Overview
The article titled "10 Essential Speech SOAP Note Examples for Therapists" offers a compassionate approach to supporting therapists in their documentation practices. It recognizes the emotional challenges healthcare providers face and emphasizes the importance of structured documentation in enhancing communication. By providing practical examples and guidelines, the article aims to alleviate the administrative burdens that can impact patient care.
Structured SOAP notes not only ensure compliance with standards but also improve patient care by offering clear frameworks for recording subjective, objective, assessment, and planning information. This clarity allows therapists to focus more on their patients and less on paperwork, fostering a nurturing environment for healing.
As you explore these essential examples, consider how implementing these strategies can transform your practice. How might clearer documentation enhance your interactions with patients? By embracing these guidelines, you can create a more effective and empathetic approach to speech therapy, ultimately benefiting both you and your patients.
Introduction
In the realm of speech therapy, effective documentation is not merely a formality; it stands as a cornerstone of quality care. Therapists often find themselves navigating the delicate balance of providing compassionate treatment while managing the complexities of paperwork. This can be emotionally taxing, as the administrative burdens can detract from the focus on patient care.
This article explores essential SOAP note examples that not only streamline documentation but also enhance therapeutic outcomes. What common pitfalls do therapists encounter in their note-taking? By adopting structured practices, how can we transform our approach to client care? These questions invite reflection on our experiences and the potential for improvement in our daily routines.
Together, let’s delve into solutions that can alleviate some of these challenges and foster a more nurturing environment for both therapists and clients alike.
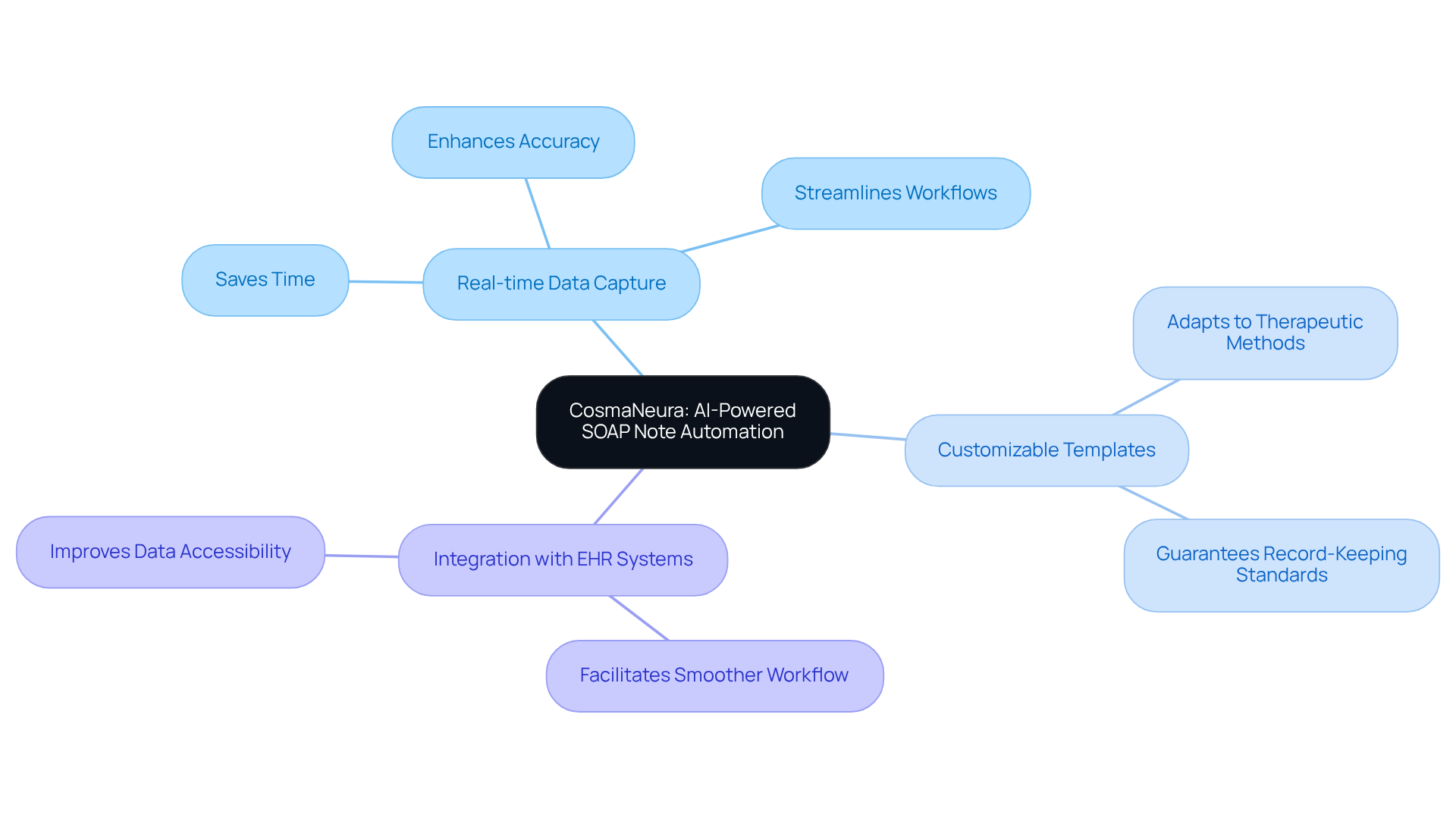
CosmaNeura: AI-Powered SOAP Note Automation for Therapists
CosmaNeura harnesses advanced AI technology to automate the generation of SOAP notes, empowering therapists to prioritize client care over administrative tasks. This innovative approach alleviates the emotional strain of managing paperwork, allowing therapists to focus on what truly matters—their clients. By streamlining client intake and record-keeping processes, CosmaNeura supports therapists in effectively managing their workloads while upholding ethical standards. This automation not only saves precious time but also enhances the accuracy of records, ultimately leading to improved outcomes for those receiving care.
- Real-time Data Capture: Automatically records client interactions during sessions, ensuring thorough and accurate documentation.
- Customizable Templates: Adapts to various therapeutic methods, guaranteeing adherence to specific record-keeping standards.
- Integration with EHR Systems: Seamlessly connects with existing electronic health record systems, facilitating a smoother workflow.
The integration of AI into therapeutic records is transforming the care landscape for individuals. Research indicates that AI can free up to 25% of clinician time, fostering more compassionate and understanding interactions. As healthcare providers increasingly recognize the advantages of AI, 68% of physicians report observing improvements in care, reflecting a growing acceptance of technology in enhancing therapeutic practices. Together, we can to create a more nurturing environment for both therapists and their clients.
