Overview
In the demanding world of healthcare, professionals often face emotional challenges that can weigh heavily on their ability to provide quality care. The article titled "10 Essential Clinical Note Templates for Healthcare Providers" addresses these concerns by offering structured templates designed to ease the burden of clinical documentation. By utilizing templates such as SOAP, DAP, and ISBAR, healthcare providers can streamline their record-keeping processes.
These tools not only improve communication among providers but also enhance the overall quality of patient care outcomes. Imagine how much more effective your team could be with clear, organized documentation at your fingertips. By alleviating administrative burdens, these templates empower healthcare professionals to focus on what truly matters—their patients.
Ultimately, the article serves as a gentle reminder of the importance of efficient documentation in the healthcare setting. We invite you to explore these templates and consider how they can transform your clinical practice. Together, let’s work towards a more compassionate and efficient healthcare environment.
Introduction
In the fast-paced realm of healthcare, where every second counts, the burden of documentation can often overshadow the core mission of patient care. Many healthcare providers feel overwhelmed by administrative tasks, which can detract from their ability to deliver compassionate care. The emergence of clinical note templates offers a promising solution, allowing providers to streamline their record-keeping processes, enhance communication, and ultimately improve patient outcomes.
However, with numerous options available, how can professionals determine which templates best suit their unique needs and workflows? This article delves into ten essential clinical note templates that not only simplify documentation but also empower providers to focus on what truly matters: delivering compassionate and effective care. By embracing these tools, healthcare professionals can find relief from the weight of paperwork and dedicate more time to their patients.
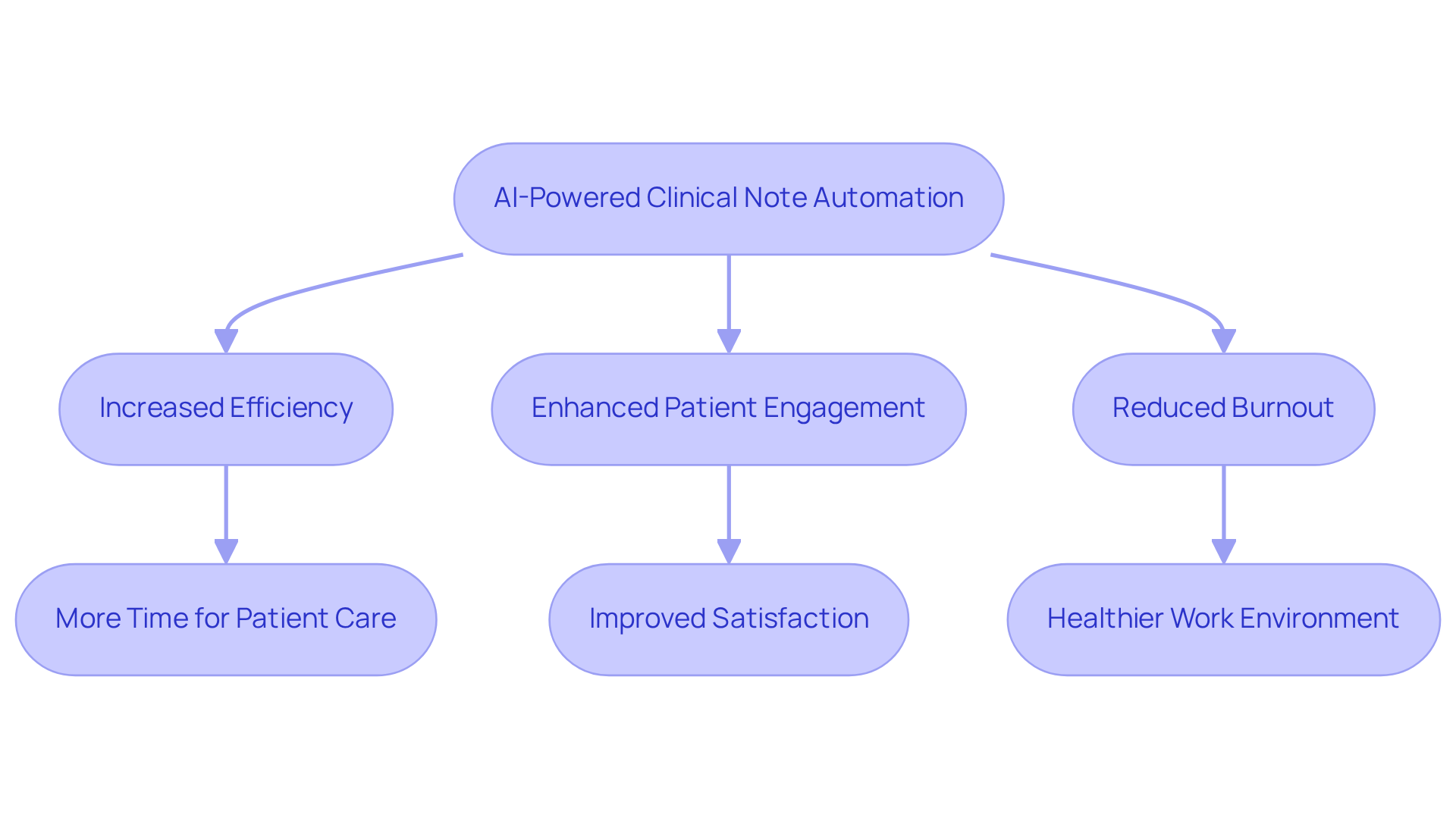
CosmaNeura: AI-Powered Clinical Note Automation for Healthcare Providers
At CosmaNeura, we understand the emotional challenges faced by healthcare providers, who often find themselves overwhelmed by administrative tasks. Our innovative AI platform is transforming clinical records by automating the creation of a clinical note template, which significantly enhances the efficiency of note-taking. Imagine reclaiming valuable time previously spent on data entry and record-keeping, allowing you to focus on what truly matters—providing outstanding patient care.
