Overview
The article "10 Essential SOAP Report Examples for Healthcare Providers" recognizes the emotional challenges that healthcare providers encounter daily. It highlights the stress and pressure that come from administrative burdens, which can significantly impact patient care. By providing effective examples and best practices for creating SOAP (Subjective, Objective, Assessment, Plan) notes, this article aims to offer solutions that can alleviate some of these pressures.
Structured documentation is not just a requirement; it is a vital tool that enhances clinical efficiency and compliance. The article details how various platforms and templates can streamline the documentation process, reduce errors, and ultimately improve patient care outcomes. Imagine how much more focused you could be on your patients if the documentation process was simplified.
By embracing these best practices, healthcare providers can experience a more manageable workflow, allowing them to dedicate more time to patient interactions. The benefits of structured documentation extend beyond efficiency; they foster a better environment for both providers and patients. We encourage you to explore these examples and consider how they might fit into your practice, leading to improved outcomes for those you care for.
Introduction
In the fast-paced world of healthcare, the emotional and administrative challenges faced by providers can feel overwhelming. The importance of effective documentation is crucial, yet often overlooked.
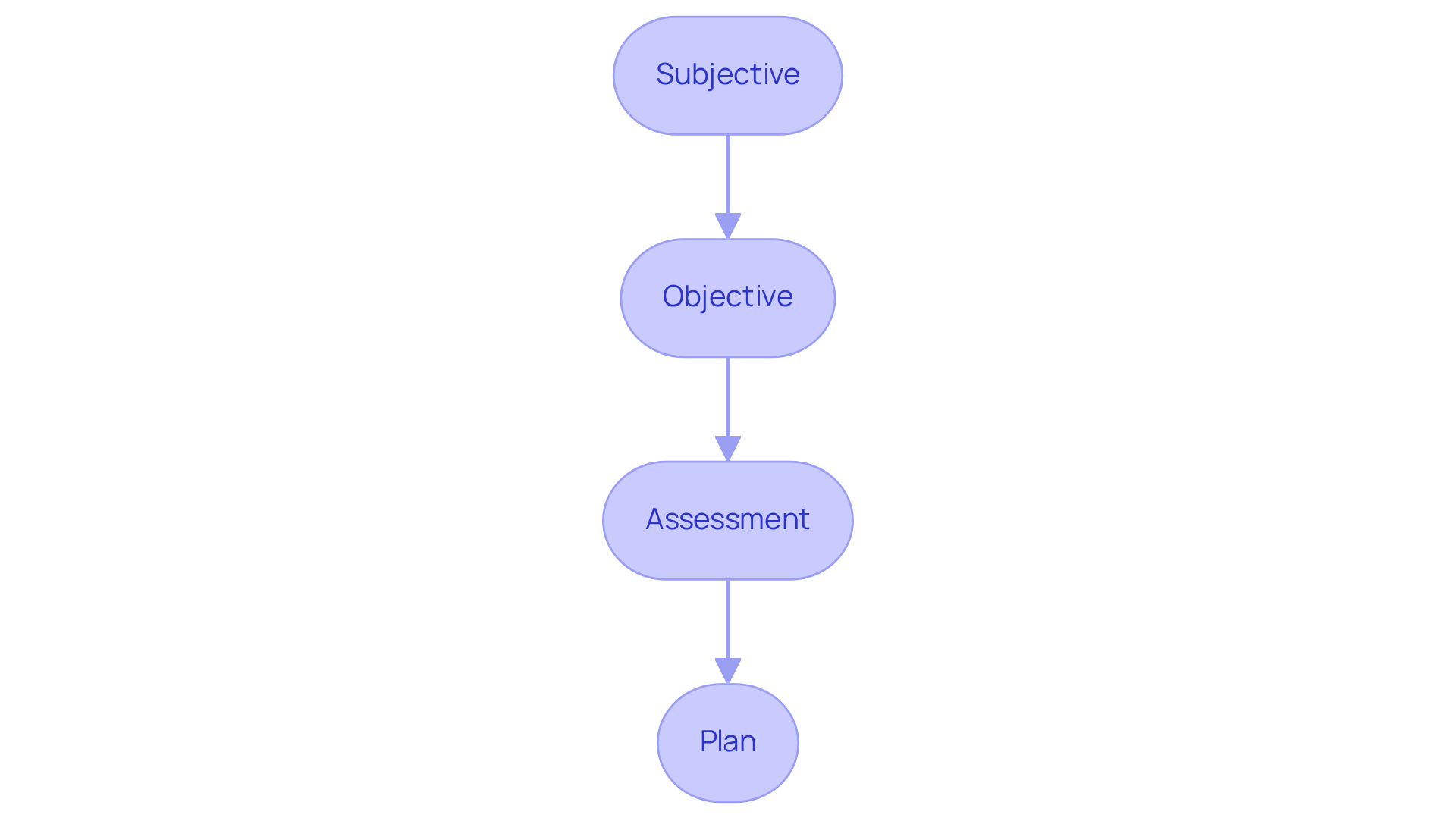
SOAP notes, a structured method for recording patient information, serve as essential tools for providers striving to enhance care while navigating these demands. This article explores ten compelling examples of SOAP reports that not only streamline documentation but also foster improved patient outcomes and compliance.
How might these examples transform the way healthcare professionals approach clinical records? What best practices can be adopted to ensure clarity and efficiency in this vital aspect of care? Let’s delve into these questions together.
