Overview
In the healthcare field, providers often face emotional challenges that can weigh heavily on their daily practice. The article titled "10 Essential Examples of Patient Notes Every Healthcare Provider Should Know" addresses these concerns by highlighting the critical importance of various types of patient notes in healthcare documentation. It discusses how comprehensive record-keeping—utilizing formats like SOAP, DAP, and therapy notes—can alleviate some of the administrative burdens that impact patient care.
By enhancing communication and ensuring continuity of care, these documentation practices not only provide legal protection but also contribute to improved patient outcomes and provider efficiency. Imagine the peace of mind that comes with organized documentation, allowing you to focus more on what truly matters: your patients.
This article serves as a gentle reminder of the power of effective record-keeping. It encourages healthcare providers to embrace these practices, ultimately fostering a nurturing environment for both patients and providers alike. Let’s take this step together towards better communication and care.
Introduction
In the intricate world of healthcare, effective documentation transcends mere bureaucracy; it stands as a vital pillar of quality patient care. Have you ever considered how patient notes not only ensure continuity but also provide essential legal protection? Structured formats like SOAP and DAP notes play a crucial role in enhancing clinical decision-making. The importance of meticulous record-keeping is profound and cannot be overstated.
As the healthcare landscape evolves, so does the pressing need for innovative solutions that can alleviate administrative burdens and foster better communication among providers. This article invites you to explore the various facets of patient documentation, shedding light on best practices, the transformative role of technology, and the significant impact these practices have on patient outcomes. By recognizing the importance of robust documentation, healthcare professionals can not only enhance care delivery but also cultivate stronger, more trusting relationships with their patients.
Understanding Patient Notes: Importance and Purpose
Patient notes are essential communication tools within , playing a vital role in ensuring continuity of support and maintaining . These notes encapsulate crucial information regarding an individual's medical history, treatment plans, and progress, which are essential for informed clinical decision-making. In 2025, the importance of comprehensive record-keeping is underscored by the fact that nearly half of individuals did not access their online medical files or portals in 2022. This reveals a communication gap that can be addressed through effective record-keeping practices (Richwine C., 2022).
By carefully recording interactions, medical providers can track changes in health status, promoting better coordination of services and increasing overall safety for individuals. This is especially important in complex situations where multiple providers are involved, as clear and thorough records ensure that all team members are aligned on the individual's treatment plan. Moreover, patient notes serve as a legal safeguard for healthcare professionals, offering a detailed account of the services rendered.
This record not only protects providers in case of disagreements but also fosters accountability and transparency in care.
The impact of patient records extends to clinical decision-making, where well-maintained notes can significantly influence treatment outcomes. For instance, case studies have shown that practices employing organized record-keeping techniques, such as those supported by CosmaNeura's AI-driven services, report higher levels of job satisfaction among providers. This is because they can focus more on patient support rather than administrative tasks. CosmaNeura's solutions include advanced automation tools that simplify processes like appointment scheduling, medical record management, and billing, allowing providers to reclaim valuable time and ultimately enhance the quality of care.
Practical examples illustrate that efficient medical records lead to improved health outcomes, facilitating timely interventions based on documented changes in an individual's condition.
In conclusion, the significance of clinical notes in medical settings cannot be overstated. They are crucial for communication, continuity of care, and legal protection, while also elevating the overall quality of patient care. As healthcare continues to evolve, the emphasis on robust record-keeping practices will remain a cornerstone of effective clinical practice. This is particularly true when aligned with ethical guidelines that reflect the moral responsibility of healthcare providers, as highlighted by CosmaNeura's commitment to Catholic teachings.
SOAP Notes: Structure and Best Practices
SOAP notes are essential for effective clinical documentation, structured into four key components: Subjective, Objective, Assessment, and Plan. The Subjective section captures the individual's reported symptoms and concerns, offering valuable insight into their experience and perspective. In contrast, the Objective section presents measurable data such as vital signs, laboratory results, and physical examination findings, providing a factual basis for clinical evaluation.
The Assessment section synthesizes the information gathered from both the Subjective and Objective components to formulate a diagnosis or clinical impression. Finally, the Plan outlines the proposed treatment strategies, follow-up actions, and any referrals necessary for comprehensive care.
Best practices for writing SOAP notes emphasize clarity and conciseness. Each part should be unique yet linked, ensuring that the records provide a comprehensive view of the individual's condition. For instance, using clear language and avoiding medical jargon can enhance understanding for all team members involved in the patient's care.
Statistics show that can significantly improve patient outcomes. Studies indicate that medical providers who follow organized record-keeping practices report greater levels of job satisfaction and efficiency. Additionally, case studies reveal that organizations implementing standardized SOAP note protocols experience enhanced communication among providers, leading to better-coordinated services.
Significantly, CosmaNeura is the sole enterprise developing AI solutions for the billion-dollar faith-centered medical market, highlighting its distinctive role in improving clinical records.
CosmaNeura's AI platform can transcribe discussions in real-time and create draft notes, simplifying the SOAP note recording process for medical providers. This ability not only conserves time but also allows clinicians to focus more on interactions with individuals, thereby enhancing the quality of service. By alleviating the administrative pressures that often lead to physician fatigue, these AI-driven solutions improve provider efficiency and focus on individuals.
For example, an organization that adopted CosmaNeura's AI solutions noted a 30% decrease in time allocated to records, enabling providers to devote more time to individual support. Furthermore, by addressing the fragmentation of medical systems, CosmaNeura's solutions enhance communication and coordination among providers, ensuring that individual information is effortlessly exchanged across various platforms.
An example of patient notes in primary settings illustrates the significance of thoroughness and precision in effective SOAP records. A well-documented SOAP note could include an individual's complaint of chest discomfort (Subjective), an ECG reading and blood pressure measurement (Objective), a differential diagnosis (Assessment), and a treatment plan detailing medication and follow-up appointments (Plan).
