Overview
This article highlights the emotional challenges healthcare providers face in documentation. It offers examples of OB SOAP notes, aiming to enhance effective patient documentation in healthcare settings. By recognizing the administrative burdens that often impact patient care, we can appreciate how organized and structured SOAP notes can improve communication among healthcare providers. This not only streamlines documentation processes but ultimately leads to better patient care outcomes.
Imagine a world where documentation feels less daunting. With structured SOAP notes, healthcare professionals can focus more on their patients and less on the paperwork. This approach fosters collaboration among providers, ensuring that everyone is on the same page. The insights shared by healthcare professionals throughout this article reinforce the value of these practices.
We encourage you to reflect on your own documentation experiences. How might organized SOAP notes alleviate some of your stress? By embracing these examples, you can contribute to a more efficient healthcare environment. Let’s work together to improve patient care outcomes, one note at a time.
Introduction
In the ever-changing world of healthcare, we understand that effective documentation is crucial for improving patient care and easing the burdens of administrative tasks. Healthcare providers often face overwhelming challenges, and SOAP notes, with their structured approach, can be a lifeline. These notes enable providers to capture essential patient information succinctly, helping to alleviate some of the stress they encounter daily.
Imagine the relief of automating note-taking with AI-driven solutions like CosmaNeura or utilizing tailored templates designed for various specialties. This integration of technology into documentation practices is not just a trend; it’s a transformative shift in how clinicians operate. By embracing these tools, healthcare professionals can focus more on what truly matters—their patients.
This article explores the significance of SOAP notes across diverse healthcare settings. We will share relatable examples, best practices, and innovative tools that not only enhance documentation efficiency but also elevate the quality of care provided to patients. Together, let’s navigate these challenges and discover how to improve both our documentation practices and the care we deliver.
CosmaNeura: Streamline Your SOAP Notes with AI-Powered Documentation
In of healthcare, professionals often face overwhelming administrative burdens that can detract from their ability to provide compassionate care. CosmaNeura understands these challenges and utilizes advanced AI technology to automate the generation of clinical records, allowing healthcare providers to focus more on what truly matters—their patients.
By seamlessly integrating AI into the documentation workflow, CosmaNeura ensures that clinical records are created in real-time during client interactions. This not only enhances precision but also boosts productivity, alleviating the stress that comes with paperwork. Imagine reclaiming valuable time to engage with patients and provide high-quality care, all while upholding ethical standards.