By simplifying the paperwork process, CosmaNeura enables you to enhance overall patient engagement. Our technology not only improves the precision of clinical records but also aligns with ethical guidelines grounded in Catholic teachings, ensuring that care remains compassionate and responsible. Have you ever considered how much more you could achieve with less time spent on documentation?
Recent studies have shown that AI medical scribes can reduce documentation time by 50-75%. This leads to substantial improvements in clinician satisfaction and reduced burnout, fostering a healthier work environment. As medical leaders increasingly acknowledge the potential of AI in automating client care processes, the demand for such solutions continues to grow. The AI medical market is projected to reach $187 billion by 2030, reflecting a significant shift towards efficiency.
CosmaNeura stands out by providing a solution that not only improves operational efficiency but also honors the fundamental principles of faith-based medical services. We invite you to explore how our platform can support you in your mission to deliver compassionate care while alleviating administrative burdens. Together, we can create a healthier future for both providers and patients.
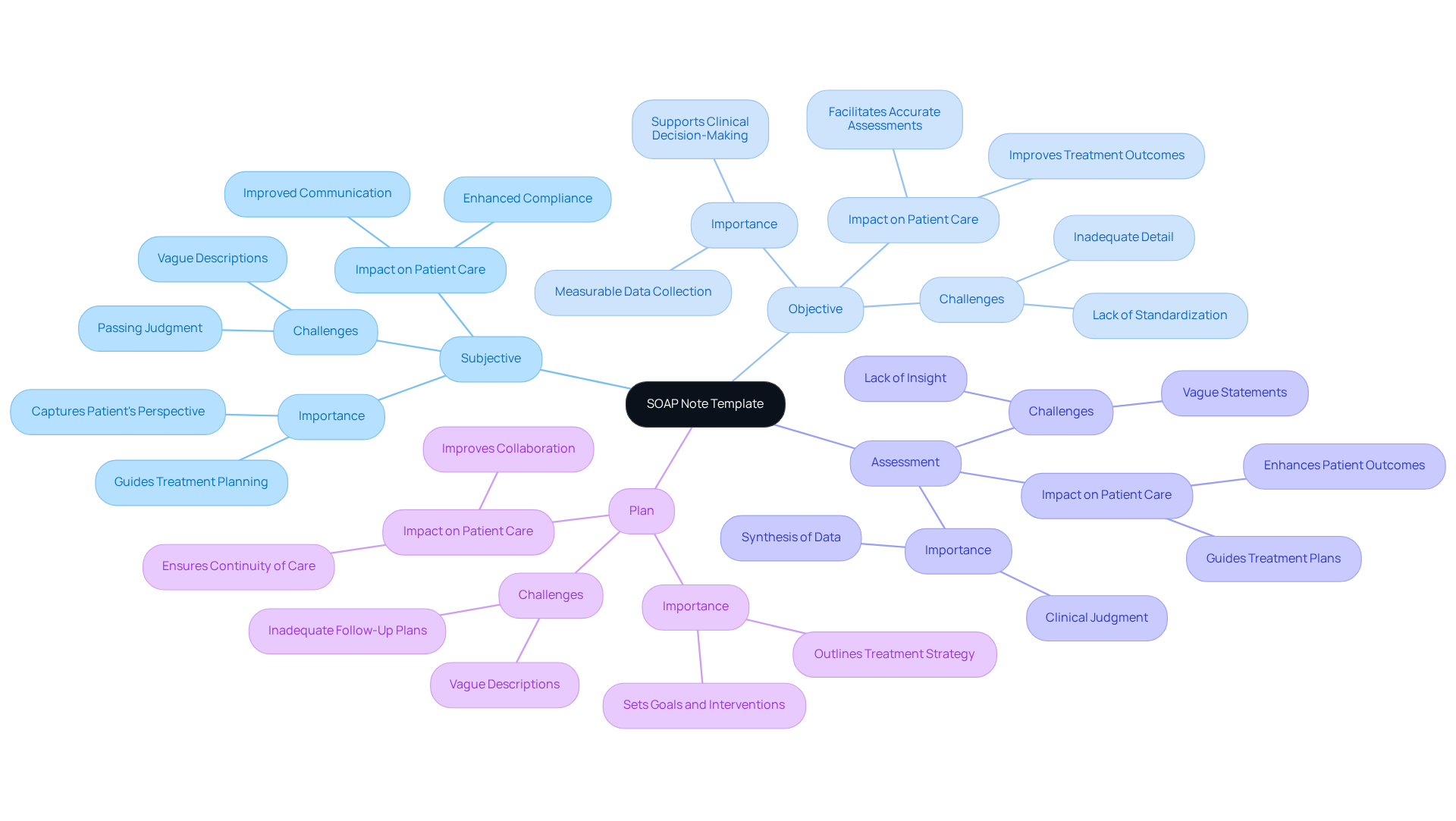
SOAP Note Template: Structured Documentation for Patient Interactions
The SOAP (Subjective, Objective, Assessment, Plan) template serves as a cornerstone of organized healthcare records, enabling providers to compassionately gather vital information about individuals. This structured format ensures that subjective experiences, such as a patient's feelings and concerns, are thoughtfully documented alongside objective findings, including measurable data like vital signs and test results. Have you ever wondered how much clarity this can bring to patient care?
Recent research reveals significant improvements in record quality, with overall SOAP scores rising from 21.9±13 to 61.8±23 following focused training interventions (p<0.001). Additionally, the Objective component scores increased from 25.3±18.3 to 71.3±25.2 after training (P<0.001). This underscores the effectiveness of organized records in enhancing clinical practice. By fostering clear communication among medical teams, SOAP records not only improve clinical decision-making but also lead to better outcomes for individuals, as evidenced by improved compliance with treatment plans and more precise evaluations.
However, challenges remain. Common errors, such as vague descriptions in the Plan component, highlight the necessity for ongoing training and meticulous attention to detail. Experts emphasize that organized records, such as a clinical note template, are crucial for efficient medical service, reinforcing the need for consistent and clear documentation that supports clinical reasoning and continuity of care.
