Overview
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver the best patient care. This article highlights the importance of clinical documentation, showcasing methods like SOAP notes, progress notes, and electronic health records (EHR) that can alleviate some of these burdens. By adopting structured documentation practices, healthcare professionals can enhance communication among themselves, significantly reduce administrative tasks, and ultimately lead to improved patient outcomes.
Imagine how much smoother your workflow could be with accurate and consistent clinical records. When documentation is streamlined, it not only lessens the load on providers but also fosters a nurturing environment for patients. This is crucial in ensuring that every patient receives the attention and care they deserve. The benefits of effective documentation extend beyond just efficiency; they create a foundation for trust and understanding between healthcare providers and patients.
As we navigate these challenges together, consider how adopting these documentation methods can transform your practice. By prioritizing structured documentation, you can enhance the quality of care you provide, making a meaningful impact on your patients' lives. Embrace this opportunity to improve not just your workflow, but the overall healthcare experience for everyone involved. Let's work towards a future where effective communication and compassionate care go hand in hand.
Introduction
In the intricate world of healthcare, maintaining precise and effective clinical documentation is not just a task; it’s a vital component that can profoundly affect patient care and outcomes. Many healthcare providers face the emotional challenge of balancing their responsibilities, often feeling overwhelmed by administrative tasks that detract from meaningful patient interactions. With the rise of advanced technologies like AI, there are now unprecedented opportunities to streamline documentation processes, allowing providers to focus more on what truly matters—their patients.
However, as the demand for accurate records continues to grow, so does the challenge of ensuring that these documents meet legal, ethical, and practical standards. How can healthcare professionals harness these innovative tools to enhance their documentation practices? By prioritizing patient well-being, they can create a more compassionate healthcare environment.
Imagine a scenario where healthcare providers can reduce their administrative burdens, leading to more time spent with patients. This not only improves the quality of care but also fosters stronger patient-provider relationships. It’s essential to explore how technology can support this shift, making documentation less of a chore and more of a seamless part of patient care.
As we navigate these changes together, let’s reflect on how we can embrace these tools to enhance our practices. What steps can we take to ensure our documentation is not only efficient but also empathetic? By working collaboratively, we can create a healthcare system that values both accuracy and compassion, ultimately benefiting everyone involved.
CosmaNeura: Streamline Clinical Documentation with AI-Powered Solutions
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from their ability to focus on patient care. CosmaNeura understands these challenges and utilizes advanced AI technology to transform clinical record-keeping procedures. By automating patient intake, triage, and documentation, this innovative platform allows medical professionals to dedicate more time to compassionate service, fostering individual well-being.
Imagine the relief of significantly improving clinical workflow efficiency. With practices utilizing AI, there is an impressive potential for up to a . This not only alleviates the administrative burden but also means that medical providers can save an estimated 200,000 hours each day. Such efficiency gains highlight how technology can empower healthcare professionals to focus on what truly matters—their patients.
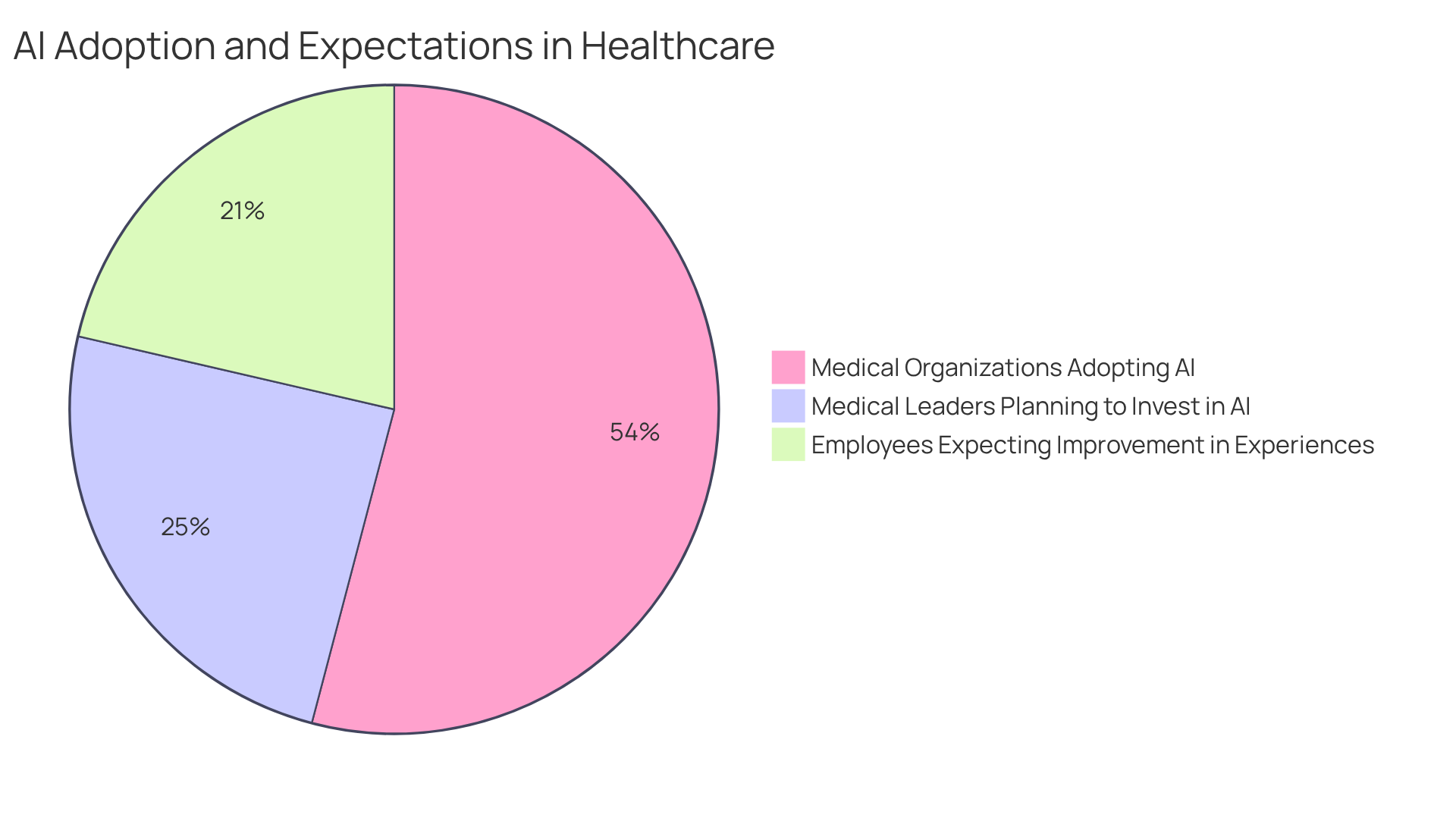
CosmaNeura's commitment to aligning its operations with Catholic teachings reinforces the importance of patient-centered care, ensuring ethical standards in medical delivery remain a priority. As the medical landscape evolves, examples of clinical documentation demonstrate that the role of AI in simplifying documentation becomes essential. Currently, 86% of medical organizations are embracing AI to enhance operational efficiency and client outcomes.
