Overview
In the demanding world of healthcare, writing effective doctors' notes is crucial. These notes are not just administrative tasks; they are vital components of patient care that significantly impact the well-being of those we serve. Have you ever felt overwhelmed by the burden of documentation? You're not alone. Many healthcare providers face this challenge, and it can detract from the time spent with patients.
Understanding the key elements of effective documentation can alleviate some of this pressure. Accurate documentation, confidentiality, and the thoughtful integration of technology are essential. By focusing on these components, we can enhance continuity of care, ensure patient safety, and improve overall healthcare efficiency. Imagine a system where your notes seamlessly support patient care rather than hinder it.
The benefits of adopting best practices in writing doctors' notes are profound. Not only do they foster better communication among healthcare providers, but they also ensure legal compliance, which is critical in our field. By embracing these practices, we can create a more supportive environment for both patients and providers.
Let’s take action together. Consider how you can implement these strategies in your daily practice. Reflect on your current documentation process and identify areas for improvement. By doing so, you contribute to a more compassionate and efficient healthcare system, ultimately benefiting those who rely on our care.
Introduction
In the intricate world of healthcare, doctors' notes are not just routine documentation; they are the backbone of effective patient care. These notes encompass a wealth of information that captures the nuances of patient encounters, from medical histories to treatment plans. They play a vital role in ensuring continuity of care across various healthcare providers. As we embrace patient engagement initiatives and integrate technology, the significance of these notes has never been more pronounced.
As healthcare evolves, we must understand the multifaceted role of doctors' notes. How can we enhance patient outcomes and foster a collaborative environment between patients and providers? This article delves into the critical components, challenges, and best practices associated with writing effective doctors' notes. By highlighting their impact on patient safety and care quality, we aim to shed light on their essential role in today's dynamic healthcare landscape. Together, let’s explore how we can improve our practices for the benefit of our patients.
Understanding the Purpose of Doctors' Notes
Writing doctors' notes is indispensable in the medical landscape, serving critical functions that extend beyond mere documentation. These notes capture detailed accounts of encounters, encompassing medical history, symptoms, diagnosis, and treatment plans. This comprehensive record is essential for ensuring continuity of care, allowing other healthcare providers to access vital information that informs ongoing treatment strategies.
Have you ever considered how effective documentation can enhance patient engagement and satisfaction? Recent studies emphasize this importance. For instance, a pilot initiative known as OurNotes invited individuals with chronic illnesses to review their medical records and contribute semi-structured histories before their visits. This co-production of medical records not only aimed to improve care quality but also sought to reduce costs by fostering better communication between individuals and clinicians.
The pilot testing of OurNotes demonstrates the practical consequences of engaging patients in their medical records, potentially resulting in better outcomes. Moreover, writing doctors' notes is crucial in legal contexts; they serve as formal evidence of the care provided and the rationale behind clinical decisions. The American Medical Association (AMA) underscores the necessity of compliance with information blocking regulations, highlighting the need for healthcare providers to maintain transparent and accessible record-keeping practices. The AMA also offers a continuing medical education module to help physicians understand and comply with these regulations, reinforcing the importance of proper documentation when writing doctors' notes.
Statistics indicate that the relative risk of individuals accessing their records remains significant. Findings show that certain demographics, such as black and multiracial individuals, may interact with their documents less frequently. Specifically, the relative risk of BIDMC individuals accessing records in the final quarter of year 2 was 0.94. This emphasizes the necessity for medical professionals to contemplate how writing doctors' notes can be customized to improve accessibility and involvement among various patient groups.
As we look ahead to 2025, the role of writing doctors' notes continues to evolve, with an increasing focus on their impact on continuity of care. By utilizing generative AI, like the solutions provided by CosmaNeura, medical providers can simplify administrative tasks, thus improving the effectiveness of record-keeping processes. Features like automated note-taking, real-time data integration, and enhanced communication tools can significantly improve the clinician-individual relationship.
Practical examples demonstrate how comprehensive records not only enhance outcomes for individuals but also fortify the clinician-individual relationship, ultimately resulting in greater job satisfaction for providers of medical services. As John N Mafi, MD, MPH, noted, "doing this in a structured data framework might be helpful, although I think it should not prevent the individual from expressing their narrative or story." By acknowledging the multifaceted significance of writing doctors' notes and incorporating advanced communication strategies, healthcare professionals can better understand the value of meticulous and precise documentation in their practice.