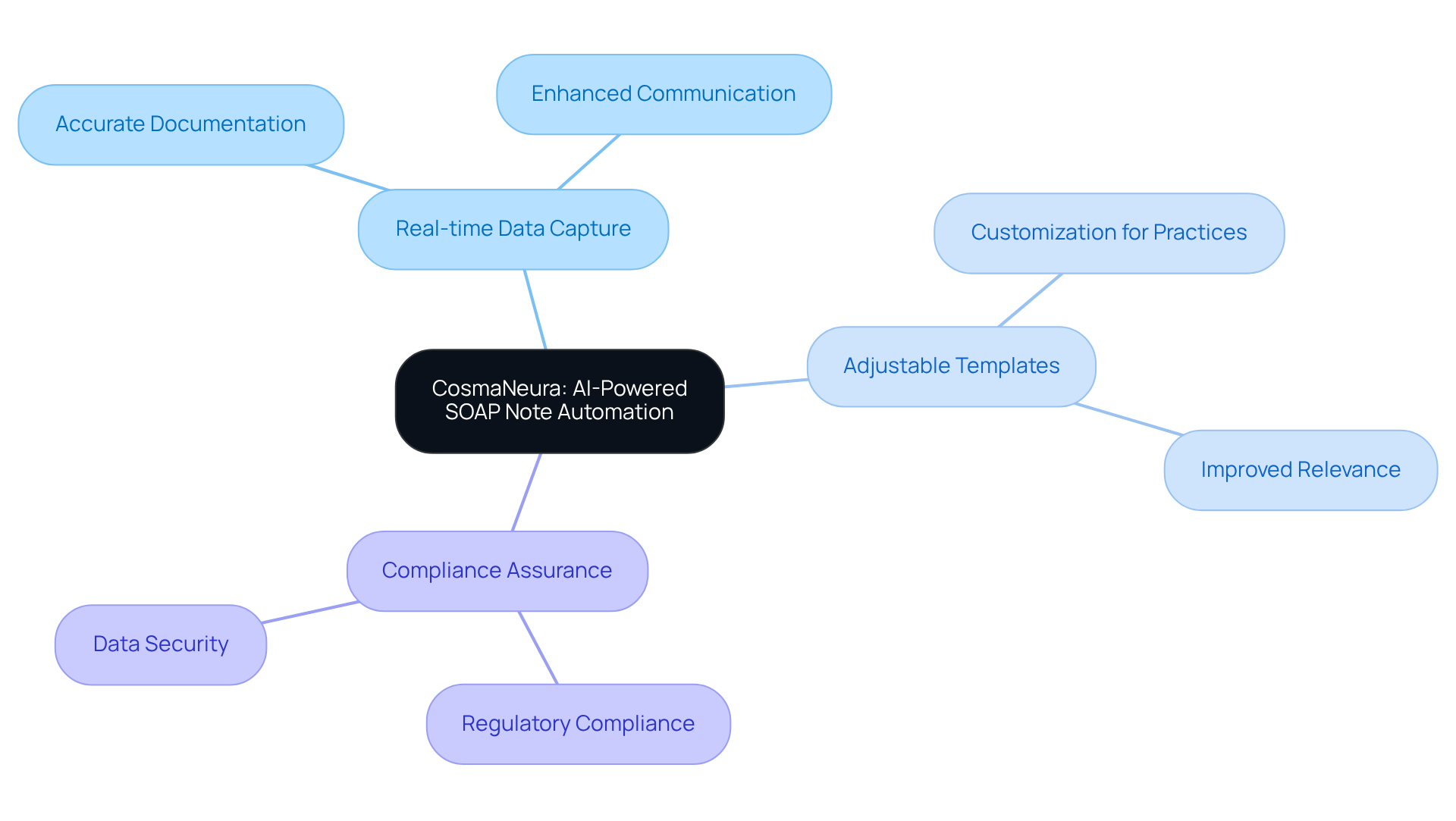
CosmaNeura: AI-Powered SOAP Note Automation for Healthcare Providers
CosmaNeura understands the challenges healthcare professionals face in managing clinical documentation. Its sophisticated AI-driven platform allows providers to focus more on patient care rather than getting bogged down by administrative tasks. Imagine the relief of knowing that a soap report example is generated quickly and accurately, following a structured format that enhances clinical records. This automation not only streamlines the process but also significantly reduces the potential for errors, ultimately improving outcomes and satisfaction.
- Real-time Data Capture: Automatically records patient interactions during consultations, ensuring accurate documentation and enhancing communication among providers. How much easier would your day be if documentation was seamless?
- Adjustable Templates: Enables providers to customize documentation to their specific practice needs, improving relevance and functionality. Tailoring your documentation can make a world of difference.
- Compliance Assurance: Ensures that all records align with regulatory standards, including HIPAA adherence, protecting individual information while tackling the difficulties of disjointed systems. You can feel confident knowing your documentation is secure and compliant.
By embracing CosmaNeura, healthcare professionals can reclaim valuable time, allowing them to nurture their patients with the care and attention they deserve. Let's transform the way we approach clinical documentation together.
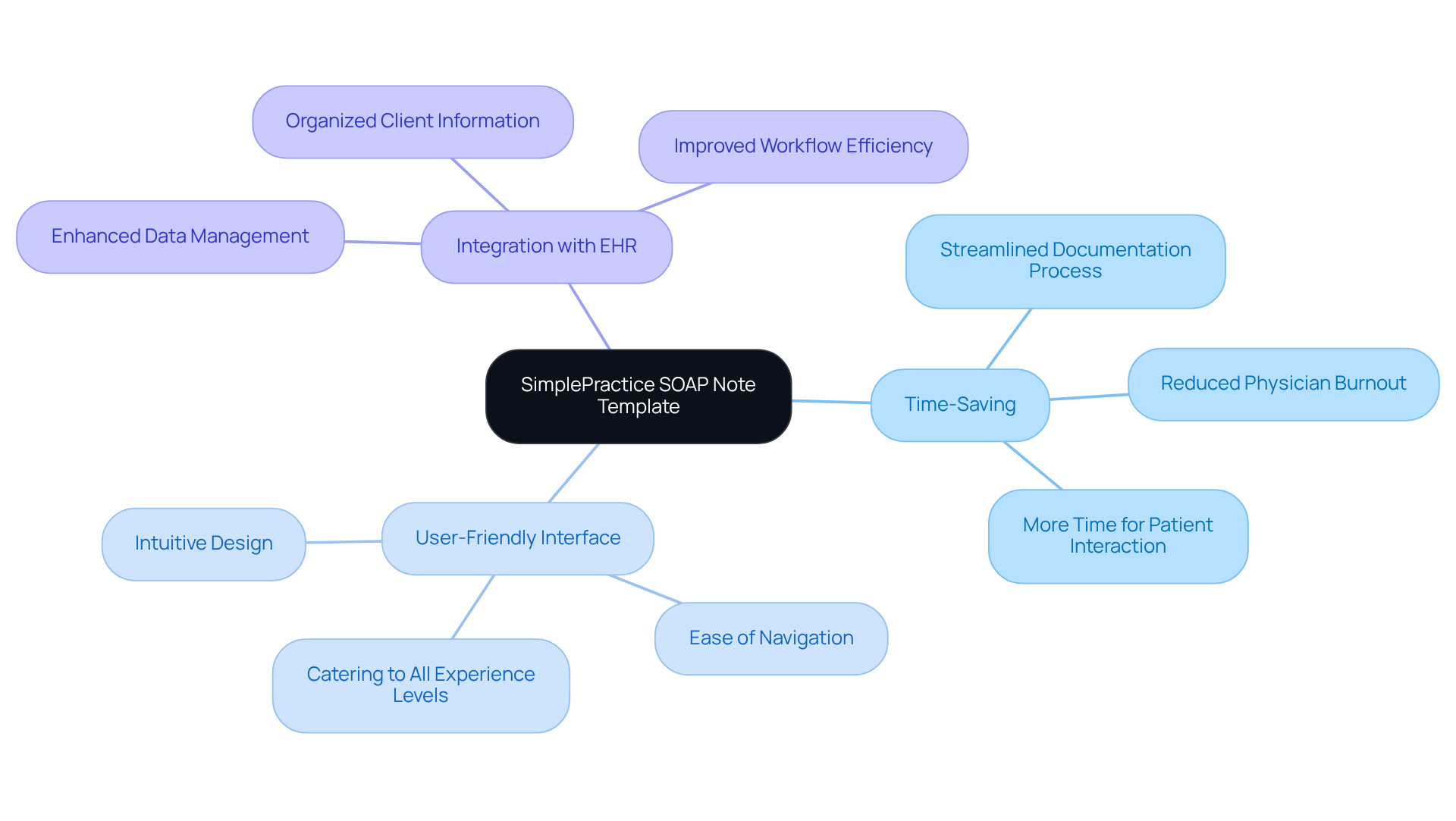
SimplePractice: Comprehensive SOAP Note Template for Efficient Documentation
Healthcare professionals often face overwhelming administrative burdens that can detract from their ability to provide compassionate care. SimplePractice offers a robust note template designed to alleviate these challenges, significantly improving record-keeping efficiency. By enabling clinicians to record client encounters seamlessly through structured fields tailored to the soap report example format, this platform ensures that documentation is both relevant and user-friendly.