What does this mean for employees? A notable 34% anticipate that AI will improve experiences for individuals, reflecting a growing appreciation for AI's positive influence in the sector. As medical leaders increasingly invest in AI—39% planned to do so for predicting outcomes and supporting clinical decisions in 2023—the transformative potential of AI in clinical workflows becomes ever more apparent.
Let's embrace this change together, recognizing that with the right tools, we can create a healthcare environment that prioritizes compassion and care.
SOAP Notes: Essential Structure for Effective Patient Documentation
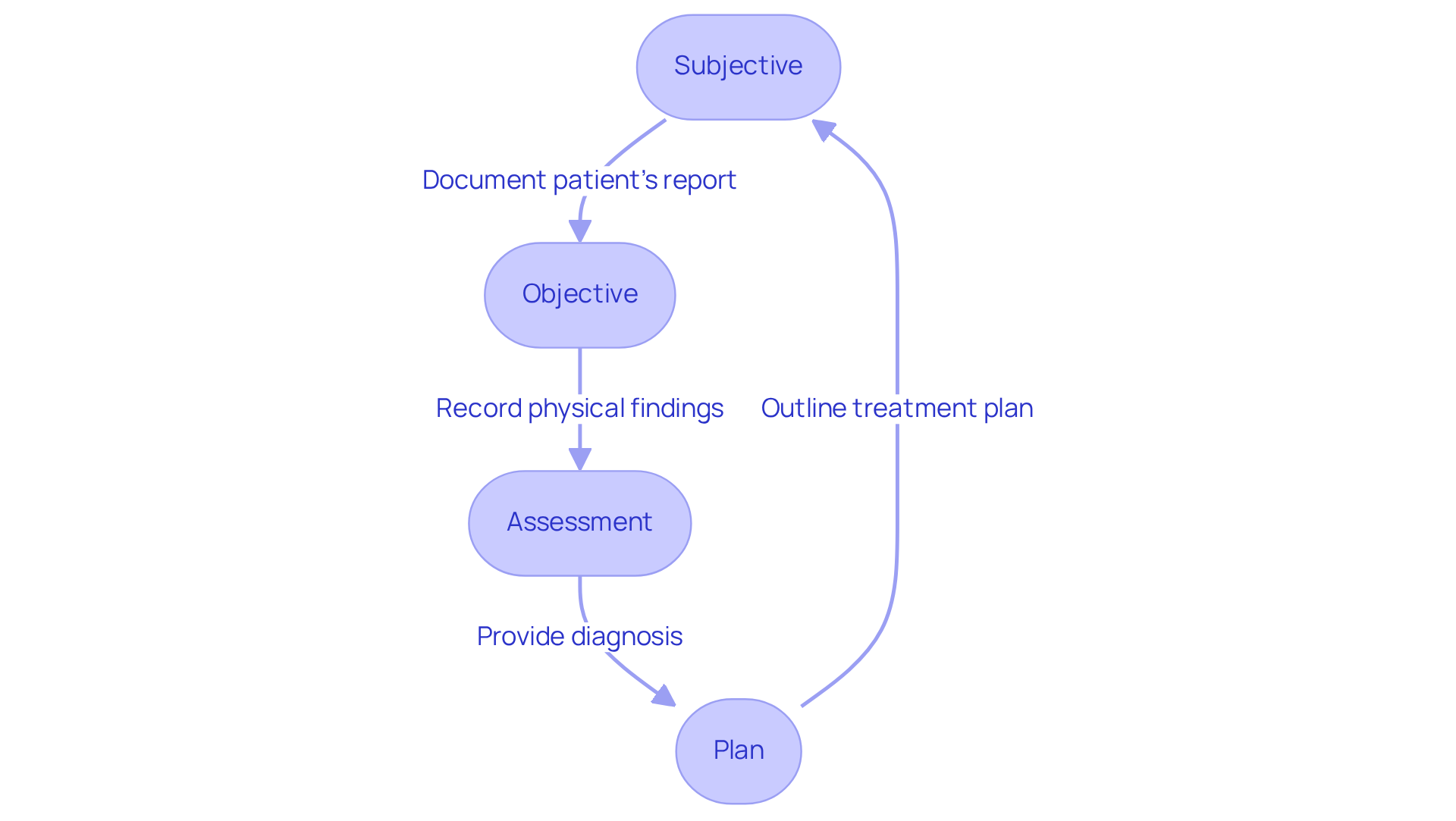
SOAP notes—Subjective, Objective, Assessment, and Plan—serve as a vital tool in the healthcare field. They provide a structured framework for documenting client encounters, which includes examples of clinical documentation to ensure that all relevant information is captured systematically. This format not only facilitates better communication among healthcare providers but also addresses the emotional challenges they face daily.
Have you ever felt overwhelmed by administrative tasks? SOAP notes are important examples of clinical documentation that significantly improve the quality of healthcare by clearly outlining subjective reports, objective findings, clinical assessments, and treatment plans. They support continuity in treatment, allowing providers to focus more on their patients rather than paperwork.
Examples of clinical documentation for writing SOAP notes include best practices such as:
- Timely record-keeping
- Clear language
- Adherence to HIPAA guidelines
These practices promote effective communication and collaboration among interdisciplinary teams. Imagine how much smoother your workflow could be with organized records!
Research shows that organized records via SOAP notes positively influence treatment outcomes. They facilitate information exchange and minimize errors, ultimately leading to enhanced satisfaction and health results. Notably, physicians spend about 35% of their time recording client information. This statistic underscores the necessity for effective documentation methods like SOAP notes.
Furthermore, AI-driven SOAP notes can save clinicians 6-10 minutes per visit. This time-saving feature significantly and improves overall efficiency in healthcare. Embracing these tools can lead to a more fulfilling practice, allowing you to devote more time to what truly matters—your patients.
