Overview
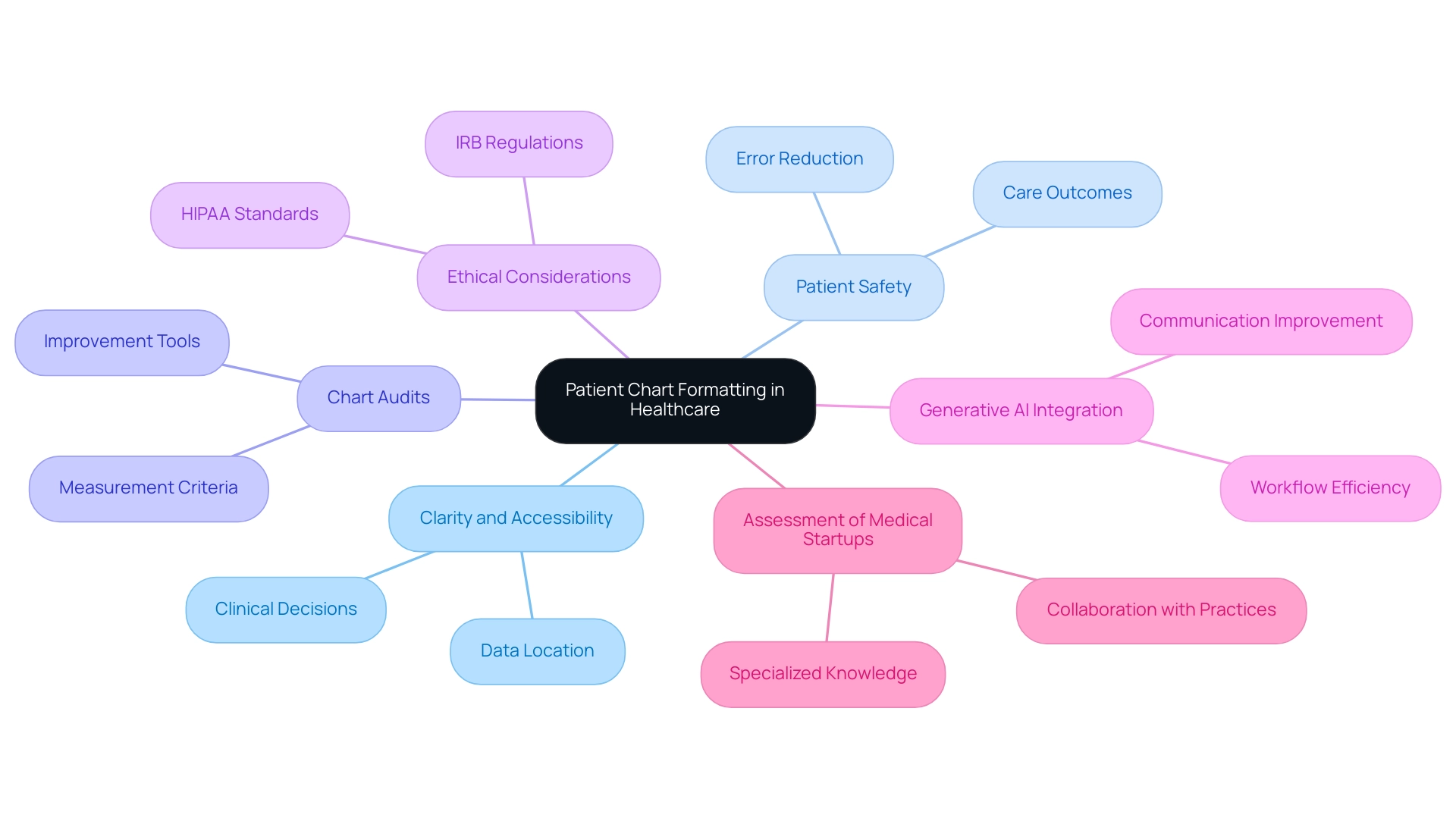
In the demanding world of healthcare, the emotional challenges faced by providers can often feel overwhelming. Best practices for patient chart format focus on standardization, training, and the integration of technology to alleviate these burdens. By adopting uniform templates and utilizing AI-driven solutions, we can significantly reduce errors and administrative pressures. This not only enhances documentation effectiveness but also improves patient care outcomes.