In a landscape where fragmented medical systems often lead to disjointed communication, organized records can bridge these gaps, ensuring that all providers involved in a patient's care are aligned. Regulatory concerns, particularly those related to HIPAA, further complicate these communication barriers, making structured documentation even more vital.
As noted by Delitto and Snyder-Mackler, a sequential approach to clinical reasoning is encouraged, aiding professionals in effectively gathering and evaluating information. Developed by Dr. Lawrence Weed in the 1960s, SOAP documentation remains a crucial resource in modern clinical practice, especially as emerging generative AI technologies aim to streamline administrative tasks and enhance patient-physician interactions. Let’s continue to embrace these tools and approaches to improve the care we provide.
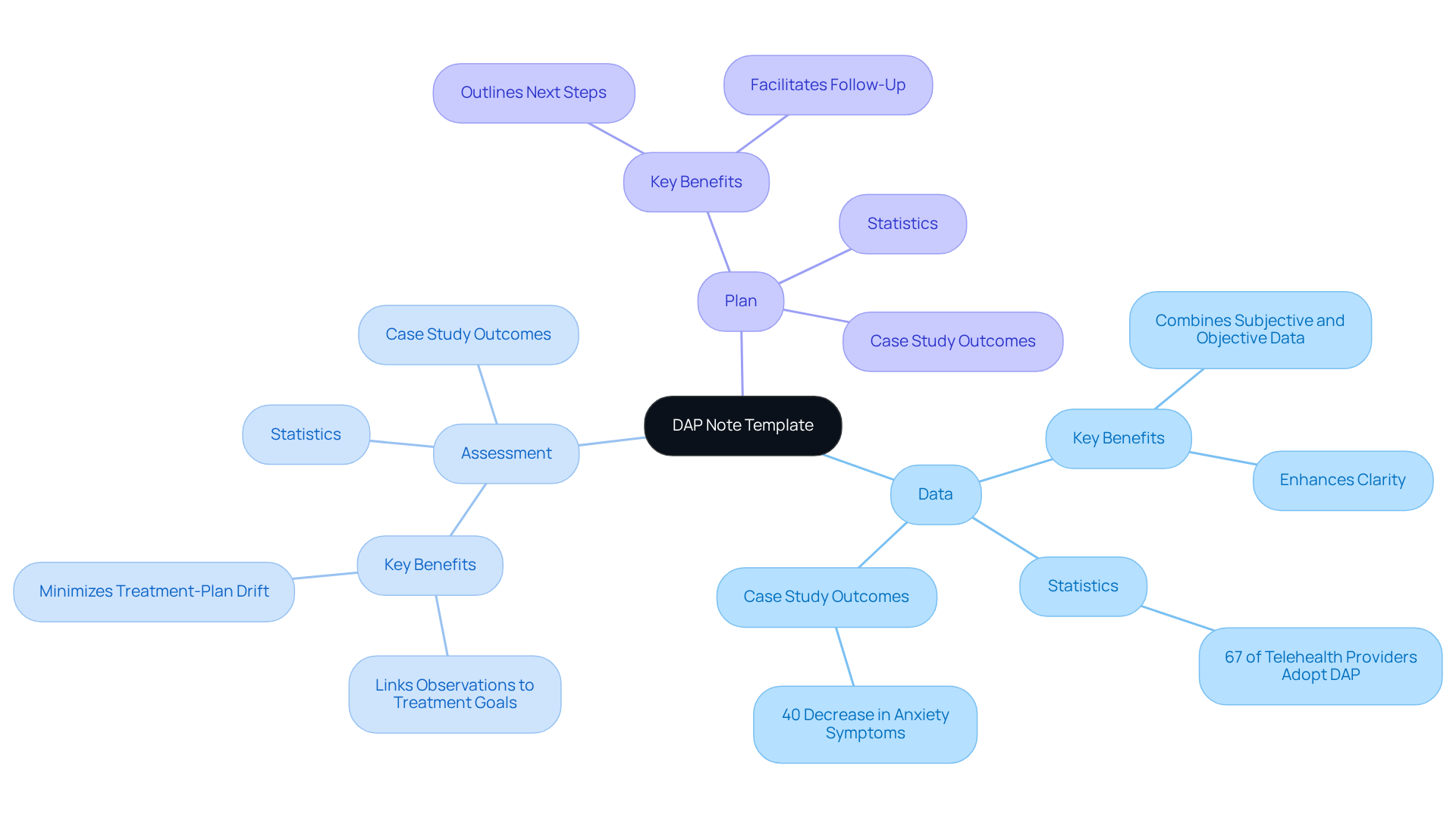
DAP Note Template: Comprehensive Assessment and Planning Framework
The DAP (Data, Assessment, Plan) note template serves as a vital tool for comprehensive evaluations and treatment planning, particularly within the often fragmented healthcare systems we navigate today. By organizing information into three distinct sections, this template ensures that clinicians can gather essential data, provide informed evaluations, and create actionable plans tailored to each individual's unique needs. This structured approach not only enhances clarity but also fosters the development of personalized treatment strategies that align with patient goals, ultimately improving communication and coordination among multidisciplinary teams.
Have you noticed the recent shift towards unified recording frameworks? A 2023 report highlights that 67% of telehealth providers are now embracing software solutions that simplify therapy records and billing. This trend underscores the efficiency of the DAP format, which allows clinicians to reduce documentation time by about 30% while meeting payer requirements. For instance, a case study revealed that therapists utilizing DAP records were able to identify anxiety triggers in clients, leading to a remarkable 40% decrease in symptoms over three months.
Moreover, the DAP framework supports effective treatment planning by directly linking observations to therapeutic objectives, minimizing the risk of treatment-plan drift. This alignment not only improves outcomes for individuals but also enhances communication among multidisciplinary teams, ensuring continuity of care. The flexibility of DAP records allows practitioners to customize documentation according to specific client circumstances, further enhancing personalized care and addressing the administrative hurdles that often impede efficient medical service delivery.
