Overview
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality care. The burden of administrative tasks can detract from the vital interactions with patients that truly matter. This is where SOAP charting comes into play, offering a compassionate solution to enhance communication and improve patient outcomes.
SOAP charting not only streamlines administrative tasks but also fosters a nurturing environment for both providers and patients. Structured SOAP notes—comprising Subjective, Objective, Assessment, and Plan components—facilitate thorough documentation. This is essential for effective treatment planning and continuity of care, especially in today’s rapidly evolving healthcare landscape.
By adopting SOAP charting, healthcare providers can alleviate some of the pressures they face. Imagine having a clear, organized way to document patient interactions that allows for more meaningful connections and better care. The benefits are profound:
- Improved patient outcomes
- Enhanced communication among staff
- A more efficient workflow
We invite you to consider how implementing SOAP charting can transform your practice. What if you could spend more time focusing on your patients rather than paperwork? Embracing this approach not only supports your professional goals but also nurtures the relationships that are at the heart of healthcare. Together, we can create a more compassionate and efficient healthcare environment.
Introduction
In the ever-evolving landscape of healthcare, we understand that effective communication and documentation are vital for delivering quality patient care. Have you ever felt overwhelmed by the complexities of patient encounters?
SOAP notes offer a systematic method for recording these interactions, emerging as a cornerstone for healthcare providers who strive for clarity and continuity in treatment. This structured approach—comprising Subjective, Objective, Assessment, and Plan components—facilitates the meticulous capture of patient narratives and clinical findings. It also enhances collaboration among medical professionals, fostering a supportive environment.
As we look toward 2025, the reliance on SOAP notes is set to grow. Recognizing their significance is crucial for improving patient outcomes and streamlining administrative processes. Imagine a world where your documentation not only supports your practice but also empowers your patients.
The integration of innovative technologies amplifies the impact of SOAP notes, making them indispensable in a healthcare environment that prioritizes efficiency and patient-centered care. Let’s embrace these tools together to enhance our practice and the care we provide.
Understanding SOAP Notes: A Comprehensive Overview
SOAP records stand as a vital example of standardized documentation, a compassionate approach that medical providers utilize to effectively document client interactions. This method, encapsulated in the acronym SOAP—Subjective, Objective, Assessment, and Plan—captures the individual’s narrative, clinical findings, and treatment strategies. Such organization is crucial for fostering clear communication among healthcare professionals and ensuring continuity of care, which is essential for patient well-being.
In 2025, the significance of SOAP records has grown, with studies indicating that over 80% of medical providers rely on this format for documentation. This statistic underscores the role of SOAP notes in enhancing the quality of care. By adopting this structured approach, providers can streamline their documentation processes, minimizing the time spent on administrative tasks and allowing for more focus on patient interactions.
Moreover, the integration of AI solutions is transforming the documentation landscape in healthcare. For instance, automated appointment scheduling alleviates the burden of administrative duties, enabling providers to devote more time to client interactions. Similarly, AI-driven medical record management organizes patient information, making it readily accessible and further enhancing administrative efficiency.
Expert insights highlight the importance of SOAP charting examples in healthcare documentation. Many professionals assert that lead to clearer communication, better diagnoses, and improved treatment planning. For example, avoiding common pitfalls—such as missing vital information or unclear documentation—can significantly enhance client service outcomes. A case study titled 'Common Mistakes in SOAP Records' illustrates that addressing these challenges can foster clearer communication and better treatment planning.
The benefits of using SOAP records extend beyond mere documentation; they are pivotal in enhancing care. By ensuring that all relevant information is captured accurately, healthcare providers can make informed decisions that directly impact health outcomes. Furthermore, the shift towards digital documentation in 2025 emphasizes the need for high accuracy in medical transcription services.
Recommendations suggest that providers choose services with accuracy rates of 99% or higher to mitigate legal risks and ensure individual safety.
As Imran Shaikh, a Content Marketing Expert, notes, 'With over 30 top-ranking articles, I leverage my MBA in Healthcare Marketing to make complex AI topics accessible and engaging.' This perspective underscores the importance of precise documentation and its profound effects on healthcare services.
Case studies have demonstrated the positive impact of efficient SOAP charting example implementation on healthcare quality. Providers who consistently use SOAP examples in their documentation report enhanced clarity in communication and a more organized approach to patient management. As the medical field evolves, the integration of AI technologies—such as automated scheduling and streamlined record management—alongside the significance of SOAP records, remains crucial, serving as foundations for effective care and operational efficiency.
