Overview
This article highlights ten effective examples of SOAP notes designed specifically for nurse practitioners, aiming to enhance their documentation practices. Have you ever felt overwhelmed by the administrative demands of your role? Structured and detailed SOAP notes can significantly improve the quality of patient care by fostering better communication among healthcare providers. They ensure comprehensive record-keeping, allowing you to focus more on meaningful patient interactions rather than getting bogged down by paperwork.
By implementing these practices, you can alleviate some of the emotional burdens that come with your responsibilities. Imagine a work environment where you can dedicate more time to your patients, knowing that your documentation is both efficient and effective. This not only benefits your workflow but also enhances the overall patient experience.
We encourage you to explore these examples and consider how they might fit into your daily routine. Together, let’s strive for a healthcare system that prioritizes compassionate care while streamlining essential tasks. Your dedication to patient well-being deserves the support of efficient documentation practices.
Introduction
In the fast-paced realm of healthcare, nurse practitioners often face the emotional strain of balancing quality patient care with the heavy burden of extensive documentation. These challenges can leave them feeling overwhelmed and stretched thin. This article explores the transformative potential of AI-powered tools, particularly focusing on SOAP note examples that simplify the documentation process.
By embracing these innovative solutions, healthcare providers can enhance their efficiency and reclaim precious time to dedicate to their patients. Imagine a world where administrative tasks no longer overshadow the compassionate care that every patient deserves. How can these advancements in documentation practices alleviate the burdens on healthcare professionals and ultimately improve patient outcomes?
Join us in discovering how these tools can not only lighten the load but also foster a more nurturing environment for both providers and patients alike.
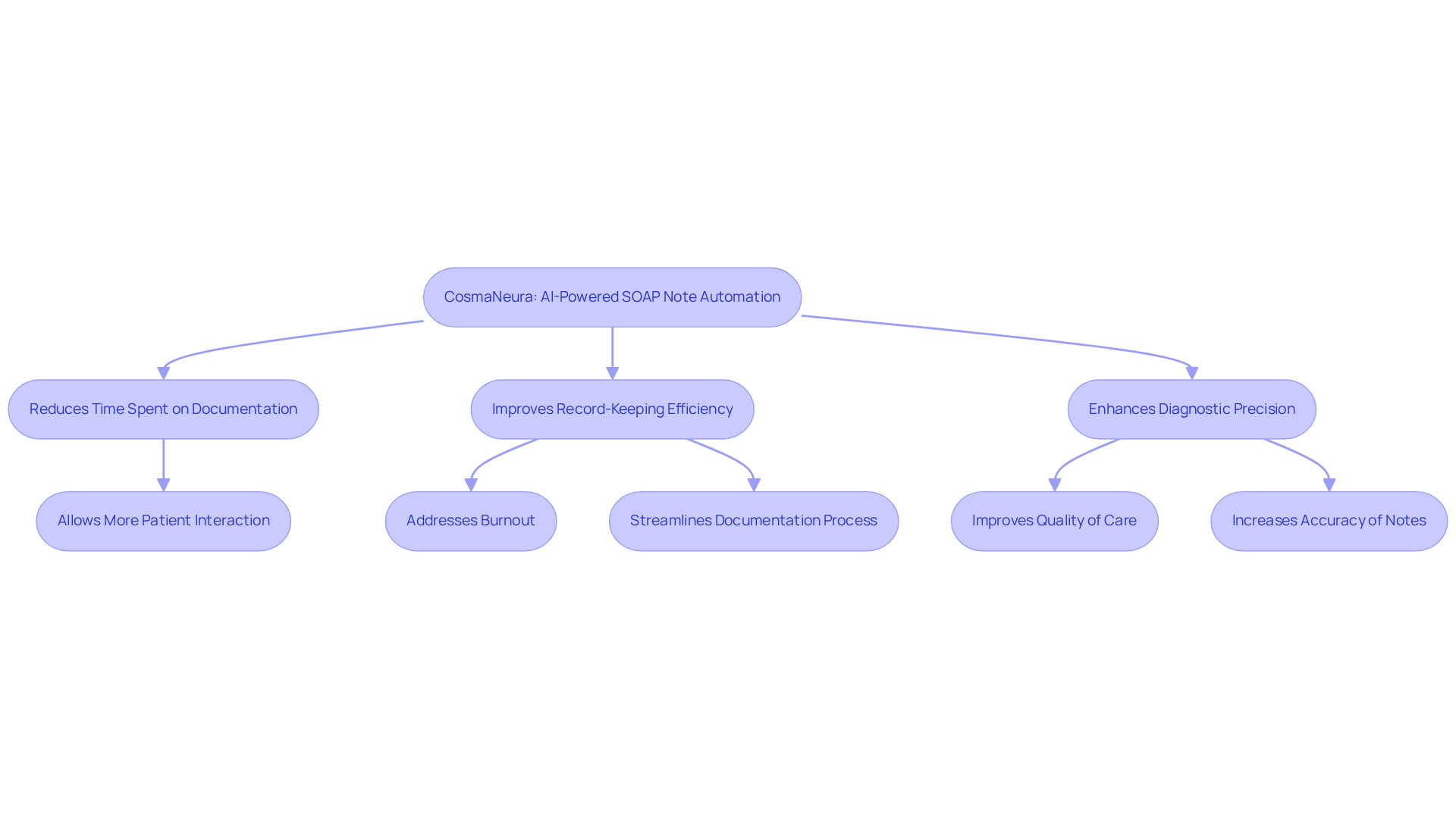
CosmaNeura: AI-Powered SOAP Note Automation for Nurse Practitioners
In the demanding world of healthcare, nurse practitioners often find themselves overwhelmed by administrative tasks, which can detract from their primary focus: patient care. CosmaNeura understands this struggle and utilizes advanced AI technology to automate the generation of a nurse practitioner SOAP note example, significantly reducing the time spent on record-keeping. Imagine what it would feel like to redirect that energy toward your patients instead of paperwork.
By ensuring that all essential information is captured accurately, CosmaNeura follows best practices in clinical records while upholding Catholic ethical standards. This innovation not only streamlines documentation but also enhances the quality of care provided to patients. Studies suggest that using a nurse practitioner SOAP note example can improve record-keeping efficiency by as much as 40%, allowing healthcare providers to regain valuable time.
Moreover, the AI technology enhances diagnostic precision and treatment strategies, addressing essential elements of care. Healthcare professionals have shared their experiences, noting significant reductions in record-keeping burnout. One nurse remarked, 'AI provides tools that can allow us to regain time to concentrate on our clients and restore joy to the practice of medicine.' This transformation in workflow is not just about efficiency; it’s about reclaiming the joy in caring for patients.
