Overview
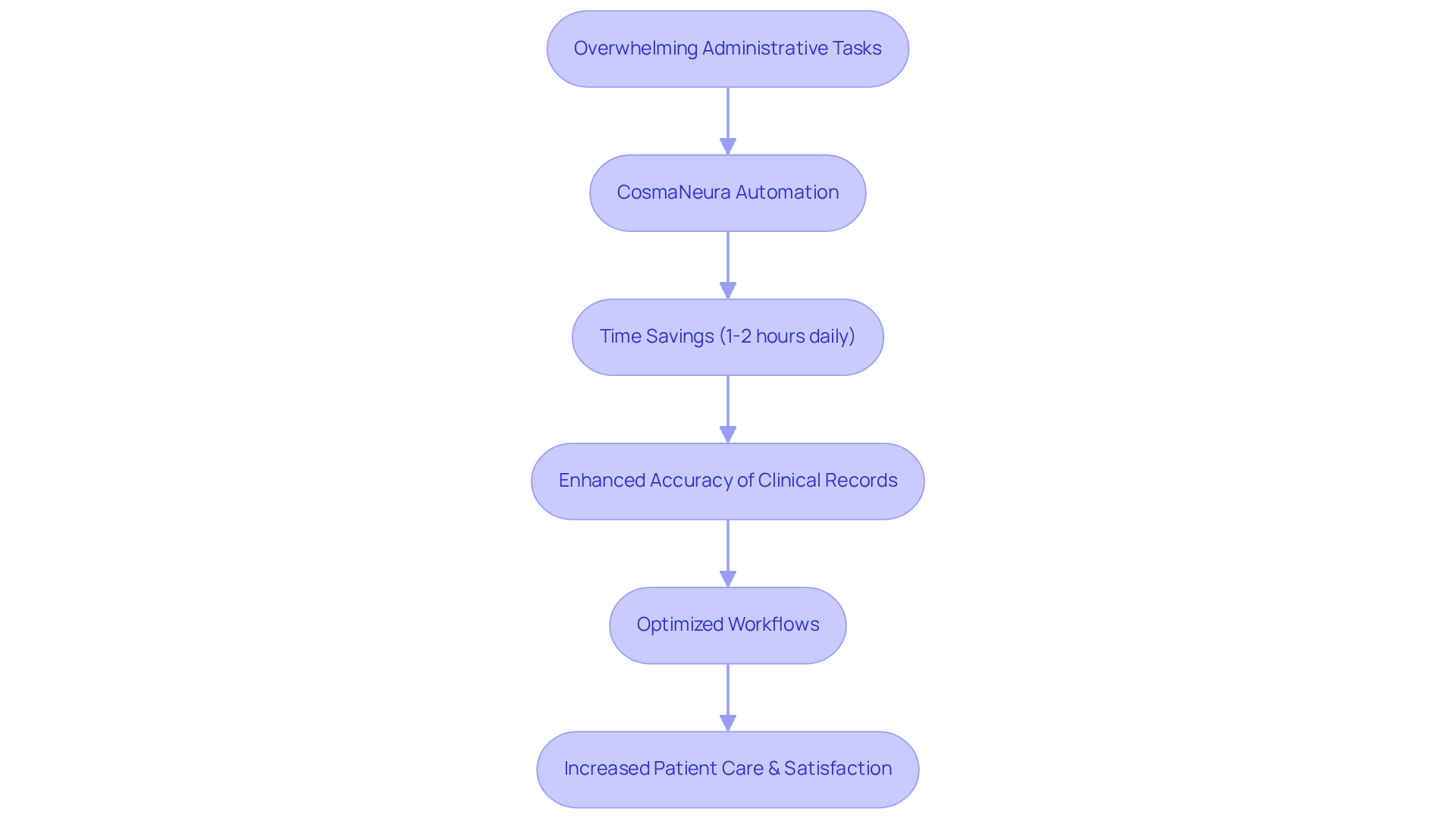
In today's fast-paced healthcare environment, many nurses face overwhelming administrative burdens that can detract from their ability to provide compassionate patient care. How often have you felt the weight of documentation pressing down on your time and energy? This is where nursing SOAP notes come into play, offering a structured approach to documentation that not only organizes information but also enhances the quality of care.
With innovative solutions like CosmaNeura, the process of note-taking can be automated. Imagine saving precious time and improving the accuracy of clinical records—all while ensuring that you can focus more on what truly matters: your patients. By integrating AI-driven technology, we can alleviate some of the stress that comes with documentation, allowing for a more nurturing and attentive approach to patient care.
Ultimately, this shift not only benefits healthcare providers but also leads to better health outcomes for patients. The ability to dedicate more time and attention to those in our care is invaluable. Let’s embrace these advancements together, ensuring that we can continue to provide the empathetic and high-quality care that every patient deserves. How might these tools transform your daily practice and enhance the connections you build with your patients?
Introduction
In the intricate landscape of healthcare, nurses often grapple with the emotional weight of balancing patient care and extensive documentation. This dual demand can feel overwhelming, as the precious time spent on administrative tasks detracts from the compassionate care they wish to provide. The emergence of AI-driven solutions, like CosmaNeura, presents a transformative opportunity to alleviate this burden, allowing nurses to reclaim valuable moments for their patients.
Yet, amidst this drive for efficiency, the critical importance of well-structured SOAP notes remains paramount. These notes are essential for ensuring effective communication and continuity of care.
So, how can healthcare professionals strike a balance between the need for speed and the meticulousness required for accurate documentation? This article explores ten compelling examples of nursing SOAP notes that not only enhance patient care but also illuminate best practices for overcoming common documentation challenges. Together, we can navigate this intricate landscape with empathy and understanding.
CosmaNeura: AI-Driven SOAP Note Automation for Nurses
In the demanding world of healthcare, nurses often face overwhelming administrative tasks that can detract from their ability to provide compassionate care. CosmaNeura understands these emotional challenges and offers a solution that automates the generation of nursing soap note examples, which significantly simplifies the record-keeping process. By integrating real-time data collection and analysis, this platform empowers nurses to effectively document their interactions with individuals, ensuring that the standard of service remains intact.