In conclusion, SOAP notes are not merely administrative tasks; they are vital tools that aid clinical decision-making and improve treatment. By adhering to best practices in SOAP note writing and utilizing innovative solutions like those provided by CosmaNeura, healthcare providers can ensure their records are effective and aligned with the highest standards of care, ultimately transforming healthcare delivery.
DAP Notes: Key Components and Usage
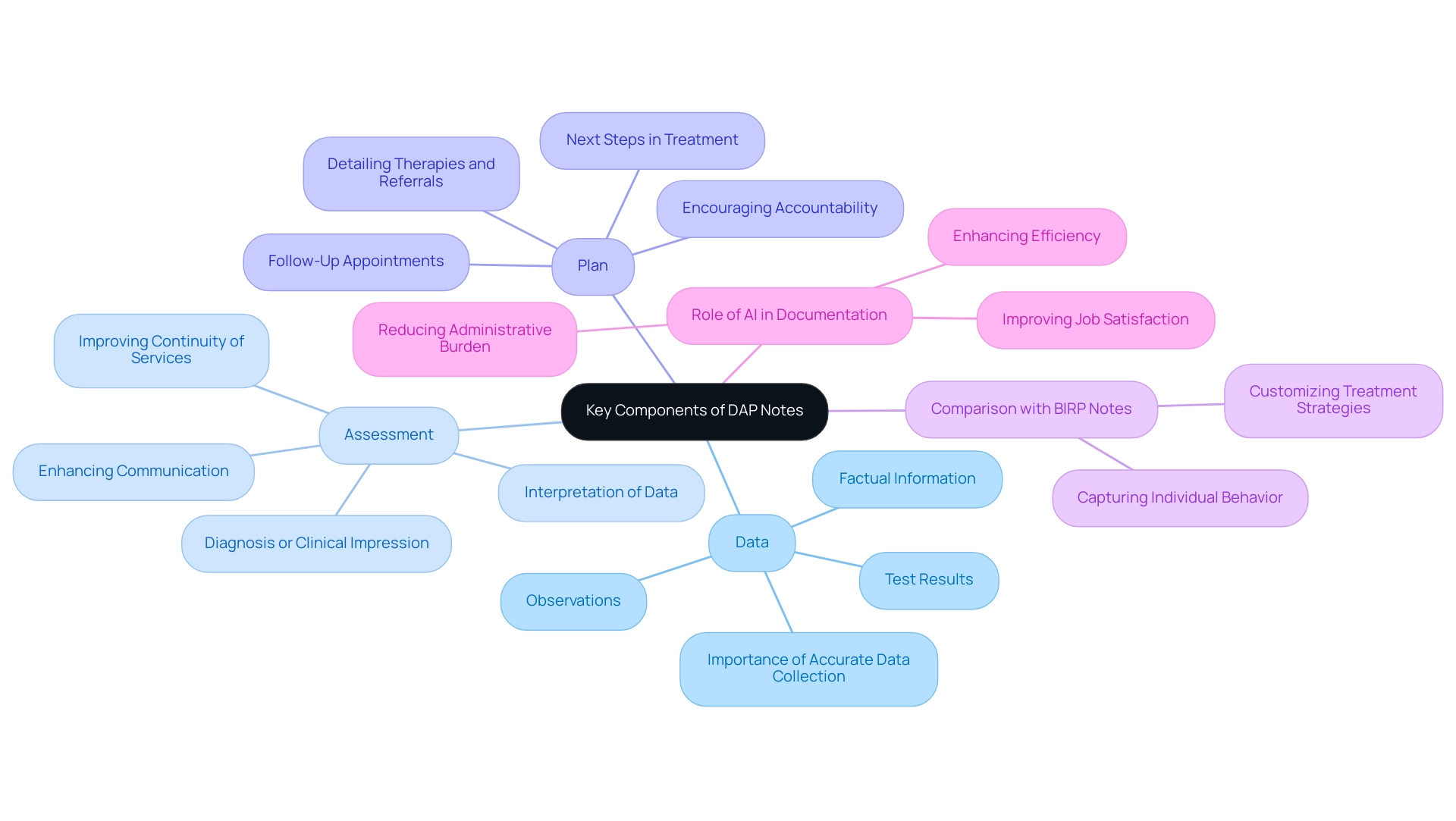
DAP notes are organized into three vital elements: Data, Assessment, and Plan, each fulfilling an important function in client records.
- Data: This section encompasses factual information collected during the individual's encounter, including observations, test results, and any relevant history. Accurate data collection is vital, as it forms the foundation for effective clinical decision-making. In mental health settings, where subjective experiences are often intertwined with objective findings, thorough documentation can significantly influence treatment outcomes.
- Assessment: Here, the clinician interprets the data, providing insights that lead to a diagnosis or clinical impression. This component is crucial for understanding the individual's condition and guiding subsequent treatment strategies. Research shows that well-documented evaluations can enhance communication among healthcare providers and improve continuity of services, ultimately benefiting outcomes for individuals.
- Plan: The final component outlines the next steps in the individual's treatment, detailing therapies, referrals, or follow-up appointments. A clear and actionable plan is essential for ensuring that individuals receive appropriate care and support. Effective planning not only supports recovery but also encourages accountability among healthcare providers.
In mental health records, DAP notes are especially beneficial as they provide a thorough perspective of the individual's experience, merging both subjective and objective information. For example, a case analysis contrasting DAP notes with , like BIRP notes, emphasizes how DAP notes can more effectively capture the subtleties of individual behavior and clinician interventions, enabling customized treatment strategies.
Furthermore, the flexibility of DAP notes—where there is no strict length requirement—allows clinicians to adapt their records to the specific needs of each individual, ensuring that all relevant information is captured without unnecessary constraints. This flexibility is essential in mental health environments, where the intricacy of individual experiences frequently necessitates thorough and subtle records.
As Marissa Moore, an experienced LPC, observes, 'Effective record-keeping is key to understanding and supporting our clients' needs.' By utilizing DAP notes effectively, providers can enhance their record-keeping practices, leading to improved treatment outcomes and a more organized approach to assisting individuals.