With automation, physicians can streamline essential processes such as:
- Appointment scheduling
- Medical record management
- Billing
This innovation aligns with the mission of improving clinical experiences, ultimately fostering a nurturing environment for both providers and patients. How much more fulfilling could your practice be if you could devote your energy to care rather than clerical tasks?
CosmaNeura invites you to explore these transformative solutions. Together, we can create that prioritizes compassion and efficiency, ensuring that every patient receives the attention they deserve.
ABA SOAP Notes: Essential Examples for Behavioral Health Providers
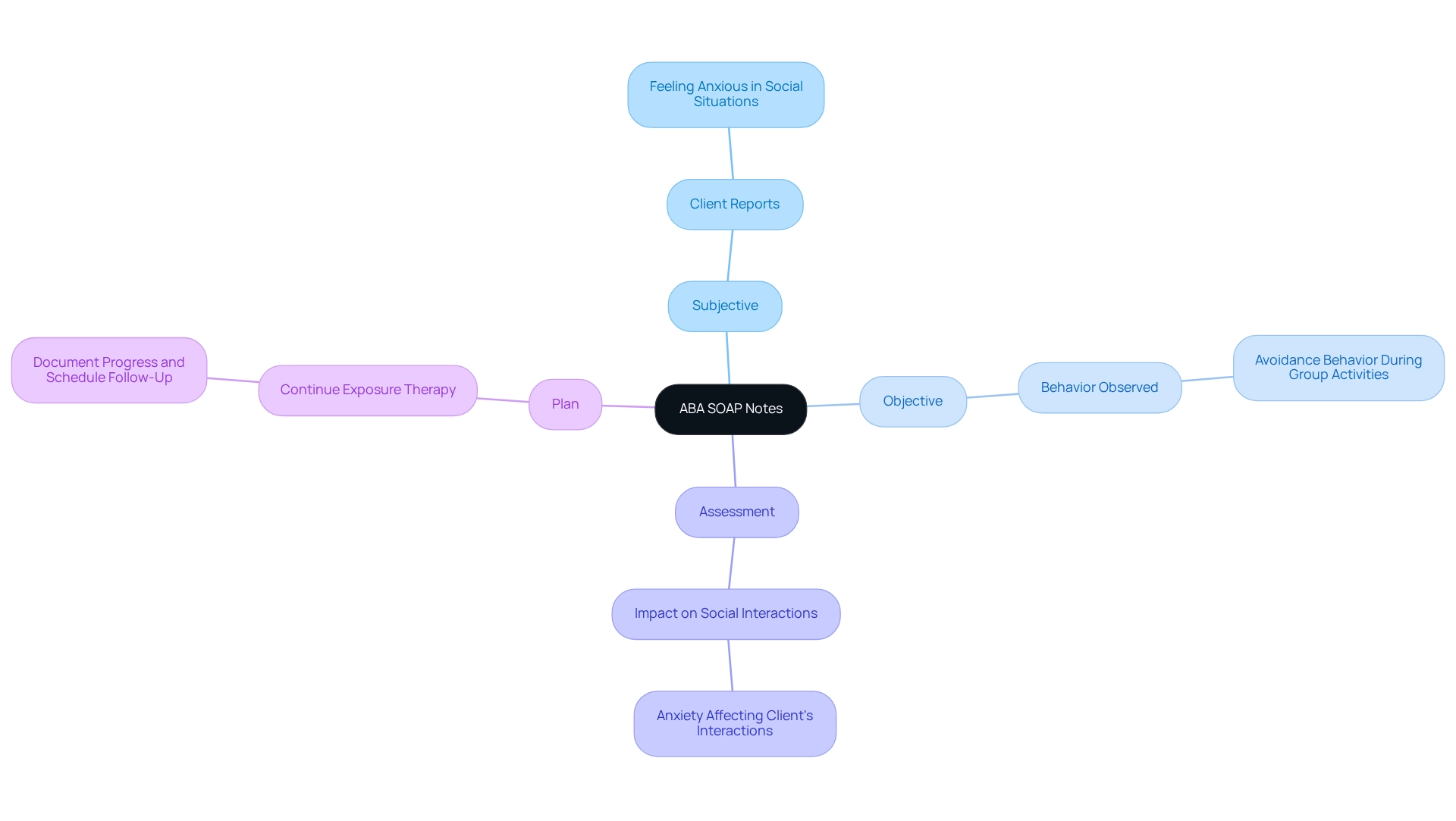
Behavioral health practitioners often face emotional challenges in their work, and utilizing ABA documentation can be a compassionate way to record client progress efficiently. This approach not only fosters a thorough understanding of treatment dynamics but also alleviates some of the administrative burdens that can impact patient care. For instance, a well-structured ABA SOAP note might include:
- Subjective: "The client reports feeling anxious when faced with social situations."
- Objective: "As detailed in the ob soap notes examples, the client exhibited avoidance behavior during group activities."
- Assessment: "The client's anxiety, as illustrated in the ob soap notes examples, appears to be impacting their social interactions."
- Plan: "Continue with exposure therapy and document ob soap notes examples, then schedule a follow-up in two weeks."
This structured method is crucial for capturing all relevant information necessary for ongoing treatment planning.
The significance of organized ABA documentation in treatment planning cannot be overstated. It not only facilitates clear communication among providers but ensures that treatment plans are tailored to meet individual client needs. As experts in the field highlight, effective documentation is essential for evaluating treatment outcomes and making necessary adjustments. Taylor Gaines, MS, BCBA, emphasizes that "SOAP documentation concentrates on subjective information, an evaluation of the session, and future planning for the client’s therapy."
Consider the case of Artemis, a comprehensive ABA practice management solution that seamlessly integrates SOAP and session notes into daily operations. By transitioning record-keeping processes to digital formats, Artemis enhances the efficiency of ABA providers, allowing them to focus more on client care rather than administrative tasks. This transformation not only improves workflow but also elevates the standard of care provided to clients, showcasing how efficient record-keeping practices can lead to better health outcomes.
In summary, employing organized ABA documentation is essential for behavioral health providers seeking to enhance . Instances of effective clinical records, including ob soap notes examples, illustrate how this method of recording can lead to improved patient care and more efficient practice management. Moreover, with advancements in AI tools such as those offered by CosmaNeura, the incorporation of organized records is becoming increasingly seamless, further enhancing the quality of care in the healthcare field.