Progress Notes: Continuous Monitoring of Patient Health
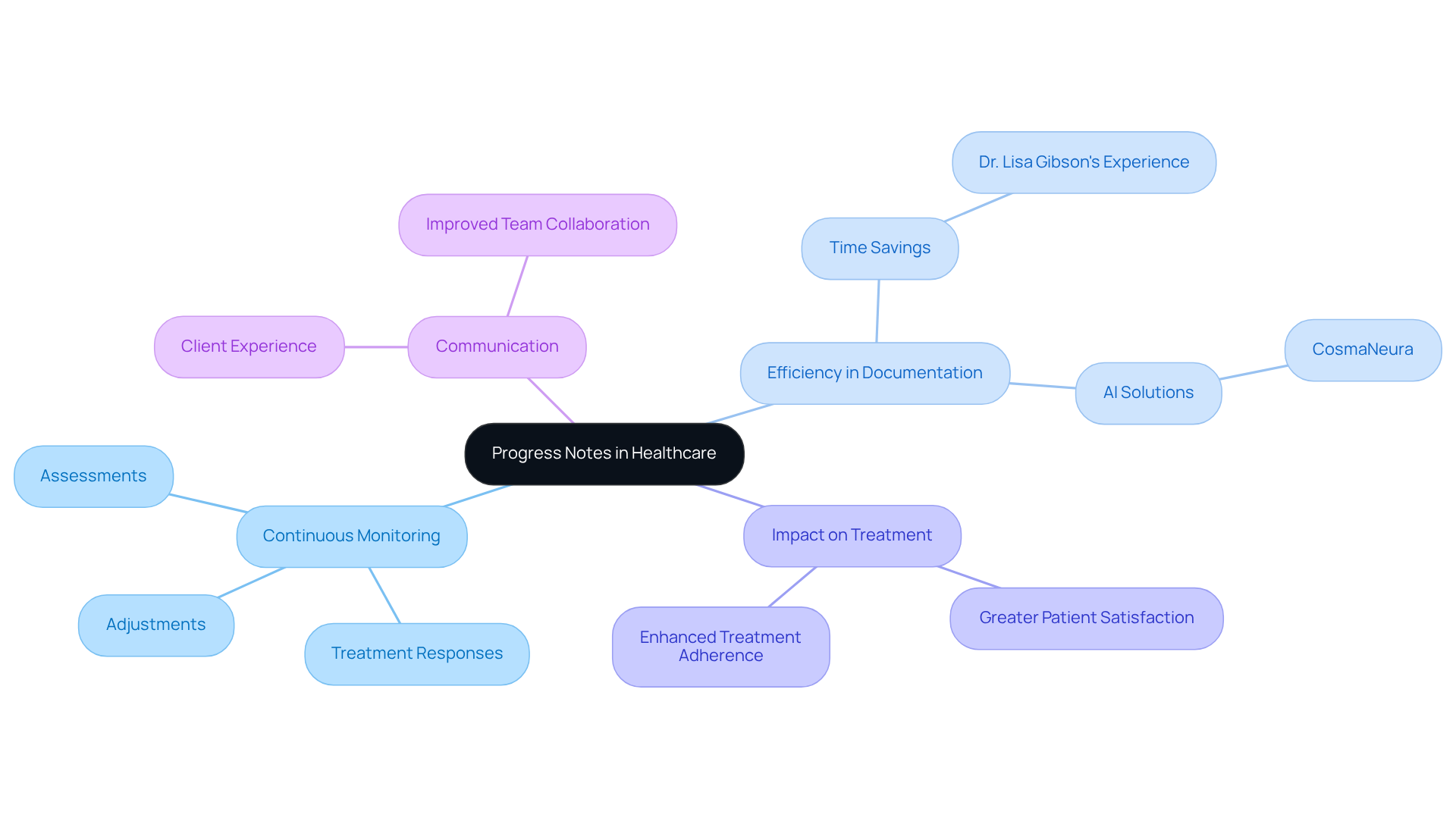
Progress notes are important examples of clinical documentation for healthcare providers, serving as a comprehensive record of ongoing assessments and treatment responses. These notes are examples of clinical documentation that meticulously document changes in a person's condition, the effectiveness of treatments, and any necessary adjustments to treatment plans. By maintaining detailed progress notes, providers can ensure continuous monitoring of individual health, which is crucial for delivering high-quality, responsive care.
Have you ever considered how much time could be saved with effective documentation? For instance, Dr. Lisa Gibson shared that she saved over two hours each day in record-keeping by utilizing a values-based progress notes template. This allowed her to focus more on her interactions with clients. Such efficiency underscores the in enhancing treatment effectiveness and monitoring responses.
Moreover, the frequency of updates to progress notes is vital. Regular documentation, such as examples of clinical documentation, not only aids in clinical decision-making but also fosters improved communication among medical teams. As medical leaders have emphasized, prioritizing client experience through diligent documentation is not merely an additional task; it is a fundamental responsibility that significantly impacts outcomes for individuals.
In today's healthcare landscape, where opioid-related adverse events rank among the top three reported medication-related issues and alarm fatigue poses a national safety challenge, the importance of progress notes is magnified. They provide a systematic approach to individual support, ensuring that all interactions are recorded and assessed. This ultimately leads to enhanced treatment adherence and greater individual satisfaction.
Let’s reflect on how we can improve our documentation practices together. By embracing effective progress notes, we can create a more compassionate and efficient healthcare environment.
Nursing Notes: Capturing Comprehensive Patient Care Insights
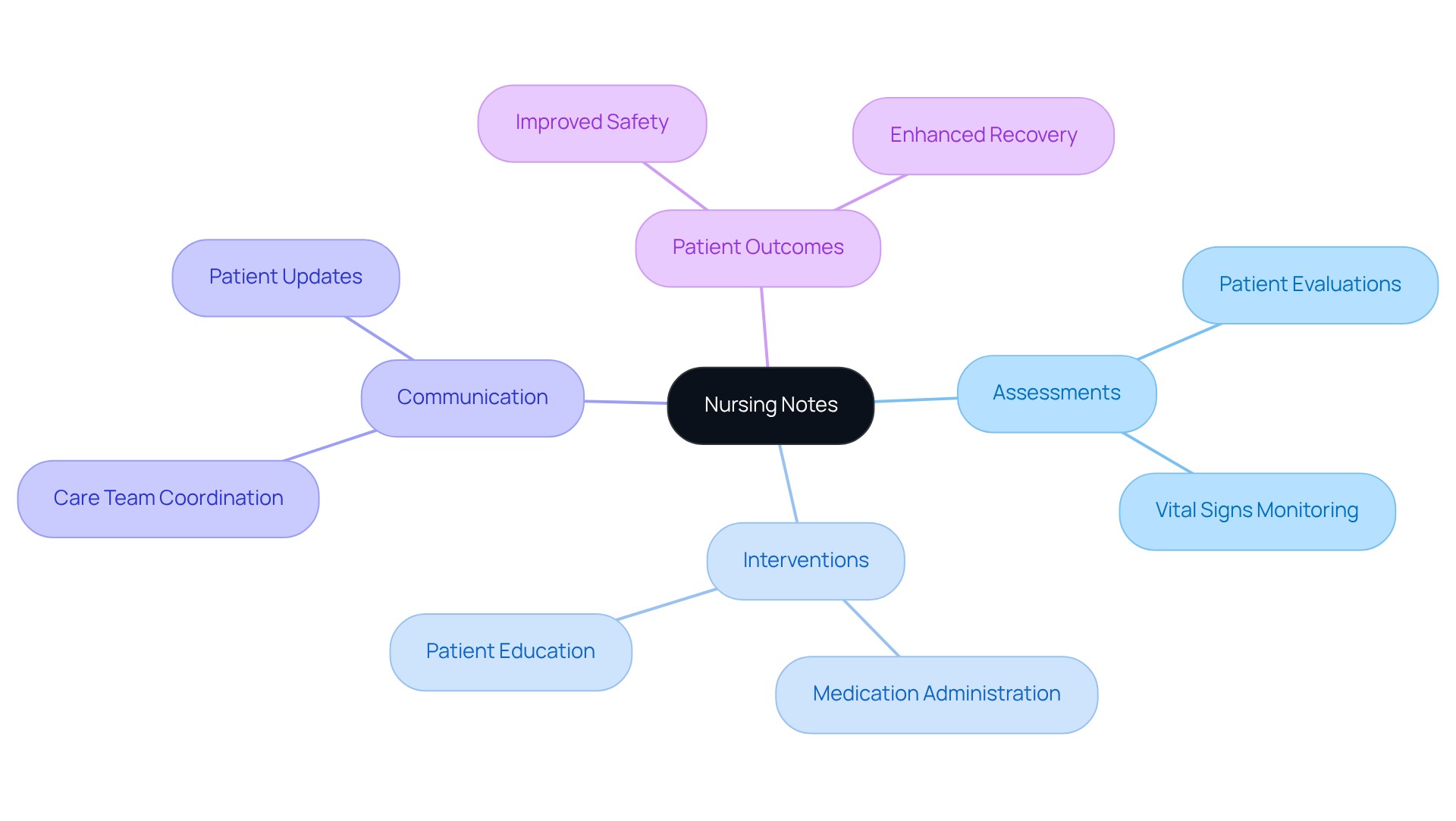
Nursing notes are essential examples of clinical documentation that capture the intricate details of client management, including assessments, interventions, and responses. Have you ever felt overwhelmed by the need to document every aspect of care? These notes not only provide a thorough account of the nursing process but also ensure that each element of individual support is thoughtfully recorded.