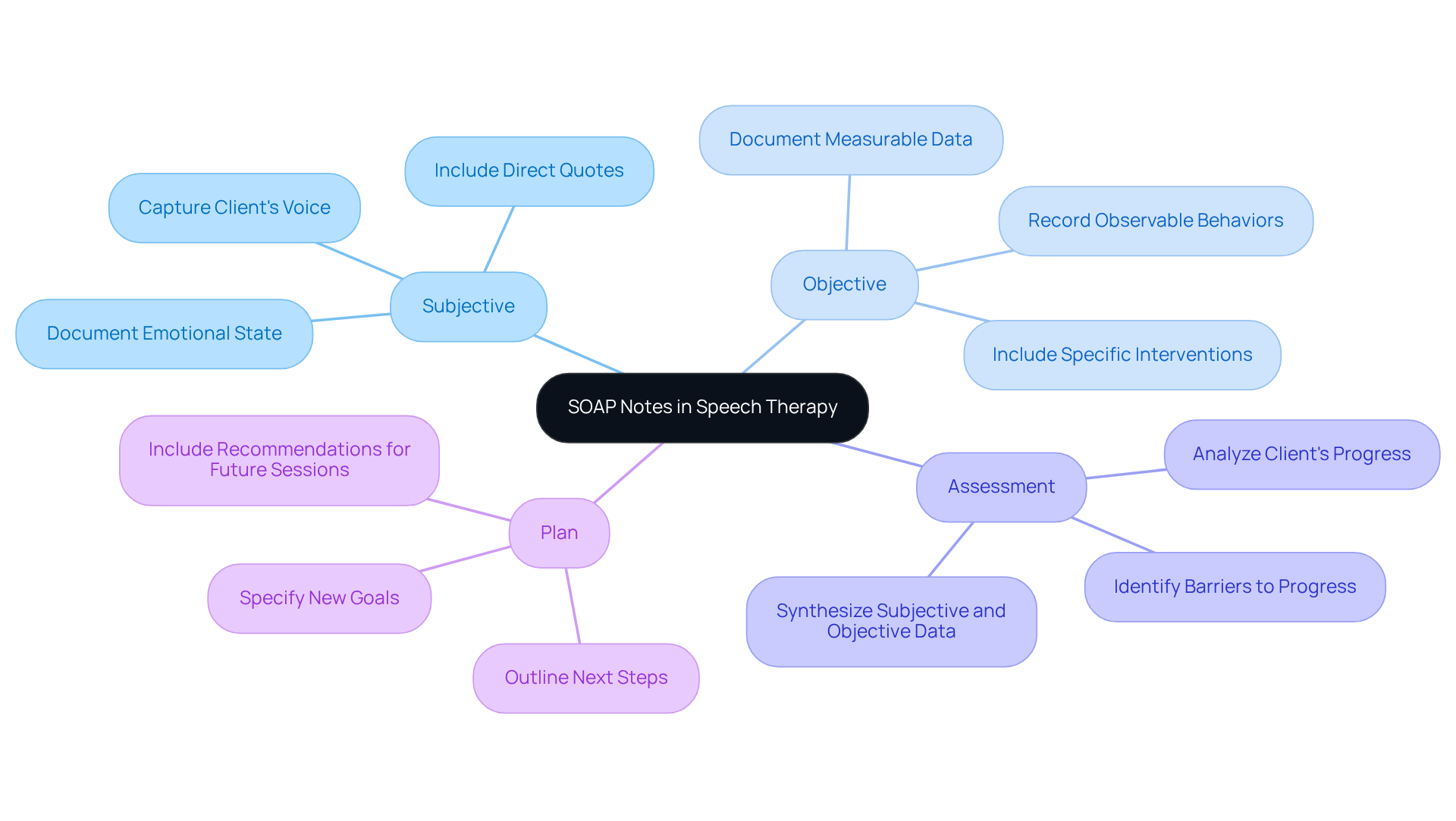
Medesk: Comprehensive Guide to Writing Speech Therapy SOAP Notes
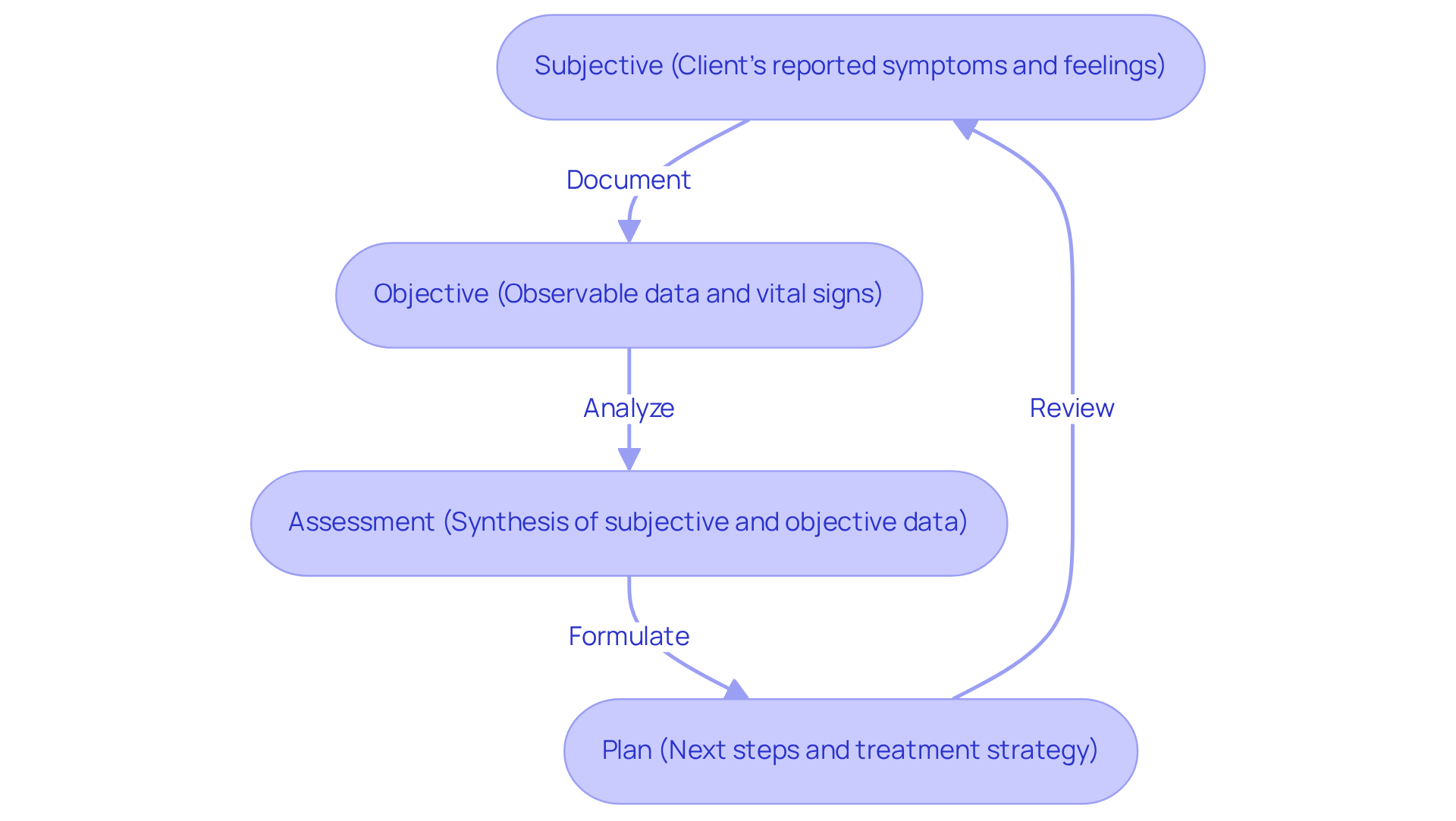
A systematic method for composing effective speech soap note examples in speech therapy is essential for fostering clear communication and meeting record-keeping standards. It’s important to recognize the emotional challenges healthcare providers face in this process. Here’s a breakdown of each component:
- Subjective: Capture the patient's reported feelings, concerns, and experiences. This section should reflect the client's voice, including when possible, to provide insight into their perspective and emotional state.
