Overview
This article addresses the emotional challenges that healthcare providers often face, particularly the weight of administrative tasks that can detract from patient care. By providing essential care notes templates, we aim to alleviate some of this burden, allowing providers to focus more on what truly matters—their patients.
Structured documentation methods, such as SOAP notes and intake forms, are highlighted as effective solutions. These tools not only enhance accuracy and efficiency but also foster better communication among healthcare professionals. When documentation is streamlined, it leads to improved patient outcomes, creating a more nurturing environment for care.
We understand that the demands of healthcare can be overwhelming, and it’s crucial to find ways to simplify these processes. By embracing these documentation strategies, healthcare providers can experience a significant reduction in stress, ultimately benefiting both themselves and their patients.
We encourage you to explore these templates and consider how they might fit into your practice. Together, we can create a more compassionate healthcare experience that prioritizes patient care and supports the well-being of providers.
Introduction
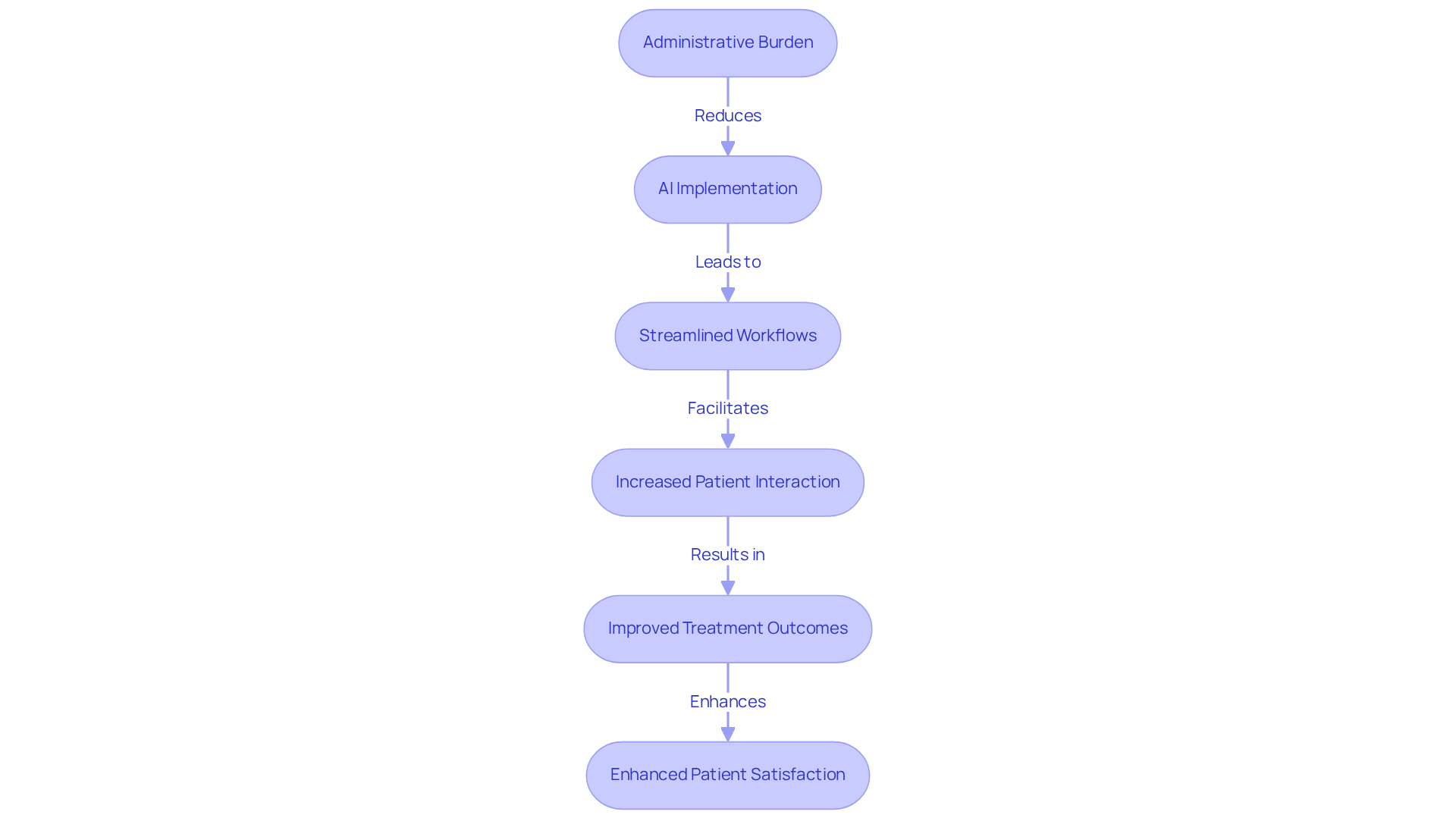
In the ever-evolving world of healthcare, providers often feel overwhelmed by the weight of administrative tasks that can detract from their core mission of patient care. This burden can lead to frustration and a sense of disconnect from the very patients they strive to help.
Fortunately, the emergence of innovative documentation solutions, such as care notes templates, offers a unique opportunity to streamline processes and enhance the quality of care delivered.
As healthcare professionals seek to improve efficiency and accuracy, they face the pressing challenge of integrating these tools into their workflows. How can adopting structured documentation practices not only alleviate administrative burdens but also enrich the overall patient experience? By embracing these solutions, providers can reclaim valuable time, allowing them to focus on what truly matters: their patients.
Let’s explore how these practices can transform the administrative landscape and foster a more compassionate approach to care. Together, we can create a healthcare environment that prioritizes both efficiency and empathy.
CosmaNeura: AI-Powered Patient Intake and Documentation Solutions
In the demanding landscape of healthcare, providers often face overwhelming administrative burdens that can detract from the quality of patient care. CosmaNeura understands these challenges and utilizes advanced AI technology to streamline client intake and documentation processes. By alleviating this administrative load, the platform allows clinicians to dedicate more time to meaningful interactions and support, addressing the rising costs of healthcare that weigh heavily on both individuals and providers.