By maintaining precise and prompt nursing notes, medical providers can significantly enhance communication within the care team. This practice ultimately leads to improved safety and better outcomes for individuals. Imagine the peace of mind that comes from knowing every detail is documented and shared effectively.
Let’s embrace the importance of these notes together. By committing to this essential practice, we can foster a supportive environment that prioritizes both patient care and team collaboration. Your dedication to keeping can make a meaningful difference in the lives of those you serve.
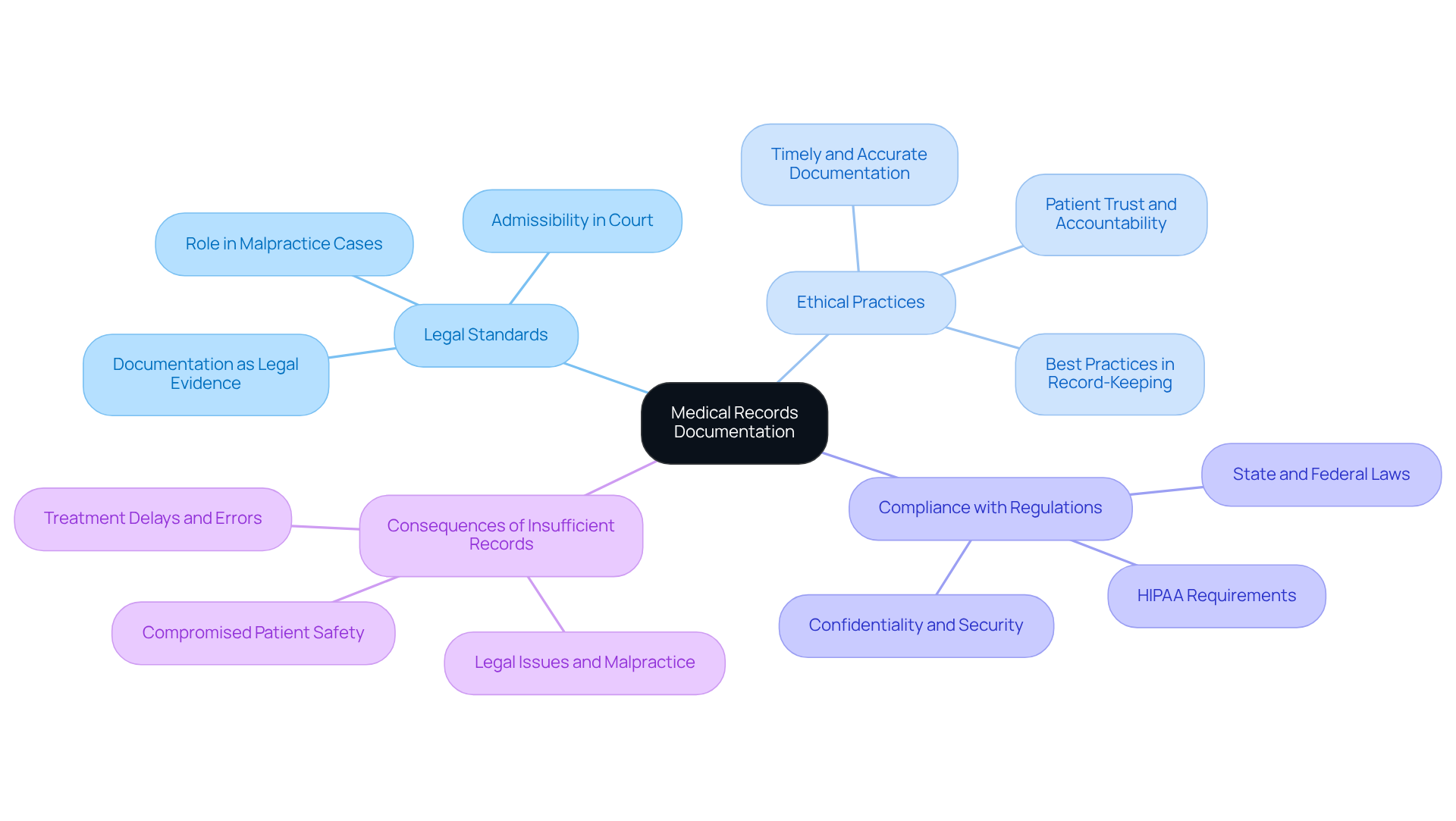
Medical Records Documentation: Upholding Legal and Ethical Standards
Precise medical records recording is crucial for upholding legal and ethical standards in the medical field. These records serve as vital legal documents that can significantly impact disagreements or evaluations. It’s essential to maintain detailed and accurate examples of clinical documentation that encompass all interactions, assessments, and treatments involving individuals. By adhering to these standards, healthcare providers not only safeguard themselves but also foster trust and accountability within the healthcare system.
Have you considered the serious consequences of insufficient records? They can lead to legal issues and compromise patient safety, as seen in numerous malpractice cases where record-keeping errors played a critical role. Furthermore, compliance with regulations like HIPAA is essential. These regulations protect individual privacy and ensure that medical records are handled with the utmost confidentiality.
Ethical record-keeping practices, such as timely and accurate data management, are not just best practices; they are fundamental to delivering quality service and preserving the integrity of the medical profession. As emphasized in the industry, 'If you didn’t document it, you didn’t do it.' This underscores the importance of meticulous record-keeping and the use of examples of clinical documentation in creating a trustworthy medical environment.
Prompt reporting and diligent record-keeping can prevent severe injuries and additional complications. This highlights the essential role of precise records in healthcare. Let’s work together to enhance our practices and ensure that every detail is captured, ultimately leading to better care for our patients.
