Overview
In the article titled "10 Essential Medical Chart Note Examples You Need to Know," the focus is on understanding the emotional challenges healthcare providers face in documentation. Effective medical chart notes are vital, especially when utilizing the SOAP note format. These notes are not just administrative tasks; they are essential tools that enhance patient care and treatment outcomes. Have you ever felt overwhelmed by the burden of documentation? You’re not alone.
Well-documented chart notes can significantly improve communication among healthcare providers. Evidence shows that comprehensive documentation practices lead to better health results and streamlined processes in medical settings. Imagine a world where your notes not only support patient care but also ease your workload.
This article encourages you to reflect on your documentation practices and consider how they impact your patients. By embracing effective charting techniques, you can foster a more nurturing environment for both yourself and those you care for. Let’s explore these essential examples together, and take a step towards enhancing your practice and patient outcomes.
Introduction
In the intricate world of healthcare, the importance of careful documentation is deeply felt. Medical chart notes are not just records; they are the lifeblood of patient care, fostering communication among healthcare providers and ensuring that vital information is accurately captured and readily available. As healthcare continues to evolve, the need for structured documentation practices, like the SOAP note format, has become increasingly clear.
Have you ever felt overwhelmed by the administrative demands of your role? The burden of paperwork can often overshadow the core mission of patient care. With the rise of technology and a growing focus on patient-centered approaches, it is crucial to learn how to effectively capture patient information and clinical insights. This understanding is essential for improving treatment outcomes.
This article will explore the key components of medical chart notes, share best practices, and highlight how innovative technologies can simplify the documentation process. By embracing these strategies, we can pave the way for enhanced patient care and safety, ensuring that every patient receives the attention and support they deserve.
Understanding Medical Chart Notes: An Overview
A medical chart note example is more than just a record; it is a vital component that captures the essence of patient care. These notes meticulously document encounters, treatments, and outcomes, serving as a crucial communication tool among healthcare providers. In 2025, the impact of precise medical records on treatment outcomes is clearer than ever. Studies reveal that the availability of standard record-keeping tools increases the likelihood of accurately recording routine practices by 2.5 times. This statistic underscores the need for medical professionals to prioritize comprehensive documentation, as improved documentation practices are directly linked to better treatment results.
Properly maintained chart notes not only enhance treatment outcomes but also streamline billing processes. During patient interactions, practitioners are encouraged to utilize a medical chart note example to update charts with relevant information, including:
- The reason for the visit
- Current diagnosis
- Physical exam notes
- Treatment plans
- Lab orders
- Prescriptions
- Progress notes
Frequent updates ensure that healthcare professionals have access to the most current and pertinent information, which is essential for effective patient management and continuity of care.
Consider the case study titled "Updating Patient Charts During Encounters." It highlights how regular updates during patient interactions lead to improved management and continuity of care. The significance of extends beyond legal documentation; they are integral to clinical decision-making. Expert opinions consistently emphasize that precise records are directly tied to enhanced treatment outcomes, enabling better-informed clinical choices.
Moreover, as Max Freedman, a Senior Analyst, notes, "medical billers and coders depend significantly on the data included in individuals’ records to produce precise medical claims." This highlights the financial implications of thorough record-keeping. Recent advancements indicate that knowledge, training, motivation, and the availability of standard tools greatly influence routine practice recording. There is a recognized need for additional high-quality studies on routine practice records in medical settings, reinforcing the ongoing focus on the importance of medical chart notes in patient care and their role in delivering high-quality medical services.
As healthcare providers, how can we ensure that our documentation practices not only meet standards but also enhance our ability to care for our patients? By embracing comprehensive charting, we can improve not only our workflows but, most importantly, the care we provide.
The SOAP Note Format: Structure and Significance
format stands as a cornerstone of effective medical documentation, providing a structured approach that includes four essential components: Subjective, Objective, Assessment, and Plan. This methodology empowers medical providers to organize their observations and clinical reasoning systematically. As Larry Weed, the theorist of the SOAP note, wisely stated, "The SOAP note is a method for medical professionals to document in a structured and organized manner."
- Subjective: This section captures the patient's reported symptoms and feelings, offering valuable insights into their personal experiences and concerns.
- Objective: Here, measurable data such as vital signs, laboratory results, and physical examination findings are meticulously documented, providing a factual basis for clinical decisions.
- Assessment: This component involves the clinician's interpretation of both subjective and objective data, culminating in a diagnosis or clinical impression that guides further action.
- Plan: The final section delineates the proposed treatment strategy, including recommendations for further tests, medications, and follow-up appointments.
Utilizing the SOAP format not only enhances clarity and consistency in medical records but also fosters better collaboration among medical teams. Have you ever considered how organized record-keeping methods like SOAP notes can significantly enhance clinical reasoning and communication? They serve as both a checklist and a cognitive aid for retrieving critical information. In reality, the SOAP note structure has emerged as a standard in medical practice, with many providers recognizing its efficiency in simplifying evaluations and treatment strategies.
CosmaNeura, the sole firm developing AI solutions for the billion-dollar faith-oriented medical market, underscores the importance of organized documentation in improving individual treatment.
