Overview
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best patient care. The article highlights the importance of effective patient documentation, showcasing examples of doctor notes that can truly make a difference. By utilizing structured documentation formats, such as SOAP notes and billing notes, healthcare professionals can alleviate some of the administrative burdens that weigh heavily on their shoulders.
These documentation methods not only improve communication and accuracy but also enhance overall patient care. When all relevant information is systematically recorded and easily accessible, it empowers healthcare providers to focus on what truly matters—their patients. Imagine the peace of mind that comes from knowing that every detail is captured, allowing for informed decision-making and continuity of care.
As we explore these solutions, consider how implementing structured documentation can transform your practice. The benefits are clear: improved efficiency, reduced errors, and ultimately, better patient outcomes. We invite you to reflect on your current documentation practices and think about how small changes can lead to significant improvements in your workflow.
Let’s take action together. Embrace the power of effective documentation and create a supportive environment for both healthcare providers and patients. By prioritizing structured notes, we can foster a culture of care that resonates throughout the healthcare community.
Introduction
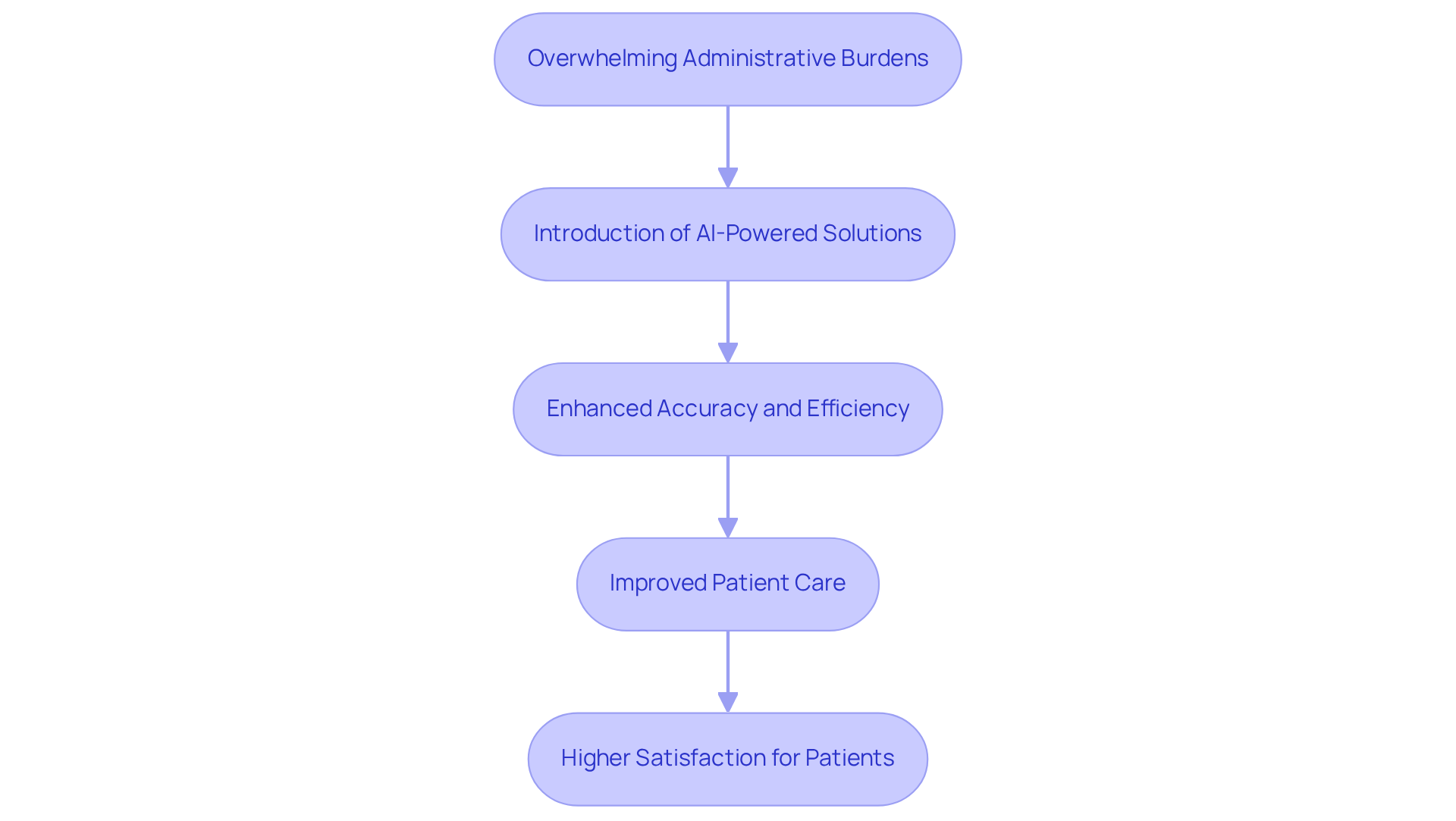
In the intricate landscape of healthcare, effective patient documentation is not merely a regulatory necessity; it is a cornerstone of quality care. Medical professionals often face emotional challenges as they navigate the complexities of record-keeping. These administrative burdens can detract from the time and attention they wish to devote to their patients.
What if there was a way to streamline this process? Imagine a scenario where providers could focus more on patient interaction rather than paperwork. The integration of structured note formats like SOAP notes, billing notes, and follow-up notes can significantly enhance both accuracy and efficiency.
Exploring various doctor note examples reveals techniques for effective documentation while also showcasing the transformative potential of AI solutions. How can healthcare practitioners leverage these tools to improve patient outcomes while ensuring meticulous record-keeping? Together, let’s consider the possibilities for creating a more compassionate and efficient healthcare environment.
CosmaNeura: Streamline Patient Documentation with AI-Powered Solutions
In today's fast-paced healthcare environment, many professionals grapple with overwhelming administrative burdens that detract from their primary focus: patient care. CosmaNeura understands these emotional challenges and introduces advanced AI technology to transform medical record processes. Imagine a world where healthcare providers can devote more time to treatment rather than paperwork—this is the promise of CosmaNeura's AI-driven solutions.
By significantly enhancing the accuracy and efficiency of record-keeping, CosmaNeura empowers providers to deliver high-quality care while upholding ethical standards aligned with Catholic teachings. This innovative approach not only simplifies workflows but also enriches the experience for individuals, ensuring that their records are both thorough and accurate. Have you ever wondered how much more you could achieve if you had those hours back?