Imagine saving 1-2 hours daily—time that can be redirected towards patient care. This automation not only conserves precious time but also enhances the accuracy of clinical records. By optimizing workflows and providing clear guidelines for record-keeping, as shown in a nursing soap note example, medical providers can focus more on delivering empathetic support. This shift ultimately leads to improved outcomes and greater satisfaction for those receiving treatment.
With 73% of medical professionals reporting documentation burnout, the efficiency achieved through is essential in alleviating this prevalent issue. It enables nurses to concentrate on what truly matters: the well-being of those they serve. How might your day change if you could spend more time caring for your patients? Embrace the support that technology can provide and take a step toward reclaiming your time and compassion in nursing.
Understanding SOAP Notes: Importance in Nursing Practice
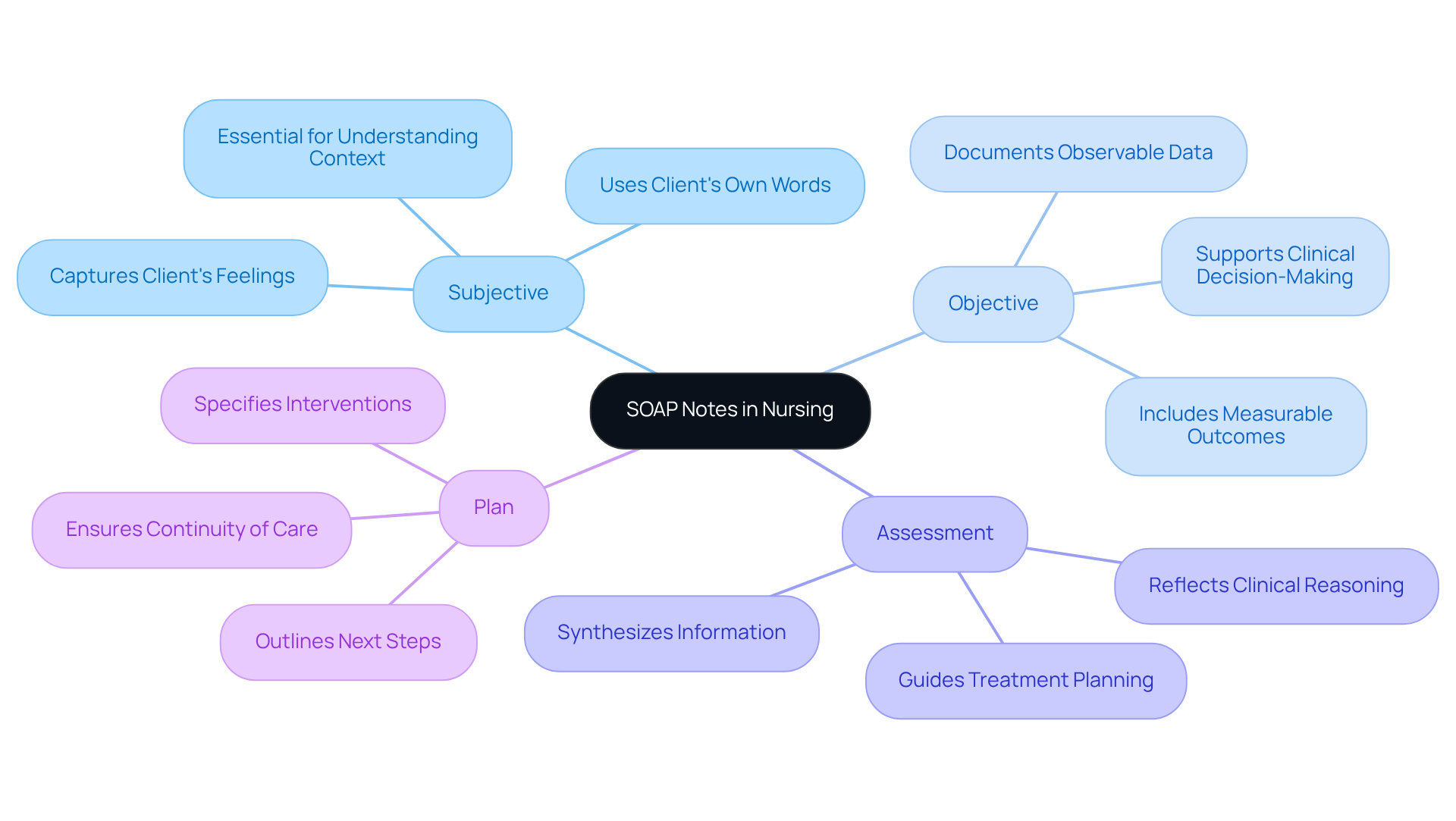
An example of nursing soap notes—Subjective, Objective, Assessment, and Plan—plays a vital role in nursing practice. They provide a structured way to document client information, fostering collaboration among medical professionals. This teamwork is crucial, especially when faced with challenges like limited access to care and rising costs. Have you ever felt overwhelmed by these hurdles? Innovative AI solutions, such as CosmaNeura's Agentic Platform, can significantly enhance the effectiveness of SOAP notes.
Research shows that miscommunication in medical records can lead to serious errors, with studies indicating that up to 80% of severe clinical mistakes stem from miscommunication during transitions of care. By integrating generative AI into documentation, healthcare professionals can alleviate administrative burdens, allowing them to focus more on what truly matters—patient care. Imagine the peace of mind that comes from knowing your documentation is accurate and efficient.
Well-crafted SOAP notes not only enhance safety but also . They provide a clear record of clinical reasoning and decision-making, which is essential for effective care. Experts emphasize that the organized format of SOAP notes promotes clarity, enabling nurses to concisely record vital client details and enhance collaboration among multidisciplinary teams.
By utilizing a nursing soap note example effectively, especially with innovative technologies, healthcare professionals can significantly enhance client outcomes and ensure continuity of care. It’s essential to review SOAP notes for precision, as even minor errors can lead to significant consequences for patient care. Let’s work together to embrace these tools and enhance our practice, ensuring that every client receives the compassionate care they deserve.