Imagine a world where the intricacies of documentation are handled seamlessly. With CosmaNeura, the AI-driven system captures and documents individual data meticulously, leading to a more efficient workflow and a significantly enhanced experience for patients. This innovative approach not only boosts operational efficiency but also aligns with the compassionate principles of Catholic teachings, ensuring that care remains patient-centered and empathetic.
Recent advancements in AI have proven transformative, showing a remarkable 30-35% improvement in treatment outcomes compared to traditional methods. This highlights the potential of AI to revolutionize medical documentation and patient care. Effective applications of AI solutions in primary care settings have demonstrated that providers can reclaim valuable hours previously spent on administrative tasks. This shift enables them to focus on delivering high-quality care while navigating the financial challenges of the medical landscape.
Our recent pilot testing with three physicians has validated these benefits, underscoring the positive impact of AI on clinician workload and patient satisfaction. As we move forward, we encourage healthcare providers to explore how CosmaNeura can support them in their mission to provide compassionate care, ultimately fostering a healthier future for all.
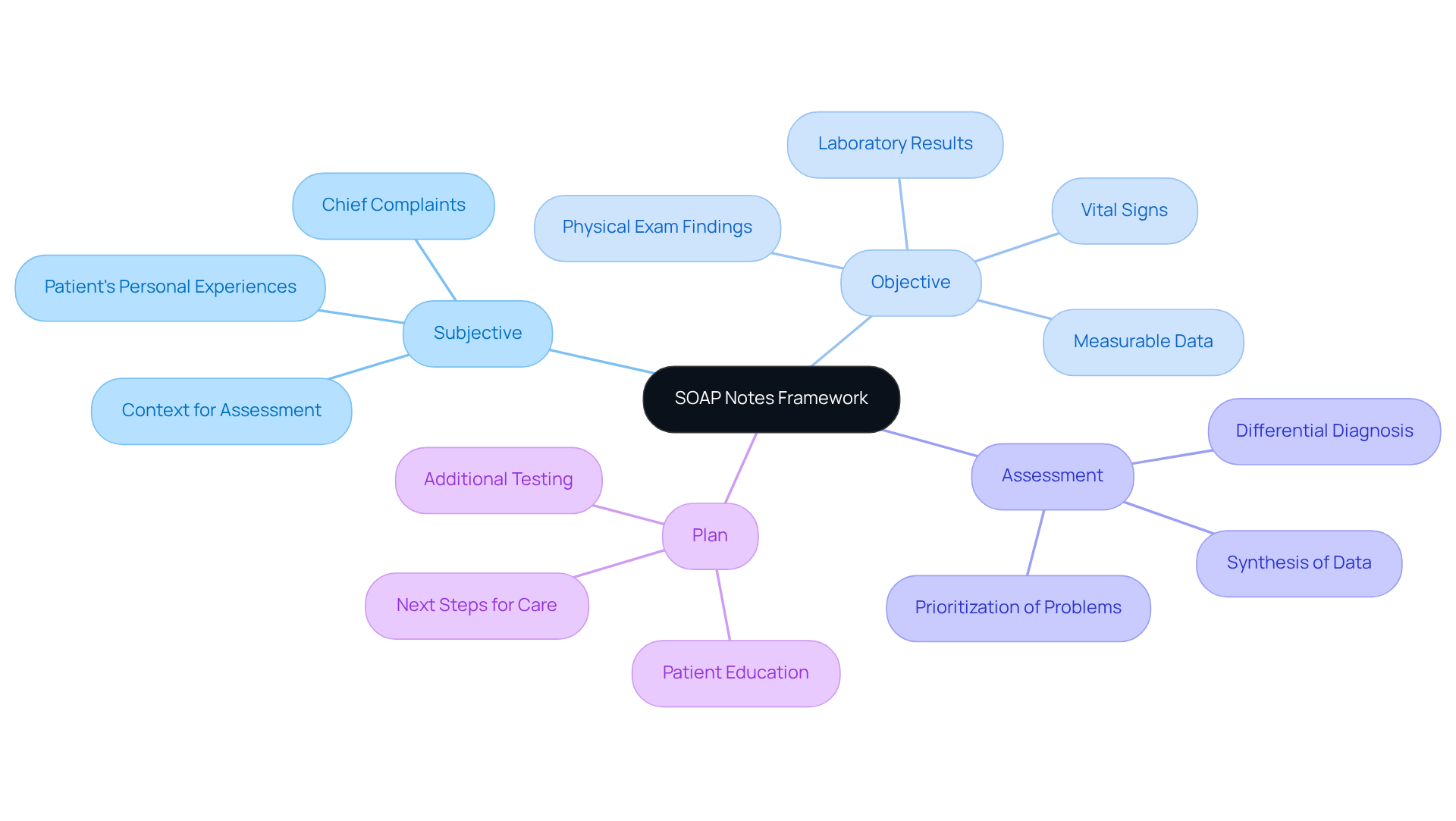
SOAP Notes: Structured Documentation for Effective Patient Care
SOAP notes—Subjective, Objective, Assessment, and Plan—offer a structured framework that can significantly alleviate the administrative burdens healthcare providers face, ultimately enhancing patient care. Have you ever felt overwhelmed by the need to capture every detail during patient encounters? This format allows for systematic documentation, ensuring that essential information is not overlooked. By embracing SOAP notes, clinicians can foster clarity and continuity of care, making it easier to track client progress and make informed decisions.
The organized nature of SOAP notes is not just about compliance with record-keeping standards; it plays a crucial role in the safety of individuals receiving care. For instance, research reveals a concerning inconsistency in documenting vital factors like drug allergies and smoking history. Internists report recording drug allergies at 61.6% and smoking history at just 37.8%. This gap underscores the urgent need for uniform record-keeping methods to improve healthcare outcomes.
