Overview
In the demanding world of healthcare, the clarity of communication can significantly impact patient care. Have you ever felt overwhelmed by the complexities of conveying critical information? This article highlights the vital role that precise clinical language plays in progress notes, aiming to alleviate some of those burdens. By employing specific clinical terminology, healthcare providers can enhance clarity, leading to improved treatment outcomes and reducing misunderstandings that might adversely affect patient health.
Imagine a scenario where every word in a progress note is carefully chosen. This not only facilitates effective communication among providers but also nurtures a collaborative environment focused on patient well-being. As we explore the benefits of clear clinical language, it becomes evident that this practice supports better healthcare delivery, ultimately fostering a more compassionate approach to patient care.
Let’s consider the positive impact of this change. By prioritizing precise language, we can minimize the risk of errors and ensure that every patient receives the attention they deserve. It’s a small adjustment that can lead to profound improvements in health outcomes. Together, we can create a healthcare environment where clarity reigns, and patient care is paramount.
As you reflect on your own experiences, think about how adopting precise clinical language could enhance your practice. Are there areas where clearer communication could make a difference? Embracing this approach not only benefits patients but also empowers us as healthcare providers to deliver the best possible care. Let’s commit to fostering an atmosphere of understanding and support through the words we choose.
Introduction
Healthcare providers often face the emotional challenge of balancing quality patient care with the heavy burden of extensive documentation. This struggle can feel overwhelming, as the clarity of progress notes is crucial. Precise clinical language not only enhances communication among professionals but also significantly impacts patient outcomes. How can providers ensure their documentation is clear and effectively captures the nuances of patient care?
This article explores ten essential clinical words that can transform progress notes into powerful tools for clarity and understanding. By doing so, we can foster better therapeutic relationships and improve healthcare delivery. Let’s delve into these solutions together, empowering you to navigate the complexities of documentation with confidence and care.
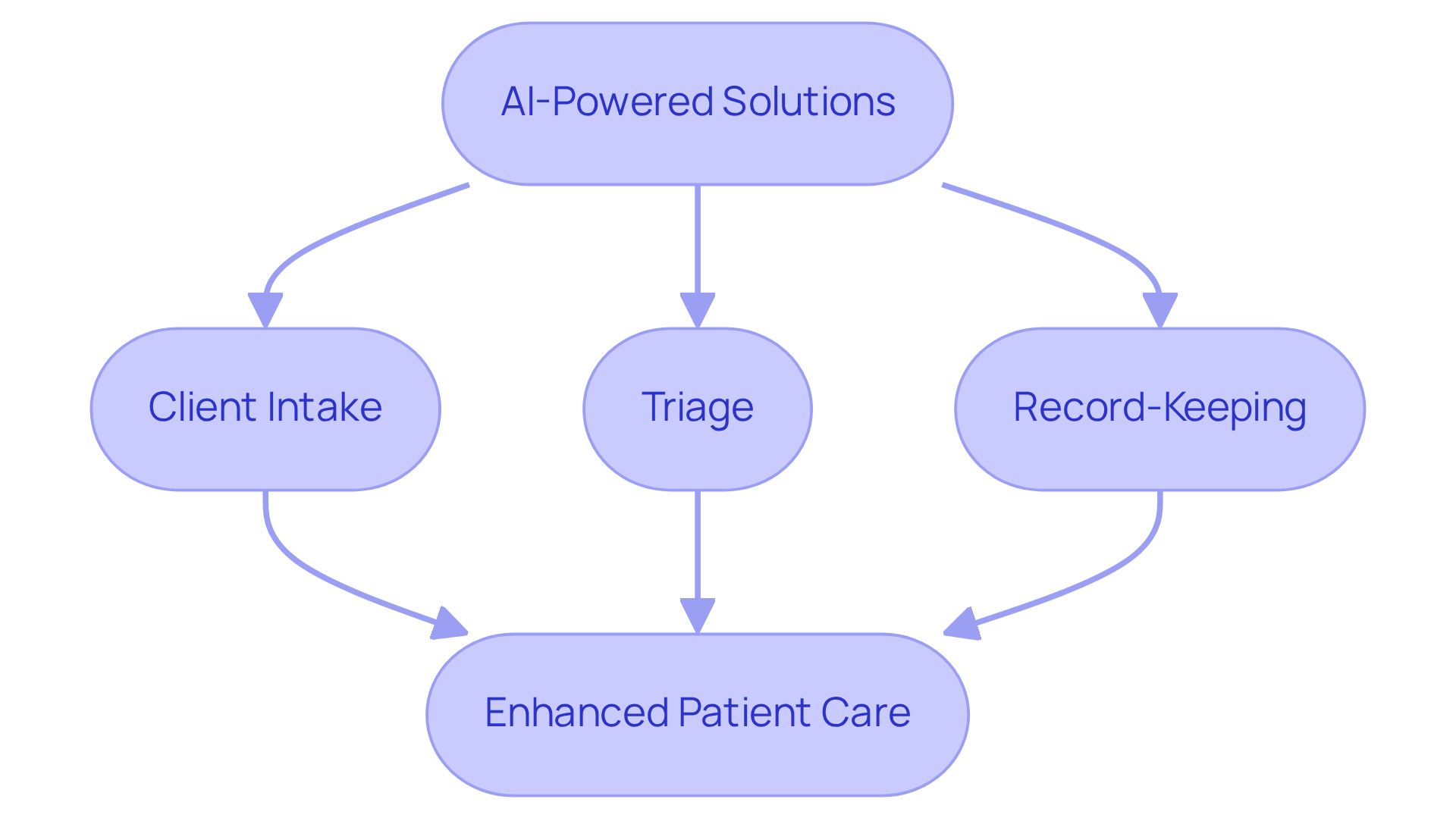
CosmaNeura: Streamline Documentation with AI-Powered Solutions
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to care for patients. CosmaNeura understands these emotional challenges and utilizes advanced AI technology to transform clinical records. This allows providers to focus on the individual needs of their patients, rather than getting lost in paperwork.
By automating crucial processes like client intake and triage, CosmaNeura significantly enhances efficiency and precision in record-keeping. Imagine reclaiming valuable time that can be devoted to providing higher quality services. This innovative approach not only alleviates the workload for healthcare professionals but also ensures adherence to ethical standards, particularly for faith-focused providers.
Research shows that methods employing AI have achieved up to a 91% decrease in document processing time. This means clinicians can concentrate more on their clients, fostering a more . It’s understandable to worry about technology diminishing human interaction in healthcare, but this shift enhances clinician productivity while nurturing those essential connections.
As one expert noted, "AI shows massive potential for improving the day-to-day work life of doctors across various clinical settings." This reinforces the transformative impact of AI in healthcare. If you’re ready to explore how CosmaNeura can support your practice, consider engaging with our solutions to enhance your care delivery.
