Overview
The article titled "10 Patient's Chart Examples Every Caring Healthcare Provider Should Know" underscores the essential role of patient charts in nurturing effective documentation, communication, and continuity of care within healthcare environments. It compassionately explores various charting methods and best practices, illustrating how meticulous and comprehensive record-keeping can significantly enhance patient outcomes. Moreover, it highlights the importance of safeguarding legal interests and fostering trust between providers and patients.
In today's fast-paced healthcare landscape, providers often face emotional challenges as they navigate administrative burdens that can detract from patient care. This article serves as a reminder that prioritizing accurate charting not only improves individual patient experiences but also strengthens the overall healthcare system.
By embracing these practices, healthcare providers can create a more supportive environment for both themselves and their patients. This article encourages you to reflect on your current charting methods and consider how these examples can inspire positive changes in your own practice.
Introduction
In the intricate world of healthcare, patient charts are not just documents; they are the lifelines of effective communication and quality care. They encapsulate a patient's medical history, treatment plans, and ongoing care, making them indispensable for healthcare providers. Have you ever felt overwhelmed by the sheer volume of information to manage? With the rise of technology and patient engagement, understanding the nuances of patient charting has never been more critical.
As administrative burdens increase, the emotional toll on healthcare providers can be significant. The integration of artificial intelligence offers promising solutions to streamline documentation processes, alleviating some of this pressure. However, it is essential to remain vigilant about the ethical implications of maintaining patient confidentiality. The landscape of patient charting is evolving rapidly, and it is vital to stay informed.
This article delves into the essential components of patient charts, exploring various charting methods and highlighting best practices to avoid common mistakes. Why does this matter? Because meticulous documentation profoundly impacts patient outcomes and safety. As healthcare continues to advance, mastering the art of patient charting is not just beneficial—it is imperative for delivering high-quality care. Let’s embark on this journey together, ensuring that we provide the best for our patients.
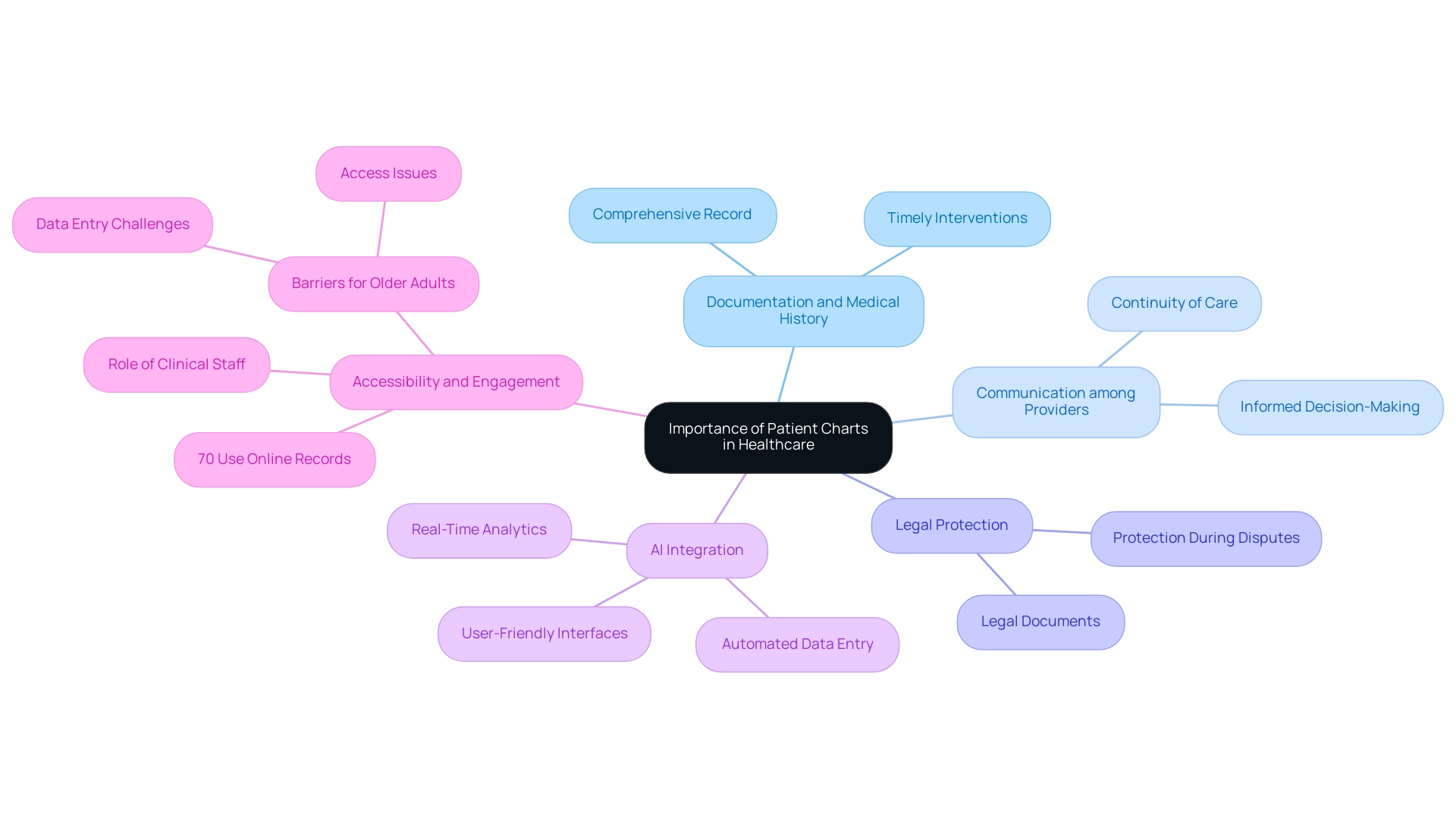
Understanding the Importance of Patient Charts in Healthcare
The example of a patient's chart is crucial for documentation, serving as a comprehensive record of an individual's medical history, treatments, and ongoing support. It plays a vital role in fostering communication among healthcare providers, which is essential for ensuring continuity of care and informed decision-making. A well-maintained patient's chart can significantly enhance outcomes by enabling timely interventions and accurate diagnoses.
