Overview
This article addresses the emotional challenges faced by nurse practitioners in their daily routines. It focuses on providing essential SOAP note templates that can significantly enhance efficiency in clinical documentation. By streamlining the recording process, these templates not only improve accuracy but also allow healthcare professionals to devote more time to meaningful patient interactions rather than getting bogged down by administrative tasks.
Imagine the relief of spending less time on paperwork and more time caring for your patients. These templates are designed with your needs in mind, recognizing the burdens that administrative tasks can place on your ability to deliver quality care. Ultimately, they contribute to better patient outcomes, supporting you in your vital role.
We encourage you to explore these templates and see how they can transform your practice. By adopting these tools, you can reclaim precious time and enhance the quality of care you provide. Your dedication to your patients deserves the best support possible.
Introduction
In the fast-paced realm of healthcare, nurse practitioners often face the emotional challenge of balancing exceptional patient care with the burdens of extensive documentation. This can feel overwhelming, as the weight of administrative tasks can detract from the quality of care they wish to provide. What if there were tools designed to alleviate this stress?
This article explores ten essential SOAP note templates that not only streamline documentation but also enhance the quality of care delivered to patients. As the demand for effective communication and precise record-keeping grows, we must ask ourselves: how can these innovative tools transform the everyday practices of nurse practitioners?
Together, let’s explore solutions that can make a meaningful difference in your practice.
CosmaNeura: AI-Powered Nurse Practitioner SOAP Note Template
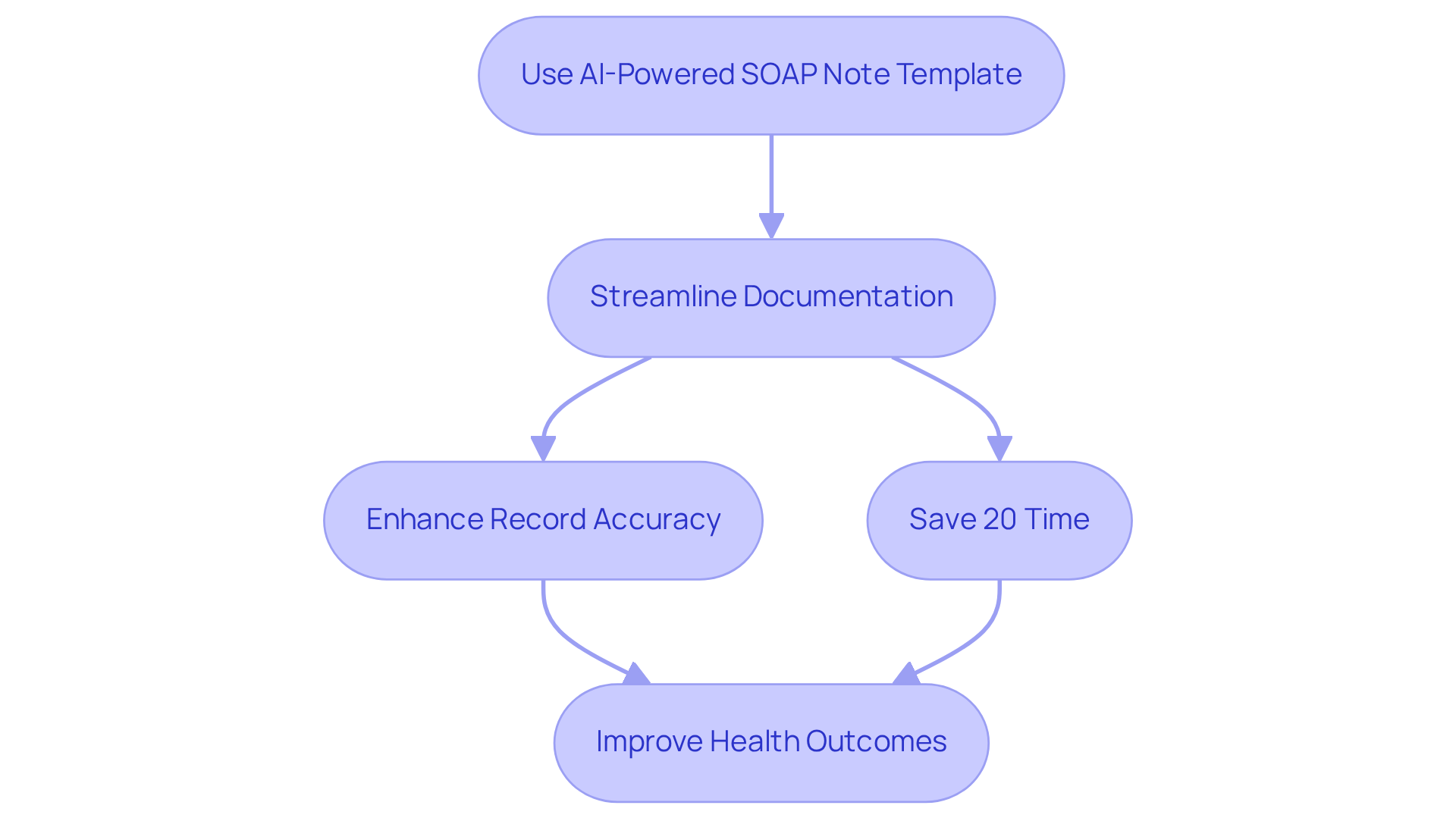
In the demanding world of healthcare, professionals often face overwhelming administrative burdens that can detract from their primary focus—patient care. CosmaNeura understands these challenges and offers a compassionate solution: a cutting-edge nurse practitioner soap note template that utilizes the power of AI. This innovative tool serves as a nurse practitioner soap note template that not only for nurse professionals but also ensures adherence to best practices in clinical record-keeping.
