to the tasks at hand, as recent statistics suggest. By navigating regulatory demands effectively, providers can enhance their record-keeping practices, which ultimately leads to better outcomes for patients and adherence in clinical settings.
What if improving these methods could significantly impact your practice? Additionally, recognizing potential conflicts of interest in clinical trials is crucial for safeguarding individual rights and maintaining ethical standards in healthcare. Together, we can foster a more transparent and compassionate healthcare environment.
Studying Nurse: Breakdown of SOAP Note Structure for Healthcare Providers
Understanding the structure of is crucial for healthcare providers. Each component plays a vital role in effective communication and documentation. Have you ever felt overwhelmed by the demands of patient care? The Subjective section captures the individual's perspective, including their experiences, feelings, and chief complaints. These elements are essential for accurate diagnosis.
The Objective section presents measurable data, such as vital signs and physical exam findings. This provides a factual basis for clinical decisions, allowing you to feel confident in your assessments. The Assessment synthesizes the subjective and objective information, guiding your thought process and helping you formulate a clinical interpretation.
Ultimately, the Plan outlines the next steps in care, detailing necessary tests, treatments, and education for individuals. Mastering this structure serves as a soap medical example that not only improves the quality of records but also promotes clearer communication among healthcare teams. This clarity can enhance outcomes for individuals, which is a shared goal we all strive for.
The transition to structured documentation has shown to significantly enhance the clarity and completeness of notes. This makes it easier for clinicians to access relevant information quickly and efficiently. Furthermore, the APSO order (Assessment, Plan, Subjective, Objective) has been observed to enhance speed, accuracy, and usability during client visits.
It is also important to consider the History of Present Illness (HPI) and utilize the OLDCARTS acronym to effectively document patient information. However, while organized records provide numerous advantages, they can also result in excessive information that may overwhelm clinicians if not managed properly. How can we find a balance?
Integrating data and a soap medical example from recent research can further illustrate the effectiveness of organized records. Yet, recognizing the constraints of that format, especially its incapacity to record changes over time, is crucial for a comprehensive understanding. Remember, we are all in this together, striving to provide the best care possible.
Immigration Justice: Training Topics on SOAP Notes for Healthcare Providers
Healthcare providers involved in immigration justice often face emotional challenges when documenting sensitive interactions. The process of recording these experiences can feel overwhelming, especially when considering the cultural nuances and legal implications involved. How can we ensure that these vital interactions are captured with the care they deserve?
Training on the soap medical example notes specifically tailored for this context addresses these concerns. By focusing on cultural competency and understanding the legal consequences of records, providers can gain the skills necessary to navigate these complexities. This specialized training not only enhances their ability to document accurately but also of their clients.