With AI's remarkable ability to reduce clinical record-keeping time by as much as 45%, medical professionals can reclaim precious hours once consumed by administrative tasks. This shift not only leads to improved outcomes but also enhances satisfaction for those receiving care. As more medical organizations recognize the vital role of AI in their operations, the potential for improved efficiency and effectiveness in care becomes increasingly clear. Let’s take this step together towards in healthcare.
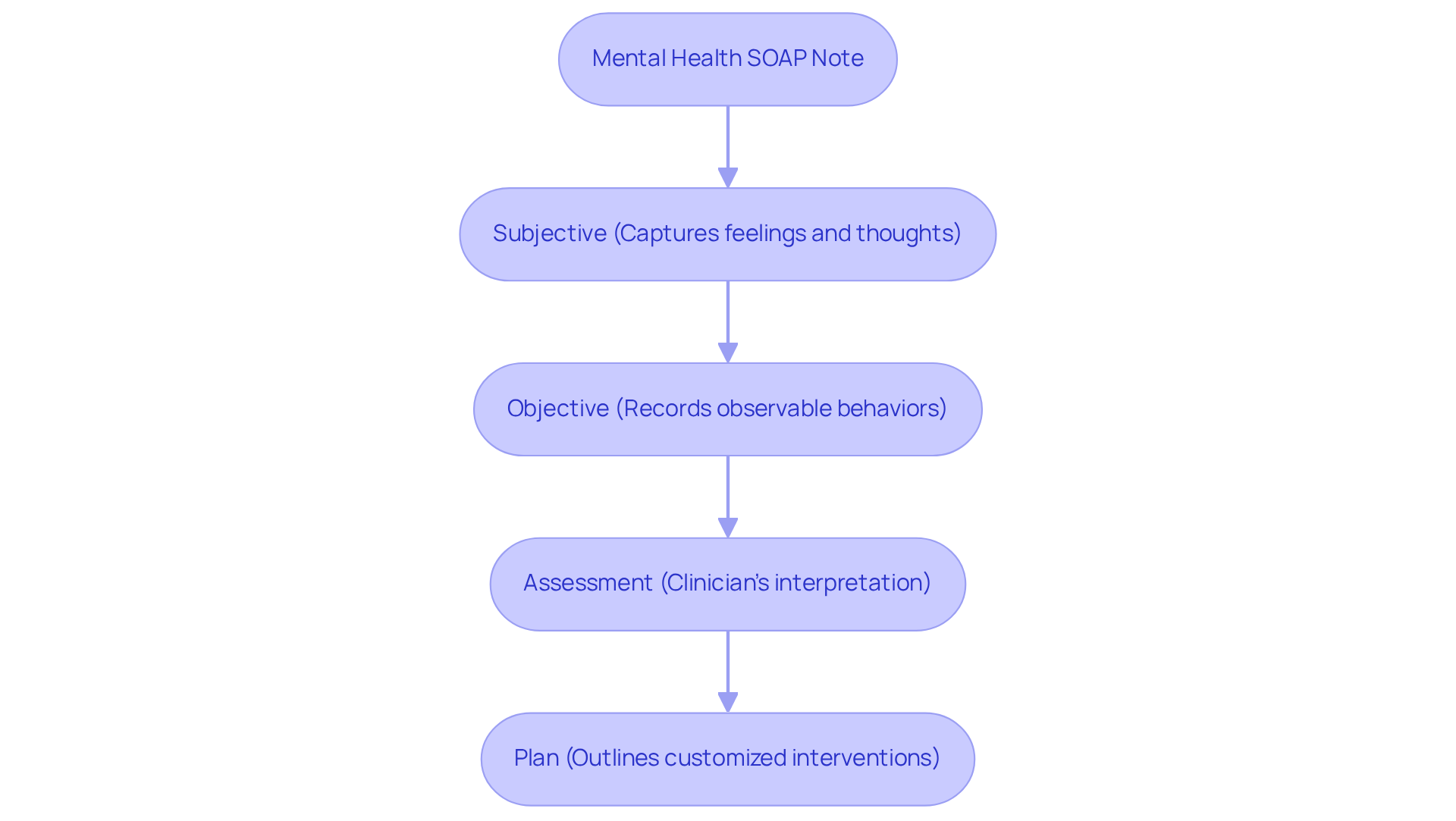
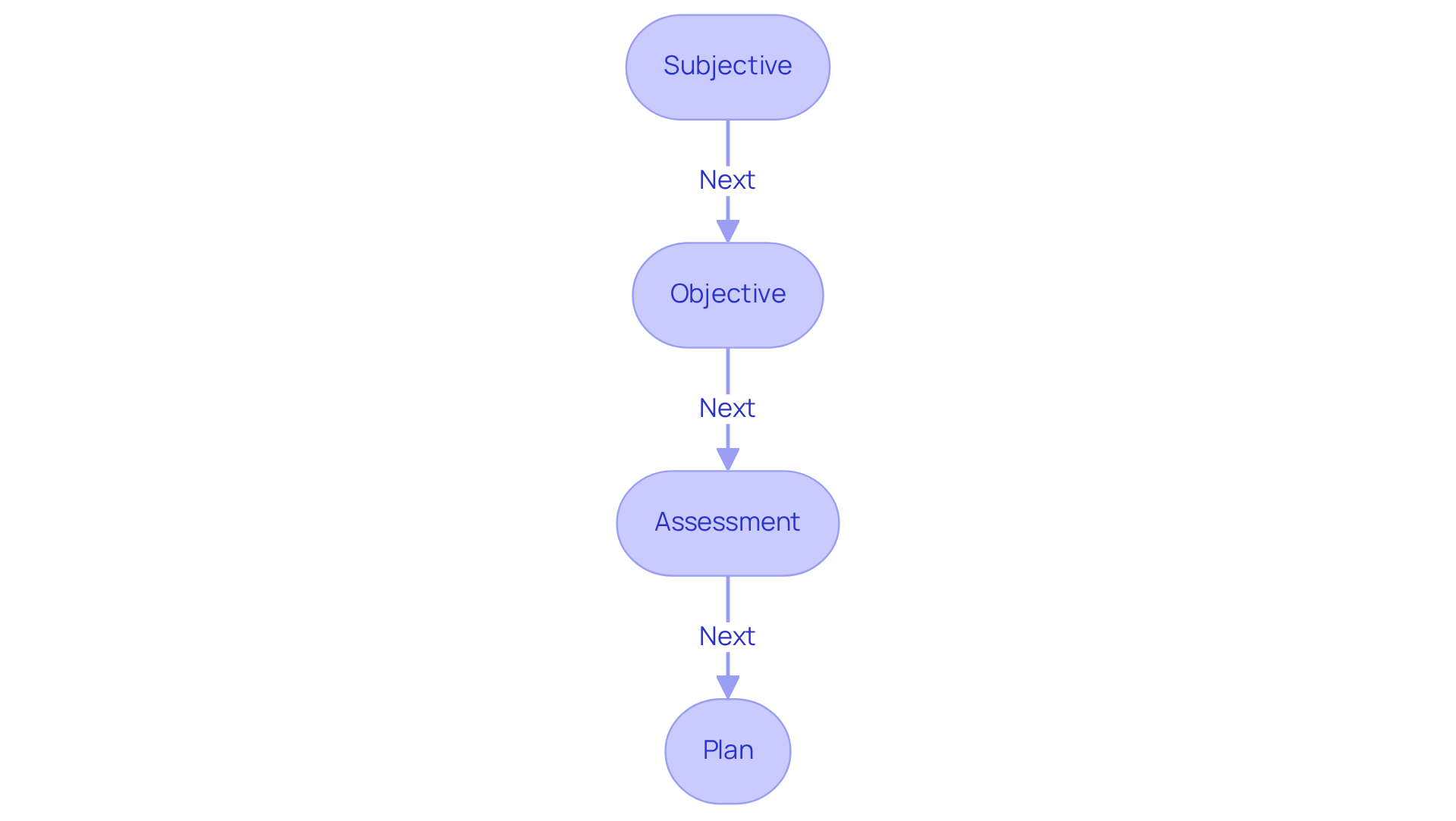
SOAP Note Example: A Comprehensive Template for Patient Interactions
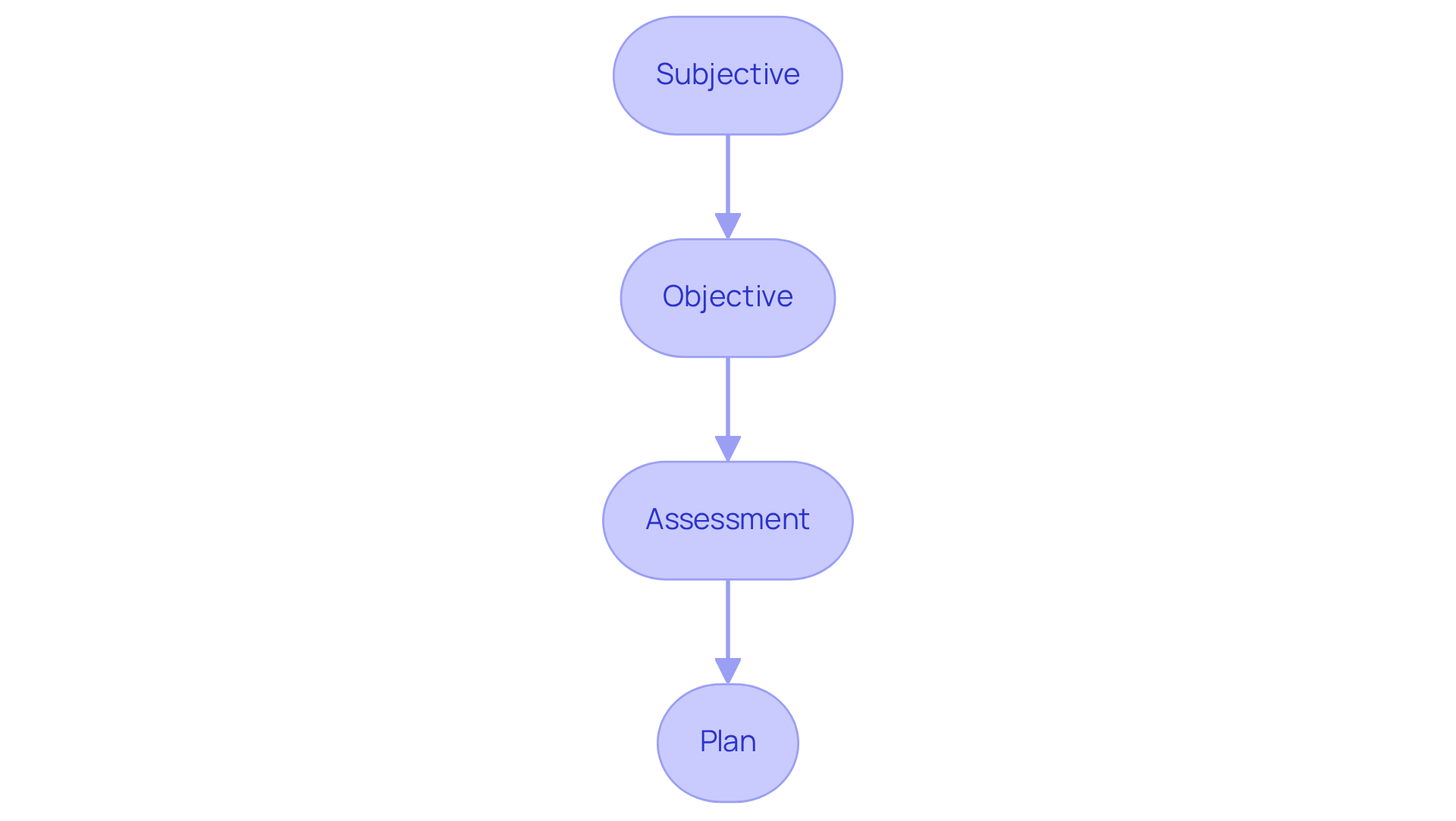
The SOAP note format serves as a vital tool in medical documentation, providing examples of doctor notes that encompass four key components: Subjective, Objective, Assessment, and Plan. This empowers healthcare providers to gather comprehensive client information efficiently.
Have you ever felt overwhelmed by the amount of information to process? The SOAP note begins with the Subjective section, where the individual's concerns and experiences are documented, often including direct quotes to maintain objectivity.
Following this, the Objective section captures measurable data, such as vital signs and physical examination findings, providing a solid foundation for the clinician's observations.
Next, the Assessment component synthesizes the information collected, allowing the provider to evaluate the individual's condition and consider potential diagnoses. This step is crucial—how can we truly understand our patients without this careful consideration?
Finally, the Plan outlines the recommended treatment strategies, including referrals, medications, and follow-up actions tailored to the individual's needs. By adhering to this organized framework, medical professionals can ensure that all relevant information, such as examples of doctor notes, is systematically documented, enhancing the quality of care and facilitating effective follow-up.
Let's embrace this structured approach to improve our practice and better serve our patients.