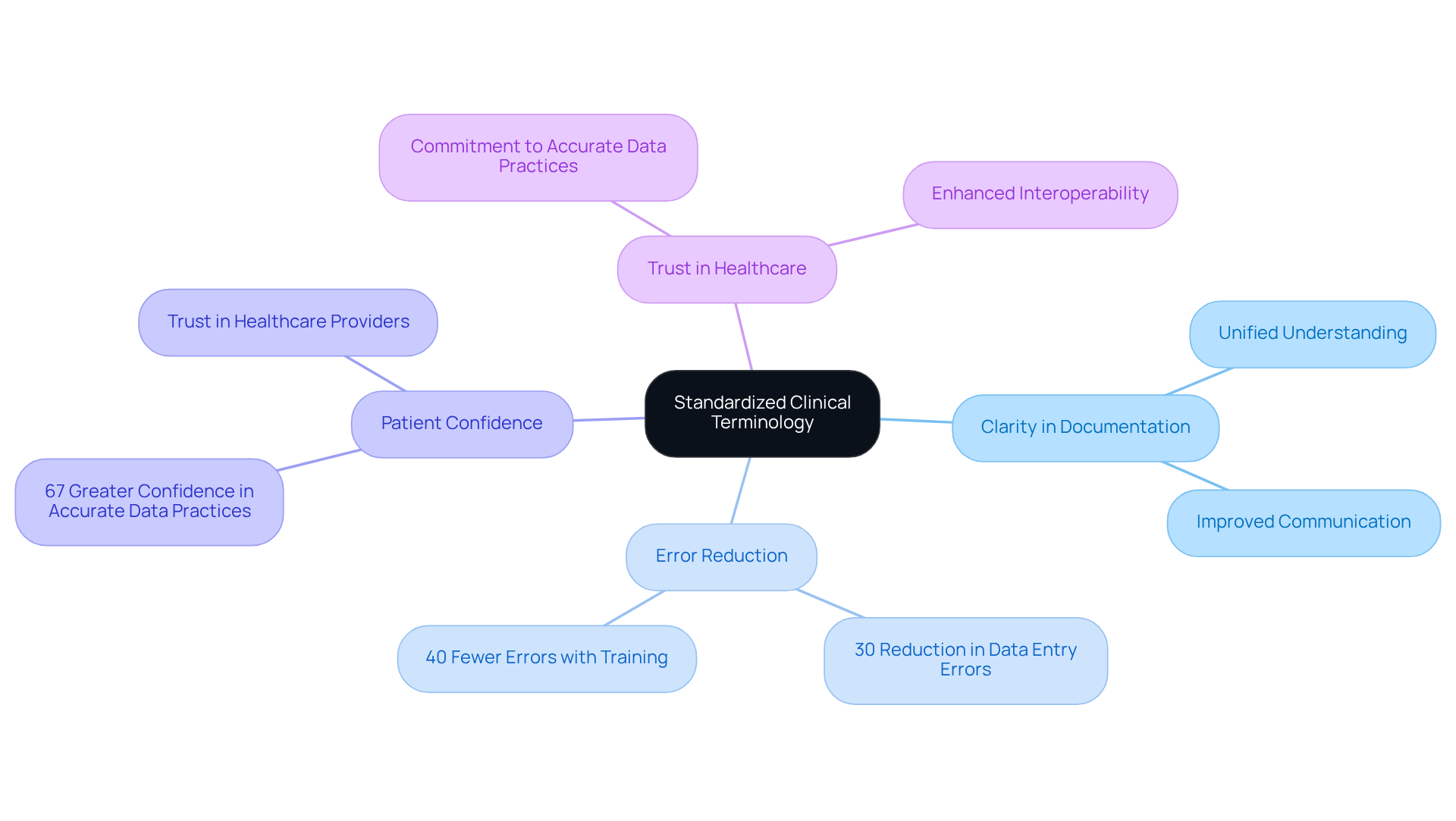
Clinical Terminology: Enhancing Clarity in Patient Documentation
In the fast-paced world of healthcare, misunderstandings can lead to serious consequences. Using standardized clinical terminology in examples of clinical documentation is a powerful way to enhance clarity and foster understanding among medical professionals. When healthcare teams adopt and definitions, they create a unified understanding of conditions, treatments, and plans. This clarity is not just a matter of efficiency; it is crucial for effective communication and collaboration, ultimately leading to improved care outcomes.
Consider this: organizations that implement standardized terminologies report a 30% reduction in errors related to data entry. Furthermore, those that conduct regular training experience 40% fewer errors, showcasing the tangible benefits of clear communication. Have you ever wondered how much more confident patients would feel knowing their healthcare providers are on the same page? Research indicates that facilities using standardized coding systems achieve a remarkable 40% improvement in the precision of health metrics. This highlights the essential role of terminology in promoting reliable documentation, such as examples of clinical documentation, and building trust.
Significantly, 67% of individuals express greater confidence in facilities that demonstrate a commitment to accurate and consistent data practices. This connection between standardized terminology and trust cannot be overstated. In practice, the use of standardized terminologies like NANDA-I, NIC, and NOC not only enhances interoperability but also facilitates value-based services, optimizing safety and quality of care.
A scoping review identified 3,547 studies related to standardized terminologies in nursing and midwifery practice, underscoring their effectiveness. As healthcare continues to evolve, the commitment to clear and consistent examples of clinical documentation remains a cornerstone of effective care management. As Nat Turner aptly stated, "Good communication is the bridge between confusion and clarity."
At CosmaNeura, we align with these principles, dedicated to improving treatment through the use of standardized terminology. Together, let’s bridge the gap between confusion and clarity, ensuring that every patient receives the compassionate and effective care they deserve.