Moreover, CosmaNeura's AI platform can simplify the record-keeping process for medical providers, aligning with the company's mission to reduce administrative burdens. By automating elements of documentation, CosmaNeura enables providers to concentrate more on client support while ensuring that vital information is precisely recorded and readily accessible. This integration of AI not only improves administrative efficiency but also changes medical service delivery, ultimately leading to better outcomes for individuals.
In addressing the challenges faced by medical providers, such as physician burnout and fragmented support systems, DAP notes play a crucial role. By enhancing the efficiency of documentation, they assist in reducing some of the administrative burdens that lead to burnout, enabling medical professionals to devote more time to patient interactions. Additionally, the organized nature of DAP notes promotes improved communication among providers, which is vital in addressing the fragmentation of services that often obstructs effective treatment.
SBAR Communication: Enhancing Team Collaboration
In the demanding world of healthcare, clear communication is vital. SBAR—Situation, Background, Assessment, and Recommendation—serves as a structured communication tool that facilitates the exchange of critical information among team members. Each component is designed to address specific needs:
- The Situation identifies the current issue.
- The Background provides essential context.
- The Assessment summarizes the clinician's findings.
- The Recommendation outlines actionable next steps.
Implementing SBAR can significantly enhance collaboration within medical teams, especially in high-pressure environments where effective communication is crucial. For example, a study in Tunisia revealed that successful integration of SBAR requires tailored training programs and culturally sensitive approaches. This underscores the importance of adapting communication tools to meet the unique needs of medical teams, ensuring that all members share a unified understanding of patient support.
Moreover, effective communication through SBAR can prevent malpractice and strengthen therapeutic relationships between providers and patients. Research shows that when medical teams embrace SBAR, they experience improved collaboration, which is essential for delivering high-quality care. Engaging senior nursing staff in the development of SBAR interventions has been identified as a key factor in sustaining its use, demonstrating the tool's effectiveness in enhancing team dynamics.
Statistics reveal that medical teams utilizing SBAR report higher levels of communication effectiveness. A study involving 83 staff nurses indicated a direct correlation between the use of SBAR and enhanced patient outcomes. By adopting SBAR, providers can ensure that vital information is communicated succinctly and accurately, ultimately leading to and improved safety. Thus, SBAR not only functions as a communication framework but also acts as a catalyst for fostering collaboration among healthcare providers, making it an essential tool in modern clinical practice.
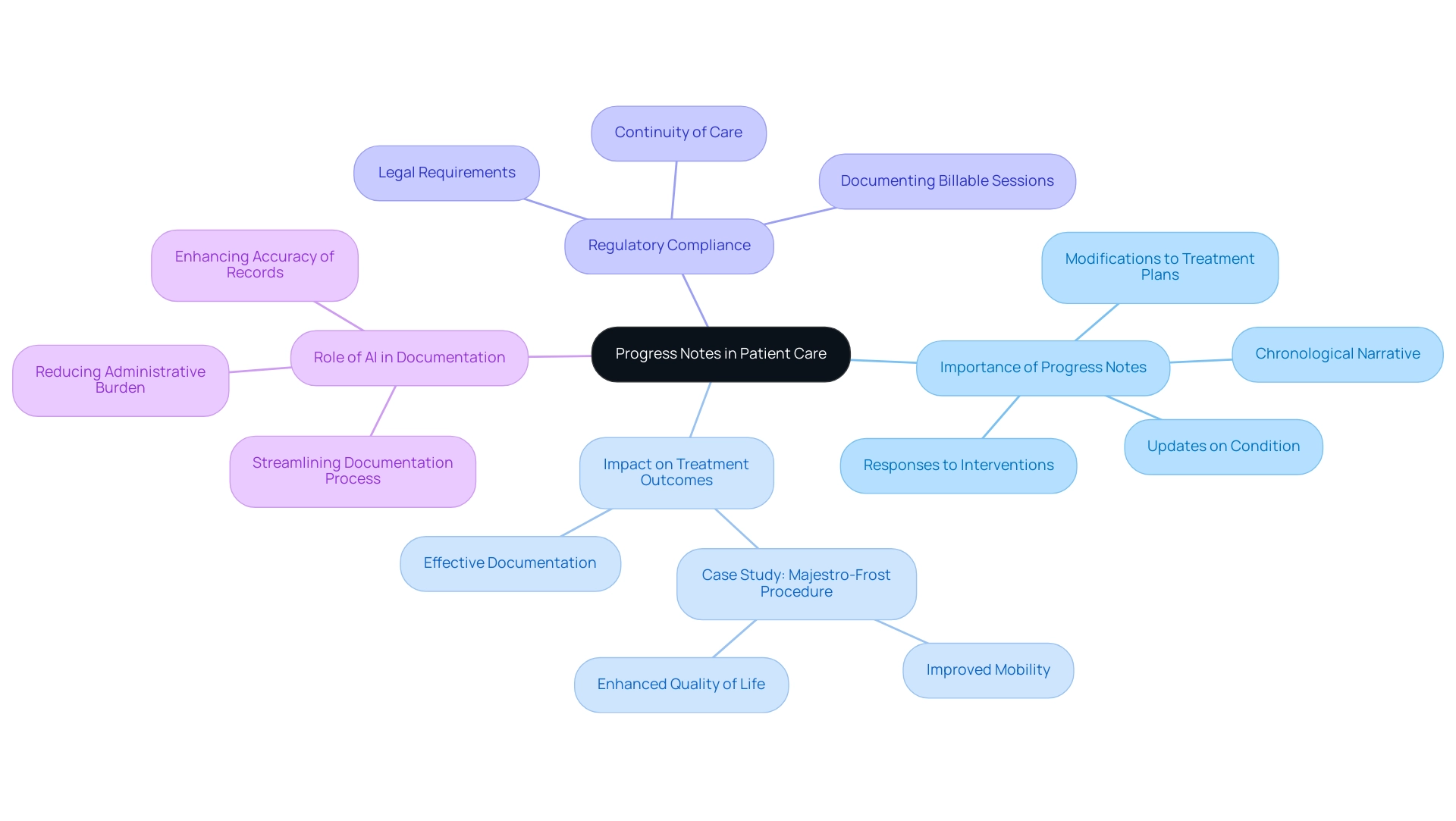
Progress Notes: Documenting Patient Progress
Progress notes are not just records; they represent a vital aspect of patient care, providing a comprehensive chronological narrative of an individual's treatment journey and progress. These notes should include updates on the individual's condition, responses to interventions, and any modifications to treatment plans. Consistently recording progress is crucial, as it enables healthcare professionals to assess the effectiveness of treatment, identify areas for improvement, and ensure that therapy aligns with the individual's goals.