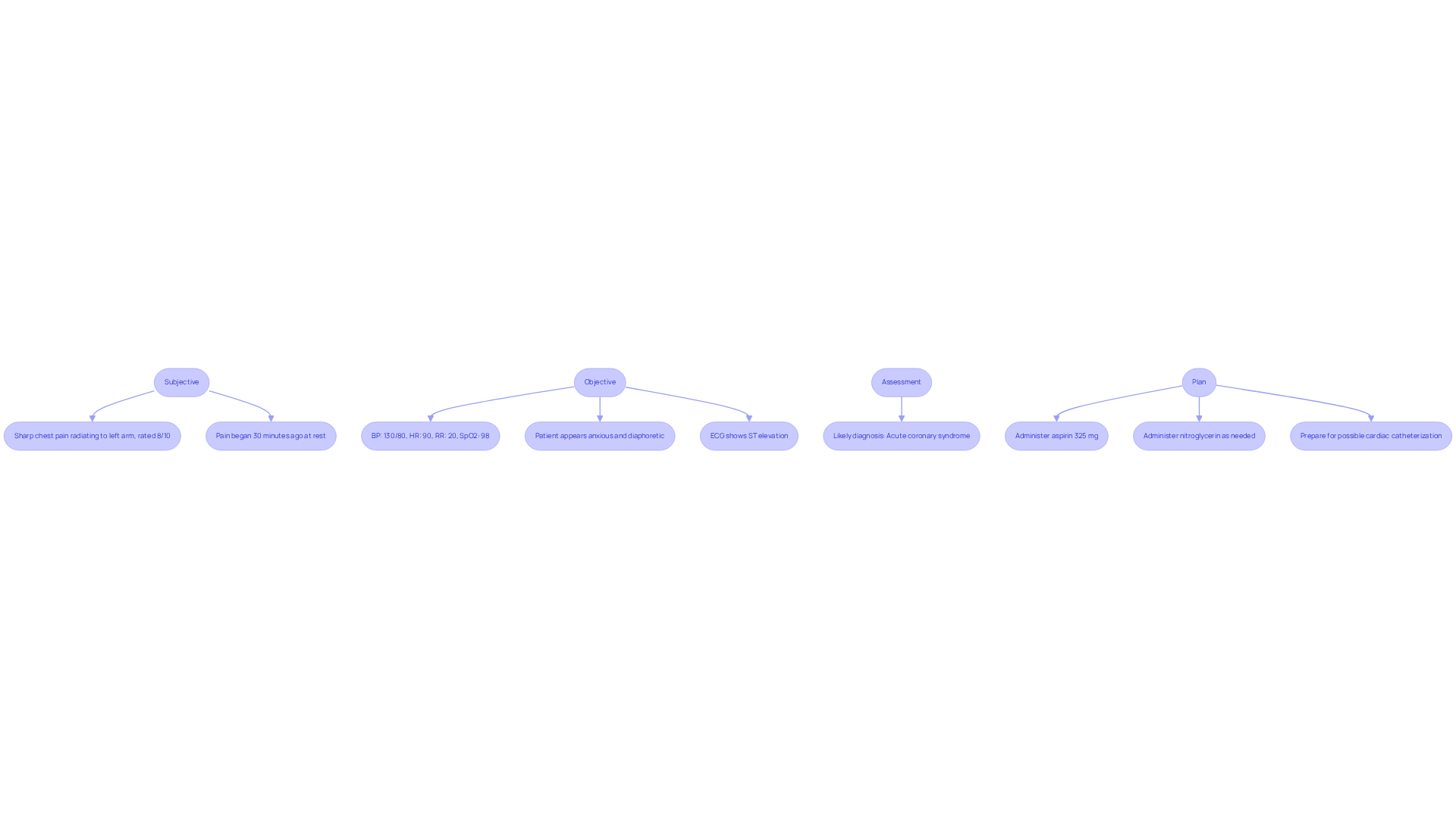
Example 1: SOAP Note for a Patient with Chest Pain
Subjective: The patient shares a distressing experience of sharp chest pain radiating to the left arm, which they rate as an 8 out of 10. They mention that the pain began just 30 minutes ago while they were at rest, highlighting the suddenness of their discomfort.
Objective: Vital signs show BP at 130/80, HR at 90, RR at 20, and SpO2 at 98%. The patient appears anxious and diaphoretic, indicating their distress. An ECG reveals ST elevation, which is concerning.
Assessment: Given the patient’s chest pain presentation and the ECG findings, the nursing soap note example would suggest that acute coronary syndrome is likely, and it’s crucial to address this promptly.
Plan: To provide relief and support, we will 325 mg and nitroglycerin as needed. Additionally, we will prepare for possible cardiac catheterization to ensure the best possible outcome for the patient.
Example 2: SOAP Note for a Patient with Diabetes Management
Subjective: The individual shares feelings of fatigue, increased thirst, and frequent urination over the past week, while expressing relief at not having experienced any recent illness.
Objective: Vital signs are stable, with BP at 120/70, HR at 78, and weight remaining unchanged. However, the blood glucose level is elevated at 250 mg/dL, and the foot exam shows no lesions.
Assessment: It appears that the individual is struggling with poorly controlled diabetes mellitus, likely due to challenges in adhering to the prescribed medication regimen. It's important to recognize that average only 50-60% and often decline over time, which can lead to less than optimal health outcomes.
Plan: We must emphasize the vital role of medication adherence in the context of a nursing soap note example. As Cindy Nee, PharmD, wisely states, "Medications can only work if they are taken!" To support this, let’s schedule a follow-up appointment in one month to reassess and adjust the insulin dosage if necessary. Additionally, incorporating educational strategies into each interaction is crucial for addressing barriers to adherence, such as cost and complexity of the regimen. These strategies are essential for enhancing overall diabetes management.
Encouraging providers to routinely assess medication adherence during patient encounters can foster a more supportive environment, ultimately leading to better health outcomes.
