Overview
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver optimal patient care. The article highlights the significance of SOAP notes, offering a comprehensive guide to their effective use in documentation. By embracing structured SOAP documentation, healthcare professionals can enhance communication among themselves, leading to improved clinical decision-making. This nurturing approach ultimately fosters better patient outcomes.
Evidence supports this notion, revealing a remarkable 30% increase in clinical evaluation precision when organized SOAP notes are utilized. Imagine the difference this could make in your daily practice! With these tools at your disposal, you can alleviate some of the administrative burdens that often hinder your focus on patient care.
Consider the benefits:
- clearer communication
- enhanced collaboration
- most importantly, improved patient outcomes
As you reflect on your current documentation practices, think about how adopting structured SOAP notes could transform your interactions with colleagues and patients alike.
We encourage you to explore the potential of SOAP notes further. By doing so, you not only enhance your own practice but also contribute to a supportive healthcare environment that prioritizes patient well-being. Together, we can make a meaningful impact on the lives of those we serve.
Introduction
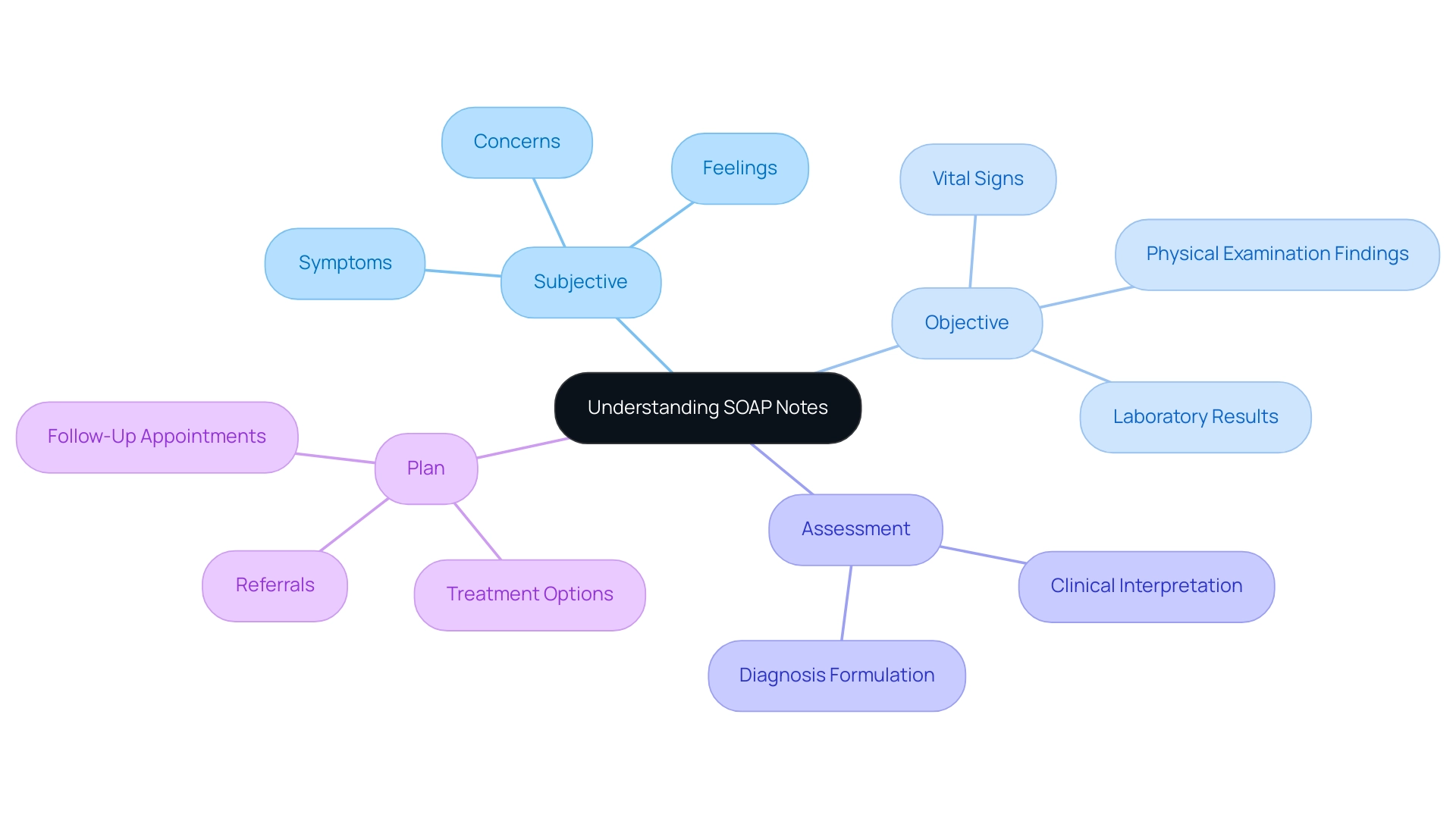
In the realm of healthcare, effective communication is not just important; it is essential. One of the most vital tools in achieving this is the SOAP note. This structured documentation method streamlines the recording of patient encounters and enhances the quality of care delivered. Comprising four key components—Subjective, Objective, Assessment, and Plan—SOAP notes provide a comprehensive framework for healthcare providers to capture essential information about their patients.