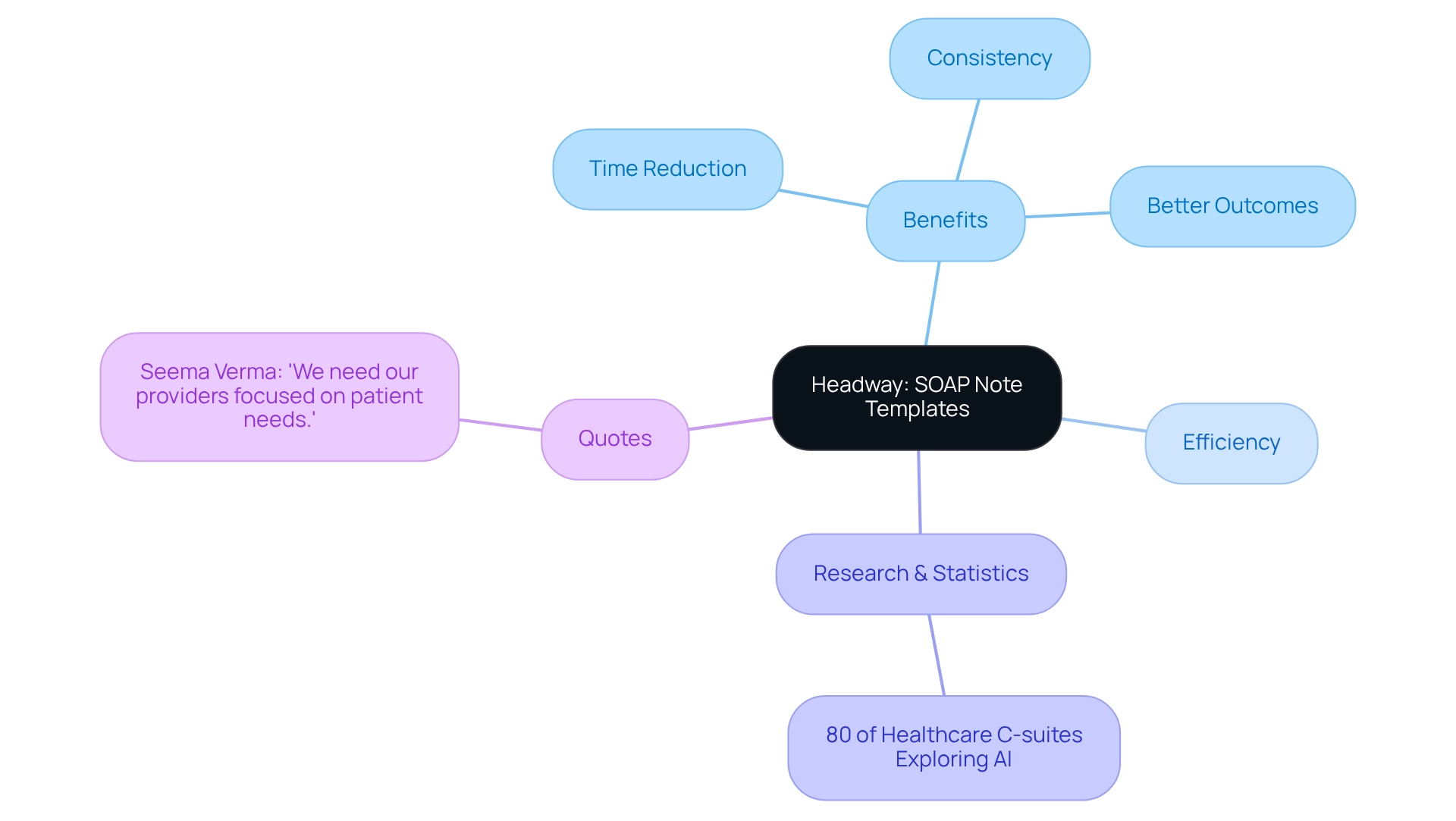
Headway: User-Friendly SOAP Note Templates for Efficient Documentation
In the demanding world of healthcare, professionals often face overwhelming administrative burdens that can detract from their primary focus: patient care. Headway understands this struggle and offers [user-friendly OB SOAP notes examples](https://healthcareitnews.com/news/oracles-new-clinical-digital-assistant-offers-genai-ambulatory-clinics) designed to simplify the record-keeping process. These OB SOAP notes examples guide clinicians through each section of the SOAP format—Subjective, Objective, Assessment, and Plan—ensuring that no critical information is overlooked.
By utilizing these accessible templates, providers can significantly reduce the time spent on documentation, allowing them to dedicate more attention to their clients. Research indicates that organized templates can enhance clinical record efficiency, with over 80% of healthcare C-suites exploring generative AI solutions to alleviate administrative pressures. This exploration underscores a growing recognition of the need for that prioritize patient care.
Moreover, the application of structured templates fosters consistency in documentation practices, ultimately leading to better outcomes for individuals. As Seema Verma, Executive VP and General Manager of Oracle Health and Life Sciences, aptly stated, 'We need our providers concentrated on the needs of those receiving care.' This sentiment resonates with the success of initiatives like Microsoft's Dragon Copilot, which has been shown to reduce clinician burnout and improve experiences for patients. By adopting effective documentation tools such as structured templates and OB SOAP notes examples, healthcare providers can enhance their workflow and elevate the standard of care they offer. Therefore, considering the adoption of accessible documentation templates is vital for modern healthcare practitioners aiming to improve both efficiency and outcomes, especially in an increasingly AI-driven landscape.