Medical Scribe Note Example: Enhancing Accuracy in Patient Records
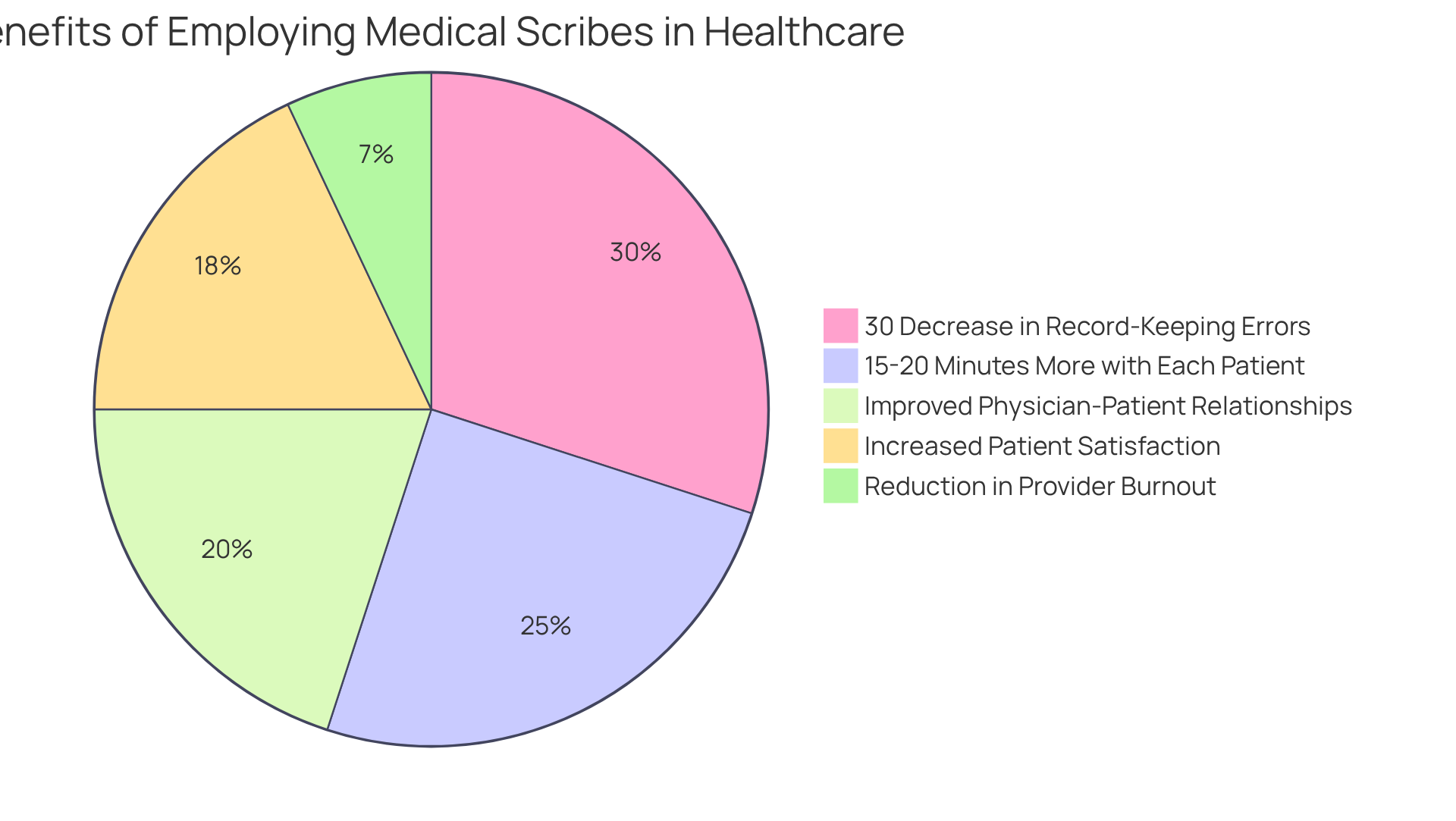
In the demanding world of healthcare, medical scribes serve as a vital support system. Examples of doctor notes typically include detailed observations recorded during visits, encompassing the individual's history, examination findings, and discussions about treatment options. For instance, a scribe might document vital signs, pertinent medical history, and examples of doctor notes that include the physician's recommendations. This thorough not only enhances the precision of client files but also allows healthcare professionals to focus more on client interaction rather than administrative tasks.
Have you ever considered how much time could be saved? Research indicates that practices employing medical scribes can achieve a 30% decrease in record-keeping errors, significantly improving safety and care quality for individuals. Moreover, with scribes managing documentation, physicians can gain an extra 15-20 minutes of direct interaction with each individual. This fosters better relationships and enhances overall satisfaction.
By ensuring that clinical notes are comprehensive and ready for billing or follow-ups without delays, scribes play an essential role in streamlining workflows and improving the efficiency of medical service delivery. In the face of challenges such as physician burnout and resistance to innovation, the integration of groundbreaking AI solutions like CosmaNeura's Agentic Platform can further enhance the capabilities of medical scribes. This allows for even greater reductions in administrative burdens and advancements in healthcare.
As Emma Johnson, a specialist in healthcare communication, wisely states, "By delegating this task to scribes, physicians can concentrate on care for individuals while ensuring records are precise." Imagine the possibilities when healthcare providers can focus more on what truly matters—their patients.
