Overview
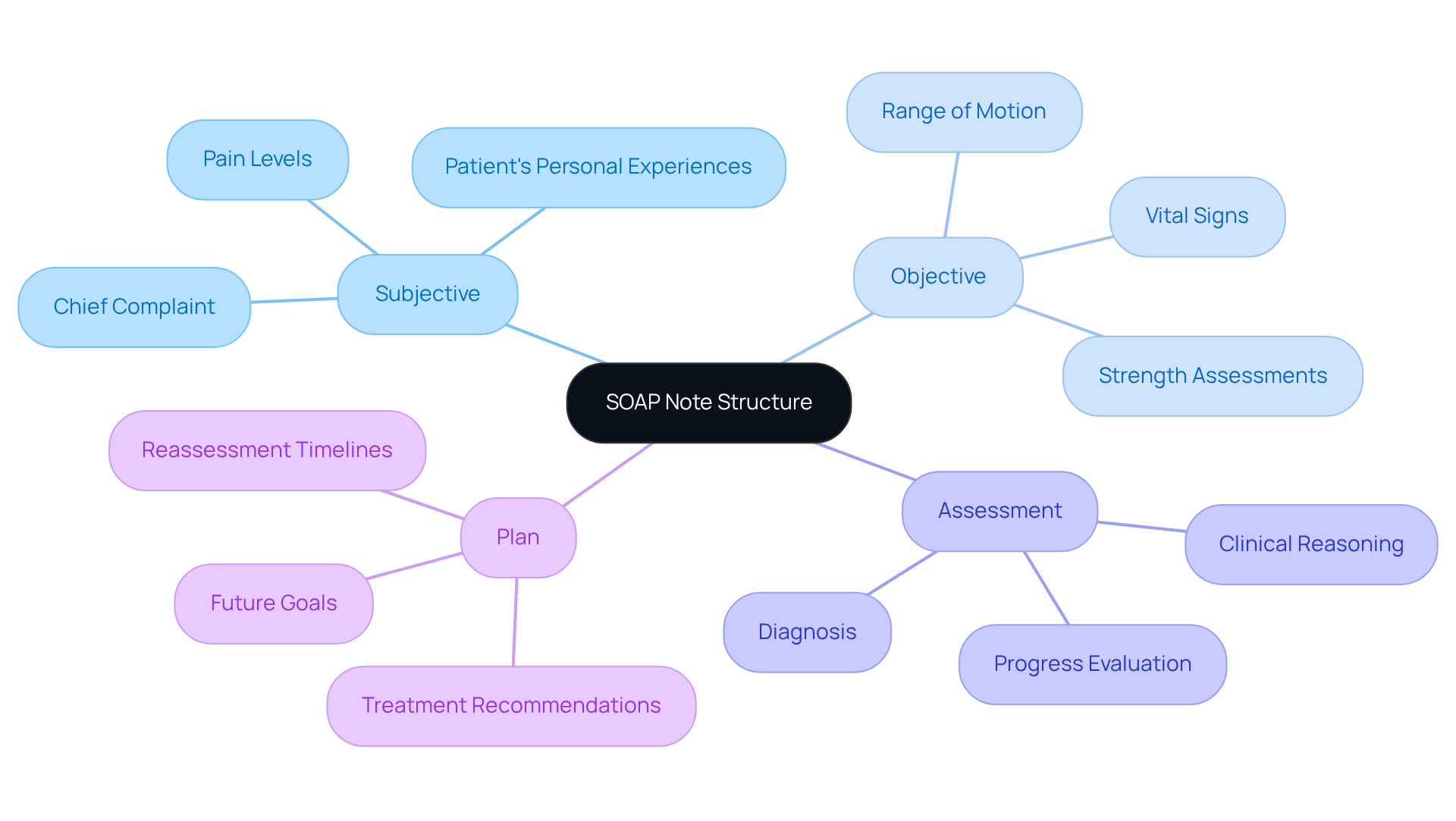
The article titled "10 Clinical SOAP Note Examples for Effective Patient Documentation" seeks to support healthcare professionals by offering practical examples of SOAP notes that can enhance patient documentation. It recognizes the emotional challenges faced by providers, particularly the overwhelming nature of administrative burdens that can detract from patient care. By emphasizing the importance of structured documentation across various specialties, it illustrates how detailed records not only improve patient care but also foster better communication among providers. This ultimately leads to enhanced health outcomes and greater job satisfaction for clinicians.
In a field where every detail matters, the article encourages healthcare providers to reflect on their documentation practices. Are you feeling the weight of administrative tasks? The examples provided serve as a gentle reminder of the positive impact that thorough documentation can have on both patient interactions and clinician well-being. By adopting these practices, healthcare professionals can alleviate some of the burdens they face.
The benefits of implementing structured SOAP notes are profound. Not only do they streamline communication, but they also empower clinicians to deliver the best possible care. As you explore these examples, consider how they might transform your own documentation process. Let this be an invitation to enhance your practice and foster a supportive environment for both patients and providers alike.
Introduction
In the fast-paced world of healthcare, effective documentation can often feel like an overwhelming burden for providers. This challenge can detract from the essential task of patient care.
How can we address this emotional strain? This article delves into the transformative power of clinical SOAP notes, showcasing ten compelling examples that not only streamline documentation but also enhance patient interactions.