Moreover, the application of organized records through SOAP notes has been linked to improved quality of patient care. Did you know that training interventions focused on SOAP note writing can lead to remarkable enhancements in record scores? Studies show total scores can increase from 21.9±13.0 to 61.8±23.0 after training (p<0.001). Such improvements not only reflect superior record-keeping practices but also support more effective clinical reasoning and collaboration among healthcare professionals.
In conclusion, adopting SOAP notes is essential for medical providers striving to meet record-keeping standards and elevate client outcomes. By promoting a systematic approach to documentation, the use of a care notes template can significantly enhance the overall quality of care in medical settings. Let’s embrace this method together for the benefit of our patients.
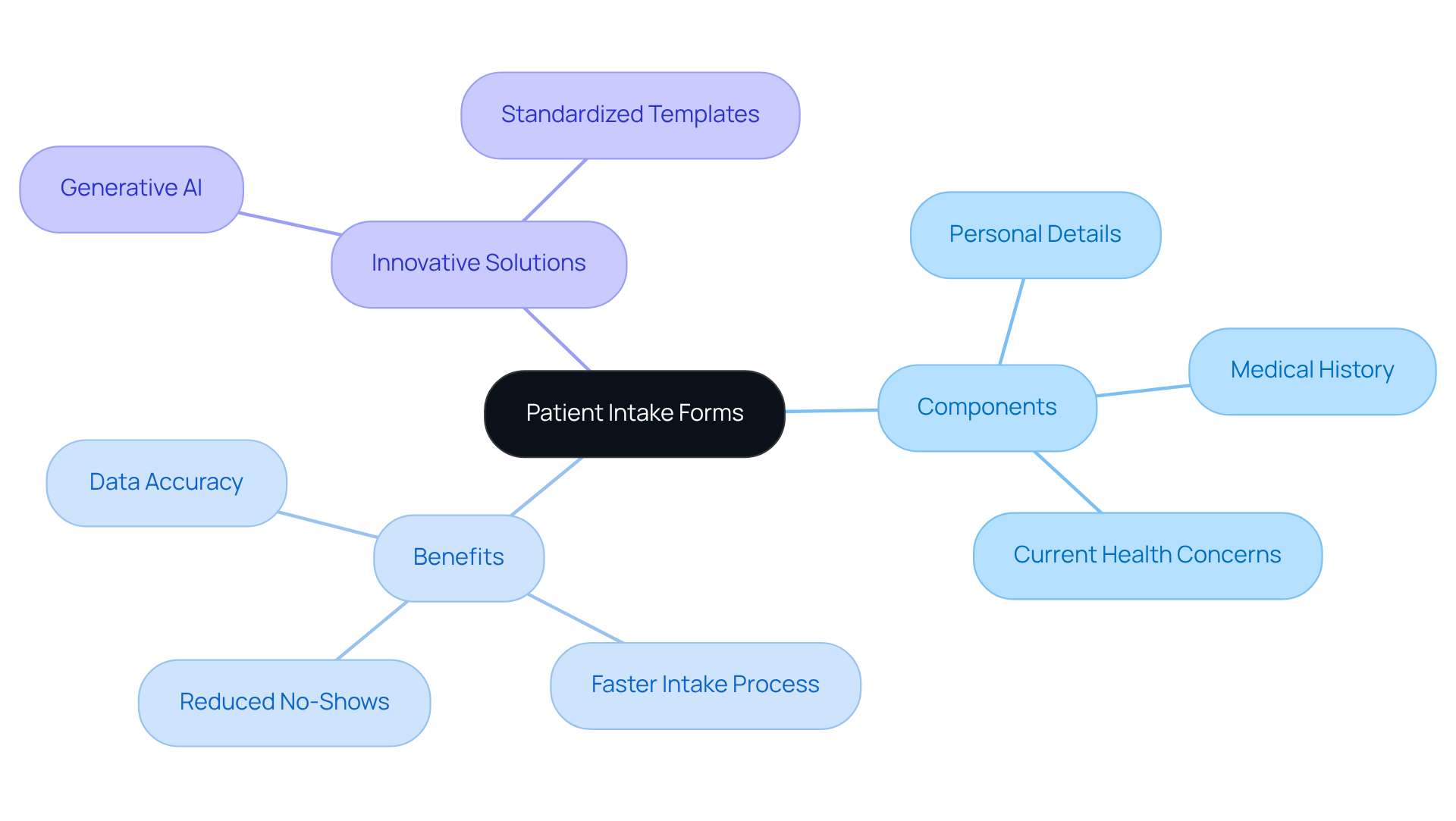
Patient Intake Forms: Essential Templates for Initial Assessments
Intake forms play a vital role in gathering essential information during an individual's initial assessment. These forms typically include sections for personal details, medical history, and current health concerns. By utilizing a care notes template, healthcare providers can efficiently collect comprehensive and relevant information. This not only speeds up the intake process but also significantly enhances data accuracy, which is crucial for making informed clinical decisions.
Imagine the peace of mind that comes with enhanced precision in intake forms. Such accuracy leads to improved outcomes for individuals, reducing the chances of mistakes that can jeopardize the quality of care. In fact, clinics that have embraced digital intake solutions report a 30% faster intake process and a 25% decrease in no-shows. This demonstrates how streamlined processes can truly make a difference.
Moreover, integrating generative AI into the intake process can automate data entry and analysis, further boosting efficiency and accuracy. The care notes template serves as a standardized form that also acts as legal documentation, ensuring compliance and safeguarding individual data. This is increasingly important in today’s medical landscape, where over 41 million medical records were exposed in 2019.
By prioritizing the use of standardized intake forms and leveraging innovative AI solutions, healthcare providers can create a more efficient, accurate, and patient-centered environment. Let’s work together to foster a healthcare experience that truly values each individual’s needs.