In the context of the billion-dollar faith-focused healthcare market, where CosmaNeura stands as the only company creating AI solutions, the importance of progress notes becomes even more pronounced.
The impact of progress notes on client care is underscored by compelling statistics; for instance, consistent records are essential for maintaining continuity of care and meeting legal requirements. Clinicians must document every billable session and clinically significant contact to comply with these regulations. Furthermore, studies have shown that effective progress notes can significantly enhance treatment outcomes.
Consider a case study investigating the Majestro-Frost procedure on individuals with cerebral palsy. It revealed that meticulous recording of treatment effects led to improved mobility and quality of life, highlighting the direct connection between detailed progress notes and positive outcomes for those receiving care.
As the medical sector increasingly embraces AI innovations, the role of progress notes is becoming even more critical. AI-driven solutions can streamline the documentation process, ensuring that all relevant interactions and treatment responses are captured efficiently. This not only alleviates the administrative burden on medical providers but also enhances the accuracy and thoroughness of records.
Expert insights further reinforce the necessity of documenting client progress effectively. As noted by Adamo Software, "We also concentrate on improving security and legal compliance, ensuring that all progress notes are securely stored, and creating a modern, efficient, and reliable medical environment." By capturing detailed information about individual interactions and treatment responses, providers can create progress notes that foster better communication within the care team, ultimately leading to more coordinated and effective support.
In this way, progress notes not only contribute to but also play a vital role in enhancing overall outcomes, aligning with the transformative potential of AI in healthcare. Let us continue to prioritize the documentation of progress, ensuring that every patient's journey is accurately recorded and supported.
Therapy Notes: Essential for Mental Health Providers
Therapy notes play a vital role in the realm of mental health, capturing the nuances of therapy sessions and providing essential insights for providers. These notes encompass an individual's presenting issues, the therapeutic interventions employed, and their responses to treatment. By documenting these elements, therapy notes fulfill multiple purposes, such as tracking client progress, informing future sessions, and serving as a legal record of treatment.
Maintaining accurate and detailed therapy notes is paramount for several reasons:
- Continuity of Care: Comprehensive notes ensure that all providers involved in a patient's care are informed about previous sessions, facilitating seamless transitions and consistent treatment approaches.
- Treatment Effectiveness: Detailed documentation allows providers to assess the effectiveness of interventions over time, enabling adjustments to be made based on the individual's evolving needs. Research indicates that thorough therapy notes can significantly enhance treatment outcomes by providing a clear framework for evaluating progress.
- Legal Protection: In the event of disputes or inquiries, well-documented therapy notes serve as a legal safeguard, demonstrating the care provided and the rationale behind clinical decisions.
- Patient Engagement: As highlighted by Participant #74, "there actually is a right to see records- so you should always write your notes as if the patient would read it anyway." This perspective encourages transparency and fosters trust in the therapeutic relationship.
Interestingly, a statistic reveals that 7.8% of comments indicated no change in note-taking practices, underscoring the need for improvement in record-keeping methods within the field.
Case studies illustrate the profound impact of effective therapy notes on mental health care. Practices that emphasize meticulous documentation have reported improved outcomes and higher satisfaction rates among providers. By including essential elements such as treatment goals, session summaries, and client feedback, mental health professionals can create a robust record that supports both client treatment and the overall therapeutic process.
Moreover, CosmaNeura's innovative AI solutions have been shown to enhance healthcare delivery by automating administrative tasks. This allows providers to concentrate on patient support while adhering to ethical standards. By bridging gaps in documentation and improving access to services, CosmaNeura exemplifies how technology can support in their documentation practices, ultimately leading to enhanced patient-centric support and improved provider efficiency.
In summary, the significance of therapy notes in mental health support cannot be overstated. They are not just administrative tasks but essential elements that improve the quality of service, support continuity, and ultimately lead to better outcomes for individuals. Reflect on your current practices—how can you enhance your documentation to better serve your clients?