Yet, amidst the push for efficiency, how can healthcare professionals ensure they maintain the personal touch that is vital for patient trust and satisfaction? This exploration reveals the delicate balance between administrative efficiency and compassionate care. It invites readers to rethink their approach to patient documentation, fostering a deeper connection with those they serve.
CosmaNeura: Streamline SOAP Note Management with AI Automation
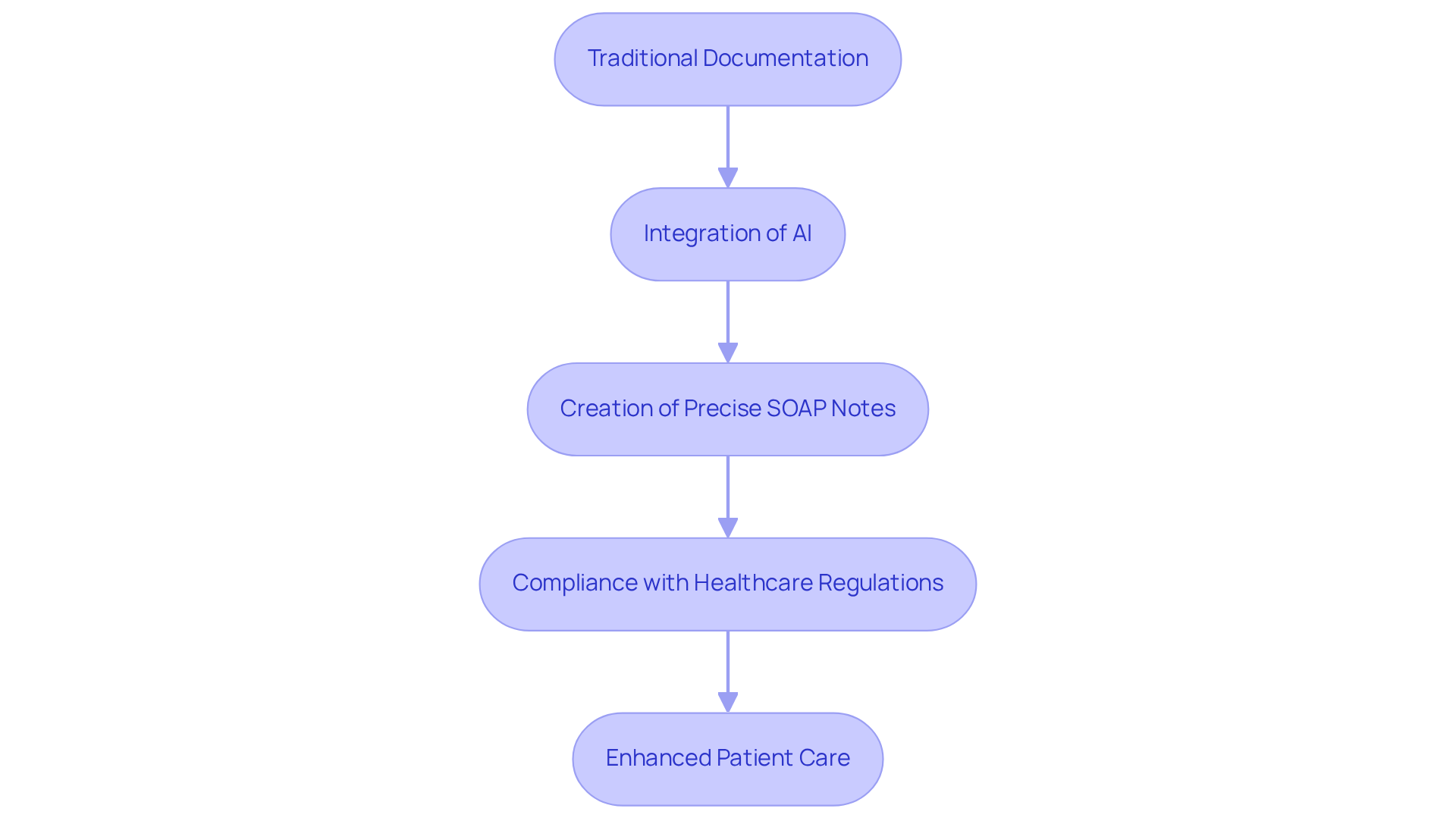
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to deliver compassionate care. CosmaNeura understands these challenges and utilizes advanced AI technology to transform the creation and management of clinical SOAP note examples. This innovation significantly reduces the time spent on record-keeping, allowing providers to focus more on their patients.
By seamlessly integrating AI into clinical workflows, healthcare professionals can create a clinical soap note example that is not only precise but also compliant with healthcare regulations. Imagine the relief of knowing that your documentation is handled efficiently, freeing you to prioritize meaningful interactions with individuals. This shift not only enhances the quality of care but also fosters a more fulfilling work environment.
Moreover, the platform's adaptability to the unique values and requirements of faith-focused providers highlights its commitment to ethical healthcare practices. With research indicating that clinicians dedicate 34% to 55% of their workday to documentation, the efficiency achieved through AI can lead to remarkable improvements in job satisfaction and patient outcomes.
In a world where every moment counts, consider how embracing such technology could transform your practice. Are you ready to reclaim your time and enhance the care you provide? With CosmaNeura, you can take a step towards a more rewarding and impactful healthcare experience.