With CosmaNeura, nurse practitioners can and elevate the quality of care they provide. This embodies the compassionate spirit of Catholic healthcare, where the focus remains on the well-being of every patient. Together, let’s embrace the future of healthcare, where technology and compassion work hand in hand.
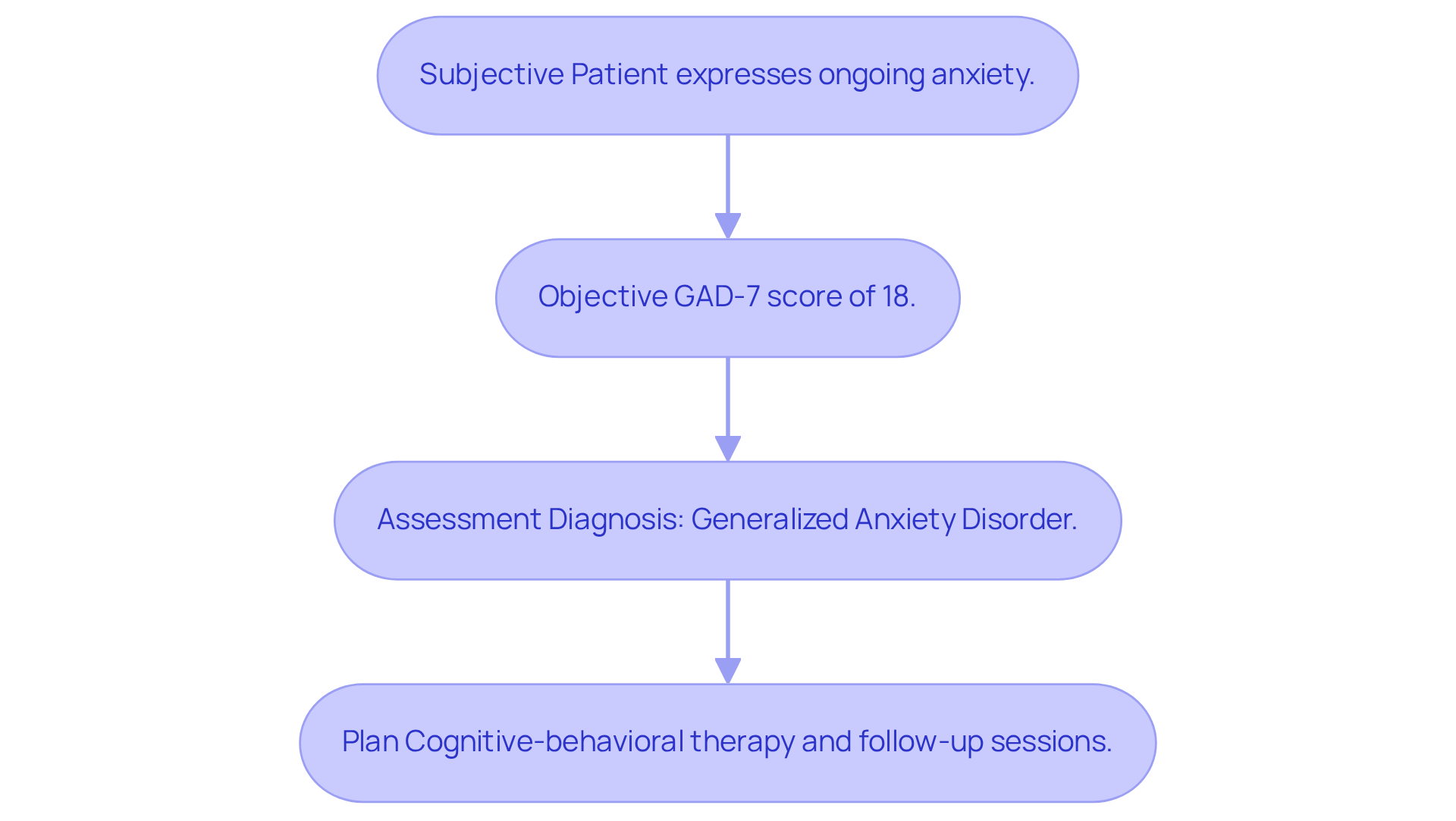
Mental Health SOAP Note Example: Documenting Patient Interactions Effectively
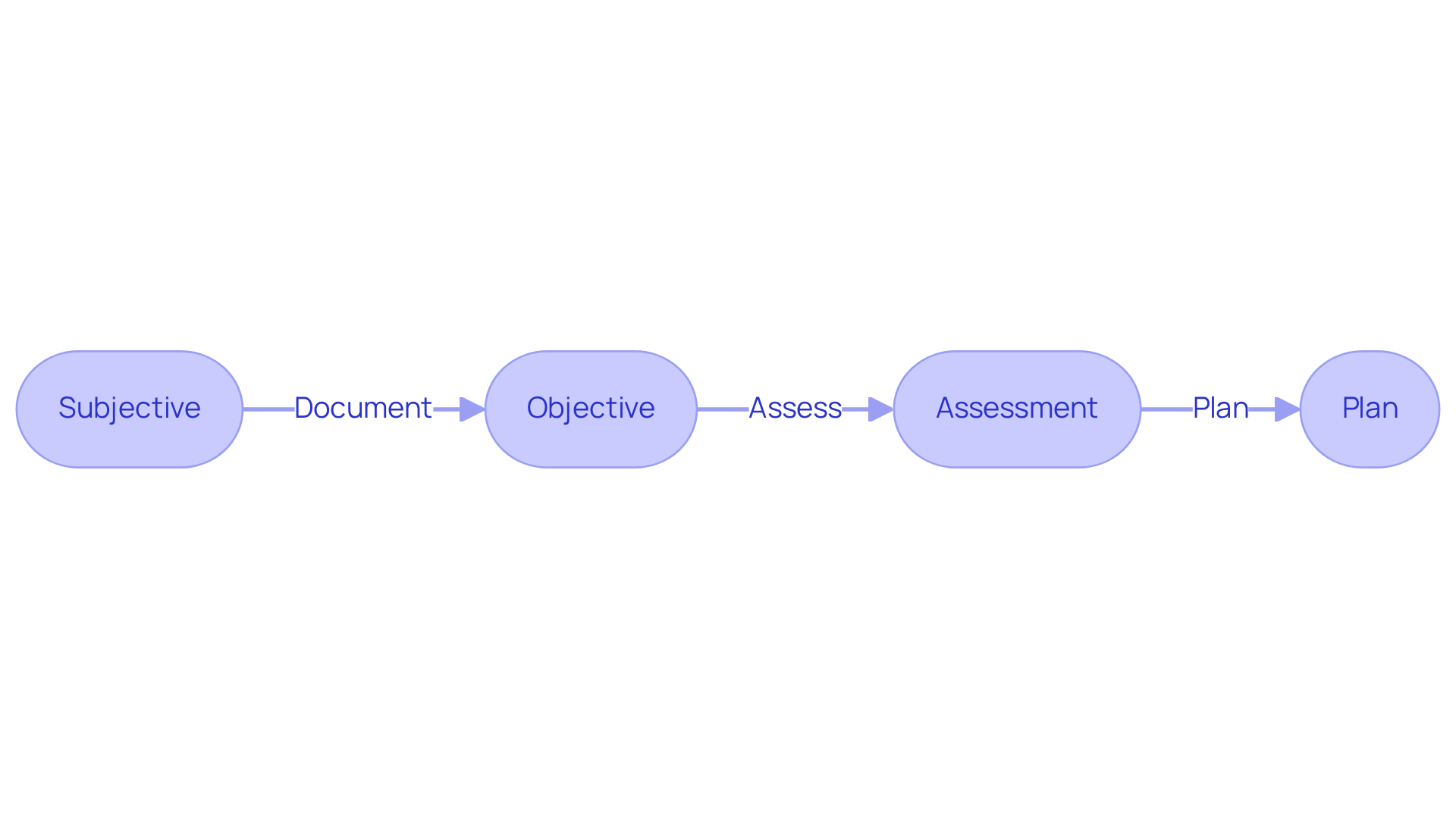
A mental health SOAP record plays a crucial role in understanding the intricate dynamics of client interactions. It encompasses four essential components: subjective observations, objective findings, assessment, and treatment plan. For instance, consider a record that captures a patient's expression of ongoing anxiety (Subjective), documents results from a psychological evaluation indicating a GAD-7 score of 18 (Objective), provides a diagnosis of generalized anxiety disorder (Assessment), and outlines a treatment plan that includes cognitive-behavioral therapy and follow-up sessions (Plan).
This structured approach not only ensures comprehensive care but also fosters better communication among healthcare providers. By doing so, it facilitates effective follow-up and necessary adjustments to treatment. Have you ever felt the burden of administrative tasks overshadowing your ability to provide care? Current trends highlight the adoption of electronic health record (EHR) systems, which often feature a nurse practitioner soap note example within their templates for SOAP entries. This innovation simplifies the documentation process, ensuring precision and adherence to legal requirements.
To enhance the quality of care, optimal methods recommend within 24-48 hours after the visit. This practice ensures that all pertinent information is documented, significantly reducing the chance of mistakes. By following these guidelines, mental health professionals can truly elevate the care they provide to those they serve. Remember, every detail counts in making a positive impact on your patients' lives.
Physical Therapy SOAP Note Example: Capturing Patient Progress and Treatment Plans
In physical therapy, navigating the complexities of patient care can be emotionally challenging. A well-organized nurse practitioner soap note example captures essential individual information, making it easier to monitor treatment and recovery. For example, a nurse practitioner soap note example may indicate that:
- The individual reports a pain level of 5/10 (Subjective)
- The range of motion has improved to 90 degrees (Objective)
- Progress towards rehabilitation goals is on track (Assessment)
- The plan includes increasing resistance in exercises (Plan)
This structured approach not only fosters better communication among healthcare professionals but also allows for timely adjustments to treatment strategies based on patient progress. By meticulously documenting subjective reports, objective measurements, assessments, and future plans, therapists can significantly enhance outcomes and ensure a comprehensive understanding of each individual's journey, similar to a nurse practitioner soap note example.