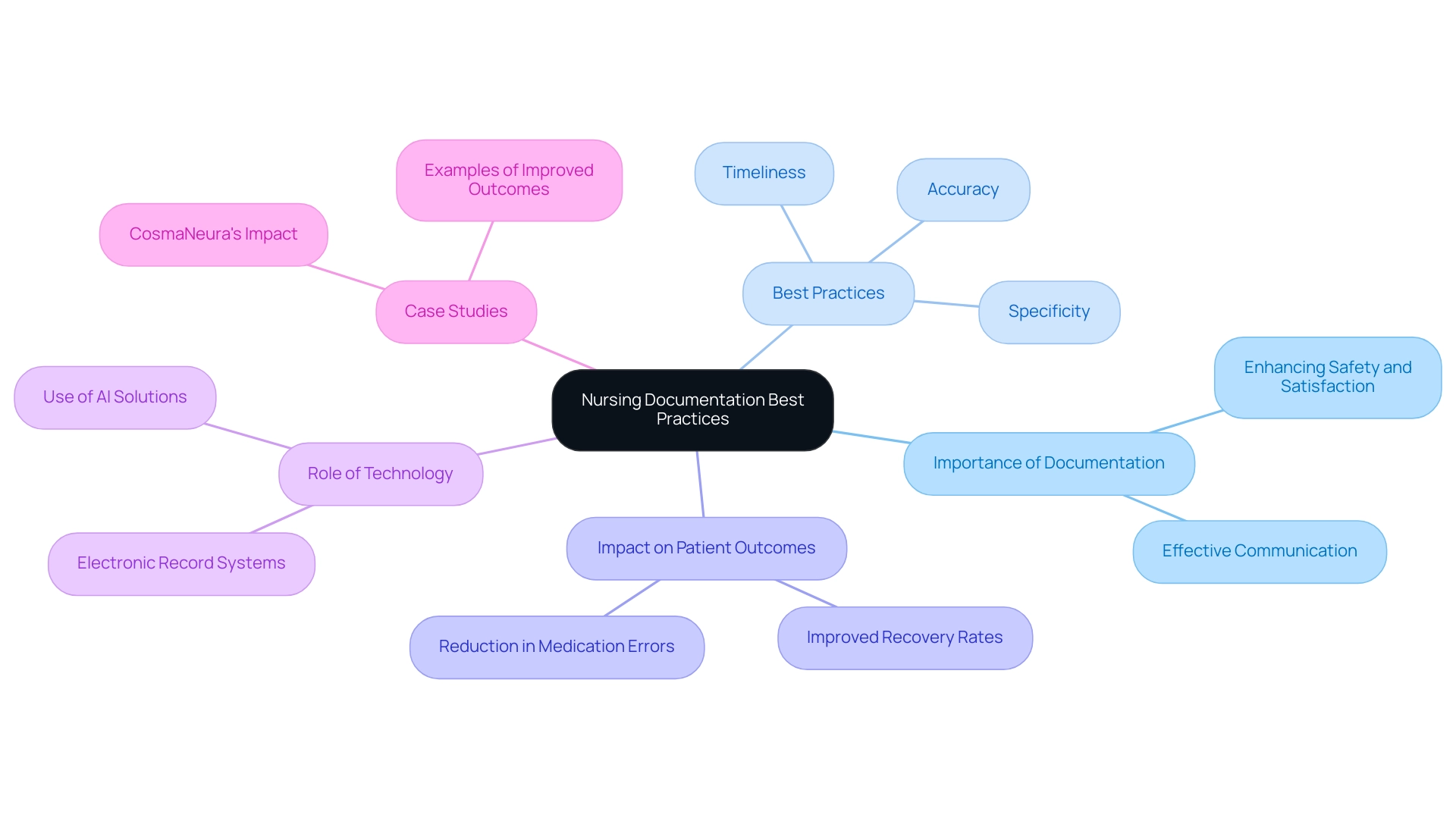
Nursing Care Notes: Best Practices for Documentation
Nursing documentation notes are not just a formality; they represent a vital aspect of , encompassing assessments, interventions, and individual responses. It's essential to adhere to best practices when writing patient notes; they should be timely, accurate, and specific. Nurses must capture not only the treatment administered but also the individual’s condition and any observed changes, exemplifying the importance of thorough patient notes.
This level of detail is crucial for effective communication among healthcare team members, ensuring that every aspect of individual support is comprehensively addressed. Prompt and precise nursing records significantly impact individual outcomes. Research indicates that well-documented patient notes can enhance safety and satisfaction, fostering better continuity of care. For instance, a recent study highlighted that healthcare workers utilizing electronic record systems reported improved accuracy and efficiency in their notes, ultimately benefiting patient care.
Importantly, the average age of individuals without harmful outcomes is 60.7 years ± 17.0, underscoring the necessity for tailored record-keeping practices that cater to diverse demographic groups.
Moreover, case studies illustrate the positive effects of diligent nursing records. In one instance, a medical facility that embraced organized documentation practices experienced a notable decrease in medication errors and an increase in recovery rates. This reinforces the role of nursing documentation as a crucial element of quality treatment, serving not only as a record-keeping tool but as a foundation for effective care.
CosmaNeura's innovative AI solutions are transforming medical service delivery by automating administrative tasks. This allows providers to focus on individual well-being while adhering to ethical standards, further emphasizing the importance of comprehensive records in improving healthcare outcomes.
By adopting optimal methods in nursing records, providers can significantly enhance the quality of service offered, leading to better outcomes for individuals and overall satisfaction. Efficient nursing records exemplify comprehensive evaluations that reflect individual progress and actions, clearly linking meticulous documentation to improved healthcare. Additionally, integrating AI solutions can help alleviate challenges such as service fragmentation and physician burnout by streamlining workflows and reducing the administrative burden on healthcare providers.
As Lisa R. shared, "I made the mistake of taking the quizzes toward the end of the week because I spent nearly every spare minute studying and reviewing, wanting to be sure I was ready. But no matter how much I studied, I didn’t do that well on the first go-round and sometimes I didn’t have time to retake the quizzes. I finally realized I needed to take it a little sooner so I could review the problems I missed. Then I did much better." This personal insight highlights the significance of timely and effective documentation practices in achieving optimal care for individuals.