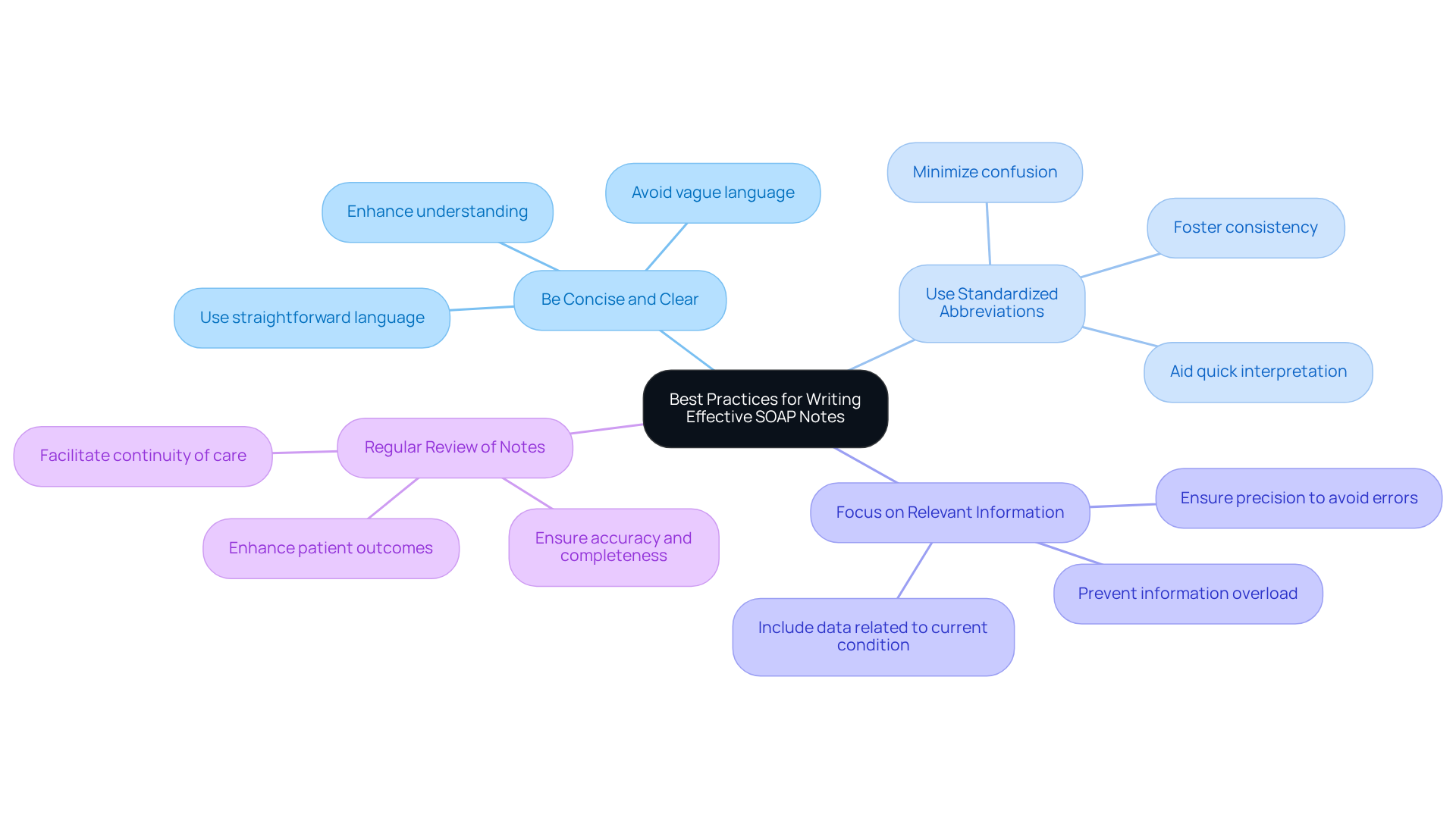
Best Practices for Writing Effective SOAP Notes
- Be Concise and Clear: It's vital to use straightforward language to effectively convey information. This approach not only enhances understanding but also ensures that critical details are communicated without ambiguity. Can we avoid vague language such as 'may' or 'seems' in notes to maintain clarity?
- Use Standardized Abbreviations: Implementing standardized abbreviations fosters consistency and clarity across documentation. This practice minimizes confusion and aids in the quick interpretation of notes by various healthcare professionals, making our communication more effective.
- Focus on Relevant Information: Concentrate on including only data related to the individual's current condition and treatment plan. This targeted approach prevents information overload and allows for more effective clinical decision-making. Remember, inadequate records can lead to medication mistakes and fatalities, underscoring the necessity for precision in our work.
- Regularly reviewing nursing soap note examples for accuracy and completeness is essential. This practice ensures that records accurately reflect the patient's status and facilitates continuity of care, ultimately enhancing patient outcomes. Continuous education in record-keeping practices significantly boosts quality, so let's prioritize this for our growth. Utilizing electronic systems for record-keeping has been shown to increase the chances of by 2.2 times, further improving our efficiency in providing care.