Imagine being able to streamline the creation of encounter records while automatically inputting and analyzing data in real-time. With AI functionalities, the precision and thoroughness of records are greatly enhanced, allowing you to devote more time to what truly matters—providing quality healthcare. In fact, healthcare professionals have noted that AI can save them over 20% of their time spent on documentation efforts.
Moreover, the nurse practitioner soap note template, when assisted by AI, plays a crucial role in improving health outcomes. By capturing essential information accurately and efficiently, they promote a more effective healthcare delivery system. As you reflect on your own experiences, consider how this technology could alleviate some of the pressures you face daily. Embrace the opportunity to enhance your practice and ultimately, the care you provide.
Heidi Health: Versatile SOAP Note Template with Examples
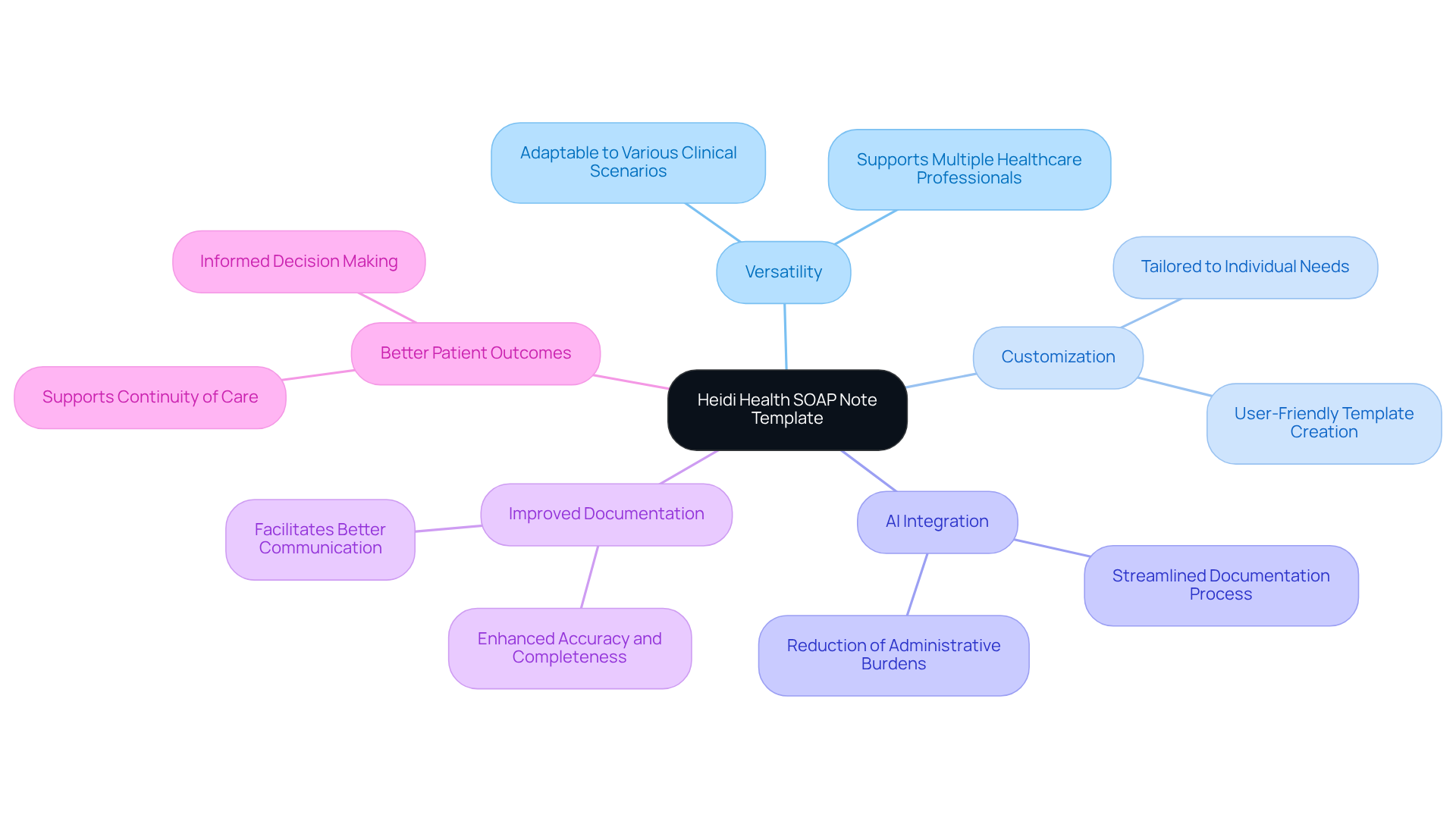
In the demanding world of healthcare, administrative burdens can weigh heavily on providers, impacting their ability to deliver compassionate care. Heidi Health provides a highly adaptable nurse practitioner soap note template, which includes a variety of examples tailored to different clinical scenarios. This invaluable resource provides a nurse practitioner soap note template that empowers nurse practitioners to document client interactions comprehensively, ensuring that all critical information is captured accurately.