Have you ever considered how accessible your medical records are? Recent studies reveal that 70% of individuals utilize their online medical records to review clinical notes. This statistic underscores the importance of accessible and well-documented information about individuals, illustrating how engagement with their records can directly influence health outcomes.
Moreover, a patient's chart exemplifies that client records are not merely administrative tools; they are legal documents that protect medical providers during disputes or audits. The ethical implications of individual-generated data are increasingly recognized, prompting future studies to explore providers' needs in facilitating effective individual data management. As the landscape of client documentation evolves, understanding the patient's chart becomes essential for enhancing the quality of support.
By integrating AI solutions from CosmaNeura, healthcare providers can simplify administrative tasks related to charting, allowing them to focus more on patient care. CosmaNeura's AI solutions feature automated data entry, real-time analytics, and user-friendly interfaces that significantly reduce the time spent on documentation. This transformation not only alleviates physician burnout but also enhances diagnostic accuracy, as illustrated in the patient's chart, leading to improved outcomes.
For instance, a case study titled "Barriers to PHR Use Among Older Adults" revealed that low-income older individuals faced challenges with data entry and access. This highlights the urgent need for a user-friendly patient's chart that boosts user engagement. The findings suggest that improving the usability of medical records can lead to better health outcomes, particularly among vulnerable groups.
Expert opinions further emphasize the importance of a patient's chart in healthcare. As clinical staff encourage individuals to manage their data and prepare for visits by reviewing their charts, the significance of these records becomes even more apparent. Richwine C. noted that individuals' access to and use of health portals and are critical for fostering engagement among users.
By enhancing the accuracy and thoroughness of individual records through AI-driven solutions from CosmaNeura, providers can promote better health results and elevate the overall quality of care offered. Looking ahead to 2025, the impact of record-keeping on medical outcomes will remain a crucial focus, as the integration of technology and individual engagement strategies continues to evolve.
Exploring Different Types of Patient Charting Methods
In the medical field, healthcare providers often face emotional challenges as they strive to efficiently record interactions with individuals. Several charting techniques, such as the patient's chart example, narrative charting, and SOAP notes (Subjective, Objective, Assessment, Plan), can help alleviate some of these burdens while offering distinct advantages.
- Narrative Charting: This method provides a comprehensive and detailed account of interactions, capturing the nuances of clinical encounters. It allows medical providers to express their observations and insights in a free-form style, which can be particularly beneficial for complex cases where a structured format may not suffice.
- SOAP Notes: In contrast, SOAP notes offer a structured framework that aids in clinical assessments. By breaking down information into four distinct categories—Subjective, Objective, Assessment, and Plan—this method facilitates clear communication among medical providers and enhances the continuity of care.
- Electronic Health Records (EHRs): EHRs represent a significant advancement in documentation, enhancing accessibility and streamlining the documentation process. They permit real-time updates, ensuring that all members of the medical team have access to the most recent client information. This capability not only enhances collaboration but also facilitates improved clinical decision-making, as illustrated in a patient's chart example.
As of 2025, the adoption rates of EHRs continue to increase, reflecting a growing acknowledgment of their significance in contemporary medical practice. Statistics show that a significant share of healthcare facilities now employ EHR systems, which are essential for effective treatment and data management. Additionally, statistical information collection in hospitals often utilizes data processing systems for tracking care and reporting, emphasizing the importance of effective methods, as seen in a patient's chart example.
Recent case studies underscore the effectiveness of different charting methods. For instance, a study on the preparation of a prediction calendar demonstrated how hospitals can anticipate flow by comparing projected numbers with actual visits. This proactive approach aids in operational management and strategic planning, showcasing the practical benefits of effective charting methods.
Notably, eighteen participants (41.9%) indicated they would recommend a similar workshop to their colleagues, reflecting the perceived value of these charting techniques.
Furthermore, it is important to recognize that the content of can vary based on the type of ambulatory practice, whether it is a solo practitioner or part of a medical group. This variability adds context to the discussion of charting methods and their applications.
In summary, understanding the various charting methods—narrative charting, SOAP notes, and EHRs—is crucial for healthcare providers. By enhancing documentation practices, as illustrated in a patient's chart example, we can collectively work towards improving care outcomes and supporting one another in this vital endeavor.
Key Components to Document in a Patient's Chart
Key components of a patient's chart encompass essential elements such as demographic information, medical history, medications, allergies, vital signs, treatment plans, and progress notes. Each entry must be clear and concise, offering a comprehensive view of the individual's health status. In 2025, the importance of recording interactions with individuals has become increasingly clear. Studies show that comprehensive records can improve outcomes and satisfaction, which is vital for fostering trust and understanding in healthcare.
Efficient record-keeping of client concerns and preferences not only supports a client-centered approach but also aligns with best practices that enhance communication and trust between providers and clients. Have you considered how your documentation practices impact your relationships with patients? By focusing on their needs, we can create a more supportive environment.
Moreover, statistics reveal that data collection from medical records via electronic means is still not the norm in many medical environments. This highlights the urgent need for improved documentation practices. By ensuring that all relevant information is captured accurately, healthcare providers can minimize errors and enhance the integrity of care, ultimately benefiting both patients and practitioners.
Incorporating insights from case studies, it is clear that the training and management of data abstractors play a crucial role in maintaining the quality of medical records. Properly trained personnel can significantly reduce data collection errors, thereby enhancing the overall reliability of medical charts. As Lucy Radovinsky, MSN, RN, notes, "The strategies outlined in this article and summarized in Table 1 will help ensure interrater reliability when abstracting data from ." This highlights the significance of training in attaining high-quality records.
Furthermore, we cannot ignore the significance of consumer involvement in record-keeping methods. For instance, Practice Fusion offers individuals access to Portals, enabling them and authorized representatives to view, download, and transmit their health record data. This initiative not only empowers individuals but also encourages better documentation practices among providers.
As medical services continue to evolve, understanding what to record in a patient's chart and adhering to these key components will be vital for delivering high-quality support. Let us foster positive relationships between provider and individual, ensuring that every patient feels valued and understood.
