Overview
This article seeks to support healthcare providers by offering essential patient note examples that can enhance documentation practices and ultimately improve patient care. We understand the emotional challenges you face in managing administrative tasks that can sometimes overshadow your focus on patients. Structured documentation formats, like SOAP and DAP notes, are crucial in alleviating these burdens. They not only streamline record-keeping but also facilitate effective communication among healthcare teams.
Imagine how much easier it would be to share vital information with your colleagues, leading to better patient outcomes and ensuring legal compliance. By adopting these structured formats, you can create a more organized approach to documentation, allowing you to focus more on what truly matters—your patients.
We encourage you to explore these documentation strategies further. Consider how implementing them can transform your daily practice and enhance the quality of care you provide. Together, we can navigate the complexities of healthcare documentation with empathy and understanding, ensuring that every patient receives the care they deserve.
Introduction
In the intricate landscape of healthcare, providers often find themselves balancing the demands of patient care with a multitude of administrative tasks. This juggling act can lead to overwhelming feelings and stress. Thus, the importance of effective documentation becomes paramount. This article explores ten essential patient note examples that not only simplify the documentation process but also elevate the quality of care provided.
As healthcare professionals increasingly seek AI-driven solutions to ease their burdens, one might wonder: how can these innovative tools truly transform the recording and utilization of patient information? By delving into these examples, we can uncover the potential for enhanced efficiency, improved patient outcomes, and a more compassionate healthcare environment. Together, let’s explore how these advancements can support your vital work in healthcare.
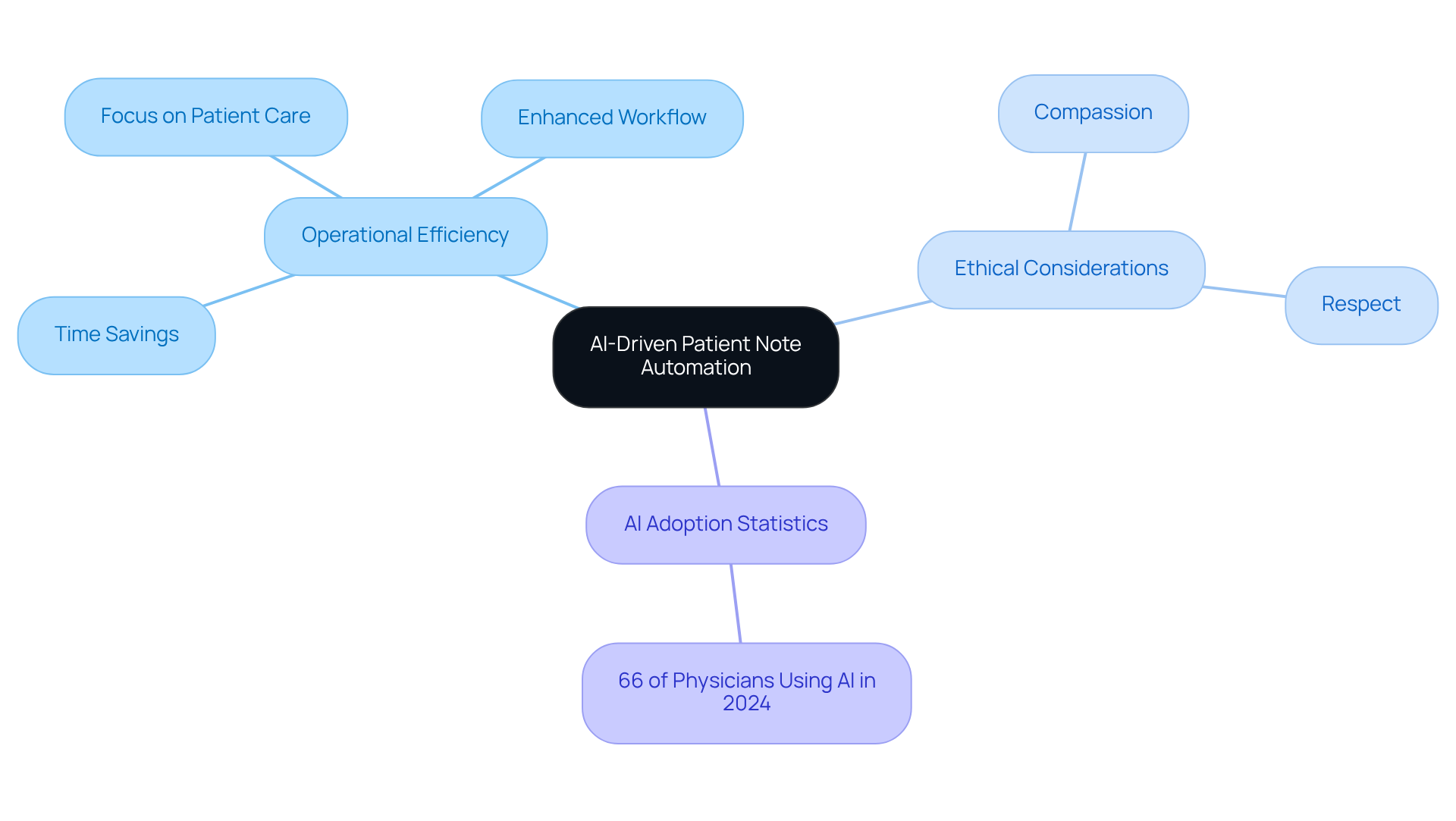
CosmaNeura: AI-Driven Patient Note Automation for Healthcare Providers
In the demanding world of healthcare, providers often face overwhelming administrative tasks that can detract from their primary focus: patient care. CosmaNeura understands these challenges and utilizes advanced AI technology to transform the patient note example for individuals who are receiving care. By independently overseeing tasks like client intake and triage, the platform significantly reduces the time healthcare providers spend on documentation, allowing them to focus on delivering high-quality patient note examples.
This automation not only enhances operational efficiency but also aligns with the ethical principles of Catholic teachings, ensuring that healthcare remains compassionate and respectful. Imagine reclaiming valuable time, enhancing workflow, and ultimately improving patient outcomes. With , healthcare providers can experience this transformation firsthand.
As we see a rise in AI adoption within healthcare, with 66% of physicians utilizing AI tools in 2024, the potential for increased efficiency and reduced administrative burdens becomes increasingly evident. This shift alleviates the strain on healthcare professionals and fosters a more patient-centered approach to care. How might your practice benefit from embracing such innovative solutions? Together, we can pave the way for a more compassionate healthcare environment.