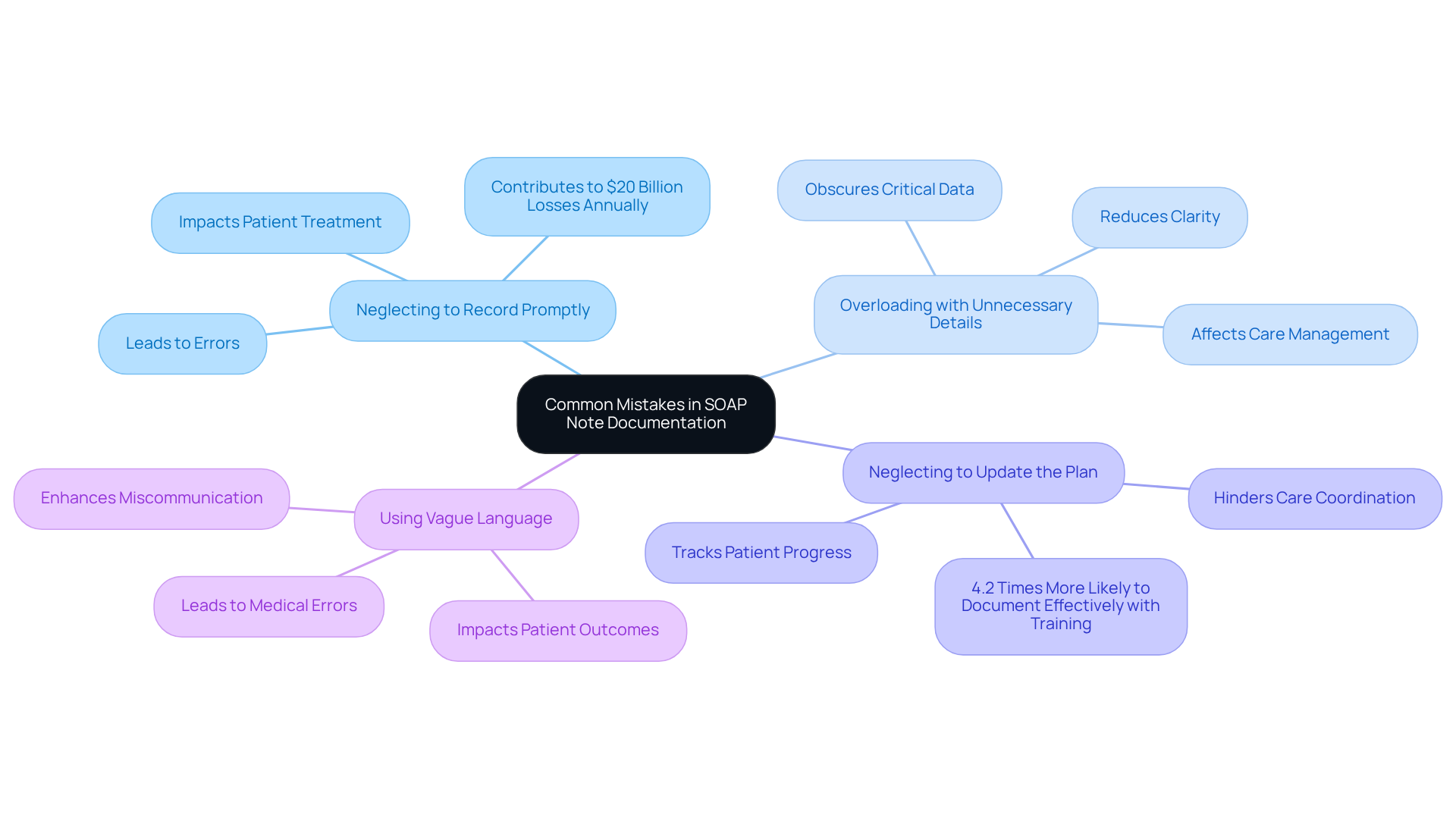
Common Mistakes to Avoid in SOAP Note Documentation
- Neglecting to Record Promptly: Have you ever felt the weight of postponed recording? It can lead to errors and overlooked details that jeopardize patient treatment. Timely entries are essential; they ensure that all relevant details are captured, supporting and continuity of care. It's concerning to note that medical errors, often stemming from poor documentation practices, contribute to approximately $20 billion in losses each year.
- Overloading with Unnecessary Details: Including irrelevant information can obscure critical data. How often do we find ourselves sifting through unnecessary details? By concentrating on relevant information that directly influences care management, we can improve clarity and effectiveness. As specialists remind us, an accurate nursing soap note example functions as a dependable source of client information.
- Neglecting to Update the Plan: Is your care plan reflecting the current state of your patient’s condition? Regular updates are crucial, facilitating better care coordination and helping to track patient progress. Health professionals trained in routine practice records are 4.2 times more likely to record effectively, underscoring the importance of ongoing education in this area.
- Using Vague Language: Specificity is key in documentation. Are we using clear language to describe our patients’ conditions? Avoiding ambiguous terms enhances communication among healthcare providers, contributing to better outcomes for individuals. Inadequate documentation practices can lead to medical errors and individual mortality worldwide, highlighting the necessity for accurate language.
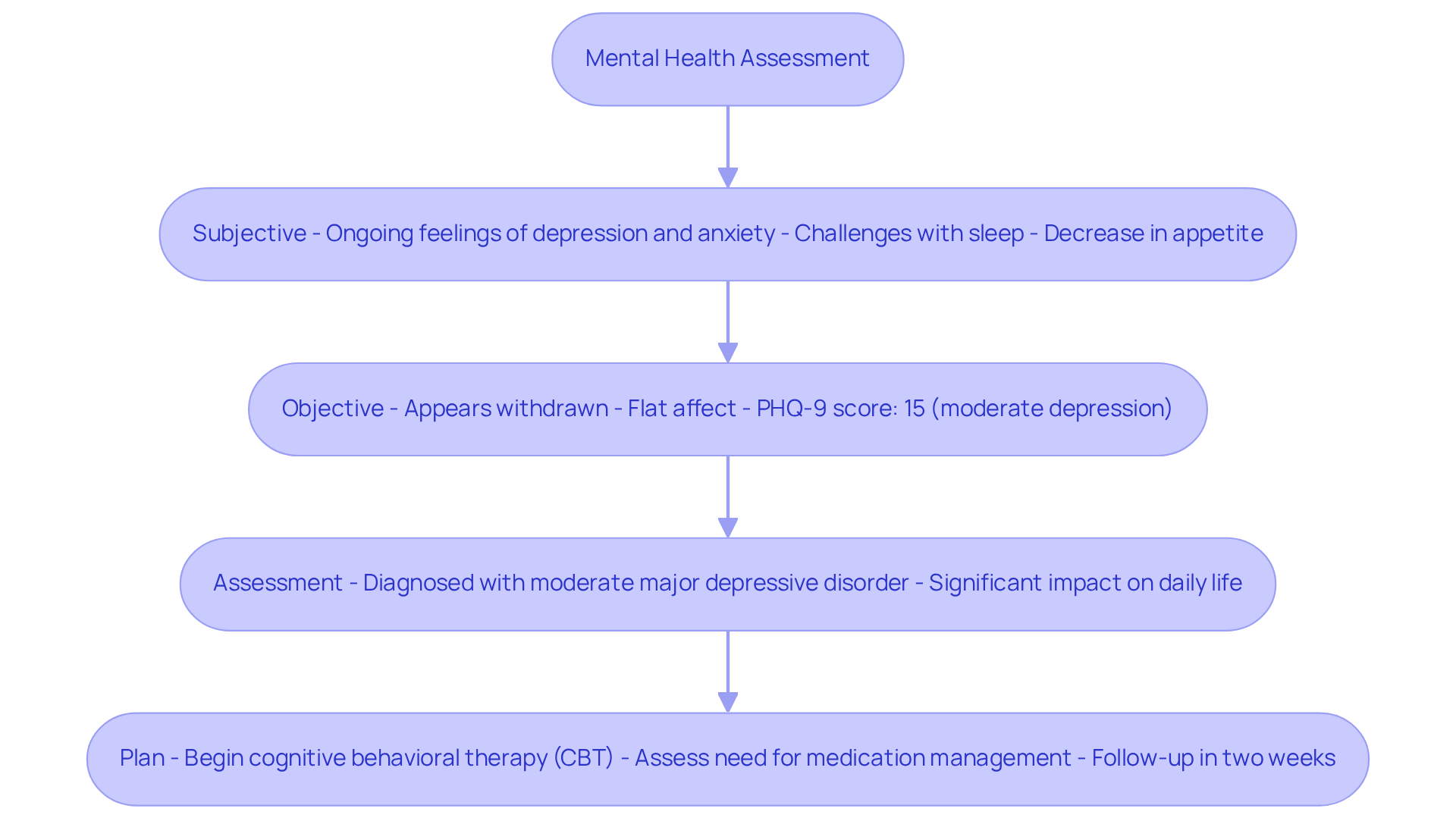
Example 3: SOAP Note for a Mental Health Assessment
Subjective: The individual shares ongoing feelings of depression and anxiety, alongside challenges with sleep and a noticeable decrease in appetite over the past two weeks.