As healthcare providers increasingly recognize the importance of thorough records, the DAP template emerges as a crucial element in fostering high-quality patient care. Additionally, the legal validity of DAP records provides an extra layer of protection for clinicians, ensuring compliance with necessary standards. However, it’s important to acknowledge the challenges healthcare professionals face in completing DAP records due to demanding schedules, which can impact the thoroughness of their reports.
In summary, the DAP template stands out as an effective framework for enhancing care and record-keeping practices, especially in light of the inefficiencies prevalent in today’s healthcare landscape. How can we further support each other in overcoming these challenges and ensuring our patients receive the best possible care?
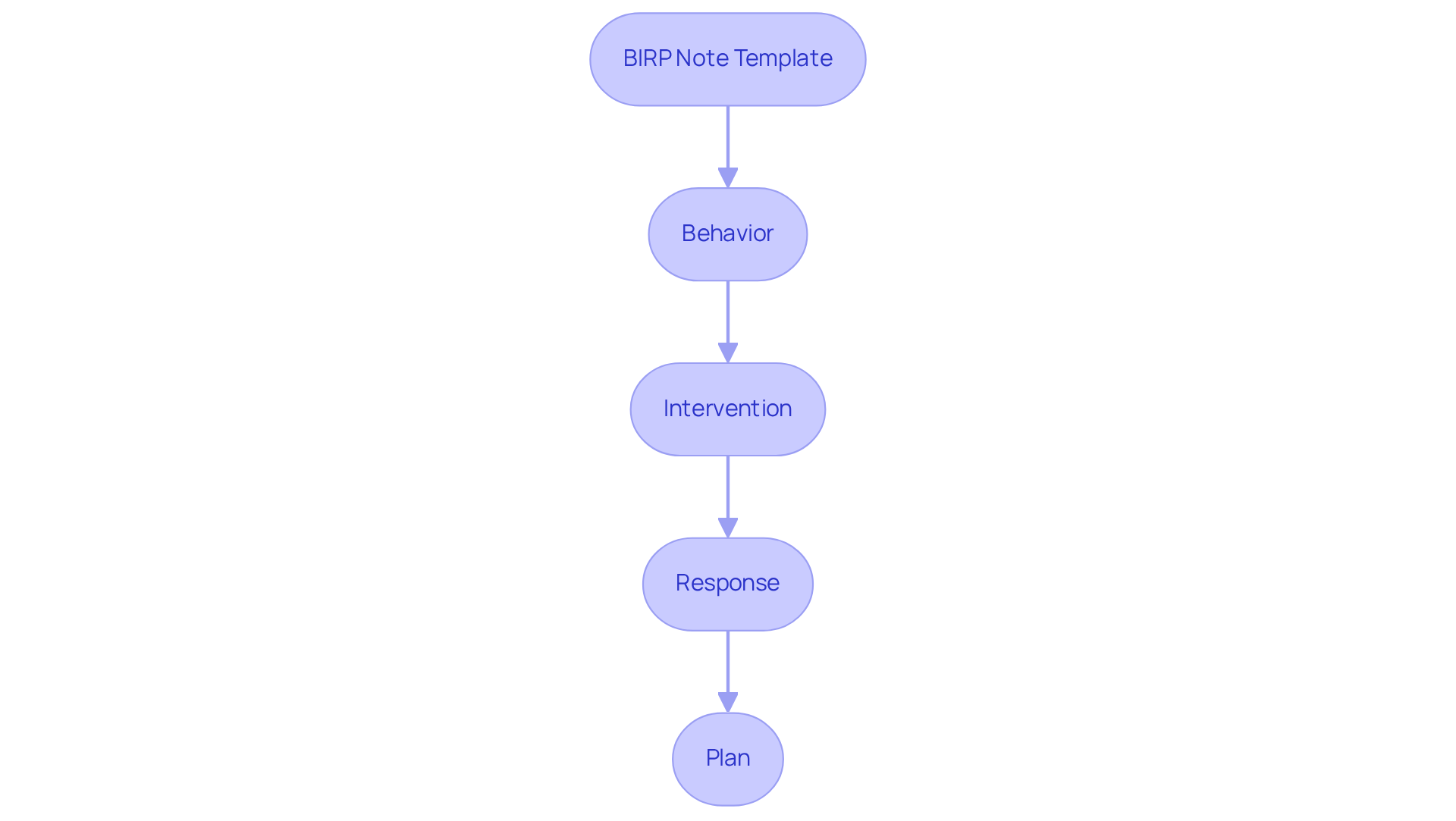
BIRP Note Template: Tailored Documentation for Behavioral Health Providers
In the demanding field of behavioral health, providers often face emotional challenges that can impact their ability to deliver optimal care. The BIRP (Behavior, Intervention, Response, Plan) clinical note template offers a compassionate solution, designed specifically for behavioral health professionals. This structured format not only facilitates comprehensive documentation of client interactions but also emphasizes four essential elements:
- The individual’s behavior
- The interventions applied
- The individual’s reaction to those interventions
- The future treatment strategy
By utilizing the BIRP template, providers can effectively address the distinct needs of those they serve, ensuring a clear and organized record of therapeutic progress. This method fosters better communication among medical professionals and aids adherence to legal and ethical standards, ultimately leading to improved outcomes for patients. Customized record-keeping methods like BIRP entries are vital in capturing the subtleties of patient care, enabling clinicians to track progress over time and adjust treatment approaches as necessary.
In the context of fragmented healthcare systems, effective records such as BIRP entries can bridge communication gaps, promoting better coordination among providers. However, newer clinicians may find BIRP records challenging due to their reliance on clinical theory. Incorporating these practices into regular documentation can significantly enhance the quality of care delivered, especially as generative AI tools emerge to alleviate administrative burdens and optimize interactions with individuals.
Are you ready to embrace this structured approach? By integrating the clinical note template into your practice, you can support your patients more effectively while navigating the complexities of healthcare documentation. Together, let’s enhance the care we provide and foster a nurturing environment for those who depend on us.