- Time-Saving: Imagine a world where the documentation process is streamlined. SimplePractice allows clinicians to spend less time on paperwork and more time interacting with clients. This shift is crucial in combating physician burnout, as it lightens the administrative load that often weighs heavily on healthcare providers.
- User-Friendly Interface: The intuitive design of SimplePractice makes navigation effortless, catering to users of all experience levels. In a high-pressure environment, this ease of use is essential for maintaining efficiency and focus on patient care.
- Integration with EHR: SimplePractice integrates seamlessly with electronic health records, enhancing data management and ensuring that client information is organized and readily accessible. This integration not only boosts workflow efficiency but also supports better patient care, allowing physicians to prioritize their patients over administrative tasks.
An organized approach to clinical records is essential as a soap report example, enhancing the quality of documentation while also helping to meet insurance standards. Clear and concise entries are vital for claims processing, serving as written evidence for insurance claims. As healthcare providers increasingly prioritize efficiency and accuracy in their documentation practices, it's important to remember the advice of Gaines: "Be thorough but not wordy. Stick to the basics and give important information." Moreover, the objective aspects of clinical documentation should include quantifiable data, such as heart rate and weight, reinforcing the importance of organized records. Ensuring that documentation is clear, signed, and dated is essential for compliance with insurance regulations.
By embracing tools like SimplePractice, healthcare providers can reclaim their time and focus on what truly matters—their patients. Are you ready to transform your documentation process and enhance your patient care?
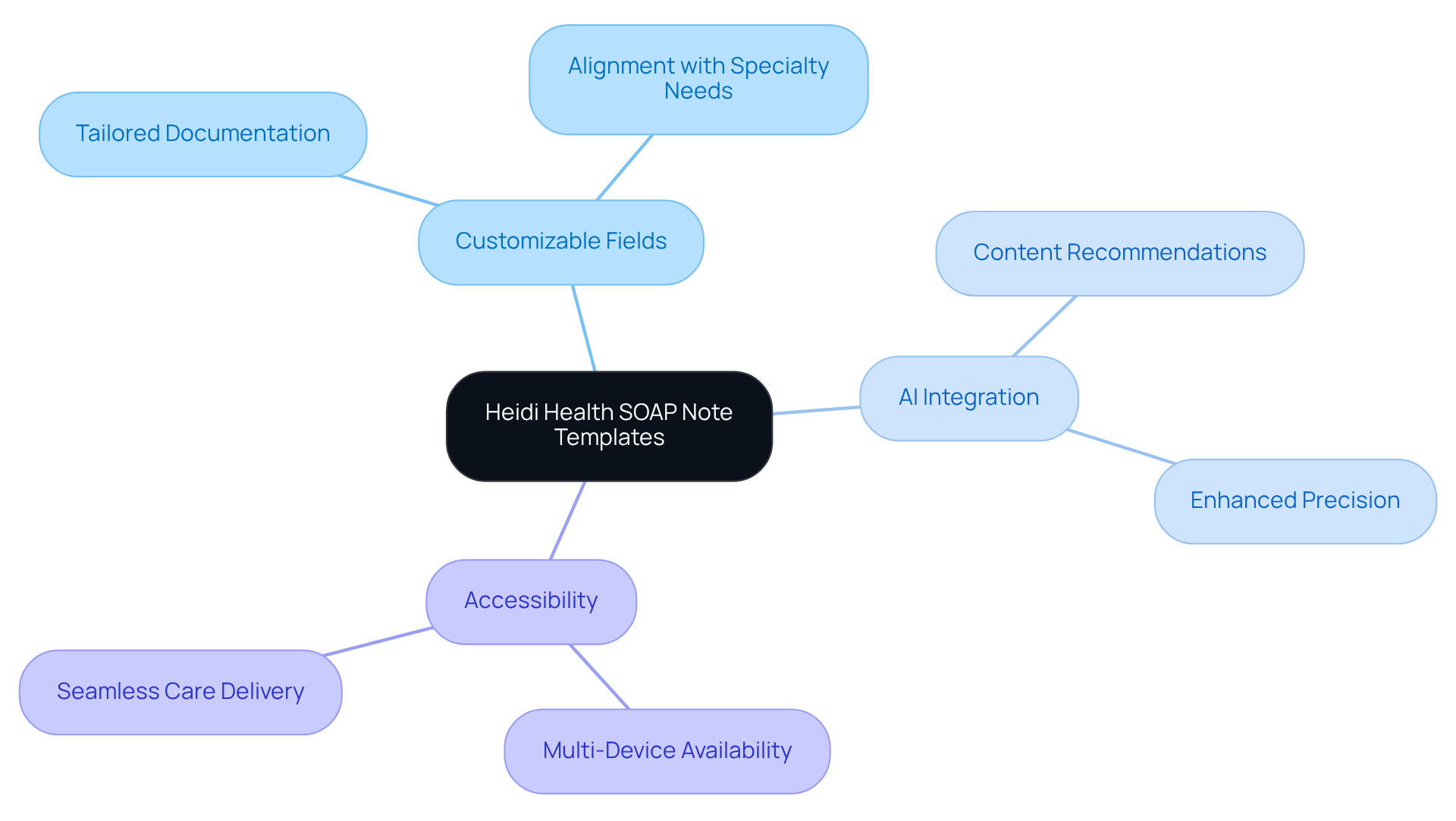
Heidi Health: Tailored SOAP Note Templates for Diverse Healthcare Practices
Heidi Health understands the emotional challenges healthcare providers face in their demanding roles. With customizable SOAP report examples designed to meet the diverse needs of providers—from primary care to specialized fields—these SOAP report examples are here to alleviate some of that burden. They are carefully crafted to ensure that all relevant information is precisely recorded, which ultimately improves the quality of care.
- Customizable Fields: Have you ever felt overwhelmed by the need for tailored documentation? Our templates, which serve as a soap report example, allow providers to easily add or modify sections to align with their specific practice requirements, ensuring that records reflect the unique aspects of their specialty.