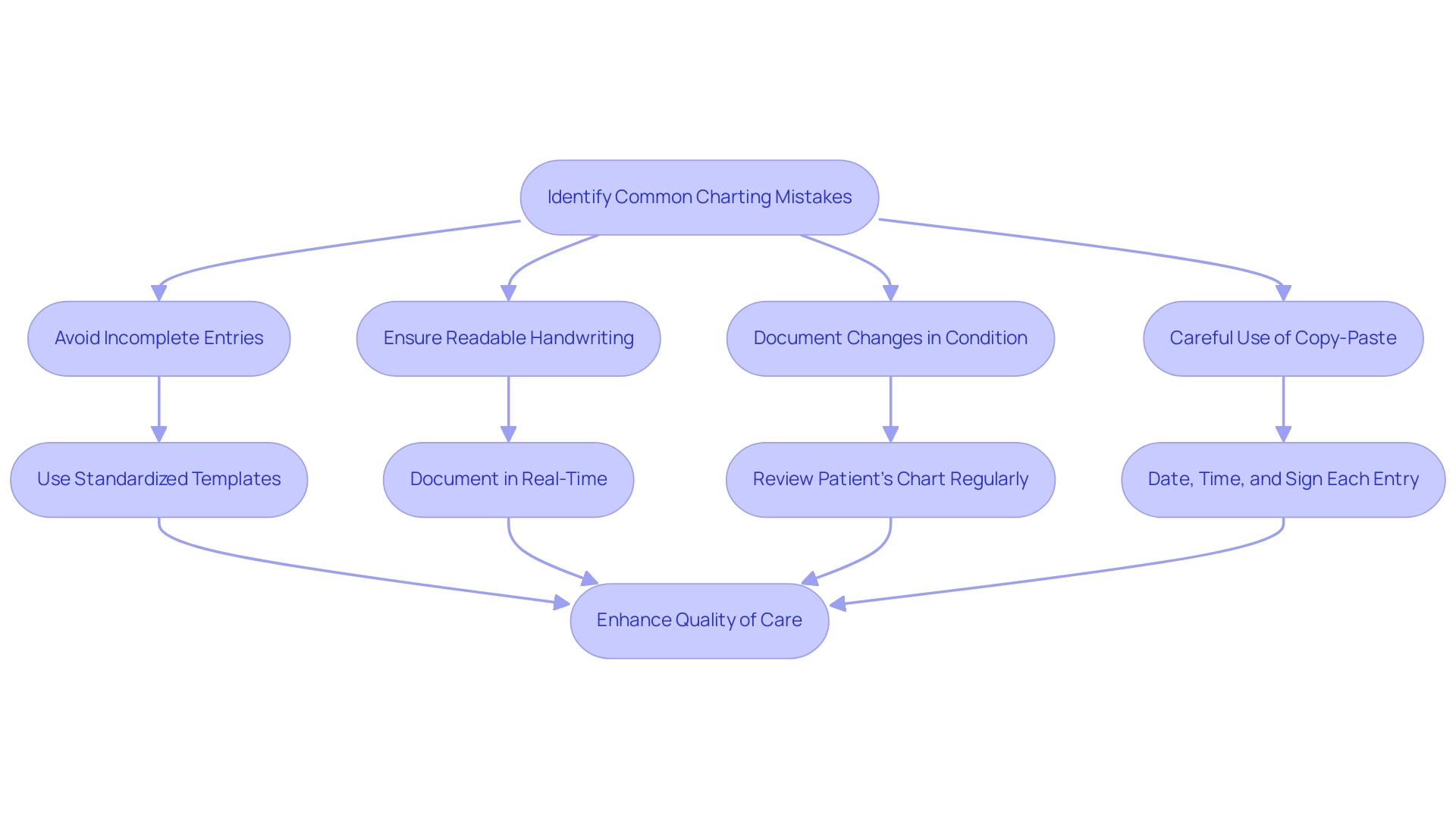
Avoiding Common Charting Mistakes: Best Practices
In healthcare, common charting errors can deeply impact safety and the quality of care we provide. Mistakes such as incomplete entries, unreadable handwriting, and neglecting to document changes in a person's condition are all too frequent. A study revealed that 12 individuals (3.4%) identified errors related to sidedness, underscoring the vital importance of precision in record-keeping.
Moreover, the careless use of the copy-paste feature in electronic health records has been shown to lead to significant errors, which can harm individuals. This situation highlights the critical need for diligent record-keeping practices. A case study titled 'Careless Use of Copy-Paste' warns that such mistakes can result in serious consequences, reinforcing the necessity for careful documentation methods.
To mitigate these risks, healthcare professionals should adopt best practices for accurate charting. Utilizing standardized templates can streamline the documentation process, ensuring consistency and clarity. It is essential to document in real-time; delays in recording information can lead to omissions and inaccuracies.
Regularly reviewing the patient's chart for precision is crucial, as it allows providers to identify and correct mistakes before they affect care. Each entry should be dated, timed, and signed to uphold accountability. As one individual poignantly noted, 'It is almost impossible to change incorrect information [about surgical candidacy]. It took months to do so,' highlighting the long-term repercussions of documentation errors.
Furthermore, it is vital to remember that mistakes in medication administration should never be concealed by altering medical records, as this can lead to serious ethical dilemmas. A notable case involved an admitting nurse who modified an individual's records to hide , resulting in a lawsuit that settled for over $1 million.
By adhering to these best practices, healthcare providers can enhance the quality of service and ensure that records reflect the highest standards of accuracy and reliability. Together, we can create a safer, more compassionate healthcare environment.
10 Essential Patient Chart Examples for Effective Documentation
- Initial Assessment Note: This foundational document serves as a patient's chart example, capturing the individual’s chief complaint, history of present illness, and relevant medical history. It establishes the groundwork for efficient care by ensuring that all essential information is readily accessible. Have you ever felt overwhelmed by the documentation process? By utilizing AI-driven solutions from CostaNera, medical providers can streamline this process, significantly reducing the time spent on initial assessments and allowing for more focus on the patient's chart example and client interaction.
- SOAP Note: Utilizing the SOAP (Subjective, Objective, Assessment, Plan) format to organize evaluations of individuals can be illustrated with a patient's chart example. This approach not only arranges information but also improves communication among healthcare providers, resulting in better outcomes for those receiving care. Imagine how much smoother the process could be! AI innovations from CosmaNeura can assist in automating parts of this documentation, ensuring that vital information is captured efficiently and accurately.