Key Components of Effective Doctors' Notes
Effective writing of doctors' notes is crucial for ensuring high-quality care and maintaining accurate medical records. Have you ever considered how these notes can impact patient outcomes? To achieve this, the following key components should be meticulously documented:
- Client Information: Clearly state the individual's name, age, and relevant medical history. This foundational information is essential for contextualizing the individual's current health status and guiding future care decisions.
- Chief Complaint: Accurately document the primary reason for the individual's visit. This should be a concise statement that captures the individual's main concern, allowing for focused assessment and treatment.
- Assessment: Summarize the individual's condition by integrating both subjective reports (what the individual describes) and objective findings (clinical observations and test results). This comprehensive overview aids in forming a clear clinical picture and informs the subsequent treatment plan. For instance, the Framingham Heart Study calculated that participants with hypertension are 1.40 times more likely to experience syncope, highlighting the importance of thorough documentation in managing such conditions.
- Plan: Outline a detailed treatment plan that includes prescribed medications, referrals to specialists, and scheduled follow-up appointments. This section should also address any education provided to individuals, ensuring that they understand their care pathway.
- Date and Signature: Each record must be dated and signed by the medical provider. This not only confirms the records but also sets a timeline for the individual's care, which is essential for continuity and legal reasons.
Integrating these elements into physicians' records not only boosts interaction among healthcare professionals but also enhances outcomes for individuals when writing doctors' notes. A case study analyzing the prevalence of metabolic syndrome among Americans estimated that 47 million Americans are affected, underscoring the necessity of effective note-taking in addressing widespread health issues.
Furthermore, as Peter Elias remarked, "When individuals observe what physicians record, it makes the difficult discussions crucial," highlighting the significance of openness in records and its effect on provider interaction.
Moreover, following interoperability standards in health IT systems is essential for guaranteeing that these records can be exchanged and comprehended across various platforms, thus improving data quality and safety for individuals. By adhering to these best practices, medical providers can significantly enhance their processes for writing doctors' notes, ultimately resulting in improved care and satisfaction for individuals.
Legal and Ethical Considerations in Writing Doctors' Notes
When writing doctors' notes, healthcare providers face a complex landscape of legal and ethical factors that are crucial for maintaining patient trust and ensuring compliance with regulations. How can we navigate this challenging terrain while prioritizing patient care?
- Confidentiality is paramount. Safeguarding patient information and sharing it only with authorized personnel is essential. With the increasing digitalization of healthcare data, HIPAA breaches have become more prevalent, with human error accounting for 43% of these incidents. This statistic underscores the importance of stringent confidentiality measures to mitigate risks associated with human oversight.
- Accuracy in documentation is vital. Truthfully and accurately recording individual information prevents misrepresentation of care. Faulty documentation not only leads to significant legal repercussions but also undermines the quality of care that patients deserve.
- Compliance with laws and regulations, particularly HIPAA, is non-negotiable. Adhering to these standards safeguards individual privacy and protects medical providers from potential legal responsibilities. Consider this: ransomware attacks have resulted in a staggering $157 million in losses for the medical sector since 2016. This highlights the financial risks associated with non-compliance. As illustrated in the case study 'Causes and Impacts of Healthcare Data Breaches,' breaches can lead to substantial financial losses, erosion of trust, and reputational damage to healthcare organizations.
- Informed Consent is another critical aspect. Obtaining consent from individuals before sharing medical information with third parties fosters transparency and reinforces the ethical obligation to respect individual autonomy. How can we ensure that our practices reflect this commitment?
In light of these considerations, medical providers must implement comprehensive security measures and conduct regular audits to protect patient information. The study found that outdated security software and weak passwords are common reasons for data breaches in healthcare, emphasizing the vulnerabilities that providers face. Furthermore, as Steve Alder, editor-in-chief of The HIPAA Journal, states, "It is necessary to prove the breach notification requirements are complied with to ensure covered entities and business associates do not overlook notifying individuals in the required timeframe."
By prioritizing ethical record-keeping practices, providers can enhance the quality of care while ensuring compliance with legal standards. Let’s work together to create a safer, more trustworthy healthcare environment for everyone.
Common Challenges in Writing Doctors' Notes and How to Overcome Them
Healthcare providers often face numerous challenges when it comes to writing doctors' notes, which can deeply impact both care and administrative efficiency.
