Overview
This article sheds light on the significance of SOAP nursing notes, particularly in the realm of clinical documentation and patient care. Have you ever felt overwhelmed by the administrative tasks that seem to pile up? You're not alone. Structured records like SOAP notes can alleviate some of that burden, enhancing communication and improving treatment outcomes.
By illustrating specific examples across various specialties, we can see how these structured records ensure comprehensive patient assessments. Imagine the peace of mind that comes from knowing your documentation is clear and effective, allowing you to focus more on your patients. The benefits are profound: better communication leads to improved care and ultimately, better outcomes for those you serve.
As you navigate the complexities of healthcare, consider how implementing SOAP nursing notes can support your practice. Embrace this tool not just as a requirement, but as a means to enhance your connection with patients and streamline your workflow. Together, we can foster a more compassionate and efficient healthcare environment.
Introduction
In the realm of healthcare, precise documentation is not merely a routine task; it serves as a cornerstone of effective patient care. Have you ever considered how much the quality of care hinges on the details captured during patient encounters? SOAP notes—standing for Subjective, Objective, Assessment, and Plan—provide a structured framework that allows healthcare professionals to record critical information. As the medical landscape evolves, the significance of these notes has only intensified, impacting everything from billing accuracy to the overall quality of care.
With advancements in technology and a growing emphasis on patient-centered practices, understanding the intricacies of SOAP notes becomes essential for healthcare providers. How can mastering these notes improve outcomes and enhance communication within your team? This article delves into the components of SOAP notes, best practices for their implementation, and the innovative trends shaping their future. Together, let’s explore how embracing this knowledge can lead to better patient experiences and a more supportive environment for healthcare professionals.
Understanding SOAP Notes: A Comprehensive Overview
Structured records embody a standardized framework that healthcare providers use to document client interactions effectively. The acronym stands for Subjective, Objective, Assessment, and Plan, with each component serving a distinct purpose in the documentation process. This systematic method not only helps clinicians organize their thoughts but also fosters clear communication among healthcare professionals, which is essential for coordinated care.
The significance of documentation in healthcare cannot be overstated. Have you ever considered how accurate documentation through structured formats is vital for the financial sustainability of medical practices? It directly influences billing precision and compliance. Moreover, the organized format of clinical documentation acts as cognitive support, enabling healthcare professionals to access and derive insights from medical records efficiently.
Dr. Lawrence Weed, a visionary in medical documentation, recognized the need for a structured approach to records, emphasizing the importance of SOAP nursing notes examples in clinical practice. In 2025, the relevance of SOAP notes continues to grow, with recent developments highlighting the necessity for accessibility to clinically relevant data within medical records. This accessibility enhances clinician efficiency, ultimately leading to better outcomes for those receiving care.
For instance, the integration of by CosmaNeura allows physicians to continuously track individuals' vital signs, such as heart rate, blood pressure, and oxygen saturation. This proactive surveillance not only enhances individual safety but also enables prompt interventions, underscoring the critical role of precise clinical documentation in capturing these interactions.
Consider a case study showcasing near-perfect accuracy in medical transcription. It highlights the importance of choosing top-notch transcription services, which can achieve accuracy rates of 99% or higher. Such accuracy reduces the chance of mistakes, protecting both individuals and healthcare professionals from potential legal consequences. It emphasizes the essential function of precise documentation in ensuring safety for those receiving care.
Best practices for medical records in 2025 involve ensuring that documentation is comprehensive yet succinct, as illustrated in SOAP nursing notes examples. This facilitates rapid reference during interactions with individuals. The influence of standardized records on treatment outcomes is significant; research indicates that efficient use of structured documentation aligns with improved safety and satisfaction for individuals. Perspectives from specialists, including insights from pioneers in medical record-keeping, reinforce that an organized approach to health records is crucial for delivering high-quality service.
In conclusion, structured records are more than just a documentation tool; they are vital to providing client-focused service. By following best practices and embracing the latest advancements in documentation standards, including the use of AI solutions for remote monitoring, healthcare providers can significantly enhance health outcomes and operational efficiency. Let's work together to improve the care we provide.