Mentalyc: Tailored SOAP Note Examples for Mental Health Professionals
Mentalyc provides tailored ob soap notes examples that are specifically designed for mental health professionals, highlighting the essential balance between subjective and objective data. For instance:
- Subjective: "The patient expresses feelings of sadness and hopelessness."
- Objective: "The individual seemed withdrawn and exhibited a flat affect during the session."
- Assessment: "The individual's symptoms align with moderate depression."
- Plan: "Increase therapy sessions to weekly and consider medication evaluation."
These ob soap notes examples highlight the importance of capturing both the individual's personal experiences and observable behaviors, which are vital for accurate diagnosis and effective treatment planning. By employing organized documentation methods, mental health professionals can enhance clarity in records, ultimately leading to improved outcomes and safety for individuals.
Have you considered how well-structured SOAP notes can transform your practice? As highlighted in the case study "The Importance of Clarity in Medical Documentation," these notes help organize relevant clinical data, making it easier for healthcare providers to access and utilize critical information. This aligns seamlessly with CosmaNeura's mission of enhancing the quality of care for individuals while embodying Catholic healthcare values.
To improve their record-keeping methods, mental health experts can explore tools such as TheraPlatform, which offers a , providing an opportunity to enhance administrative efficiency.
As a best practice, we encourage mental health experts to utilize organized clinical records. This approach not only streamlines record-keeping but also enriches care quality and safety, reflecting the compassionate spirit of Catholic healthcare.
Zanda Health: Understanding the Key Components of SOAP Notes
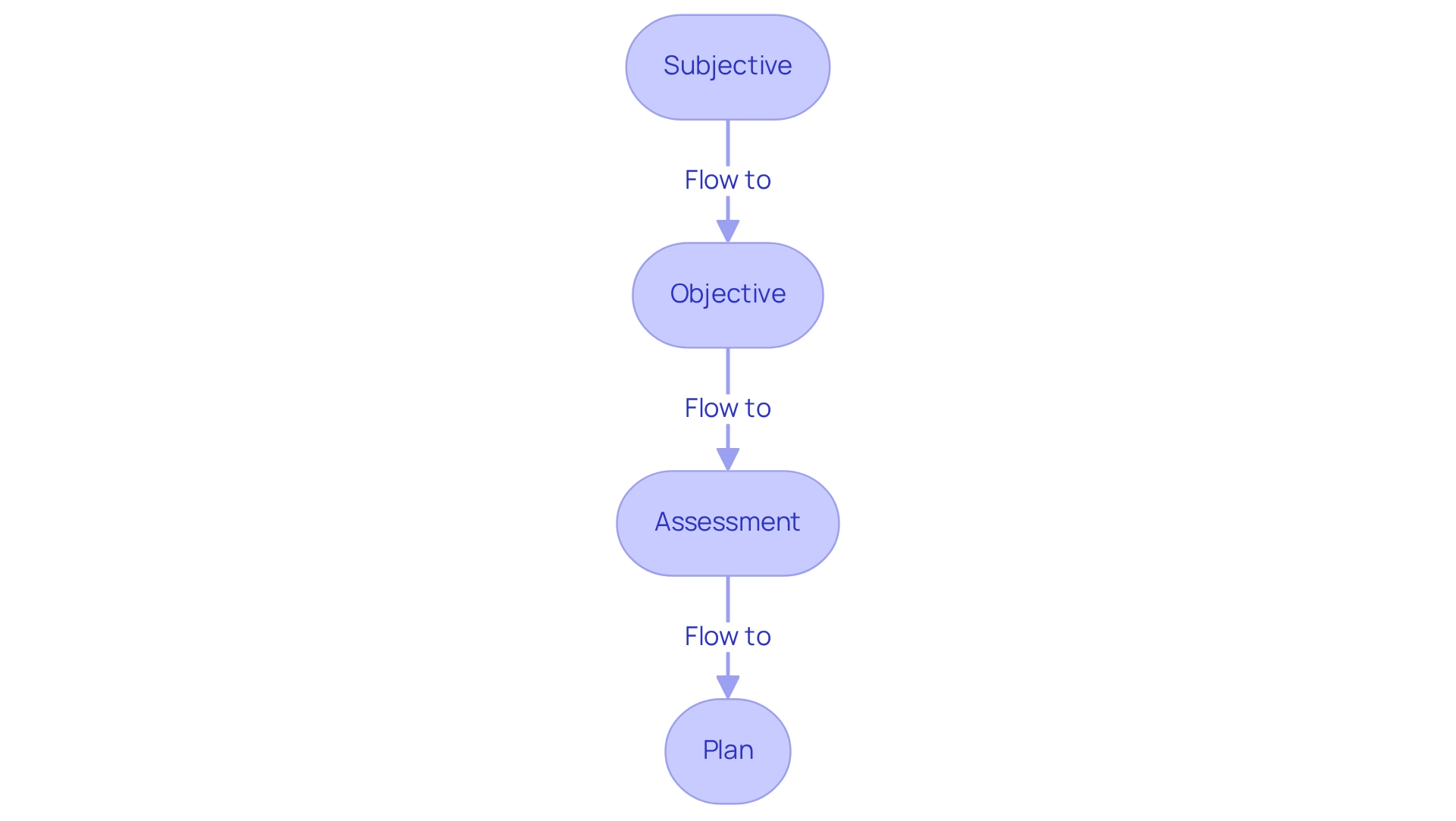
OB SOAP notes examples are structured into four essential components that facilitate effective clinical documentation and communication among healthcare providers:
- Subjective
- Objective
- Assessment
- Plan
Understanding examples is crucial, as they not only enhance continuity of care but also significantly improve patient outcomes. Have you ever considered how effective documentation can transform patient experiences? A recent study emphasized that the APSO order of documentation surpassed the conventional format regarding speed and usability for physicians, highlighting the necessity for effective clinical communication.