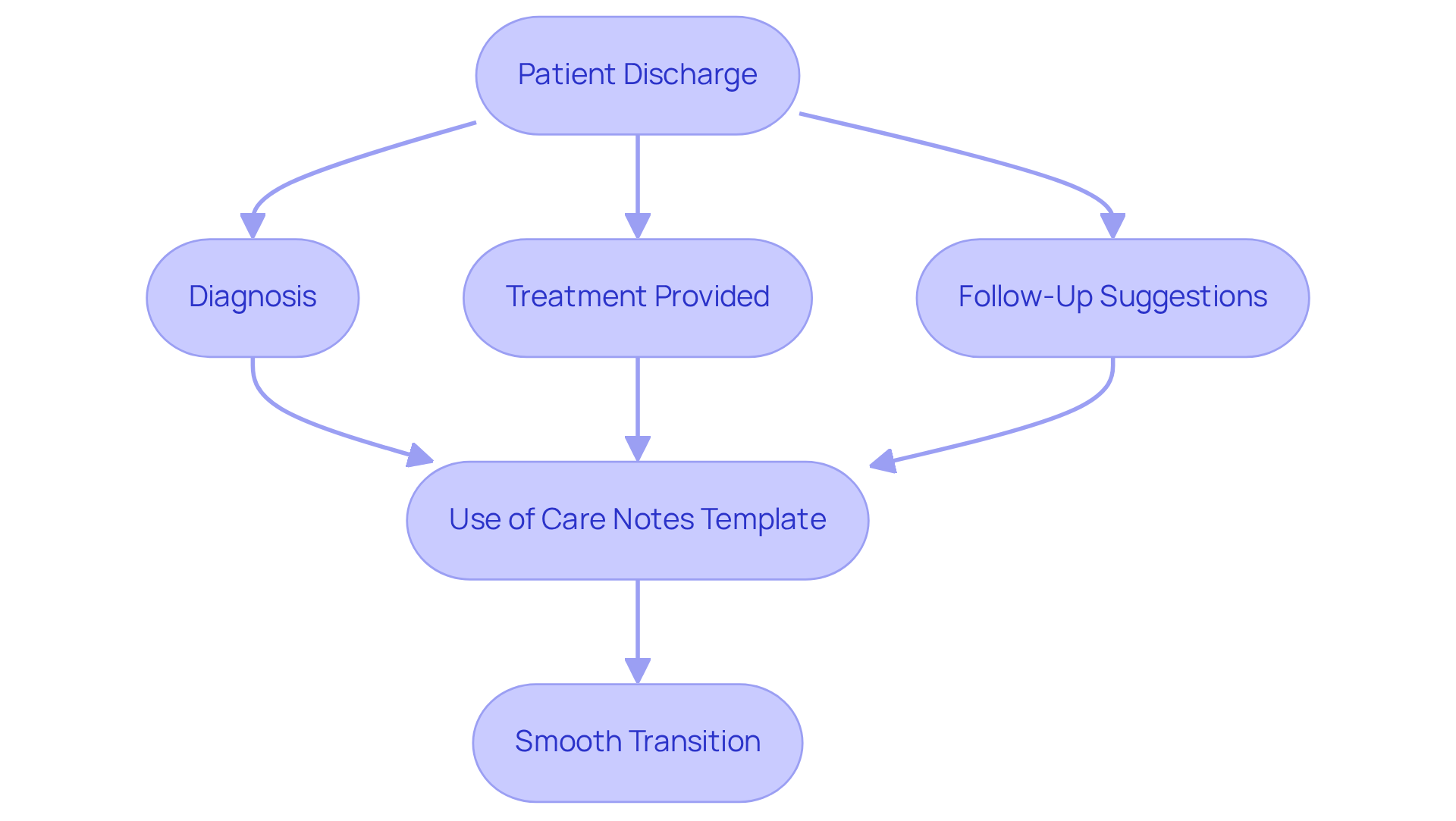
Discharge Summary Notes: Key Templates for Patient Transition
Discharge summary notes are vital documents that encapsulate an individual's hospital experience while offering essential follow-up guidance. Have you ever considered how challenging it can be for healthcare providers to ensure that every detail is captured accurately? Effective care notes templates typically include crucial elements such as the individual's diagnosis, treatment provided, and suggestions for ongoing support. By providing a clear and concise summary, healthcare professionals can facilitate a smooth transition for individuals moving from the hospital to home or other support environments.
This record is not just a formality; it is essential for ensuring that all members of the care team are well-informed about the individual's status and needs. This understanding enhances safety and satisfaction for everyone involved. Recent studies indicate that compliance rates for discharge records have improved significantly. The use of a care notes template leads to better adherence to national guidelines, which is a positive step forward.
Moreover, the use of standardized formats, like the SBAR (Situation-Background-Assessment-Recommendation) model, has shown to improve the clarity and completeness of discharge summaries. This improvement ultimately decreases the risk of hospital readmissions and enhances overall outcomes for individuals. Imagine the peace of mind that comes with knowing that every detail is accounted for and that individuals are set up for success after leaving the hospital.
Generative AI can further simplify the record-keeping process by automating data entry and ensuring adherence to guidelines, which helps reduce administrative burdens. As the medical field continues to evolve, prioritizing effective discharge documentation remains essential. It fosters continuity of treatment and ensures high-quality experiences for individuals. Let us embrace these tools to enhance our care and support for those we serve.