Imagine being able to customize a nurse practitioner soap note template that meets your unique needs—this adaptability makes the nurse practitioner soap note template an essential tool for enhancing clinical records. By integrating innovative AI solutions like CosmaNeura's Agentic Platform, healthcare providers can effectively address these administrative challenges and improve the quality and efficiency of their record-keeping processes. Ultimately, this integration leads to .
Effective SOAP record keeping not only fosters improved communication among healthcare teams but also supports continuity of care. It underscores the importance of comprehensive and accurate record maintenance in clinical practice. Are you ready to enhance your documentation process and elevate the quality of care you provide? Let's embrace these solutions together for the benefit of our patients.
Nurse.org: Comprehensive Guide to Writing SOAP Notes
At Nurse.org, we understand the emotional challenges faced by healthcare providers when it comes to documentation. Creating a nurse practitioner soap note template, which includes Subjective, Objective, Assessment, and Plan, can feel overwhelming. However, this organized record-keeping approach is essential for guaranteeing clarity and accuracy. It allows nurse specialists to gather all relevant information efficiently, ultimately alleviating some of the administrative burdens that can impact patient care.
By following the SOAP format, practitioners can significantly enhance communication within healthcare teams, leading to improved care outcomes. Did you know that inadequate records can result in communication mistakes that jeopardize individual safety and care quality? Statistics show that organizations adopting often observe a remarkable decrease in these errors. In fact, compliance scores can enhance by as much as 30% within the initial month.
Experts stress that clear and concise clinical documentation is not merely a best practice; it is a crucial protection for both individuals receiving care and healthcare providers. By emphasizing clarity in the nurse practitioner soap note template, practitioners can enhance clinical decision-making and ensure accurate representation of individual narratives in their care plans. Yet, we must acknowledge that the SOAP format has limitations, particularly its inability to document changes over time, which is vital in many clinical situations.
As Dr. Larry Weed pointed out, the benefit of a nurse practitioner soap note template is to arrange information in a manner that is easy to locate, ensuring that all pertinent patient data is gathered for informed decision-making. Moreover, the incorporation of AI tools can further enhance record-keeping practices, streamlining workflows and improving accuracy. We encourage you to explore how these tools can support your efforts in providing the best care possible.

NP Charting School: Practical SOAP Note Examples and Tips
At NP Charting School, we understand the emotional challenges faced by nurse practitioners when it comes to record-keeping. Practical SOAP examples and essential tips incorporating a nurse practitioner soap note template are designed to ease these burdens, illustrating efficient documentation of diverse client interactions. It's crucial to capture all essential information, as common mistakes, such as neglecting to record normal vital signs, can lead to incomplete patient evaluations. How can we avoid these pitfalls?
By focusing on clarity and conciseness in your notes, you can ensure that both subjective and objective data are thoroughly documented. Statistics show that trained nurses are significantly more effective at recording, boasting a 93.9% success rate when utilizing structured reporting forms. In Ethiopia, the frequency of nursing record-keeping methods is estimated at 50.01%, highlighting the urgent need for improved record quality.
What methods can ? Utilizing a nurse practitioner soap note template has been shown to improve both quality and compliance with legal requirements. Remember, records are often referred to as the 'tip of the iceberg of care issues,' emphasizing their vital significance. By implementing these approaches, you can enhance your record-keeping abilities, ultimately leading to improved care outcomes for your patients.
Key Solutions:
- Focus on clarity and conciseness in documentation.
- Utilize structured reporting forms.
- Adopt standardized formats for record-keeping.
By embracing these strategies, you can make a meaningful difference in your practice and the lives of those you care for.

Nursing Process: Real-World Nurse Practitioner SOAP Note Examples
The Nursing Process highlights the importance of practical nurse provider SOAP note templates, specifically the nurse practitioner soap note template, which demonstrate efficient recording across various clinical situations. These examples serve as a valuable resource for professionals, showing how to accurately and efficiently capture patient information. Have you ever felt overwhelmed by the need to document effectively? By reviewing these records, nurse practitioners can utilize a nurse practitioner soap note template to organize their written accounts in a way that meets both clinical and legal standards, ultimately easing some of that burden.