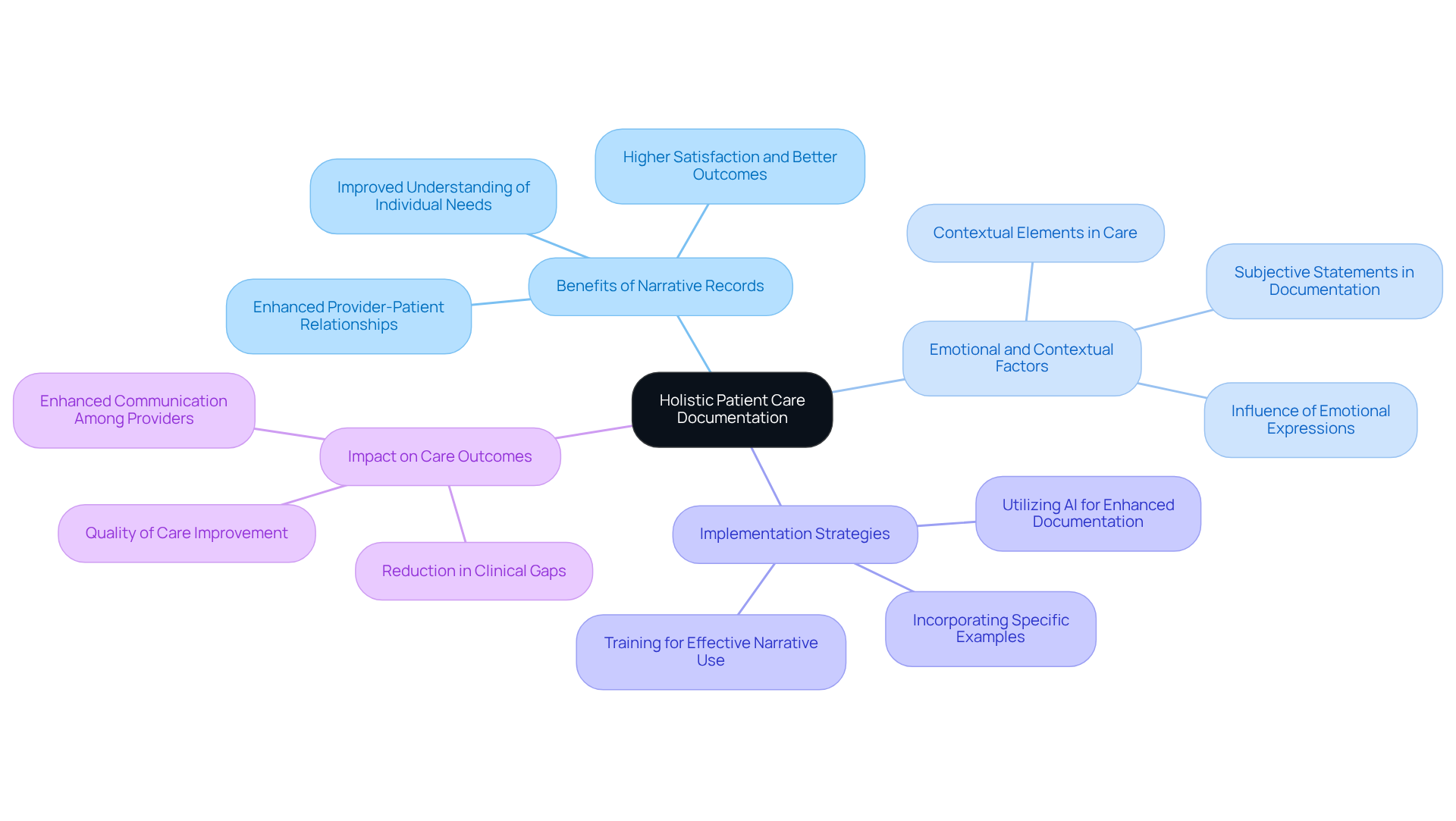
Narrative Note Template: Holistic Patient Care Documentation
The narrative template offers a flexible structure for capturing care in a thorough and illustrative manner. This approach allows healthcare providers to encompass the complexities of client interactions, including emotional and contextual elements that can profoundly influence care outcomes. Have you ever considered how storytelling can enhance your understanding of an individual's journey? By utilizing narrative records, providers can create a more detailed account, fostering deeper relationships and improving comprehension of individual needs.
Recent studies highlight that narrative documentation is regarded as the gold standard in therapy. It supports high-quality care by capturing nuances that structured formats often overlook. This method not only enhances provider relationships but also enables a more personalized approach to care, ultimately leading to greater satisfaction and improved outcomes. Imagine the impact of connecting isolated electronic health records through AI platforms, facilitating collaborative decision-making between individuals and providers—this is crucial for optimized outcomes.
The importance of detailed records in medical settings cannot be overstated. They play a vital role in communicating the full spectrum of individual experiences and clinical reasoning, thereby enhancing the overall quality of care. To effectively implement narrative notes, medical professionals might consider incorporating specific examples from individual interactions that illuminate emotional and contextual factors. This ensures a comprehensive understanding of each individual's journey, nurturing a supportive environment for both providers and patients.
CBE Template: Efficient Documentation for Significant Patient Changes
The Charting by Exception (CBE) template is a compassionate solution aimed at improving record-keeping efficiency, focusing on the crucial changes in a patient's condition. Have you ever felt overwhelmed by the sheer volume of information you need to manage? This method effectively reduces redundant details, allowing healthcare providers to swiftly identify and address critical issues that truly matter. By utilizing this template, providers can simplify their record-keeping processes, leading to significant time savings.
Hospitals that have embraced CBE report a remarkable decrease in record-keeping time, enabling clinicians to dedicate more attention to direct patient care. Imagine the difference this could make in your daily routine! The incorporation of AI in the CBE process further enhances this efficiency by automating routine tasks, thereby reducing the risk of burnout—an alarming 53% among physicians—and ensuring that essential information is captured accurately.