As the healthcare landscape evolves, the significance of accurate and clear documentation becomes even more pronounced. It influences everything from clinical decision-making to legal protection. Have you ever felt overwhelmed by administrative burdens that detract from patient care? Exploring the intricacies of SOAP notes reveals their crucial role in fostering continuity of care, improving patient outcomes, and supporting healthcare professionals in their mission to deliver high-quality care.
By embracing SOAP notes, healthcare providers can alleviate some of these challenges, ensuring that they focus on what truly matters—their patients. Let’s delve deeper into how this vital tool can transform your practice and enrich the patient experience.
Understanding SOAP Notes: Definition and Purpose
SOAP notes nursing represent a compassionate approach used by healthcare professionals to thoughtfully document client interactions. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, with each element playing a vital role in the documentation process:
- Subjective: This section captures the individual's perspective, including their symptoms, feelings, and concerns, providing valuable context for the medical provider.
- Objective: Here, measurable data is recorded, such as vital signs, physical examination findings, and laboratory results, which are crucial for an accurate clinical assessment.
- Assessment: This component offers a clinical interpretation of the subjective and objective data, allowing providers to synthesize information and formulate a diagnosis.
- Plan: The final section outlines the next steps in care, including treatment options, referrals, and follow-up appointments.
Understanding this structure is essential for effective communication among medical providers and for maintaining accurate records. Organized records like SOAP have been shown to significantly enhance medical organizations' ability to monitor billing and improve cash flow, underscoring their importance in the administrative aspects of care. By optimizing processes like appointment scheduling and medical record handling, AI solutions can ease the burden of time-consuming administrative tasks, allowing providers to focus more on delivering high-quality care.
Consider the impact in physical therapy environments, where SOAP records foster smooth communication among therapists, physicians, and individuals, monitoring progress and directing treatment modifications. A case study highlighted that methods employing SOAP documentation achieved nearly flawless precision in , which is essential for reducing legal risks and ensuring safety for individuals. This accuracy not only protects patients but also safeguards medical providers from potential lawsuits.
As Ditto Transcripts emphasizes, 'We provide economical rates, adaptable choices, quick processing times, HIPAA-compliant security, and the finest customer support in the sector,' underscoring the significance of high-quality transcription services.
Current best practices for SOAP notes nursing stress the necessity of clarity and consistency in record-keeping. By adhering to these practices, medical providers can ensure that all relevant information is captured, thereby facilitating better decision-making and continuity of care. Expert opinions consistently emphasize that standardized documentation, such as SOAP notes nursing, is crucial for enhancing care and improving overall medical outcomes.
Notably, CosmaNeura stands out as the only company providing AI solutions tailored for the faith-focused medical market, aligning with the values and needs of providers in this sector. CosmaNeura's AI solutions specifically enhance administrative efficiency by automating appointment scheduling and streamlining medical record management, allowing providers to reduce administrative burdens and concentrate on care. For instance, practices utilizing CosmaNeura's solutions have reported a 30% decrease in time spent on administrative tasks, resulting in enhanced satisfaction and care outcomes.