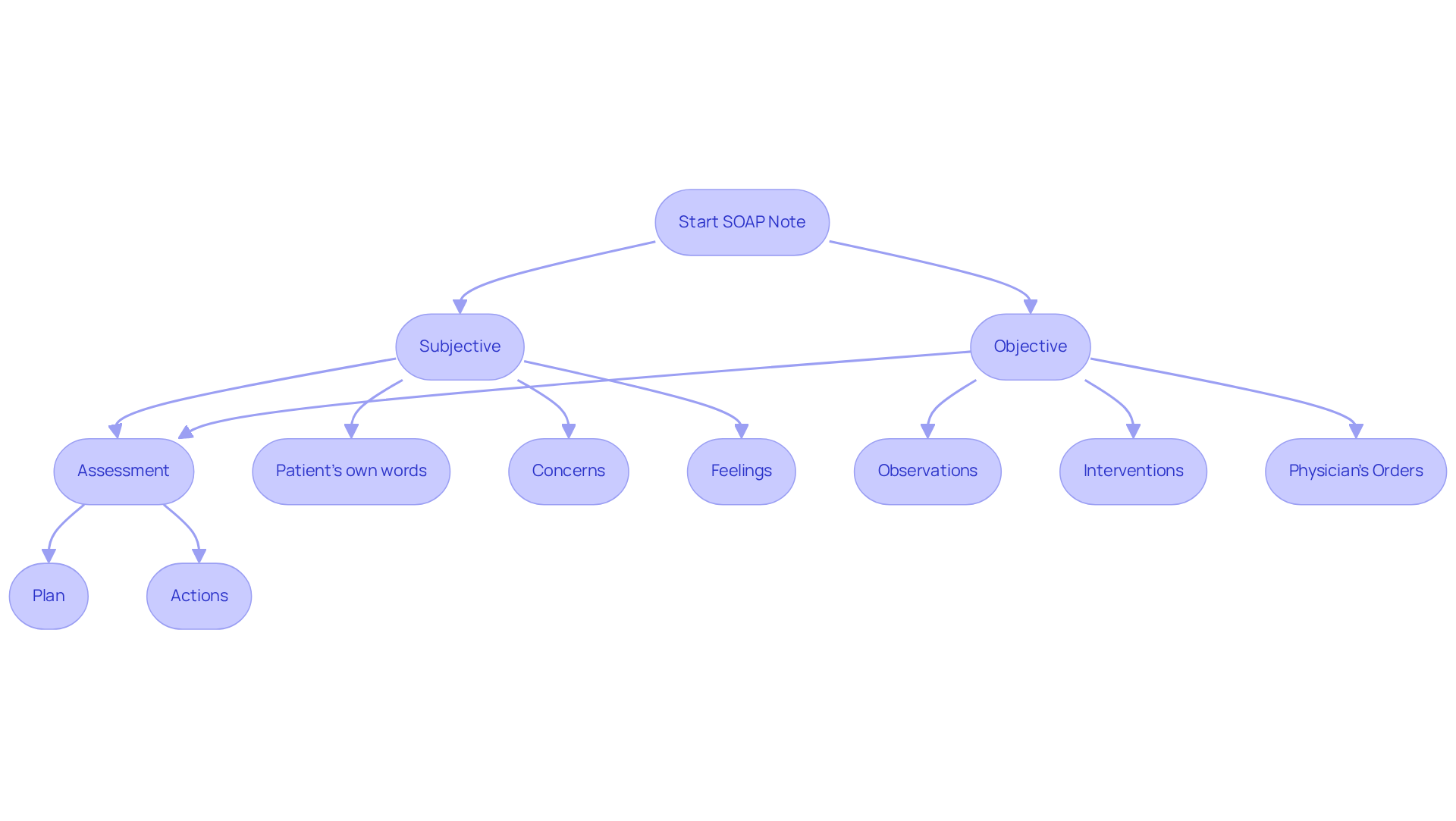
Accurate documentation is not just a routine task; it's crucial for legal compliance in healthcare. Statistics indicate that incomplete or inaccurate details in SOAP records can lead to improper treatment and potential liability concerns. Therefore, it’s essential to include all necessary components:
- date
- time
- physician’s orders
- observations
- interventions
- responses from the individual
By ensuring these elements are present, we take a significant step toward safeguarding both our patients and ourselves.
Expert insights remind us that the nurse practitioner soap note template aids in clinical reasoning and serves as a legal safeguard. Well-organized nurse practitioner soap note templates not only improve communication among healthcare professionals but also guarantee , which is vital for patient safety. Moreover, capturing individual information precisely within the Subjective section while recording objective findings in the Objective section enhances the legal defensibility of our records. This careful attention to detail can make a world of difference.
Ultimately, the impact of accurate documentation on legal compliance cannot be overstated. By adopting best practices in SOAP documentation with a nurse practitioner soap note template, nurses can significantly decrease the likelihood of legal issues while enhancing the quality of care for individuals. Let’s commit to these standards together, ensuring we provide the best possible care while navigating the complexities of our responsibilities.
SoapNoteAI: Step-by-Step Guide for Writing SOAP Notes
Creating a nurse practitioner soap note template can feel overwhelming, especially for nursing professionals who are new to this documentation format. SoapNoteAI provides a thorough step-by-step guide, breaking down each element into manageable sections. This organized approach not only alleviates the stress of documentation but also offers clear guidance for effective patient encounter records. By following this method, practitioners can produce detailed and compliant notes that enhance communication and continuity of care.
The consists of four key components: Subjective, Objective, Assessment, and Plan. Each section serves a distinct purpose in documenting patient interactions:
- Subjective: This section captures the patient's personal experiences, feelings, and history, including the chief complaint and any relevant symptoms. How often do we wish to understand our patients better?
- Objective: Here, measurable data such as vital signs, physical examination findings, and laboratory results are documented, providing a factual basis for clinical decisions. Isn’t it reassuring to have concrete data to guide our actions?
- Assessment: This combines information from the Subjective and Objective sections to formulate a clinical judgment about the individual's condition. It’s a critical step that connects the dots in patient care.
- Plan: Finally, this outlines the next steps in care, including treatment options, follow-up appointments, and education for individuals. How can we ensure our patients feel supported in their journey?
Organized records are essential in nursing, as they not only enhance effective communication among healthcare providers but also ensure that care is based on precise and thorough information. Research shows that nurse practitioners who utilize the nurse practitioner soap note template report enhanced efficiency and better outcomes for those in their care. Furthermore, the APSO order has been shown to enhance speed, task success, and usability during chronic disease visits. By adopting these optimal methods, healthcare practitioners can significantly improve their record-keeping abilities, ultimately resulting in superior care for individuals. As Vivek Podder wisely notes, "SOAP records are a crucial element of information regarding the health condition of the individual as well as a communication document among healthcare professionals." Embracing this structured approach is a step toward nurturing better patient outcomes.