Moreover, the integration of AI algorithms can analyze large datasets to identify genetic markers and biomarkers associated with specific diseases or treatment responses. This capability enables medical providers to customize treatments for individual patients, maximizing effectiveness and minimizing adverse effects. For instance, a healthcare facility that adopted AI-driven analysis alongside SOAP notes reported a 30% boost in treatment effectiveness due to more tailored plans.
Real-world applications of a medical chart note example illustrate its impact on clinical documentation. A study titled 'SOAP Notes: A Structured Documentation Method' indicated that practices using a medical chart note example, such as SOAP notes, experienced improved care outcomes due to better-organized information flow. However, it is essential to acknowledge the limitations of the traditional SOAP model, which has led to adaptations like the SOAPE model, addressing the need for capturing changes over time in individual conditions.
AI can enhance the SOAP format by offering real-time data analysis, enabling dynamic updates to records that reflect ongoing changes in health status.
As we move through 2025, the significance of SOAP notes in clinical records continues to grow, with trends suggesting a heightened dependence on structured formats to ensure thorough individual records. Healthcare experts consistently advocate for organized records, emphasizing their importance in enhancing job satisfaction and care quality. By embracing the SOAP note format and leveraging AI solutions, providers can elevate their documentation practices, ultimately leading to improved health outcomes and a more efficient healthcare system.
Capturing Patient Perspectives: The Subjective Section
of a SOAP note is essential for documenting the individual's own words regarding their symptoms, concerns, and feelings. This section not only captures the individual's experience but also significantly influences clinical decisions. Research indicates that over 40% of individuals are at significant risk due to misunderstanding, forgetting, or ignoring care recommendations. This underscores the need for effective communication in this area.
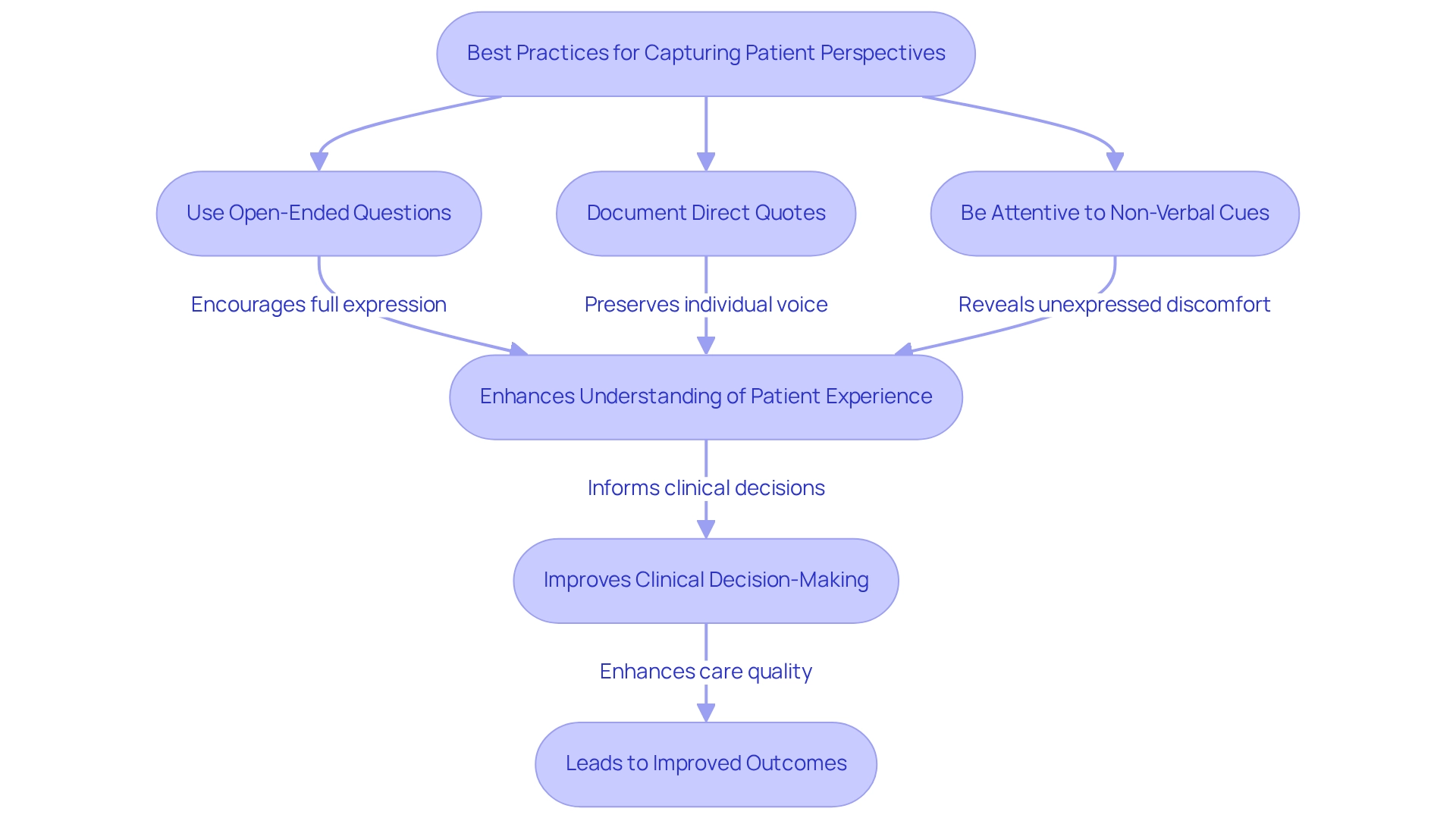
To effectively capture patient perspectives, consider the following best practices:
- Use open-ended questions: Encourage patients to express themselves fully, allowing for a richer understanding of their experiences. This method aligns with the transformative potential of AI-driven solutions, which can enhance communication and understanding between individuals and providers.