- Medication Administration Record: Accurately tracking medications administered, including dosages and times, is essential for ensuring safety and adherence to treatment protocols. CosmaNeura's AI solutions can help monitor medication adherence and flag potential issues, thus enhancing care for individuals.
- Progress Note: The patient's chart example should summarize changes in the individual's condition and their response to treatment. Regular updates are crucial for tracking progress and modifying plans as needed. Have you considered how AI from CosmaNeura can facilitate the documentation of the patient's chart example notes? This allows for quicker updates and better tracking of outcomes.
- Discharge Summary: Providing a comprehensive overview of the patient's hospital stay, including diagnoses, treatments received, and follow-up guidance, is crucial for continuity of support post-discharge. AI tools from CosmaNeura can assist in generating the patient's chart example efficiently, ensuring that all relevant information is communicated effectively to the next provider.
- Referral Note: Documenting the reason for referral and any pertinent medical history, while including a patient's chart example, is vital. Clear communication in referrals ensures that specialists have the necessary context to provide optimal care. CosmaNeura's AI can streamline this process by automatically filling in relevant client data, reducing the administrative burden on providers.
- Consent Form: Documenting individual consent for procedures or treatments within the patient's chart example not only protects the provider legally but also strengthens the individual's autonomy in their healthcare decisions. AI solutions from CosmaNeura can simplify the consent process, making it easier for individuals to understand their options and providing a patient's chart example for providers to document consent accurately.
- Nursing Note: Including observations and interventions performed by nursing staff in the patient's chart example is crucial for monitoring health management. These notes ensure that all team members are informed of the individual's condition. AI from CosmaNeura can improve the efficiency of nursing records, allowing for more time dedicated to direct care.
- Lab Results: Recording and analyzing laboratory findings pertinent to the individual's treatment aids in timely decision-making and enhances the overall quality of care. AI from CosmaNeura can assist in analyzing lab results and flagging critical values for immediate attention in a patient's chart example.
- Education Record: Noting any information given to the individual regarding their condition or treatment plan is essential for enabling individuals to comprehend their health management. AI-driven tools from CosmaNeura can assist in customizing educational materials to individual requirements, enhancing engagement and comprehension.
In 2025, the significance of initial assessment notes in treatment cannot be overstated. Statistics show that the average duration needed to evaluate each file in a medical record review was 13.02 minutes in the early phases, greatly enhancing to 5.06 minutes in subsequent stages, emphasizing the efficiency achieved through effective record-keeping practices. Moreover, case studies, like the Korea National Patient Safety Incidents Inquiry Survey, highlight the importance of in identifying adverse events, emphasizing the essential role of detailed records in improving safety and service quality.
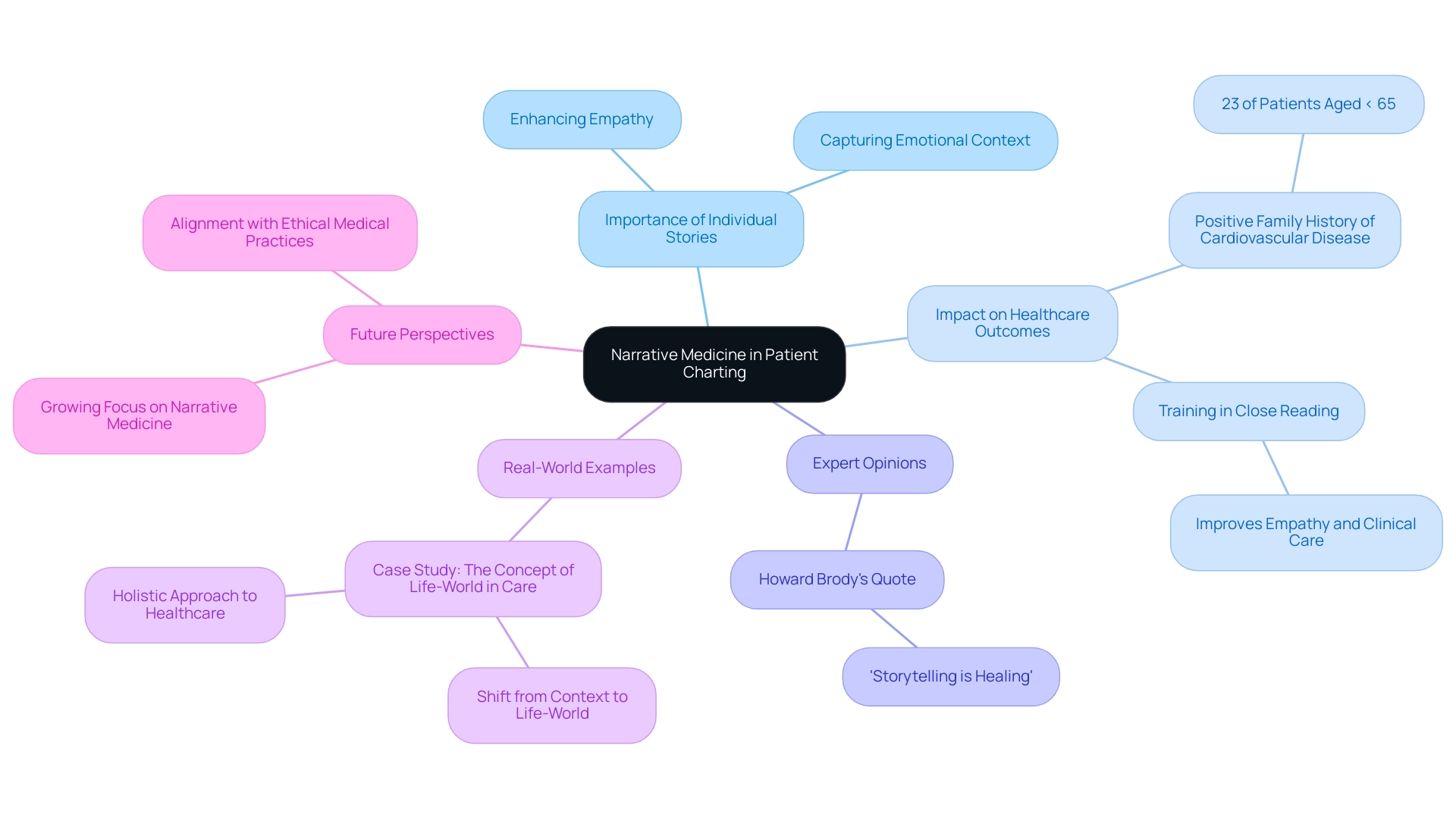
Incorporating Narrative Medicine into Patient Charting
Narrative medicine represents a transformative approach that highlights the importance of integrating individual stories into clinical documentation. By capturing the emotional and contextual dimensions of a person's experience, healthcare providers can nurture deeper empathy and understanding—key elements in tailoring care to meet specific needs. This method encourages providers to document brief narratives in the patient's chart that reflect significant experiences, concerns, and preferences, enriching the clinical record in a meaningful way.