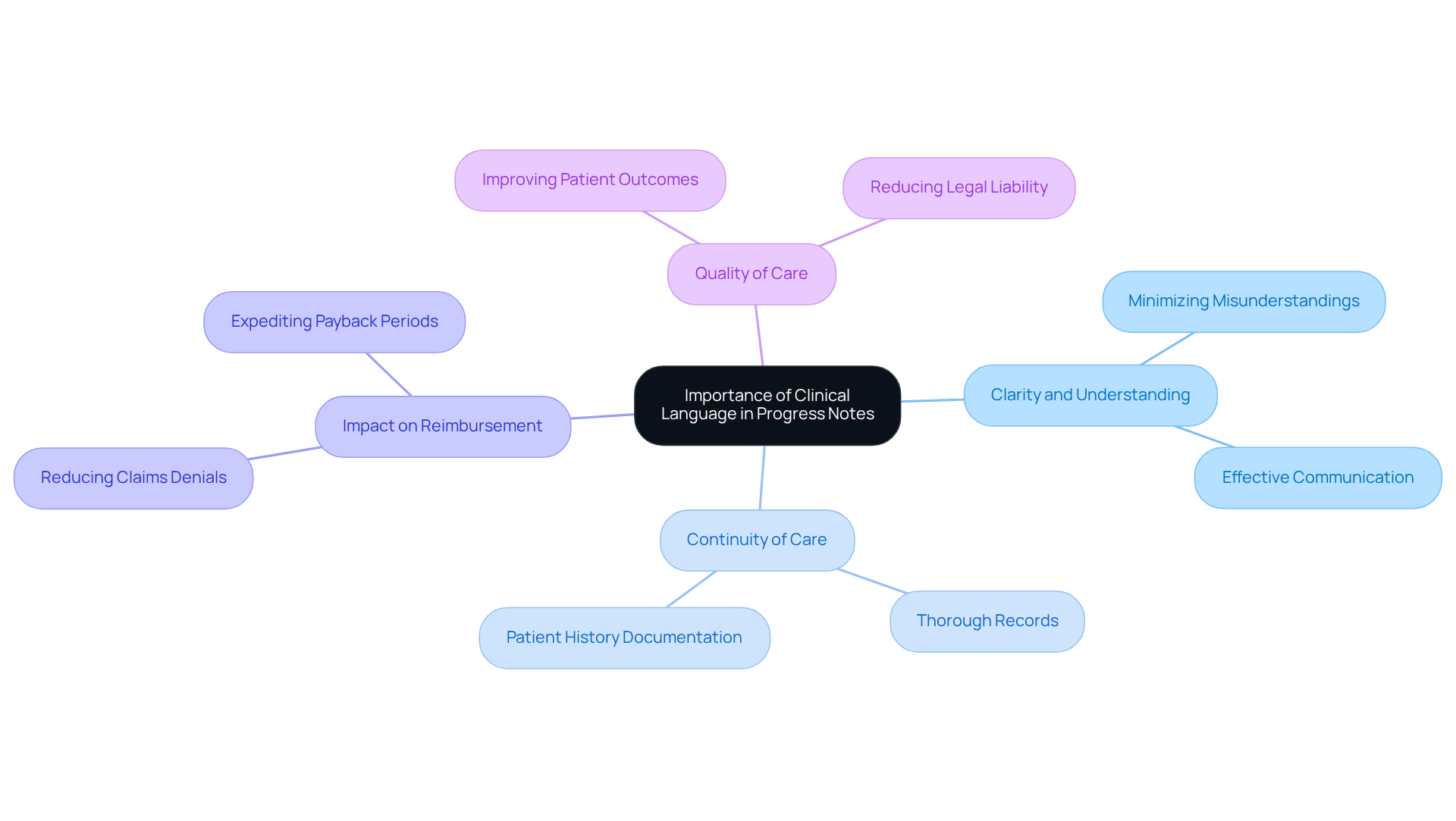
Clinical Language: Importance in Progress Notes for Clarity
Using to use in progress notes is vital for fostering clarity and understanding among healthcare providers. Have you ever felt overwhelmed by the administrative demands of your role? Thorough records play a crucial role in effectively communicating an individual's condition, treatment progress, and any changes in their health status. This clarity not only supports the continuity of care but also minimizes misunderstandings that could adversely affect patient outcomes.
Research shows that insufficient records can lead to postponed payments, rejected claims, and decreased reimbursement rates, ultimately compromising the quality of patient treatment. Conversely, efficient record-keeping practices can enhance reimbursement rates, reduce claims denials, expedite payback periods, and lower legal liability. Imagine the peace of mind that comes with knowing your records are complete and well-organized—expert opinions highlight that this reduces the likelihood of errors, thereby improving the overall quality of care provided.
As we reflect on the [importance of effective record-keeping](https://consensus.com/blog/why-is-documentation-important-in-healthcare), consider this: "Effective record-keeping is essential for delivering quality healthcare." The significance of clarity in progress notes, particularly through the use of clinical words to use in progress notes, cannot be overstated, as it directly influences patient outcomes and the efficiency of healthcare delivery. Let's commit to nurturing our practices, ensuring that every detail is captured with care, for the benefit of those we serve.