The Subjective Component: Capturing Patient Voices
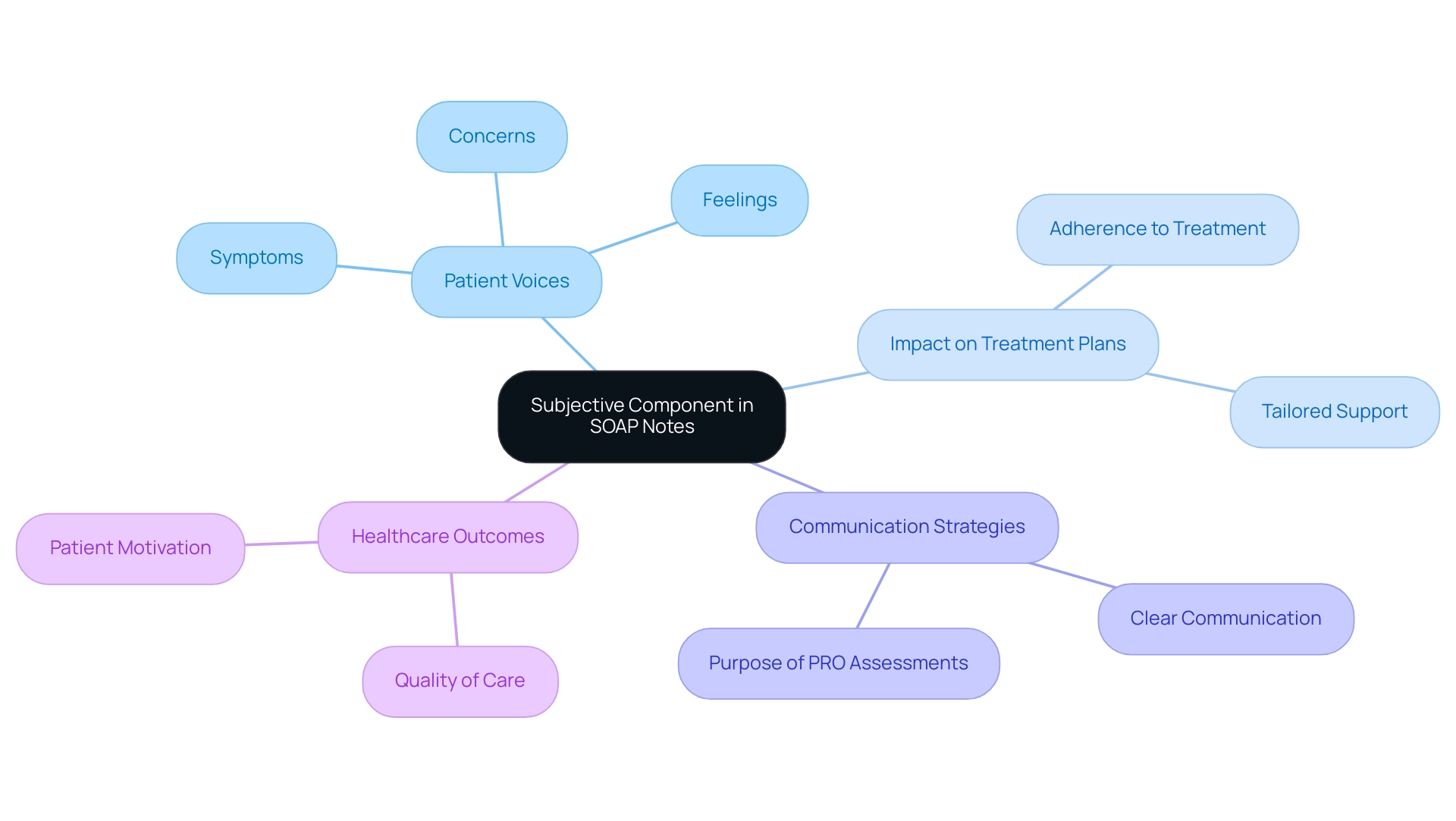
The subjective component of is vital, encompassing information shared directly by individuals, including their symptoms, feelings, and concerns. This section is essential for healthcare providers, as it offers insight into the individual's perspective, enabling tailored support that meets their unique needs. For example, when someone expresses, 'I have been feeling anxious and have trouble sleeping,' it not only reveals their mental health status but also guides further assessment and intervention strategies.