Imagine a healthcare environment where communication flows seamlessly among providers. The article emphasizes that these practices foster better collaboration, ensuring that every patient receives higher quality care. By addressing the administrative challenges head-on, we can create a nurturing atmosphere that prioritizes patient well-being.
As we reflect on the importance of these changes, consider how they can transform your daily practice. Embracing technology and standardization is not just about efficiency; it’s about empowering healthcare providers to focus on what truly matters—caring for patients. Let’s take these steps together to enhance our documentation processes and ultimately improve the lives of those we serve.
Introduction
In the intricate landscape of healthcare, the organization and clarity of patient information can profoundly impact outcomes. How often do we consider that patient chart formatting can be a matter of life and death? It serves as a crucial element, ensuring that healthcare providers have immediate access to vital data necessary for making informed decisions swiftly.
As the industry navigates the challenges of documentation errors and the overwhelming volume of data, the need for standardized practices becomes increasingly clear. This article explores the significance of effective patient chart formatting, emphasizing proven strategies, the role of technology, and the ethical considerations that underpin this essential aspect of healthcare delivery.
By examining these themes, we recognize that enhancing documentation practices is not just an administrative task; it is a foundational component of delivering compassionate and high-quality patient care. Let us delve deeper into how we can improve our practices for the benefit of our patients and ourselves.
The Significance of Patient Chart Formatting in Healthcare
The stands as a cornerstone of effective medical delivery, significantly shaping the clarity and accessibility of information regarding individuals. Well-structured charts empower healthcare providers to swiftly locate essential data, crucial for making timely and informed clinical decisions. Consider how a meticulously organized chart can facilitate tracking an individual's medical history, medications, and treatment plans—each vital for comprehensive management.
Research indicates that adopting can substantially reduce the risk of errors, thereby enhancing patient safety and improving overall care outcomes. Chart audits have become invaluable tools for identifying areas of improvement and ensuring safety in medical practices. These audits underscore the necessity of clearly defining measurement criteria and summarizing data effectively to inform actionable changes.
Recently, 18 participants attended a meeting focused on these audits, highlighting the collaborative effort to enhance charting practices.
In faith-centered medical environments, particularly those aligned with Catholic teachings, the emphasis on compassion and thoroughness in documentation amplifies the importance of effective chart formatting. Ethical factors, such as compliance with IRB regulations and HIPAA standards, ensure that health information remains confidential while promoting high-quality care. As Claire Snyder, Principal Investigator, noted, "The modified Delphi methodology facilitated the development of the consensus recommendations," emphasizing the need for methodological rigor in chart reviews.
Moreover, the advent of generative AI presents unique opportunities to enhance medical workflow efficiency. By integrating AI solutions into client record systems, medical professionals can improve communication, lessen administrative burdens, and ultimately enhance care. Case studies reveal that common mistakes in retrospective chart reviews (RCRs) often arise from inadequate chart organization.
By addressing these pitfalls and implementing best practices, medical providers can elevate the quality, validity, and reliability of their data, leading to better clinical outcomes. The influence of patient chart format on clinical decision-making is profound; it is essential for fostering an environment where medical professionals can deliver compassionate and effective care.
However, to fully realize the potential of these advancements, evaluating medical startups effectively is crucial. Traditional accelerators often fall short, lacking the specialized knowledge required to assess the unique challenges and opportunities presented by generative AI in the medical field. At CostaNera, we recognize the significance of comprehensive assessments and collaborate directly with small, private practice professionals to ensure that the integration of AI solutions is not only effective but also aligned with the specific needs of the healthcare landscape.
Challenges in Patient Chart Documentation: Identifying Common Pitfalls
Healthcare providers often face significant emotional challenges in managing chart records. Time limitations, excessive data, and inconsistent formatting create stress and frustration. Statistics reveal that time constraints can lead to hurried entries; during a transition to a new EHR system, research found that 15.3% of health records contained at least one error, with 85.9% of these categorized as significant mistakes. This underscores the risk of incomplete or inaccurate information due to rushed recording processes.
The overwhelming volume of data that must be documented can further intensify these issues, often resulting in critical details being overlooked. Additionally, the irregular patient chart format among different providers or departments complicates the record-keeping process, making it challenging to access and understand individual information effectively. For example, during the migration from the QuadraMed EHR system to the EPIC EHR system at the Princess Margaret Cancer Center, a quality improvement study highlighted the difficulties in maintaining accurate patient records, illustrating the potential impact of record-keeping errors on patient care.