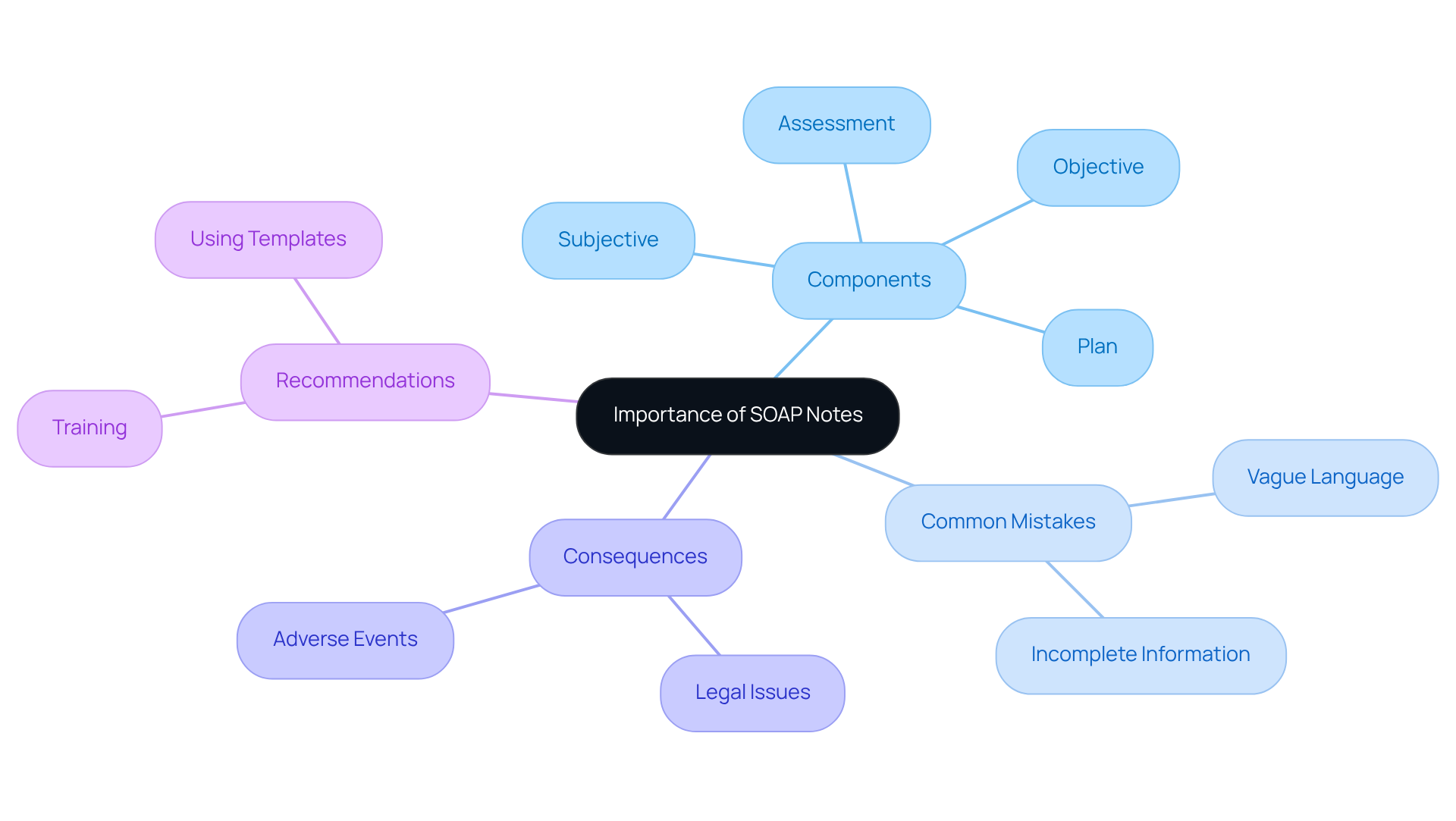
Studying Nurse: Importance of SOAP Notes and Common Mistakes to Avoid
SOAP records serve as a foundation of clinical documentation, acting as vital communication tools that ensure continuity of care among healthcare providers. They consist of four essential components: Subjective, Objective, Assessment, and Plan. Together, these elements empower practitioners to evaluate, diagnose, and treat individuals effectively. Yet, it’s important to acknowledge that frequent can significantly impact client care.
One common challenge is the use of vague language, which can lead to misinterpretations and hinder clinical decision-making. Have you ever encountered a situation where ambiguous terms obscured the severity of a patient's condition? Such instances can complicate treatment plans. To address this, practitioners should strive for clarity and specificity in their notes, ensuring every detail is accurately captured.
Incomplete information represents another critical mistake often arising from time constraints or administrative burdens. Research indicates that administrative duties consume about 16% of a doctor's working hours, frequently resulting in hurried record-keeping. This can lead to missing vital details, such as changes in a patient's health status, which are crucial for ongoing care. Implementing organized record-keeping guidelines and utilizing AI scribe tools—capable of reducing recording time by up to 95%—can help alleviate these challenges, allowing for more comprehensive and prompt updates.
Real-world instances illustrate the repercussions of inadequate record-keeping. For example, a case study revealed that failing to document client consent led to legal consequences for a physical therapist. This underscores the necessity of obtaining and recording consent before treatment. Moreover, a lack of timely updates on individual status has been linked to 80% of adverse events in healthcare, highlighting the importance of precise and prompt record-keeping.