- Objective: Document measurable data and observable behaviors from the session. This includes specific interventions used, quantitative assessments, and any relevant physical observations, ensuring that the information is clear and unbiased.
- Assessment: Analyze and synthesize the subjective and objective data to evaluate the client's progress toward treatment goals. This section should highlight any barriers to progress and strategies to overcome them, providing a comprehensive view of the client's condition.
- Plan: Outline the next steps in treatment, specifying new goals or modifications to existing strategies. This section should include actionable recommendations for future sessions, such as home exercises or referrals to other professionals.
By adhering to this structured format, therapists can enhance the quality of their speech soap note examples. This not only ensures compliance with insurance requirements but also facilitates effective collaboration with other healthcare providers, ultimately benefiting patient care.
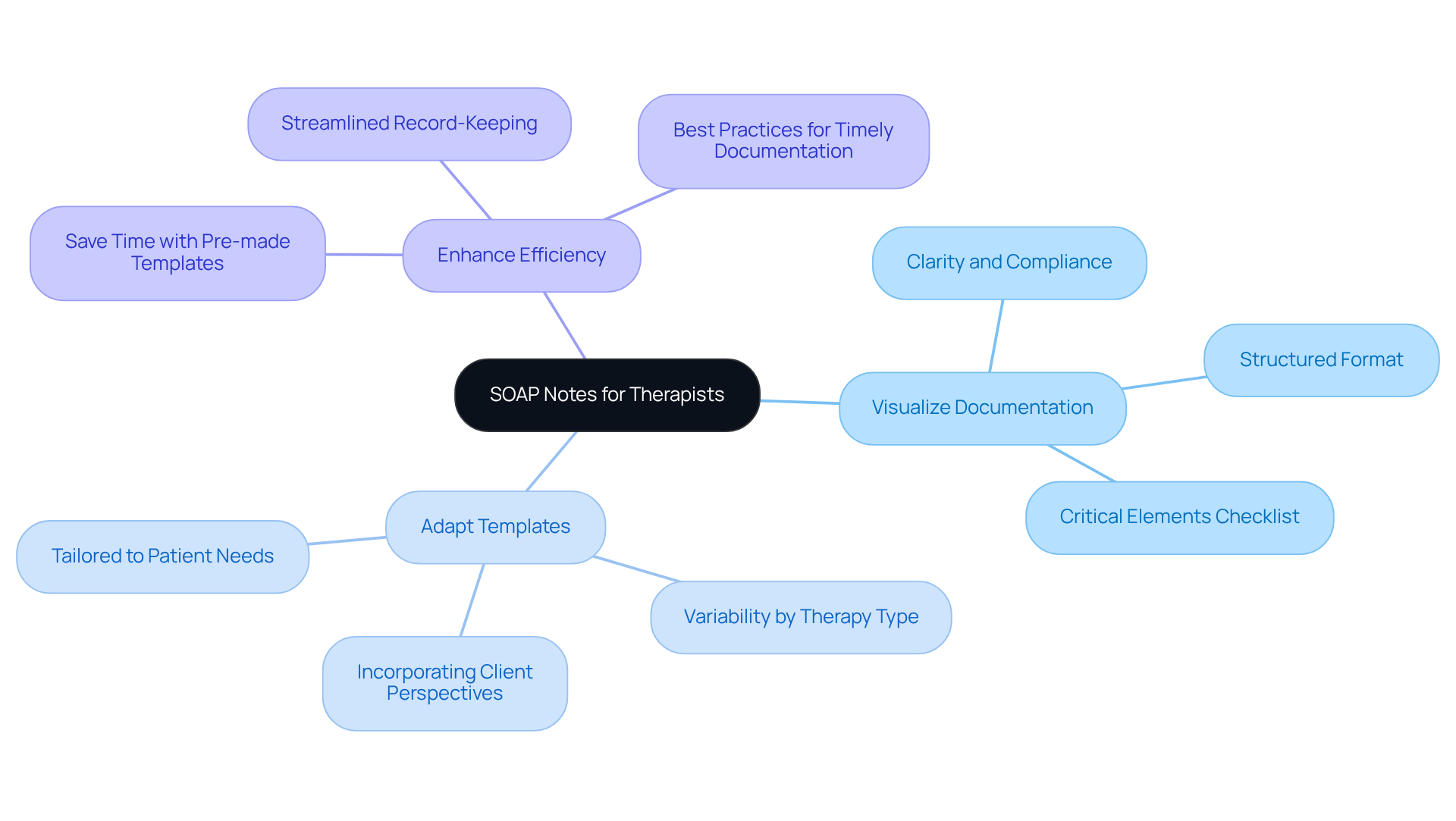
Mentalyc: Diverse SOAP Note Examples and Templates for Therapists
Mentalyc understands the emotional challenges that therapists face in their practice. We aim to ease the administrative burdens that can impact patient care with an extensive selection of and templates tailored for various therapy situations. These resources empower therapists to:
- Visualize Documentation: Gain insights into structuring notes effectively for diverse conditions and treatments, ensuring clarity and compliance with insurance standards.