As we move forward into 2025, the focus on the significance of SOAP notes nursing for client records remains strong, as they play a crucial role in ensuring that healthcare providers deliver high-quality, coordinated care.
The Structure of SOAP Notes: Breaking Down the Components
A SOAP note is a structured method of documentation that consists of four essential components, each playing a critical role in patient care:
- Subjective (S): This section captures the individual's personal account of their symptoms, feelings, and experiences. It is vital for understanding the individual's perspective and is often articulated in their own words, providing valuable context for their condition.
- Objective (O): This component includes quantifiable and observable data, such as vital signs, results from physical examinations, and laboratory findings. It creates a factual basis for the clinical evaluation, ensuring that the medical professional has a clear understanding of the individual's physical condition.
- Assessment (A): In this part, the healthcare provider synthesizes the subjective and objective data to formulate a clinical judgment or diagnosis. This section reflects the provider's critical thinking and clinical reasoning, showcasing their ability to integrate various pieces of information into a coherent understanding of the individual's health.
- Plan (P): The final component outlines the proposed interventions, treatments, and follow-up actions. It acts as a roadmap for the individual's ongoing care, ensuring that all team members are aligned on the next steps in the treatment process.
Effective communication through SOAP notes in nursing is crucial for clinicians, as it enables accurate and succinct conveyance of medical information. Have you considered how organized SOAP notes can enhance your clinical decision-making? Research indicates that such structured documentation significantly improves patient outcomes. For instance, a study emphasized that medical providers who employed organized SOAP notes reported a 30% rise in the precision of their clinical evaluations.
Moreover, by integrating AI solutions from CosmaNeura, healthcare providers can streamline their record-keeping processes, alleviating the administrative burdens that contribute to physician burnout. Imagine a world where automated data entry and intelligent recommendations for documentation allow you to focus more on patient care. CosmaNeura's AI solutions not only enhance the precision of SOAP entries but also empower physicians to concentrate on what truly matters—their patients—ultimately improving outcomes and reducing stress.
Expert insights highlight the significance of mastering the elements of SOAP documentation. As noted by Kunal Sindhu, MD, "As with any skill, practice makes perfect. Try to view SOAP records as learning opportunities, and with enough effort and time, you’ll become proficient in drafting these vital medical communications." This authoritative viewpoint emphasizes the importance of mastering SOAP documentation for effective care of individuals.
In practice, instances of can be observed in . For instance, a case study from 2023 demonstrated how a primary care clinic improved patient outcomes by implementing a standardized SOAP notes structure. This resulted in better tracking of patient progress and more tailored treatment plans. This method not only simplified record-keeping but also fostered a culture of responsibility and ongoing enhancement among medical professionals.
Moreover, since CosmaNeura is the sole company offering AI solutions customized for the faith-centered medical sector, our platform assists providers in improving their record-keeping methods while following ethical standards. Together, we can navigate the challenges of healthcare documentation with compassion and care.
The Importance of Accurate Documentation in Nursing
Precise record-keeping stands as a cornerstone of nursing practice, fulfilling essential functions that significantly influence both care and provider protection.
- Legal Protection: Well-documented notes are crucial in safeguarding medical providers against legal disputes or malpractice claims. They serve as concrete evidence of the care delivered and the rationale behind clinical decisions. Did you know that insufficient records are a leading cause of legal disputes in nursing? This highlights the necessity for meticulous record-keeping. Legal specialists emphasize that comprehensive medical documentation is vital for protecting providers and ensuring accountability in clinical practice.
- Continuity of Care: Accurate records are essential for ensuring that all members of the medical team are aware of an individual's condition and treatment plan. This facilitates seamless transitions in care, especially in complex cases involving multiple providers. Research shows that improved record-keeping methods can enhance continuity of care, ultimately leading to better outcomes for individuals receiving treatment.
- Quality Improvement: Record-keeping plays a vital role in evaluating care practices and outcomes, contributing to ongoing quality enhancement efforts within healthcare environments. A study in the Ilu Aba Bora Zone of Ethiopia revealed that only 51.1% of health professionals demonstrated good record-keeping practices, underscoring the need for enhanced training and the adoption of electronic record management tools. This calls for further research to standardize record-keeping practices across clinical settings.