To enhance the quality of records using the nurse practitioner soap note template, professionals should consistently train on recording standards and adopt tools that simplify the process. By avoiding common mistakes and focusing on accurate, thorough records with the use of a nurse practitioner soap note template, nurse professionals can significantly improve patient outcomes and ensure a higher standard of care.
Consider exploring training opportunities and technologies that can support you in this vital aspect of healthcare. Your commitment to improving documentation not only benefits your practice but also profoundly impacts the lives of those you care for.
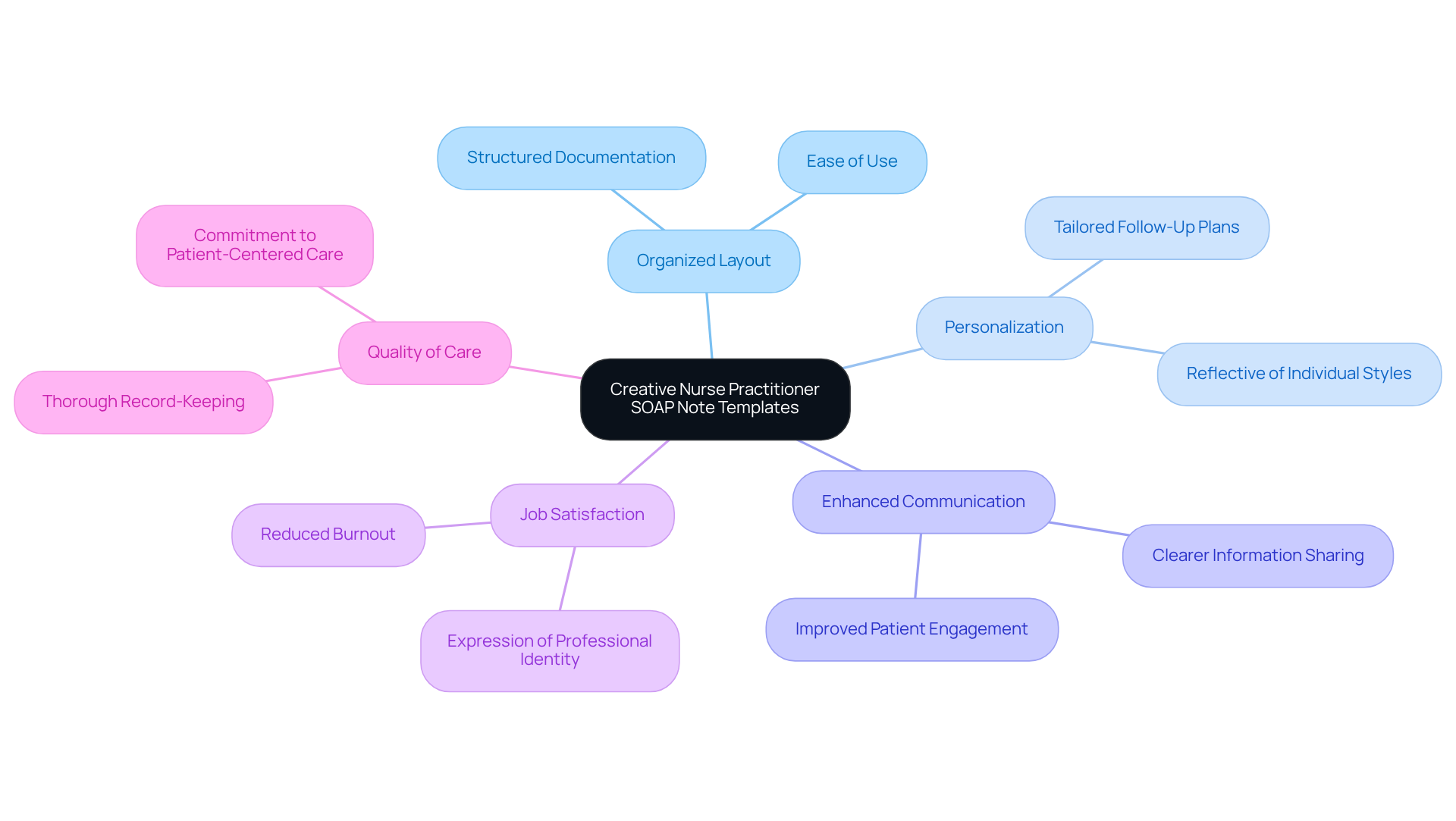
Pinterest: Creative Nurse Practitioner SOAP Note Templates
Innovative designs for the nurse practitioner soap note template found on sites like Pinterest can significantly ease the recording process. These not only provide an organized layout for records but also encourage personalization, making the documentation more engaging and reflective of individual styles. Have you considered how unique elements in your SOAP notes could enhance client engagement and satisfaction? Customized nurse practitioner soap note templates can include specific preferences or tailored follow-up plans, which not only improve communication but also demonstrate a commitment to patient-centered care.
Experts emphasize that innovation in clinical records can lead to greater job satisfaction among professionals. It allows them to express their professional identity while ensuring thorough and accurate record-keeping. By using a nurse practitioner soap note template, you can simplify the record-keeping process and improve the overall quality of care provided to your patients. Imagine the positive impact this could have on your daily practice and your patients' experiences.