The Subjective Component: Capturing Patient Perspectives
The Subjective section of a SOAP note holds profound importance, as it encompasses information communicated directly by the individual, including their symptoms, feelings, and concerns. This component is vital because it sheds light on the individual's lived experience, enabling providers to grasp the context of their condition more effectively. For example, an individual may express their pain level, emotional state, or any recent changes in their health status.
Accurately documenting this information not only empowers providers to tailor their care strategies but also fosters a more compassionate healthcare environment.
In 2025, the importance of capturing perspectives from individuals receiving care has gained even more momentum, with studies showing that reported outcomes (Pros) significantly influence treatment decisions and health results. The Swedish Arthroplasty Register, for instance, has recorded over 515,703 primary hip arthroplasties and 333,693 primary knee arthroplasties, underscoring the need for comprehensive data collection that includes individual experiences.
Moreover, incorporating technology, such as CosmaNeura's intelligent transcription services, can ease the documentation of these subjective insights, saving providers an average of 2.5 hours in administrative tasks. This efficiency allows for a greater focus on healthcare, ensuring that the subjective information collected is both accurate and meaningful. By alleviating the administrative burden and fragmented communication often encountered by healthcare providers, these services enhance interactions between patients and providers.
As Dr. Alexander S McLawhorn notes, "The integration of Proms within big data ecosystems has the potential to transform health services."
Expert insights highlight that the subjective component of is not merely a formality; it is a crucial element that enhances patient-centered care. Healthcare providers have observed that when they actively listen to and document perspectives, it leads to increased satisfaction and improved outcomes. For instance, the use of intelligent transcription services has been associated with a 20% rise in satisfaction scores due to the heightened focus on interactions.
As we move forward, the ability to effectively gather and apply subjective information in SOAP records will be essential in nurturing a medical system that prioritizes the individual's perspective, while AI-driven innovations facilitate more effective care delivery.
The Objective Component: Documenting Clinical Findings
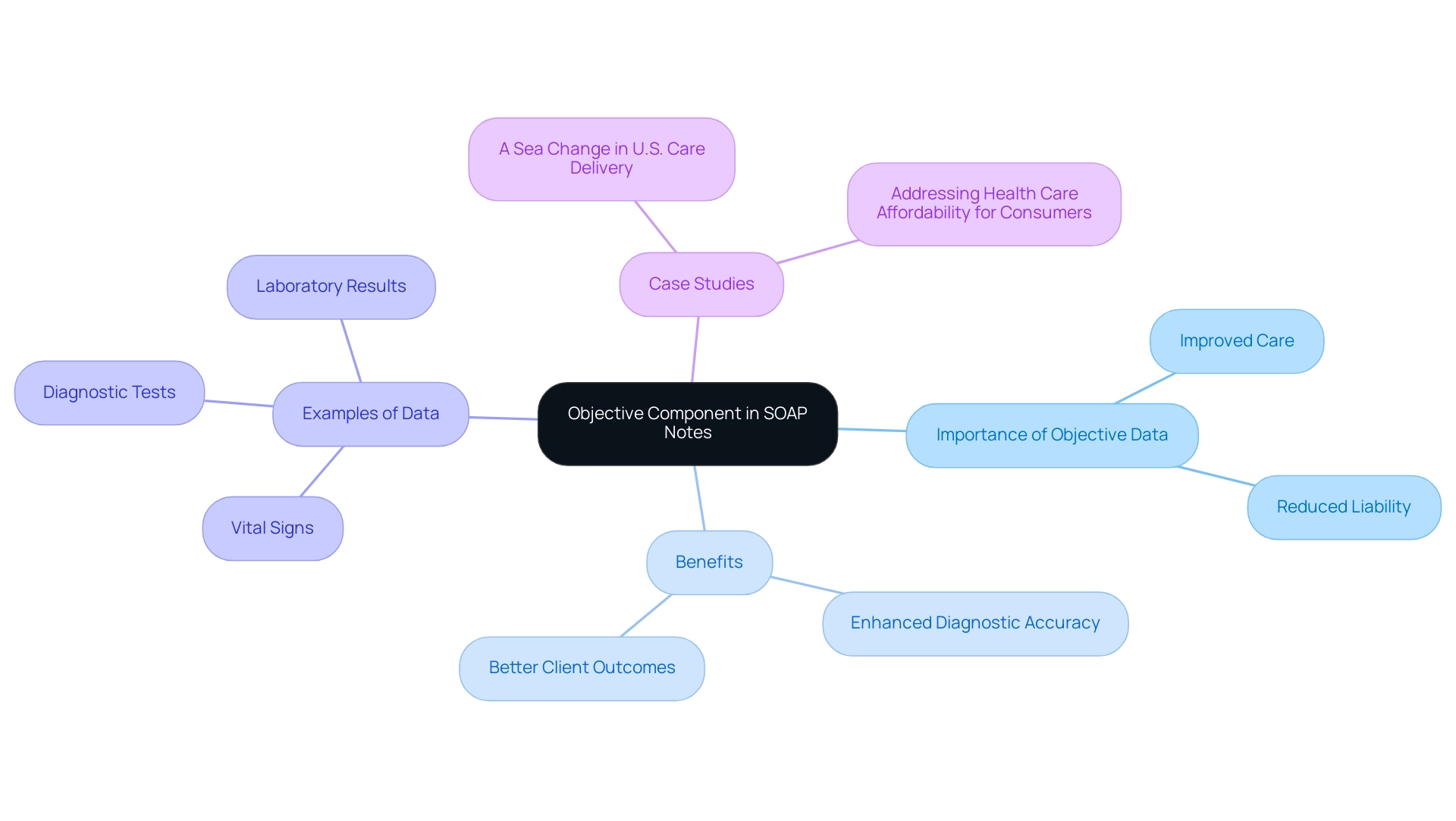
The Objective section of a SOAP note is not just a technical requirement; it is a vital part of our commitment to providing compassionate care. This section encapsulates observable and measurable data collected during client encounters, including vital signs, findings from physical examinations, and results from diagnostic tests. For instance, recording an individual's blood pressure, heart rate, or lab results—such as glucose levels or cholesterol measurements—helps us understand their health better.