The impact of narrative medicine on healthcare outcomes is truly significant. For instance, research shows that 23% of individuals under 65 reported a positive family history of cardiovascular disease, underscoring the necessity of understanding backgrounds in clinical decision-making. Furthermore, training in close reading has been proven to enhance clinicians' abilities to interpret complex narratives, ultimately fostering greater empathy and improving clinical care.
Expert opinions consistently emphasize the vital role of storytelling in medical care. As Howard Brody, a physician and literary scholar, wisely states, 'Storytelling is healing.' This highlights how the narratives individuals construct about their illness experiences can profoundly shape their overall health journey.
Real-world examples illustrate the successful incorporation of personal narratives into a patient's chart for healthcare documentation. A notable case study titled "The Concept of Life-World in Care" advocates for a shift from merely documenting contextual data to engaging with the rich, interpretive narratives that define an individual's lived experience. This comprehensive method not only enhances the quality of support but also aligns with the principles of narrative medicine, emphasizing the importance of understanding an individual's life-world.
This understanding holds particular significance for primary care providers, enabling a more holistic approach to care that resonates with the mission of CosmaNeura to enhance experiences while adhering to ethical medical practices.
As we look to 2025, the focus on narrative medicine within patient charts continues to grow. Providers are increasingly recognizing its role in improving outcomes for individuals. By weaving individual narratives into clinical documentation, providers can foster a more comprehensive and empathetic understanding of those they serve, ultimately leading to and outcomes. This approach not only aligns with the evolving landscape of primary care but also reflects a commitment to Catholic teachings that guide ethical medical practices.
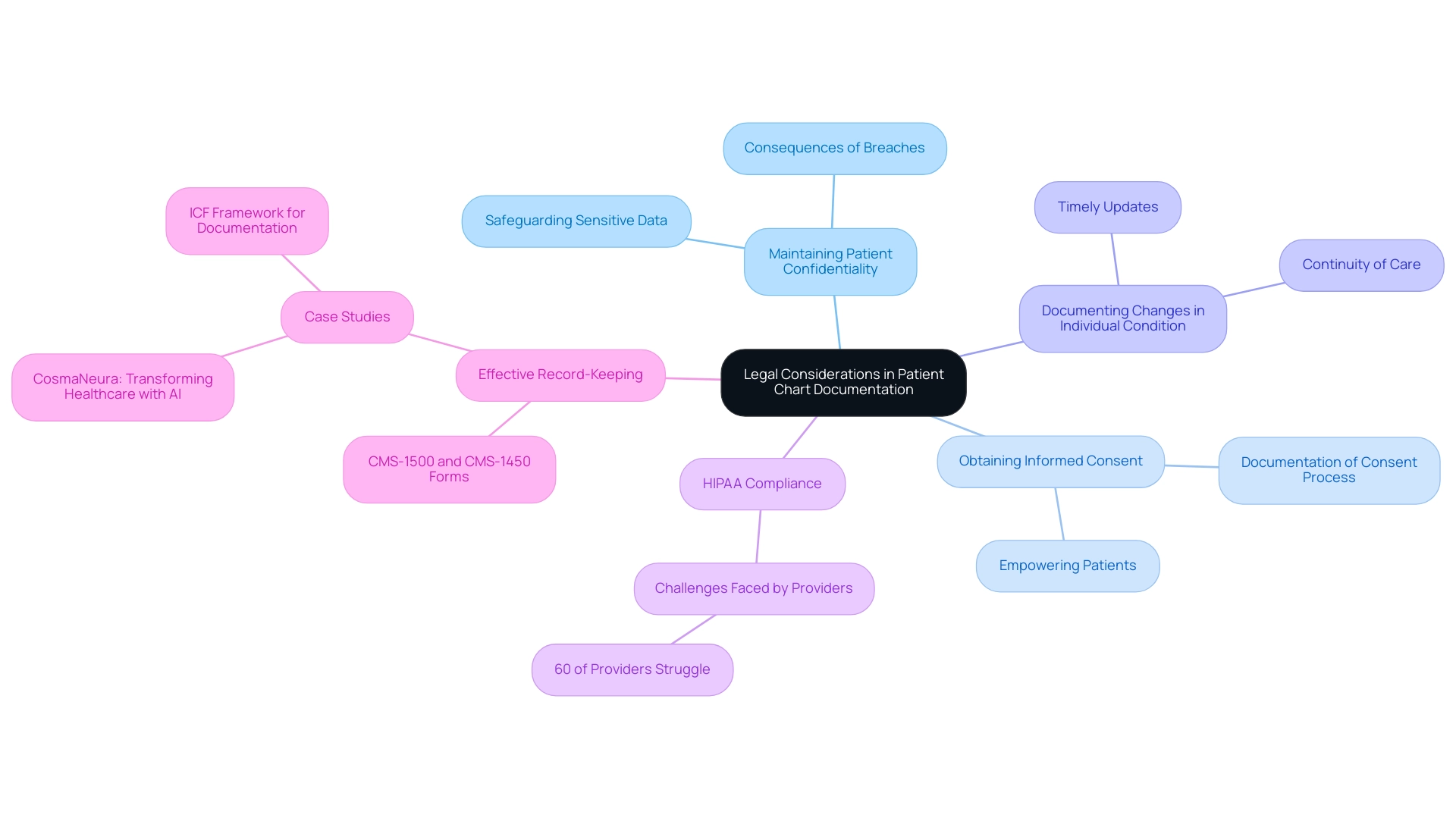
Legal Considerations in Patient Chart Documentation
Patient charts, including the example of a patient's chart, are not just records; they are vital legal documents that must adhere to strict regulations and standards. As healthcare providers, it’s our responsibility to ensure that every entry is accurate, complete, and timely. This diligence is crucial in mitigating potential legal repercussions. Let’s explore some key legal considerations that can make a difference:
- Maintaining Patient Confidentiality: Protecting patient information is of utmost importance. We must implement strong measures to safeguard sensitive data in the patient’s chart example, especially in electronic health records (EHRs). Breaches can lead to serious legal consequences, and we want to avoid that for our patients and ourselves.