Telehealth Note Example: Documenting Virtual Patient Consultations Effectively
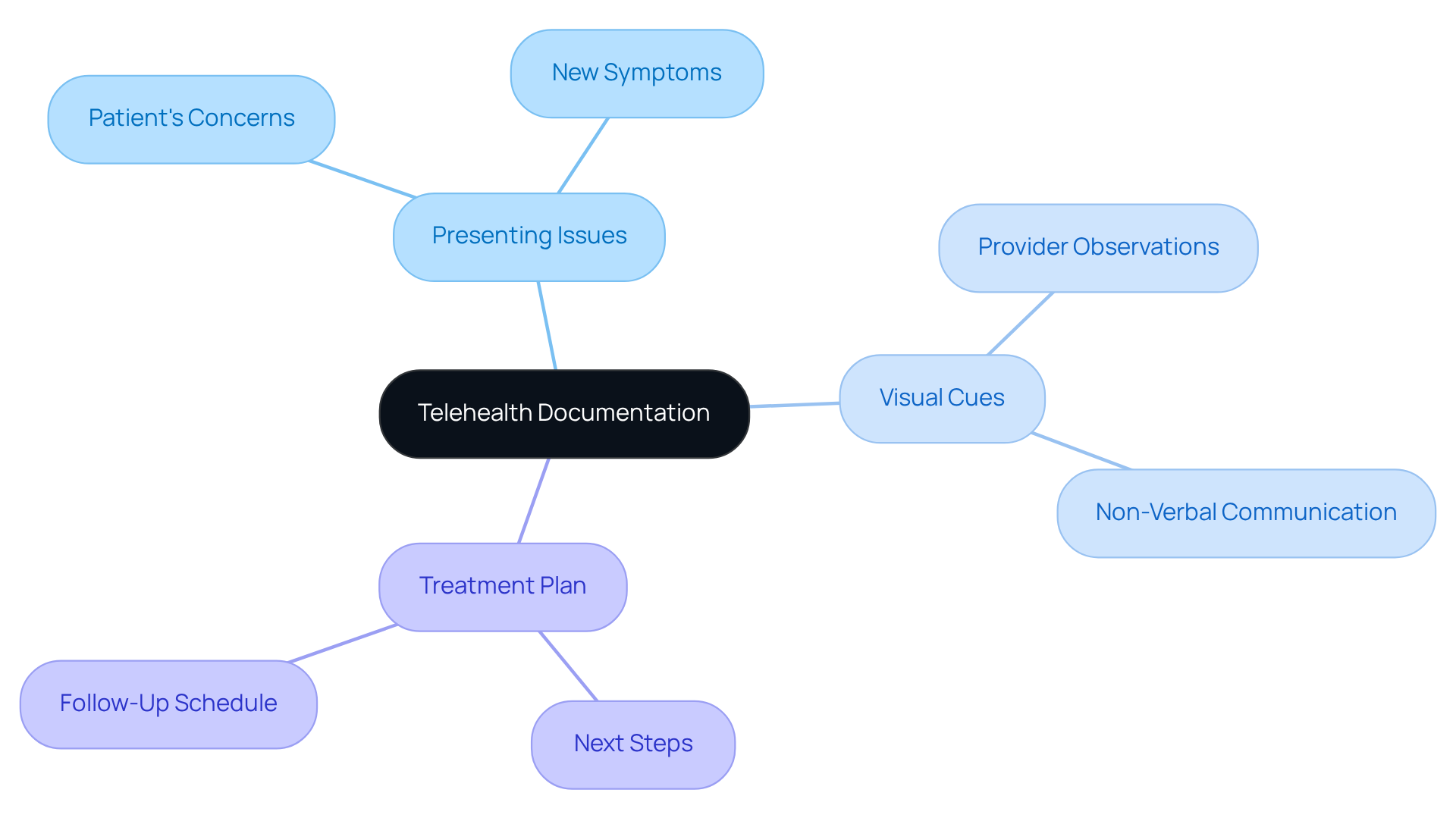
In the realm of telehealth, it's essential to recognize the emotional challenges healthcare providers face. The shift to virtual appointments can feel overwhelming, and thorough documentation is vital to ensure that client interactions are well-captured. Telehealth sessions should generate examples of doctor notes that include the same essential components as conventional face-to-face appointments, such as:
- The individual's presenting issues
- Any visual cues observed during the consultation
- The treatment plan discussed
Consider a well-crafted telehealth note that serves as examples of doctor notes, detailing an individual's concerns regarding a new symptom. It should reflect the provider's assessment based on visual observations and outline the agreed-upon next steps. This comprehensive record not only promotes continuity of support but also serves as a crucial reference for upcoming consultations.
It's heartening to note that over 80% of doctors believe telehealth improves access to services, and 62% feel their clients are more satisfied since utilizing these virtual options. Keeping precise and comprehensive notes is crucial for enhancing the virtual experience. Moreover, with telehealth services gaining popularity—utilized by 74.4% of doctors in 2022, almost three times that of 2018— become essential for guaranteeing high-quality care and satisfaction.
Additionally, as 54.9% of physicians now use telehealth to manage chronic diseases, a significant increase from 9.9% in 2018, the need for comprehensive documentation is increasingly pressing. By embracing these practices, we can ensure that our clients receive the compassionate care they deserve, even in a virtual setting.
Mental Health SOAP Note Example: Capturing Patient Insights and Treatment Plans
In a mental health SOAP note, the Subjective section captures the individual's feelings and thoughts, providing insight into their emotional state. Have you ever considered how these insights can shape our understanding of a patient's needs? The Objective section records observable behaviors, such as body language or speech patterns, which can be critical for understanding the individual's condition. These details matter deeply. The Assessment reflects the clinician's interpretation of the individual's mental state, synthesizing subjective and objective data to form a diagnosis. Finally, the Plan outlines therapeutic interventions customized to the individual's needs, ensuring a tailored approach to care.
For instance, examples of doctor notes, like a mental health SOAP note, might outline an individual's reported anxiety symptoms, including sensations of restlessness and trouble focusing. The therapist's observations during the session, such as fidgeting and avoidance of eye contact, would be noted in the Objective section. The Assessment could indicate a diagnosis of generalized anxiety disorder, while the Plan might include a treatment strategy involving cognitive-behavioral therapy (CBT) sessions, relaxation techniques, and follow-up appointments.
Efficient record-keeping like this not only assists in monitoring individual progress but also improves communication among healthcare professionals. Isn't it reassuring to know that better communication can lead to better treatment results? By capturing comprehensive patient insights, clinicians can ensure that treatment plans are responsive to the evolving needs of their patients, fostering a more effective therapeutic alliance. Moreover, with 21% of adults facing at least one mental health condition, the significance of comprehensive records in mental health services cannot be emphasized enough.
Tackling challenges in record-keeping methods, such as time limitations and insufficient training, is crucial for enhancing the quality of care. Training health professionals can significantly ; those who receive training are 4.2 times more likely to document effectively. Furthermore, employing electronic systems for record-keeping can enhance practices, facilitating providers in maintaining precise and thorough records. By incorporating generative AI into these documentation processes, healthcare providers can streamline their workflows, reduce administrative burdens, and ultimately improve the quality of service. How can we support each other in overcoming these challenges together?
Nursing Note Example: Essential Elements for Comprehensive Patient Care
Nursing notes play a crucial role in effective client management, encompassing vital signs, medication administration, client responses, and any changes in condition. Have you ever considered how a comprehensive nursing note might detail an individual's temperature, the administration of pain medication, and the reported pain level? This detailed record is essential for ensuring that all members of the medical team are well-informed about the individual's status, facilitating timely and informed decisions regarding treatment.