Objective: The individual appears withdrawn, showing a flat affect. Importantly, there are no signs of suicidal ideation. The PHQ-9 score stands at 15, indicating moderate depression.
Assessment: The individual is diagnosed with moderate major depressive disorder, highlighting the significant impact of these symptoms on daily life.
Plan: Begin cognitive behavioral therapy (CBT) as the primary intervention, assess the need for medication management, and schedule a follow-up appointment in two weeks to monitor progress and adjust the treatment plan as needed.
Accurate records in mental health services are vital, as they not only foster effective communication among healthcare professionals but also act as a [nursing soap note example](https://blog.cosmaneura.com/10-essential-soap-notes-templates-for-healthcare-providers) to ensure that treatment strategies are tailored to the individual's evolving needs. With major depressive disorder affecting approximately 7% of adults in the U.S., understanding how to through a nursing soap note example is crucial to improve outcomes. As John Green wisely stated, 'We need never be hopeless, because we can never be irreparably broken.' This underscores the importance of approaching mental health challenges with compassion and understanding.
Moreover, the stigma surrounding mental illness can hinder individuals from seeking help, making precise documentation even more critical in providing appropriate support. Consider utilizing resources such as the Positive Psychology Toolkit©, which offers valuable exercises and interventions to aid in mental health management. Healthcare providers should also remain aware of available resources for suicide prevention and mental health support, ensuring they can guide individuals toward the assistance they need.
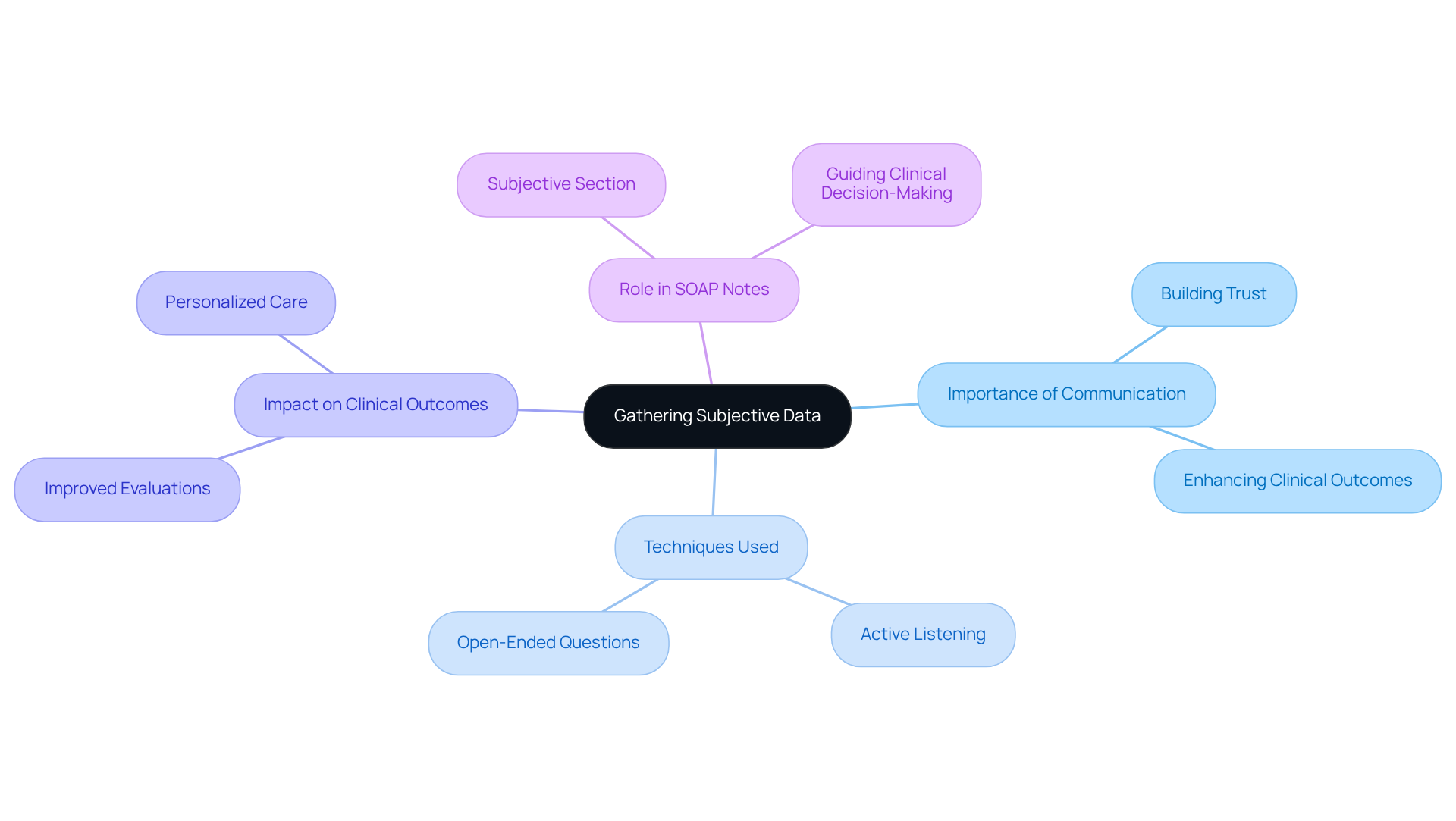
Gathering Subjective Data: Key to Effective SOAP Notes
Collecting subjective information is crucial for providing effective care. It requires healthcare providers to actively listen and engage individuals through open-ended questions. This compassionate approach not only uncovers the individual's emotions, experiences, and concerns but also builds trust, encouraging them to share vital information.