Ultimately, CBE transforms the record-keeping environment in the medical field, fostering a more effective and patient-focused approach. It’s time to embrace this change and prioritize what truly matters: the well-being of your patients.

POMR Template: Problem-Centric Documentation for Patient Care
The Problem-Oriented Medical Record (POMR) template addresses the emotional challenges faced by healthcare providers by transforming documentation to focus on specific clinical issues. This organized method empowers healthcare professionals to systematically tackle each issue, ensuring a thorough consideration of all facets of care. Have you ever felt overwhelmed by the volume of administrative tasks? Recent studies reveal that utilizing POMR significantly enhances clinical reasoning, leading to improved patient outcomes through targeted interventions.
For instance, one study found that the application of POMR improved the precision and utility of clinical notes, with scores rising from 37.5 to 39.0. This demonstrates a clear advantage in record quality. Additionally, implementing POMR has been associated with a decrease in cognitive load, which is crucial in alleviating clinician burnout—a pressing concern in today's medical environment, costing the system around $4.6 billion each year. By streamlining administrative tasks and enhancing documentation efficiency, the POMR template can serve as a vital tool in leveraging generative AI and technologies like automated scheduling and electronic medical records, ultimately easing the burdens faced by providers.
Despite these benefits, current usage rates of POMR remain suboptimal. This highlights the need for ongoing education and support to encourage its integration into everyday clinical practice. By adopting POMR, medical professionals can enhance their clinical reasoning skills, resulting in improved care and satisfaction for individuals. Wouldn't it be rewarding to see the positive impact on patient care and your own well-being? Let's work together to embrace these solutions for a brighter future in healthcare.

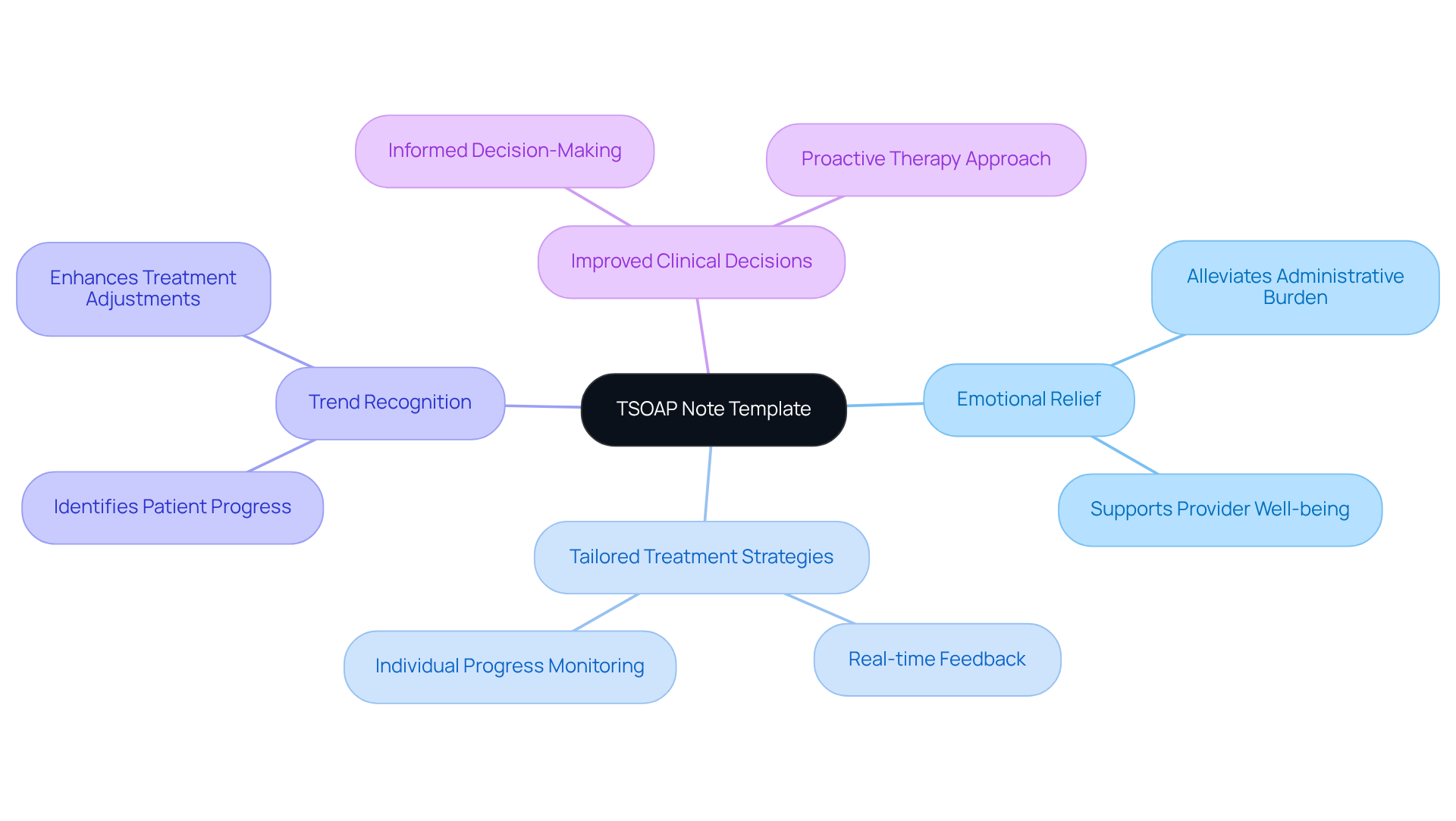
TSOAP Note Template: Focused Documentation for Therapeutic Sessions
The TSOAP (Therapeutic SOAP) template serves as a vital tool for healthcare providers, designed to alleviate some of the emotional burdens they face in recording therapeutic sessions. By blending the structured format of traditional SOAP entries with a focus on therapeutic interventions, TSOAP allows providers to capture the intricate nuances of the therapeutic process.