Since December 2016, continuous monitoring of article usage has highlighted the persistent significance of in the medical field. How can we address these obstacles?
To tackle these challenges, healthcare professionals must commit to standardized practices that promote consistency and clarity in patient chart formats. As Pamela Ballou-Nelson, PhD, RN, MSPH, CMPE, emphasizes, "Maximizing client access and scheduling" is vital in overcoming these hurdles. The integration of advanced technology, particularly AI-driven solutions, can streamline documentation workflows, significantly reducing the administrative burden on providers.
By leveraging these tools, clinicians can redirect their focus toward delivering high-quality care, ultimately enhancing both job satisfaction and patient outcomes. For instance, CosmaNeura's platform exemplifies this approach, providing administrative efficiency and enhanced care that align with the mission of transforming medical delivery through innovative solutions. Furthermore, addressing the issues of physician burnout and disjointed medical systems through AI can further improve the efficiency of record-keeping practices, ensuring that medical professionals can deliver optimal care without being overwhelmed by administrative tasks.
Proven Strategies for Effective Patient Chart Formats
To enhance the effectiveness of client chart formats, healthcare providers can adopt several proven strategies that resonate with their commitment to compassionate care:
- Standardization: Implementing uniform templates for records is crucial for ensuring consistency across all charts. This approach includes using common terminologies and a patient chart format for vital signs, medications, and treatment plans, which can significantly reduce variability and improve clarity in patient records. For instance, a newborn screening dataset revealed that precise records led to 13,456 true positives, underscoring the importance of standardization in achieving reliable outcomes.
- Training: Regular training sessions for staff on best practices in charting can lead to a marked reduction in errors and an improvement in documentation quality. Evidence suggests that effective training programs can enhance staff competency, leading to better patient outcomes and more reliable data collection. This aligns with the mission of faith-based healthcare organizations, who prioritize compassionate and competent care.
- Utilization of Technology: Leveraging electronic health records (EHR) systems that offer customizable templates and automated prompts is essential for guiding providers in capturing essential information accurately. Such technology not only streamlines the patient chart format but also ensures adherence to standardized practices, which is essential for maintaining high-quality client records. As illustrated by the case study of Kodjin, compliance with health IT standards can transform documentation practices and enhance integration within the healthcare ecosystem.
- Real-time Documentation: Encouraging providers to document interactions in real-time during consultations minimizes the risk of forgetting critical details. This practice not only improves the accuracy of the information documented but also enables prompt clarification of any uncertainties during the interaction. As pointed out by Pamela Ballou-Nelson, PhD, RN, MSPH, CMPE, optimizing patient access and scheduling is crucial, and immediate record-keeping plays a key role in achieving this.
- Feedback Mechanisms: Establishing feedback loops where providers can review and discuss record-keeping practices fosters a culture of continuous improvement. By consistently evaluating records quality and sharing insights, medical teams can pinpoint areas for improvement and execute required modifications efficiently. Furthermore, being cognizant of possible challenges like selection bias and insufficient data triangulation can further enhance the record-keeping process.
Integrating these techniques not only conforms to best practices but also addresses the urgent requirement for standardization in the patient chart format for , which has been shown to enhance overall health service delivery and safety for individuals, particularly within the realm of faith-based medical care.
Leveraging Technology for Enhanced Patient Chart Documentation
In today's fast-paced healthcare environment, technology is transforming medical recordkeeping, with AI-driven solutions like those from CostaNera leading the way. These innovations are designed to alleviate the emotional strain on healthcare providers by automating routine tasks such as appointment scheduling and medical record management. This allows providers to focus more on meaningful interactions with individuals, fostering a more compassionate care experience. For instance, during telehealth sessions, CosmaNeura's AI facilitates real-time transcription, ensuring that documentation is both accurate and comprehensive, freeing clinicians from the burdens of manual entry.
Moreover, advanced electronic health record (EHR) systems enhance this process by providing alerts for missing information, suggesting appropriate billing codes, and allowing for seamless retrieval of individual data. By streamlining these administrative tasks, physicians can reclaim valuable time to concentrate on delivering high-quality care to their patients. It's concerning to note that physicians currently spend 34 to 55 percent of their workday on documentation, leading to an annual opportunity cost of $90 to $140 billion in the U.S. How can we shift this dynamic to prioritize patient interactions?