Have you ever noticed how effective communication can transform an interaction? Research shows that using effective communication techniques significantly enhances the quality of interviews, leading to improved clinical outcomes. When healthcare providers prioritize communication, they and treatment strategies.
In the context of a nursing soap note example, the Subjective section plays a vital role in documenting these insights. It informs the Assessment and Plan sections, guiding clinical decision-making. By mastering these communication skills, healthcare providers can capture a comprehensive view of the individual's health. This is essential for delivering personalized and effective support.
Remember, every interaction is an opportunity to connect and understand better. How can you enhance your communication skills today?
Documenting Objective Data: Enhancing SOAP Note Accuracy
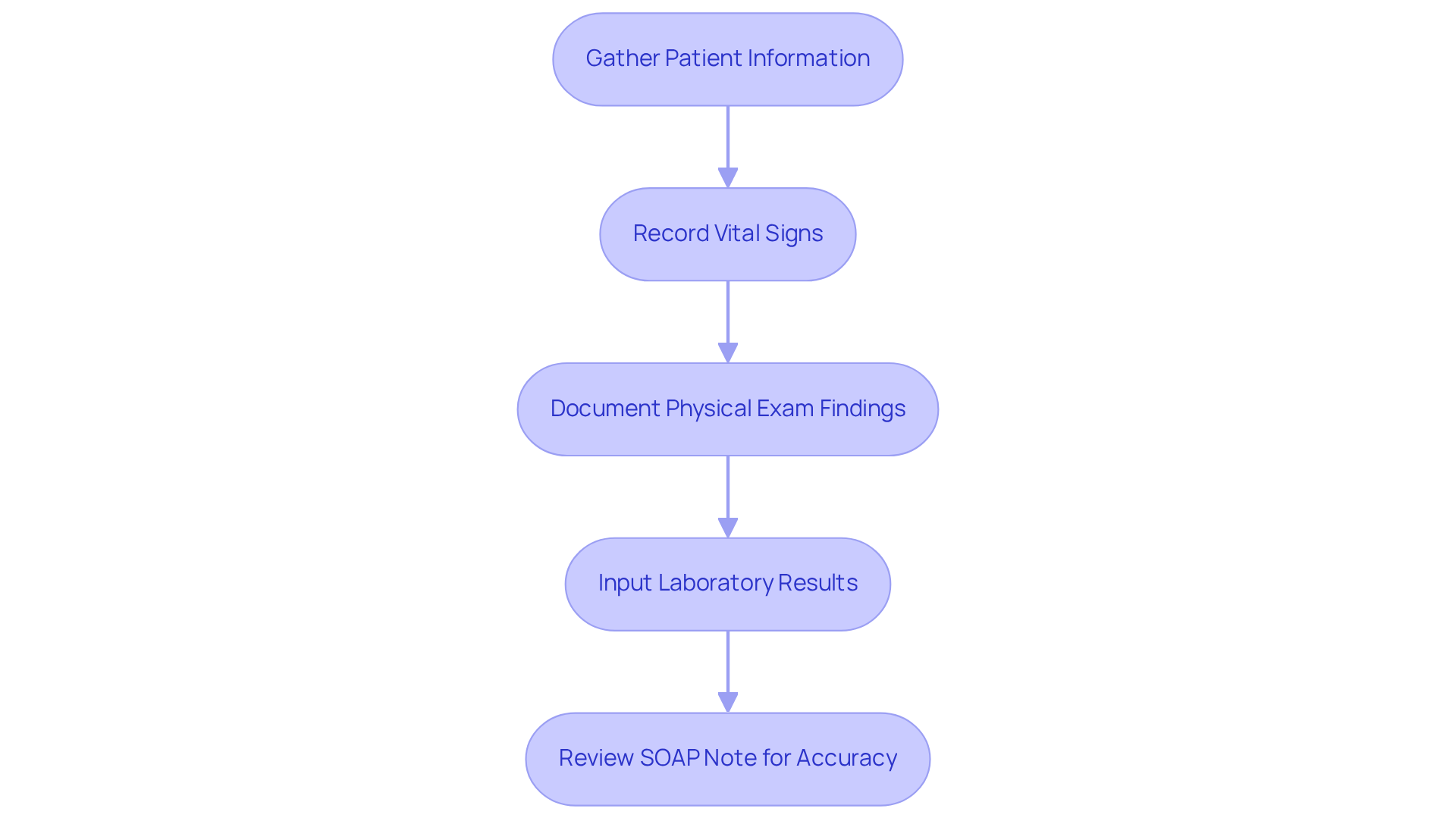
Documenting [objective data is essential](https://nevadastate.edu/son/rn-bsn/understanding-the-role-of-subjective-vs-objective-nursing-data) in providing compassionate care. It involves recording measurable and observable information, such as vital signs, physical examination findings, and laboratory results. Have you ever felt overwhelmed by the administrative tasks that can distract from patient care? Recording this data precisely and promptly is crucial, as it reflects the individual's current condition and supports informed decision-making.
Utilizing a along with standardized formats and terminology not only enhances the clarity of the documented information but also makes it more useful for all involved in patient care. By streamlining this process, we can alleviate some of the burdens faced by healthcare providers, allowing more time to focus on what truly matters—caring for patients. Remember, each piece of data contributes to a fuller understanding of the patient's needs.
As you navigate the complexities of documentation, consider how utilizing a nursing soap note example can enhance both your efficiency and the quality of care you provide. Embracing these strategies fosters a supportive environment, ensuring that every patient feels valued and understood. Let's work together to create a system that prioritizes compassionate care through meticulous documentation.