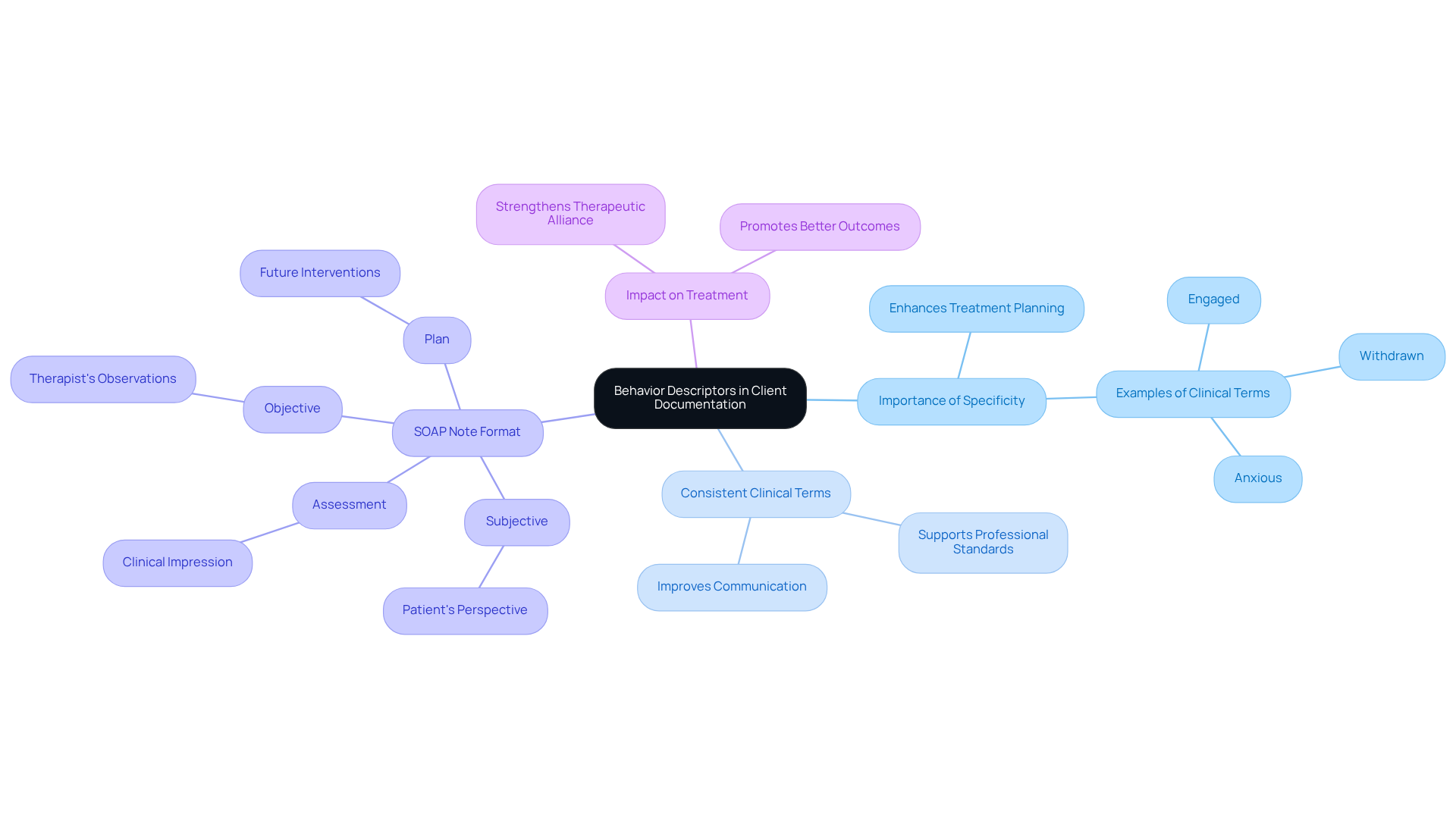
Behavior Descriptors: Key Terms for Accurate Client Documentation
Incorporating precise behavior descriptors, which are clinical words to use in progress notes, is crucial for accurate documentation of the individual. Have you ever considered how terms like 'engaged,' 'withdrawn,' and 'anxious' can illuminate an individual's emotional and behavioral state? This level of specificity not only aids in effective treatment planning but also fosters a unified understanding among team members regarding the individual's progress and challenges through the use of clinical words to use in progress notes. By recording these behaviors precisely, providers can tailor interventions more effectively, ultimately enhancing the quality of service provided.
Moreover, employing consistent clinical words to use in progress notes supports adherence to professional standards and enhances communication among care teams. This strengthens the therapeutic alliance and promotes better outcomes for clients. To ensure thorough recording, it’s essential to follow the , which incorporates clinical words to use in progress notes, including the 'Subjective,' 'Objective,' 'Assessment,' and 'Plan' sections. Have you finalized your records within 24 to 72 hours of the visit? This practice is vital for ensuring accuracy and compliance.
As Innocent Turner wisely states, "When someone reads a note, they need to understand how your patient presented, what's going on with them right now, how you helped them, and how they received that help." Incorporating at least three elements of the mental status exam in progress notes emphasizes the need for specificity in record-keeping through the use of clinical words to use in progress notes. Let’s commit to enhancing our documentation practices together for the benefit of our patients.
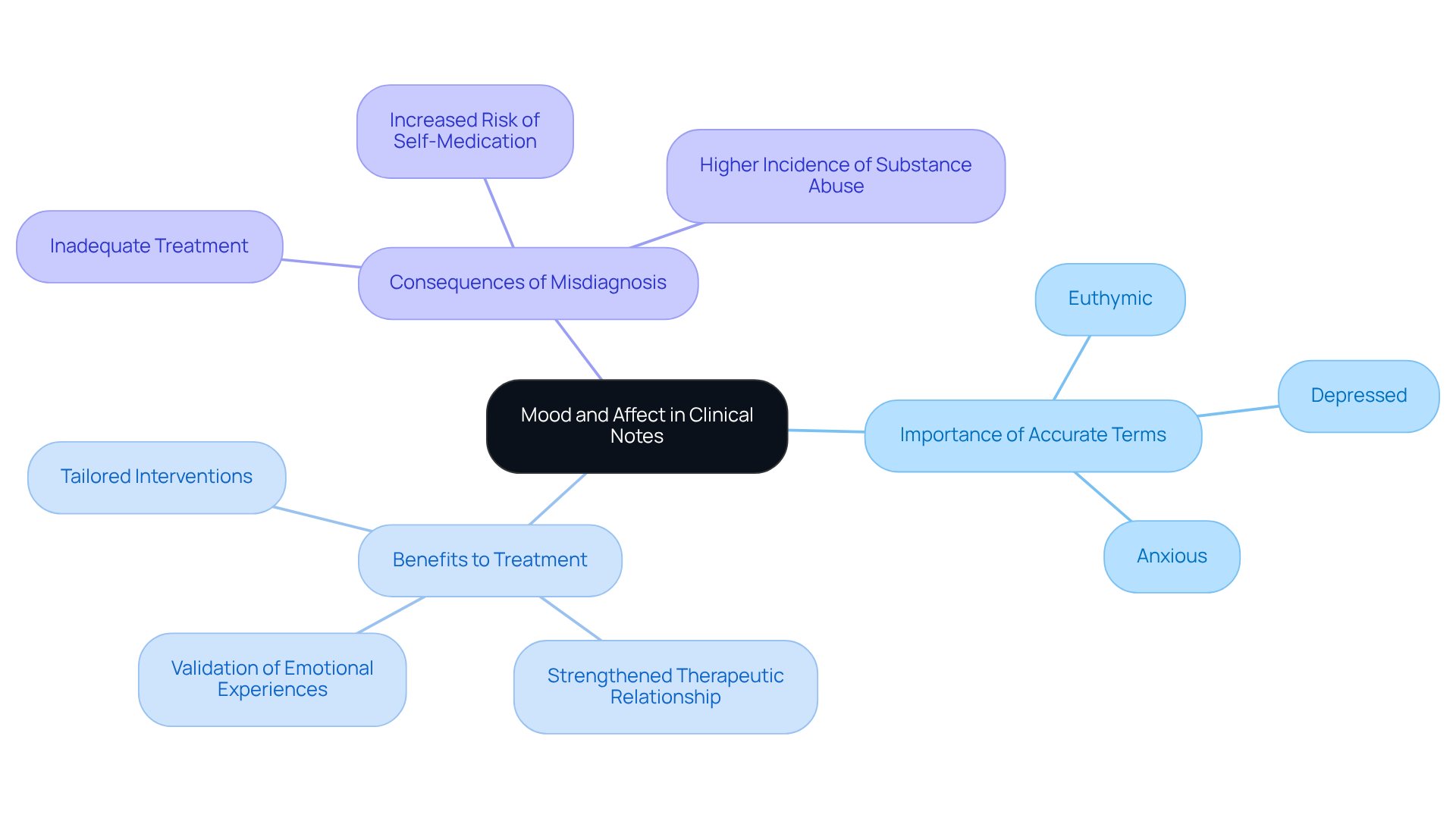
Mood and Affect: Essential Clinical Terms for Progress Notes
Understanding a person's mood and affect is crucial for grasping their emotional condition. Have you ever considered how specific clinical words to use in progress notes, like 'euthymic,' 'depressed,' or 'anxious,' can aid clinicians in assessing emotional well-being? By using these precise terms, healthcare providers can tailor interventions that truly resonate with their clients. This careful documentation, which utilizes clinical words to use in progress notes, not only informs treatment plans but also strengthens the therapeutic relationship, validating the emotional experiences of those seeking help.