In 2025, the emphasis on objective data in assessments has grown significantly. Studies show that accurate documentation of clinical findings can truly enhance the quality of care we provide. Recent statistics reveal that medical providers who consistently utilize objective data in their SOAP records report improved diagnostic accuracy and better client outcomes. Notably, Nurse Practitioners (NPs) and Physician Assistants (PAs) are much less likely than physicians to be named as defendants in medical professional liability cases. This highlights how crucial accurate documentation is in reducing liability risks.
Many medical professionals assert that the objective component in SOAP notes forms the backbone of effective clinical decision-making. By relying on concrete data, we can create a more comprehensive understanding of a patient's health status, which is essential for developing tailored treatment plans. A case study titled "A Sea Change in U.S. Care Delivery" illustrates that NPs and PAs are less frequently implicated in claims related to care events, reinforcing the necessity for objective data documentation.
To effectively document clinical findings in medical environments, practitioners should adopt that emphasizes clear and concise entries in the Objective section. This means not only recording vital signs but also integrating results from diagnostic imaging and laboratory tests. For example, documenting an individual's respiratory rate alongside oxygen saturation levels can provide a more complete picture of their respiratory health.
Case studies have shown that medical organizations prioritizing objective data documentation experience fewer errors in assessments and enhanced communication among treatment teams. By embracing a systematic method for recording clinical observations in a soap charting example, we can improve our practice and ultimately lead to better health outcomes for those we serve. Furthermore, as employers promote healthier lifestyles through wellness programs and preventive care services, the significance of precise documentation in enhancing outcomes becomes even more critical.
In summary, let’s commit to fostering a culture of thorough documentation. By doing so, we not only protect ourselves but also ensure that our patients receive the best possible care. Together, we can make a meaningful difference in the lives of those we serve.
The Assessment Component: Analyzing Patient Data
The Assessment section of a SOAP charting example is crucial, capturing the healthcare provider's clinical judgment from both subjective and objective data. This may encompass a definitive diagnosis, differential diagnoses, or an assessment of the individual's progress. For instance, a provider might conclude that an individual's symptoms align with a specific condition based on the comprehensive information gathered.
In 2025, the integration of AI-driven solutions in this process has proven invaluable. These advancements significantly enhance the accuracy of assessments, ultimately improving patient outcomes. Effective evaluations lead to more precise diagnoses, empowering clinical judgment while alleviating the stress on medical providers. Have you considered how technology can support your clinical assessments? Statistics reveal that 65% of U.S. adults favor AI involvement in , highlighting a growing trust in these innovative tools.