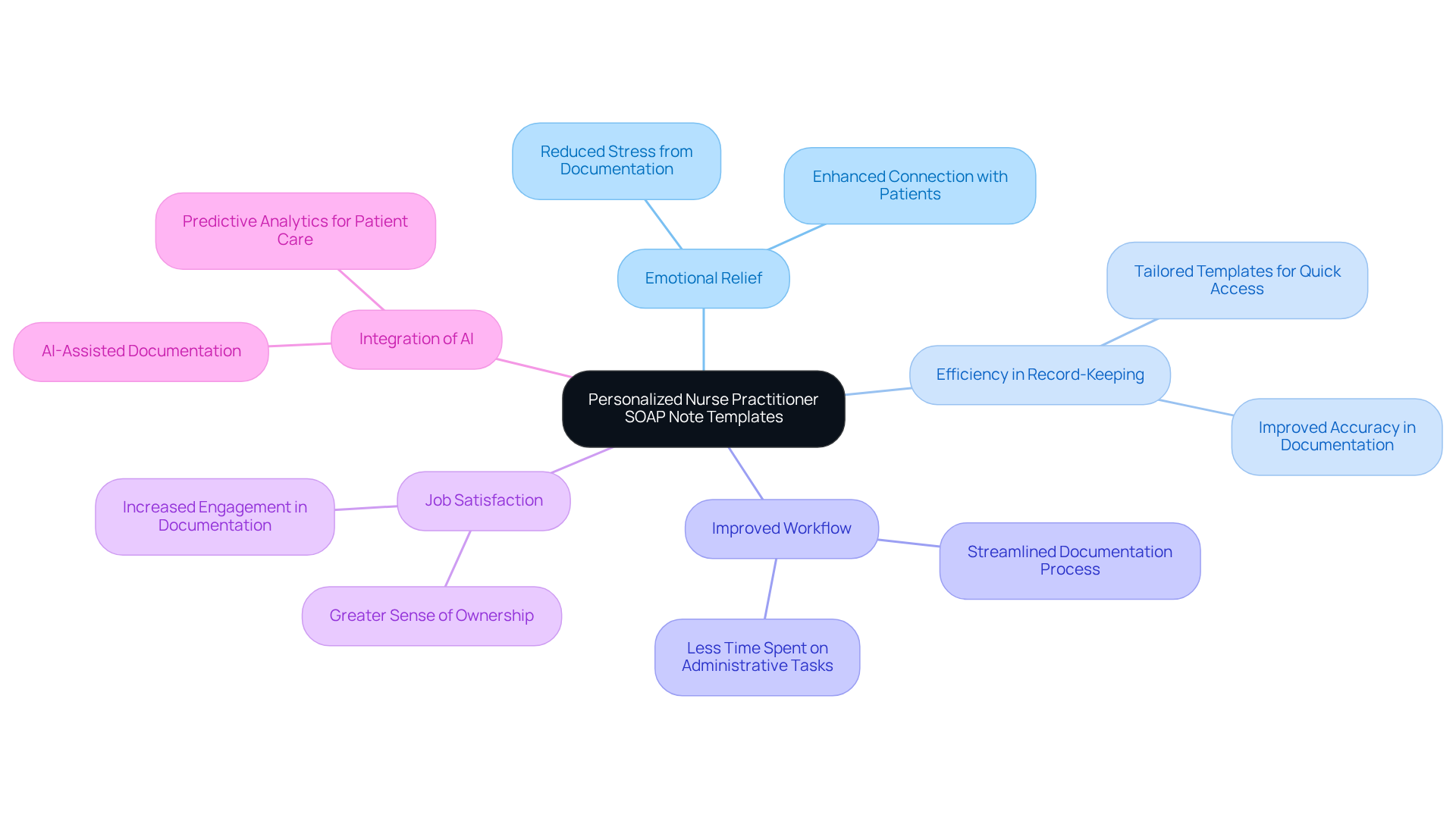
Etsy: Personalized Nurse Practitioner SOAP Note Templates
Healthcare providers often face emotional challenges that can weigh heavily on their daily practice. The administrative burdens they encounter can detract from the quality of patient care they strive to deliver. Customized nurse practitioner SOAP note templates available on platforms like Etsy provide a thoughtful solution to this concern. These templates allow professionals to tailor their records to their unique preferences and styles, transforming a typically monotonous task into a more engaging experience.
By utilizing the nurse practitioner SOAP note template, nurse professionals not only improve their record-keeping efficiency but also ensure that all vital information is accurately captured. This approach aligns with the growing recognition among healthcare providers that can lead to improved workflow and job satisfaction. Have you ever felt overwhelmed by the paperwork? Real-world examples illustrate that those who embrace customized templates report a smoother record-keeping process, ultimately allowing them to focus more on the care of their patients.
The integration of generative AI with these customized templates fosters a sense of ownership and connection to the documentation process. This addresses the administrative burdens that often detract from patient care, which is crucial for delivering high-quality healthcare. Imagine a work environment where you can seamlessly document while feeling more connected to your patients. By taking this step, you can reclaim valuable time and energy, enhancing both your professional satisfaction and the care you provide.