Additionally, documenting factors affecting progress is crucial, as it provides a holistic view of the individual's condition. Accurate documentation is vital for legal purposes, ensuring compliance with regulations and safeguarding patient confidentiality. To elevate the , healthcare providers should prioritize clarity and consistency in their language.
Consider utilizing innovative AI solutions like CosmaNeura's Agentic Platform. These tools can help address administrative challenges, boost efficiency, and ultimately enhance patient-focused service. By implementing optimal techniques in SOAP record documentation, healthcare providers can improve healthcare quality and responsibility while embracing the transformative potential of generative AI in the medical field.
Family Medicine SOAP Note Template: Structuring Comprehensive Patient Assessments
A well-organized family medicine SOAP format plays a crucial role in providing thorough evaluations of individuals. It’s essential to include sections for:
- Medical history
- Current medications
- Allergies
- Family health history
For example, a nurse practitioner SOAP note example could detail an individual's complaint of fatigue (Subjective), include vital signs and lab results (Objective), provide a diagnosis of hypothyroidism (Assessment), and outline a plan for medication adjustment and follow-up testing (Plan). This comprehensive approach not only addresses all aspects of an individual's health but also significantly improves the quality of records.
Have you ever felt overwhelmed by the administrative burdens that can impact patient care? Research suggests that implementing structured documentation can greatly enhance record quality. Studies show an impressive increase in the Qnote score from 64.35 to 77.2 after transitioning from unstructured to structured formats. This shift leads to , which are vital for delivering high-quality care.
Moreover, detailed SOAP records enhance data reuse, aiding in the continuous management of individuals and quality assessment. Current best practices advocate for structured templates to ensure that all relevant information is captured efficiently. This ultimately improves clinical outcomes and provider efficiency.
By utilizing generative AI, healthcare providers can streamline the record-keeping process by automating repetitive tasks and ensuring that critical information is captured accurately. This integration not only simplifies record-keeping but also preserves the expressiveness of clinical entries, balancing the advantages of structured records with the need for individualized care. As Luc H E Karssemakers, MD, highlights, 'Structured documentation led to a significant improvement in record quality,' underscoring its importance in clinical practice.
Embracing these tools and practices can transform your approach to patient care, allowing you to focus more on what truly matters—your patients.