A clinical trial evaluating the AI-powered documentation tool, Dragon Ambient Experience (DAX) Copilot, revealed that about half of the clinicians reported reduced time spent on electronic health records and less frustration. This trial, conducted in outpatient clinics in North Carolina and Georgia, aimed to assess the tool's impact on clinician recording time and overall experience. However, the study also highlighted that many clinicians did not experience the expected time-saving benefits, indicating a need for ongoing research to enhance the effectiveness of such tools.
Furthermore, a recent survey revealed that 39% of participants somewhat agree that AI will enhance satisfaction among individuals, underscoring the potential advantages of AI in medical record-keeping. The varying optimism among specialties, with pathologists being the most optimistic and psychiatrists the least, reflects a broader perspective on the acceptance of AI across the medical field. How can we foster a more supportive environment for these innovations?
By utilizing AI solutions, medical providers can reduce mistakes and enhance the overall quality of care. As Jesse M. Ehrenfeld, AMA President, insightfully noted, "Now this may not fall into a regulatory framework under FDA authority, but it could become a market differentiator to identify from all the products in the oncoming tidal wave." As the medical landscape evolves, the role of technology in managing patient chart formats becomes increasingly essential. There is a growing consensus among physicians across various specialties acknowledging its potential to enhance efficiency and satisfaction while addressing the challenges of innovation resistance in the field.
This resistance often stems from concerns about maintaining the quality of service and interactions, which startups like CosmaNeura must navigate to gain acceptance among doctors. We must collectively explore how to bridge this gap, ensuring that the integration of technology supports rather than hinders that patients deserve.
Ethical Considerations in Patient Chart Documentation
Ethical considerations in chart documentation are vital, especially in faith-focused healthcare environments. Providers face the emotional challenge of prioritizing practices that uphold confidentiality, autonomy, and informed consent for individuals. How can we ensure that interactions are accurately documented while safeguarding against biases or discrimination?
The historical evolution of medical records, spanning over 4,000 years, showcases a significant transition from ancient written forms to modern electronic health records (EHRs). This shift was designed to address issues like illegible handwriting and accessibility challenges, ultimately revolutionizing documentation for individuals. Yet, it has sparked ongoing discussions about finding the right balance between individual privacy and the benefits of medical research.
Statistics reveal that health professionals encountering more ethical dilemmas are 3.56 times more likely to maintain a positive attitude towards confidentiality compared to those facing fewer dilemmas. Moreover, those with direct client contact exhibit a 3.06 times greater likelihood of valuing confidentiality than their counterparts without such contact. These insights underscore the importance of fostering an atmosphere of trust and respect between individuals receiving care and those delivering it.
A successful method for managing the patient chart format not only addresses data privacy but also enhances disease diagnosis and tailored treatment. By adhering to ethical guidelines rooted in Catholic teachings, we reinforce our commitment to compassionate care. Regular evaluations of patient chart formats are essential for upholding these ethical standards, ensuring that healthcare professionals protect individual information while improving healthcare outcomes.
As specialists remind us, "Nurses have a duty to themselves, their profession, and those they serve to uphold ." By prioritizing confidentiality in documentation, healthcare professionals can profoundly influence the quality of care provided. Let us come together to support one another in this noble endeavor.
Impact of Effective Documentation on Patient Outcomes
Effective documentation in is essential for optimizing outcomes. It’s important to recognize the emotional challenges healthcare providers face when managing documentation. Precise and thorough documentation enables medical professionals to make informed choices regarding diagnosis and treatment, ultimately leading to enhanced health outcomes. For instance, well-documented health histories facilitate precise evaluations and personalized treatment plans, significantly reducing the risk of medical errors.
Moreover, adopting the patient chart format for efficient record-keeping improves communication among healthcare teams. This ensures that all professionals involved in an individual's care are well-informed and coordinated. Such a collaborative approach not only enhances patient safety but also improves patient satisfaction, as individuals feel more secure and confident in the care they receive.
Research indicates that poor record-keeping can lead to significant medical errors. Studies show that inadequate management of the patient chart format is a common factor in adverse patient outcomes. A notable case study highlighted a provider who faced serious repercussions for billing Medicare based on inadequate records. This underscores the importance of maintaining integrity in medical recordkeeping. It serves as a stark reminder that the patient chart format must be both accurate and timely; any alterations made post-audit can lead to severe consequences.