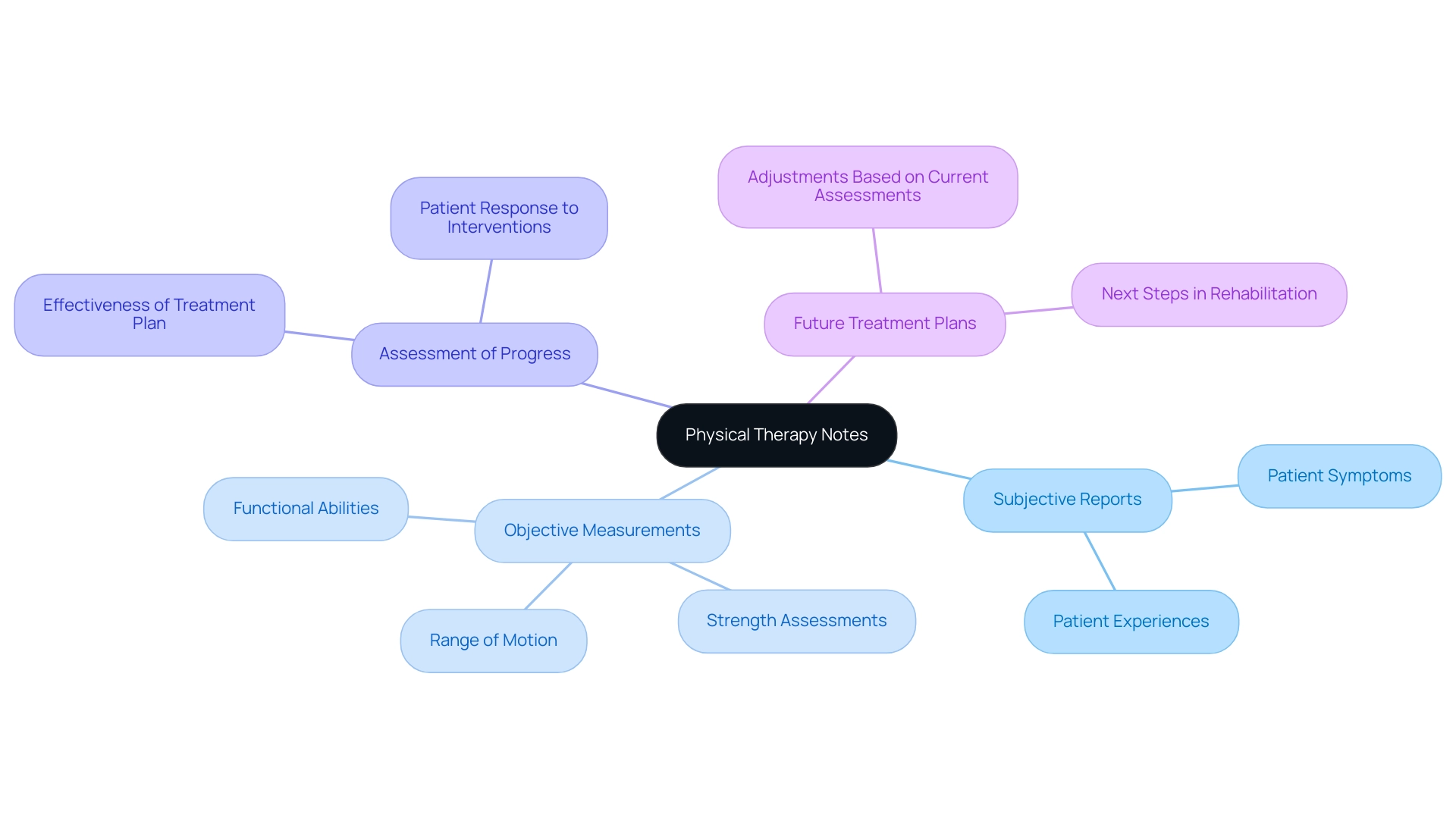
Physical Therapy Notes: Key Elements and Examples
are more than just records; they are a vital part of an individual's rehabilitation journey, documenting progress and guiding future treatment decisions. These notes include essential components such as the individual’s subjective reports, objective measurements, assessments of progress, and plans for ongoing treatment. Each entry should exemplify comprehensive and accurate documentation, reflecting the individual’s reactions to therapy and any modifications made to the treatment plan.
Research shows that diligent record-keeping can profoundly impact rehabilitation outcomes. For example, a study revealed that physical therapists who maintained detailed notes were better equipped to track client progress and adjust interventions effectively, leading to improved recovery rates. The Bureau of Labor Statistics anticipates a 28% expansion in the field of physical therapy from 2016 to 2026, underscoring the growing need for skilled professionals who can provide high-quality support backed by thorough record-keeping practices.
Key elements of effective physical therapy notes include:
- Subjective Reports: Capturing the individual’s own descriptions of their symptoms and experiences.
- Objective Measurements: Documenting quantifiable data such as range of motion, strength, and functional abilities.
- Assessment of Progress: Evaluating the treatment plan’s effectiveness and the individual’s response to interventions.
- Future Treatment Plans: Outlining the next steps in the rehabilitation process based on current assessments.
By prioritizing comprehensive record-keeping, healthcare providers can meet rehabilitation goals while enhancing patient satisfaction and outcomes. The integration of AI-driven solutions, like those developed by CosmaNeura, can further improve these practices, allowing providers to focus on delivering high-quality services while ensuring that all essential information is accurately noted. For instance, AI tools can help alleviate challenges like service fragmentation, making it easier for providers to access pertinent individual information and enhancing communication and coordination.
Moreover, AI can help reduce physician burnout by automating repetitive record-keeping tasks, enabling medical professionals to spend more time engaging directly with clients.
Physical therapists in home health services, who often provide personalized assistance, earned a median annual salary of $99,710 as of May 2023. This reflects the value placed on their expertise and the crucial role of their records in ensuring effective treatment. Additionally, with individuals often required to pay a copayment of 10 euros per prescription along with 10% of treatment costs, comprehensive records become essential in justifying treatment expenses and optimizing billing practices. By embracing AI advancements, CostaNera aims to enhance documentation practices, ultimately improving care and addressing the broader challenges faced in medical delivery.