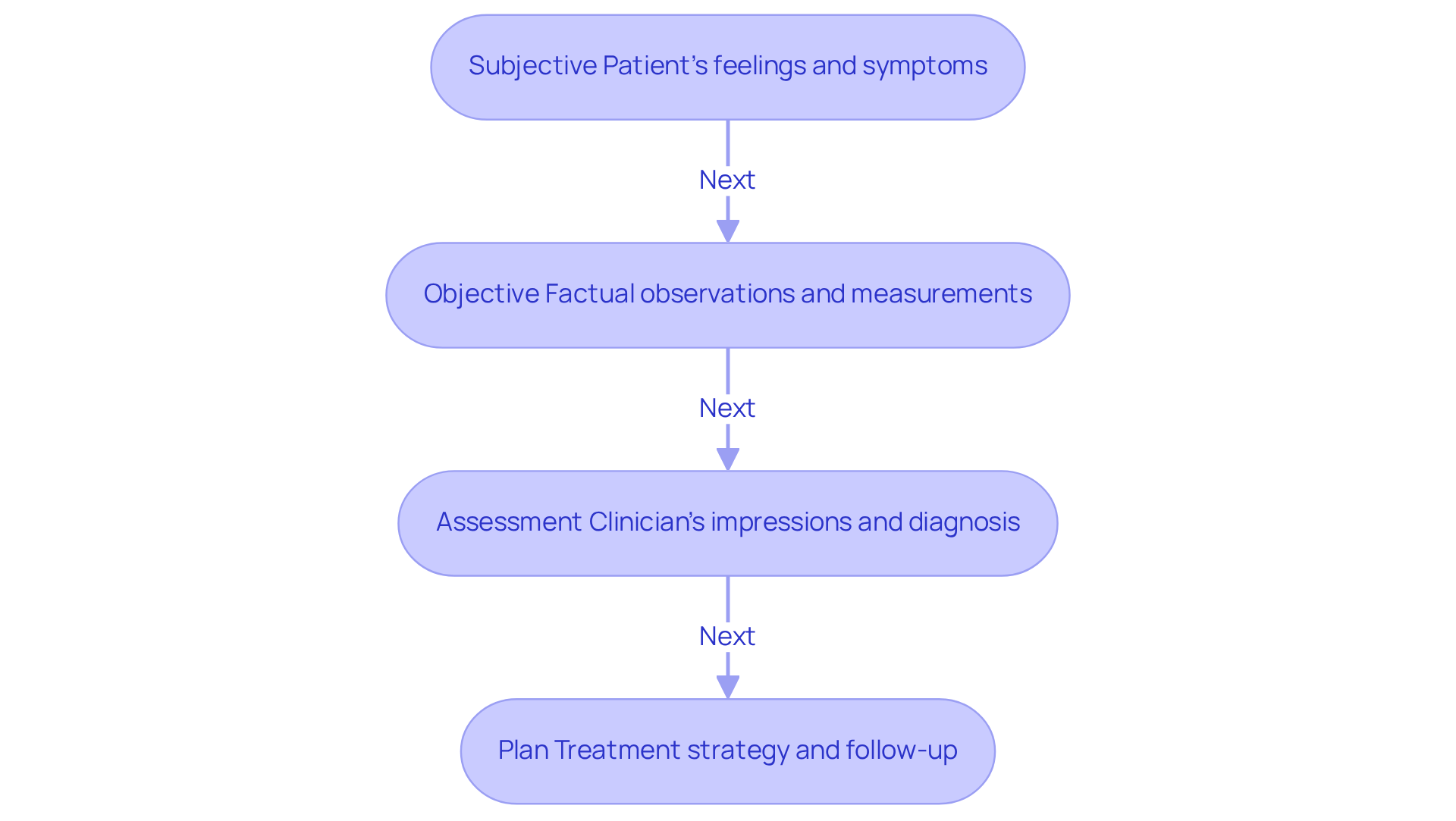
SOAP Note Example: Effective Documentation for Patient Interactions
A SOAP record serves as a vital tool in clinical writing, comprising four essential elements: Subjective, Objective, Assessment, and Plan. For example, consider a SOAP note for a patient dealing with hypertension:
- Subjective: The patient shares feelings of headaches and dizziness.
- Objective: Blood pressure measures at 150/95 mmHg.
- Assessment: The diagnosis indicates uncontrolled hypertension.
- Plan: The treatment strategy involves increasing the medication dosage and scheduling a follow-up appointment in two weeks.
This structured format serves as a that not only supports thorough record-keeping but also enhances clinical decision-making by providing a clear and systematic overview of the patient’s condition. Efficient record-keeping methods, like the SOAP format, are increasingly recognized among healthcare professionals for their role in improving health outcomes and streamlining care processes. Have you considered how regular use of SOAP notes can lead to better monitoring of patient progress and more informed treatment plans?
By leveraging AI tools, such as those provided by CosmaNeura, healthcare providers can automate repetitive documentation tasks, ensuring that vital information is captured effectively. This allows physicians to focus more on patient interactions rather than administrative tasks, ultimately elevating the quality of care. Embracing these solutions can truly transform the way we approach patient care, fostering a more compassionate and attentive healthcare environment.
Mental Health SOAP Note Example: Tailoring Documentation for Counseling Sessions
In mental health settings, addressing the emotional challenges faced by patients is crucial. An effective SOAP note can be structured to reflect this understanding:
- Subjective: The patient shares feelings of significant anxiety and difficulty sleeping, stating, 'I feel overwhelmed and can't seem to relax.' With an average of 4-5 hours of sleep per night, these only heighten their anxiety.
- Objective: The individual appears visibly restless, showcasing a rapid speech pattern and fidgeting throughout the session. These observable behaviors underscore the profound impact of anxiety on their daily life.
- Assessment: The clinician identifies Generalized Anxiety Disorder (GAD), recognizing the substantial effect of anxiety on daily functioning and the client’s expressed fear of losing control.
- Plan: The treatment plan includes introducing cognitive-behavioral therapy (CBT) techniques to help manage anxiety symptoms, along with considering a medication evaluation for further options. A follow-up session will be scheduled in one week to monitor progress.
This structured format not only supports clinicians in tracking emotional and psychological changes effectively but also fosters clear communication among healthcare providers, enhancing continuity of care. Have you considered how incorporating direct quotes from clients can enrich the documentation's depth and accuracy? Additionally, well-crafted SOAP records serve as essential legal documents, ensuring clarity and reducing the risk of misinterpretation or liability. By utilizing SOAP records, mental health practitioners can create a patient note example that thoroughly documents patient interactions, leading to improved treatment planning and outcomes. Let’s continue to explore how we can enhance patient care together.