- Document direct quotes: Whenever possible, preserve the individual's voice by recording their exact words. For instance, instead of simply noting 'individual reports discomfort,' a more comprehensive entry could state, 'Individual shares, “I have a sharp pain in my lower back that worsens when I bend over.”' This level of detail provides a clearer understanding of the individual's condition and can be further analyzed through AI tools to identify patterns and enhance treatment.
- Be attentive to non-verbal cues: Observing body language and facial expressions can reveal discomfort or distress that may not be verbally expressed. AI innovations can assist in analyzing these non-verbal signals, enriching the overall understanding of individual experiences.
As noted by Ensieh Ashrafi, 'The writer(s) also express their thanks and appreciation to the respected reviewers who offered constructive and valuable recommendations for enhancing the quality of this article,' highlighting the importance of detailed records in improving care for individuals.
A validation study on the Health Engagement (PHE) scale, involving 382 participants with chronic illnesses, confirmed the effectiveness of capturing involvement through subjective documentation. The research identified significant correlations between individual involvement and activation measures, emphasizing the relevance of subjective data in enhancing care quality. This aligns with CosmaNeura's mission to improve medical service delivery through AI solutions designed for faith-based providers, ensuring that individual perspectives are prioritized in clinical decision-making.
Integrating these strategies into your medical chart note example not only enhances individual engagement but also enriches the clinical decision-making process, ultimately leading to improved outcomes for individuals. By utilizing AI-powered tools, healthcare professionals can further elevate the quality of their records and interactions with individuals, addressing challenges such as physician burnout and fragmented services.
Documenting Measurable Data: The Objective Section
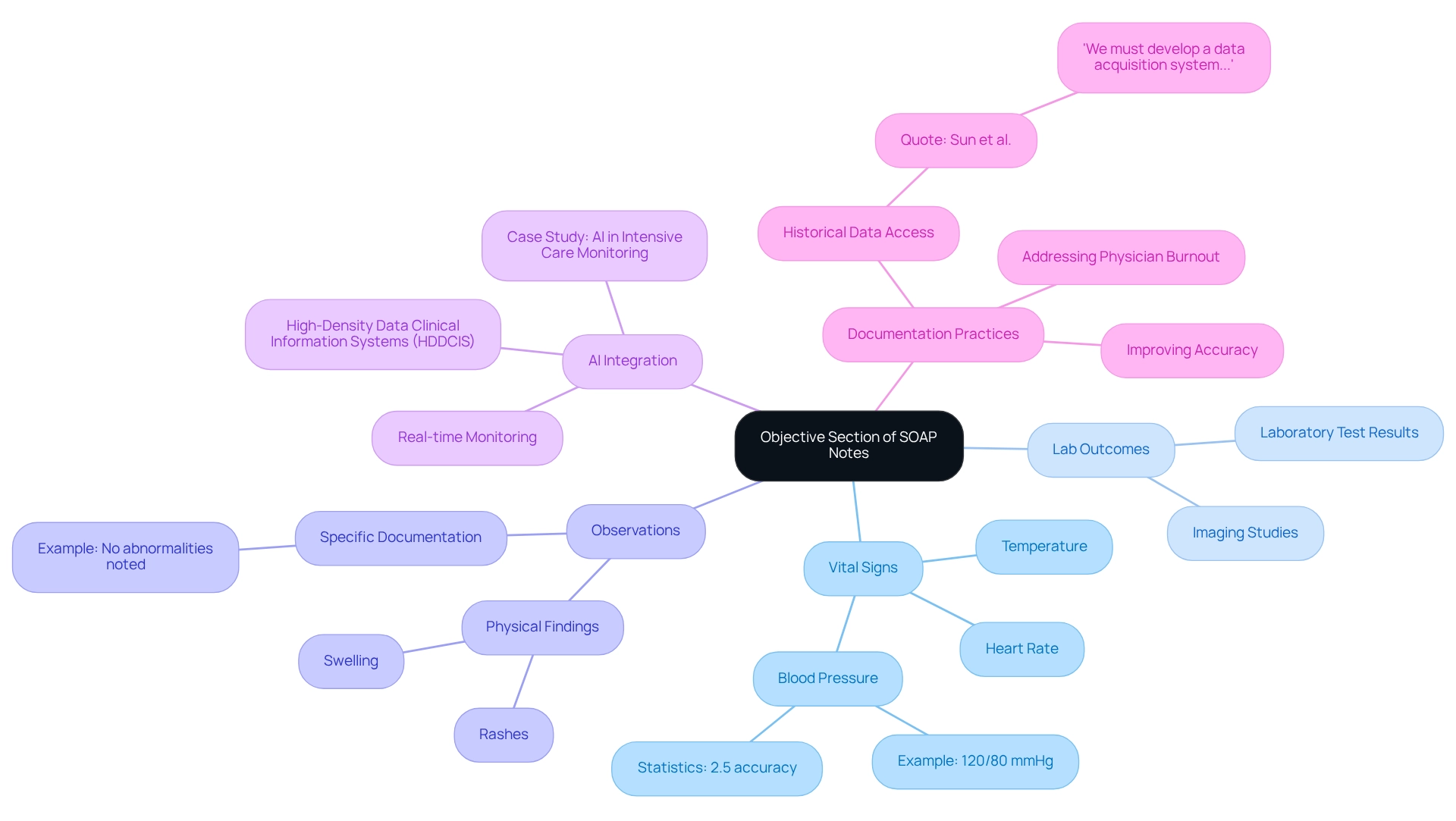
The Objective section of a SOAP note is crucial for capturing measurable and observable data gathered during client encounters. This includes vital signs, physical examination findings, and outcomes from diagnostic tests—elements that are essential for informed clinical decision-making and enhancing individual well-being through AI-driven solutions.
To ensure comprehensive records in this section, it is vital to:
- Accurately record vital signs such as blood pressure, heart rate, and temperature.
- Include outcomes from laboratory tests and imaging studies.