Mental Health SOAP Note Example: Documenting Patient Interactions Effectively
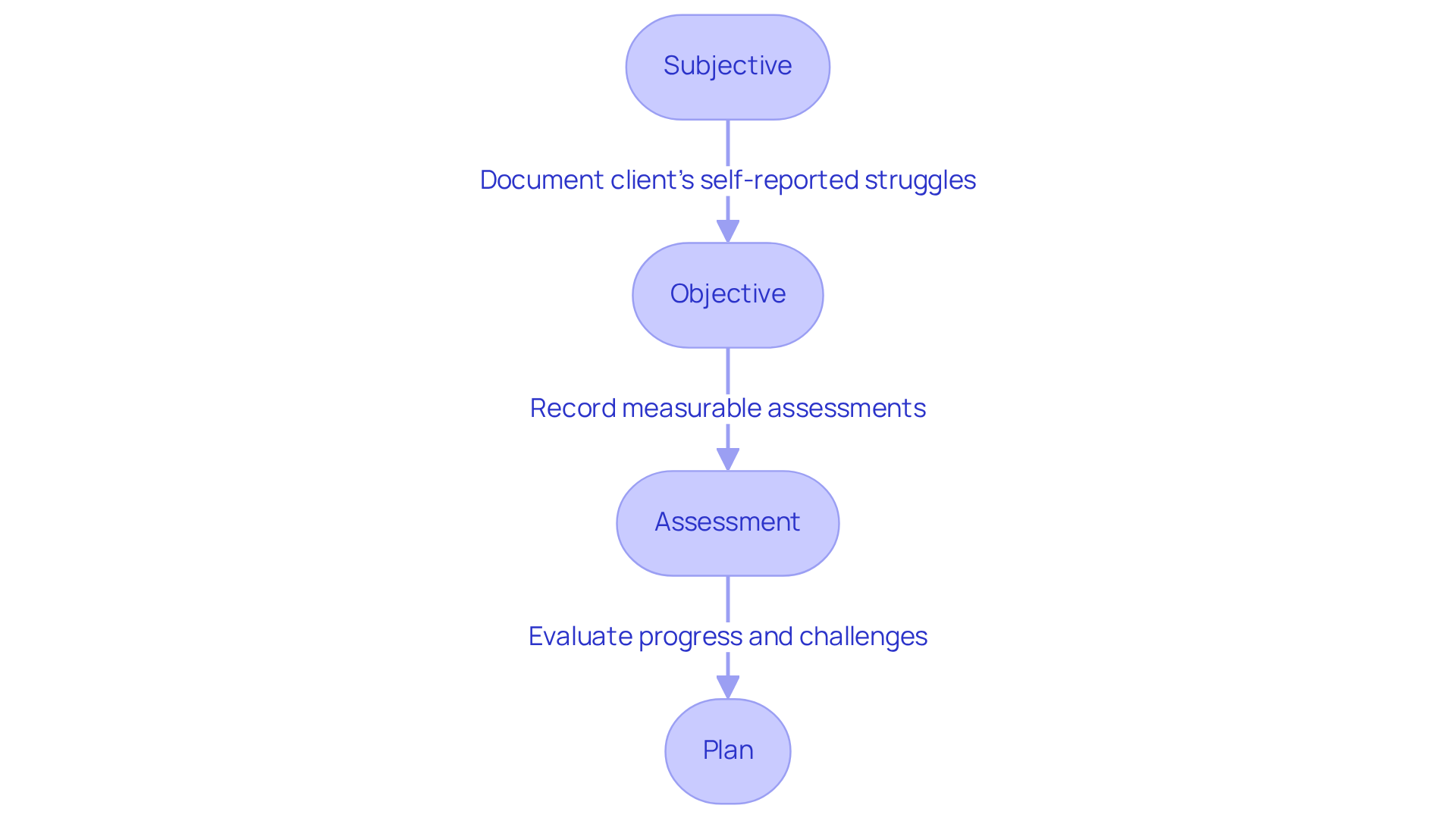
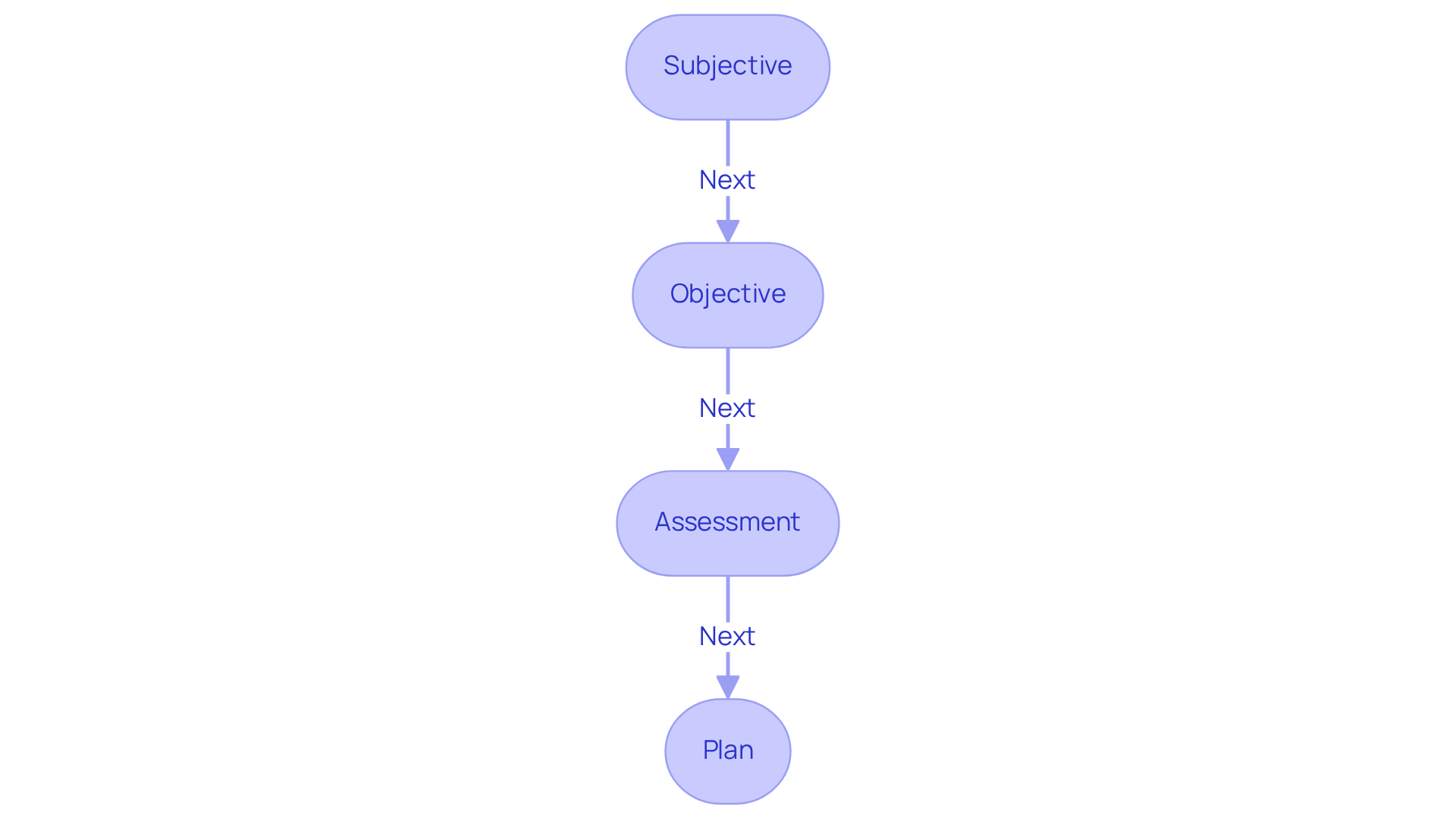
In a mental health SOAP note, the Subjective part captures the individual's self-reported experiences, such as feelings of anxiety and stress stemming from recent life changes. Have you ever felt overwhelmed by everything happening at work and home? For example, an individual might convey, 'I feel overwhelmed with everything happening at work and home.' This expression of distress is crucial for understanding their emotional state.
The Objective section documents observable behaviors, such as restlessness, fidgeting, or changes in speech patterns, like a rapid speech rate or hesitance. Recognizing these signs can help clinicians better understand the individual's experience.
The Assessment reflects the clinician's evaluation, noting the individual's heightened anxiety levels and potential triggers, which is essential for effective treatment planning.
Finally, the Plan outlines therapeutic interventions, including scheduled cognitive-behavioral therapy sessions and follow-up appointments to monitor progress. This structured approach not only ensures comprehensive documentation of the patient's mental health but also facilitates effective communication among healthcare providers. By doing so, we enhance the quality of care, ultimately supporting the individual's journey towards healing and well-being.
Pediatric SOAP Note Example: Capturing Developmental Milestones and Concerns
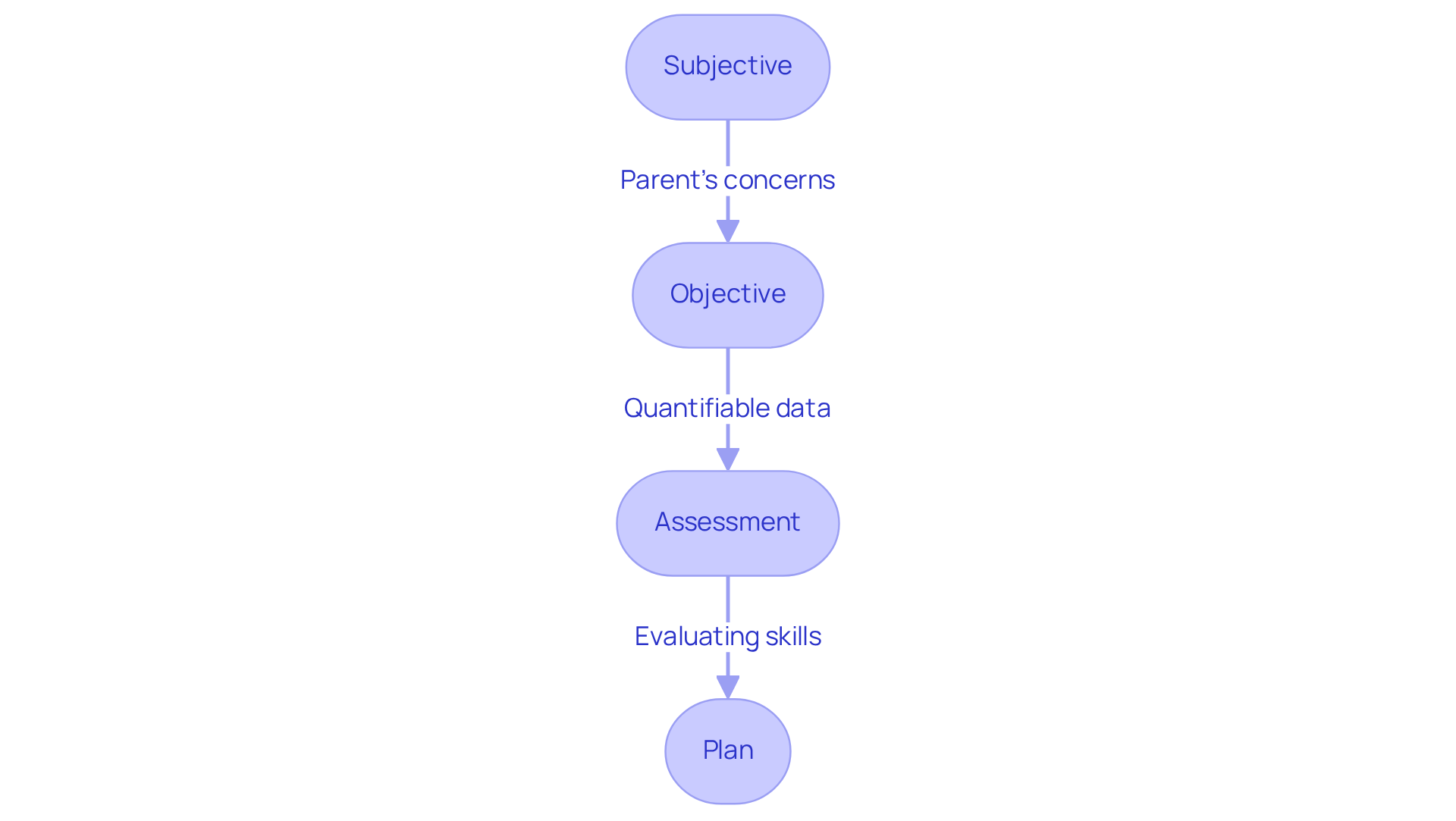
In the Subjective part of a clinical soap note example for pediatrics, a parent often shares their heartfelt worries about their child's speech delays. This moment is crucial, as it reflects the emotional challenges parents face.