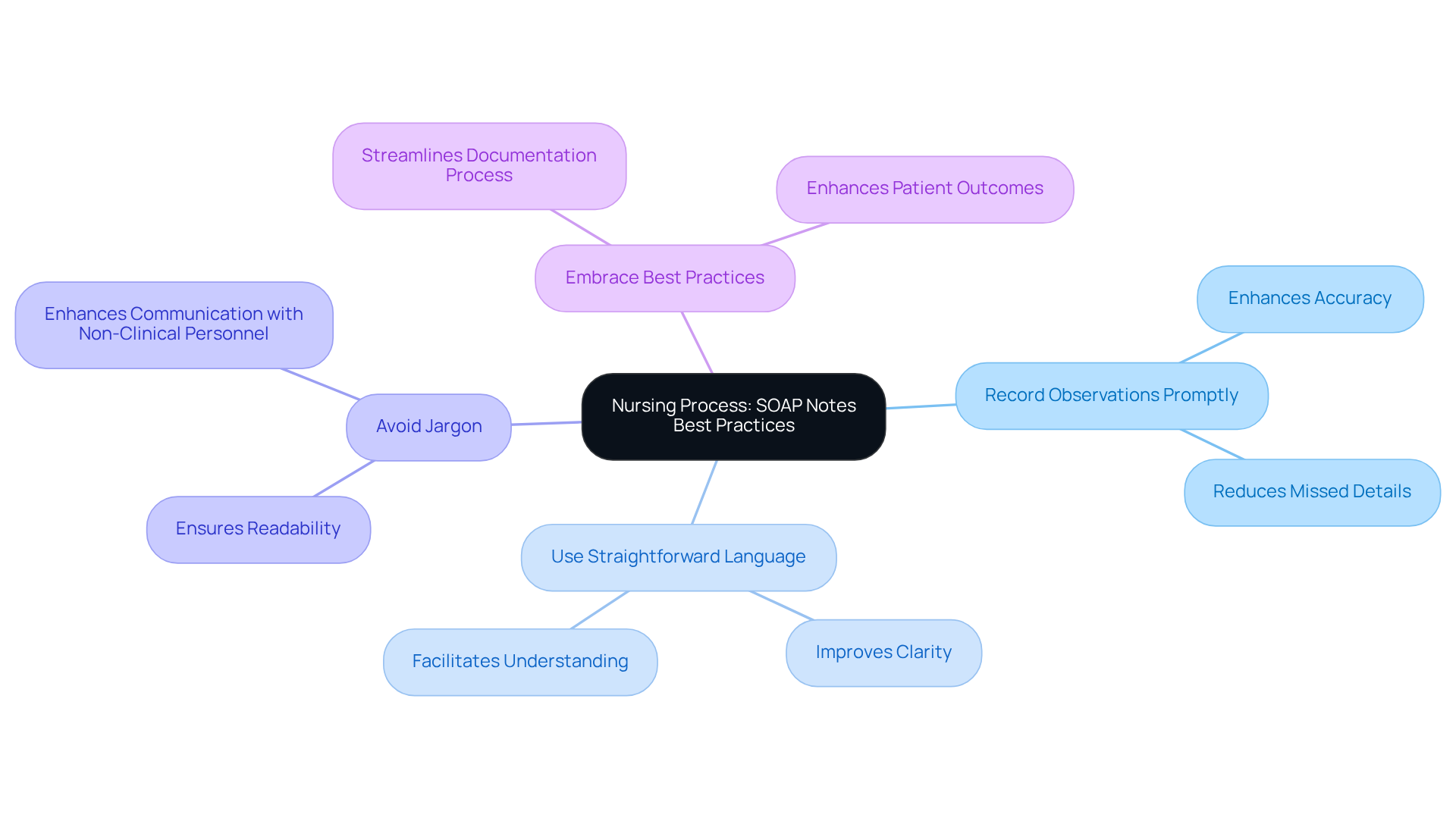
Nursing Process: Best Practices for Writing SOAP Notes
The Nursing Process highlights the best practices for composing a nurse practitioner SOAP note template, emphasizing the importance of clarity, conciseness, and accuracy in documentation.
Have you ever felt overwhelmed by the need to document effectively? Essential suggestions include:
- Recording observations promptly after client interactions
- Using straightforward language
Avoiding jargon can make a significant difference in communication. By embracing these best practices, nurse practitioners can utilize the nurse practitioner SOAP note template to [transform their SOAP notes into powerful tools for communication](https://ehsinsight.com/blog/best-practices-for-writing-medical-soap-notes) and continuity of care. This not only streamlines their work but ultimately , fostering a nurturing environment for those they serve.
Conclusion
The exploration of nurse practitioner SOAP note templates highlights their vital role in enhancing documentation efficiency and patient care. Are you feeling overwhelmed by administrative tasks? Integrating innovative tools and best practices, such as AI-powered solutions and customizable formats, can significantly streamline your record-keeping processes. This not only alleviates your burdens but also ensures that essential patient information is accurately captured and readily accessible.
Throughout this article, we have discussed various templates and resources, emphasizing the importance of clarity, organization, and adaptability in SOAP note documentation. From AI-driven templates like CosmaNeura to versatile examples from Heidi Health, each solution offers unique features that empower you as a nurse practitioner to improve your documentation practices. By understanding common mistakes and employing best practices, you can enhance the quality of your SOAP notes, ultimately leading to better patient outcomes and more effective communication among healthcare teams.
The significance of adopting these efficient documentation strategies cannot be overstated. Investing time in mastering SOAP note templates and recognizing their benefits will not only improve your individual practice but also contribute to a higher standard of care in our healthcare system. Embrace these tools and insights to transform the way you approach documentation, ensuring that patient care remains at the forefront of nursing practice. Together, we can make a difference.