- Document observable physical findings, such as rashes or swelling.
For instance, rather than stating 'individual appears healthy,' a more effective entry would be 'The blood pressure is 120/80 mmHg, heart rate is 72 bpm, and no abnormalities noted during the physical exam.' This level of specificity not only improves the clarity of the medical record but also aids in better evaluations and aligns with the ethical standards highlighted by CosmaNeura.
Current statistics reveal that only 2.5% of blood pressure observations have both systolic and diastolic readings ending in zero without prior abnormal readings. This underscores potential inaccuracies in vital signs records, which can lead to misinformed treatment decisions. It highlights the importance of precise and accurate vital signs in medical charting, emphasizing the necessity for healthcare providers to adopt rigorous documentation practices to ensure quality care.
Moreover, recent advancements in clinical information systems (CIS) have uncovered significant inefficiencies, as much bedside information is often discarded. The integration of (HDDCIS) with artificial intelligence (AI) is transforming the monitoring of individuals, especially in intensive treatment environments. This integration enables real-time identification of clinically significant events, thereby enhancing outcomes for individuals and operational efficiency.
As highlighted in a case study on AI in intensive monitoring, the potential of AI to improve individual monitoring is substantial, demonstrating the real-world application of precise data documentation.
In accordance with the latest guidelines for recording objective data in medical practice, it is crucial to emphasize measurable data in the objective section of SOAP notes. This can be illustrated through a medical chart note example. As Sun et al. stated, 'we must develop a data acquisition system that facilitates the access and review of historical data for medical personnel.' This quote reinforces the argument for improving documentation practices and the need for historical data access.
By following these practices, medical professionals can significantly enhance the quality of services provided to individuals, aligning with the ethical standards and compassionate values highlighted by CosmaNeura.
Furthermore, addressing the challenges faced by medical providers, such as physician burnout and disjointed service systems, is essential. AI tools can alleviate the administrative load on medical professionals, allowing them to focus more on direct client care. By incorporating AI solutions, CosmaNeura aims to enhance the efficiency of documentation processes, ultimately leading to better patient outcomes and a more sustainable medical environment.