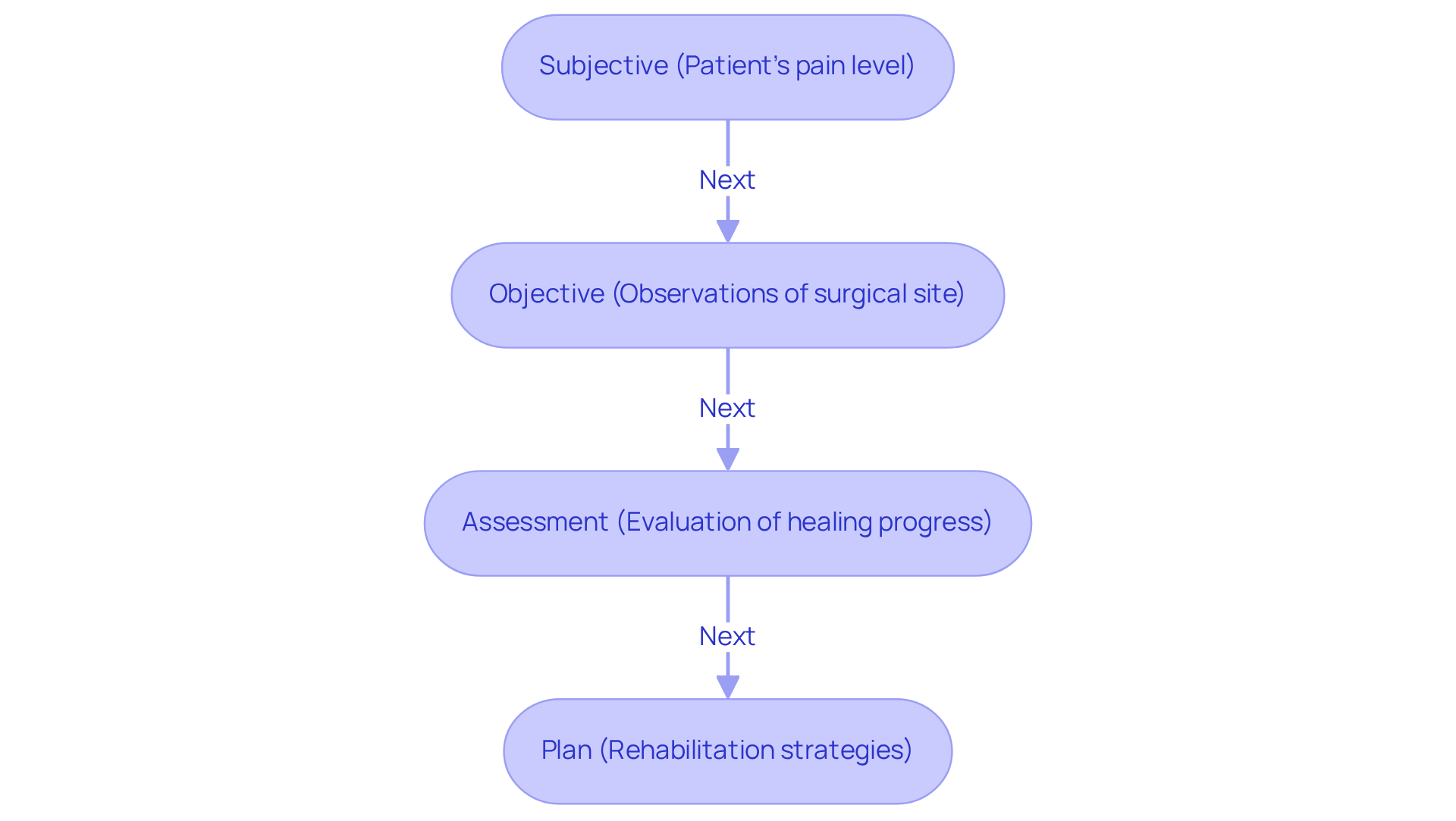
Orthopedic Surgery SOAP Note Example: Documenting Surgical and Recovery Processes
An orthopedic surgery SOAP document plays a crucial role in capturing the surgical procedure conducted, the individual's subjective pain reports, an evaluation of recovery progress, and a detailed rehabilitation plan. For instance, a note might reflect that the individual reports pain at a level of 6/10 (Subjective), the surgical site appears clean with no signs of infection (Objective), the individual is healing as expected (Assessment), and the plan includes physical therapy sessions twice a week (Plan). This organized record is essential for efficiently monitoring recovery, fostering communication among healthcare professionals, and ensuring suitable follow-up support.
Thorough records after surgery not only assist in tracking recovery but also enhance the overall quality of service provided. By integrating organized SOAP records, practices can experience considerable improvements in record-keeping efficiency. In fact, those utilizing AI Medical Scribes report 75% quicker reporting. Imagine how much more time you could spend caring for your patients!
Innovative AI solutions, such as CosmaNeura's Agentic Platform, help healthcare providers alleviate administrative burdens, allowing them to focus more on what truly matters—caring for individuals. To enhance your documentation practices, consider adopting , such as a nurse practitioner soap note example, that align with current healthcare standards.
Key Components of an Orthopedic Surgery SOAP Note:
- Subjective: Patient's pain level and personal reports.
- Objective: As recorded in a nurse practitioner soap note example, observations of the surgical site and any physical assessments.
- Assessment: Evaluation of the patient's healing progress as illustrated in a nurse practitioner soap note example.
- Plan: Outline of rehabilitation strategies, including a nurse practitioner soap note example that details the frequency of therapy sessions.