In the Objective section, we gather quantifiable data such as the child's age, weight, and developmental milestones achieved, as illustrated in a clinical soap note example. These details are essential for assessing growth and progress. For example, at 2 years, children typically understand about 50% of language and can follow 2-step instructions, which are important benchmarks to consider.
During the Assessment, the clinician compassionately evaluates the child's speech and language skills, creating a clinical soap note example that identifies specific areas of concern that may need attention.
The Plan then outlines thoughtful recommendations for speech therapy sessions and includes a clinical soap note example for regular follow-ups, ensuring that the child's progress is monitored closely. This thorough documentation not only addresses immediate concerns but also reassures parents that all developmental aspects are taken into account in their child's ongoing care.
As pediatricians emphasize, capturing developmental milestones is vital for early intervention. Addressing these concerns early can significantly improve outcomes for children with delays. Remember, 'The earlier developmental delays are identified and addressed, the more positive the prognosis.' This gentle approach not only supports the child but also provides parents with the reassurance they need during a challenging time.
Occupational Therapy SOAP Note Example: Integrating Patient-Centered Goals
In a clinical soap note example, the Subjective section captures the individual's self-reported challenges in daily activities. This section offers valuable insight into their personal experiences and needs, allowing for a more compassionate understanding of their situation.
The Objective section in a clinical soap note example documents specific functional assessments, such as range of motion or strength tests, providing measurable data to support clinical decisions.