- Adapt Templates: Tailor templates to meet the unique needs of individual patients and align with different therapy styles, capturing the client's perspective accurately.
- Enhance Efficiency: Utilize pre-made templates to [streamline record-keeping processes](https://blog.cosmaneura.com/10-essential-medical-soap-note-templates-for-healthcare-providers), saving time while ensuring consistency and accuracy. Best practices recommend dedicating 5 to 7 minutes for composing progress records to prevent backlog and guarantee prompt recording.
Consider the practical tools available for documenting conditions like stuttering, dysphagia, and articulation disorders using speech soap note examples. These examples not only improve clinical practice but also support therapists in navigating the complexities of documentation. The organized format of clinical records not only enhances efficiency but also guarantees compliance with insurance and legal requirements, underscoring the significance of quality documentation. Embrace these resources to foster a more compassionate and effective therapeutic environment.
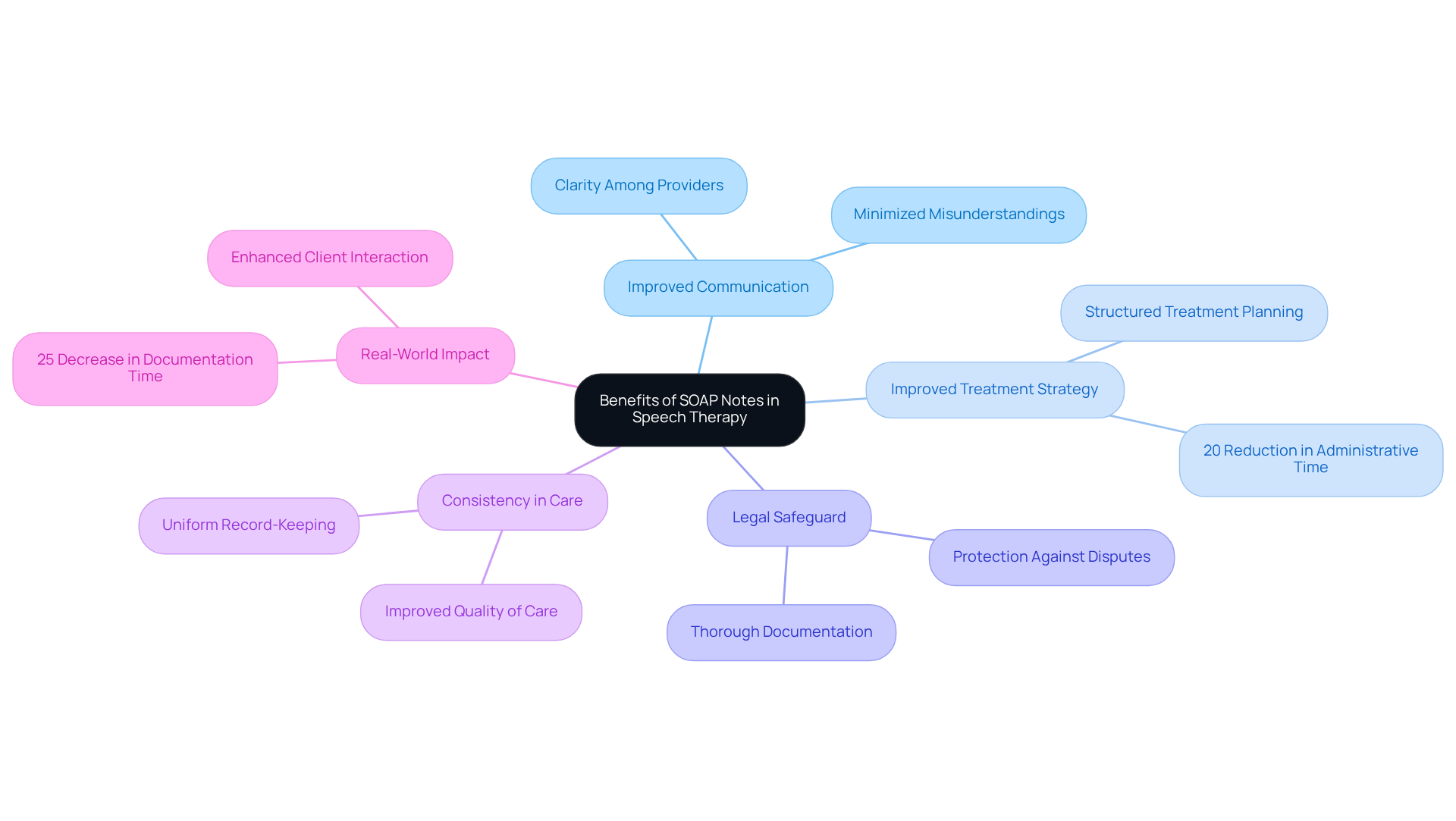
Quenza: Benefits of SOAP Notes in Speech Therapy
The use of speech soap note examples in speech therapy provides several significant advantages that can truly make a difference in patient care.
- Improved Communication: Have you ever felt the frustration of miscommunication among healthcare providers? Using speech soap note examples enhances clarity, ensuring that all team members are updated on a patient's progress. This structured format minimizes misunderstandings, which is crucial in collaborative care settings.
- Improved Treatment Strategy: Imagine a world where treatment planning is efficient and straightforward. Speech soap note examples provide a structured method for recording individual requirements, promoting effective treatment planning. Studies show that organized records can reduce up to 20% of time allocated to administrative duties, allowing therapists to focus more on what truly matters—client care.
- Legal Safeguard: Documentation is more than just paperwork; it creates a thorough account of patient interactions, essential for legal and insurance purposes. This record acts as a safeguard against disputes, ensuring that clinicians have clear evidence of diagnoses and treatments.
- Consistency in Care: Consistency is key in providing quality care. Utilizing speech soap note examples encourages a among therapists, which leads to enhanced quality of care. Consistent practices not only improve communication with insurance reviewers but also support compliance with legal standards.
- Real-World Impact: Consider the example of a telehealth clinic that adopted an integrated practice management system. They reported a 25% decrease in documentation time, enabling therapists to devote more time to meaningful interactions with individuals. This efficiency not only improves workflow but also enhances outcomes by allowing timely adjustments to treatment plans.