Furthermore, 52% of individuals view AI-based detection as a significant advancement in medical care. This underscores the importance of integrating innovative solutions into the assessment process. Case studies demonstrate that medical systems implementing strong evaluation protocols, including AI tools that automate task assignments and allow real-time monitoring of individual progress, report enhanced precision in diagnosis and treatment planning. For example, a pertinent case study named 'Data Security Meeting Scalability' emphasizes the need to preserve data security while ensuring rapid access to information, which is vital in the context of SOAP records.
Today's healthcare settings effectively enforce robust security protocols, including HIPAA adherence and encryption. This promotes a safe and cooperative environment for treatment. Expert insights reinforce that the assessment component of a SOAP charting example is essential for informed clinical judgment. Vivienne van der Walle, Founder and Medical Director, states, 'Anything that takes away time from individuals is a pain point for a site, and anyone who resolves that is assisting in the well-being of those individuals.'
This highlights the importance of minimizing time spent on administrative tasks through AI solutions. By doing so, healthcare providers can focus more on meaningful interactions with individuals. Thorough evaluations lead to improved treatment, facilitating a nuanced understanding of conditions that ultimately benefit both providers and individuals alike.
Key Solutions:
- Integrate AI-driven tools to enhance assessment accuracy.
- Automate administrative tasks to free up time for patient care.
- Ensure robust data security to protect sensitive information.
By embracing these solutions, we can create a more supportive environment for both healthcare providers and patients.
The Plan Component: Developing Effective Care Strategies
The Plan section of a soap charting example is crucial as it outlines the proposed course of action for an individual's care. This section may include treatment recommendations, referrals to specialists, follow-up appointments, and education for individuals. For instance, a provider might suggest physical therapy for someone recovering from surgery or prescribe medication for managing a chronic condition.
A clearly articulated plan not only aligns all healthcare team members in their approach but also significantly contributes to improved health outcomes.
In 2025, effective treatment strategies documented in SOAP notes are more vital than ever, especially given the ongoing challenges such as clinical staff shortages and budget constraints. Health system leaders remain hopeful about enhancing experiences for individuals, underscoring the significance of well-organized treatment plans. Research indicates that thorough treatment planning can lead to improved outcomes for individuals, with statistics showing that organized methods can reduce hospital readmission rates by as much as 20%.
Furthermore, the global healthcare industry generates up to 5.2% of the world’s greenhouse gas emissions, highlighting the necessity for effective treatment strategies that not only enhance patient outcomes but also promote sustainability in healthcare.
Consider case studies like the digital transformation of a major hospital chain in Vietnam, co-led by Kavita Rekhraj. This initiative demonstrates the positive impact of formulating treatment plans utilizing SOAP documentation. Not only did it improve operational capabilities, but it also enhanced service delivery, showcasing the effectiveness of structured documentation in real-world settings, as illustrated in a soap charting example. Experts emphasize the significance of the Plan component in SOAP notes. Healthcare professionals, such as Minni Särkkä-Hietala, with over fifteen years of experience in health and human services consulting, advocate for detailed support strategies, noting that a well-defined plan fosters collaboration among providers and ensures continuity of service.
As evolves, the importance of care plans in documentation cannot be overstated, particularly as organizations strive to prioritize equity in design and access to care for all patients. How can we ensure that every individual receives the care they deserve? By embracing structured treatment plans, we can make a meaningful difference in the lives of those we serve.
Conclusion
The significance of SOAP notes in the healthcare landscape is profound. This structured documentation method—comprising Subjective, Objective, Assessment, and Plan components—enhances communication among healthcare providers and streamlines patient care. As reliance on SOAP notes grows, their role in improving patient outcomes and operational efficiency becomes increasingly critical.
Innovative technologies, such as AI-driven solutions, further amplify the effectiveness of SOAP notes. By reducing administrative burdens and facilitating accurate documentation, these tools enable healthcare providers to capture comprehensive patient narratives and clinical findings. This capability empowers providers to make informed decisions, leading to better diagnoses and treatment plans. Such a holistic approach fosters a more empathetic healthcare environment, ensuring that patients feel heard and valued.
As we look toward 2025 and beyond, embracing the structured methodology of SOAP notes will be essential for navigating the complexities of patient care. Prioritizing clarity and continuity in documentation enhances collaboration among healthcare professionals, ultimately improving the quality of care delivered. The future of healthcare is rooted in effective communication; SOAP notes are poised to remain at the forefront of this evolution, driving positive change in patient management and outcomes.
How can we, as a community of caregivers, ensure that we are fully utilizing the potential of SOAP notes? By recognizing their importance and integrating them into our daily practices, we can create a more compassionate and efficient healthcare system for everyone.