Analyzing Information: The Assessment Section
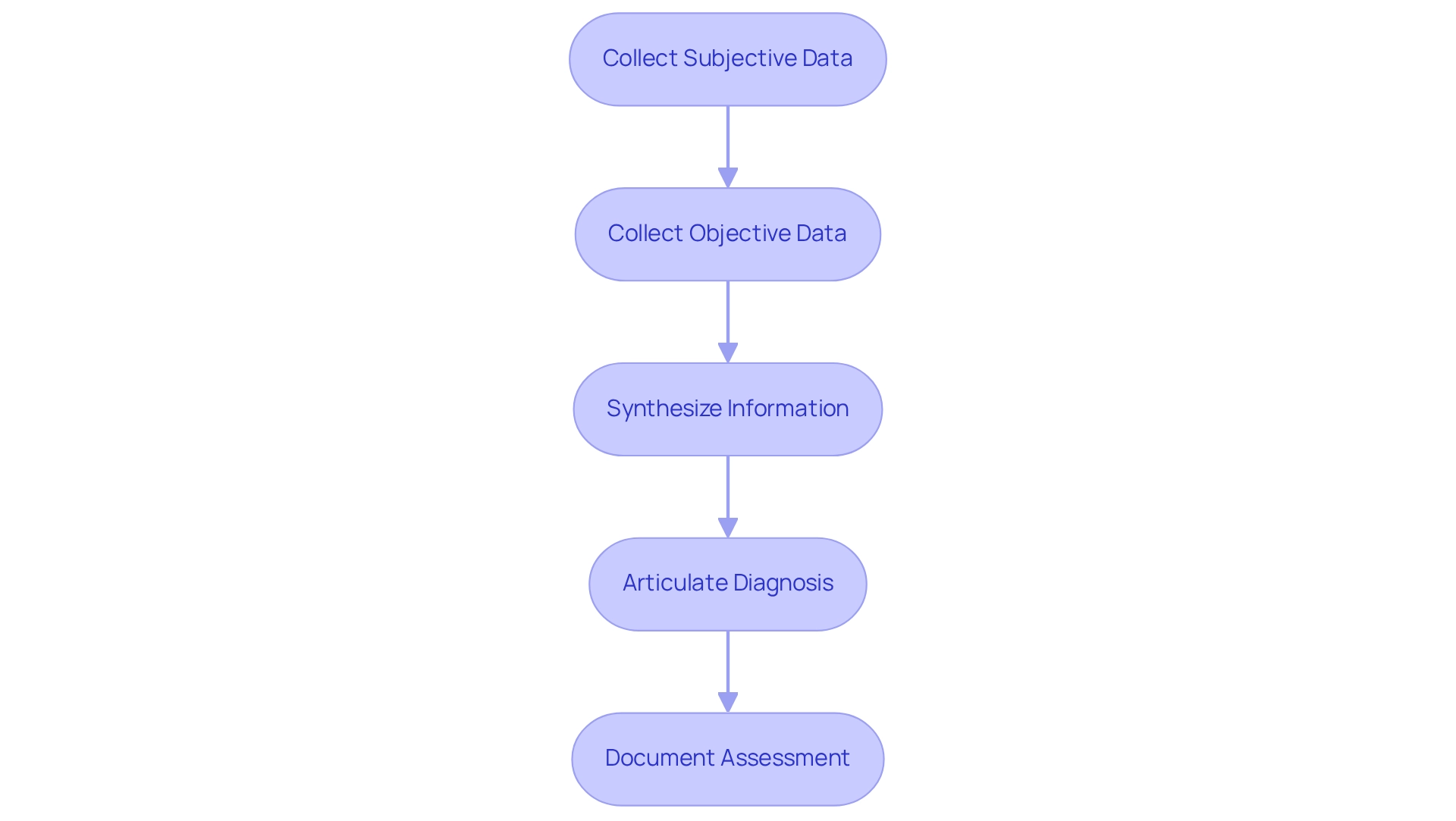
The Assessment section of a SOAP note is a crucial part of the healthcare process, where providers synthesize information from both subjective and objective sections to form a clinical impression or diagnosis. This section is vital for guiding treatment decisions and ensuring continuity of care.
To effectively document the assessment, consider these key points:
- Clearly articulate the diagnosis or differential diagnoses derived from the collected data.
- Incorporate relevant clinical reasoning that supports the assessment.
Reflecting on the individual’s history and presenting symptoms is essential during your analysis.
For example, an evaluation might indicate: 'Assessment: Acute bronchitis secondary to viral infection, as evidenced by the individual's cough, wheezing, and recent upper respiratory infection.' This clarity not only enhances communication among healthcare providers but also strengthens the reliability of the records.
Recent findings underscore the importance of thorough assessments in clinical practice. Research suggests that precise clinical evaluations grounded in SOAP notes can significantly influence treatment choices. Data reveals that high-quality records are linked to improved health outcomes. Notably, Augnito offers high transcription and coding accuracy for SOAP note-taking, crucial for maintaining documentation integrity.
A case study involving Ditto Transcripts highlighted their commitment to 99% accuracy in medical transcription services, allowing healthcare providers to focus more on care rather than paperwork. This ultimately improves the experience for those receiving treatment. It emphasizes the importance of selecting a medical transcription service with high accuracy rates to mitigate legal risks and ensure safety for individuals.
Moreover, expert insights stress the necessity of clinical reasoning in medical assessments. Imran Shaikh, a Content Marketing Expert and SEO Specialist at Augnito AI, states, "It’s essential that these basic aspects of the SOAP note are clearly stated and accurate to ." Effectively synthesizing individual information in the assessment section can lead to better diagnostic accuracy and treatment planning.
As the medical field continues to evolve, the emphasis on accurate and thoroughly documented evaluations remains crucial. This ensures that providers can deliver top-notch services while adhering to best practices in documentation.
Outlining Future Care: The Plan Section
The Plan section of a SOAP note is crucial, as it outlines the suggested course of action for the individual, ensuring that all members of the healthcare team are synchronized in their treatment approach. This segment not only promotes clear communication but also improves outcomes by offering a structured framework for follow-up support.
To craft an effective plan, consider the following best practices:
- Clearly specify any medications, therapies, or interventions to be initiated, ensuring that the rationale for each choice is evident.