Pediatric SOAP Note Example: Tailoring Documentation for Young Patients
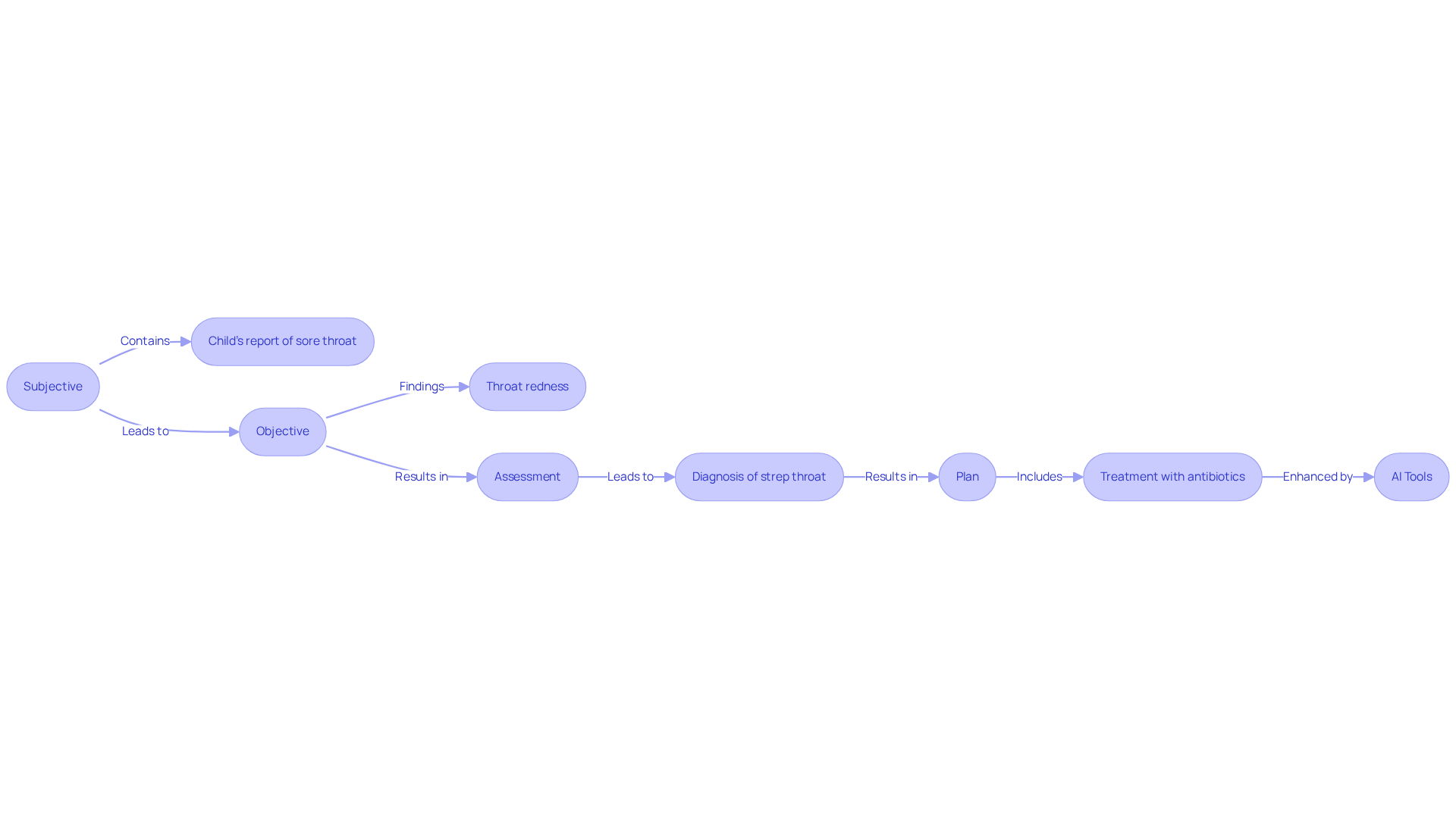
In the world of pediatric care, healthcare providers often face emotional challenges when addressing the health needs of children. An effective nurse practitioner soap note example for a pediatric record must capture these nuances, encompassing subjective complaints, objective findings from physical examinations, assessments of developmental milestones, and follow-up plans. For instance, a nurse practitioner soap note example might detail a child's report of a sore throat (Subjective), followed by an examination revealing throat redness (Objective), a diagnosis of strep throat (Assessment), and a treatment plan including antibiotics (Plan).
This organized method not only tackles the particular health issues of young patients but also enhances the overall . By concentrating on these customized elements, healthcare providers can ensure that records reflect the unique developmental and health aspects relevant to children. Have you considered how administrative burdens can impact patient care?
Moreover, utilizing AI resource platforms, such as automated record-taking tools and growth tracking applications, can simplify the process of creating organized clinical records and monitoring developmental milestones. This ultimately enhances efficiency and precision in pediatric treatment. Effective SOAP documentation, such as a nurse practitioner soap note example, not only improves communication among healthcare professionals but also aids in achieving better outcomes for individuals, ensuring that children receive the best possible care.
To improve documentation methods, healthcare professionals should think about incorporating AI tools that assist in monitoring growth milestones and creating immunization reminders. This highlights the significance of thorough records in pediatric healthcare. By embracing these innovative solutions, we can nurture a more effective and compassionate approach to caring for our youngest patients.
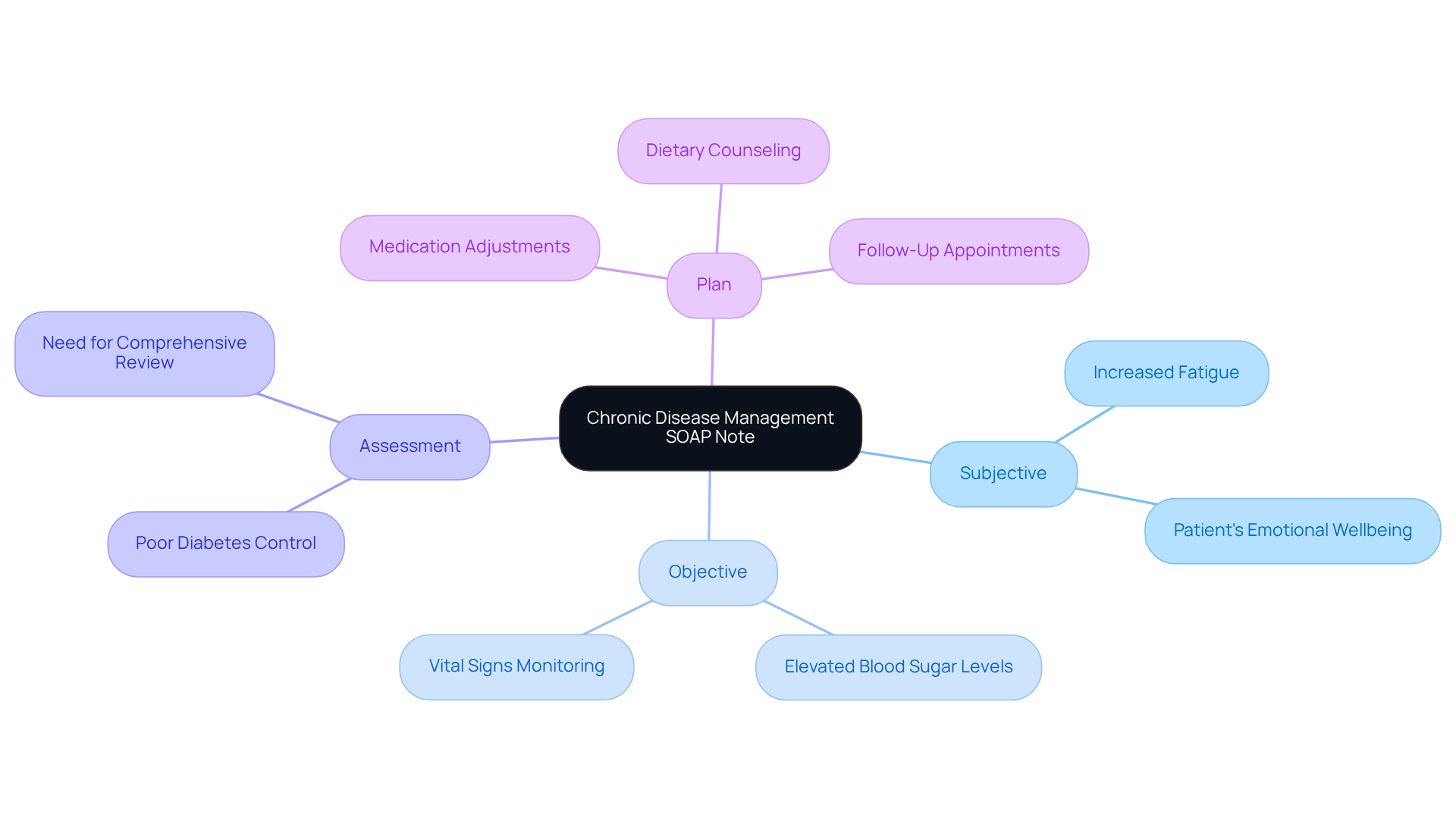
Chronic Disease Management SOAP Note Example: Tracking Patient Outcomes Over Time
A nurse practitioner soap note example for chronic disease management is not merely a formality; it is essential for capturing a comprehensive view of an individual's health. It should encompass the individual's subjective accounts of symptoms, objective lab results, an evaluation of disease control, and a plan for ongoing management. For instance, a nurse practitioner soap note example might detail that the individual reports increased fatigue (Subjective), recent lab results indicate elevated blood sugar levels (Objective), the assessment reveals poor diabetes control (Assessment), and the plan includes medication adjustments along with dietary counseling (Plan).