The Assessment serves as a clinical soap note example by evaluating the individual's progress towards their personalized goals, highlighting areas of improvement or concern. It's important to note that studies indicate 65% of therapist-caregiver pairs exhibit poor agreement in goal-setting. This statistic underscores the significance of involving caregivers in this process to foster a supportive environment.
Ultimately, the Plan provides a clinical soap note example that details customized interventions, such as adaptive equipment training or home modifications. These interventions ensure that therapy is not only effective but also aligned with the individual's personal aspirations and family values. This structured approach fosters a collaborative environment, enhancing the therapeutic relationship and promoting better outcomes.
How can we further engage caregivers in this vital process? Together, we can create a more nurturing experience for everyone involved.
Physical Therapy SOAP Note Example: Tracking Progress and Outcomes
In a clinical soap note example for physical therapy, the Subjective part begins with the individual’s self-reported pain levels during specific movements. This offers essential context for treatment and acknowledges the emotional challenges faced by patients. In a clinical soap note example, the Objective section captures measurable data, such as range of motion and strength assessments, which are critical for evaluating progress. For instance, when an individual reports an increase in exercise repetitions from 12 to 15 while maintaining the same weight, this indicates meaningful improvement.
The assessment serves as a clinical soap note example that synthesizes this information to analyze the individual’s progress toward rehabilitation goals. Meanwhile, the Plan provides a clinical soap note example that outlines recommendations for continued therapy sessions, specific exercises, and timelines for reassessment. This organized method not only enables efficient monitoring of the individual’s recovery journey but also improves communication among healthcare providers.