The significance of nursing records extends beyond single client interactions; they enhance communication among medical professionals, ensuring continuity of care. Research indicates that nurses who utilize organized record-keeping formats are three times more likely to provide sufficient records. This highlights the importance of . Furthermore, effective nursing notes contribute to improved patient care quality, as they offer a clear record of interventions and outcomes, which is vital for evaluating treatment efficacy. In Ethiopia, it is noted that only 50% of nursing services are properly recorded, underscoring the need for enhancements in record-keeping practices.
Consider the impact of incorporating examples of doctor notes into effective nursing record-keeping practices. For instance, documenting an individual's reaction to a new medication not only informs the medical team but also aids in adjusting treatment plans based on real-time feedback. Additionally, highly motivated nurses are found to be 27 times more likely to engage in proper record-keeping, emphasizing the significance of motivation in improving record quality. By prioritizing thorough and precise nursing notes, healthcare providers can significantly enhance care coordination and overall quality, ultimately leading to improved health outcomes.
However, insufficient records can lead to increased patient mortality and medical errors, highlighting the urgent need to enhance nursing record-keeping practices. Technological solutions, such as those offered by CosmaNeura, which provide real-time transcription and summarization for telehealth sessions, can further improve efficient record-keeping methods. By embracing these advancements, we can foster a nurturing environment that prioritizes patient care and well-being.

Pediatric SOAP Note Example: Tailoring Documentation for Young Patients
When crafting a , it's vital to consider the child's developmental stage and actively involve parents or guardians in the process. Have you ever thought about how a parent's insights can illuminate a child's emotional landscape? For instance, in the Subjective section, a clinician might note a parent's observations about their child's persistent sadness or anxiety regarding school. The Objective section should encompass measurable data, such as the child's growth metrics or behavioral assessments, providing a clear picture of their well-being.
The Assessment reflects the clinician's professional evaluation of the child's overall health, integrating both subjective reports and objective findings. This comprehensive approach fosters a deeper understanding of the child's needs. Ultimately, the Plan must detail any essential interventions, referrals, or follow-up actions tailored to the child's individual requirements. For example, arranging a follow-up session in one week can ensure continuity of support, reinforcing the child's journey towards improved mental health.
This thorough and personalized method enhances the significance of the records while promoting better communication and continuity of care for young patients. As Vivian Chung Easton highlights, documenting therapy sessions with children and adolescents necessitates a unique approach, as their needs, treatment, and challenges differ from those of adult clients. Furthermore, maintaining accurate documentation is not only a legal and ethical responsibility for therapists but also a crucial element in capturing all relevant information efficiently.
Utilizing examples of doctor notes, specifically SOAP notes designed for children and adolescents, leads to improved communication, enhanced treatment planning, and legal compliance. This ultimately benefits the overall care provided to young clients, nurturing their growth and development in a supportive environment.
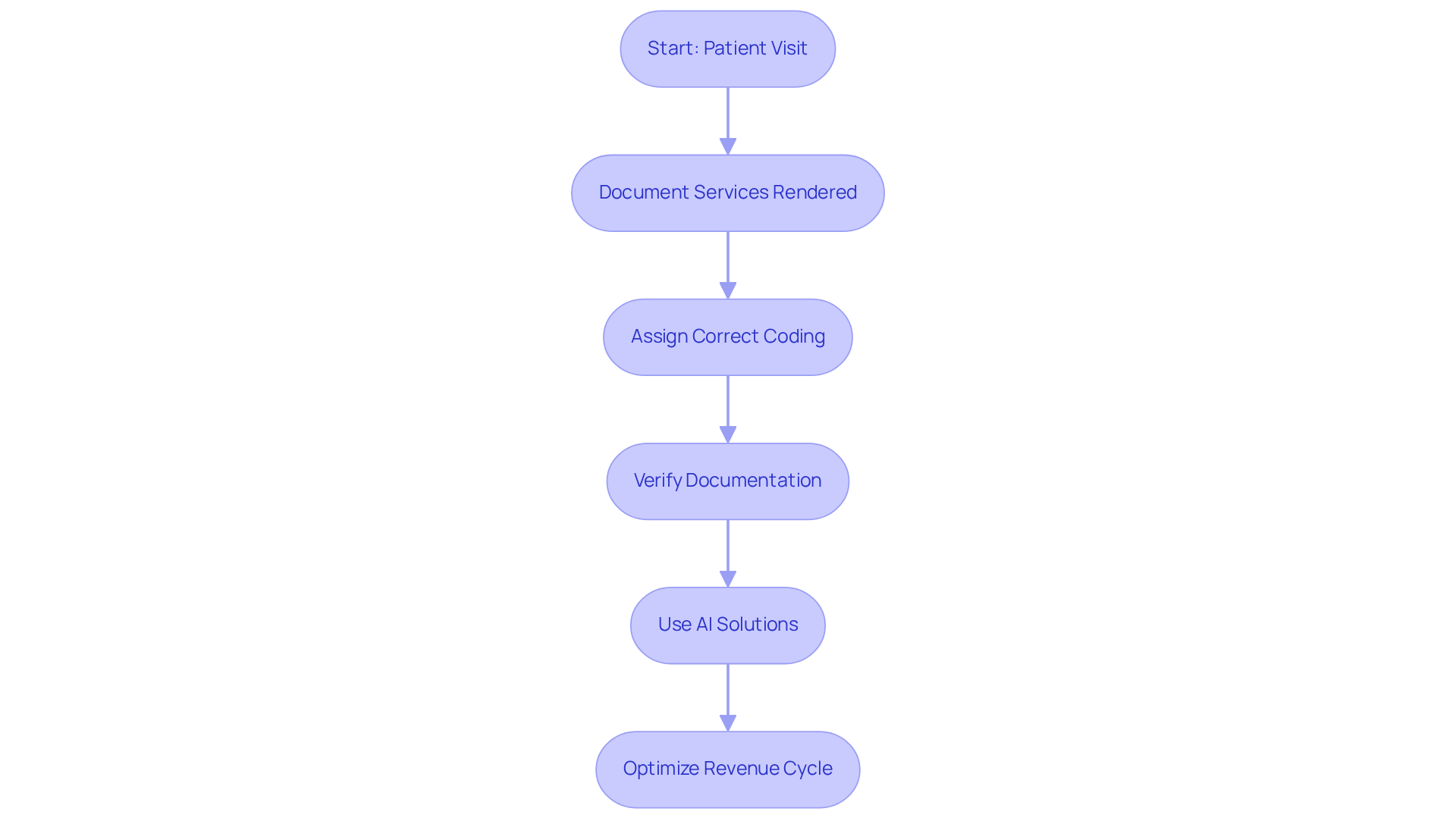
Billing Note Example: Ensuring Accurate Coding and Revenue Optimization
In the demanding world of healthcare, providers often feel overwhelmed by the complexities of billing. A comprehensive billing note is not just a formality; it serves as a vital tool that encompasses detailed information about the services rendered, the corresponding billing codes, and relevant client details, which may include examples of doctor notes. For example, when documenting a patient's visit for a specific procedure, it is crucial to refer to examples of doctor notes that include the relevant CPT code to ensure clarity and accuracy. This meticulous approach is essential for optimizing the revenue cycle and significantly reducing the risk of billing errors, which can lead to substantial financial losses.