Have you ever felt overwhelmed by the administrative tasks that can overshadow patient care? TSOAP records empower healthcare providers to monitor individual progress methodically. This ensures that treatment strategies are tailored based on real-time feedback and results, making a significant difference in patient outcomes.
Organized records not only enhance the clarity of medical files but also help in recognizing trends in individual progress. This ultimately leads to more informed clinical decisions. The importance of tracking client progress through TSOAP records is profound. It fosters a proactive approach to therapy, enabling providers to respond promptly to the evolving needs of those they serve.
By embracing TSOAP, you can transform your practice, ensuring that your clients receive the compassionate care they deserve. Consider how implementing this approach could enhance your therapeutic relationships and improve client outcomes.
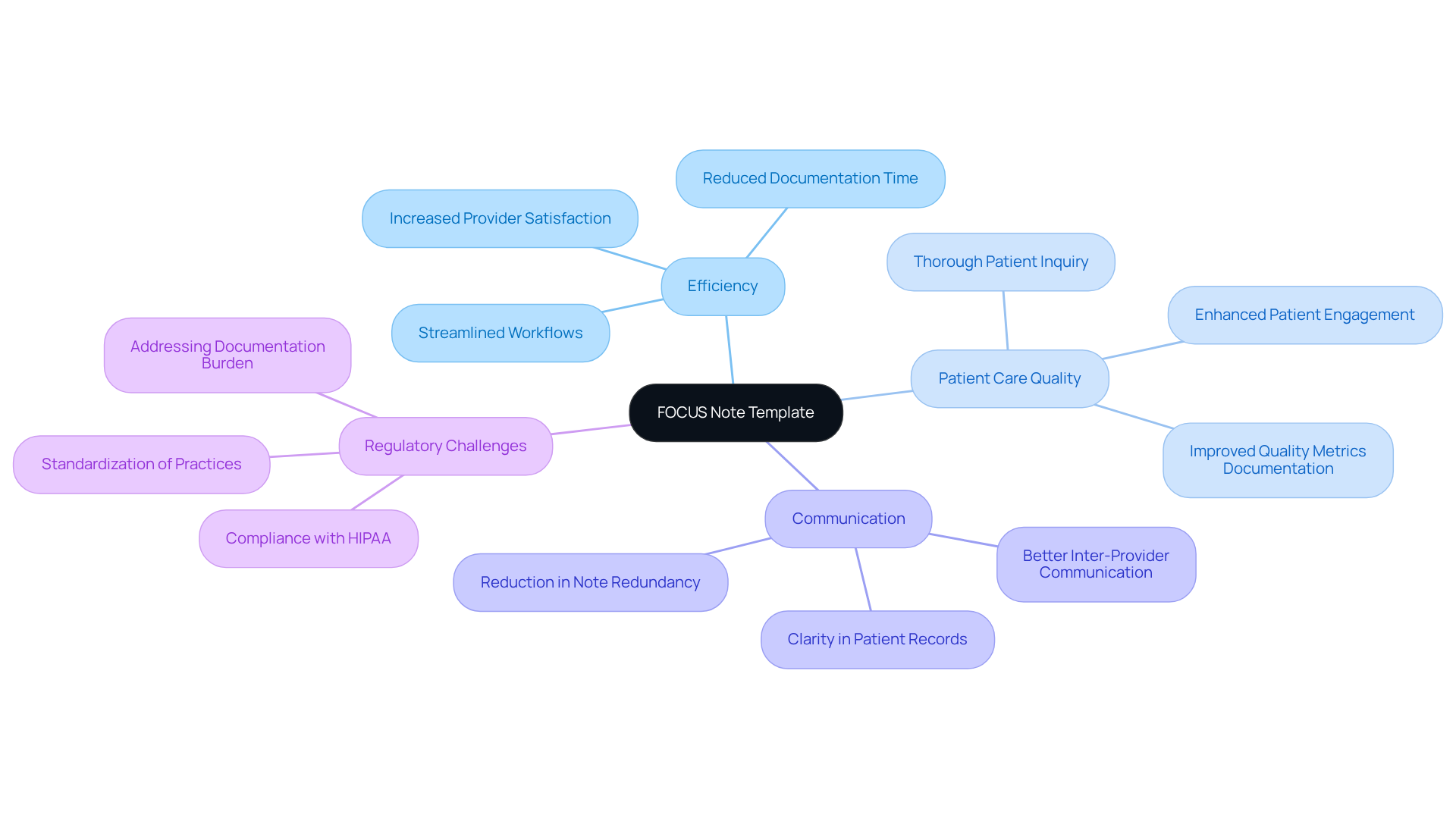
FOCUS Note Template: Streamlined Documentation for Patient Care
The FOCUS note template is thoughtfully designed to alleviate the documentation burden that healthcare providers face daily. By concentrating on the essential aspects of care, this targeted approach fosters an environment where vital information is easily accessible. Have you ever felt overwhelmed by record-keeping demands? By utilizing the FOCUS template, providers can enhance their efficiency and prioritize client care, particularly in fragmented medical systems that often hinder communication and coordination.
This streamlined approach not only reduces the time spent on documentation but also enriches the quality of interactions with patients, allowing for deeper engagement. As trends indicate a growing awareness of the need for more efficient record-keeping methods, medical practitioners are increasingly striving to balance thoroughness with efficiency. Imagine a world where concise documentation leads to improved medical service delivery, addressing regulatory challenges like HIPAA while keeping patient care at the forefront.
Ultimately, the clinical note template serves as an example of how thoughtful documentation can transform the healthcare experience. We invite you to explore this innovative solution and discover how it can support your practice in navigating the complexities of patient care.