In summary, clinical documentation is essential in speech therapy. It fosters effective communication, enhances treatment planning, and ensures legal compliance—all while improving the overall quality of care. Let’s embrace these practices to nurture our patients’ journeys toward better health.
SimplePractice: Practical SOAP Note Examples for Speech Therapy Sessions
At SimplePractice, we understand the emotional challenges therapists encounter in their daily practice. Documentation can often feel overwhelming, yet it is essential for enhancing patient care and ensuring efficient communication. Here are some valuable SOAP note examples that can help streamline your documentation process:
-
Example 1:
- Subjective: "Patient reports feeling more confident in speaking after last week's session."
- Objective: "Patient completed articulation exercises with 90% accuracy."
- Assessment: "Progress noted in articulation skills; continue current plan."
- Plan: "Introduce new vocabulary exercises next session."
-
Example 2:
- Subjective: "Parent states, 'My child is using more words at home.'"
- Objective: "Observed increased word usage during play activities."
- Assessment: "Positive response to therapy; maintain current strategies."
- Plan: "Focus on expanding vocabulary in upcoming sessions."
These serve not only as models for developing your own records but also highlight the critical role of organized documentation in monitoring client progress. By documenting effectively, you can foster clear communication among healthcare professionals, ensuring continuity of care and improving treatment outcomes. Have you considered how optimal documentation methods can enhance your clinical efficiency and management of individuals?
Integrating statistics—such as a documented reduction in interest in activities or heightened anxiety—can provide deeper insights into patient progress through clinical records. Additionally, incorporating client quotes like, "I just can't shut my brain off at night," can strengthen the emotional connection and relatability of your examples. Including case studies that illustrate the practical application of therapeutic documentation can offer tangible evidence of their effectiveness in clinical settings.
It’s also important to recognize the limitations of structured documentation formats. They may not capture changes over time, a crucial consideration for healthcare providers. By consistently reviewing and updating your entries for clarity and precision, you can greatly enhance your records. How might this practice impact your therapeutic relationships and patient outcomes? Remember, you’re not alone in navigating these challenges; together, we can foster better documentation practices that ultimately benefit both you and your clients.
SoapNoteAI: Automated SOAP Note Generation for Speech Therapists
In the demanding world of healthcare, speech therapists often face emotional challenges that can hinder their ability to provide the best care. SoapNoteAI offers a compassionate solution for automated documentation creation, specifically designed to ease the burden of administrative tasks. By addressing the usual reluctance to change, this innovative tool empowers therapists to utilize speech soap note examples, allowing them to focus more on their clients and less on paperwork.
- Voice Recognition: Imagine being able to convert your spoken notes into a structured SOAP format effortlessly. This technology can reduce documentation time by up to 50%, allowing you to dedicate more time to client care. It's a relief to know that you can maintain a high quality of care without being overwhelmed by administrative duties.
- Customizable Templates: Every practice is unique, and SoapNoteAI understands that. With and examples of speech soap notes, you can tailor your notes to fit your specific needs, ensuring that your records align perfectly with your treatment methods and your clients' requirements. This personalization enhances the quality of care you provide.
- Integration with EHR: Seamless integration with existing electronic health record systems means you can enhance your workflow efficiency without disrupting your established practices. This smooth record-keeping process is crucial for gaining physician buy-in and fostering collaboration in patient care.
- HIPAA Compliance: Your clients' privacy and security are paramount. SoapNoteAI adheres to HIPAA regulations, ensuring that personal health information (PHI) is protected at all times.
By embracing SoapNoteAI, you can reclaim valuable time that was once spent on administrative tasks. This not only improves your interactions with clients but also enhances the overall quality of care you provide. The application of voice recognition technology simplifies record-keeping and boosts therapy effectiveness, leading to better outcomes for individuals.
Moreover, by addressing common concerns about innovation in healthcare, SoapNoteAI helps mitigate physician burnout, creating a more supportive and effective healthcare environment. Are you ready to transform your practice and improve your clients' experiences? Engage with SoapNoteAI today and take the first step towards a more fulfilling professional journey.
Headway: Compliance Benefits of SOAP Notes for Therapists
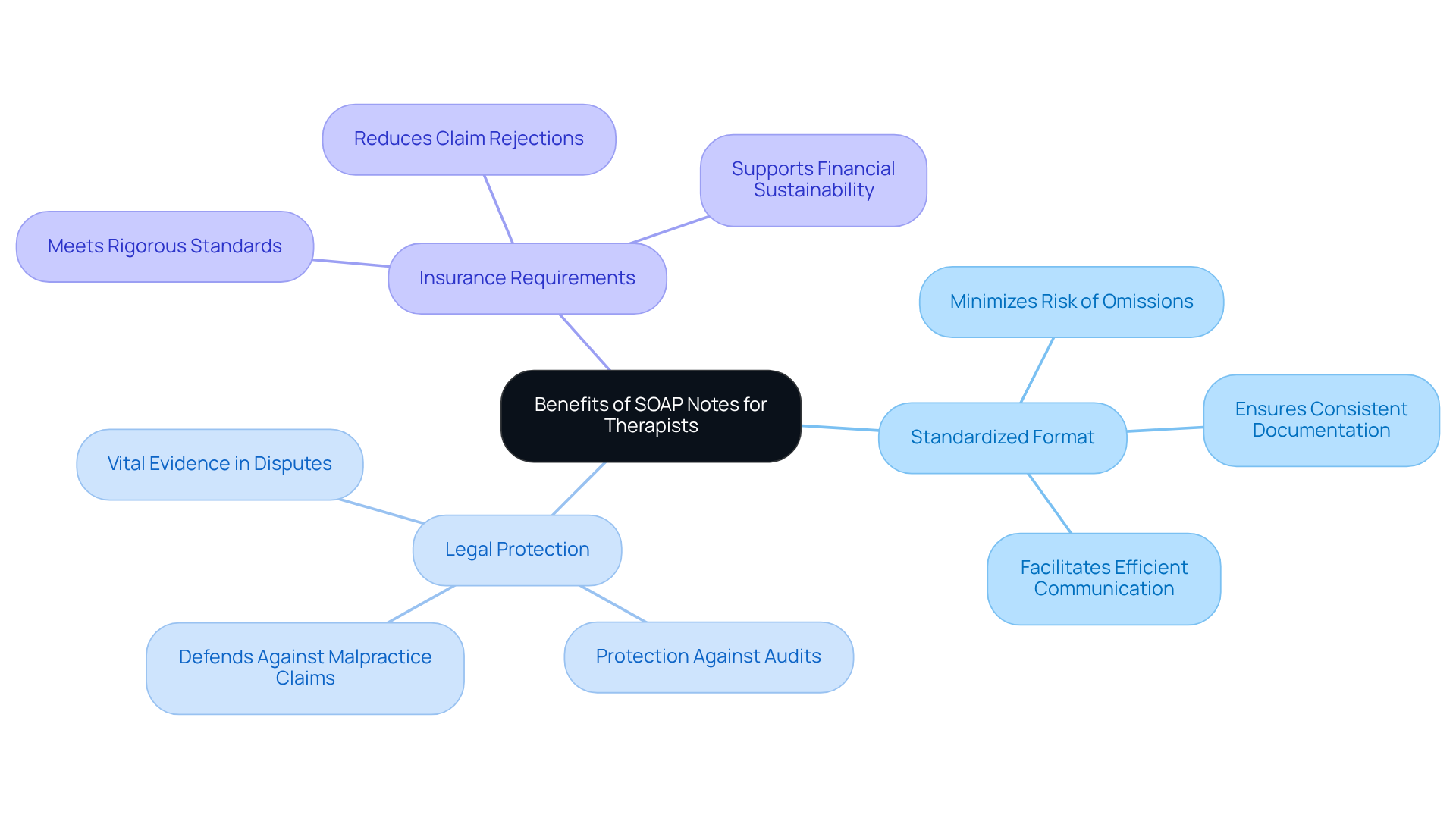
The compliance benefits of using SOAP notes are truly significant for therapists, especially when considering the emotional and administrative challenges they face in insurance documentation and legal protection. For healthcare startups navigating regulatory hurdles, these benefits can be a lifeline.