Yet, we must acknowledge the constraints of the model, particularly its inability to record changes over time—an essential aspect in evolving clinical settings. As noted in the case study titled 'Limitations of the Note Model,' extensions like the SOAPE framework have been suggested to tackle this gap by including a clear evaluation of treatment effectiveness over time. This evolution reflects the ongoing need for adaptability in clinical record-keeping practices.
Integrating efficient documentation into practice can result in better communication among healthcare professionals, ultimately improving care for individuals. As healthcare continues to evolve, understanding and implementing OB SOAP notes examples will remain essential for delivering high-quality, patient-centered care. We encourage healthcare professionals to actively incorporate these elements into their record-keeping methods to enhance client outcomes. Together, we can foster a more compassionate and effective healthcare environment.
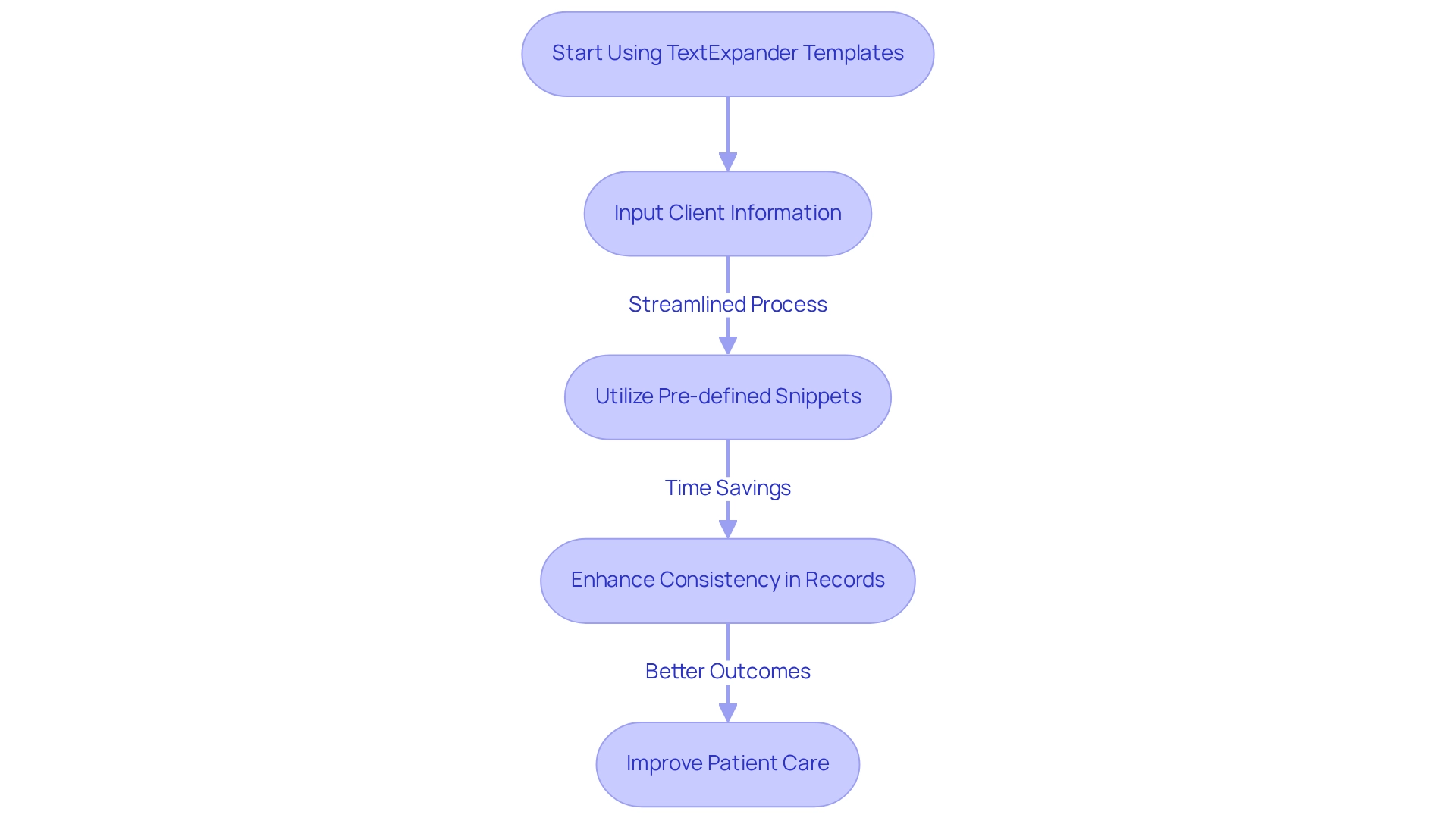
TextExpander: Efficient SOAP Note Templates for Consistent Documentation
Healthcare providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. TextExpander recognizes these emotional challenges and offers customizable that simplify record-keeping processes. Imagine the relief of swiftly inputting client information with pre-defined snippets, eliminating the repetitive task of writing common phrases or sections. This approach not only saves valuable time but also fosters consistency in records across different interactions, ultimately enhancing clarity and communication.
In 2025, statistics suggest that regular recording practices significantly improve patient care outcomes. Studies demonstrate that standardized template forms can reduce recording time by as much as 30%. Furthermore, a case study analyzing template usage in clinical encounters highlighted notable improvements in both efficiency and adherence to quality measures. By utilizing statistical techniques, the research assessed the effectiveness of these templates, shedding light on their positive impact on record-keeping practices.
As Dr. Bojrab aptly noted, "So far, it's just been great out of the box," emphasizing the immediate benefits of adopting such tools. By nurturing consistency in documentation, TextExpander not only enhances healthcare providers' efficiency but also contributes to better patient care, as seen in ob soap notes examples. If you're interested, anonymized data from the study can be provided upon request from qualified researchers, further supporting the effectiveness of standardized documentation templates. Consider how these tools could transform your practice and improve the care you provide.