- Include details about follow-up appointments and any necessary referrals to specialists, which are essential for thorough management.
- Document any education offered during the visit, reinforcing the individual's understanding and involvement in their treatment.
For example, a well-structured plan might read: 'Plan: Initiate albuterol inhaler as needed for wheezing, schedule a follow-up appointment in two weeks, and refer to a pulmonary specialist for further evaluation.' This clarity not only encourages continuity of support but also aligns with findings that highlight the significance of treatment plans in improving adherence to prescribed interventions. Indeed, statistics show that almost 50% of individuals in the U.S. do not follow their prescribed treatment plans, which can lead to expensive hospital readmissions and heightened healthcare costs.
Furthermore, case studies have demonstrated that efficient treatment planning greatly enhances client outcomes. For instance, a study on post-discharge call programs highlighted the necessity of structured follow-up strategies, despite acknowledging limitations in its methodology, such as the lack of a control group and potential biases. This underscores the need for additional research to confirm the effectiveness of such interventions, emphasizing that clear treatment plans are essential to successful care management.
Moreover, deficiencies in management frequently occur due to insufficient coordination among providers and individuals, making the Plan section even more vital in facilitating effective communication. As Jack London remarked, "The writers wish to recognize the contributions of Vito Corleone and Jack London from the Patient Pal organization in gathering and supplying information for this study," emphasizing the collaborative efforts in enhancing recipient support.
In summary, the Plan section of SOAP notes serves as and is not merely a formality; it is a vital component of patient care that can lead to improved adherence and better health outcomes when executed thoughtfully.
Examples of Effective SOAP Notes: Best Practices
Effective SOAP notes exemplify best practices in medical records, serving as a vital tool for healthcare providers. They not only facilitate communication but also address the emotional challenges faced by professionals in the field. Have you ever felt overwhelmed by administrative tasks? These notes can alleviate some of that burden, allowing you to focus more on what truly matters—your patients.
Here are a few examples that highlight their structure and clarity:
-
Example 1:
- Subjective: 'Patient reports a persistent headache for the past three days, rated 7/10 in severity.'
- Objective: 'Blood pressure 130/85 mmHg, pulse 78 bpm, no neurological deficits observed.'
- Assessment: 'Tension headache likely due to stress.'
- Plan: 'Recommend over-the-counter analgesics, hydration, and follow-up if symptoms persist.'
-
Example 2:
- Subjective: 'Patient states, “I feel anxious about my upcoming surgery.”'
- Objective: 'Patient appears anxious, with a heart rate of 90 bpm.'
- Assessment: 'Preoperative anxiety.'
- Plan: 'Discuss anxiety management techniques, schedule preoperative counseling session.'
These examples illustrate the importance of clarity, detail, and patient-centered language in SOAP notes. A study has shown that the APSO order can enhance speed, task success, and usability for physicians compared to , indicating a shift towards more efficient documentation practices. Moreover, the organized format of SOAP notes greatly decreases administrative time and enhances communication among specialists, resulting in improved outcomes for individuals.
For instance, a case study demonstrated that standardized SOAP notes promote clearer communication and improve collaboration among healthcare providers, ultimately leading to enhanced care. Isn't it reassuring to know that effective documentation can lead to better patient outcomes?
However, it is important to acknowledge the limitations of the SOAP note model, particularly its inability to effectively serve as a medical chart note example for documenting changes over time. This limitation highlights the need for extensions like SOAPE to provide a more comprehensive view of patient progress. As Dr. Safran from Beth Israel Deaconess Medical Center remarked, 'There’s likely no one who has more fundamentally influenced how we arrange our tasks than Larry Weed,' underscoring the considerable effect of organized record-keeping on medical practice.
In 2025, the focus on effective documentation continues to expand, with best practices developing to encompass detailed and clear SOAP notes that not only satisfy clinical needs but also adhere to patient-centered principles. Let’s embrace these practices together for the benefit of our patients and our peace of mind.