Research shows that standardized records, like structured notes, can decrease medical mistakes by as much as 25%, greatly enhancing patient safety and care quality. Furthermore, clinics that adopt organized note practices experience a 15-20% decrease in denied insurance claims. This highlights the significance of careful documentation in ensuring compliance and justifying treatment necessity.
The structured note methodology, theorized by Larry Weed almost 50 years ago, remains vital today. It serves as an essential legal document that safeguards therapists and clinics by illustrating compliance with professional standards. By embracing these practices, we can better support our patients and improve outcomes for those receiving care.
How can we further enhance our documentation to ensure the best for our patients?
Speech Therapy SOAP Note Example: Documenting Communication Progress
In a clinical soap note example for speech therapy, the Subjective part captures the client's self-reported struggles with articulation, including difficulty pronouncing specific sounds or expressing thoughts clearly. Have you ever considered how AI tools could enhance this aspect? By analyzing individual responses and suggesting relevant follow-up questions, these tools can help gather more detailed insights, making the process feel more supportive.
The Objective section serves as a clinical soap note example by recording measurable speech assessments, including fluency rates and vocabulary usage, which provide concrete data on the client's performance. Imagine the efficiency gained by automating data collection and analysis—AI can ensure accuracy, allowing healthcare providers to focus more on what truly matters: the client.
In the Assessment phase, we evaluate the client's progress towards established speech goals, as outlined in a clinical soap note example, acknowledging both improvements and ongoing challenges. With AI tools, tracking these metrics over time becomes seamless, offering a clearer picture of the client's development. This clarity can be incredibly reassuring for both clients and providers alike.
Finally, the Plan provides a clinical soap note example that outlines targeted exercises and strategies tailored to the client's needs, such as articulation drills or engaging language games. By employing AI for record-keeping, healthcare providers can simplify their processes, enabling greater emphasis on care and fostering meaningful connections with individuals. This organized approach not only facilitates effective tracking of the client's journey but also supports informed decision-making in therapy, ensuring that every step taken is in the best interest of the client.
Geriatric SOAP Note Example: Addressing Complex Health Needs
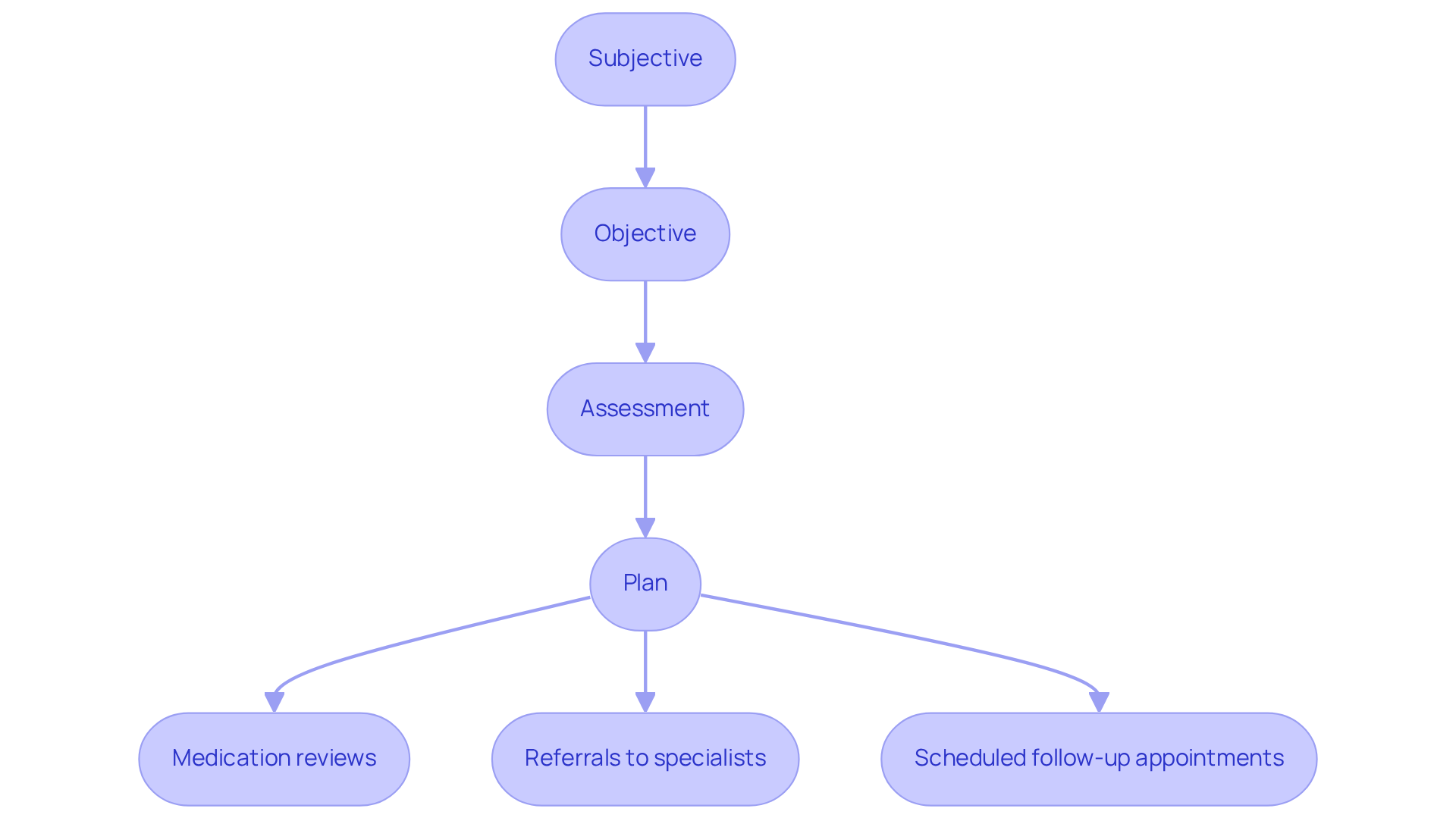
In the realm of elder care, the process begins with the Subjective section of a clinical soap note example, where individuals share their chronic pain and mobility concerns. This highlights the importance of attentive listening and meticulous record-keeping, as these elements are crucial in understanding their experiences.