Upheal: Versatile SOAP Note Examples for Diverse Healthcare Settings
Upheal offers a variety of adaptable documentation samples tailored for diverse healthcare settings, including primary care, mental health, and rehabilitation. Consider, for instance, how may be structured:
- Subjective: "The patient reports a persistent cough lasting two weeks."
- Objective: "Vital signs are stable; lung auscultation reveals wheezing, which can be referenced in the ob soap notes examples."
- Assessment: "Possible bronchitis; further evaluation is recommended according to ob soap notes examples."
- Plan: "Prescribe a bronchodilator and schedule a follow-up in one week, following the ob soap notes examples."
This flexibility in documentation empowers healthcare professionals to efficiently gather individual information, ensuring that the nuances of each specialty are thoughtfully addressed. By allowing modifications to SOAP notes, communication among providers is enhanced, ultimately improving care through a comprehensive understanding of each patient's unique circumstances.
Moreover, platforms like CosmaNeura are transforming healthcare record-keeping practices by automating administrative tasks, allowing providers to focus more on patient care. A case study highlights how CosmaNeura's AI-driven services significantly boost record-keeping efficiency, a necessity in today's fast-paced healthcare landscape. This innovation helps to overcome the resistance often encountered in healthcare, providing solutions that elevate the quality of care without compromising the vital interactions with those receiving treatment.
Data from the Spring 2024 G2 Market Reports indicate that effective communication tools, such as those offered by Klara, can profoundly enhance record-keeping practices, leading to improved outcomes for patients. As healthcare organizations prioritize consumer experience, they will find that efficient record-keeping, including adaptable clinical summaries, is essential for thriving in a rapidly evolving environment.
Ultimately, it’s about making healthcare more responsive and compassionate. How can you leverage these tools to improve your practice and the care you provide?
NCBI: Academic Insights on the Clinical Significance of SOAP Notes
Research highlights the emotional challenges faced by healthcare providers, particularly regarding the importance of structured records in clinical reporting. These organized formats not only improve communication among healthcare professionals but also alleviate some of the administrative burdens that can hinder patient care. By ensuring that all relevant individual information is precisely recorded and easily accessible, structured records help providers focus more on what truly matters—the well-being of their patients.