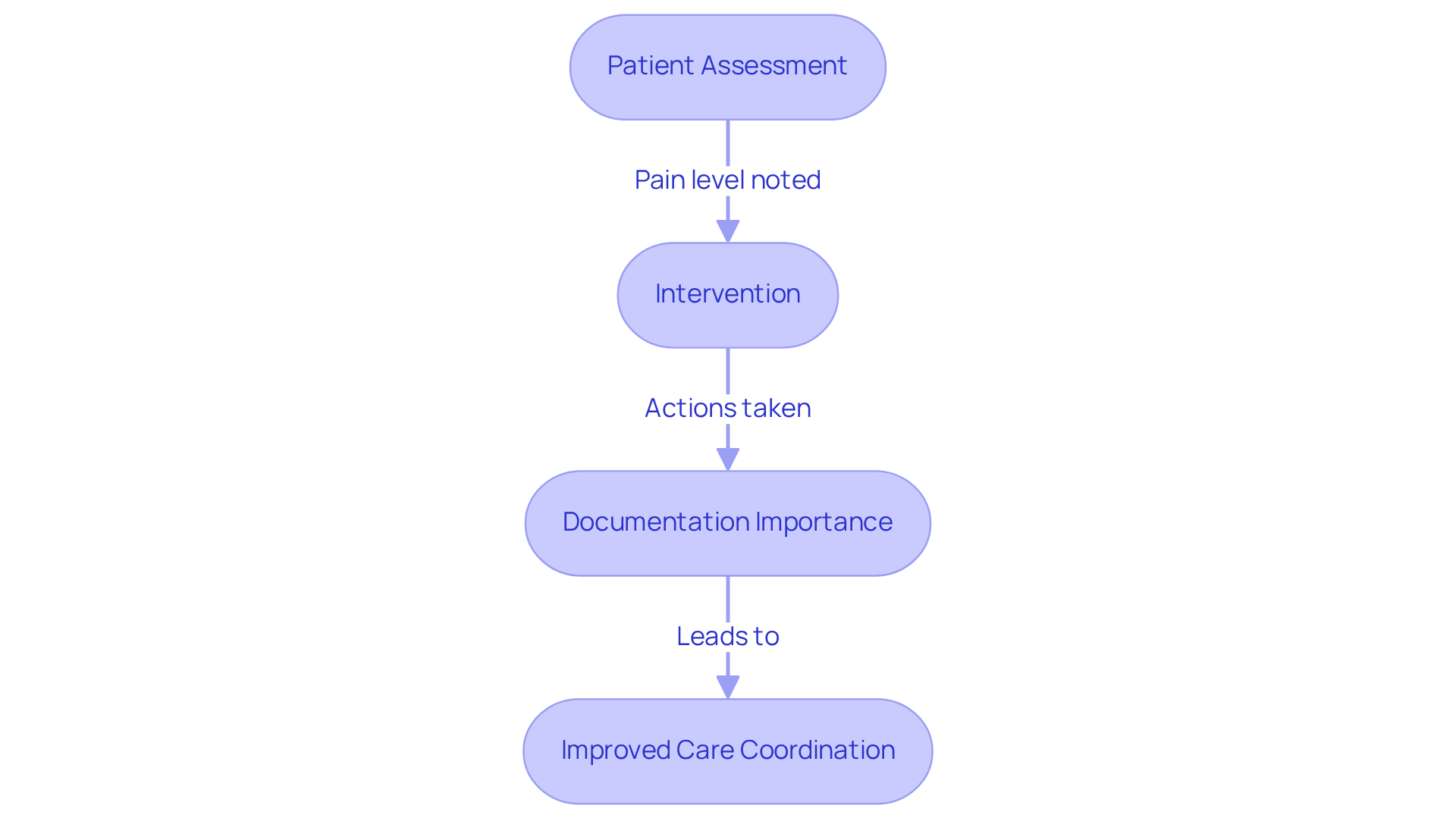
Nursing Care Note Example: Ensuring Comprehensive Patient Care
A nursing care note example might include:
- Date/Time: 09/02/2025, 10:00 AM.
An example of a patient note is as follows: Patient Name: John Doe. - Assessment: The patient note example shows that the patient reports a pain level of 7/10 in the left leg.
- Intervention: Administered prescribed pain medication and applied ice pack, as documented in the patient note example.
This record is essential. It guarantees that all assistance given is precisely logged, enabling smooth communication among healthcare professionals. Efficient nursing records not only improve the quality of healthcare but also greatly decrease the time nurses allocate to administrative duties. On average, nurses dedicate approximately 132 minutes to recording information during a 12-hour shift, accounting for about 18 percent of their time. By adopting thorough record-keeping methods, nurses can enhance coordination of services and results for individuals.
Have you considered how AI tools could simplify your record-keeping tasks? These tools are progressively being employed to enable nurses to concentrate more on direct client support. A study emphasized that nurses with access to organized recording sheets were 51% more likely to engage in effective record-keeping. This transition towards structured record-keeping methods is crucial. Almost half of nursing support was traditionally unrecorded, resulting in deficiencies in treatment.
Nursing experts stress the significance of detailed records. As one specialist remarked, "Thorough documentation of individuals' health is essential for guaranteeing seamless treatment and improving safety for those receiving services." By implementing efficient documentation methods, healthcare professionals can enhance their workflow and raise the overall quality of service provided to individuals. Together, let’s embrace these tools to foster a more .