- Obtaining Informed Consent: Documenting informed consent is essential for our legal protection. It’s important to ensure that individuals fully understand the procedures and treatments they are agreeing to, with clear documentation of this process. This not only protects us but also empowers our patients.
- Documenting Changes in Individual Condition: Timely updates regarding any changes in a patient’s condition are crucial. This practice not only aids in continuity of care but also serves as a legal safeguard. The patient’s chart example highlights how we actively monitor and respond to patient needs, reinforcing our commitment to their well-being.
Statistics from 2025 reveal that approximately 60% of medical providers faced challenges in maintaining HIPAA compliance within their electronic health records systems. This underscores the ongoing need for training and resources to ensure we adhere to regulations. Furthermore, understanding the CMS-1500 claim form for non-institutional providers, alongside the CMS-1450 form for institutional providers, emphasizes the importance of precise record-keeping practices across various healthcare settings.
The legal factors in the patient’s chart example are further illuminated by case studies, such as the implementation of the ICF framework in speech-language pathology. This framework promotes a comprehensive approach to patient care by categorizing health and disability areas, aiding in effective treatment planning and record-keeping practices. Additionally, CosmaNeura's AI platform serves as a practical example, assisting healthcare providers in maintaining compliance and enhancing record-keeping practices. This aligns with the company’s mission to alleviate administrative burdens while upholding ethical standards.
Expert insights reveal the significance of effective record-keeping in safeguarding against malpractice risks. As , MD, points out in "Charting Practices to Protect Against Malpractice: Case Reviews and Learning Points," using a patient’s chart example to focus on common problematic areas can significantly reduce the chances of legal issues stemming from inadequate record-keeping.
In conclusion, it is essential for medical providers to prioritize HIPAA compliance and legal factors in chart records. By doing so, we not only protect ourselves legally but also enhance the standard of treatment we provide to our patients. Let’s continue to support each other in navigating these challenges together.
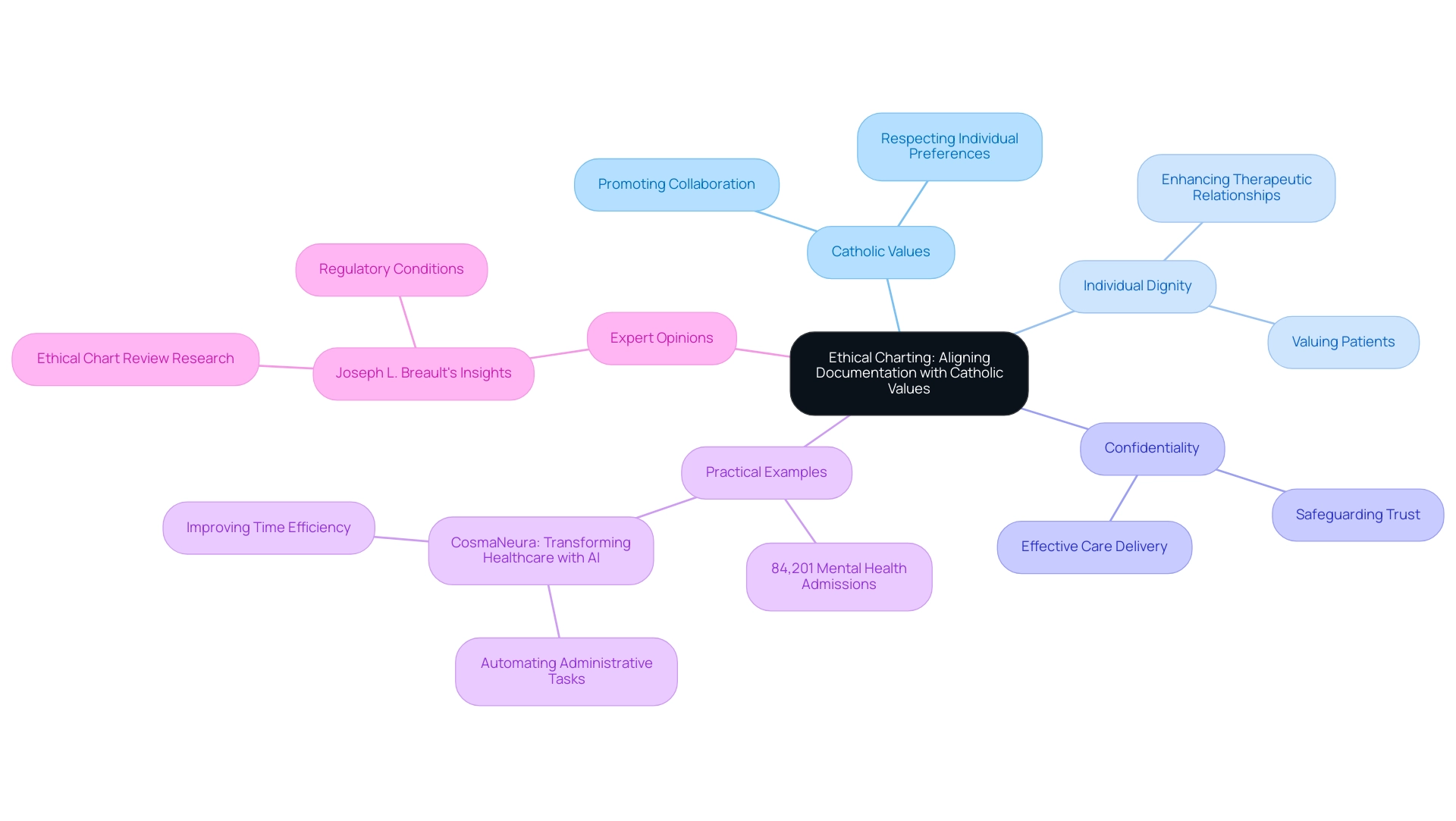
Ethical Charting: Aligning Documentation with Catholic Values
Ethical charting stands as a cornerstone of healthcare records, particularly when it aligns with Catholic values that prioritize individual dignity and autonomy. How can healthcare professionals embody these principles in their interactions? By recording interactions in a way that promotes collaboration in decision-making, they not only respect individual preferences but also enhance the therapeutic relationship. This approach fosters an environment where patients feel valued and understood.