Acknowledging and documenting emotional states with clinical words to use in progress notes fosters a compassionate approach to support, ultimately enhancing the quality of treatment offered. With occurrence rates of in primary health individuals ranging from 23% to 35%, the need for accurate record-keeping becomes even more apparent. As Dr. Martin A Katzman emphasizes, improving detection quality by primary care physicians is essential for better care.
Failing to use clinical words to use in progress notes when documenting emotional states can lead to misdiagnosis and inadequate treatment. This highlights the vital role that thorough documentation plays in effective clinical practice. By embracing this practice, we can ensure that every individual receives the compassionate and informed care they deserve.
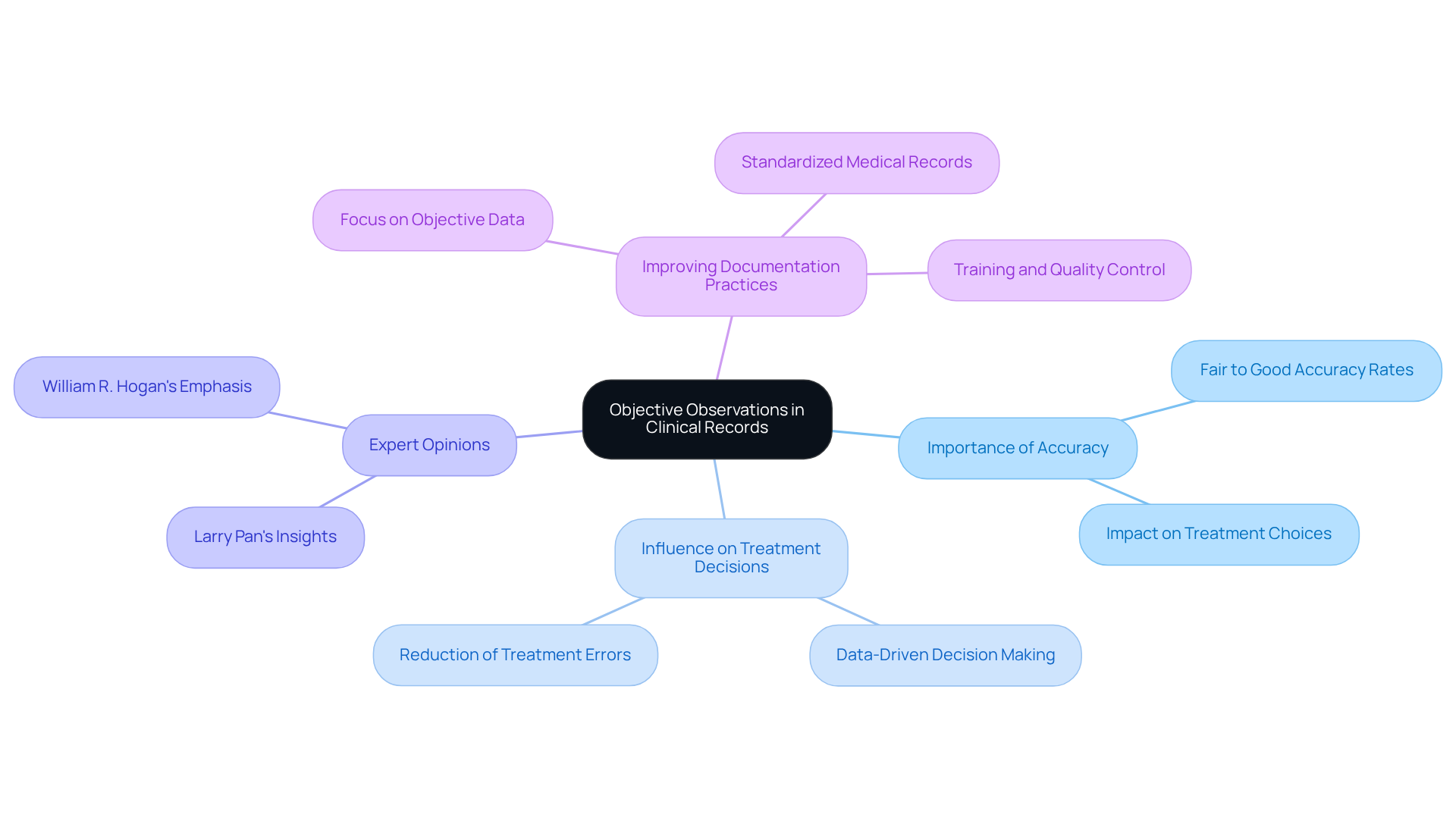
Objective Observations: Ensuring Accuracy in Clinical Records
Objective observations are crucial in ensuring the accuracy of clinical records. These observations, grounded in measurable and observable data—such as vital signs, physical examination results, and specific individual behaviors—help clinicians create a factual basis for treatment decisions. This, in turn, enhances the reliability of clinical records and supports effective care for individuals.
Have you ever considered how vital accurate data is to your practice? Research shows that the accuracy of data in clinical client records (CPRs) is generally perceived as fair to good, with most studies reporting correctness and completeness rates exceeding 80%. This level of accuracy is not just a statistic; it directly influences treatment choices and outcomes for those you care for.