Care Plans: Structuring Patient Management
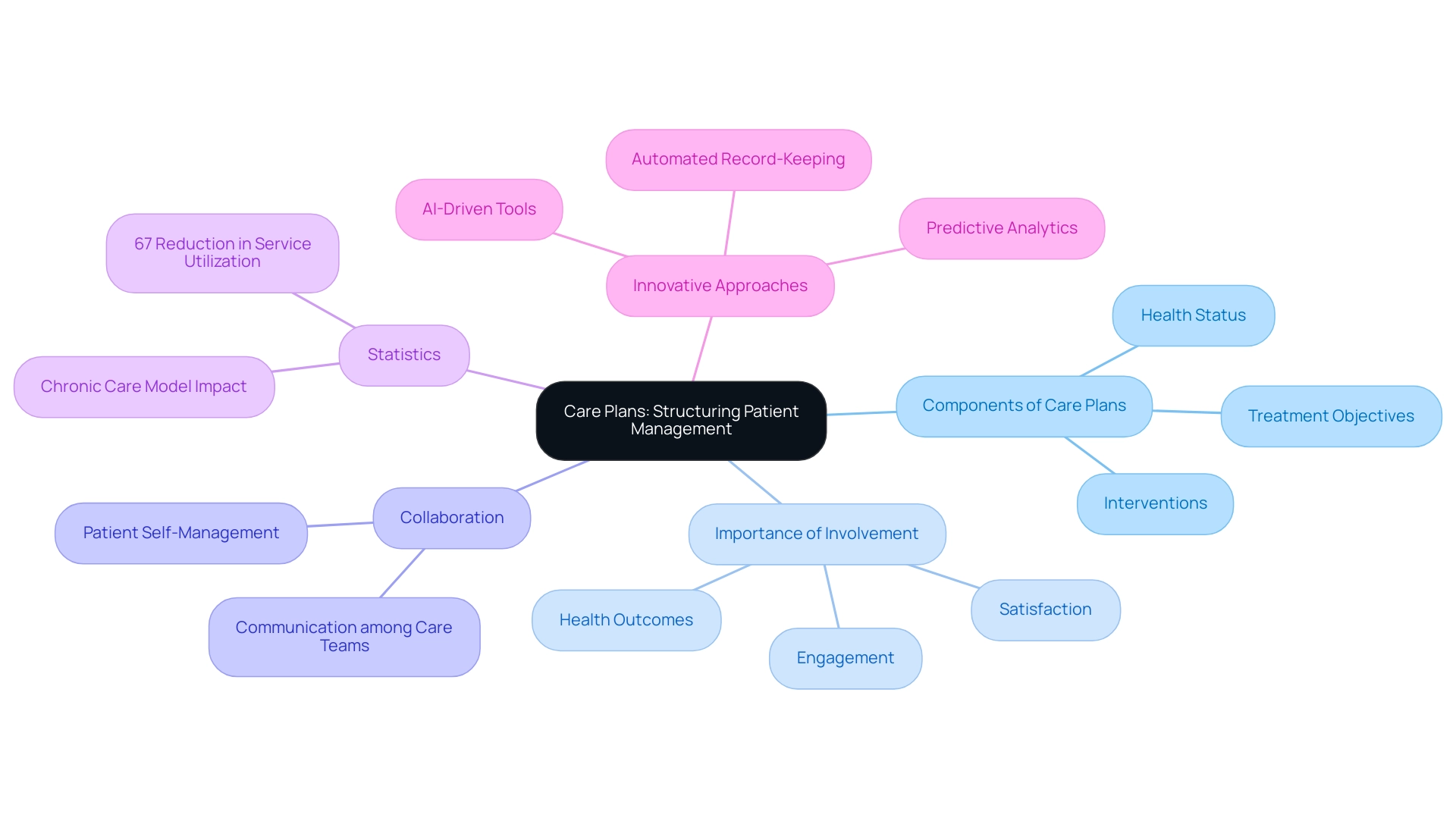
Care plans are essential documents that comprehensively outline an individual's health status, treatment objectives, and the necessary interventions to achieve those goals. They serve as a strategic roadmap for healthcare providers, ensuring that all team members are aligned with the individual's needs and the approaches in place to address them. Frequent evaluations and modifications of treatment plans are vital, as they enable changes based on the individual's progress and changing needs.
Involving individuals in the planning process significantly boosts their engagement and satisfaction. Have you noticed how efficient management strategies can enhance communication among support teams? This approach enables individuals in self-management, ultimately resulting in improved health outcomes. A significant case study named 'Impact of Plans on Individual Management' emphasizes how plans function as extensions of medical records and agreements between individuals and medical providers.
The findings suggest that well-structured treatment plans not only enhance management continuity but also ensure that treatment decisions are clearly documented and understood by all parties involved.
Statistics further emphasize the effectiveness of treatment plans in management, with 67% of studies indicating reductions in service utilization or expenses linked to the Chronic Care Model. This model highlights the significance of organized treatment plans in promoting improved outcomes for individuals and maximizing resource utilization. The study is registered under ClinicalTrials.gov Identifier: NCT02992431, providing credibility to the findings discussed.
To create effective treatment plans, healthcare providers should focus on clear structuring, incorporating specific goals, measurable outcomes, and defined interventions. Expert insights suggest that a collaborative approach, where individuals actively engage in , can lead to increased satisfaction and adherence to treatment protocols. As mentioned by Swinglehurst et al., the use of computer templates in chronic disease management influences 'how disease is defined; how assistance is delivered; what it means to be a recipient of treatment; and what it means to be a clinician.'
By prioritizing client involvement and utilizing AI-driven tools, such as predictive analytics and automated record-keeping systems, providers can significantly enhance user engagement, streamline workflows, and ultimately improve overall satisfaction with their care experience. Moreover, tackling challenges such as the fragmentation of healthcare systems and increasing costs through innovative care planning can result in more efficient resource allocation and enhanced outcomes for individuals.