- Safety of Individuals: Clear and precise records significantly reduce the risk of errors, ensuring that individuals receive the correct treatments and interventions. The availability of standard record-keeping tools has been shown to increase the likelihood of noting routine practices by 2.5 times, directly correlating with improved patient safety and care quality.
In conclusion, accurate record-keeping is not just a regulatory requirement; it is fundamental for delivering . As the medical field evolves, the importance of precise record-keeping in nursing will only grow. By integrating reliable measures of documentation burden and their connection to clinical outcomes, we can further enhance the role of documentation in nursing practice. Let’s embrace these practices to ensure we provide the best care possible.
Tips for Writing Effective SOAP Notes
Creating effective SOAP records can be a challenging task for medical professionals, often compounded by administrative burdens that detract from patient care. To alleviate these pressures, consider the following best practices:
- Be Clear and Concise: Utilize straightforward language, steering clear of unnecessary jargon. Clarity is essential for ensuring that your notes are easily interpretable by other healthcare professionals.
- Use Standardized Terminology: Consistency in terminology not only maintains clarity but also minimizes the risk of misinterpretation, which is crucial for safety.
- Prioritize Relevant Information: Concentrate on the most significant details that directly influence care for individuals. Avoid extraneous information that could obscure critical insights. The plan portion of a SOAP document should detail the treatment strategy, including prescribed medications, guidance for the individual, referrals, and follow-up appointments.
- Record in Real-Time: Whenever possible, write your observations right after the interaction with the individual. This practice enhances accuracy and completeness, which are vital for effective communication.
- Review and Revise: Dedicate time to examine your records for any errors or omissions before finalizing them. This step is essential for improving the quality of your records and ensuring they meet the standards anticipated in medical environments.
As Olga Goncharov, , observed, 'This saves time and avoids expensive errors that can harm your reputation with clients and insurers alike.' By implementing these strategies, medical providers can significantly enhance their abilities in SOAP notes nursing writing, ultimately leading to better outcomes for individuals. Effective records not only assist in clinical decision-making but also align with the ethical standards upheld in faith-focused healthcare practices, reinforcing the commitment to compassionate care as emphasized by CosmaNeura's mission. Remember, each note you take is a step towards better care for those you serve.
Examples of SOAP Notes: Learning from Real-World Scenarios
Effective documentation using the [SOAP notes nursing format](https://medicalaid.org/understanding-soap-notes-for-clinical-rotations) is essential for delivering high-quality care. It’s important to recognize the emotional challenges that healthcare providers face when managing documentation. Here are a few illustrative examples of SOAP notes that demonstrate best practices in nursing:
Example 1:
- Subjective: The patient reports experiencing a headache for the past two days, rating the pain intensity as 7 out of 10.
- Objective: Vital signs are stable: BP 120/80, HR 72, Temp 98.6°F. A thorough neurological examination reveals no deficits. Notably, there is no visible swelling or bruising.
- Assessment: The symptoms suggest a likely tension headache, potentially exacerbated by stress factors.
- Plan: Recommend over-the-counter analgesics, encourage hydration, and schedule a follow-up appointment in one week to reassess.
Example 2:
- Subjective: The patient expresses feelings of anxiety regarding an upcoming surgical procedure, stating, "I feel anxious about my upcoming surgery."
- Objective: The individual appears visibly restless, with a heart rate recorded at 85 bpm.
- Assessment: Anxiety is identified as being related to the anticipated surgical intervention.
- Plan: Provide reassurance, engage in a discussion about the surgical procedure, and consider a referral to a counselor if anxiety persists beyond the immediate pre-operative period.
These examples highlight the importance of capturing both subjective and objective data to form a comprehensive assessment and plan. In 2025, the focus on well-recorded SOAP notes nursing is more essential than ever. Research shows that detailed records are linked to better health outcomes. For instance, medical practitioners who consistently utilize improved clarity in communication and a reduction in errors during care.
Furthermore, it is significant that medical records have increased in both length and scope compared to fifty years ago, reflecting the evolving nature of record-keeping practices. Have you considered how this evolution impacts your daily practice?