- Standardized Format: The SOAP format ensures that all necessary information is documented consistently. This minimizes the risk of omissions that could lead to complications in patient care or legal disputes. For startups that may lack established processes, this consistency is crucial.
- Legal Protection: By offering a clear and organized account of patient interactions, therapy records serve as vital evidence in case of disputes or audits. This protection is particularly important for startups that may face as they establish their practices.
- Insurance Requirements: Clinical documentation fulfills the rigorous standards set by insurance providers, enabling more efficient claims processing and reducing the chances of claim rejections due to insufficient or contradictory records. For healthcare startups, adhering to these standards is essential for financial sustainability.
By following this structured format, therapists not only enhance the quality of care they deliver but also fortify their practices against legal and financial risks. In a constantly evolving healthcare environment that demands specialized knowledge and compliance assistance, embracing these practices can be a transformative step forward.
Mentalyc: Common Mistakes to Avoid in SOAP Note Writing
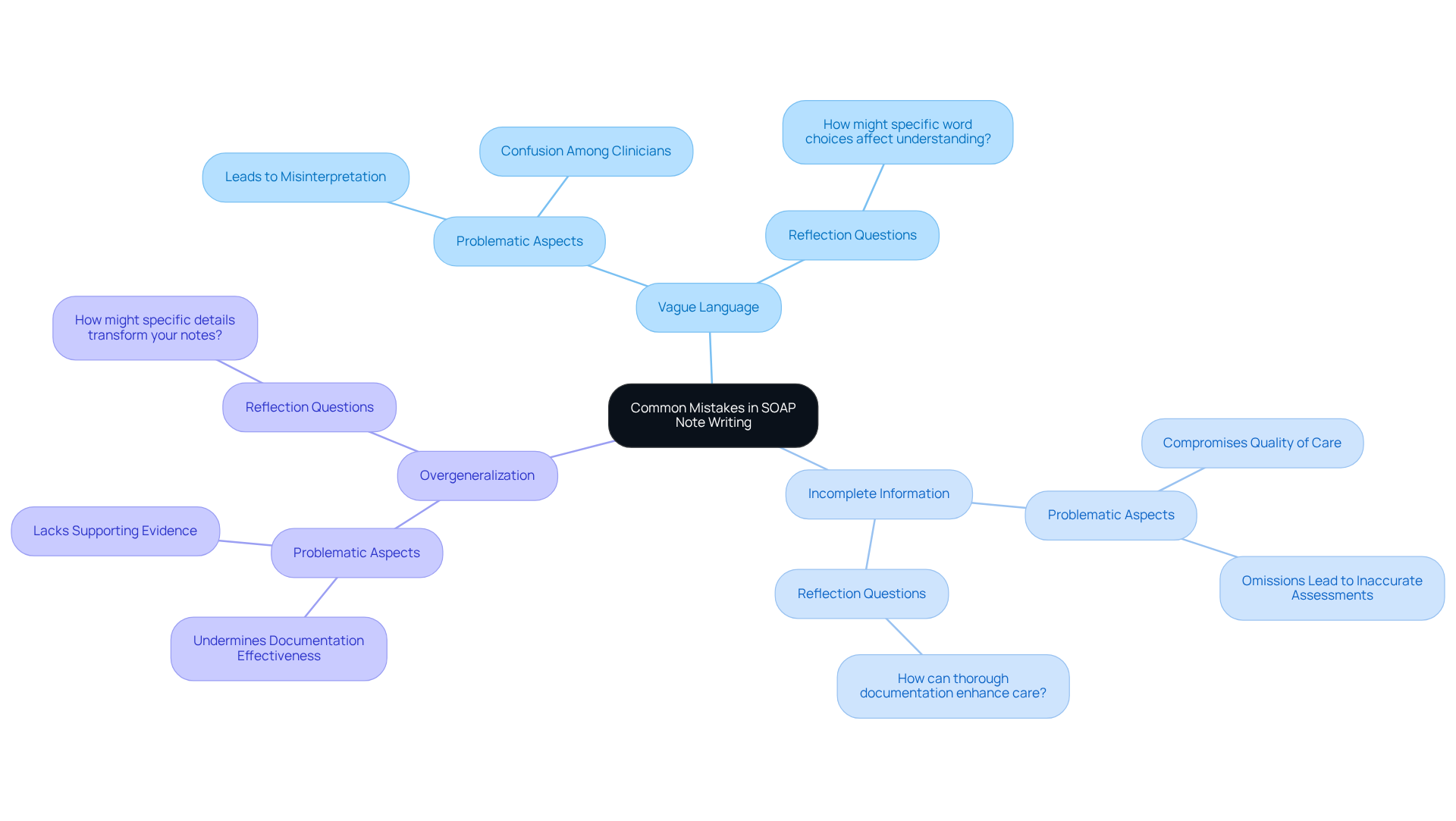
Mentalyc recognizes the emotional challenges therapists face when crafting SOAP notes, highlighting several critical mistakes to avoid:
- Vague Language: Ambiguous terms can lead to misinterpretation and confusion. Specificity in descriptions is essential to convey accurate information about individuals receiving care. Have you considered how your word choices might affect understanding?