- Time Constraints: Have you ever felt overwhelmed during office visits? A staggering half of physicians report feeling time pressure, often resulting in incomplete or hurried records. To alleviate this stress, consider using templates or dictation software for note-taking. This approach not only simplifies the process but also allows providers to focus more on client interactions while ensuring thorough documentation. Cosmonaut's administrative efficiency features, including telehealth transcription services, can help automate record-keeping tasks, easing these pressures.
- Complex Medical Terminology: The intricate jargon can create barriers between medical providers and patients. It's essential to prioritize clear and concise language that fosters understanding and enhances communication among the care team.
- Inconsistent Documentation Practices: Have you noticed variability in note formats? This inconsistency can lead to confusion and compromise the quality of care. Standardizing documentation practices improves clarity and boosts the overall efficiency of the medical team in writing doctors' notes. Regular training sessions can reinforce best practices, ensuring that all staff members are aligned in their record-keeping efforts.
- Expert Insights: The sustainability of practice is at risk when providers feel overburdened. Urmimala Sarkar emphasizes that long hours are not sustainable, which is why none of the providers in her practice work full-time. Exploring options like reducing workloads or pursuing nonclinical positions can help alleviate some of the stresses associated with record-keeping, allowing providers to maintain their passion for care. CosmaNeura's platform supports these sustainable practices by minimizing administrative burdens.
- Case Studies: What strategies have you seen emerge from primary care practices? Many providers have successfully transitioned to part-time work or alternative care models, showcasing proactive approaches to managing workloads while ensuring quality interactions with clients. These case analyses underline the importance of adapting to challenges, aligning with CosmaNeura's mission to enhance medical service delivery.
By addressing these challenges head-on and implementing effective solutions, such as those offered by CosmaNeura, medical providers can refine their record-keeping practices. This ultimately leads to improved care for individuals and greater job satisfaction, all while adhering to ethical principles rooted in Catholic teachings.
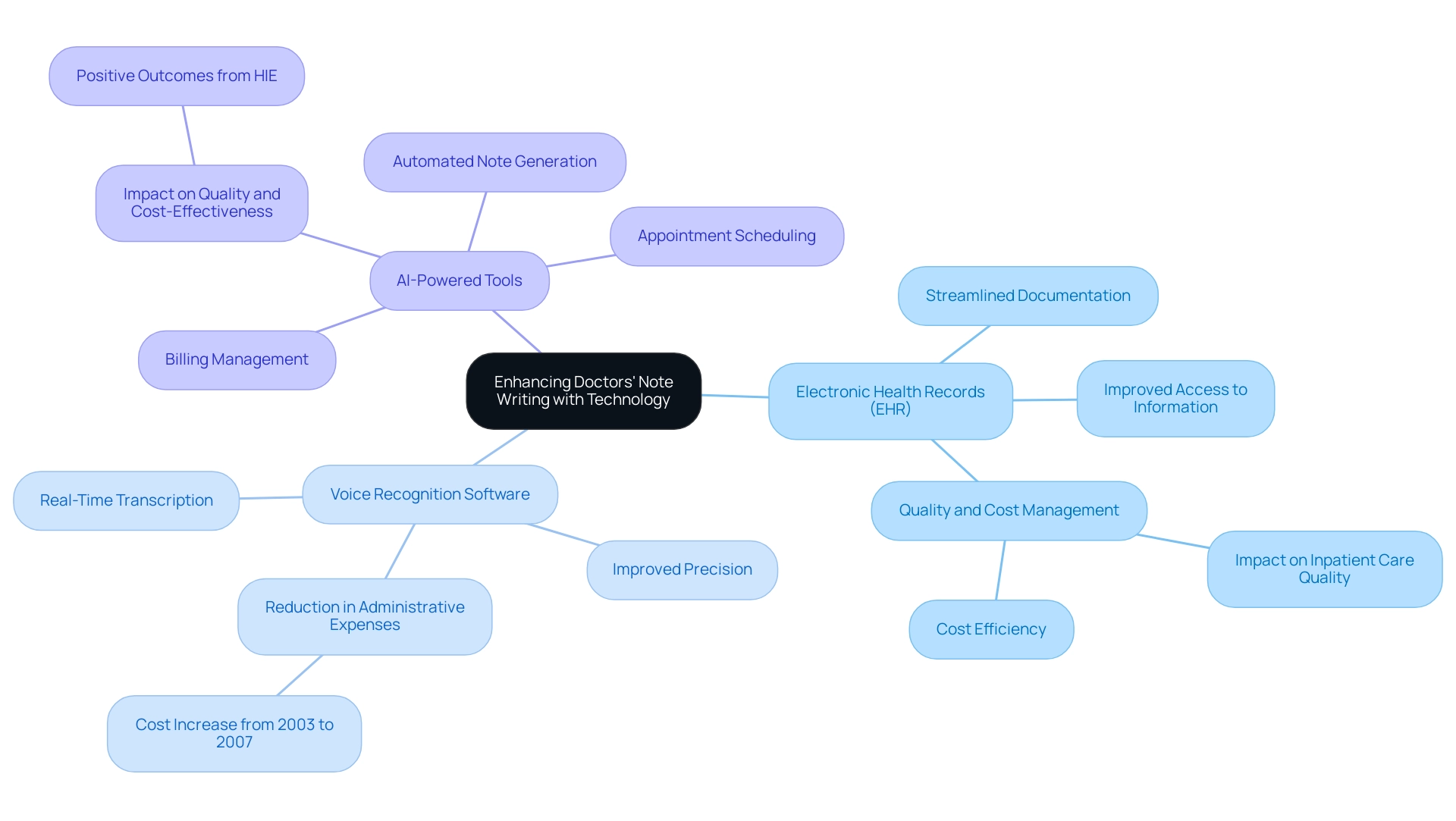
Leveraging Technology to Enhance Doctors' Note Writing
In today's fast-paced healthcare environment, technology plays a vital role in alleviating the stress of writing doctors' notes. By streamlining administrative tasks, healthcare providers can focus more on what truly matters: patient care. Have you ever felt overwhelmed by the documentation demands? You're not alone. Here are several effective strategies to leverage technology for improved documentation:
- Electronic Health Records (EHR): Implementing EHR systems can significantly streamline the documentation process. These systems offer easy access to comprehensive client information and customizable templates, facilitating quicker and more organized note-taking. Studies indicate that the adoption of EHRs has led to improved documentation efficiency, with many healthcare providers reporting a reduction in time spent on administrative tasks. As noted by Jürgen Stausberg, MD, in the Journal of Medical Internet Research, "The research questions were twofold. What is the effect of EMs on the quality of inpatient care? What is the effect of EMs on the costs for inpatient care?" This emphasizes the essential function of EHRs in both quality and cost management, ultimately improving care for individuals.
- Voice Recognition Software: The integration of voice-to-text technology allows clinicians to transcribe notes in real-time during or right after interactions with individuals. This approach not only speeds up the record-keeping process but also improves precision, capturing the nuances of client interactions without the delay of manual entry. Research indicates that hospitals have experienced a reduction in administrative expenses, which increased from 24.4% in 2003 to 24.9% in 2007, emphasizing the necessity for efficient documentation practices to manage escalating costs and ease the burden on providers.
- AI-Powered Tools: Utilizing AI-driven tools, such as those offered by CosmaNeura, can further optimize the note-writing process. These advanced technologies can analyze interactions and generate comprehensive notes, ensuring that all relevant information is captured accurately. Specific features of CosmaNeura's solutions include automated appointment scheduling and billing management, streamlining these administrative tasks and freeing up time for medical providers. By automating aspects of the documentation process, medical providers can reclaim valuable time that can be redirected towards direct patient care. The impact of such technologies is emphasized by case studies demonstrating that health information exchanges (HIE) have positively influenced both the quality of care and cost-effectiveness in medical environments, with many studies showing significant improvements.
As we look to the future, the landscape of writing doctors' notes continues to evolve with technology, offering innovative solutions that enhance efficiency and accuracy. By adopting these tools, healthcare providers can improve their record-keeping practices, ultimately leading to better patient outcomes and increased job satisfaction. Together, let's embrace these advancements to create a more compassionate healthcare experience.