In 2025, studies have shown that using organized records, such as structured assessment forms, is linked to enhanced patient outcomes. This illustrates the vital role these records play in efficient healthcare provision. Furthermore, the transition to digital formats within Electronic Health Records (EHRs) has significantly improved medical records management, allowing for seamless integration of clinical entries into daily workflows.
The Objective section of clinical records provides measurable data gathered by practitioners, which is essential for enhancing accuracy and reliability. The use of ob soap notes examples has been associated with increased efficiency in clinical workflows, enabling providers to dedicate more time to patient care rather than administrative tasks. This organized approach not only enhances clinical decision-making but also fosters a culture of accountability and transparency in healthcare practices.
However, as noted by , there are risks and benefits associated with quoting patients in medical records. Understanding these dynamics is crucial, and clinical ethicists can play a significant role in mitigating risks, thus promoting more reflective and thoughtful charting practices. How can we, as a community, ensure that our documentation practices support both our responsibilities and our patients' needs? Let's engage in this important conversation together.
OT Potential: Specialized SOAP Note Examples for Occupational Therapists
OT Potential offers tailored ob soap notes examples specifically created for occupational therapists, emphasizing the essential components of effective record-keeping. Consider this:
- Subjective: "The client reports difficulty with daily living activities due to decreased mobility."
- Objective: "The client demonstrated limited range of motion in the right shoulder during assessment."
- Assessment: "The client's functional limitations are impacting their independence."
- Plan: "Implement a tailored exercise program to improve mobility and schedule weekly follow-ups."
These ob soap notes examples emphasize the in occupational therapy. In 2025, statistics reveal that comprehensive record-keeping practices are vital; physicians who have received occupational therapy education see 42% higher referral rates. This underscores the significance of thorough records in enhancing health outcomes and ensuring that functional restrictions are clearly articulated. As Libby Rogers emphasizes, combining clinical expertise with empathy is crucial for effective care. A comprehensive approach to record-keeping is essential for occupational therapists striving to deliver the highest standard of service.
Reflecting on these practices, how can we enhance our documentation to better serve our clients? By prioritizing effective record-keeping, we not only improve our practice but also foster a deeper connection with those we care for.
Mentalyc: Common Mistakes to Avoid When Writing SOAP Notes
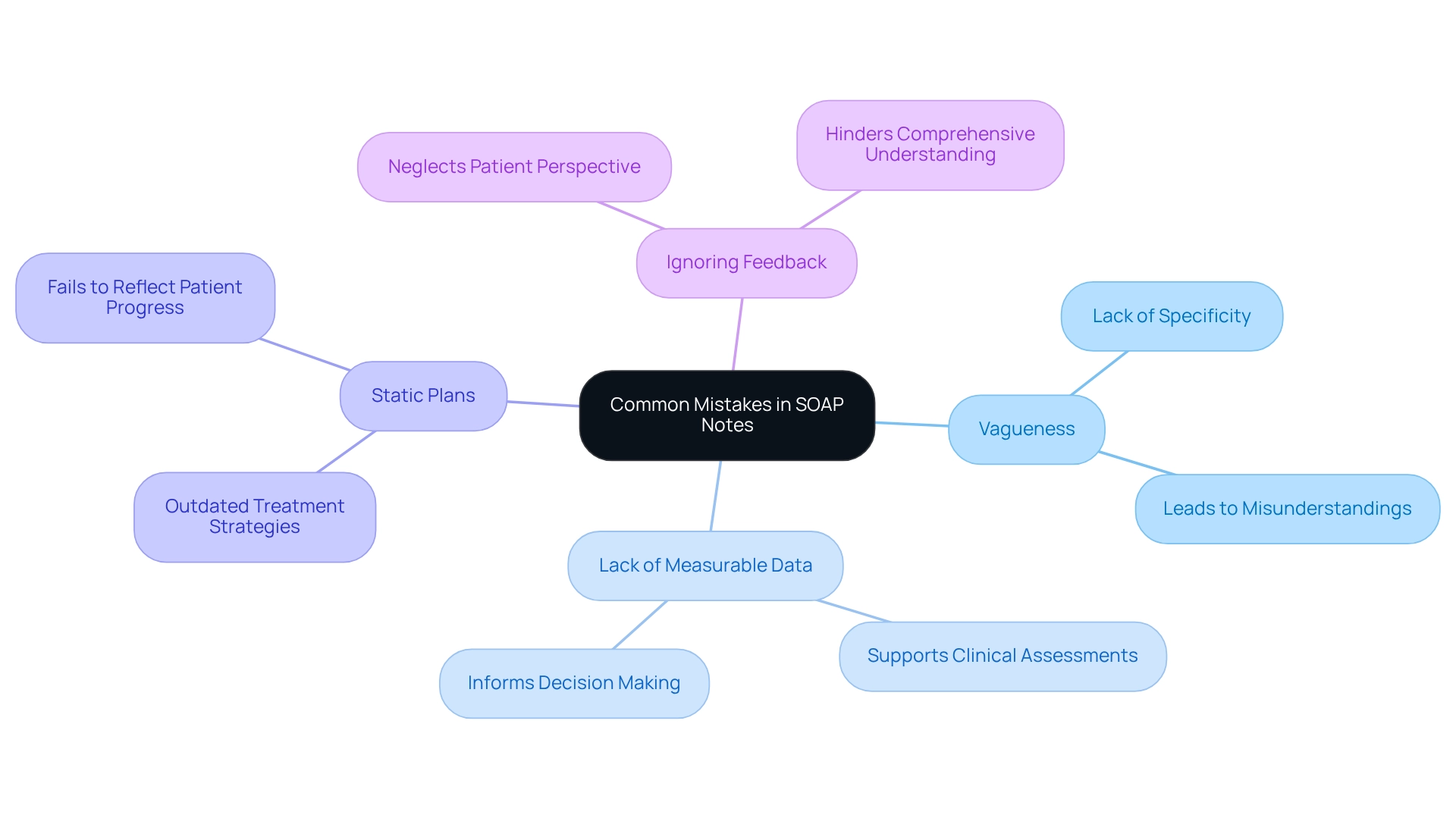
Creating clinical records can be challenging, and steering clear of common mistakes is essential for maintaining high-quality documentation. Have you ever felt overwhelmed by the details? Addressing typical pitfalls can significantly enhance your written accounts. Here are some key mistakes to watch for:
- Vagueness: Descriptions that lack specificity can lead to misunderstandings and hinder care.
- Lack of Measurable Data: The objective section should include quantifiable information to support clinical assessments and decisions.
- Static Plans: Failing to update the plan based on the assessment can result in outdated or ineffective treatment strategies.