Moreover, the ethical implications of record-keeping practices deserve careful consideration. Providers must ensure that their charting safeguards confidentiality and trust—two vital elements for effective care delivery. In 2025, the significance of ethical charting practices is highlighted by the statistic of 84,201 mental health admissions recorded. This underscores the essential need for sensitive and respectful records in mental health services, where ethical considerations are crucial for building trust and ensuring safety.
Expert opinions further support the importance of ethical charting. Joseph L. Breault, Chair of the Medicine & Institutional Review Board at Ochsner Clinic Foundation, notes that societies carefully weigh the benefits and risks of chart review research. He concludes that such research is ethical when it adheres to specific regulatory conditions. This perspective aligns with the Catholic commitment to ethical practices in medical services, ensuring that records meet both individual needs and moral standards of support.
Practical examples illustrate how aligning records with Catholic principles can enhance individual support. Consider CosmaNeura, that aids healthcare providers in implementing ethical charting practices. By automating administrative tasks and ensuring compliance with ethical guidelines, it alleviates some pressures on physicians, allowing them to focus more on patient care. How might this shift impact the quality of interactions?
This alignment not only guarantees adherence to regulatory standards but also cultivates a culture of respect and compassion in provider-patient interactions. Ultimately, this leads to improved patient outcomes and satisfaction, reinforcing the integral role of ethical considerations in medical documentation.
Additionally, understanding the shape of data distribution can influence the choice of the most appropriate measure of central tendency, further informing ethical charting practices. Grasping this concept enables providers to make more informed choices in their record-keeping processes. Furthermore, the ethical conclusion in the United States regarding chart review research emphasizes that such practices are acceptable if they meet specific regulatory conditions, further supporting the necessity for ethical charting in medical settings.
Continuous Improvement in Patient Charting Practices
Enhancing patient charting methods is essential for improving the precision and effectiveness of medical recording. Many healthcare providers face emotional challenges due to the pressures of record-keeping. By consistently assessing and revising these protocols, service providers can adapt to changing standards and technologies, ultimately easing some of this burden.
Participating in ongoing training and education is vital. Research indicates that such efforts significantly influence charting precision, with organizations observing up to a 63% decrease in recording errors after focused training programs. Isn’t it encouraging to see such tangible improvements?
This statistic reflects the success seen in Continuous Quality Improvement (CQI) initiatives, which achieved a remarkable 63% reduction in pressure ulcer prevalence from 2008 to 2010. These examples highlight the profound benefits of continuous improvement efforts.
As we move toward 2025, the emphasis on ongoing education remains crucial, especially as medical records evolve alongside technological advancements. The latest training programs focus on integrating electronic health records (EHRs) and standardized templates. These innovations simplify record-keeping processes and alleviate the administrative load on providers. For instance, a recent workshop at the 2024 Internal Medicine Society of Australia and New Zealand (IMSANZ) conference showcased the use of run charts and statistical process control (SPC) charts, helping general physicians better understand variations in medical data.
Post-workshop surveys revealed that over 95% of participants felt more confident in utilizing . This underscores the need for comprehensive training in documentation practices, fostering a culture of growth and support.
Implementing feedback mechanisms, such as peer reviews and audits, serves as another effective strategy for identifying areas for improvement. These practices not only nurture accountability but also promote collaboration among medical teams. As Bonetti wisely noted, "Overall process quality cannot be measured directly; we must resort to the use of quality indicators as easy to assess surrogate markers reflecting overall quality."
This perspective reinforces the importance of using measurable indicators to drive ongoing improvement in patient charting practices. However, we must also acknowledge the barriers to SPC application, such as knowledge gaps and data collection difficulties. Addressing these challenges is crucial for the successful implementation of continuous improvement practices.
In summary, adopting new tools and technologies, along with a commitment to ongoing training, is vital for providers aiming to enhance their documentation practices. By prioritizing continuous improvement, providers can ensure that their charting processes remain efficient, accurate, and aligned with best practices in the ever-evolving field of medical services. Let’s embrace this journey together, fostering an environment of support and growth.