- Incomplete Information: Omitting key details, such as normal vital signs in the objective section, can severely compromise the quality of care. Every part of the medical documentation must be thoroughly filled out to offer a complete perspective of the patient's condition. Reflect on how thorough documentation can enhance your care.
- Overgeneralization: Broad statements without supporting evidence can undermine the effectiveness of documentation. Offering specific examples and pertinent information improves the clarity and usefulness of documentation. How might specific details transform your notes into valuable resources?
Moreover, therapists must ensure that any changes to medication incorporate a clear justification, as this is essential for thorough documentation. By identifying and addressing these challenges, therapists can significantly enhance the clarity and efficacy of their records. This, in turn, leads to and more streamlined record-keeping practices. Let's commit to refining our documentation habits together for the benefit of our patients.
Quenza: Tips for Effective SOAP Note Documentation
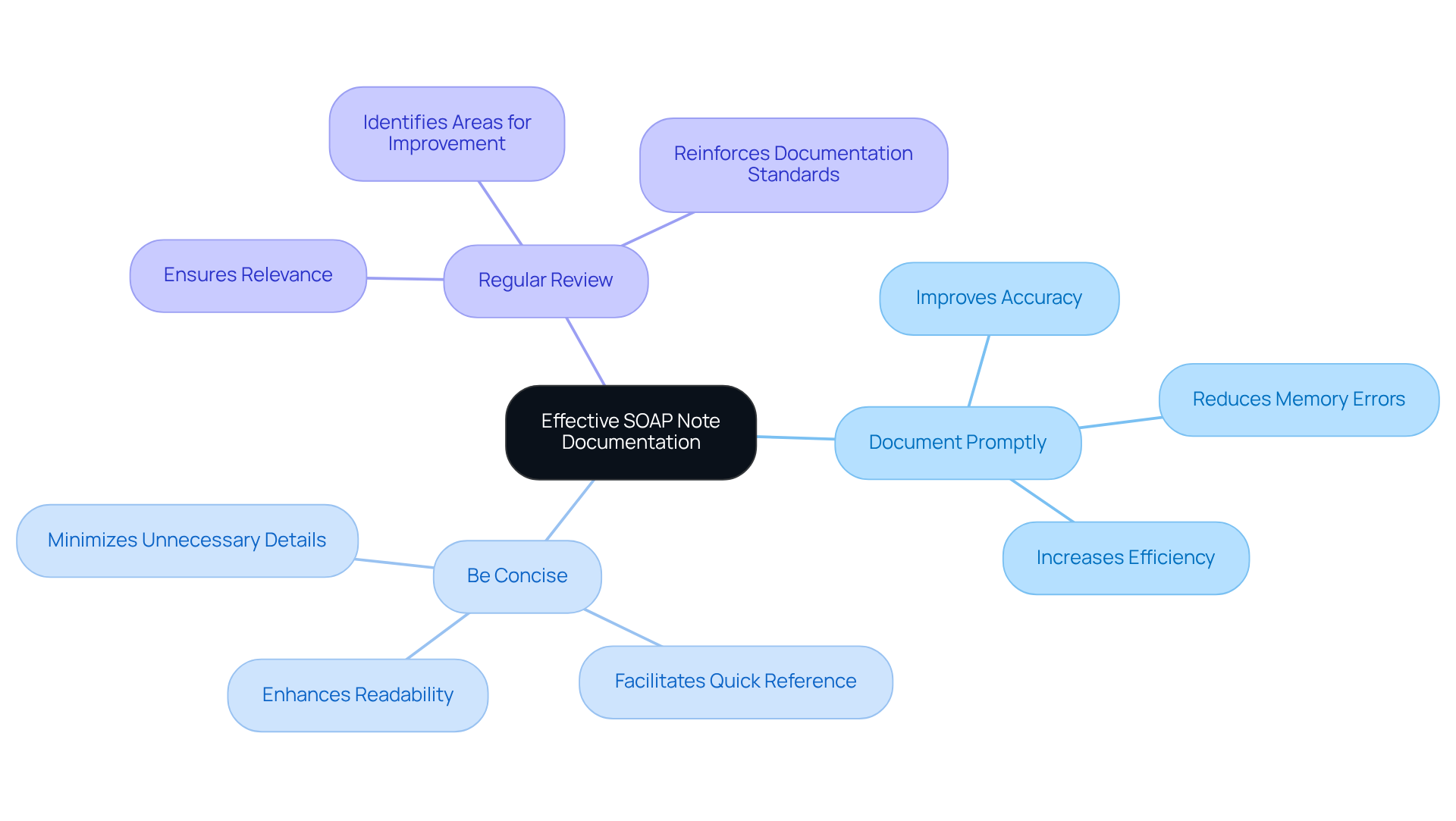
Effective record keeping through speech soap note examples is crucial for therapists who genuinely care about enhancing their clinical practice. Are you feeling overwhelmed by the demands of documentation? You're not alone. Here are several key strategies that can help improve the quality and efficiency of your notes:
- Document Promptly: Writing notes immediately after a session captures accurate details and minimizes memory-related errors. This practice is vital, as studies indicate that can significantly improve quality by 36.6% while decreasing recording time by 42%. Imagine the relief of knowing that you’re minimizing the time allocated to administrative tasks and focusing more on your clients.
- Be Concise: Utilize clear and direct language to convey essential information without unnecessary elaboration. Concise language not only improves readability but also ensures that critical details are easily accessible for future reference. For instance, in a speech-language pathology case, a client mentioned heightened vocal demands and occasional vocal fatigue, which can be illustrated through speech soap note examples. This highlights how precise records can make a significant difference in monitoring progress.
- Regular Review: Periodically revisiting and updating your records ensures they remain relevant and accurate. This practice can help identify areas for improvement and reinforce the importance of maintaining high documentation standards. As mentioned, "Documenting observations immediately after patient visits guarantees precision and reduces memory-related errors."
By applying these techniques, you can achieve more efficient documentation, ultimately benefiting both you and your clients. Remember, taking these steps not only eases your workload but also enhances the care you provide.