Moving to the Objective section, vital signs and evaluations of cognitive function are documented, providing essential insights into the individual's overall health.
The Assessment then evaluates the individual's condition, considering factors such as polypharmacy and cognitive decline—issues often faced by older adults. This thoughtful analysis is pivotal in tailoring care to meet their unique needs.
Finally, the Plan outlines a range of multidisciplinary interventions, including:
- Medication reviews
- Referrals to specialists
- Scheduled follow-up appointments
This comprehensive documentation serves as a clinical soap note example and is not just a formality; it is vital for effectively managing the intricate health requirements of older individuals. By improving communication among healthcare providers, it supports continuity of care. Well-organized documentation not only tracks changes in functional abilities and cognitive status but also ensures that essential geriatric-specific factors are acknowledged. Ultimately, this leads to enhanced outcomes for individuals, fostering a nurturing environment that prioritizes their well-being.
Dermatology SOAP Note Example: Documenting Skin Assessments and Treatments
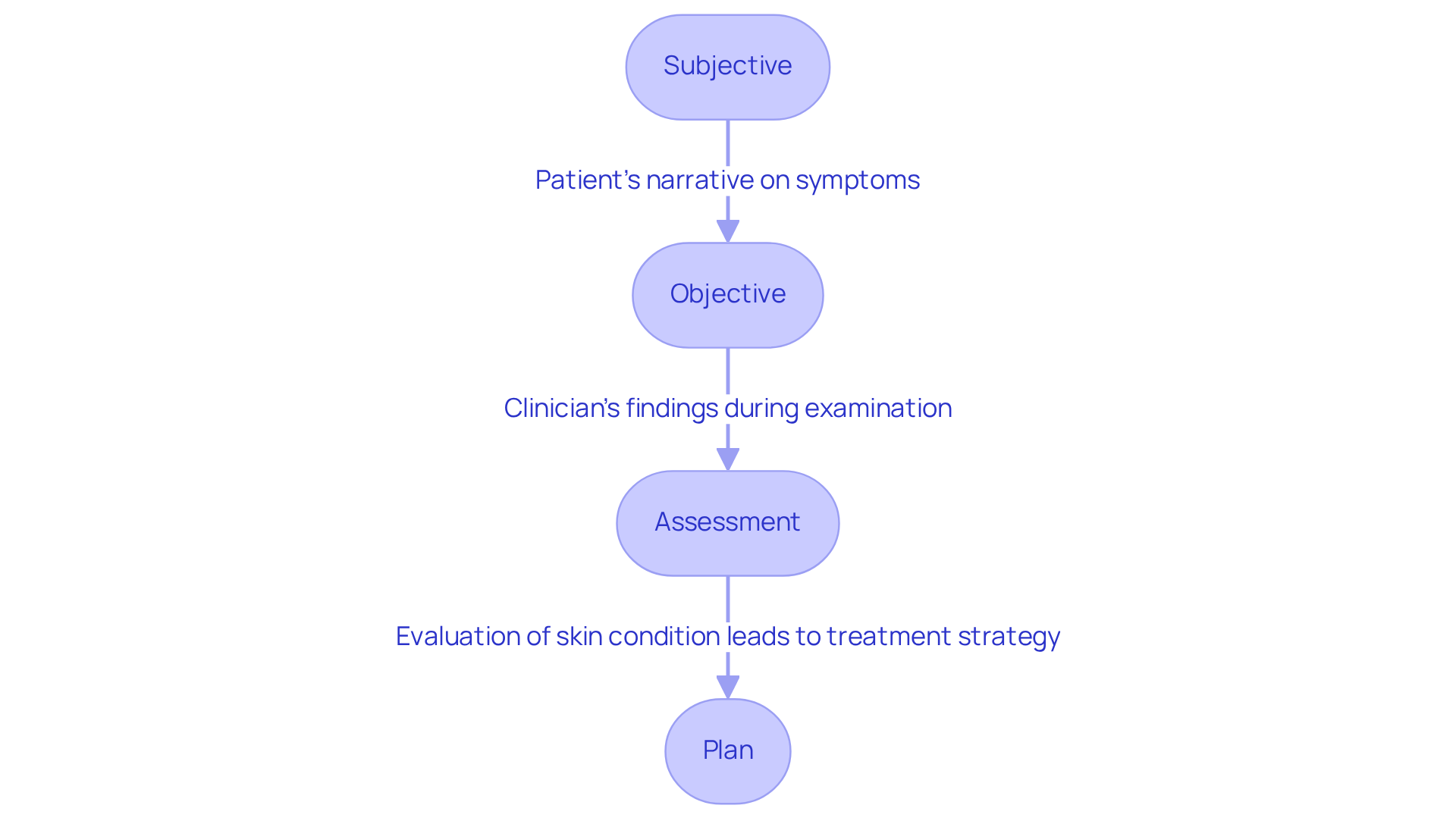
In a clinical soap note example specific to dermatology, the Subjective part captures the individual's narrative regarding skin symptoms, such as itching, rashes, or changes in skin texture. Have you ever felt persistent dryness or discomfort in specific areas? Understanding these personal experiences is crucial. The Objective section of a clinical soap note example documents the clinician's findings during the physical examination, detailing lesion characteristics like size, color, and texture. This information is vital for an accurate diagnosis and shows how much we care about your skin health.