Specialty Consultation Note Example: Documenting Complex Patient Cases
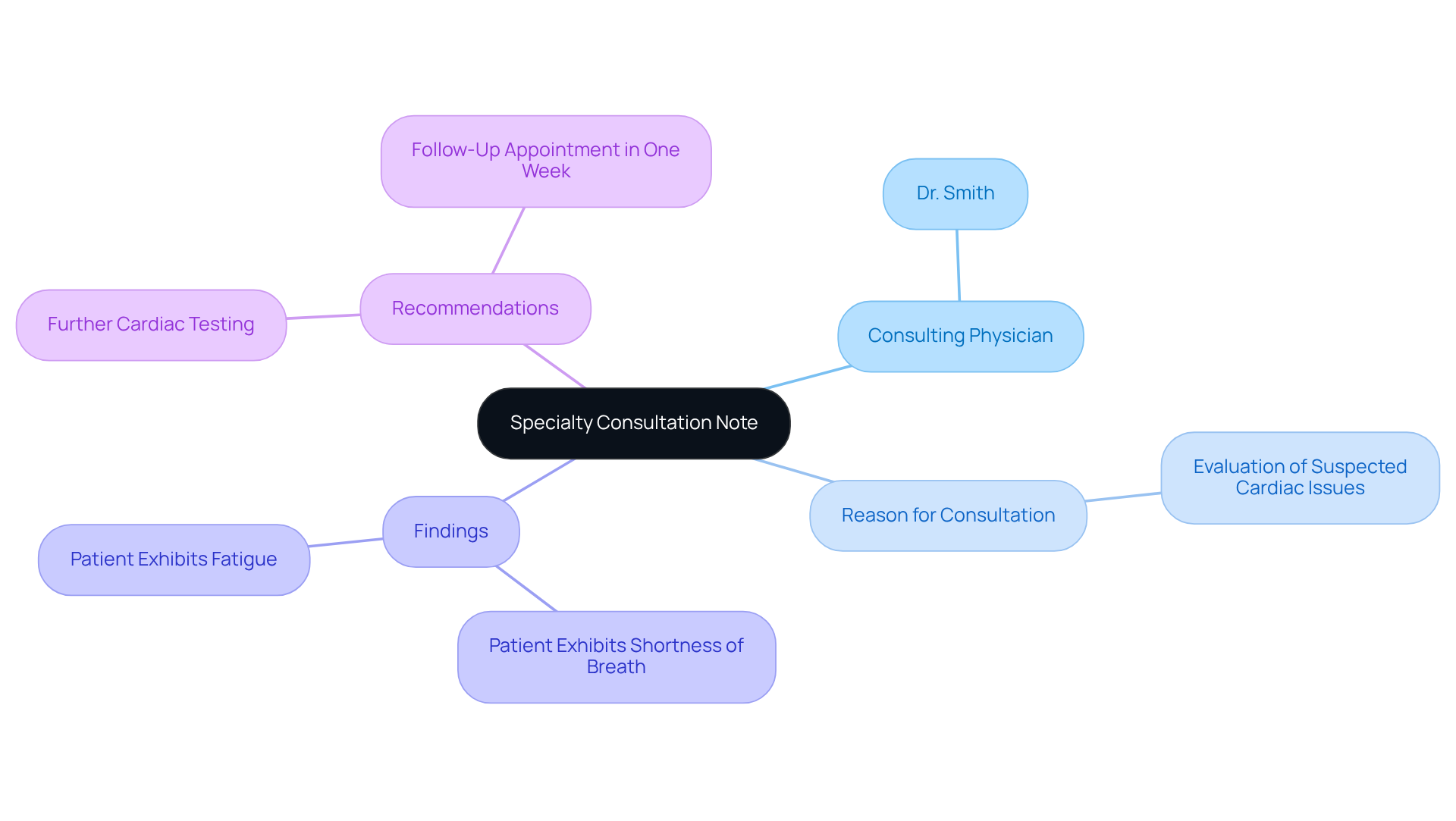
A well-organized specialty consultation document is essential for fostering effective communication between healthcare providers and specialists. Have you ever considered how crucial this can be for patient care? For instance, a specialty consultation note might include the following elements:
- Consulting Physician: Dr. Smith
- Reason for Consultation: Evaluation of suspected cardiac issues
- Findings: Patient exhibits shortness of breath and fatigue
- Recommendations: Further cardiac testing and follow-up appointment in one week
This format ensures that all relevant information is communicated effectively. It helps facilitate timely decision-making, ultimately enhancing patient care. Efficient documentation not only supports the continuity of treatment but also greatly influences outcomes for individuals. Research shows that prompt access to specialized treatment can lead to an 84% boost in satisfaction among individuals and a decrease in unnecessary referrals.
Furthermore, clear and succinct records assist experts in swiftly understanding the individual's condition, enabling more precise evaluations and actions. By emphasizing thorough documentation, healthcare providers can enhance collaboration. This approach not only improves the quality of services delivered to individuals but also nurtures a supportive environment for all involved. Together, let’s prioritize in our practice.
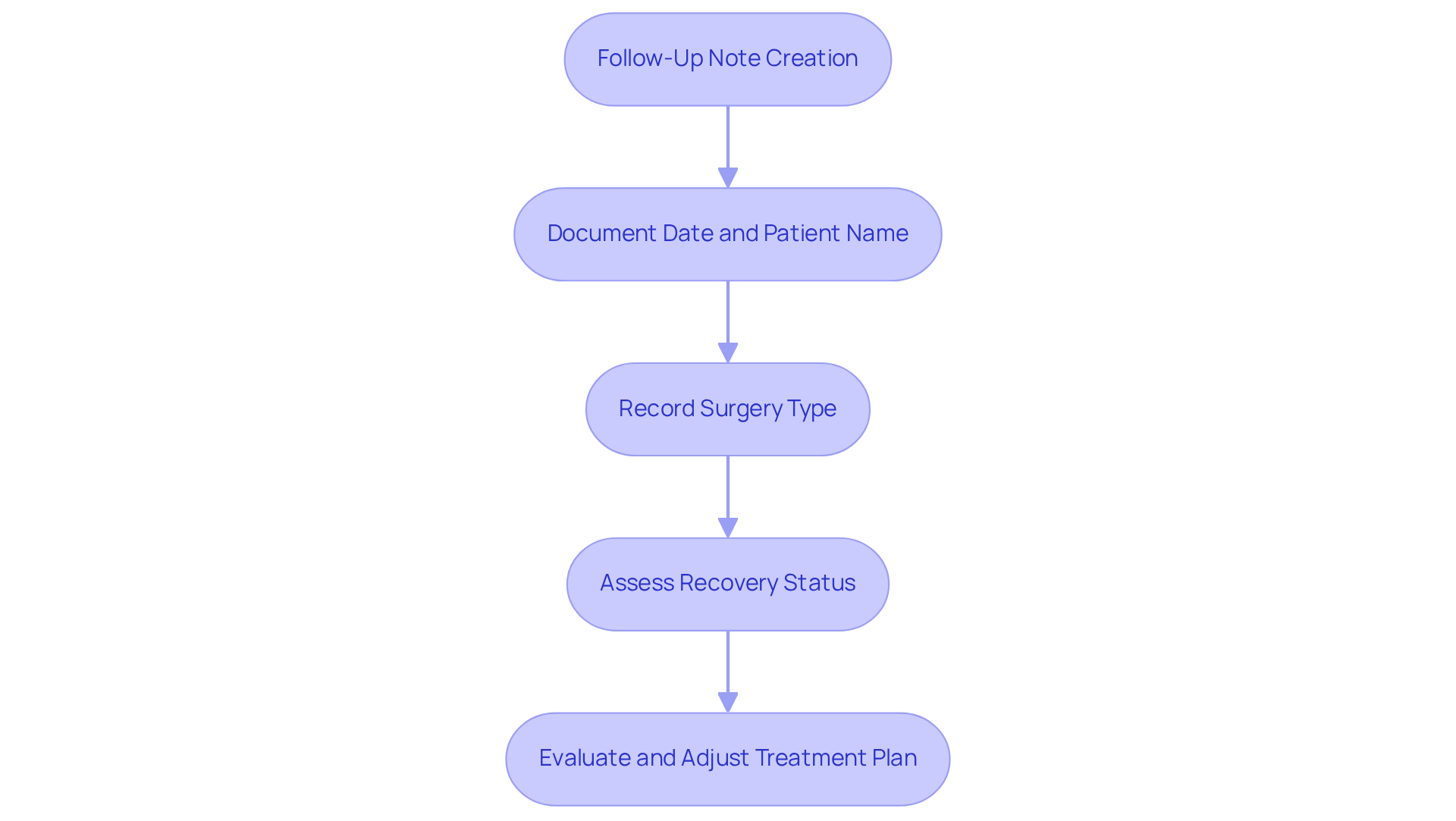
Post-Surgery Follow-Up Note Example: Tracking Recovery Progress