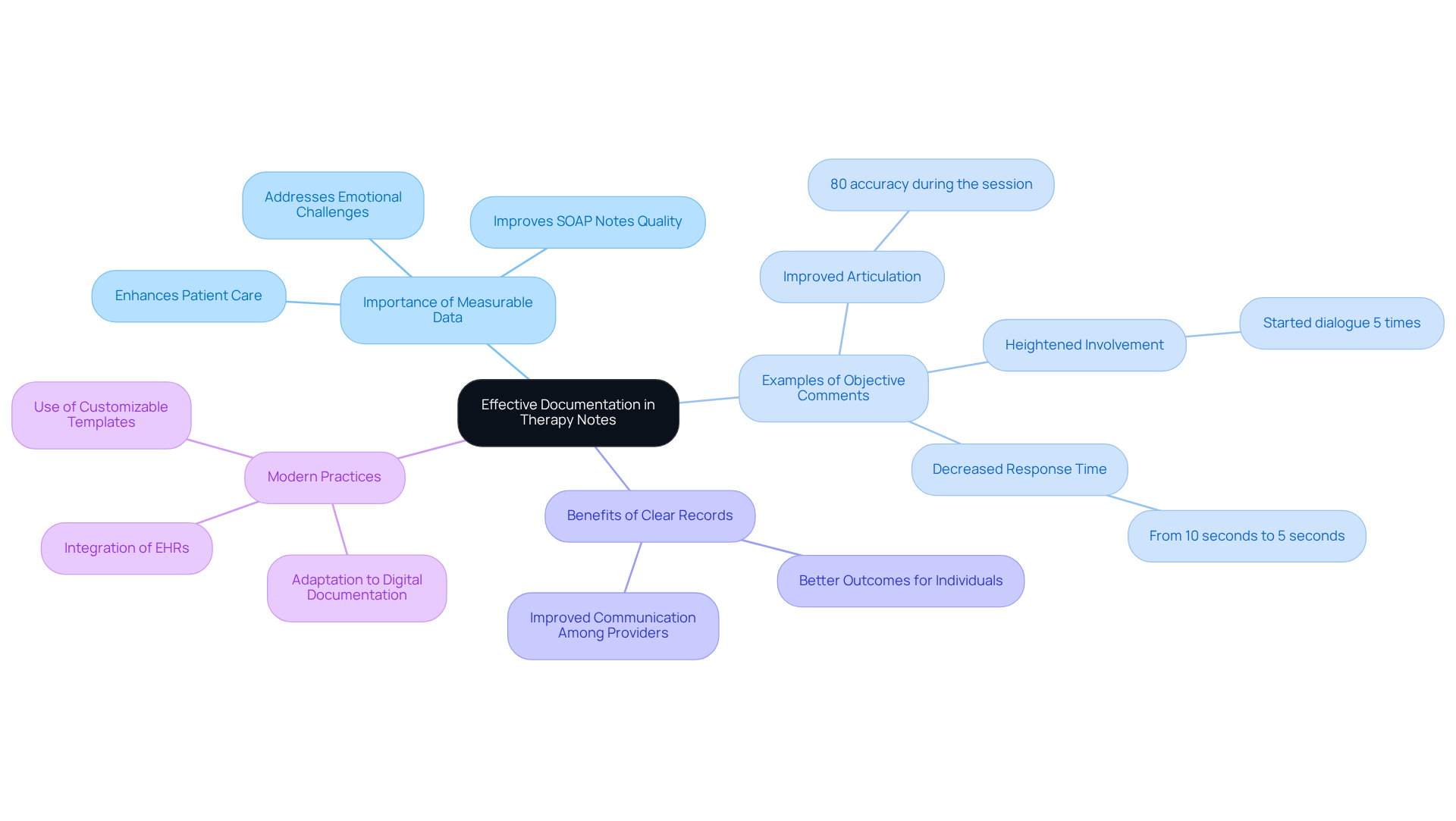
Medesk: Examples of Objective Comments in SOAP Notes
Effective record-keeping in therapy notes is essential for enhancing patient care, and it begins with the inclusion of measurable data. This practice not only improves the but also addresses the emotional challenges healthcare providers face in managing their documentation. Consider these examples of objective comments that therapists can incorporate:
- "Patient demonstrated improved articulation of /s/ sounds with 80% accuracy during the session."
- "Noted heightened involvement during group tasks, with the individual starting dialogue 5 times."
- "Patient's response time decreased from 10 seconds to 5 seconds when prompted to repeat phrases."
These speech SOAP note examples demonstrate how documenting observable and measurable data can significantly impact clinical practice. By maintaining precise records of measurable outcomes, therapists can monitor progress more effectively and guide future treatment choices. Research shows that clear and concise records lead to better outcomes for individuals and improved communication among healthcare providers.
The structured approach method, proposed by Larry Weed nearly 50 years ago, serves as a systematic way of clinical reasoning and documentation. By focusing on quantifiable information, therapists can ensure their documentation is thorough and efficient, ultimately enhancing care for individuals. However, it’s important to acknowledge that documentation formats have constraints, such as the inability to capture changes over time, which can impact the evaluation of individual progress.
As medical documentation evolves, adapting SOAP notes to modern practices—especially in the realm of digital documentation—becomes crucial for maintaining clarity and relevance in patient care. Embracing these changes not only alleviates administrative burdens but also fosters a more compassionate approach to patient care. How can you integrate these practices into your routine to enhance your documentation and ultimately support your patients better?
Conclusion
In the realm of speech therapy, the utilization of SOAP notes emerges as a cornerstone of compassionate patient care. Have you ever felt overwhelmed by the administrative tasks that take time away from your clients? By adopting structured documentation practices, therapists can alleviate this burden, allowing more focus on what truly matters—their clients' well-being.
Innovative solutions, such as AI-powered tools, further enhance this efficiency, transforming the way therapists approach record-keeping. Each component of the SOAP note—Subjective, Objective, Assessment, and Plan—plays a vital role in ensuring clarity and specificity in documentation. This clarity is essential to prevent misunderstandings and elevate the quality of care provided.
Moreover, exploring common mistakes and best practices serves as a valuable guide for therapists striving to refine their documentation skills. Imagine the impact of improved documentation on patient outcomes—it's not just about paperwork; it's about fostering a nurturing therapeutic environment.
Ultimately, embracing effective SOAP note practices not only lightens the emotional load of paperwork but also enhances clinical efficiency. By prioritizing clear and organized documentation, therapists can ensure compliance with legal and insurance standards, contributing to better health outcomes for their clients. Engaging with these practices is essential for any therapist dedicated to delivering high-quality care in an increasingly complex healthcare landscape. Let's commit to this journey together, for the benefit of our clients and ourselves.