- AI Integration: Imagine having AI technology at your fingertips! These templates recommend pertinent content based on user interactions, greatly enhancing both precision and effectiveness in record-keeping.
- Accessibility: In today’s fast-paced environment, accessibility is key. Our templates are available across various devices, enabling healthcare providers to document patient encounters anytime and anywhere, thus facilitating seamless care delivery.
As we look ahead to 2025, the incorporation of AI in generating customized clinical summaries is becoming increasingly common. A significant number of healthcare organizations are embracing such technologies to enhance their record-keeping processes. This shift not only boosts the efficiency of clinical workflows but also supports providers in delivering high-quality care. Industry leaders emphasize the importance of personalization in clinical records, acknowledging that tailored solutions are crucial for addressing the specific requirements of various healthcare environments. Together, we can navigate these challenges and enhance the care we provide.
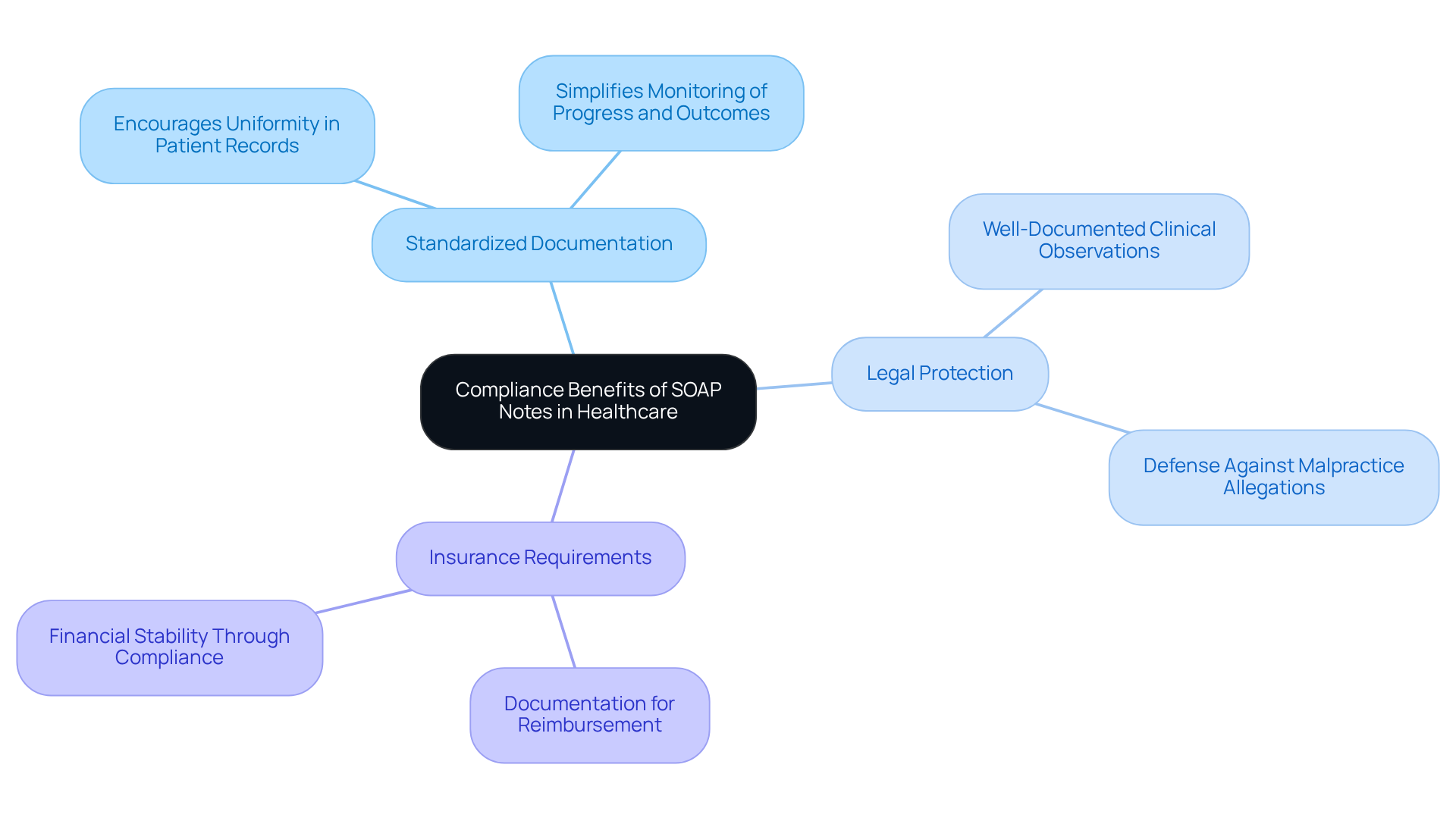
Headway: Compliance Benefits of Using SOAP Notes in Healthcare
Headway recognizes the emotional challenges healthcare providers face and emphasizes the compliance benefits of employing structured notes in their environments. By following an organized format, providers can ensure their documentation aligns with legal and regulatory standards, which is crucial for safeguarding both clients and practitioners.
- Standardized Documentation: Have you considered how a structured format can encourage uniformity in patient records? This consistency simplifies the monitoring of progress and outcomes?
- Legal Protection: Imagine the peace of mind that comes from knowing well-documented clinical observations serve as legal records, providing security for practitioners in case of disagreements or claims.
- Insurance Requirements: Many insurance providers require documentation for reimbursement. Adhering to these standards is vital for your financial stability.
As we look ahead to 2025, the legal advantages of standardized documentation are increasingly recognized. Not only do they enhance communication among healthcare professionals, but they also serve as a robust defense in legal matters. By maintaining adequate records through structured summaries, such as a soap report example, you can significantly reduce risks associated with malpractice allegations. This underscores the importance of diligent record-keeping in medical practice, ensuring that you can focus on what truly matters—providing compassionate care to your patients.
NCBI: Clinical Significance and Best Practices for SOAP Notes
As stated by NCBI, such documentation serves an essential function in clinical records by offering a systematic method for logging individual information. Optimal methods for composing a soap report example involve being succinct, employing straightforward language, and ensuring that all pertinent information is incorporated.