A post-surgery follow-up message is vital for tracking a patient's recovery and ensuring optimal treatment. Have you considered how these messages can ease the emotional burden on both patients and healthcare providers? For example, a follow-up note might include:
- Date: 09/02/2025
- Patient Name: Jane Doe
- Surgery Type: Appendectomy
- Recovery Status: Patient reports mild pain, no signs of infection.
This guide not only assists healthcare professionals in but also enables prompt modifications to the treatment plan. Efficient follow-up records can greatly influence recovery monitoring, offering a clear account of the individual's progress and any arising issues. Surgeons often stress that comprehensive documentation is crucial; as one remarked, "Precise follow-up records are essential for comprehending an individual's healing process and guaranteeing they receive the highest quality of care." By keeping thorough records, healthcare providers can improve outcomes for individuals and create a more responsive healthcare environment. How can you ensure that your follow-up practices foster a nurturing atmosphere for recovery?
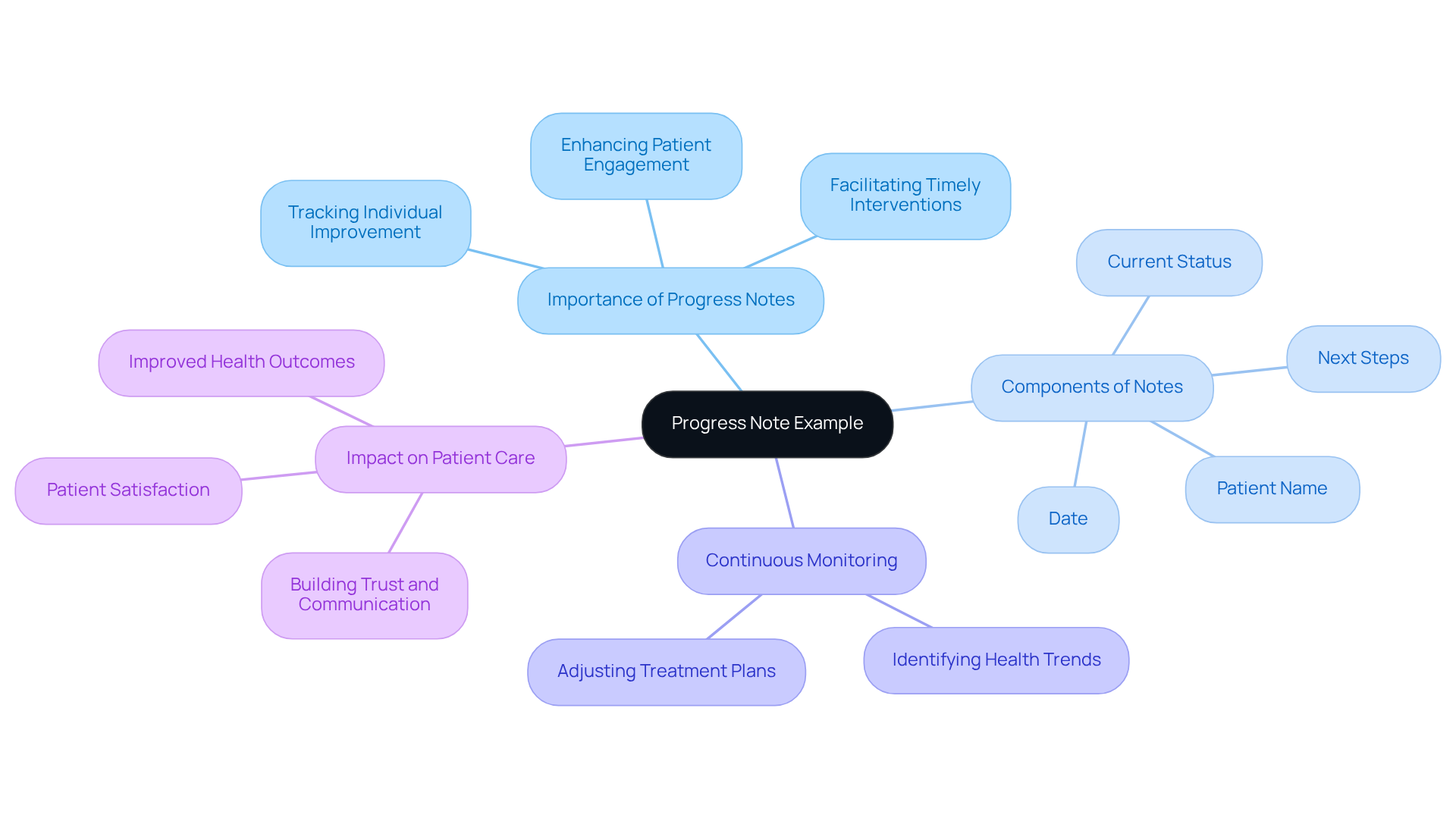
Progress Note Example: Continuous Monitoring of Patient Health
A well-organized progress note is essential for recording individual improvement over time. Have you ever considered how this simple act can make a significant difference in patient care? For instance, consider the following example:
- Date: 09/02/2025
- Patient Name: John Smith
- Current Status: Patient shows improvement in symptoms with medication.