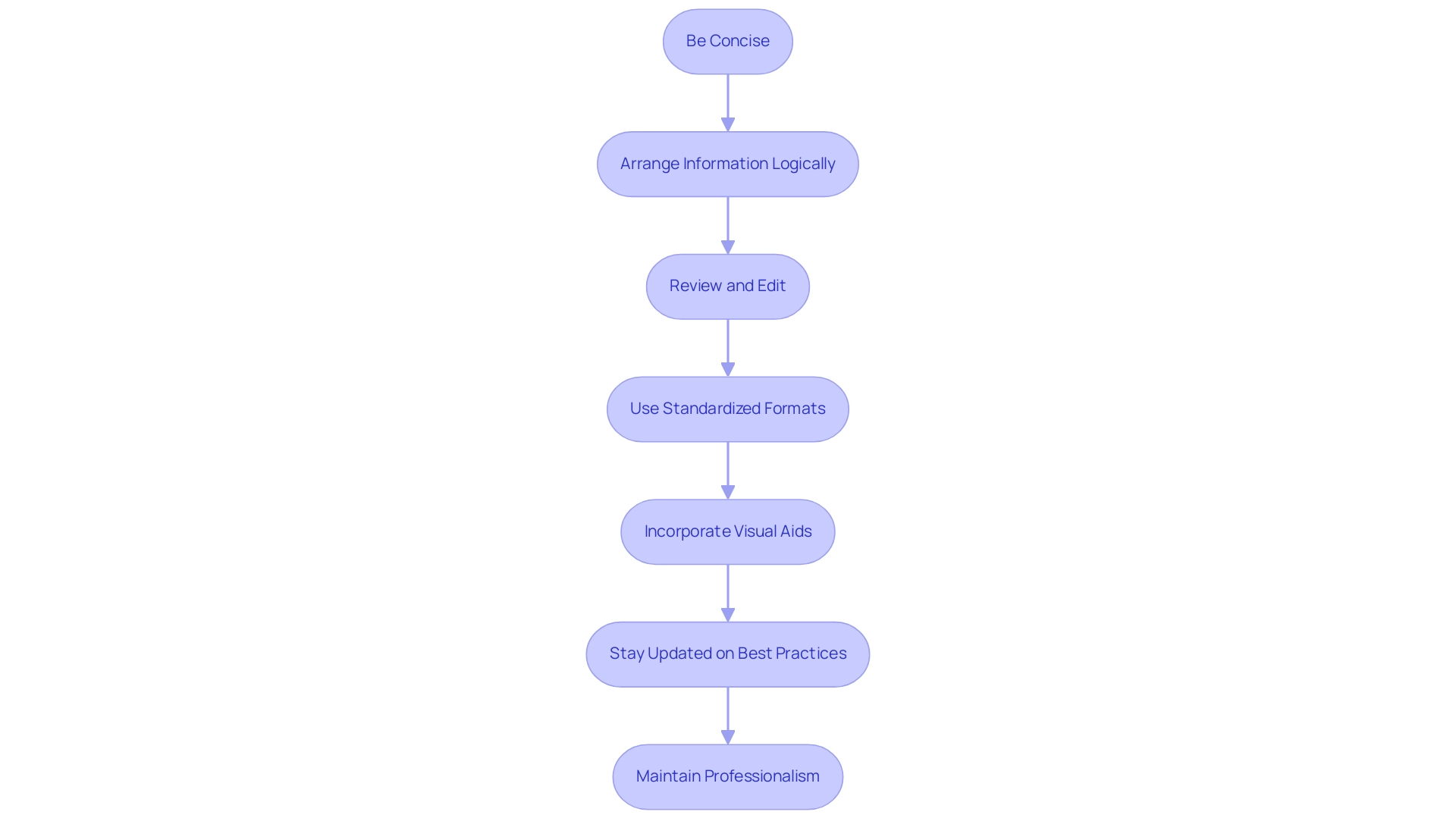
Best Practices for Writing Clear and Effective Doctors' Notes
Writing clear and effective doctors' records can be challenging, but with a few best practices, you can make this process easier and more efficient.
- Be Concise: Use straightforward language and remove unnecessary details that may clutter your records. Brief entries not only reflect the quality of care provided but also save valuable time later. This highlights the importance of maintaining precise and thorough medical files.
- Arrange Information Logically: Structure your entries in a coherent manner, ensuring a logical flow that allows others to follow easily. This organization is crucial for effective communication among healthcare providers, fostering collaboration and understanding.
- Review and Edit: Always take a moment to review your records for clarity and accuracy before finalizing them. This practice helps catch errors and enhances the overall quality of your documentation.
- Use Standardized Formats: Adopting standardized formats, such as SOAP (Subjective, Objective, Assessment, Plan), can significantly improve consistency and clarity in your records. These formats enhance the quality of medical documentation, making it easier for others to interpret and utilize.