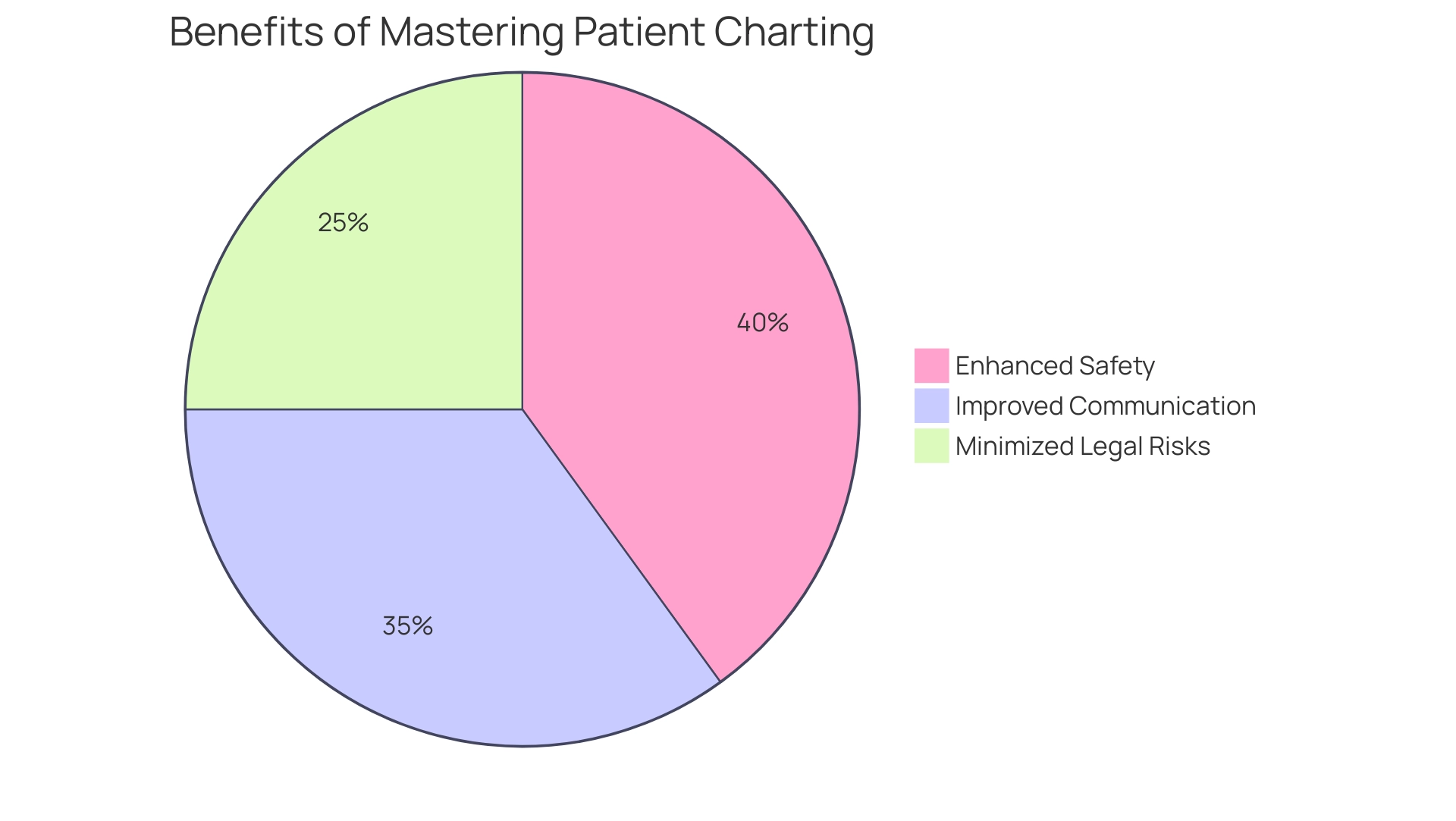
The Benefits of Mastering Patient Charting for Healthcare Providers
Mastering the patient's chart example is crucial for healthcare providers, as it brings about significant benefits such as enhanced safety, improved communication among care teams, and minimized legal risks. Effective documentation, including a patient's chart example, empowers providers to make informed clinical decisions, which directly correlates with better outcomes for individuals. Consider this: studies have shown that involvement in data quality efforts can lead to a reduction in medication errors, with many expressing a strong willingness to participate in error prevention initiatives.
This aligns with findings from six articles published on number line visualizations in 2018, which underscore the importance of clear data representation in improving outcomes.
Moreover, streamlined charting practices, as illustrated by a patient's chart example, not only save valuable time but also allow providers to focus more on patient support rather than administrative burdens. By automating time-consuming tasks like appointment scheduling and medical record management, CosmaNeura enables providers to regain several hours each week, significantly enhancing their ability to offer compassionate care. This automation is a vital aspect of CosmaNeura's AI solutions in healthcare, designed to alleviate the administrative workload and empower providers to concentrate on patient-centered services.
The impact of effective documentation on safety is profoundly illustrated in a patient's chart example. Research indicates that including evaluative cues in visual displays can reduce perceived urgency for non-critical out-of-range results, promoting a more measured approach to care. A compelling case study, 'Including Harm Anchor Reference Points in Visual Displays,' demonstrated that providing evaluative cues regarding test results lessened perceived urgency, showcasing the essential role that meticulous charting, as exemplified by a patient's chart example, plays in the medical delivery system.
Furthermore, EHR vendors like CosmaNeura must offer necessary functionalities to support contributions to data quality efforts, reinforcing the role of technology in enhancing charting practices. Ultimately, mastering the patient's chart example not only fosters but also embodies the compassionate spirit vital to centered care. As noted by Masterson Creber, funding research in this area emphasizes the importance of patient engagement in improving data quality and reducing medication errors, further highlighting the need for effective documentation practices.
- Enhance safety through effective documentation.
- Improve communication among care teams.
- Minimize legal risks with meticulous charting.
Reflect on how these solutions can transform your practice and patient interactions. Together, we can create a healthcare environment that prioritizes compassion and quality care.
Conclusion
Patient charts are at the heart of effective healthcare communication and quality care. They serve as essential tools for documenting medical histories, treatment plans, and ongoing patient interactions. Have you considered how understanding various charting methods—from narrative styles to SOAP notes and electronic health records—can empower you? This knowledge equips healthcare providers to choose the most effective documentation practices, streamlining processes and enhancing patient engagement and outcomes. It truly demonstrates the critical nature of accurate and accessible patient information.
Moreover, the importance of avoiding common charting mistakes cannot be overstated. By adhering to best practices and incorporating continuous improvement strategies, you can significantly reduce errors and enhance the integrity of patient care. Training and the integration of advanced technologies, such as AI solutions, play a pivotal role in transforming documentation practices. This transformation enables you to focus more on patient care rather than administrative burdens, fostering a more compassionate healthcare environment.
As the landscape of healthcare continues to evolve, the emphasis on ethical charting aligned with patient dignity and autonomy remains paramount. The integration of narrative medicine fosters a deeper understanding of patients' experiences, promoting empathy and personalized care. Ultimately, mastering patient charting is not just about compliance or efficiency; it is about ensuring high-quality care that respects and responds to the individual needs of patients. This reinforces your commitment to delivering compassionate and effective healthcare. How can you further enhance your charting practices to better serve your patients today?