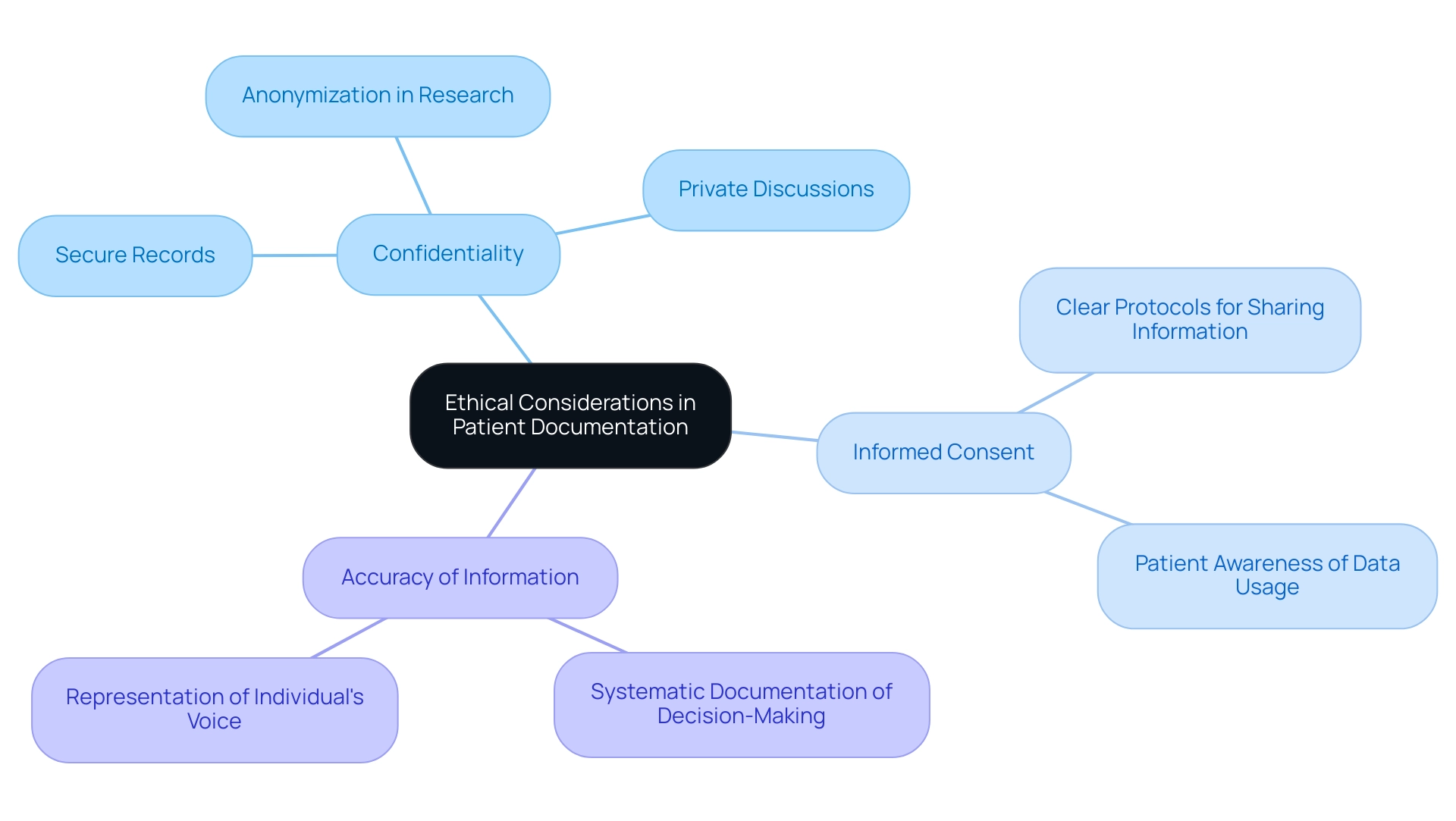
Ethical Considerations in Patient Documentation
Ethical considerations in documentation are essential, encompassing confidentiality, informed consent, and the accuracy of recorded information. Healthcare providers must prioritize the security of medical records, ensuring that sensitive information is disclosed only to authorized individuals. This commitment is especially vital in faith-oriented healthcare settings, where adherence to ethical standards not only strengthens compassionate service but also aligns with the moral teachings of the Catholic faith.
Documentation should genuinely represent the individual's voice and preferences, promoting autonomy and respect. Have you considered how systematic documentation of decision-making processes can enhance transparency and accountability, particularly in critical situations like out-of-hospital cardiac arrests? This approach not only improves the quality of care but also fosters trust between patients and providers. Confidentiality plays a vital role in maintaining that trust.
Statistics reveal that individuals are significantly more inclined to share their health data with medical professionals than with government agencies. This underscores the importance of a secure and trustworthy environment. Experts emphasize that maintaining confidentiality and obtaining informed consent are foundational to ethical medical practices. For example, providers can implement clear protocols for sharing information, ensuring that individuals are fully informed about how their data will be used.
Real-world examples of maintaining confidentiality include anonymizing records during research and ensuring that discussions about care occur in private settings. By prioritizing these ethical considerations, healthcare providers not only comply with legal requirements but also enhance . This fosters a culture of trust and respect in their practice. Furthermore, as highlighted in the case study, the impact of these practices can be profound.
Conclusion
Effective patient documentation is fundamental to delivering high-quality healthcare. It’s essential to recognize the emotional challenges faced by healthcare providers in this demanding environment. Throughout this article, we have explored the critical roles of various documentation formats—including SOAP, DAP, and SBAR notes. These structured approaches not only enhance communication and continuity of care but also provide legal protection, ultimately leading to improved patient outcomes.
Have you ever felt overwhelmed by administrative tasks? The integration of innovative technologies, such as those provided by CosmaNeura, has emerged as a transformative force in healthcare documentation. By automating these burdens, these solutions empower healthcare providers to focus more on meaningful patient interactions. This shift increases efficiency and significantly enhances the overall quality of care delivered to those we serve.
As we navigate the evolving healthcare landscape, the importance of meticulous documentation practices remains paramount. By prioritizing structured documentation and embracing technological advancements, healthcare professionals can foster stronger relationships with their patients. This ensures that care is not only effective but also ethically sound. Remember, robust documentation practices are not just about compliance; they are essential for cultivating trust, improving health outcomes, and advancing the overall quality of patient care in a rapidly changing environment. Let us commit to these practices together, for the benefit of our patients and the integrity of our profession.