Consider this: statistics show that precise medical coding can increase providers' revenue by as much as 20%. However, coding mistakes can result in costs of approximately $36 billion each year. With nearly 50% of all Medicare claims containing errors and 80% of medical bills overall containing inaccuracies, the need for is paramount. Have you ever encountered the frustration of duplicate billing? It's a common error that can lead to serious implications, including fraud charges.
By employing efficient billing methods, such as using AI-driven solutions like those provided by CosmaNeura, healthcare providers can protect their financial stability and improve trust among clients. This not only promotes a more sustainable practice but also allows providers to focus more on what truly matters: patient care. Let’s work together to ensure that every detail is captured accurately, fostering a healthier financial future for your practice.
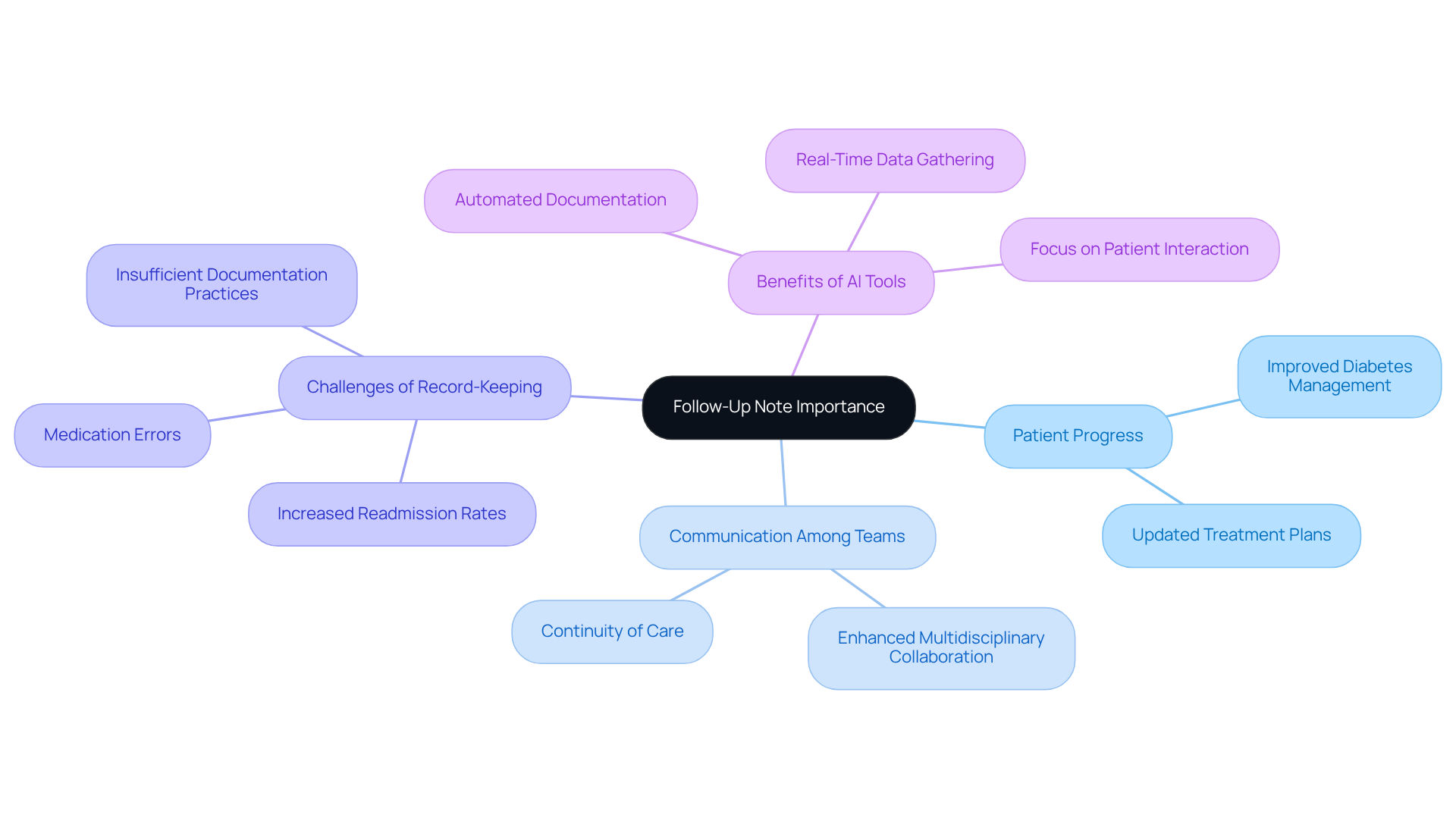
Follow-Up Note Example: Documenting Patient Progress and Future Care Plans
A follow-up note is crucial for summarizing an individual's progress since their last visit, capturing any changes in symptoms or treatment responses. Have you ever considered how these notes can reflect an individual’s journey? For instance, examples of doctor notes might include details on an individual’s improved management of diabetes, such as updated blood sugar levels and adjustments to the treatment plan. This thorough is vital for enabling medical professionals to make informed decisions about ongoing treatment, ultimately supporting the individual's health journey.
High-quality follow-up notes not only enhance communication among multidisciplinary teams but also ensure continuity of care, which is essential for patient safety. Have you experienced the challenges of insufficient record-keeping? Such methods can lead to negative outcomes, like increased readmission rates and medication errors, underscoring the need for comprehensive and precise follow-up notes in medical environments.
By leveraging generative AI, medical providers can automate the documentation process, ensuring that follow-up notes are created swiftly and accurately. Imagine the relief of having AI tools assist in gathering relevant individual information and treatment updates. This allows medical professionals to focus more on meaningful interactions with individuals rather than administrative tasks.
Therefore, thorough and accurate examples of doctor notes, enhanced by AI tools, are essential in healthcare settings. They not only streamline processes but also foster a nurturing environment for individuals, ensuring that their health journey is supported every step of the way.