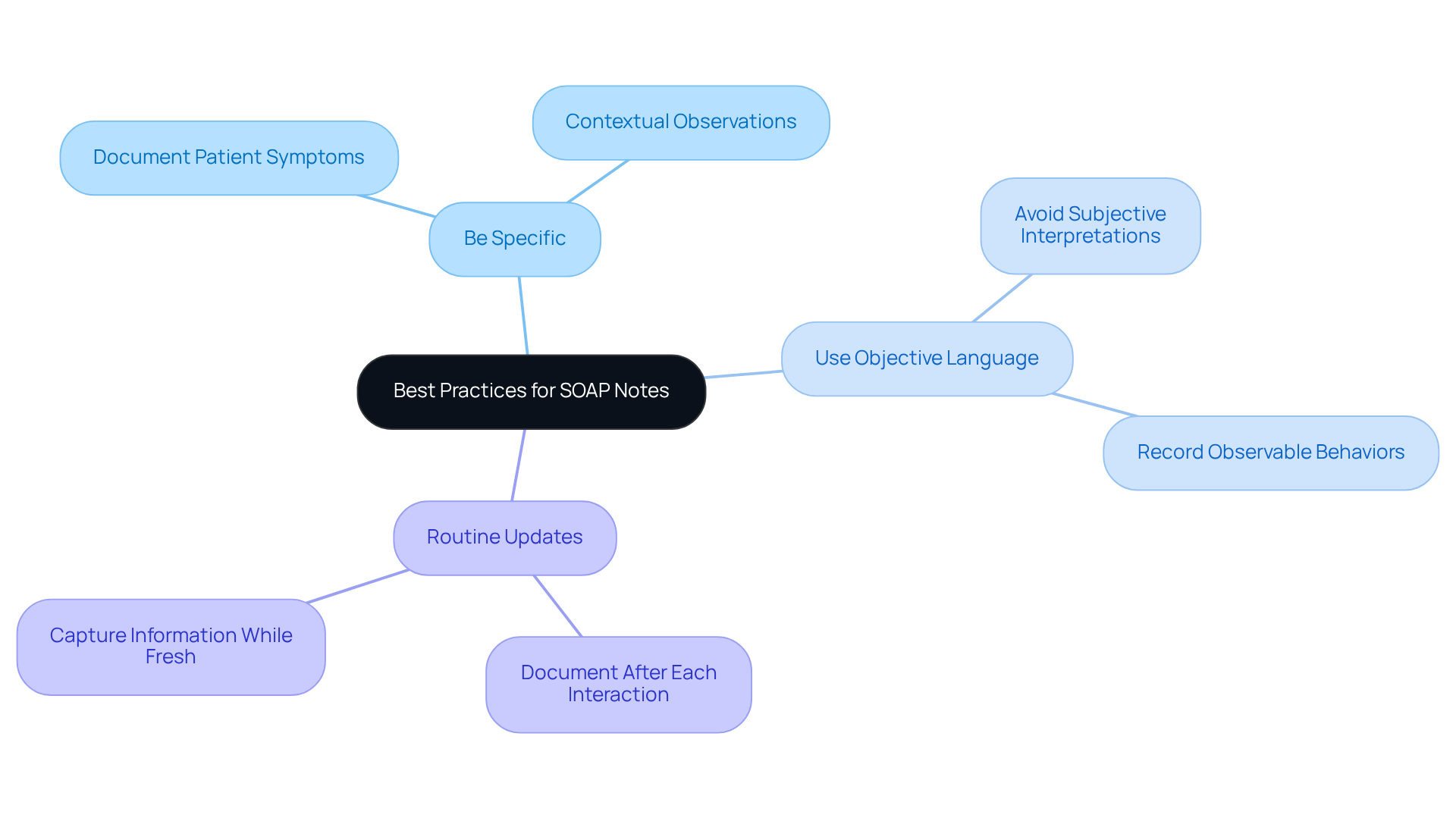
Best Practices:
- Be Specific: Clearly document patient symptoms and observations to provide a comprehensive view of their condition. For instance, when an individual expresses feeling 'hopeless' and lacking motivation, it is crucial to observe the duration and context of these emotions, along with any relevant triggers.
- Use Objective Language: To maintain professionalism and accuracy, avoid subjective interpretations. Instead of indicating a client 'seems anxious,' record observable behaviors, such as fidgeting or difficulty maintaining eye contact.
- Routine Updates: Ensure that documentation is refreshed promptly after every client interaction. Documenting session summaries right after a meeting aids in capturing pertinent information while it is recent, reducing the chance of overlooking essential details and enabling precise monitoring of the patient's progress over time.
Incorporating these best practices, as shown in the soap report example, not only enhances the quality of documentation but also supports clinical decision-making and optimizes workflows in healthcare settings. Remember, your attention to detail can significantly impact patient care and outcomes.
Psylio: SOAP Note Examples for Mental Health Counseling
Psylio understands the emotional challenges that mental health professionals encounter and offers specific soap report examples tailored for mental health counseling. These examples are designed to assist clinicians in effectively recording their interactions with individuals, all while being sensitive to their emotional states.
- Subjective: Patients often express feelings of anxiety and difficulty sleeping, reflecting their internal struggles.
- Objective: Clinicians may observe a tense demeanor and avoidance of eye contact, which can indicate deeper emotional issues.
- Assessment: It is possible that patients are experiencing heightened anxiety due to recent life changes, which deserves careful consideration.
- Plan: Continuing therapy sessions and introducing relaxation techniques can be beneficial steps in supporting patient well-being.
By utilizing the soap report example, mental health professionals can enhance their documentation practices, ultimately leading to improved patient care and understanding.
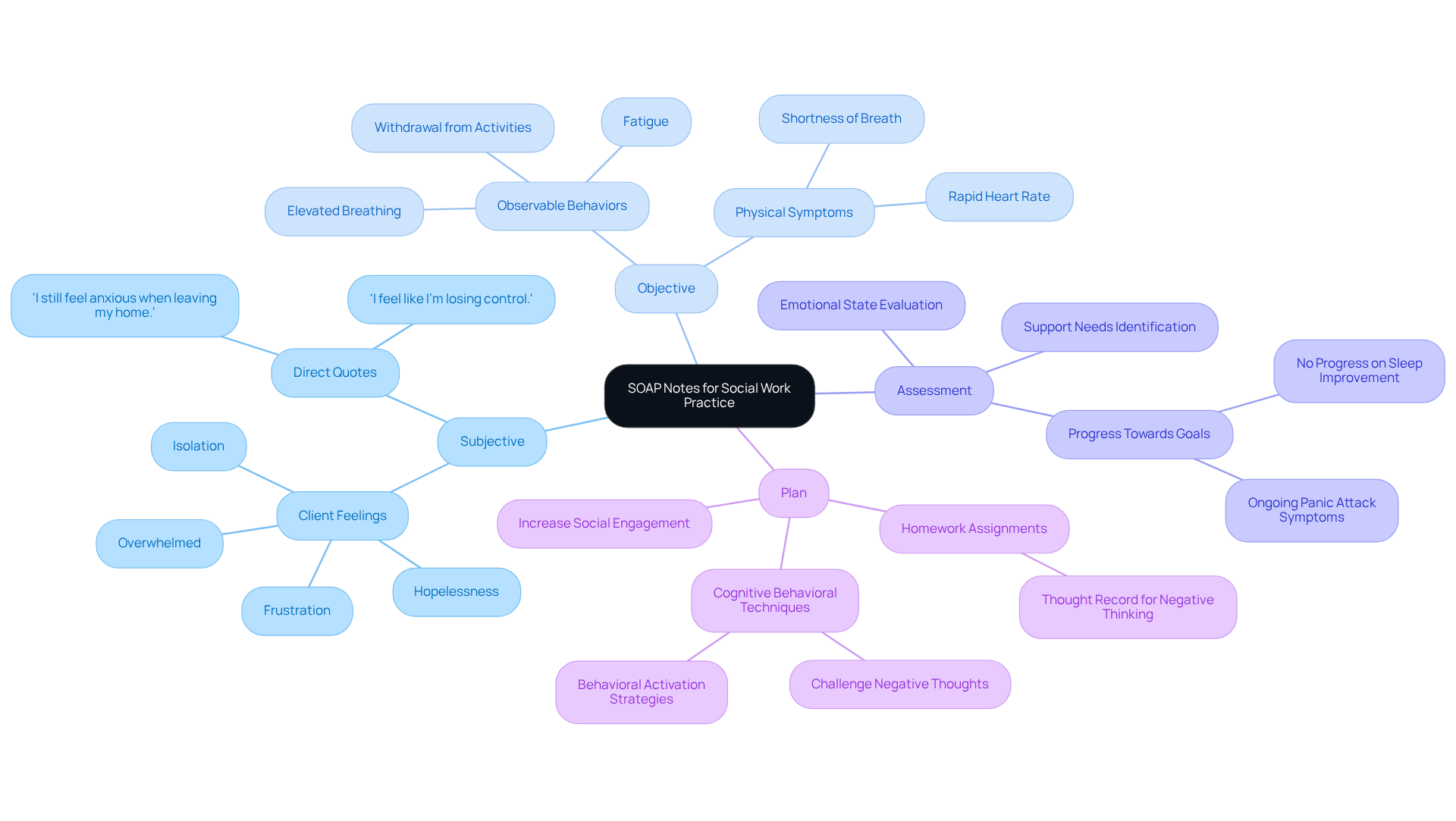
Social Work Portal: Writing SOAP Notes for Social Work Practice
The Social Work Portal offers compassionate guidance on creating a soap report example that is structured and tailored for social work practice. These records serve as a soap report example, which is vital for capturing client interactions and ensuring that all relevant information is documented for effective case management.