- Next Steps: Continue current treatment plan and schedule follow-up in one month.
This format not only aids in tracking individual progress but also highlights the in improving health outcomes. Studies show that efficient documentation methods can lead to enhanced experiences and outcomes for individuals, as those who feel engaged in their treatment often report greater satisfaction levels.
Healthcare providers emphasize that continuous monitoring records are vital for identifying trends in individual health, allowing for timely interventions. Regular updates can reveal whether a treatment plan is effective or if adjustments are needed, ultimately resulting in enhanced care.
Furthermore, insights from healthcare experts underscore that effectively recording progress fosters a collaborative atmosphere where individuals feel valued and understood. This approach not only enhances communication but also builds trust, which is crucial for successful healthcare delivery.
In summary, employing organized progress records and highlighting ongoing observation can greatly influence health results. It establishes an essential practice for healthcare professionals, encouraging them to engage more deeply with their patients and positively impact their care journey.
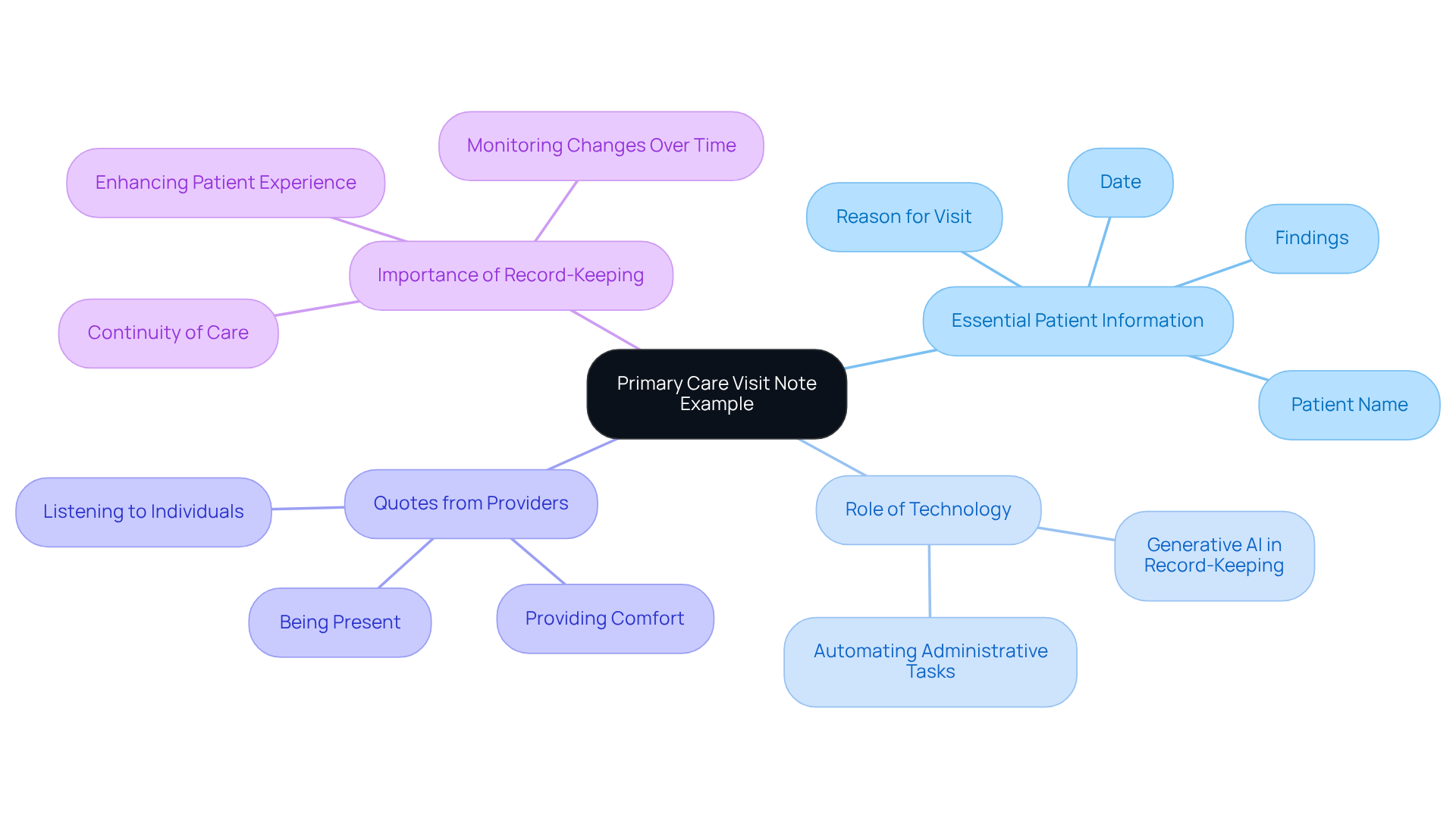
Primary Care Visit Note Example: Capturing Essential Patient Information
A primary care visit record serves as a vital instrument for gathering essential individual information, ensuring continuity of care. For instance, consider the following example:
- Date: 09/02/2025
- Patient Name: Sarah Johnson
- Reason for Visit: Annual check-up
- Findings: Vital signs within normal limits, no concerns reported.
This patient note example captures the individual's current health condition and lays the groundwork for future interactions. Yearly check-up records are crucial in monitoring changes over time, enabling healthcare providers to make based on comprehensive individual histories.
Efficient record-keeping is essential in primary care, promoting a deeper understanding of client needs and enhancing the overall experience for individuals receiving care. Have you considered how generative AI can simplify the record-keeping process? This technology ensures that crucial client information is gathered effectively and precisely. It can also help incorporate feedback from individuals into notes, further improving the quality of records and strengthening the individual-provider relationship. Additionally, generative AI can automate administrative tasks such as scheduling appointments and managing medical records, significantly reducing the time spent on these burdensome activities. As highlighted by healthcare leaders, prioritizing client experience is vital for organizational success, and comprehensive documentation plays a key role in this process.
Including quotes from primary health providers can further illustrate the importance of capturing vital individual information. One provider remarked, "Listening to individuals and recording their concerns is essential for improving the experience of those receiving care." Another stated, "You can always offer comfort even if a cure is not feasible," emphasizing the emotional aspect of care. This underscores that healing involves being present for someone in need, not just eliminating diseases.