As the saying goes, 'If you didn't document it, it didn't happen.' Ongoing training for medical professionals, especially nurses, is essential in enhancing the patient chart format and improving record-keeping practices. Recent findings reveal that newly appointed nurses exhibit record-keeping skills comparable to their more experienced counterparts. This suggests that targeted training can bridge gaps in record quality. By emphasizing efficient record-keeping, medical practitioners can greatly enhance care quality, minimize mistakes, and promote a culture of responsibility and excellence in clinical practice.
What steps can you take today to improve your documentation practices? Remember, every effort counts towards better patient care.
Key Takeaways: Implementing Best Practices in Patient Chart Formatting
Efficient patient chart format is essential for enhancing service delivery and ensuring high-quality care. As healthcare providers, we often face emotional challenges that can impact our ability to deliver the best care possible. Here are some key takeaways to consider:
- Prioritize Standardization: Implementing standardized templates for is vital for achieving consistency and clarity in records. This method not only improves communication among medical providers but also reduces the risk of mistakes, ultimately resulting in better outcomes for individuals. As emphasized in the wider healthcare framework, implementing a standardized patient chart format can significantly improve patient satisfaction and decrease reporting errors.
- Embrace Technology: Utilizing advanced technologies, such as AI and electronic health record (EHR) systems, can significantly simplify record-keeping processes. For instance, CosmaNeura's platform is developing advanced algorithms for retrospective billing analysis, which aligns with the theme of optimizing records. These tools assist in lessening administrative loads, enabling healthcare professionals to concentrate more on care for individuals. The incorporation of AI in record-keeping has been shown to save providers several hours each day, enhancing overall efficiency and enabling more meaningful patient interactions.
- Focus on Training: Regular training sessions for staff on best practices for record-keeping are crucial. Ongoing education ensures that all team members are informed about the latest standards and techniques, thereby enhancing the quality and precision of the patient chart format. This commitment to training can lead to a more competent workforce and improved interactions with individuals, ultimately enhancing the care model focused on those receiving treatment.
- Maintain Ethical Standards: Upholding ethical guidelines is crucial in medical records. Ensuring confidentiality and trust not only complies with legal requirements but also fosters a positive relationship between providers and individuals. CosmaNeura's dedication to Catholic teachings strengthens the integrity of the healthcare system, ensuring that ethical standards are upheld in all record-keeping practices.
- Evaluate Impact: It is important to continuously assess the influence of record-keeping methods on outcomes and satisfaction of those receiving care. Regular evaluations using the patient chart format can identify areas for improvement and highlight successful strategies. For instance, practices that have embraced standardized templates have reported improved satisfaction among individuals and decreased errors in record-keeping. As mentioned by Moon YJ, 'Preoperative high-sensitivity troponin I and B-type natriuretic peptide, alone and in combination, for risk stratification of mortality after liver transplantation,' highlights the essential importance of precise recording in healthcare.
By adopting these best practices, healthcare providers can significantly enhance the quality of care they deliver. This ensures that patient documentation is not only effective but also aligned with the highest standards of care, while addressing the challenges faced in the healthcare landscape through innovative AI-driven solutions.
Conclusion
Effective patient chart formatting is a vital part of the healthcare system, significantly influencing the quality of care and patient outcomes. By adopting standardized practices, healthcare providers can enhance the clarity and accessibility of patient information. This not only minimizes errors but also fosters a culture of safety. The integration of advanced technologies, especially AI-driven solutions, streamlines documentation processes, enabling healthcare professionals to devote more time to meaningful patient interactions rather than administrative tasks.
Training and continuous education are crucial in ensuring that staff are well-versed in best practices. This ultimately leads to improved documentation quality, which is essential for maintaining patient trust. Ethical considerations, such as upholding patient confidentiality and informed consent, must always be prioritized in documentation practices, reinforcing the bond between healthcare providers and patients.
By implementing these thoughtful strategies, healthcare organizations can significantly enhance their documentation practices. This leads to better clinical outcomes and increased patient satisfaction. The commitment to refining patient chart formatting is not just an operational necessity; it represents a fundamental aspect of delivering compassionate and effective care in today’s complex healthcare environment. Embracing these changes will pave the way for a more efficient, patient-centered healthcare system that prioritizes the well-being of every individual. How can we further support each other in this journey toward excellence in patient care?