Imagine the relief healthcare providers can feel when utilizing AI algorithms to examine extensive volumes of medical data. These tools can analyze individual history and test outcomes, aiding in making precise diagnoses and developing customized treatment plans. AI enhances the subjective component by identifying patterns in patient-reported symptoms. It improves the objective section by analyzing lab results for trends, informs the assessment through predictive analytics, and optimizes the plan by suggesting tailored interventions.
This information is crucial for efficiently managing chronic conditions. It empowers healthcare providers to track changes over time, modify treatment plans as needed, and ultimately enhance outcomes for individuals. Frequent updates in a nurse practitioner soap note example not only improve communication among treatment teams but also ensure that all members are aligned on the individual's health status and interventions. This reinforces the significance of in chronic disease management.
How can we ensure that we are fully supporting our patients in their journeys? By embracing these practices, we can cultivate a more compassionate approach to care, ultimately leading to better health outcomes.
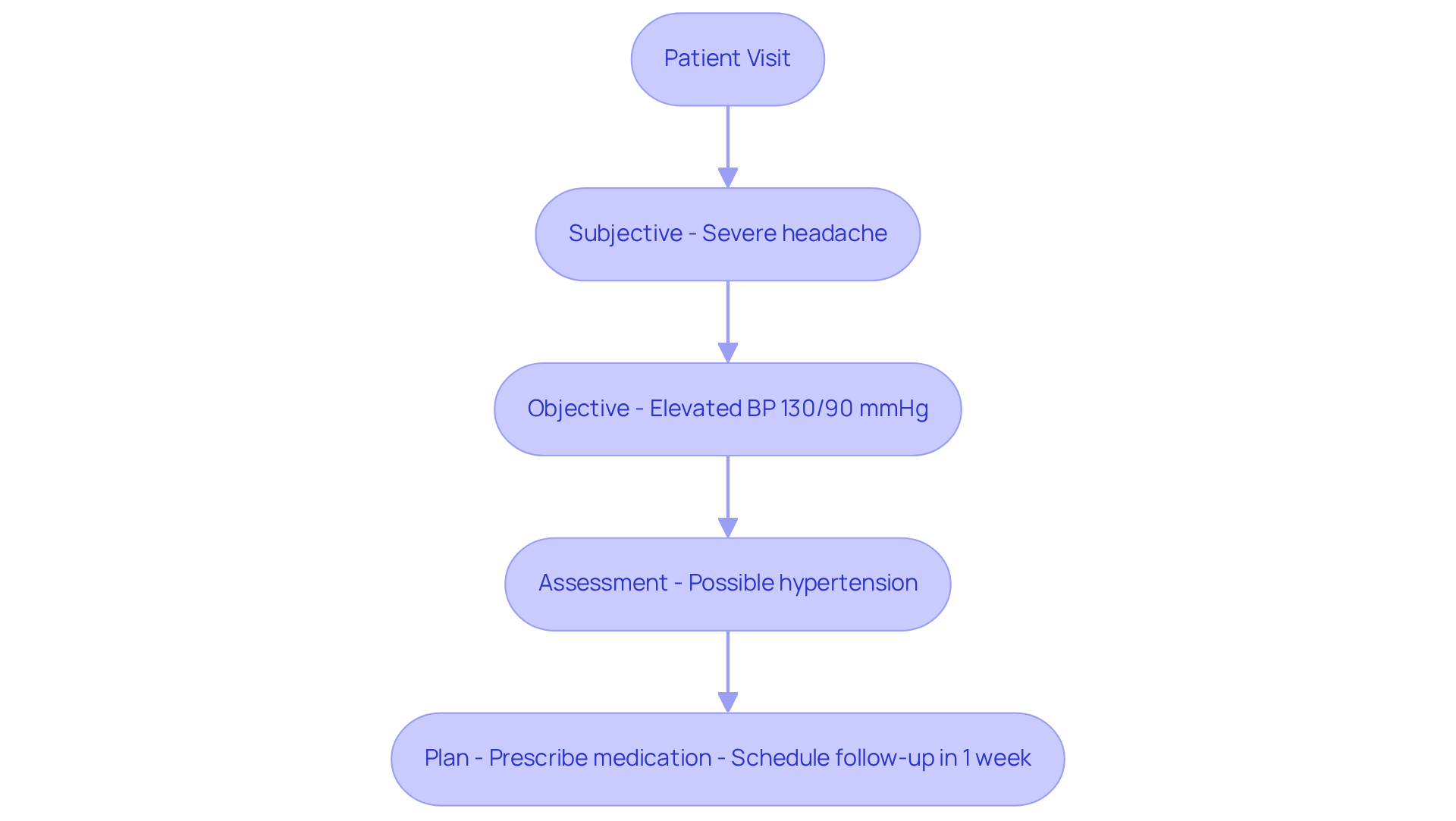
Urgent Care SOAP Note Example: Efficiently Documenting Acute Patient Visits
In urgent treatment, healthcare providers often face overwhelming emotional challenges. An effective [nurse practitioner SOAP note example](https://npchartingschool.com/examples-of-a-soap-note) must quickly summarize the individual's subjective complaints, objective findings from the examination, an assessment of the condition, and a treatment plan. For instance, imagine an individual reporting a severe headache (Subjective), with a physical examination showing elevated blood pressure at 130/90 mmHg (Objective). The assessment could indicate possible hypertension, while the plan might include prescribing medication and scheduling a follow-up in one week.