To enhance record-keeping methods, healthcare professionals should consider frequently gathering input from individuals and incorporating it into their records. This approach not only improves the quality of documentation but also strengthens the patient-provider relationship, ultimately leading to better health outcomes. How can we work together to make this a reality?
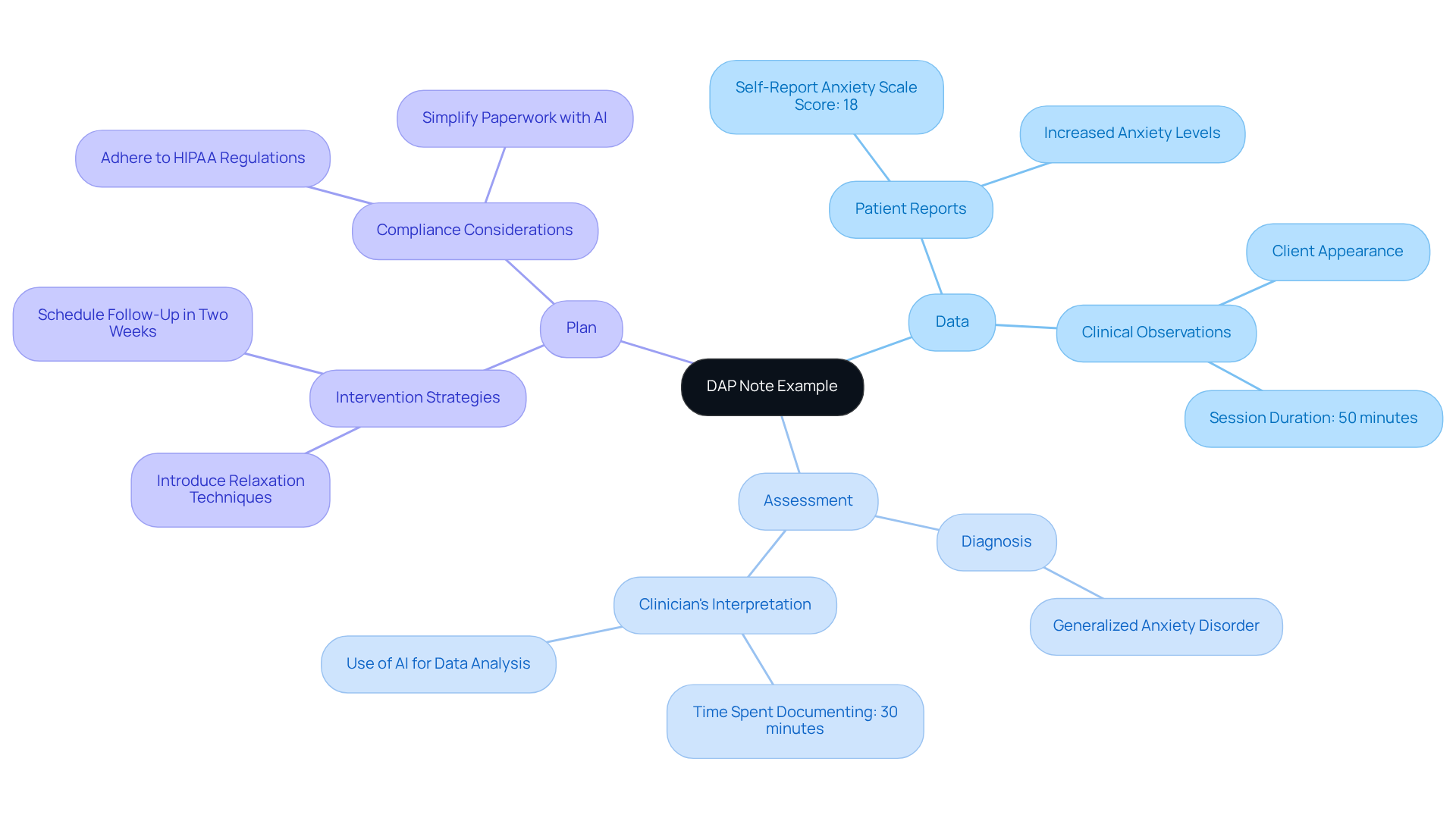
DAP Note Example: An Alternative Approach to Patient Documentation
A DAP note example might include:
- Data: The patient reports increased anxiety levels, highlighting a need for further assessment. With a history of anxiety and a recent , indicating moderate anxiety levels, it’s crucial to address these concerns. By utilizing AI-powered tools, clinicians can automate the collection of such data, ensuring accuracy and saving valuable time.
- Assessment: The symptoms align with generalized anxiety disorder, reflecting the individual's emotional state and challenges. It's understandable that clinicians might spend as much as 30 minutes documenting after each session. This emphasizes the time efficiency achieved by utilizing DAP records. Generative AI can assist in analyzing medical data, enabling faster and more precise evaluations.
- Plan: Introduce relaxation techniques and schedule a follow-up in two weeks to monitor progress and adjust interventions as necessary. It is essential to adhere to HIPAA regulations when writing DAP notes to ensure compliance and legal protection. By simplifying the paperwork process through AI, healthcare providers can focus more on client care rather than administrative duties.
This organized format not only aids in concise recording but also serves as a patient note example that guarantees essential patient information is captured effectively. DAP records should generally be concise, typically ranging from 150-250 words per session, to maintain clarity. While DAP records simplify record-keeping processes and improve communication, clinicians may face challenges such as preserving objectivity and ensuring consistency among providers. How can we navigate these challenges together to enhance the quality of care offered?