Moreover, expert opinions highlight that incorporating objective data not only boosts record accuracy but also fosters better communication among healthcare providers. As Larry Pan noted, "the aim of this study is to demonstrate that standardized medical records can be used as a data abstraction training tool and a quality control measure to assess the validity of medical record data abstraction." Additionally, William R. Hogan emphasized, "the accuracy of these data is therefore of great importance."
To improve clinical documentation practices, it is essential for healthcare providers to prioritize the clinical words to use in progress notes, focusing on the in their records. By ensuring that all pertinent measurable information is captured, you can support optimal patient management and enhance the quality of service provided. Let’s work together to make this a reality for better patient outcomes.
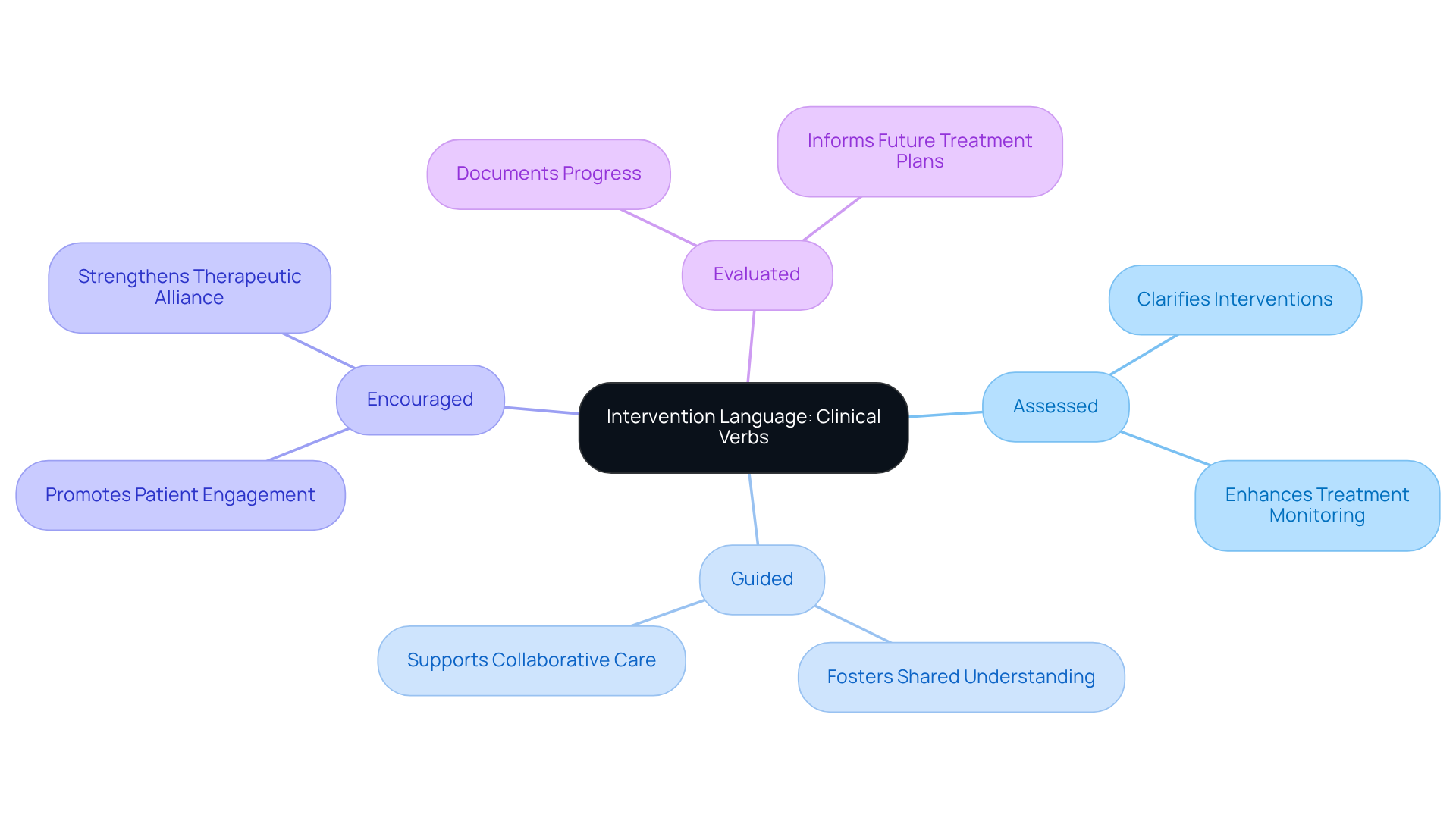
Intervention Language: Clinical Verbs for Documenting Therapist Actions
Understanding the emotional challenges healthcare providers face in documenting therapy sessions is essential. Utilizing to use in progress notes is not just a task; it's a vital part of effective patient care. Terms like 'assessed,' 'guided,' 'encouraged,' and 'evaluated' do more than clarify interventions—they foster a shared understanding among team members about the therapeutic approach. This specificity is crucial for monitoring progress accurately, offering a detailed perspective on the treatment journey.
Moreover, using specific action terms helps create a common language within the support team. When everyone is aligned on the strategies being implemented, it enhances the overall quality of care. By focusing on clinical words to use in progress notes, therapists can significantly improve their records, ultimately benefiting both patient care and professional accountability. However, many therapists find it challenging to shift into the record-keeping mindset after sessions. This struggle can hinder the clarity of their notes, impacting the quality of care.
Accurate documentation is not only essential for effective treatment; it also fulfills legal and ethical obligations, ensuring adherence to standards that protect both patients and providers. As you reflect on your practice, consider how adopting precise language can enhance your documentation process. What steps can you take to make this transition smoother? Remember, every effort you make in this area contributes to better outcomes for your patients and a more cohesive support team.