Common Mistakes to Avoid in Medical Chart Notes
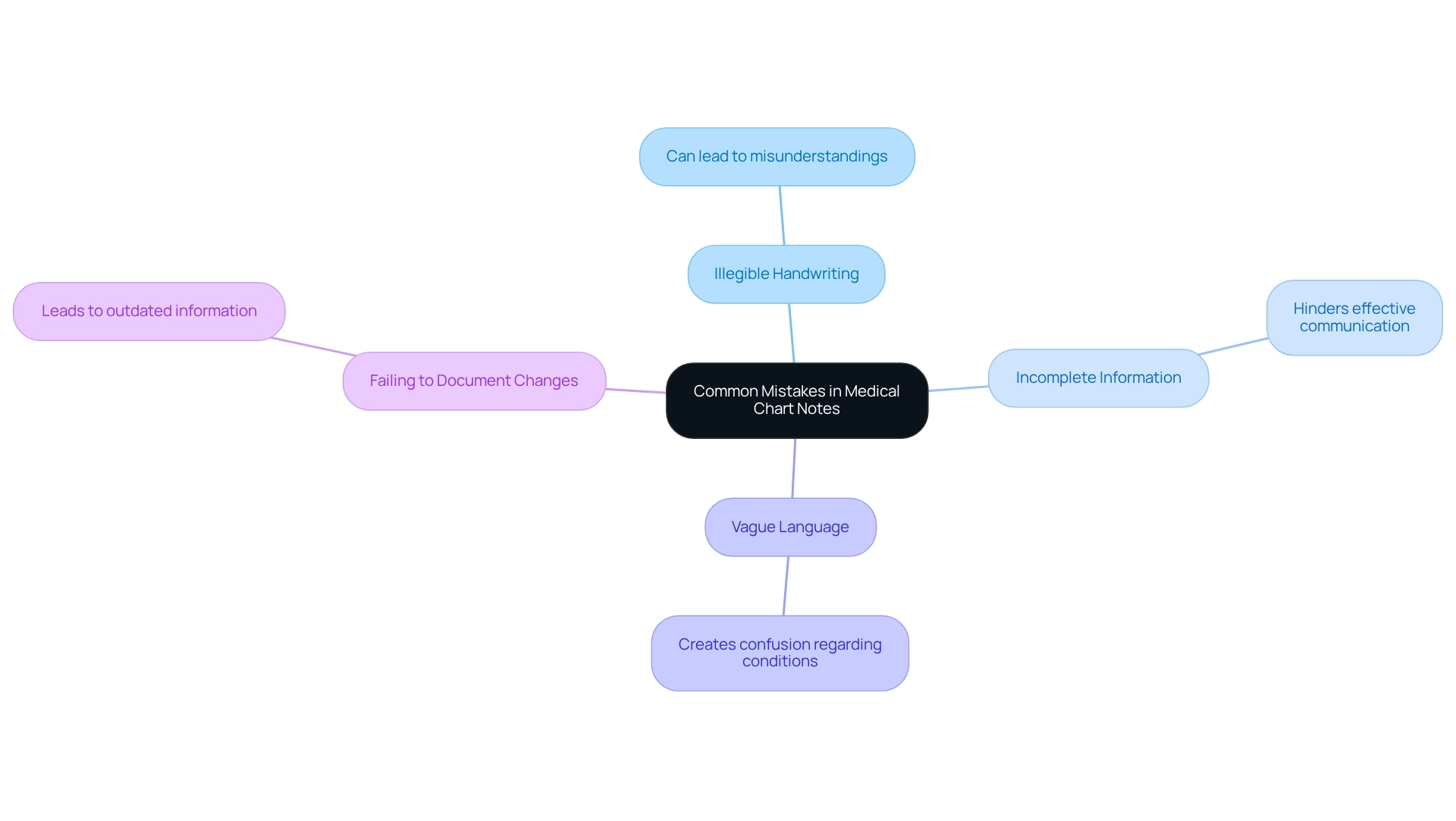
Frequent errors in a medical chart note can lead to serious repercussions, impacting both safety and the quality of care. It’s essential to recognize these critical pitfalls to avoid:
- Illegible Handwriting: Clear and legible notes are vital, especially in handwritten records. When handwriting is unclear, misunderstandings and misinterpretations can arise, potentially compromising the safety of those receiving care.
- Incomplete Information: Always ensure that all relevant details are included, such as medical history, treatment plans, and follow-up instructions. Incomplete documentation can hinder effective communication among healthcare providers and negatively affect outcomes for individuals.
- Using Vague Language: Avoid ambiguous terms; specificity in descriptions is crucial to prevent misinterpretation. For instance, using terms like 'improved' without context can create confusion regarding an individual's actual condition.
- Failing to Document Changes: It’s crucial to update the chart with any changes in an individual's condition or treatment plan. Neglecting to document these changes can lead to outdated information that adversely impacts clinical decisions.
Statistics reveal that record-keeping errors significantly influence patient care, with a staggering 58.9% of patient-reported mistakes potentially affecting the diagnostic process. This underscores the urgent need for careful record-keeping practices. Furthermore, medication errors occur at rates ranging from 8% to 25% during medical administration, highlighting the real-world impacts of these errors and the necessity for improved training and protocols.
As the Institute of Medicine (IOM) wisely advises, "Avoid extending duty hours beyond what was previously scheduled for the day." This statement emphasizes the importance of appropriate record-keeping methods in relation to provider workload and client safety. By being mindful of in medical chart notes, healthcare professionals can enhance the quality and reliability of their records, ultimately leading to improved patient safety and care.
Moreover, the fragmentation of medical systems and the resulting administrative burdens contribute to physician burnout, making precise record-keeping even more essential. Utilizing CosmaNeura's AI solutions can help alleviate these burdens by automating repetitive tasks and ensuring that documentation is accurate and comprehensive. For instance, CosmaNeura's AI can assist in identifying incomplete notes or suggesting specific language to enhance clarity, thus promoting better outcomes for individuals and increasing the overall efficiency of healthcare delivery.