- Subjective: Clients may express feelings of isolation and frustration, highlighting their emotional challenges.
- Objective: It’s important to document observable behaviors, such as withdrawal from social activities, to create a complete picture.
- Assessment: Evaluate the client's emotional state and identify potential support needs, fostering a deeper understanding of their situation.
- Plan: Develop a thoughtful plan aimed at increasing social engagement and providing necessary support services.
Structured assessment and plan records, as a soap report example, are invaluable for thorough documentation during therapy sessions, illustrating medical necessity for insurance purposes. The adaptability of documentation in group therapy settings enhances its effectiveness for social workers. By utilizing templates, professionals can achieve greater consistency and efficiency in record-keeping, allowing them to devote more time to client care rather than administrative tasks. By mastering this structured framework, social workers can ensure their records are effective, legally sound, and ultimately contribute to improved client outcomes.
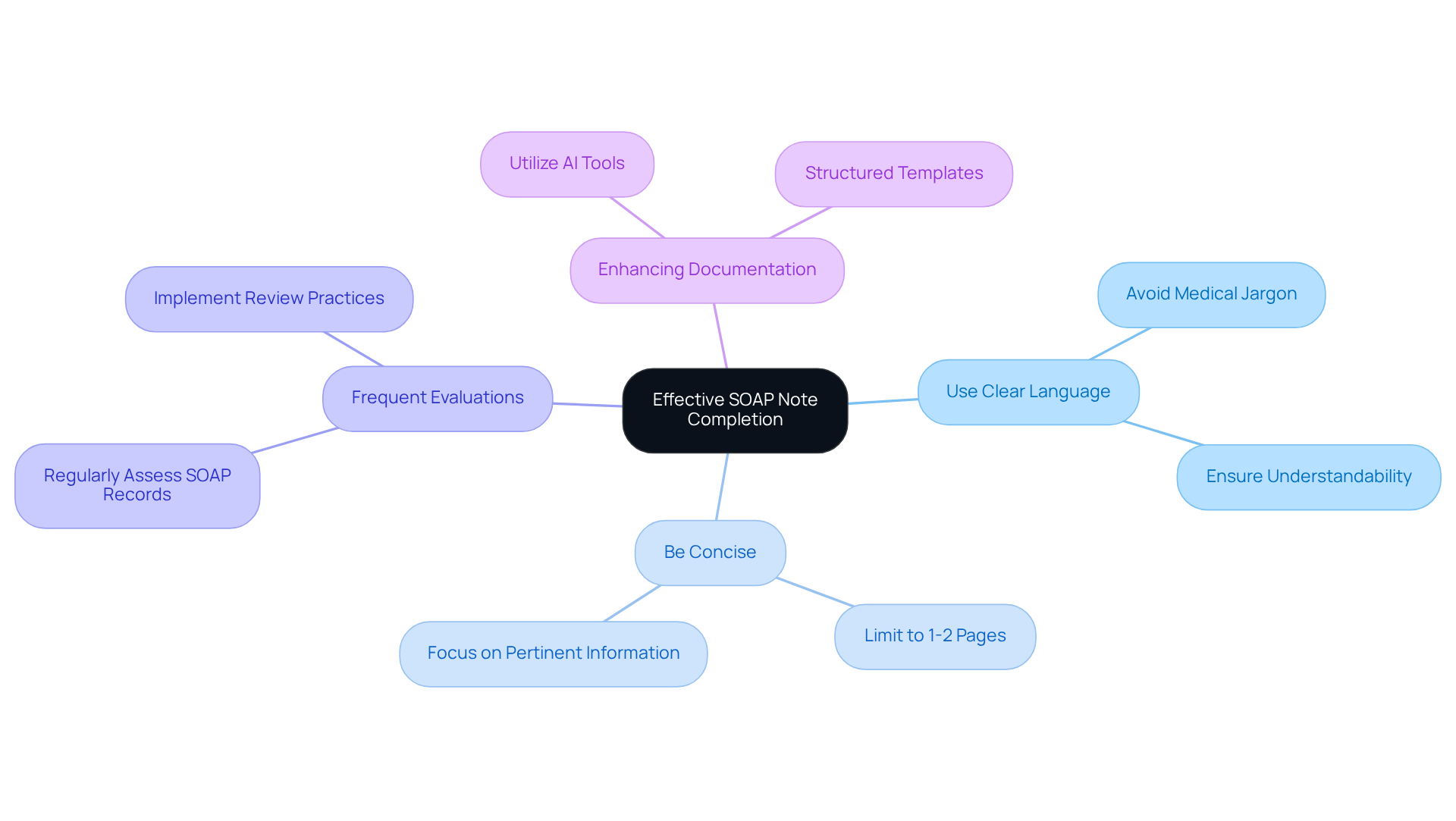
SonderMind: Tips and Examples for Effective SOAP Note Completion
Effective completion of a soap report example is essential for healthcare providers aiming to improve clarity and conciseness in their documentation. It’s understandable that amidst the demands of patient care, administrative tasks can feel overwhelming. Here are some key strategies that can help ease this burden and enhance your documentation:
- Use Clear Language: Have you ever felt lost in medical jargon? By avoiding complex terms and ensuring that notes are easily understandable for all members of the healthcare team, you foster better communication and collaboration.