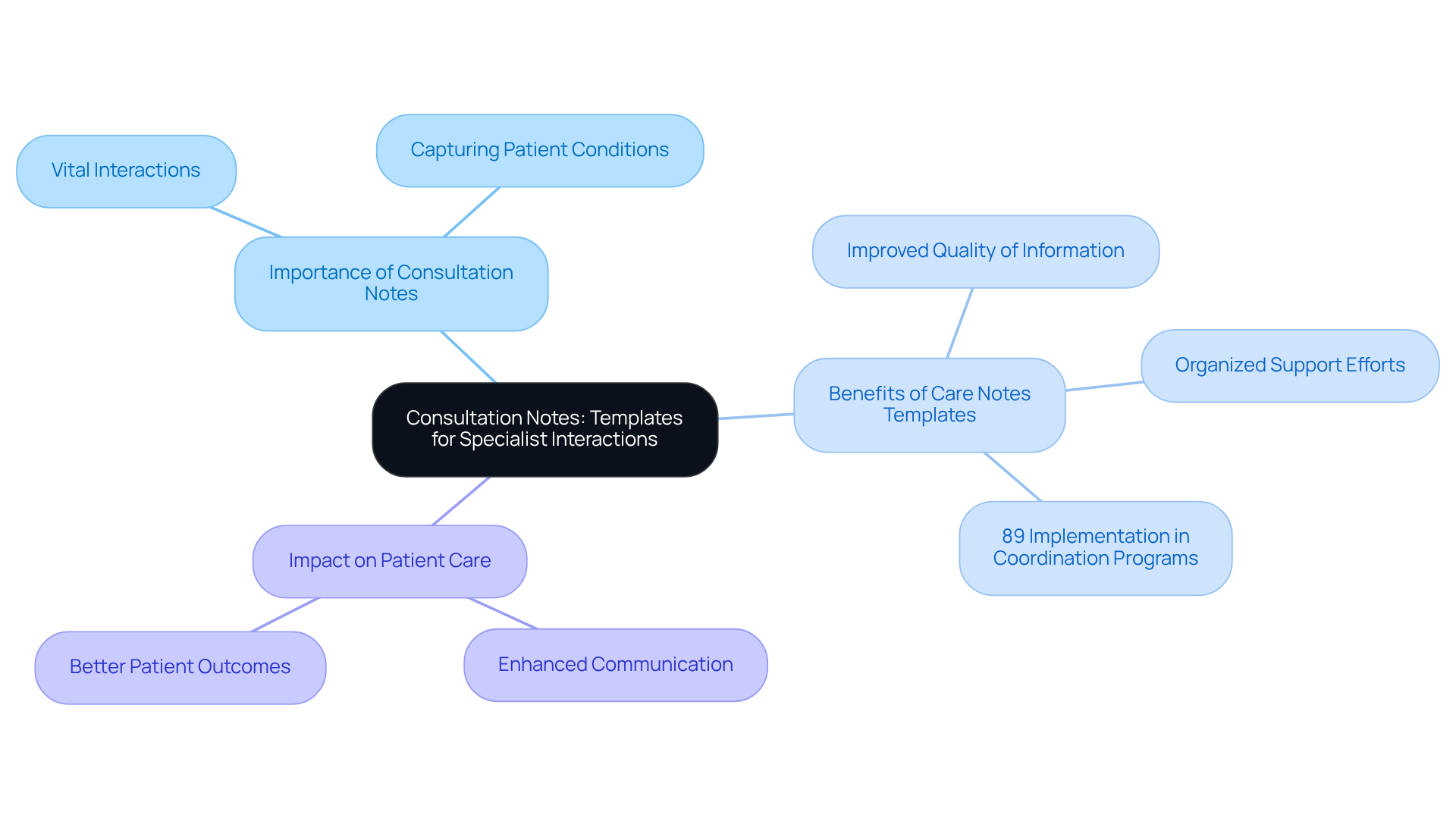
Consultation Notes: Templates for Specialist Interactions
Consultation notes are essential documents that capture the vital interactions between primary health providers and specialists. They hold important details about an individual's condition, specialist findings, and management recommendations. Have you ever considered how these notes can significantly impact patient care? By employing a care notes template, we ensure that all pertinent information is recorded clearly and precisely. This clarity is crucial for effective communication among medical providers.
Care notes templates not only improve the quality of information shared but also facilitate organized support efforts. This ultimately leads to better outcomes for individuals. Recent trends reveal that 89% of coordination programs have implemented systematic processes to assess individual needs. This statistic underscores the significance of thorough documentation in fostering collaboration across the healthcare continuum.
By adopting these best practices, providers can significantly enhance the efficiency and effectiveness of service delivery. Imagine the positive impact on your patients when you streamline communication and ensure that every detail is captured. Let's work together to make these improvements a reality, as they can transform the way we care for those we serve.
Emergency Department Notes: Templates for Urgent Care Documentation
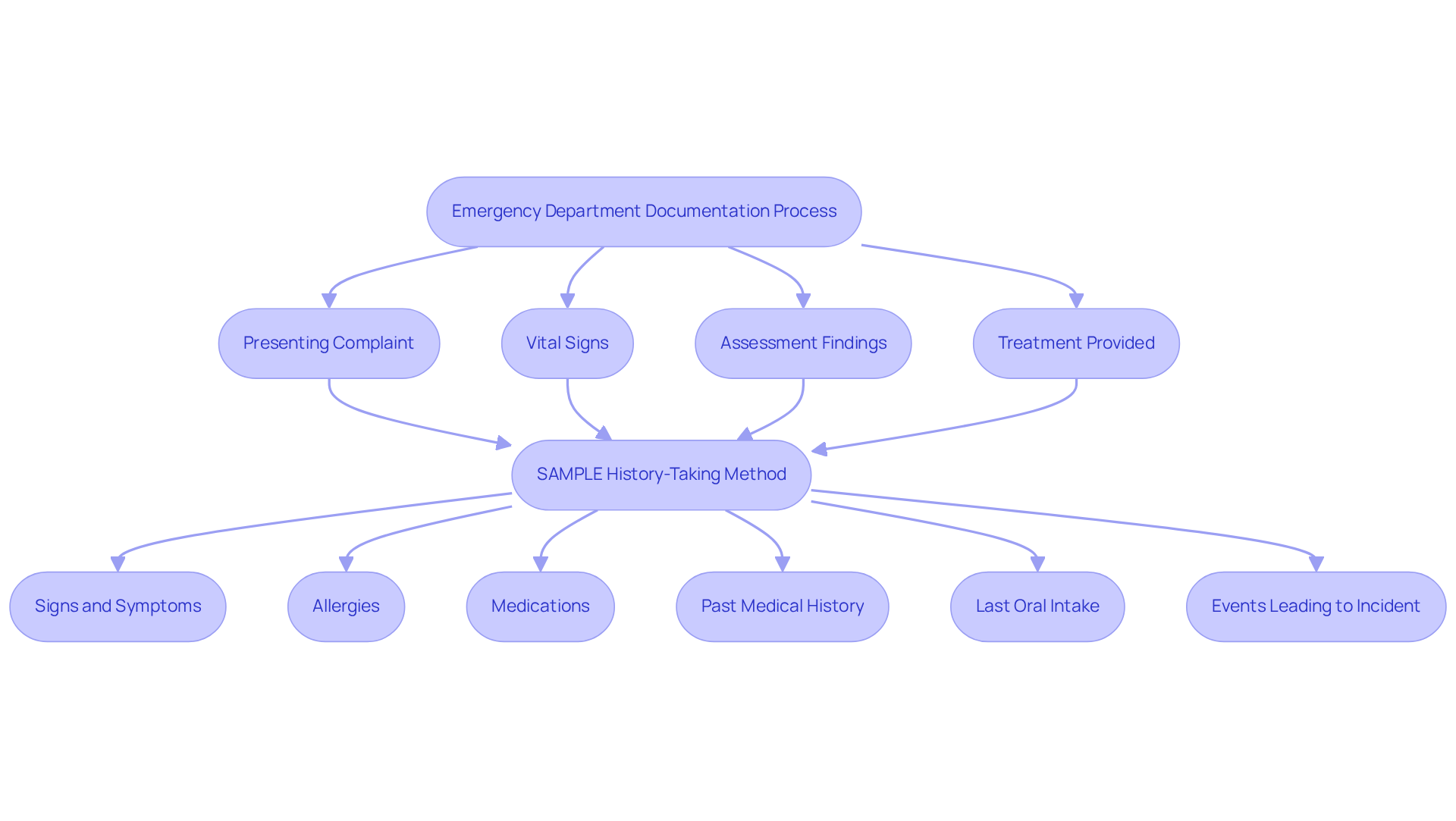
Emergency department notes play a crucial role in capturing the unique interactions that occur in urgent treatment settings. These notes are not just records; they are lifelines for individuals in need. The care notes template typically includes sections for the individual's presenting complaint, vital signs, assessment findings, and treatment provided, ensuring that vital information is documented quickly and accurately. This is essential for delivering prompt and effective care.
Have you ever considered how organized record-keeping can significantly improve health outcomes? Studies reveal that after introducing new templates, adherence rates for recording key components, such as signs and symptoms, skyrocketed from 68.2% to 96.9%. This remarkable level of accuracy not only enhances continuity of care but also fulfills legal and billing requirements, underscoring the importance of meticulous record-keeping in emergency settings.