- Incorporate Visual Aids: Consider utilizing visual aids like graphs and charts when appropriate. Research on visual aids in reporting shows their effectiveness in making statistical reports more engaging and easier to interpret, which can be beneficial in clinical records as well.
- Stay Updated on Best Practices: As we approach 2025, it’s essential to remain informed about evolving best practices for writing doctors' notes effectively. Engaging with recent literature and expert advice can provide valuable insights into enhancing your record-keeping skills.
- Maintain Professionalism: In situations where someone requests records that may not be justified, it’s important to uphold professionalism. Openly discuss any concerns with the individual, providing suitable medical guidance and alternative solutions while ensuring that your records remain precise and ethical. As Dr. Dave Nicholas observes, maintaining professionalism in these interactions is vital for preserving the integrity of medical records.
By embracing these best practices, you can enhance the quality of your records, which is especially important in the context of Cosmonauts, the only company developing AI solutions for the billion-dollar faith-focused medical market. Your efforts in improving record-keeping not only benefit your practice but also significantly impact patient care.
The Impact of Effective Doctors' Notes on Patient Care
Effective writing of doctors' notes plays a crucial role in enhancing patient care across multiple dimensions:
- Improved Continuity of Care: Comprehensive and well-documented notes ensure that all healthcare providers involved in a patient's treatment have access to accurate information. This seamless sharing of data facilitates informed decision-making, which is essential for coordinated care.
- Enhanced Patient Safety: Clear and precise records significantly reduce the risk of errors and miscommunication. In fact, documentation errors in the United States contribute to at least one death and 1.3 million injuries annually. By reducing these risks, efficient records contribute to safer care environments, highlighting the vital significance of thorough documentation.
- Enhanced Engagement of Individuals: When individuals can easily comprehend their medical records, they are more inclined to take an active part in their healthcare. This engagement fosters better adherence to treatment plans, ultimately resulting in improved health outcomes. Increasing understanding of educational tools in health portals can further improve individual knowledge and confidence in managing their well-being.
- Expert Insights: Research suggests that strategies aimed at minimizing document clutter should concentrate on various elements, including the layout of document templates and clinician training. Such enhancements can improve the quality of records, further benefiting care for individuals. As Dr. Bell notes, addressing these factors is essential for enhancing record-keeping practices.
- Case Studies: The implementation of innovative platforms like CosmaNeura demonstrates the transformative impact of AI on record-keeping practices. By alleviating administrative burdens, these solutions empower healthcare providers to concentrate on interactions with individuals, addressing the concerns of risk-averse doctors and enhancing job satisfaction. CosmaNeura's method demonstrates how efficient documentation practices can be incorporated into daily workflows, ultimately resulting in enhanced care for individuals.
- Examples of Improved Safety: Enhanced documentation practices have been associated with better outcomes for individuals. For instance, writing doctors' notes in a streamlined manner can help prevent medication errors and ensure that critical patient information is readily available during care transitions. In summary, effective writing of doctors' notes is not merely an administrative task; it is foundational to delivering high-quality, safe, and patient-centered care.
Conclusion
Effective doctors' notes are not just administrative tasks; they are pivotal in shaping the quality of patient care in our healthcare system. These notes serve multiple essential functions: they capture detailed accounts of patient encounters, foster continuity of care, and enhance communication among healthcare providers. By integrating patient engagement initiatives and leveraging technology—such as electronic health records and AI-powered tools—healthcare professionals can significantly improve the accuracy and efficiency of documentation.
The importance of adhering to best practices in writing doctors' notes cannot be overstated. Key components, including clear patient information, a concise chief complaint, a thorough assessment, and a well-structured plan, contribute to effective documentation. This not only enhances communication but also ensures legal compliance and ethical standards. Overcoming common challenges—like time constraints and complex medical terminology—through streamlined processes and standardized formats can further support our goal of delivering high-quality patient care.
Ultimately, the impact of effective doctors' notes extends far beyond administrative tasks; they are integral to improving patient safety, engagement, and overall health outcomes. As the healthcare landscape evolves, prioritizing meticulous documentation empowers healthcare providers to deliver exceptional care. This fosters a collaborative environment that benefits both patients and clinicians alike. Embracing these practices is essential for navigating the complexities of modern healthcare and ensuring that patient care remains at the forefront.
How can we ensure that our documentation reflects the compassion we bring to our patient interactions? Let's commit to making our notes not just a requirement, but a vital part of the caring process.