In 2025, the significance of subjective data in SOAP notes has been highlighted by recent statistics showing that effective communication of patient-reported outcomes (PROs) greatly enhances the quality of care. When individuals feel heard and understood, their adherence to treatment plans improves, leading to better health outcomes. Notably, the MUST score range of 0–8, with a score of 2 or higher indicating nutritional risk, serves as a quantitative measure that underscores the importance of capturing patient-reported outcomes in evaluating overall health.
Furthermore, a case study titled "Perception and Assessment of Respondent Burden" demonstrated that clear communication regarding the purpose of PRO assessments is crucial for maintaining participant motivation and improving compliance rates. Expert insights reveal that capturing individual voices in healthcare documentation is not just a best practice but a necessity for effective decision-making. As Olalekan Lee Aiyegbusi noted, effective communication is fundamental in healthcare settings.
By incorporating subjective information into documentation, such as SOAP nursing notes, providers can ensure that treatment plans genuinely reflect the needs and preferences of those they serve. This approach ultimately fosters a more compassionate and effective healthcare environment. As we move forward, the emphasis on gathering personal information in clinical documentation will remain essential in enhancing patient-centered support.
The Objective Component: Documenting Factual Data
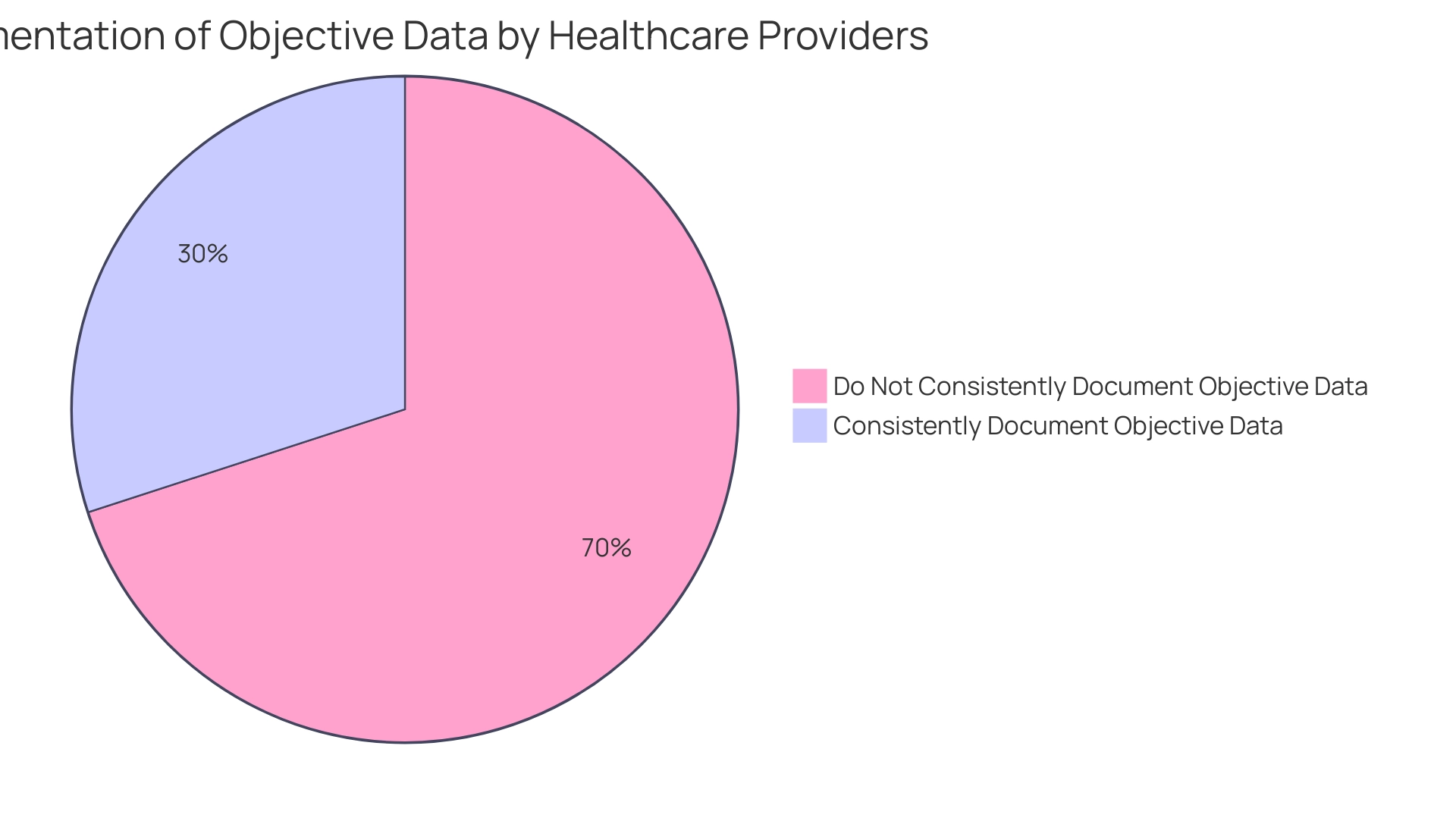
The objective element of medical documentation is essential, as it encompasses quantifiable and observable information gathered during client interactions. This includes vital signs, physical examination findings, and results from diagnostic tests. For example, a clinician might record, 'Blood pressure: 120/80 mmHg, heart rate: 72 bpm.' Such documentation establishes a factual basis for assessing an individual's current health status, supporting informed clinical decision-making.
In 2025, the emphasis on accurate vital signs documentation remains paramount. Studies indicate that nurses dissatisfied with their profession reported a significant association with missed nursing care, reflected in an Adjusted Odds Ratio (AOR) of 2.2. This underscores the critical nature of thorough documentation. Current statistics reveal that only 30% of healthcare providers consistently document objective data in medical records, highlighting the urgent need for enhanced practices in this area.