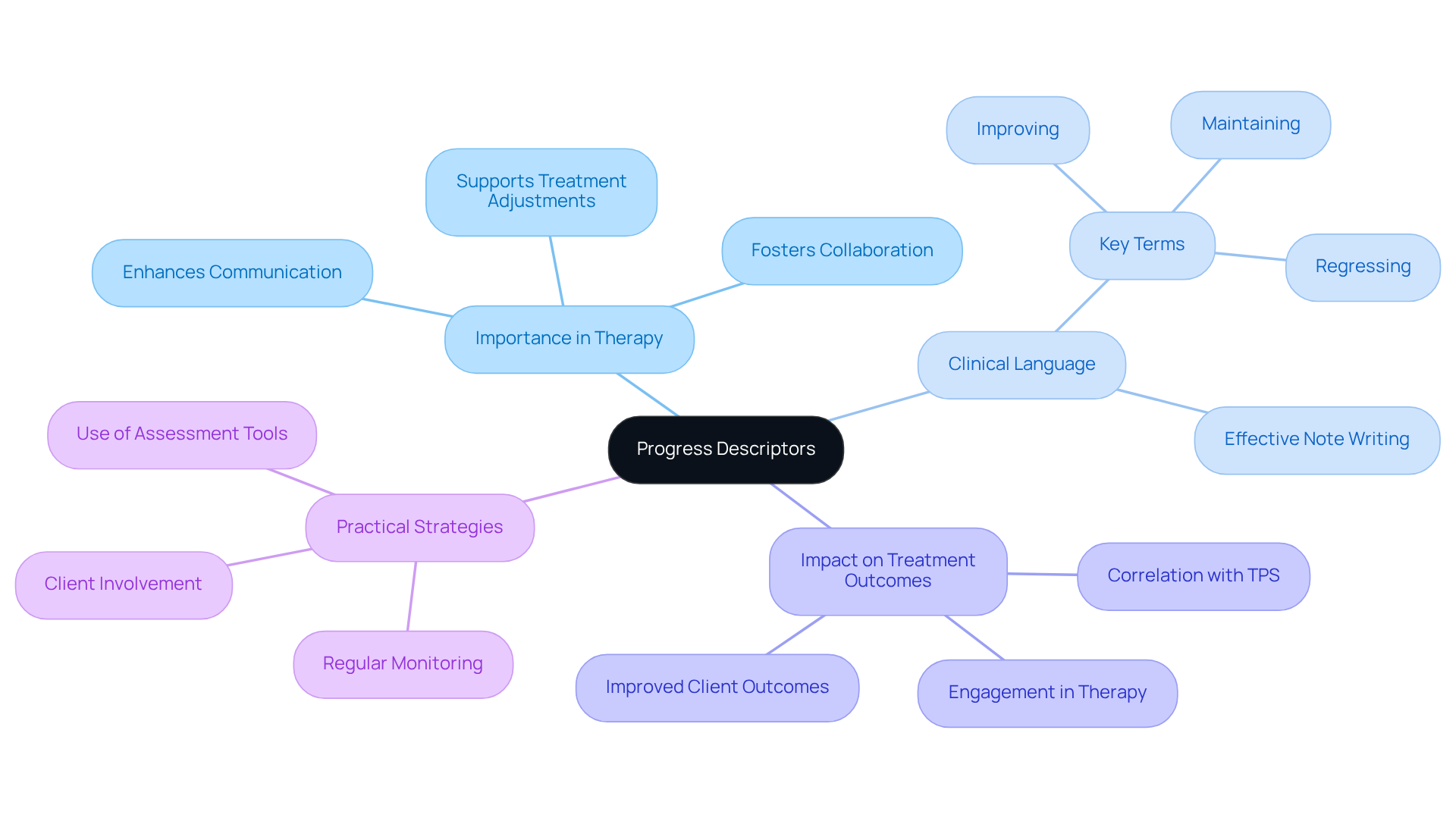
Progress Descriptors: Language for Documenting Client Development
Progress descriptors play a crucial role in documenting individual development in therapy. Have you ever considered how terms like 'improving,' 'maintaining,' or 'regressing' can illuminate a patient's journey through treatment? By using clinical words to use in progress notes, practitioners can effectively communicate changes in a patient's condition, which allows for timely adjustments to the treatment plan and fosters a collaborative approach to support. As Vivian Chung Easton, Clinical Product Lead at Blueprint, emphasizes, 'Writing clear and concise progress notes with clinical words to use in progress notes is key to maintaining continuity of care and demonstrating the impact of therapeutic interventions.'
Furthermore, studies reveal that structured progress notes can lead to enhanced treatment outcomes. There is a significant correlation between the and other assessment tools, such as the PHQ-9 and GAD-7. Integrating clinical words to use in progress notes not only enhances communication among healthcare professionals but also actively engages patients in their therapeutic journey. This involvement ultimately promotes better outcomes.
In a world where administrative burdens can weigh heavily on healthcare providers, embracing these practices can lighten the load and enhance the quality of care. Let’s take a moment to reflect on how we can incorporate these strategies into our daily routines, ensuring that every patient feels supported and understood.
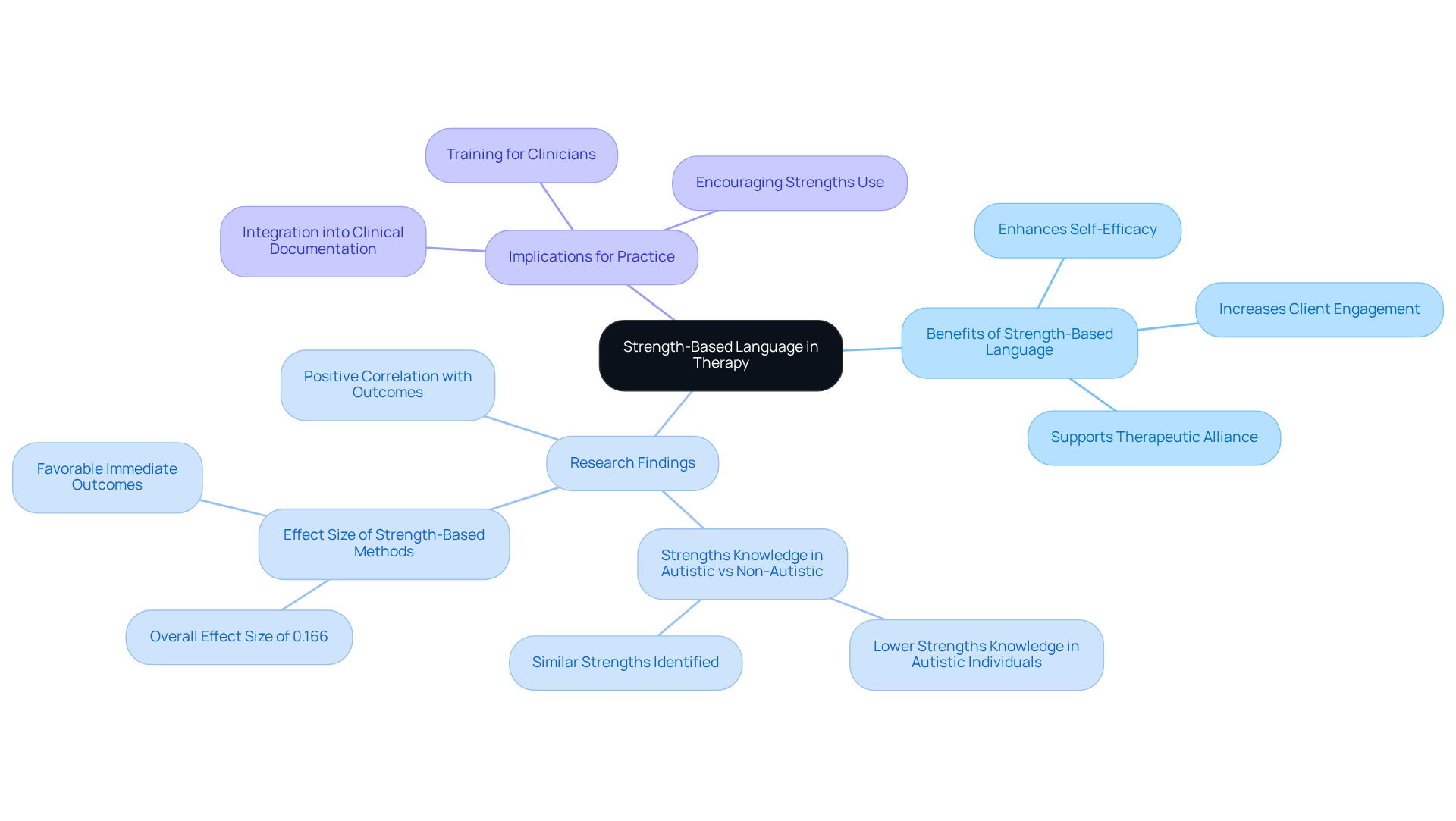
Strength-Based Language: Enhancing Client Engagement in Notes
Incorporating strength-based language in progress notes is vital for nurturing participant engagement. Have you ever considered how highlighting patients' strengths and accomplishments can transform their narrative? By using expressions like 'demonstrated resilience' and 'utilized coping strategies,' clinicians not only reflect individual progress but also inspire continued involvement in the therapeutic journey.