Compliance and Ethical Considerations in Medical Charting
Compliance and ethical considerations are at the heart of effective medical charting. Healthcare providers often face the emotional challenge of navigating complex regulations like HIPAA, which are essential for protecting individual privacy and confidentiality. With enforcement actions on the rise—evidenced by the average HIPAA fine reaching $98,643 in 2022—it's clear that strict adherence to compliance protocols is not just necessary but vital for peace of mind.
Key considerations include:
- Patient Consent: Have you secured explicit consent from your patients before sharing their information? This practice not only aligns with ethical standards but also shields you from potential legal repercussions.
- Accurate Documentation: Are all your entries truthful and reflective of the individual's condition? Inaccurate documentation can lead to serious consequences, including legal liabilities and compromised care.
- Confidentiality: How are you safeguarding client records? It's crucial to restrict access to authorized personnel only, ensuring sensitive information remains secure. Notably, 58% of data breaches in the medical sector stem from hacking or IT-related incidents, highlighting the urgent need for robust security measures.
By prioritizing compliance and ethical standards, medical providers can foster trust with clients and uphold the integrity of their documentation practices. Furthermore, with a staggering 450% increase in Right of Access fines from 2019 to 2022, the importance of maintaining rigorous compliance cannot be overstated. As Steve Alder, editor-in-chief of , wisely states, "It is necessary to prove the breach notification requirements are complied with to ensure covered entities and business associates do not overlook notifying individuals in the required timeframe."
Case studies reveal that while many medical providers have established policies regarding mobile device usage, a significant 40% do not utilize mobile encryption. This gap in security practices underscores the critical need for comprehensive measures to protect individual information.
In summary, adhering to ethical standards and compliance regulations not only protects medical providers from potential fines but also enhances the overall quality of service. Let us work together to ensure that compliance becomes a cornerstone of compassionate care.
Leveraging Technology for Efficient Medical Charting
In the demanding world of healthcare, utilizing technology in medical chart notes can greatly alleviate the documentation burden and enhance precision, ultimately benefiting patient care. Have you ever felt overwhelmed by the administrative tasks that distract from your primary focus—caring for individuals? Here are several key ways technology can support you:
- Electronic Health Records (EHRs): EHR systems have revolutionized access to patient information, allowing providers to retrieve and update chart notes in real-time. The adoption of comprehensive EHR systems has surged from just 3.6% in 2009 to an impressive 63.2% today, underscoring their essential role in modern healthcare. CosmaNeura's platform enhances this by automating administrative tasks such as appointment scheduling, medical record management, and billing. This automation enables providers to concentrate on what truly matters—patient care—while ensuring adherence to Catholic teachings. For instance, by automating appointment reminders, CosmaNeura significantly decreases no-show rates, leading to better resource utilization and greater satisfaction among those receiving care.
- Speech-to-Text Software: This innovative technology allows providers to dictate notes swiftly, significantly reducing the time spent on documentation. By transforming spoken language into text, it empowers clinicians to focus more on their interactions with patients rather than on administrative tasks. Cosmonaut's speech-to-text integration ensures that notes are accurately captured and readily accessible, enhancing workflow efficiency.
- Templates and Standardized Forms: Utilizing templates guarantees that all necessary information is consistently captured across patient encounters. This standardization not only improves the quality of records but also streamlines the creation of medical chart notes. CosmaNeura offers customizable templates that adapt to various specialties, ensuring that all pertinent information is gathered without unnecessary repetition.
The impact of EHRs on medical record-keeping is profound. A recent study indicated that 65% of hospitals plan to enhance their EHR functionalities, reflecting a proactive approach to improving documentation practices despite existing challenges. This aligns with CosmaNeura's mission to transform medical services through innovative solutions.
Moreover, EHR systems have shown the ability to improve individual outcomes, reduce medical errors, and enhance overall efficiency in medical service delivery. By embracing these technological advancements, healthcare providers can significantly enhance their documentation efficiency, leading to and satisfaction. How can you start integrating these solutions into your practice today?
Conclusion
The significance of meticulous medical chart notes cannot be overstated; they are truly the backbone of effective patient care. Have you ever considered how structured documentation practices, like the SOAP note format, can transform patient encounters? By ensuring comprehensive recording, healthcare providers facilitate seamless communication and enhance clinical decision-making, ultimately leading to improved treatment outcomes.
Each component of SOAP notes—Subjective, Objective, Assessment, and Plan—plays a vital role in capturing patient information. Best practices for documenting patient perspectives, measurable data, and clinical assessments underscore the importance of accuracy and detail. Moreover, the integration of technology, such as Electronic Health Records and AI-driven solutions, streamlines the documentation process, alleviating administrative burdens that can weigh heavily on providers.
As healthcare continues to evolve, the emphasis on structured and thorough documentation will only grow. By prioritizing accurate medical charting and leveraging technological advancements, healthcare professionals can enhance the quality of care provided to patients. In doing so, they not only improve individual patient outcomes but also contribute to a more efficient and effective healthcare system as a whole. Embracing these strategies is essential for navigating the complexities of modern healthcare and ensuring that every patient receives the attention and support they deserve.