Moreover, implementing best practices in record-keeping, like the SAMPLE history-taking method—covering Signs and Symptoms, Allergies, Medications, Past Medical History, Last Oral Intake, and Events leading to the incident—can enhance compliance and overall safety for individuals. Yet, challenges such as time constraints and individuals' reluctance to share information can impede the effective use of the SAMPLE tool.
What if there was a way to alleviate these burdens? By leveraging generative AI, medical providers can streamline these recording processes with a care notes template, reducing the administrative load and allowing more focus on compassionate care for individuals. For instance, generative AI can automatically fill the care notes template with individual data, ensuring accuracy and saving precious time.
Therefore, it is imperative for healthcare providers to prioritize efficient documentation strategies in their practice. Let’s work together to create a more supportive environment for both providers and patients, ensuring that care remains at the forefront of our efforts.
Mental Health Treatment Plans: Essential Templates for Therapeutic Care
Mental health treatment plans are vital documents that outline the goals, objectives, and interventions tailored to an individual's therapeutic care. These templates typically include sections detailing the individual's diagnosis, presenting issues, and specific treatment strategies. Have you ever considered how these structured plans can make a difference? By utilizing care notes templates, providers can effectively meet the unique needs of each person, fostering accountability and facilitating progress tracking.
This organized approach not only enhances the effectiveness of therapy but also significantly contributes to positive outcomes for individuals. Recent trends highlight a growing emphasis on careful record-keeping practices, essential for ensuring comprehensive care and improving treatment adherence. As medical professionals increasingly recognize the importance of organized records, the potential for enhanced responsibility among individuals and therapeutic success becomes evident.
Moreover, integrating innovative AI solutions, like those offered by CosmaNeura's Agentic Platform, can help alleviate challenges such as physician burnout and resistance to innovation. By streamlining documentation processes and reducing administrative burdens, healthcare professionals can devote more time to individual support. This shift ultimately promotes a more efficient, accessible, and patient-centered healthcare environment. How can we further support our healthcare providers in this journey?