Research shows that when therapists employ positive language, it correlates with higher session productivity ratings from patients. This reinforces the therapeutic alliance, creating a supportive environment. Focusing on strengths can significantly enhance individuals' self-efficacy and motivation, fostering resilience and encouraging effort in overcoming challenges.
This compassionate approach aligns with findings that suggest yield favorable immediate outcomes in therapy sessions. It's a reminder of the importance of integrating clinical words to use in progress notes into clinical documentation. By recognizing and celebrating clients' capabilities, clinicians validate their experiences and promote a more engaged and proactive approach to treatment. How can we further embrace this nurturing language in our practice?
Note Templates: Structuring Progress Notes for Consistency
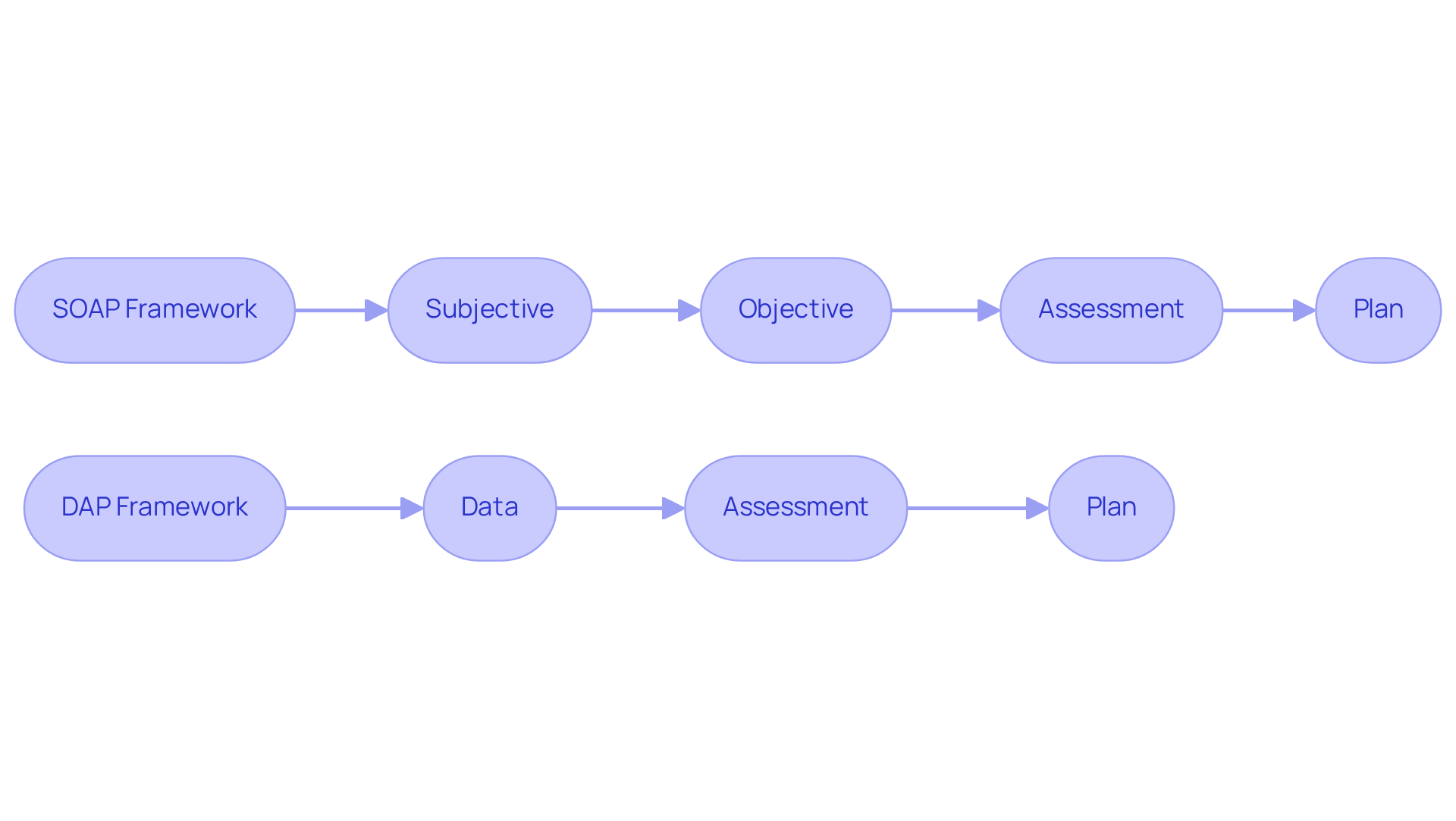
In the demanding world of healthcare, the emotional challenges faced by providers can often feel overwhelming. Utilizing is crucial for ensuring consistency in the clinical words to use in progress notes, which can alleviate some of these burdens. Frameworks such as SOAP (Subjective, Objective, Assessment, Plan) and DAP (Data, Assessment, Plan) include clinical words to use in progress notes, providing a systematic approach to documenting patient interactions and allowing providers to focus more on patient care.
By following a standardized format, healthcare providers can ensure they incorporate clinical words to use in progress notes to capture all pertinent information. This not only enhances communication among team members but also supports continuity of care, creating a more nurturing environment for patients. Research suggests that the application of these templates results in enhanced record quality, with compliance rates significantly rising from 36% to 65% over time.