This is crucial. Prompt record-keeping can greatly improve efficiency in urgent care environments, enabling providers to concentrate on delivering quality care. Best practices indicate that the nurse practitioner SOAP note example ought to be finalized swiftly, preferably within 24 hours of the client interaction, to ensure precision and adherence to billing regulations. Have you noticed how organized templates can decrease record-keeping time by as much as 35%? This allows for more time dedicated to client interactions.
By incorporating generative AI solutions like CosmaNeura's Agentic Platform, healthcare professionals can automate elements of record-keeping, further enhancing efficiency and alleviating administrative burdens that contribute to physician burnout. Medwriter's voice recognition technology can save time by automatically transcribing visits, allowing for seamless documentation.
By following these practices and utilizing innovative AI tools, healthcare professionals can improve communication, ensure continuity of support, and enhance overall outcomes for individuals. Let's embrace these solutions together for a more compassionate and efficient healthcare experience.
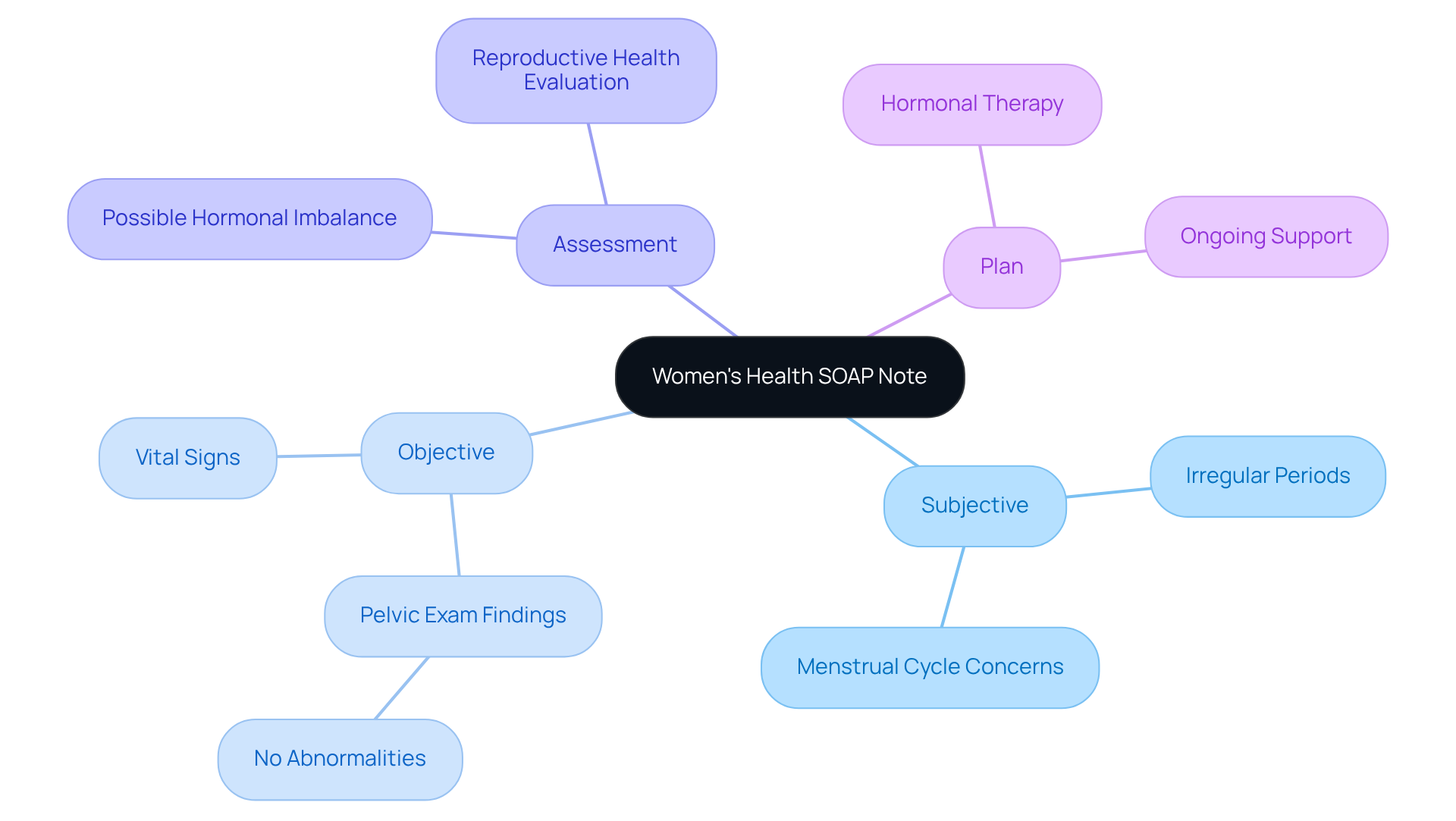
Women's Health SOAP Note Example: Comprehensive Documentation for Female Patients
A comprehensive women's health nurse practitioner soap note example is essential for addressing the unique challenges that women face. It should include:
- Subjective accounts regarding menstrual cycles
- Objective results from gynecological exams
- A thorough evaluation of reproductive health
- A detailed plan for ongoing support
For instance, a nurse practitioner soap note example could include documenting an individual's report of irregular periods (Subjective), findings from a pelvic exam that reveal no abnormalities (Objective), an assessment suggesting a possible hormonal imbalance (Assessment), and a plan that includes hormonal therapy (Plan). This meticulous approach not only acknowledges the specific health needs of women but also significantly enhances their overall health outcomes.
As specialists in the area, including Dr. Beth Garner, emphasize, effective record-keeping is vital for building trust and ensuring that support is tailored to each individual. This ultimately leads to and health outcomes. It's important to recognize that it can take up to 17 years for new evidence to be integrated into standard clinical practice. This highlights the necessity of thorough documentation in keeping women's health practices current and evidence-based.