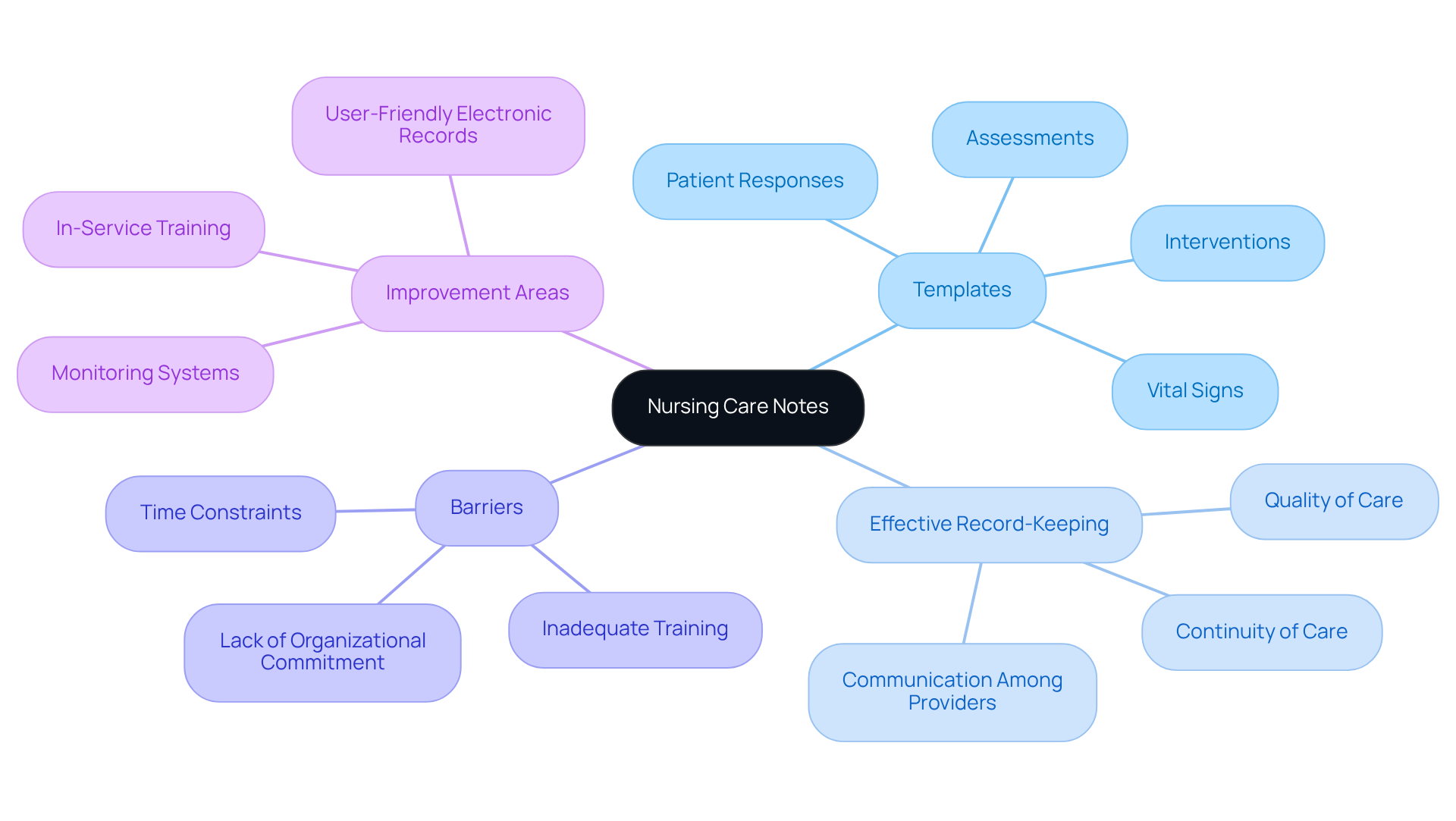
Nursing Care Notes: Templates for Comprehensive Patient Monitoring
Nursing documentation plays a crucial role in capturing the ongoing support and observation of individuals. These templates typically include sections for vital signs, assessments, interventions, and patient responses. By employing a care notes template, nurses can effectively ensure that all relevant information is recorded accurately and efficiently. This record is not just a formality; it is essential for maintaining continuity of care, fostering communication among healthcare providers, and guaranteeing that patients receive the highest quality of care.
Yet, it is concerning to note that only 42% of nurses demonstrate effective record-keeping practices, highlighting a significant area for improvement. What barriers might be contributing to this? Challenges such as time constraints and inadequate training complicate the ability to maintain thorough records. Integrating insights from respected figures, such as Florence Nightingale, who emphasized the importance of detailed documentation, can enrich our understanding of this issue.
Moreover, grasping the organizational factors that influence record-keeping practices is vital for addressing the difficulties nurses face in their documentation efforts. How can we better support our healthcare providers in overcoming these challenges? By recognizing and addressing these emotional and practical hurdles, we can foster an environment that empowers nurses to excel in their roles and enhances patient care overall.
Social Work Case Notes: Essential Templates for Client Documentation
Social work case notes play a vital role in documenting interactions with clients and tracking their progress over time. These templates typically include sections for client demographics, presenting issues, interventions, and outcomes. By utilizing a care notes template, social workers can ensure that they capture all relevant information accurately and consistently. This record is crucial for effective case management, facilitating communication among team members, and ensuring that clients receive the support they need.
Have you considered how monitoring client progress can transform care? Recent trends highlight a rising focus on this significance, with many practitioners acknowledging that direct quotes from clients can greatly enhance the richness of records. Such quotes not only reflect clients' emotional states but also provide valuable insights into their journeys, fostering a more personalized approach to care.
As the field progresses, the incorporation of a care notes template becomes increasingly essential for enhancing service delivery and outcomes in social work. Furthermore, with around 70,000 social workers anticipated to exit the profession annually, efficient record-keeping is crucial for supporting professionals and managing workloads. Social workers assist individuals in alleviating pain, managing recovery, and advocating for social equity, significantly contributing to the fabric of society. This underscores the importance of diligent record-keeping, ensuring that every client's story is heard and valued.

AI-Enabled Note-Taking Tools: Enhancing Documentation Efficiency
AI-enabled note-taking tools are transforming the record-keeping landscape for medical professionals, addressing the significant emotional challenges posed by traditional methods. These advanced technologies, including natural language processing and machine learning, simplify the record-keeping process by capturing essential information in real-time. This innovation is crucial in healthcare, where many doctors feel hesitant to adapt due to concerns about maintaining the quality of service and their interactions with patients.