Imagine the difference this structured approach can make—not just in clinical decision-making, but in fostering a more organized and efficient workflow. Ultimately, this benefits patient outcomes, allowing providers to deliver the compassionate care their patients deserve. As noted by Dr. Raj Mehta, the use of evidence-based templates is associated with improved note quality without significant changes in total charting time.
Therefore, healthcare professionals are encouraged to implement organized note templates. By doing so, they can enhance their record-keeping methods, reduce administrative burdens, and focus on what truly matters: the well-being of their patients.
Avoiding Vague Language: Ensuring Precision in Clinical Documentation
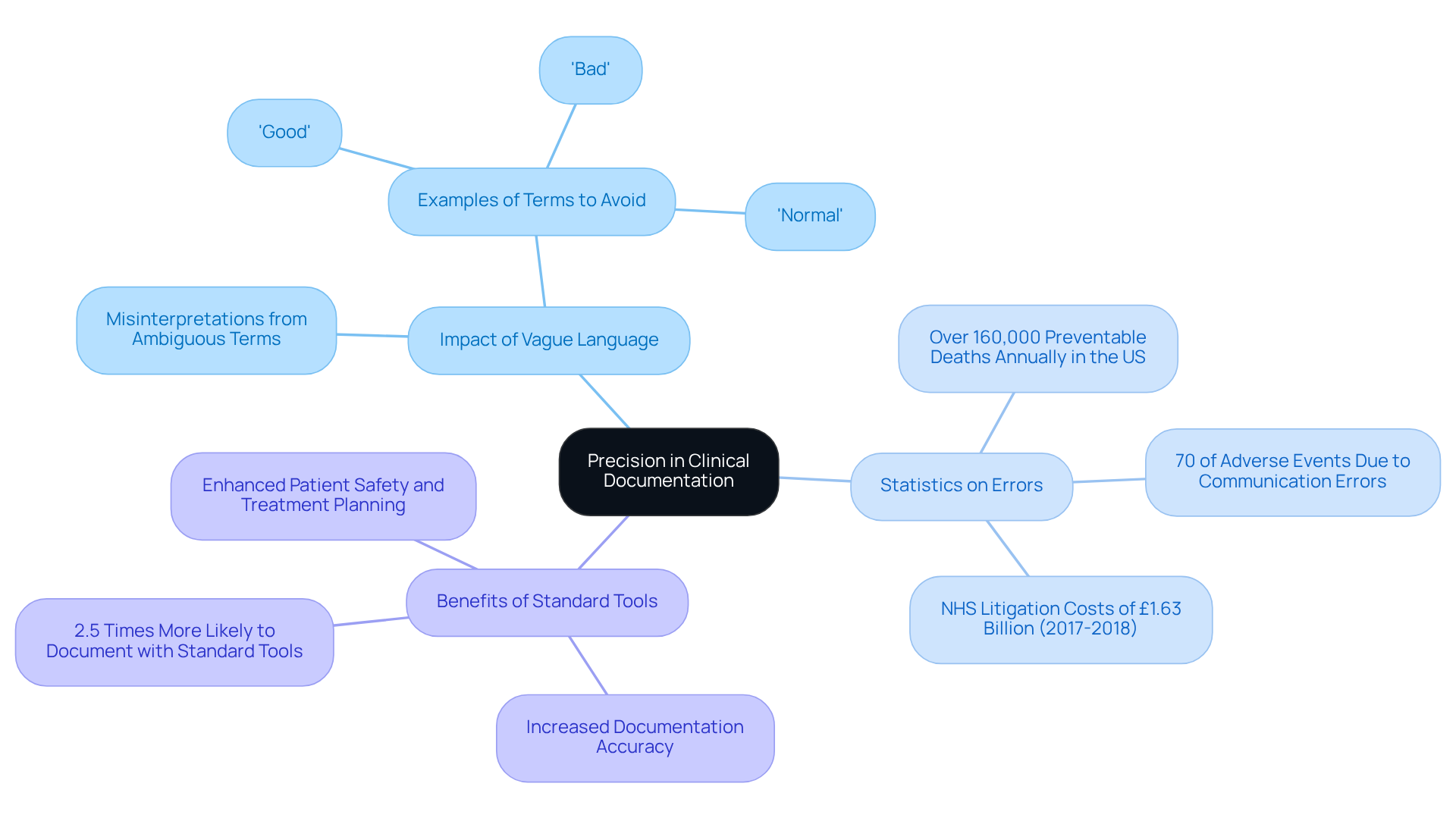
In the demanding world of healthcare, it is essential to use clinical words to use in progress notes to avoid vague language and foster precision and clarity. Have you ever considered how terms like 'good,' 'bad,' or 'normal' can lead to misinterpretations? Such ambiguity contributes to communication errors, which are a significant factor in 70% of adverse events, as highlighted in risk management literature. By using clinical words to use in progress notes that accurately reflect a client's condition and progress, clinicians can mitigate these risks.
This commitment to precision not only enhances the quality of records but also involves the use of clinical words to use in progress notes, supporting and patient safety. Research reveals that over 160,000 preventable fatalities occur annually in the US due to avoidable mistakes—an alarming statistic that underscores the serious repercussions of inadequate record-keeping methods. Furthermore, employing standard recording tools has been shown to increase the likelihood of health professionals documenting their routine practices by 2.5 times.
Imagine the positive impact on patient outcomes when healthcare providers prioritize precise language and utilize appropriate tools. By enhancing the reliability of their documentation, they can ultimately reduce the risk of preventable errors. Let’s work together to create a safer, more effective healthcare environment for everyone.
Conclusion
Utilizing precise clinical language in progress notes is essential for enhancing clarity and ensuring effective communication among healthcare providers. By focusing on specific terms and structured documentation, healthcare professionals can significantly improve the quality of care they deliver, ultimately benefiting patient outcomes.
Have you ever considered the emotional challenges healthcare providers face daily? Throughout this article, we have highlighted key points such as the importance of behavior descriptors, mood and affect terminology, and the need for objective observations. These elements not only aid in documenting a patient's journey but also promote a shared understanding among care teams. Additionally, employing strength-based language and structured note templates can streamline documentation processes, reduce administrative burdens, and enhance the therapeutic alliance.
In conclusion, embracing effective language for clinical documentation is not merely a task; it is a commitment to improving healthcare delivery. By prioritizing clarity and precision in progress notes, healthcare providers can foster better communication, reduce the risk of errors, and create a more compassionate environment for patient care. The call to action is clear: let us invest in refining documentation practices to ensure that every patient receives the thoughtful, informed care they deserve.