- Ignoring Feedback: The subjective section should reflect the individual's perspective, as their input is vital for a comprehensive understanding of their condition.
By addressing these common errors, you can significantly enhance the clarity and effectiveness of your documentation. Enhanced records not only facilitate better patient outcomes but also contribute to your professional satisfaction. Recent insights emphasize the importance of precise records in patient-centered care. For instance, Simply.Coach has demonstrated that using adaptable templates can simplify the recording process. This enables therapists to concentrate more on client care while ensuring adherence to privacy regulations. As a result, the quality of records improves, leading to better client outcomes.
Providing clear, actionable guidance in the Plan section is essential. It ensures that patients feel informed and supported throughout their treatment journey. As the Simply.Coach Team states, 'You’re not just documenting symptoms but also ensuring that aligns with the client’s goals and progress in the long term.' By incorporating these practices, you can foster a more effective and patient-centered approach to healthcare documentation. Remember, every detail matters in making a difference in your patients' lives.
Conclusion
Effective documentation practices, particularly through the use of SOAP notes, are essential for enhancing patient care and reducing administrative burdens in healthcare settings. Healthcare providers often face overwhelming challenges in managing paperwork, which can detract from the quality of patient interactions. The structured format of SOAP notes—comprising Subjective, Objective, Assessment, and Plan—provides a clear framework that facilitates communication among providers, ensuring that critical patient information is accurately captured and easily accessible.
Innovative tools, such as AI-driven solutions like CosmaNeura and user-friendly templates from platforms like Headway and TextExpander, are transforming the documentation landscape. These technologies not only streamline the note-taking process but also allow clinicians to focus more on patient interactions rather than paperwork. By automating and simplifying documentation, healthcare professionals can improve their efficiency and ultimately enhance the quality of care they provide. How might your daily routine change if you could spend less time on documentation?
Moreover, the integration of tailored examples for specific specialties, such as ABA, mental health, and occupational therapy, underscores the versatility and importance of using structured SOAP notes. These examples illustrate how effective documentation can lead to better treatment planning and patient outcomes, reinforcing the notion that clear and precise notes are vital in the fast-paced environment of healthcare. Imagine the positive impact on patient care when documentation aligns seamlessly with clinical needs.
As healthcare continues to evolve, embracing efficient documentation practices is crucial. By prioritizing structured SOAP notes and leveraging modern technology, healthcare providers can navigate the complexities of patient care more effectively, ensuring that they remain focused on what truly matters—providing high-quality care to their patients. The journey towards improved documentation is not just about efficiency; it’s about fostering a culture of accountability, transparency, and compassion in healthcare delivery. Let’s take this step together, prioritizing patient care and enhancing our documentation practices for the better.