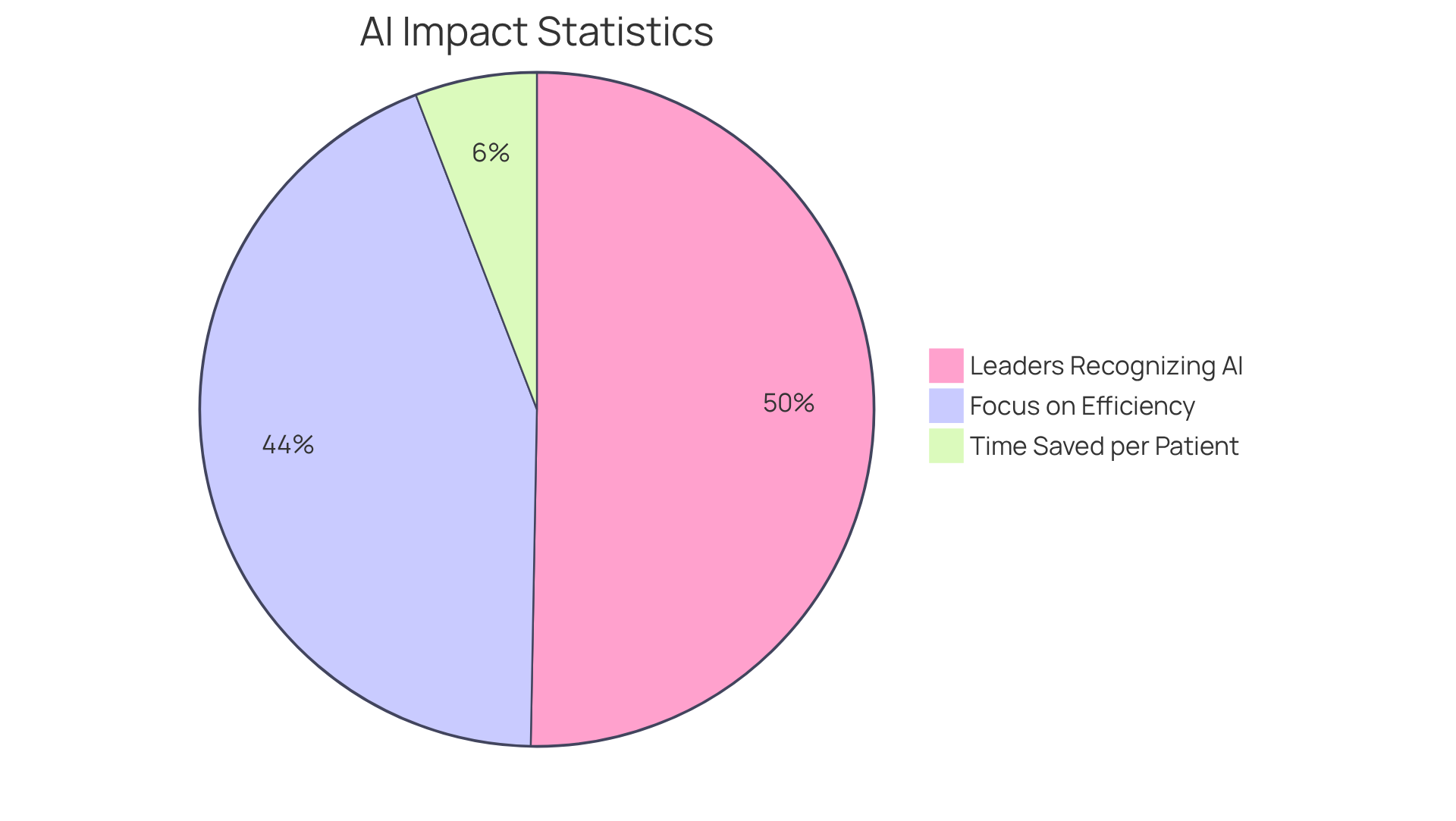
By integrating AI seamlessly into clinical workflows, providers can reclaim valuable time that was once consumed by documentation. Reports indicate that documentation time can be reduced by up to 72%, with AI potentially cutting this time by 50-70% for physicians. This newfound efficiency allows healthcare providers to focus more on patient interactions and care, effectively addressing the issue of physician burnout while enhancing administrative efficiency.
As more medical organizations embrace AI, it is heartening to see that 86% of leaders recognize its potential to streamline administrative tasks. Notably, 75% of these leaders identify administrative efficiency as the area with the greatest potential for improvement. Furthermore, 45% of organizations utilizing generative AI reported a return on investment within the first year, underscoring the financial advantages of AI adoption.
A compelling case study from a large regional health system in the Western U.S. illustrates this point: implementing an AI solution to streamline patient records not only improved coding but also saved clinicians an average of 10 minutes per patient each day on follow-up documentation. As a result, AI tools are not only enhancing operational efficiency but also fostering better care delivery and greater provider satisfaction. This transformation in healthcare delivery addresses the pervasive challenges faced by providers, paving the way for a more supportive and effective healthcare environment.
Conclusion
The integration of essential care notes templates within healthcare practices is more than just a procedural enhancement; it signifies a vital shift toward more efficient, patient-centered care. How often do you feel overwhelmed by administrative tasks that take time away from patient interactions? By adopting structured documentation methods, healthcare providers can alleviate these burdens, allowing for greater focus on the individuals they serve and leading to improved outcomes.
The transformative potential of tools like CosmaNeura's AI-powered solutions exemplifies how technology can streamline processes, enhancing both the clinician's experience and the quality of care delivered. Throughout this discussion, we've uncovered key insights regarding various documentation templates such as:
- SOAP notes
- Patient intake forms
- Discharge summaries
- Mental health treatment plans
Each of these templates plays a crucial role in ensuring thorough and accurate record-keeping, which is essential for effective communication among healthcare teams and for fostering continuity of care.
The evidence presented highlights the marked improvements in efficiency and patient safety that arise from implementing standardized documentation practices. Ultimately, the call to action is clear: healthcare providers must embrace these innovative documentation strategies and technologies to cultivate a more effective and compassionate care environment. By prioritizing structured templates and leveraging AI capabilities, the healthcare community can not only enhance operational efficiency but also significantly improve patient outcomes.
This commitment to excellence in documentation will pave the way for a healthier future, ensuring that every patient's story is accurately captured and valued in their healthcare journey. Let us work together to create a system that truly reflects our dedication to patient care.