- Be Concise: Focus on the most pertinent information. Keeping your written content to 1-2 pages not only prevents overwhelming the reader but also ensures that critical details stand out.
- Frequent Evaluations: Regularly assessing SOAP records can significantly improve the quality of your notes. Healthcare practices that implement frequent reviews often notice enhancements in the clarity of their documentation.
Many healthcare providers have successfully improved their record clarity by using structured templates and AI tools, as demonstrated in a soap report example. For instance, Priority Physicians achieved a remarkable 70% decrease in charting time and reclaimed $16,000 in lost clinical time after adopting AI-assisted record-keeping.
- Quotes on Clarity: Renowned physician Dr. Lawrence L. Weed emphasized the importance of clarity in records, stating that "the structured format assists healthcare professionals in applying their clinical reasoning to evaluate, diagnose, and manage an individual based on the information given."
- Enhancing Documentation: To further elevate your records, consider utilizing AI tools that simplify the process and reduce administrative burdens. These tools can help ensure that your records are not only precise but also comply with legal standards, thereby enhancing overall care for your patients.
By applying these strategies, you can develop efficient documentation that supports clinical decision-making and ultimately improves patient outcomes. Remember, every step you take towards clearer documentation is a step towards better patient care.
CanadianPA: Diverse SOAP Note Examples Across Medical Specialties
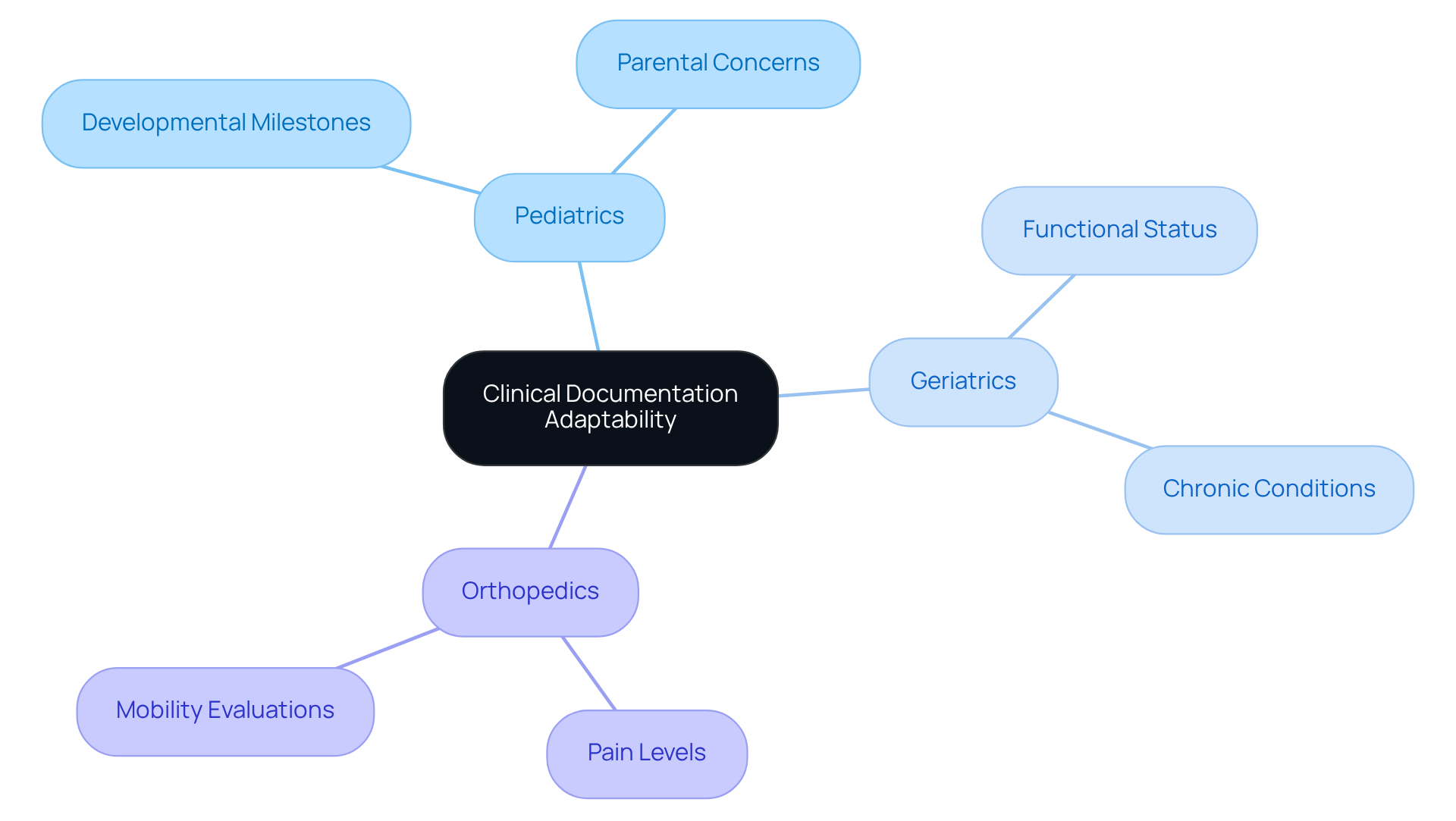
The adaptability of clinical documentation is a vital aspect of its role across various medical fields, allowing healthcare professionals to customize records to meet specific clinical needs. The format, which encompasses Subjective, Objective, Assessment, and Plan, provides a structured framework for gathering information and guiding clinical decision-making.
- Pediatrics: In pediatric care, clinical records often highlight developmental milestones and parental concerns. This ensures the unique aspects of child health are thoroughly documented, capturing not only the child's growth but also addressing the family's perspective, which is essential for effective treatment planning.
- Geriatrics: For elderly individuals, documentation focuses on functional status and chronic conditions, reflecting the complexities of aging. This adaptation allows healthcare providers to monitor changes in health status and adjust care plans accordingly, enhancing the quality of life for older adults.
- Orthopedics: In orthopedic settings, documentation emphasizes pain levels and mobility evaluations, providing crucial information for treatment decisions. By carefully documenting these factors, clinicians can assess individual progress and modify interventions as needed.
The impact of specialty-specific clinical summaries on medical records is significant, as they enhance clarity and efficiency in individual files. In 2025, statistics indicate that healthcare providers using customized formats report a 30% improvement in record accuracy and a 25% reduction in time spent on record-keeping. As one clinician noted, 'Customized clinical summaries not only simplify our record-keeping process but also enhance our ability to deliver targeted care to individuals.' This evolution in record-keeping practices underscores the importance of tailoring records to meet the specific needs of various medical specialties, ultimately improving care for individuals and clinical outcomes. Moreover, the APSO format (Assessment, Plan, Subjective, Objective) has emerged as an alternative structure that boosts usability, facilitating quicker access to critical information.