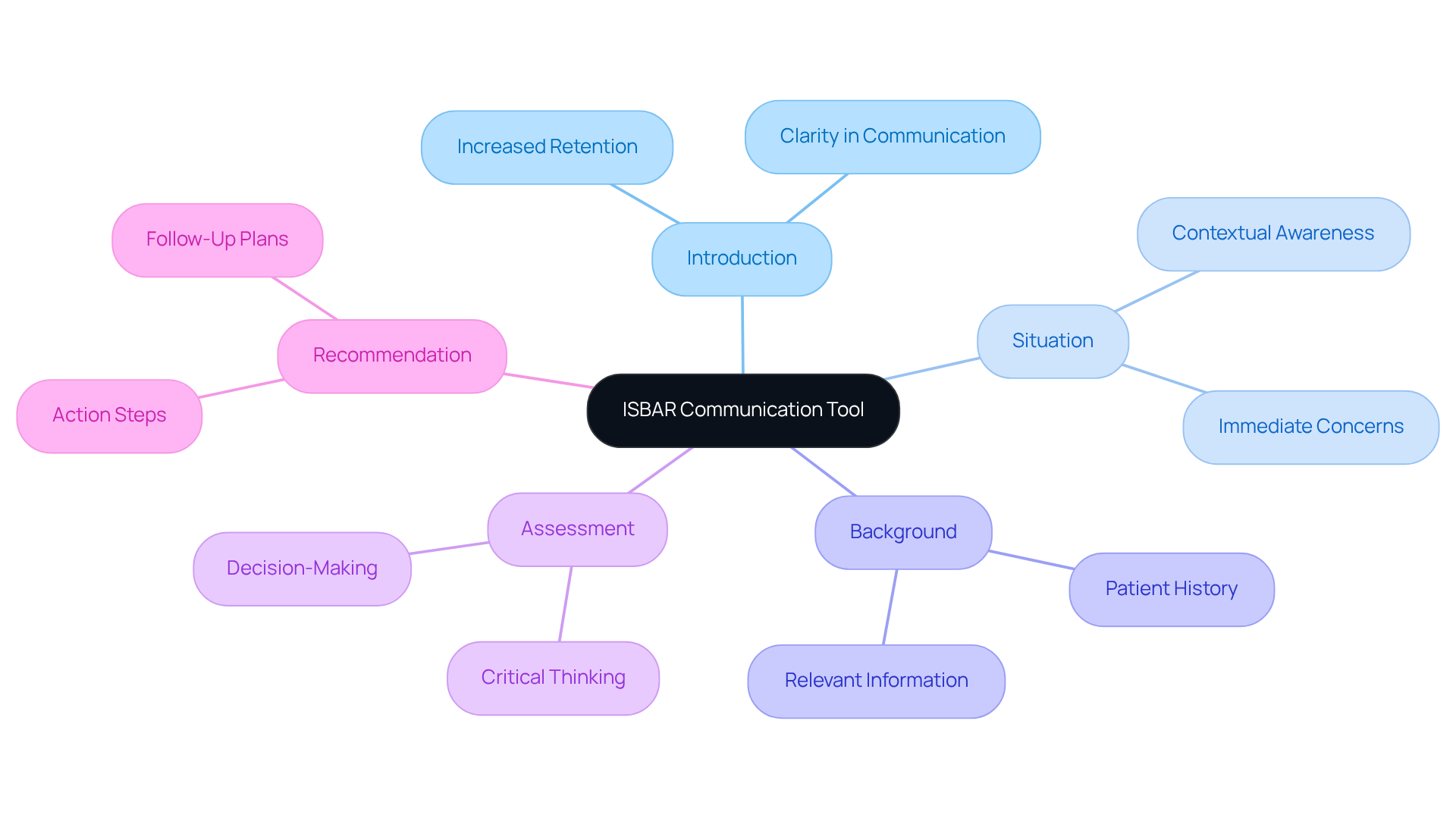
ISBAR Template: Effective Communication Tool for Healthcare Teams
In the demanding world of healthcare, effective communication is not just a necessity; it’s a lifeline. The ISBAR (Introduction, Situation, Background, Assessment, Recommendation) template serves as a vital tool for medical teams, ensuring that essential information is shared clearly and efficiently. Have you ever felt overwhelmed by the sheer volume of information during handovers? This structured format not only alleviates that stress but also fosters a nurturing environment for collaboration among providers.
Research shows that using ISBAR can enhance key information retention by up to 19% for nurses and 18% for physicians. Imagine the difference this could make in clinical handovers, significantly boosting their effectiveness. By embracing the ISBAR framework, medical teams can improve their communication processes, especially in high-stakes settings like emergency departments, where the risk of clinical errors can be daunting.
Furthermore, adopting ISBAR has been found to reduce inquiries during handovers by approximately 30%. This indicates a more effective transfer of information, which is crucial for patient safety. As healthcare providers, we all share the goal of delivering the best care possible, and ISBAR not only enhances patient safety but also promotes interdisciplinary teamwork.
The integration of ISBAR into clinical practice is essential for fostering a culture of effective communication. This culture is increasingly recognized as a cornerstone of quality healthcare delivery. Let’s commit to nurturing this environment together, ensuring that our communication supports not just our work but, most importantly, the patients we serve.
Conclusion
The exploration of essential clinical note templates underscores the transformative role these tools play in enhancing healthcare documentation and patient care. By adopting structured templates such as SOAP, DAP, BIRP, and others, healthcare providers can alleviate administrative burdens, allowing them to focus more on delivering quality care to their patients.
Consider the emotional challenges faced by healthcare providers. The weight of documentation can often overshadow the core mission of patient care. Each template serves distinct purposes; for example, the DAP template offers comprehensive assessment capabilities, while the narrative approach captures the complexities of individual patient journeys. The integration of AI technologies, like those offered by CosmaNeura, further amplifies these benefits by automating routine tasks, reducing clinician burnout, and fostering a more satisfying work environment.
In light of the increasing demands on healthcare providers, embracing these clinical note templates is not just an option but a necessity. By prioritizing efficient documentation practices, healthcare teams can enhance communication, improve patient outcomes, and create a more compassionate care experience. The call to action is clear: healthcare professionals are encouraged to explore and implement these innovative solutions. Together, we can pave the way for a more effective and patient-centered healthcare system.