Imagine the impact of documenting subjective experiences related to immigration status with precision and empathy. This approach not only fosters better client care but also strengthens legal processes. By equipping providers with the right tools and knowledge, we can create a more compassionate healthcare environment.
Let’s work together to ensure that every healthcare provider feels confident in their ability to support their clients through these challenging situations. Engaging in this training is a crucial step towards making a meaningful difference in the lives of those we serve.
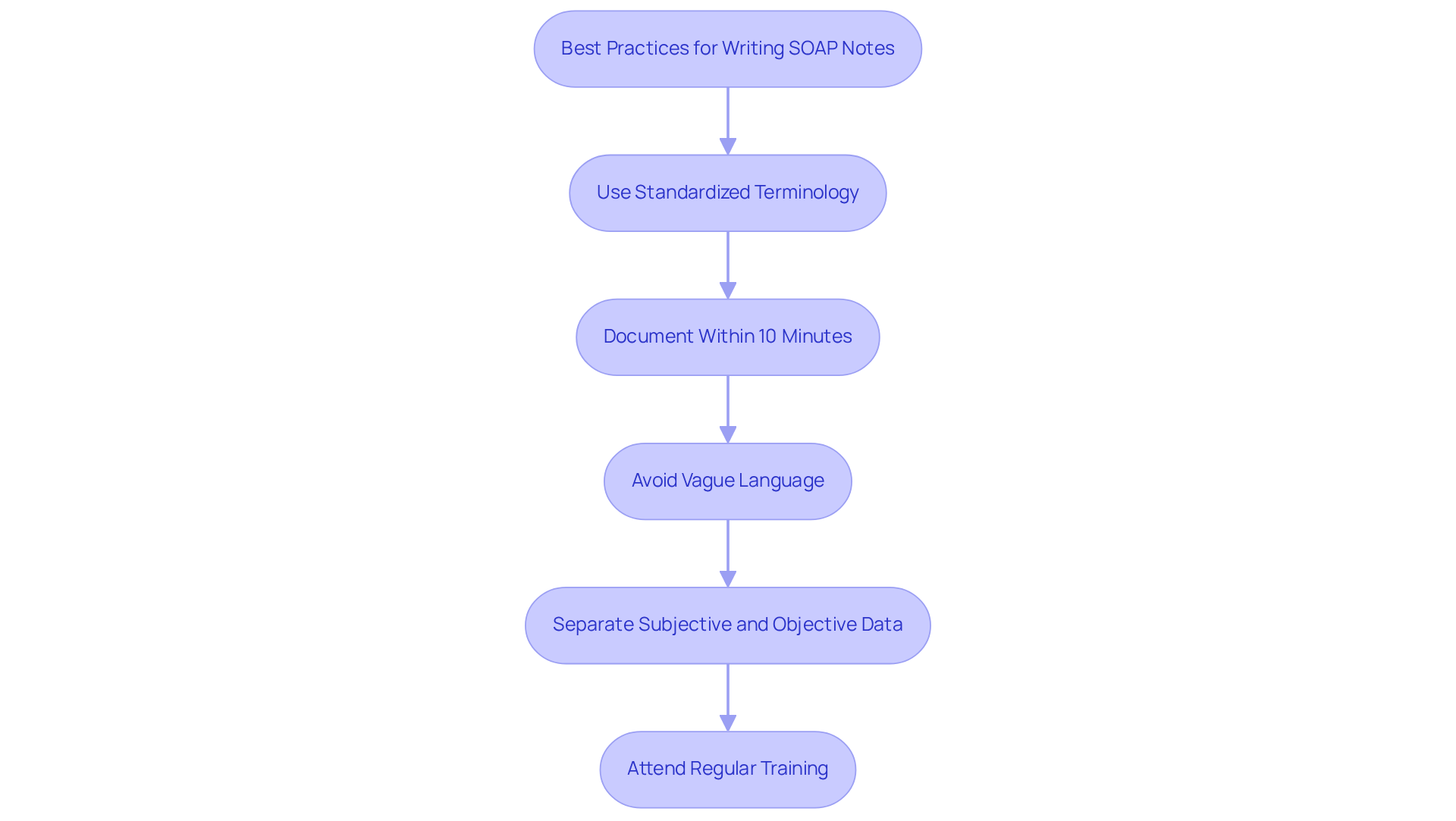
Studying Nurse: Best Practices for Writing Clear and Compliant SOAP Notes
In the demanding world of healthcare, providers often grapple with the emotional challenges of maintaining clear and compliant records, such as the SOAP medical example. Prioritizing standardized terminology is crucial, as it significantly enhances record quality and fosters clarity. Imagine the difference it makes when specific terms replace vague pronouns—this not only improves clarity but also ensures that all relevant information is accurately captured.
Swift documentation after client interactions is essential; ideally, records should be . This practice supports precision and thoroughness. It's vital to avoid vague language and to clearly distinguish between subjective and objective data, as this separation enhances readability and facilitates better clinical decision-making.
Regular role-specific training sessions and updates on documentation standards can feel like a burden, yet they are vital for maintaining compliance and improving the overall quality of patient care. As Rachel Logan wisely states, 'When effectively used, SOAP medical example notes provide the roadmap for safe, high-quality, and patient-centered care.' By embracing these best practices, providers can create comprehensive records that not only support effective communication but also enhance continuity of care. Let's work together to ensure that every patient receives the compassionate care they deserve.
Conclusion
In the realm of healthcare, mastering SOAP notes transcends mere administrative duty; it embodies a vital skill that enriches patient care and fosters communication among providers. This article has shed light on the multifaceted nature of SOAP documentation, highlighting its significance across various settings—from clinical trials to nursing practice and even immigration justice. The integration of AI tools, like CosmaNeura, serves as a testament to how technology can alleviate the documentation burden, enabling healthcare professionals to prioritize patient engagement over paperwork.
Key insights discussed include:
- The necessity for structured documentation
- The profound impact of clear communication on treatment outcomes
- The urgent need for comprehensive training in SOAP note writing
By embracing best practices and utilizing organized templates, healthcare providers can significantly minimize errors and enhance the quality of care delivered to patients. Moreover, the article underscores the critical role of accurate documentation in legal contexts, reinforcing the belief that meticulous records are essential not only for clinical efficacy but also for protecting patient rights.
Ultimately, the call to action is unmistakable: embracing the principles of effective SOAP note writing is crucial for all healthcare providers. By prioritizing clarity, compliance, and compassion in documentation, professionals can contribute to a more efficient and supportive healthcare environment. It is essential to engage in ongoing training and leverage available resources to refine these skills, ensuring that every patient receives the high-quality care they truly deserve.