Creating a Comprehensive Plan: The Final Component of SOAP Notes
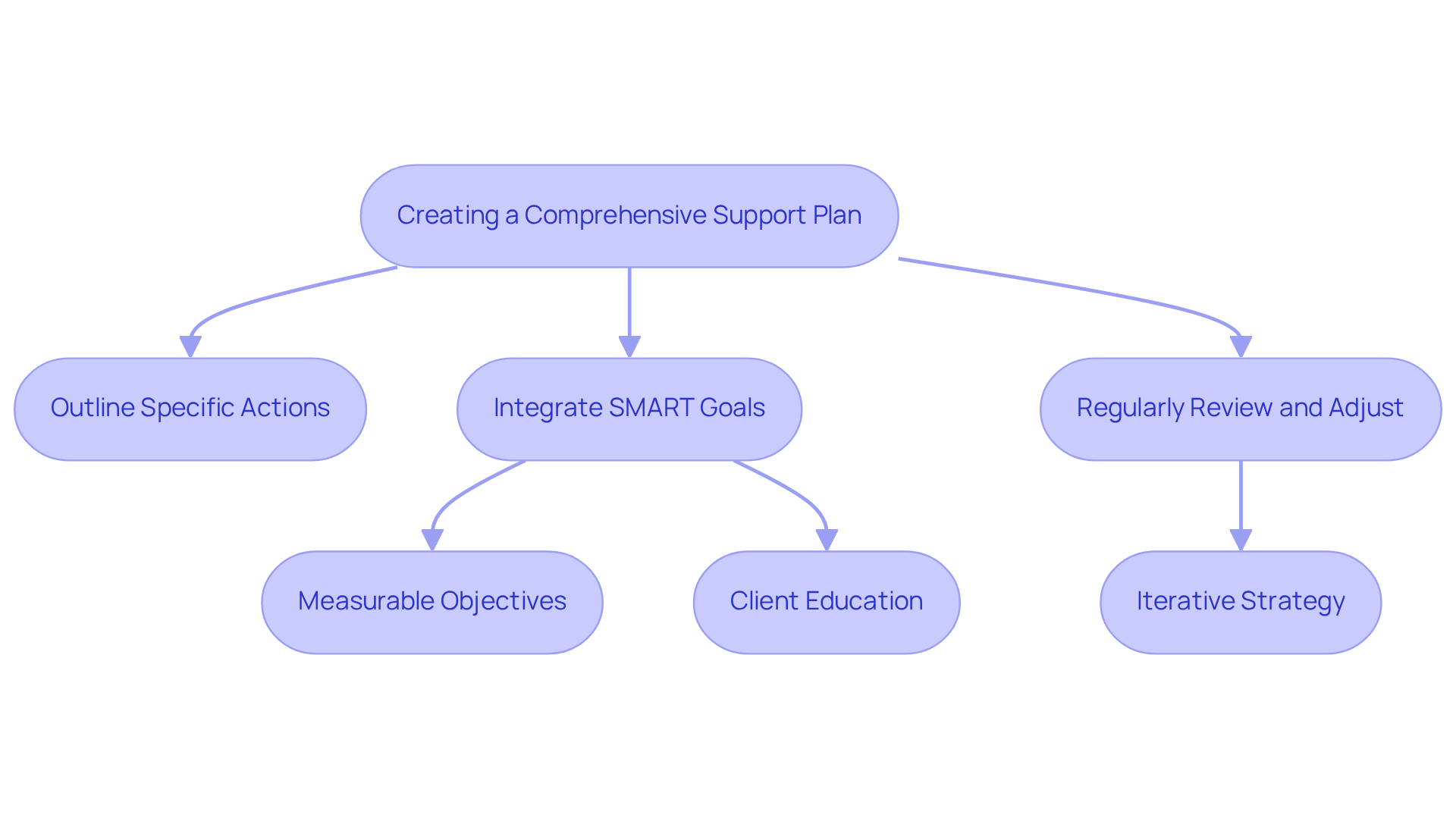
Creating a comprehensive support plan is essential for addressing the unique needs of individuals. It involves outlining specific actions, follow-up measures, and tailored education that resonates with their requirements. This plan should be realistic, measurable, and time-bound, ensuring it truly addresses individual concerns while promoting health and well-being.
Have you considered how integrating SMART goals into your treatment plans can provide a structured approach to setting measurable objectives? This method aligns beautifully with the critical role of client education in achieving better health outcomes. For instance, individuals managing chronic conditions who received targeted education experienced significant improvements in their health, underscoring the vital role effective education plays in treatment strategies.
Regularly reviewing and adjusting the strategy based on the individual's progress is key to effective management. This ensures that interventions remain relevant and impactful. This iterative process not only enhances patient engagement but also fosters a collaborative approach to care, ultimately leading to improved patient outcomes.
Furthermore, using a nursing soap note example for documentation can enhance communication among healthcare providers and ensure legal defensibility. This practice further bolsters the , creating a supportive environment where patient needs are prioritized.
Conclusion
Recognizing the emotional challenges faced by healthcare providers, the significance of effective nursing SOAP notes cannot be overstated. This article illustrates how structured documentation can transform patient care. By leveraging the SOAP format—Subjective, Objective, Assessment, and Plan—nurses can enhance communication and improve accuracy. This shift ultimately allows them to focus more on meaningful patient interactions rather than administrative tasks.
Key insights reveal that utilizing AI-driven solutions, like CosmaNeura, can significantly alleviate documentation burdens. This enables healthcare professionals to redirect their efforts towards providing compassionate care. The examples provided highlight the necessity of precise record-keeping and the importance of clear communication. Moreover, continuous education plays a crucial role in maintaining high standards of documentation.
In light of these insights, the call to action is clear: healthcare providers must embrace innovative tools and best practices in documentation. This commitment can enhance patient outcomes and satisfaction. By prioritizing accuracy and clarity in SOAP notes, nurses can reclaim valuable time for patient care. This ensures that every individual receives the attentive and compassionate support they truly deserve. The integration of technology and effective communication strategies is not merely about efficiency; it embodies a commitment to excellence in nursing practice.