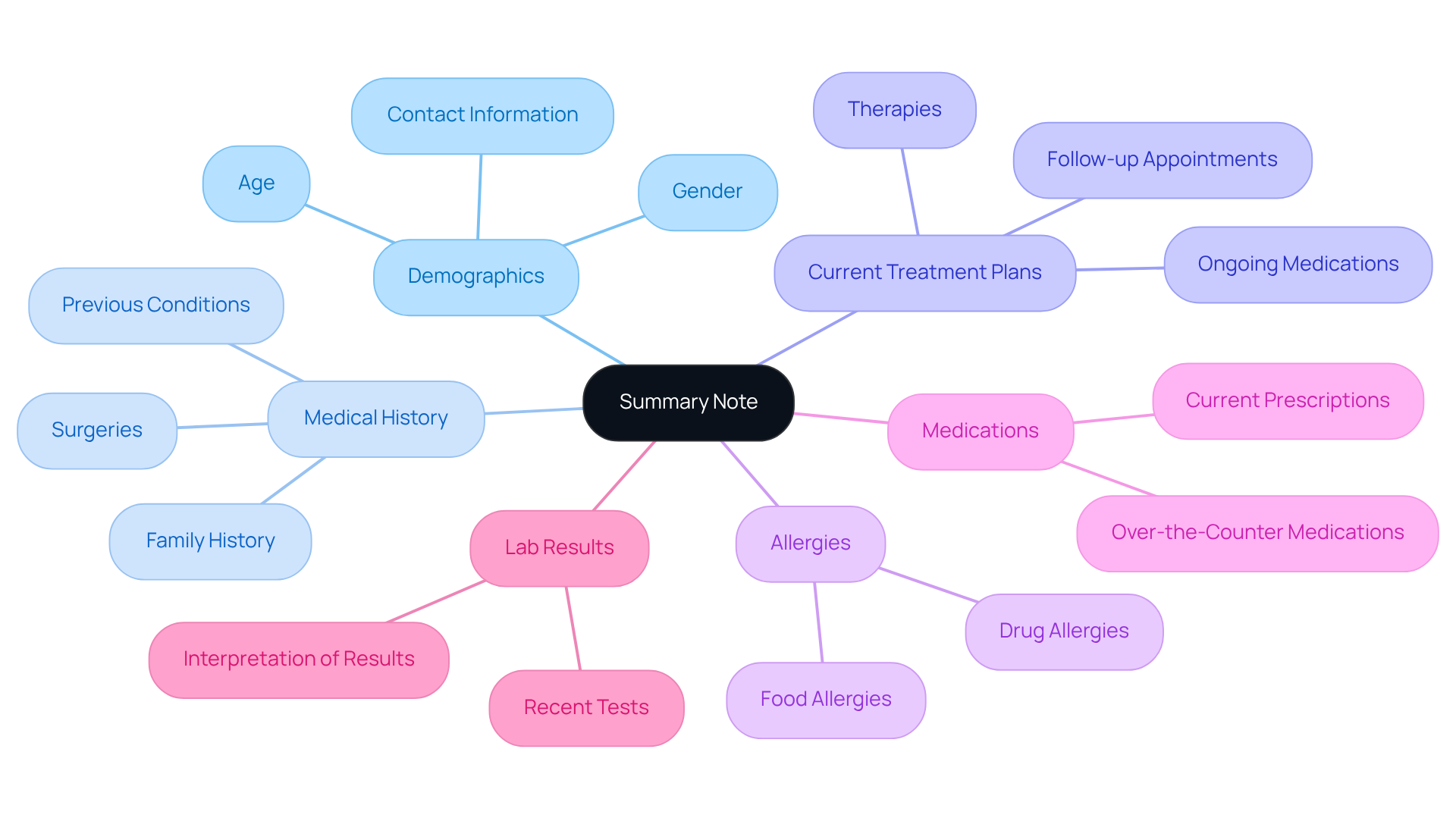
Summary Note Example: Quick Reference for Patient Information and Care Coordination
In the fast-paced world of healthcare, a summary note becomes an invaluable resource, encapsulating essential individual information such as demographics, medical history, and current treatment plans. Have you ever felt overwhelmed by the sheer volume of details to remember? A well-crafted summary note can ease that burden, outlining critical aspects like allergies, medications, and recent lab results. This swift guide is not just a convenience; it’s essential for [medical practitioners during consultations](https://blog.cosmaneura.com/10-essential-md-548-instructions-for-healthcare-providers), ensuring they have all readily accessible. This promotes a smoother coordination of services, ultimately benefiting patient care.
As one healthcare expert insightfully noted, "A Medical Summary Report plays a crucial role in care by providing a comprehensive overview of an individual’s medical history, current condition, and treatment plan, facilitating continuity of care." By streamlining access to critical data, summary notes significantly enhance provider efficiency, allowing for more focused and informed patient interactions. Imagine the difference it can make when healthcare providers can devote their full attention to patients, knowing they have the necessary information at their fingertips.
Incorporating summary notes into daily practice not only alleviates stress but also fosters a nurturing environment for both patients and providers. Let’s embrace this tool together, ensuring that we prioritize what truly matters—compassionate and effective patient care.
Conclusion
In the healthcare landscape, effective patient documentation is not just a task; it is a cornerstone for ensuring high-quality care and seamless operations. The integration of structured documentation methods, such as SOAP notes and detailed billing records, empowers healthcare providers to maintain comprehensive and accurate patient records. This ultimately enhances the quality of care delivered. By embracing innovative solutions like CosmaNeura's AI-driven technology, professionals can significantly reduce the administrative burden. This shift allows them to focus more on meaningful patient interactions and less on overwhelming paperwork.
Throughout this article, we’ve explored various examples of doctor notes that illustrate how different documentation formats serve specific purposes. From capturing mental health insights to optimizing billing processes, each note type—be it a nursing note, telehealth documentation, or a follow-up summary—plays a crucial role in fostering effective communication among healthcare teams. It ensures continuity of care, which is vital for patient safety and treatment outcomes. The importance of accuracy in these records cannot be overstated; it directly impacts the well-being of those we serve.
As the healthcare industry continues to evolve, adopting advanced documentation practices—enhanced by AI solutions—becomes essential. This not only promotes efficiency but also nurtures a compassionate environment where patient care remains the top priority. By embracing these strategies, we can pave the way for a future where healthcare providers deliver the best possible care. This is backed by precise and thorough documentation that supports their efforts every step of the way. Let’s work together to create a healthcare experience that prioritizes both efficiency and compassion.