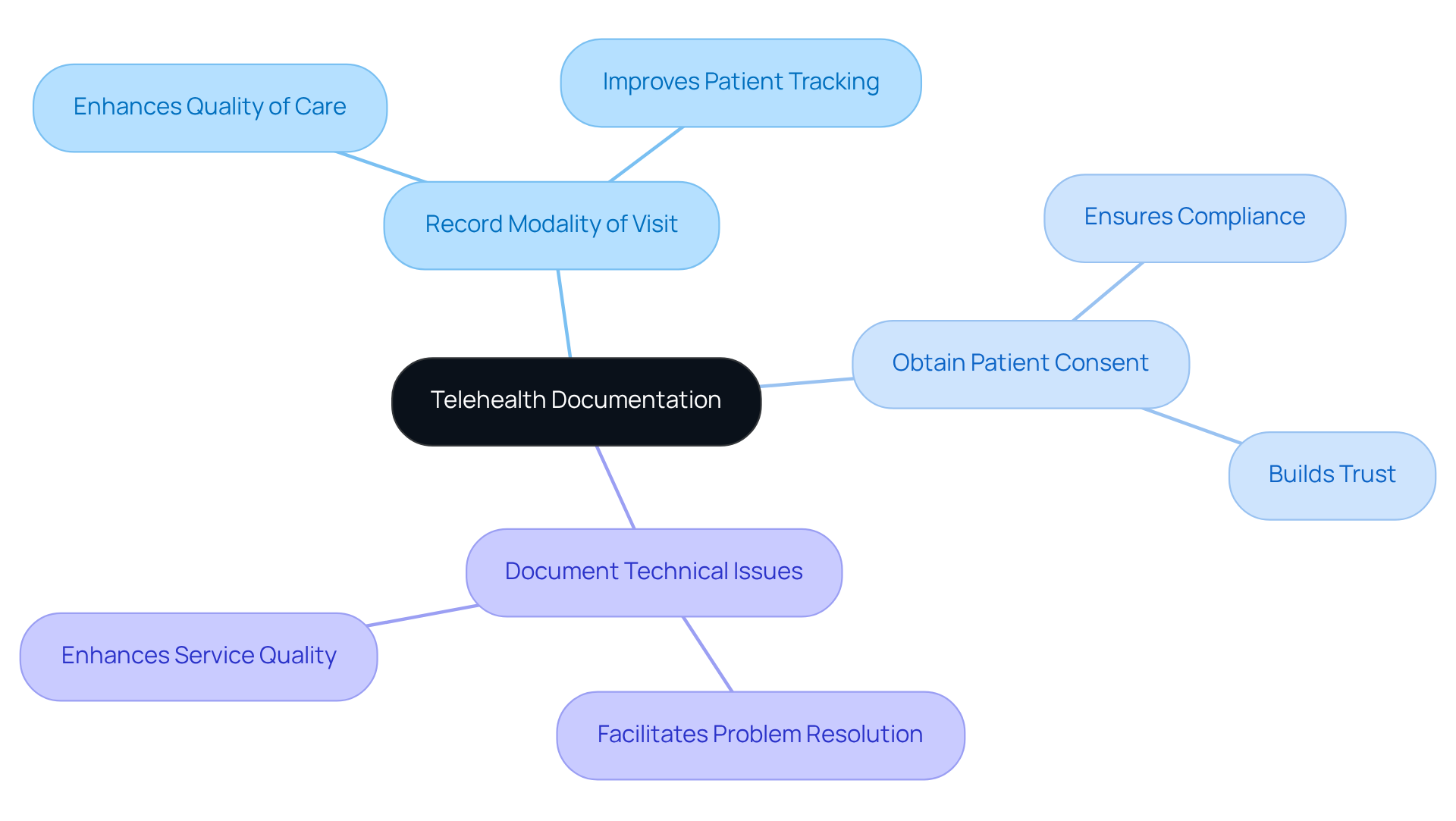
Telehealth Documentation: Adapting to New Healthcare Delivery Models
Telehealth documentation can feel overwhelming for many healthcare providers. It requires careful attention to specific elements to maintain compliance and ensure the provision of quality service. Providers must record the modality of the visit, obtain consent from the individual, and document any technical issues that may occur during the session. This thorough method not only meets legal requirements but also significantly enhances the overall quality of healthcare.
Consider how maintaining detailed records can improve continuity of care. It allows for better tracking of patient progress and treatment outcomes, which is essential in providing compassionate care. Moreover, comprehensive records serve as protection against possible legal disputes, ensuring that providers can demonstrate compliance with established standards.
As telehealth progresses, the significance of thorough records remains crucial in building trust and transparency in patient-provider relationships. Reflect on this: based on a recent survey, 68% of physicians indicated a wish to utilize telehealth services more often. This emphasizes the increasing importance of accurate records in our evolving healthcare landscape.
Julia Shaver, MD, highlights that telemedicine can be comparable to face-to-face care for specific conditions. This underscores the necessity for to facilitate this shift. By embracing these practices, we can foster a more supportive environment for both providers and patients.
Key Solutions for Effective Telehealth Documentation:
- Record the modality of each visit.
- Obtain clear consent from patients.
- Document any technical issues that arise.
By focusing on these elements, including examples of clinical documentation, we can collectively enhance the quality of care we provide, ensuring that our patients feel valued and understood.
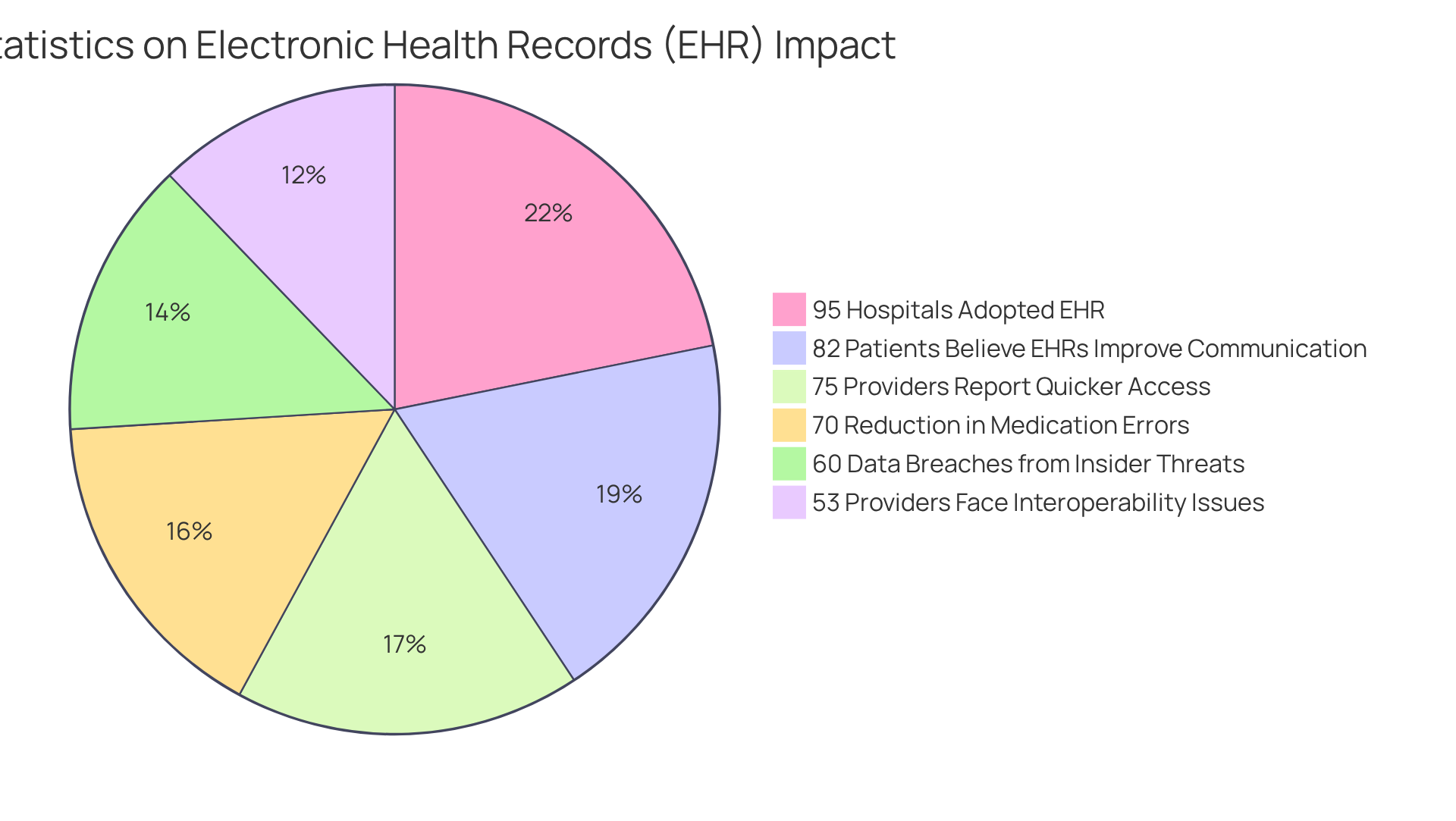
Electronic Health Records (EHR): Revolutionizing Patient Documentation
Electronic Health Records (EHR) have truly transformed the way we record health information, providing a centralized, digital platform for managing individual data. Imagine the relief of knowing that over 95% of hospitals in the U.S. have adopted EHR systems, significantly enhancing accessibility and streamlining documentation processes. This has led to an impressive 75% of providers reporting quicker access to client information. Furthermore, it’s heartening to know that 82% of patients believe EHRs improve communication between medical providers, fostering better care coordination.