Upheal: Practical SOAP Note Example for Healthcare Providers
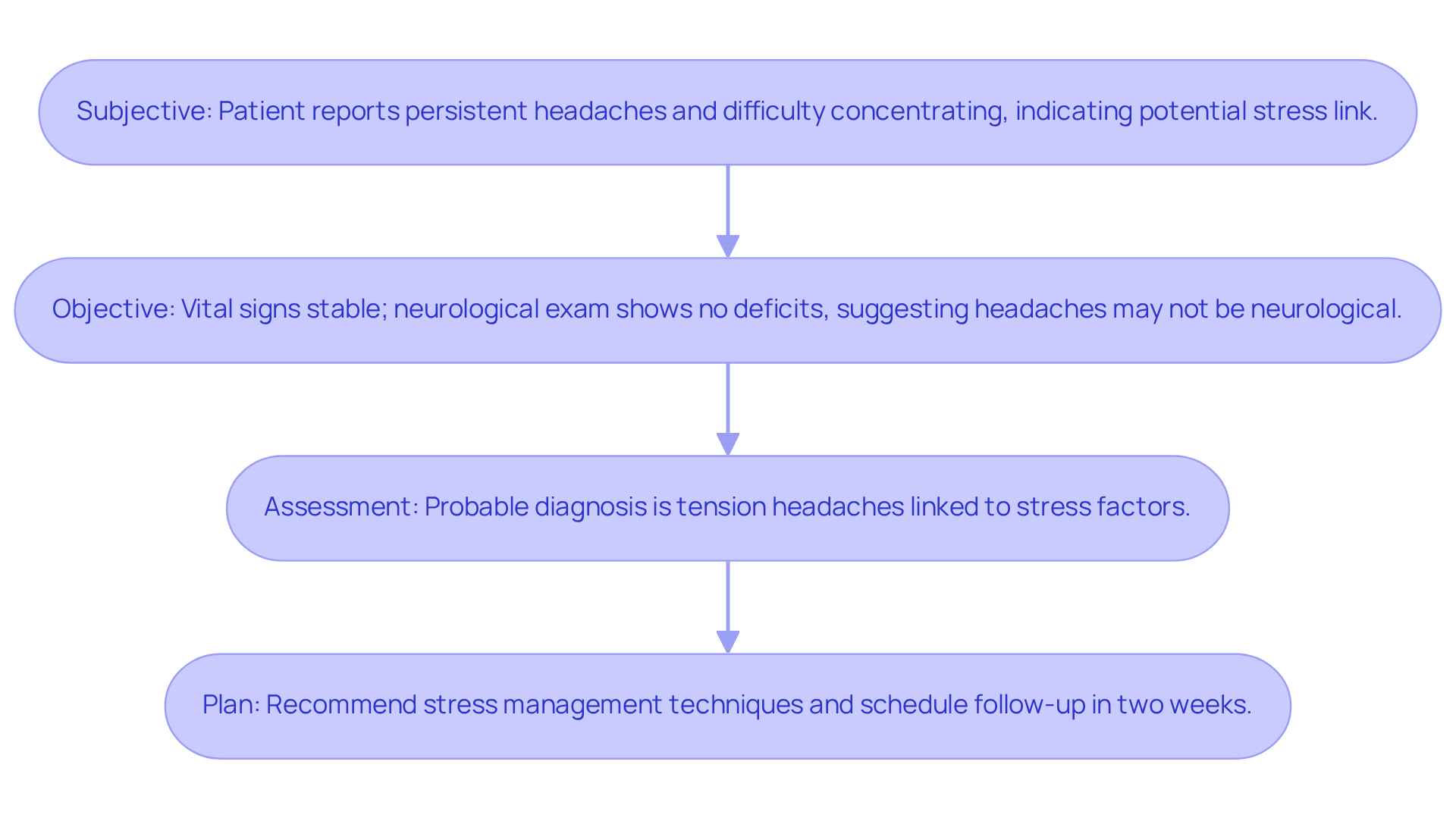
A practical soap report example can serve as a valuable reference for healthcare providers who may feel overwhelmed by documentation practices. Here’s a structured example that can ease some of that burden:
- Subjective: The patient reports persistent headaches and difficulty concentrating, indicating a potential link to stress.
- Objective: Vital signs are stable; a neurological examination reveals no deficits, suggesting that the headaches may not be of neurological origin.
- Assessment: The probable diagnosis is tension headaches, linked to stress factors in the individual's life.
- Plan: Recommend stress management techniques, including mindfulness and relaxation exercises, and schedule a follow-up appointment in two weeks to reassess symptoms.
Utilizing organized records such as this soap report example not only simplifies documentation but also enhances clinical decision-making. In 2025, the effectiveness of SOAP notes in follow-up care is highlighted by their ability to improve communication and minimize follow-up errors, ultimately leading to better outcomes. By adhering to current best practices for documenting client interactions, healthcare providers can ensure clarity and consistency in their records, which is essential for effective care coordination.
Moreover, incorporating generative AI solutions can significantly enhance the quality and consistency of records. Customized soap report examples can greatly streamline the documentation process, especially when managing numerous individuals. By automating repetitive tasks and optimizing workflows, healthcare providers can dedicate more time to patient care, transforming the patient experience and outcomes.
Have you considered how these strategies could alleviate some of the stress in your practice? Embracing these tools not only supports your documentation efforts but ultimately fosters a more compassionate approach to patient care.
Conclusion
Embracing the structured approach of SOAP notes is crucial for healthcare providers who face the emotional challenges of documentation. The weight of administrative burdens can often overshadow the primary focus on patient care. By implementing efficient and customizable templates, professionals can streamline their workflows, ensuring that patient interactions are documented accurately and effectively. The integration of AI-driven solutions, such as those offered by CosmaNeura and SimplePractice, empowers providers to shift their focus back to what truly matters: compassionate patient care.
Throughout this article, we’ve highlighted various platforms and their unique features, showcasing how tailored SOAP note examples can meet the specific needs across different healthcare specialties. From compliance assurance to the benefits of real-time data capture, the importance of structured documentation is clear. Best practices, such as maintaining clarity and conciseness, reinforce the value of organized records in improving patient outcomes and ensuring regulatory compliance.
Ultimately, the evolution of SOAP notes represents a significant opportunity for healthcare professionals to enhance their documentation practices. By adopting these strategies and tools, providers can reclaim valuable time, reduce errors, and foster a more compassionate approach to patient care. The journey toward improved documentation is not just about efficiency; it’s about enriching the quality of care delivered to patients and ensuring that their needs are met with precision and empathy. How will you take the next step in enhancing your documentation practices?