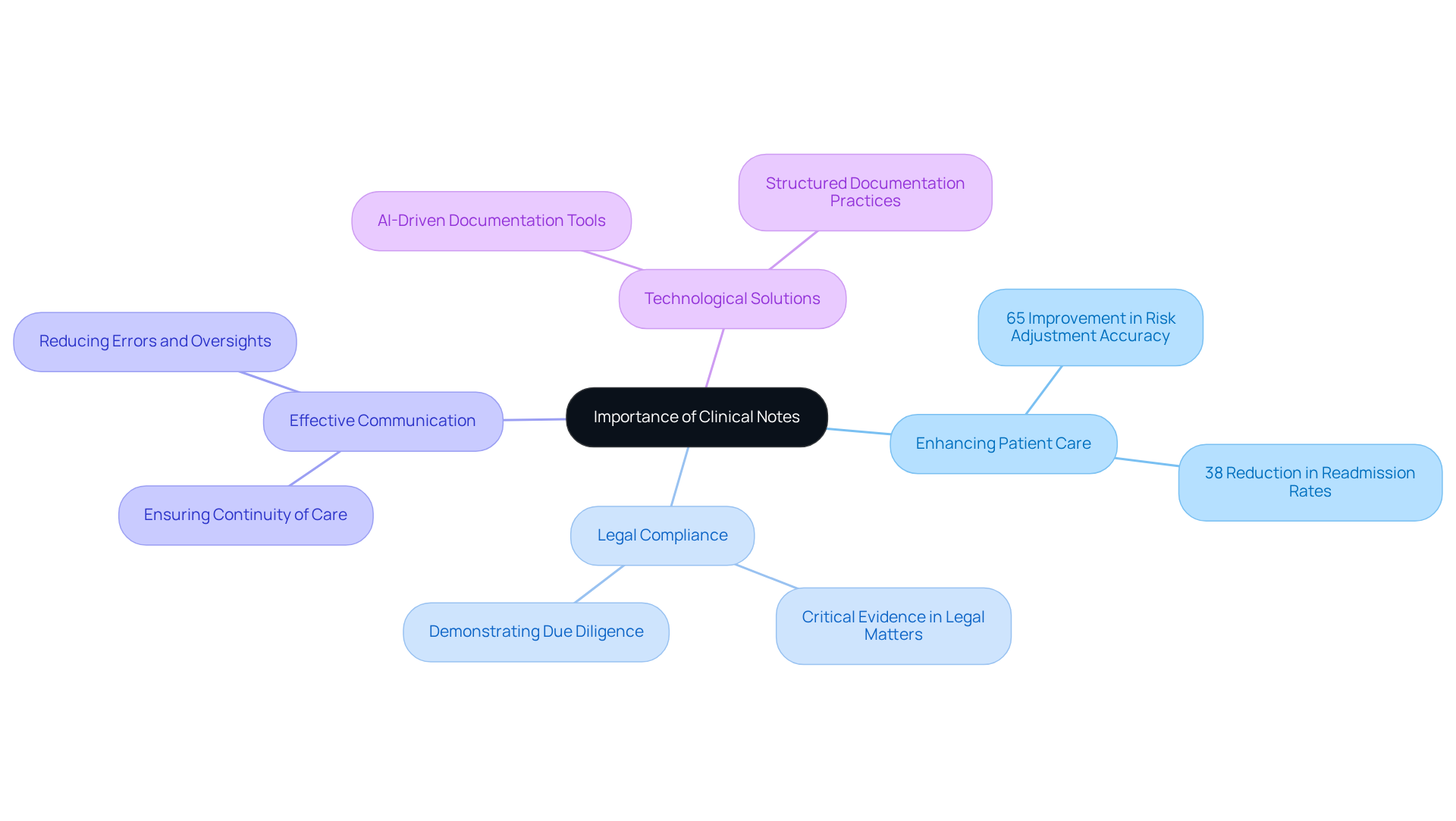
The Importance of Clinical Notes: Enhancing Patient Care and Legal Compliance
A patient note example plays a vital role in enhancing patient care, ensuring continuity of treatment, and providing legal protection for healthcare providers. It’s essential to recognize that precise and thorough records are not just bureaucratic requirements; they are crucial for effective communication among healthcare teams and for meeting regulatory standards. For example, structured documentation has been shown to significantly improve the quality of electronic health records (EHRs), leading to a remarkable 65% improvement in risk adjustment accuracy for organizations that have adopted these protocols. By prioritizing clinical records, providers can truly enhance healthcare outcomes while also safeguarding their practices from potential legal challenges, which can be illustrated with a patient note example.
Healthcare experts emphasize that a patient note example serves as critical evidence in legal matters, demonstrating due diligence and appropriate care. As specialists remind us, "the quality of clinical records is crucial as it affects the standard of healthcare, safety of individuals, and the frequency of medical mistakes." Moreover, , including a patient note example, have a direct impact on healthcare results; research indicates that medical organizations implementing comprehensive Clinical Record Enhancement (CRE) initiatives experience improvements in quality metrics and healthcare outcomes, including a significant 38% reduction in readmission rates.
Furthermore, efficient clinical records are essential for ensuring that all providers involved in a patient's treatment are on the same page, thereby reducing the risk of errors or oversights. This becomes especially important in complex cases requiring collaboration among multiple providers, which can be illustrated by a patient note example. By leveraging innovative AI solutions like CosmaNeura's Agentic Platform, healthcare providers can tackle administrative challenges, streamline record-keeping processes, and ultimately enhance patient outcomes. Emphasizing a patient note example not only improves care but also safeguards practices against potential legal pitfalls, as inaccuracies in documentation can lead to delayed reimbursements averaging $1,200 per claim.
In light of these challenges, how can healthcare providers ensure that their clinical documentation is both thorough and effective? By embracing structured documentation practices and utilizing advanced technology, providers can alleviate administrative burdens, focus more on patient care, and enhance the quality of care, as demonstrated in a patient note example. Let’s work together to prioritize clinical records and create a more supportive and effective healthcare experience for everyone involved.
Conclusion
In the realm of healthcare, effective patient documentation is not just a task; it is a cornerstone for delivering high-quality care. Have you ever felt overwhelmed by the administrative burdens that take your focus away from what truly matters? The exploration of ten essential patient note examples reveals how structured recording can streamline these tasks and enhance the overall patient experience. By embracing innovative solutions like AI-driven automation, healthcare providers can reclaim valuable time, allowing them to concentrate on patient care.
Throughout this article, we’ve highlighted the significance of various note formats, such as SOAP, DAP, and nursing care notes. Each serves a unique purpose in documenting patient interactions and treatment plans. Imagine the relief of integrating AI tools, like those offered by CosmaNeura, which can reduce the burden of documentation while ensuring accuracy and compliance. This shift not only fosters a more compassionate approach to healthcare but also leads to improved patient outcomes and satisfaction.
Ultimately, the importance of meticulous clinical documentation cannot be overstated. It safeguards healthcare providers against legal challenges and facilitates seamless communication among care teams. This ensures that every patient receives the attention and treatment they deserve. By prioritizing effective patient note-taking and exploring advanced documentation methods, healthcare professionals can significantly enhance their practice. This is not just beneficial; it is essential for the future of patient care. Embrace these changes and witness the transformation in your healthcare environment—your patients will thank you.