However, we must acknowledge the challenges that persist in this evolving landscape. Data entry mistakes remain a concern, with 60% of medical data breaches attributed to insider threats, underscoring the importance of robust employee training. Additionally, 53% of healthcare providers face hurdles with EHR interoperability, and the potential for information overload can hinder clinical decision-making. It’s crucial to implement effective strategies to manage the vast amounts of data generated. Addressing these challenges is essential to fully optimize the advantages of EHR systems in clinical practice, ensuring they continue to facilitate efficient and effective care.
Moreover, it’s encouraging to note that EHR implementation has led to an average reduction of 70% in medication errors, highlighting their positive impact on patient safety. As we look ahead, the worldwide EHR market is expected to expand to USD 43.62 billion by 2032, reflecting the growing significance of these systems in medical services. Together, we can navigate these challenges and , ensuring that they serve as a powerful tool for enhancing patient care.
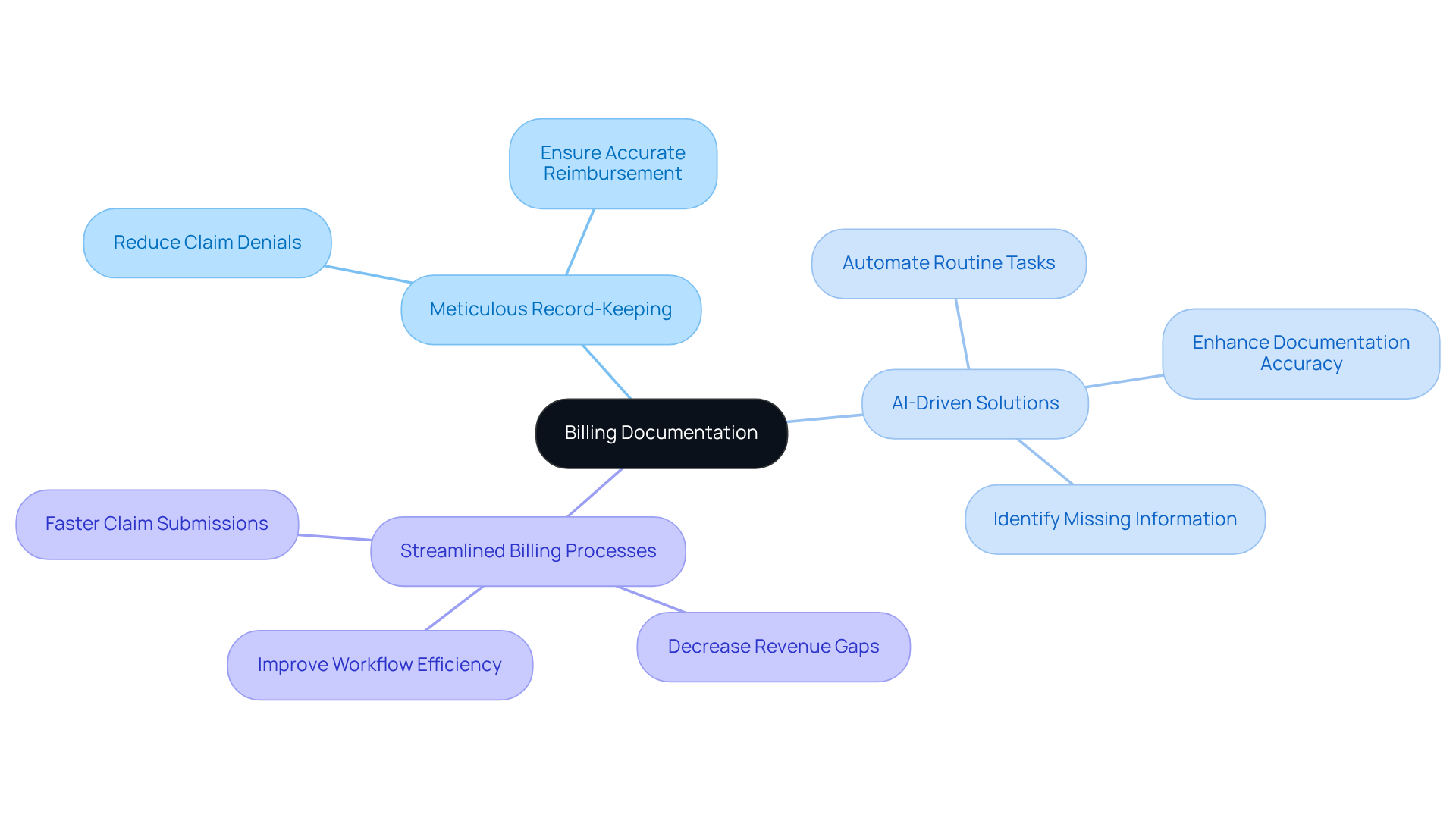
Billing Documentation: Ensuring Accurate Reimbursement Processes
Billing records are a vital lifeline for healthcare providers seeking accurate reimbursement for their invaluable services. Comprehensive records of patient encounters, treatments, and diagnoses are essential to substantiate billing claims and reduce the risk of denials. Inadequate records are a leading cause of claim denials, representing 42% of coding denials. This statistic underscores the importance of meticulous record-keeping. By prioritizing thorough and precise billing records, providers can significantly improve their financial sustainability, ensuring they receive fair compensation for the care they deliver.
Moreover, precise billing records directly influence . The average denial rate for medical claims ranges from 5% to 10%, with nearly 12% of claims submitted containing inaccurate codes, resulting in delayed payments. By enhancing record-keeping practices, healthcare organizations can bridge revenue gaps and streamline their billing processes, ultimately fostering a more stable financial environment.