Moreover, incorporating diverse viewpoints and experiences in clinical trials, as advocated by Linda Goler Blount, is crucial for improving health outcomes. It ensures that services are attentive to the distinct needs of women. How can we, as healthcare providers, ensure that we are meeting these needs effectively? By fostering an environment of understanding and support, we can make a meaningful impact on women's health.
Geriatric SOAP Note Example: Documenting Complex Health Needs in Older Adults
A geriatric SOAP record must compassionately encapsulate the individual's subjective complaints, objective findings from thorough assessments, an evaluation of overall health status, and a strategic plan for ongoing treatment. For instance, a nurse practitioner soap note example may document that the individual reports heightened confusion (Subjective), cognitive evaluations suggest mild dementia (Objective), the assessment identifies a need for memory support (Assessment), and the plan encompasses referrals to specialists and family counseling (Plan). This thorough record-keeping is essential for addressing the complex health requirements of older adults. It not only assists in clinical decision-making but also fosters improved communication among providers.
Geriatric support specialists emphasize that using a nurse practitioner soap note example can significantly enhance patient outcomes. By ensuring that all aspects of a patient's health are considered and addressed, these notes ultimately lead to more personalized and effective treatment strategies. Considering that approximately 20% of men and 30% of women aged 65 and above presently require assistance with at least one Activity of Daily Living (ADL), the importance of comprehensive record-keeping becomes even more apparent.
Addressing the physical, social, and psychological challenges faced by older adults underscores the necessity of effective documentation in geriatric care. Have you considered how your documentation practices impact your patients' experiences? Reflecting on this can guide us toward more compassionate care. Together, we can ensure that every older adult receives the they deserve.
Conclusion
In the realm of healthcare, the significance of effective documentation is profound, especially for nurse practitioners. Have you ever felt overwhelmed by paperwork? This article highlights the transformative potential of utilizing structured SOAP notes across various specialties, showcasing how these notes can enhance patient care. By integrating AI-driven solutions like CosmaNeura, healthcare providers can alleviate administrative burdens, allowing them to dedicate more time to patient interactions rather than paperwork.
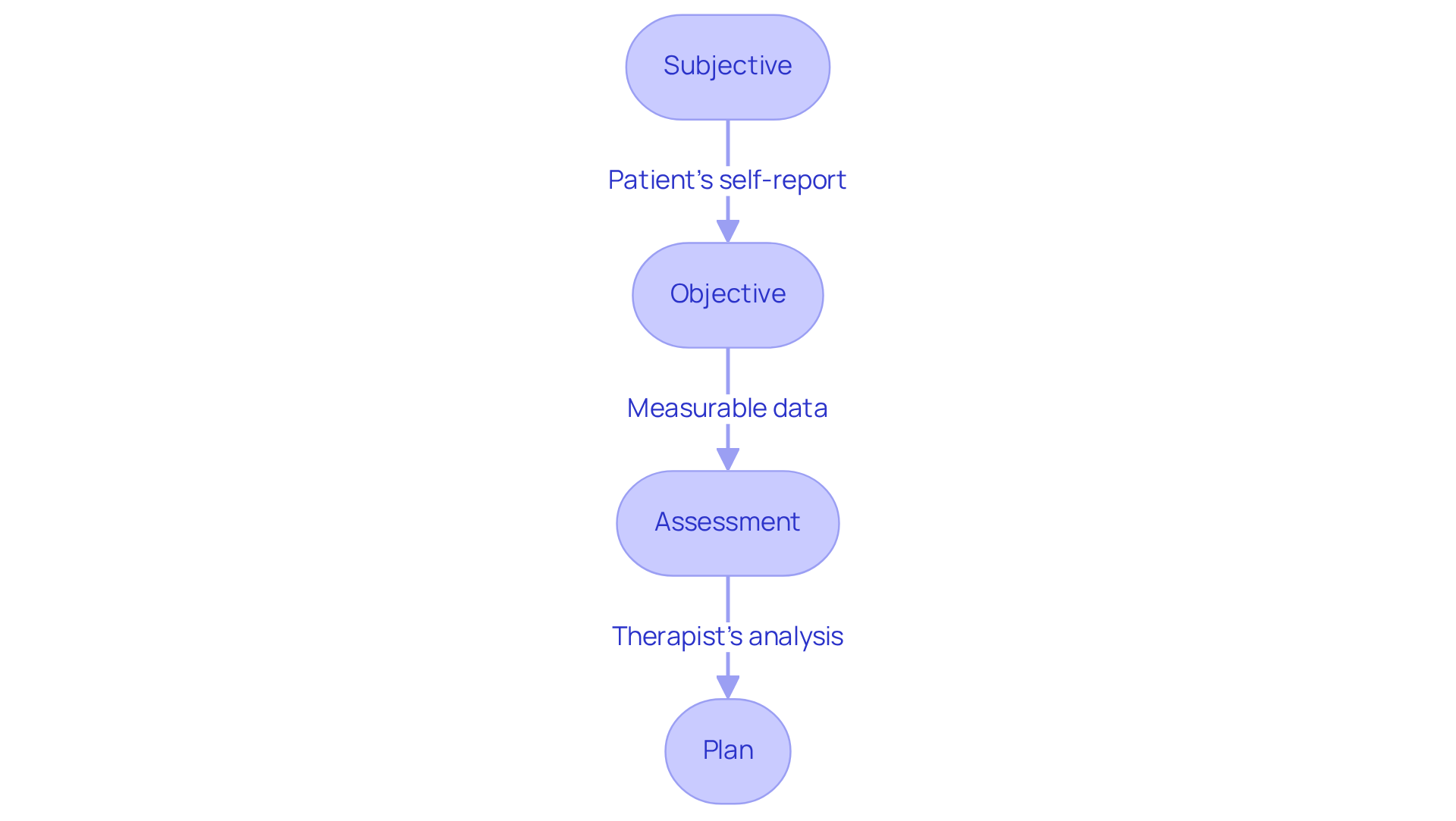
Throughout our discussion, we explore key examples from mental health to geriatrics, illustrating the diverse applications of SOAP notes. Each specialty presents unique challenges, yet the structured approach of SOAP—Subjective, Objective, Assessment, and Plan—ensures comprehensive documentation that fosters clear communication among healthcare teams. Best practices, such as timely record finalization and adopting electronic health record systems, can dramatically improve efficiency and accuracy in patient care.
Ultimately, embracing innovative documentation practices and AI technologies is essential for modern healthcare. By prioritizing effective SOAP note practices, healthcare professionals can enhance their workflow and improve patient outcomes. As the healthcare landscape evolves, let us commit to compassionate, efficient care, ensuring that every patient receives the attention and support they deserve.