The clinical soap note example evaluates the skin condition, documenting any changes since the last visit. It may include differential diagnoses based on the documented symptoms and findings. This process not only reassures patients but also strengthens the bond between healthcare providers and those they serve. Finally, the Plan outlines the treatment strategy, which could be documented in a clinical soap note example involving topical medications, lifestyle modifications, or referrals to specialists for further evaluation.
This organized method guarantees thorough records of the individual's skin health and improves communication among healthcare professionals. Imagine the better outcomes for those receiving care when everyone is on the same page! Effective documentation practices are essential, as they facilitate better clinical decision-making and adherence to ethical standards in patient care. Let’s work together to ensure that every individual feels heard and supported in their journey to better skin health.
Counseling SOAP Note Example: Reflecting on Therapeutic Sessions
An example of a clinical soap note shows that the Subjective part captures the client's self-reported feelings, such as sadness rated at 6 out of 10, and anxiety related to work deadlines. This aspect is crucial, as it allows us to understand the emotional challenges the client faces. The Objective part records observable behaviors, including changes in mood, engagement levels, and any physical signs of distress, which are essential for a comprehensive view of the client's state.
The Assessment evaluates the client's progress towards therapeutic goals, noting improvements or setbacks in emotional regulation and coping strategies. This evaluation not only highlights the journey but also fosters a sense of hope and motivation for both the client and the counselor. Finally, the Plan outlines actionable strategies for coping, such as mindfulness exercises or cognitive-behavioral techniques, and suggests future session topics to address ongoing concerns.
This structured documentation, which includes a clinical soap note example, is essential for tracking the client's emotional journey, ensuring continuity of care, and guiding future interventions effectively. By focusing on these elements, we can better support our clients and help them navigate their emotional landscapes with compassion and understanding.

General Practice SOAP Note Example: Comprehensive Patient Documentation
In the world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best care. A general practice clinical soap note example serves as a crucial tool in this process. It begins with the Subjective section, where the individual's chief complaint and medical history are thoughtfully recorded. Next comes the Objective part, capturing vital signs and findings from physical examinations. This structured approach helps in understanding each patient's unique situation as illustrated in a clinical soap note example.
In a clinical soap note example, the Assessment section evaluates the individual's overall health status by synthesizing both subjective and objective data, leading to a well-informed diagnosis. Finally, the Plan outlines treatment options, referrals, and follow-up appointments, ensuring a comprehensive approach to care. It’s important to recognize that thorough records not only foster effective communication among healthcare providers but also enhance care coordination, ultimately resulting in better outcomes for individuals.
Have you considered how current trends are shaping this process? The adoption of electronic health records (EHRs) has significantly streamlined documentation, with over 95% of U.S. hospitals utilizing these systems as of 2021. This shift has led to a remarkable 30% increase in the availability of real-time patient data for clinical research and analysis. Such advancements underscore the importance of thorough documentation in enhancing the quality of care.
By embracing these practices, we can alleviate some of the administrative burdens that often weigh on healthcare providers. Together, let’s commit to improving our documentation processes, ensuring that we provide the compassionate and effective care that every individual deserves.
Conclusion
Embracing effective patient documentation through clinical SOAP notes is vital for enhancing healthcare delivery. This structured approach not only streamlines the documentation process but also significantly improves communication among healthcare providers, ultimately leading to better patient outcomes. Imagine a world where healthcare professionals can focus more on patient interactions and less on administrative tasks—this is where tools like AI automation come into play, fostering a more compassionate care environment.
Throughout this article, we've explored various clinical SOAP note examples, highlighting their importance across different specialties such as:
- Mental health
- Pediatrics
- Occupational therapy
- Physical therapy
- Speech therapy
- Geriatrics
- Dermatology
- Counseling
- General practice
Each example underscores the necessity of capturing subjective experiences, objective findings, assessments, and tailored plans to ensure comprehensive patient care. The integration of AI in documentation practices not only enhances efficiency and accuracy but also paves the way for improved job satisfaction among providers and better health outcomes for patients.
As the healthcare landscape continues to evolve, the call to action is clear: let’s prioritize the implementation of structured documentation practices and consider the benefits of AI technologies to transform patient care. By committing to these best practices, healthcare professionals can alleviate administrative burdens, ensure compliance, and ultimately provide the compassionate, effective care that every individual deserves. The future of healthcare documentation is not just about efficiency; it's about enhancing the quality of care and fostering meaningful connections between providers and patients.