Incorporating advanced technologies, such as AI-driven solutions, can further bolster record-keeping efforts. AI systems enhance overall record accuracy by identifying missing information and suggesting appropriate coding. These tools not only improve accuracy but also automate routine tasks, allowing providers to focus more on patient care. As medical expenses continue to rise, the importance of efficient billing records cannot be overstated; they are a cornerstone of financial well-being in the healthcare sector.
Key Solutions to Enhance Billing Records:
- Prioritize meticulous record-keeping to reduce claim denials.
- Implement AI-driven solutions for improved accuracy and efficiency.
- Streamline billing processes to decrease revenue gaps.
By taking these steps, healthcare providers can create a more supportive financial environment, ensuring that they can continue to deliver the compassionate care their patients deserve.
AI Tools in Clinical Documentation: Boosting Efficiency and Accuracy
AI tools are truly transforming clinical records, offering a compassionate solution to the emotional challenges faced by healthcare providers. By automating labor-intensive tasks, these tools not only improve accuracy but also streamline overall efficiency. Have you ever felt overwhelmed by the demands of manual data entry? Real-time transcription abilities enable medical providers to record interactions with individuals precisely during consultations, significantly reducing the time spent on these tedious tasks.
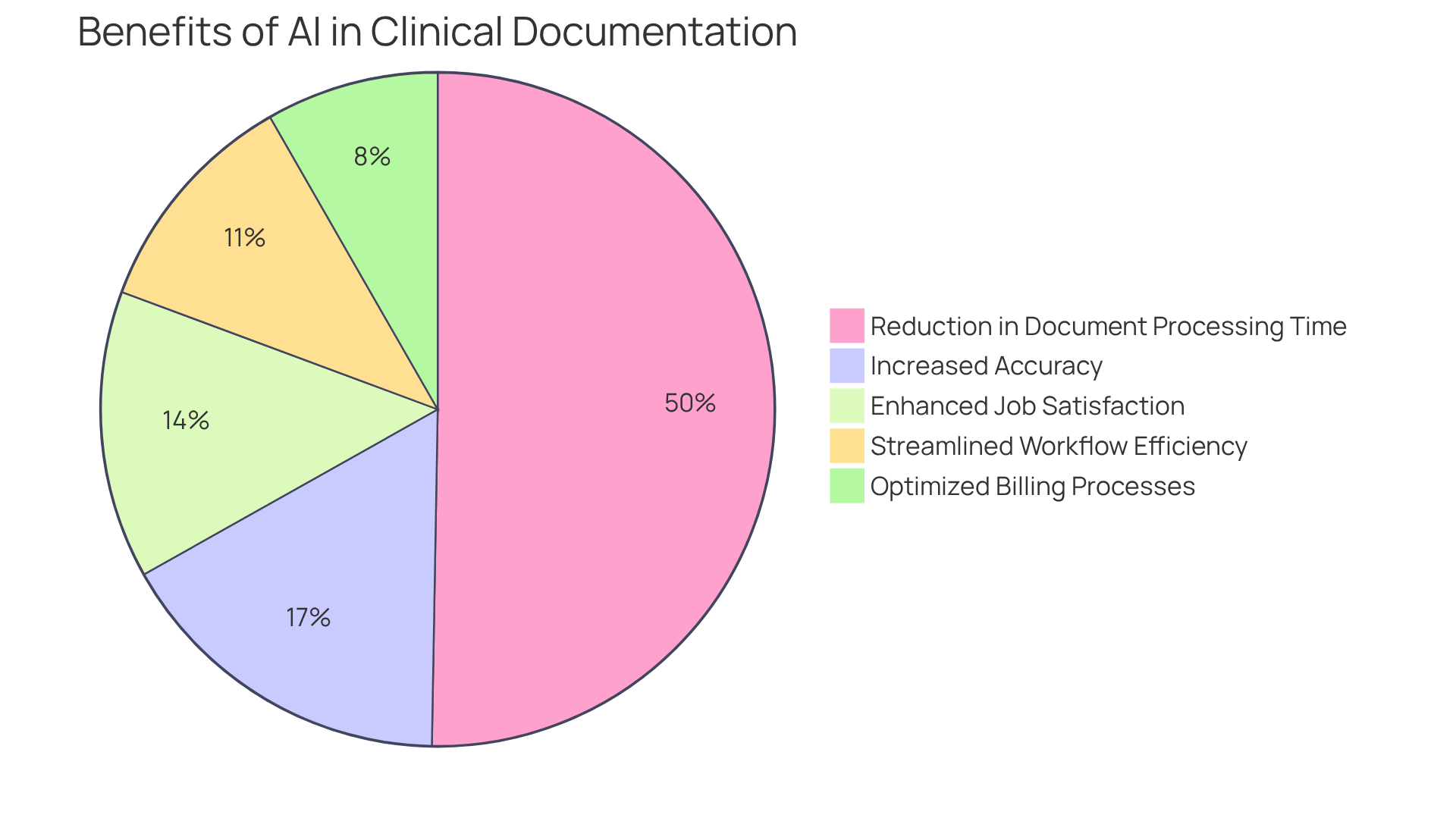
Practices that have embraced Document Services AI report an impressive 91% reduction in document processing time. This remarkable statistic underscores the potential of technology to enhance operational efficiency and alleviate those administrative burdens that can detract from patient care. Furthermore, CosmaNeura's AI can suggest appropriate billing codes based on documented encounters, aiming to maximize billings and uncover past billing opportunities. Imagine the relief of optimizing revenue potential while minimizing errors!
By integrating AI into examples of clinical documentation processes, healthcare providers can significantly reduce administrative pressures. This shift leads to , allowing you to focus on what truly matters—delivering high-quality patient care. Let’s embrace these advancements together, fostering a supportive environment where both providers and patients can thrive.
Conclusion
In the realm of healthcare, effective clinical documentation is not just a task; it is a cornerstone of patient care. Have you ever felt overwhelmed by administrative duties? By harnessing innovative tools and methodologies, such as AI-powered solutions, healthcare providers can streamline their documentation processes. This shift allows for prioritizing patient interactions over paperwork, enhancing workflow efficiency and promoting a more compassionate approach to care.
Throughout our exploration, we’ve seen various examples of clinical documentation, including:
- SOAP notes
- Progress notes
- Nursing notes
- The vital role of electronic health records (EHR)
Each type plays a significant role in improving communication and ensuring compliance with legal standards. Can you imagine the relief of reducing the burden on healthcare professionals? The integration of AI tools amplifies these benefits, fostering an environment where quality care can truly thrive.
As the healthcare landscape evolves, embracing effective documentation practices is essential. By prioritizing accuracy, clarity, and compassion in clinical records, healthcare providers can improve operational efficiency and build stronger, trust-based relationships with their patients. It is imperative for all stakeholders in the healthcare system to commit to these practices. Are we doing enough to ensure that every patient receives the high-quality care they deserve? Let’s take this step together, ensuring that compassion and efficiency go hand in hand.