Moreover, case studies have shown that mastering SOAP notes nursing early in clinical training significantly benefits nursing students, positioning them ahead of their peers in medical school applications and internships. By practicing effective SOAP notes nursing, medical professionals can ensure that all pertinent information is captured. This ultimately leads to improved care and satisfaction for individuals.
CosmoNauts, as the sole organization developing AI solutions for the faith-oriented medical sector, highlights the significance of thorough record-keeping in enhancing the quality of care for individuals. Let’s commit to improving our documentation practices together, ensuring that we provide the best possible care for our patients.
Common Challenges in Writing SOAP Notes and How to Overcome Them
Writing SOAP records can present several challenges that healthcare providers must navigate to ensure effective documentation.
Vague Language: Ambiguous terms can lead to misinterpretation, compromising patient care. It is crucial to use specific language in your descriptions to convey clear and accurate information.
Incomplete Information: Each section of the SOAP document must include all relevant details. A thorough examination of your records can help confirm completeness, ensuring that no critical information is overlooked.
Time Constraints: In fast-paced clinical environments, finding the time to write comprehensive notes can be a significant hurdle. In fact, a recent report indicated that more than 44% of service providers disagreed that it was easy to document care in electronic health records (EHRs). Integrating note-taking into your workflow can help make this task more manageable. For instance, utilizing ambient AI scribe technology can streamline documentation processes, allowing providers to focus more on patient interactions rather than administrative tasks. This technology not only improves efficiency but also reduces the administrative burden that contributes to physician burnout, as emphasized in recent discussions about transforming medical delivery through AI innovations. The use of complicated medical jargon can confuse readers and detract from the clarity of the information. Striving for simplicity and clarity in your writing enhances understanding and facilitates better communication among medical teams.
To effectively overcome these challenges, consider the following strategies:
- Regular Practice: Consistently writing SOAP notes can improve your skills and confidence. The more you practice, the more skilled you will become.
- Seek Feedback: Engaging with colleagues for constructive input can provide insights into areas for improvement and reinforce best practices.
- Utilize Templates: Implementing standardized formats can streamline the record-keeping process, ensuring that all necessary components are included and reducing the cognitive load associated with writing.
By addressing these common pitfalls, providers can significantly enhance the quality of their records. Research shows that medical practitioners who implement organized methods for record-keeping express greater job satisfaction and enhanced professional wellbeing. In fact, providers on the [CosmaNeura platform](https://cosmaneura.com) are positioned to gain significant advantages in job satisfaction and professional wellbeing.
Furthermore, the modified PDQI-9 Scribe Quality Assessment Tool serves as a real-world example of how AI technology is being utilized to enhance the quality of clinical documentation, ensuring accuracy and reliability across various specialties. Embracing these AI-driven solutions can lead to more effective patient care and . Additionally, addressing broader challenges such as physician burnout and through the implementation of AI tools can further enhance the overall healthcare delivery process.
Conclusion
Effective communication in healthcare is essential, and it heavily relies on structured documentation methods like SOAP notes. These notes are not just a tool; they are a lifeline for enhancing patient care. By breaking down patient encounters into four distinct components—Subjective, Objective, Assessment, and Plan—healthcare providers can ensure that critical information is accurately captured and communicated. This structured approach aids clinical decision-making and plays a crucial role in legal protection, continuity of care, and quality improvement.
In a fast-paced healthcare environment, the significance of accurate and clear documentation cannot be overstated. With time often limited, how can we ensure that our documentation meets the highest standards? By adhering to best practices such as clarity, relevance, and real-time documentation, healthcare professionals can overcome common challenges associated with SOAP notes. Furthermore, implementing AI solutions can streamline the documentation process, reducing administrative burdens and allowing providers to focus more on what truly matters—patient interactions.
As the healthcare landscape continues to evolve, the emphasis on the importance of SOAP notes will only grow. Mastering this documentation method is essential for delivering high-quality, coordinated care that ultimately leads to improved patient outcomes. By embracing the SOAP framework, healthcare providers not only enhance their communication but also reinforce their commitment to compassionate and effective patient care.
Let's reflect on the journey ahead. How can we support each other in mastering these vital skills? Together, we can create an environment where effective communication flourishes, ensuring that every patient receives the care they deserve. Embrace the SOAP methodology, and take a step towards enhancing your practice and patient interactions.