Real-world examples illustrate effective vital signs recording in clinical notes. The implementation of the Quality of Interactions Tool in a healthcare setting facilitated real-time data entry, enhancing the reliability of vital signs monitoring. This approach ensured high inter-rater agreement among observers, improving documentation accuracy and fostering a deeper understanding of nursing practices related to vital signs assessment. As healthcare continues to evolve, the latest trends in emphasize the integration of technology to streamline documentation processes.
Expert opinions reinforce that measurable data is essential for evaluations, reminding healthcare providers to prioritize accurate and comprehensive documentation in their practice. However, it's crucial to acknowledge that the study's findings may not generalize beyond UK hospitals. The presence of observers could have influenced staff behavior, although most reported feeling unaffected by the observation. How can we support each other in overcoming these challenges? Together, we can strive for better documentation practices that ultimately enhance patient care.
The Assessment Component: Analyzing Patient Information
The evaluation element of clinical documentation is essential in weaving together subjective and objective information, ultimately leading to informed clinical decisions about a patient's condition. For example, a clinician might note, 'Patient presents with symptoms consistent with generalized anxiety disorder, as evidenced by reported anxiety and sleep disturbances.' This evaluation is not merely a formality; it is vital for guiding treatment strategies and ensuring that support is tailored to each individual's unique needs.
Research indicates that a well-organized assessment can significantly influence treatment outcomes. Indeed, studies have shown that the accuracy of clinical evaluations based on structured documentation can enhance healthcare by making pertinent information readily accessible. This is particularly important in today’s healthcare landscape, where the risk of inaccuracies in electronic medical records can jeopardize patient safety.
Organized evaluations help mitigate this risk by providing clear and precise documentation that healthcare providers can rely on. Moreover, clinicians have highlighted the importance of efficiently integrating client data within clinical records. As Imran Shaikh, a Content Marketing Expert and SEO Specialist at Augnito AI, pointed out, ensuring the accuracy of the individual's name, date/time, heading, and signature is crucial to prevent significant time loss and potential health risks.
This underscores the need for meticulous documentation practices, which can be further enhanced through AI-driven solutions that alleviate administrative burdens on healthcare providers. In practice, the assessment component should not only reflect the clinician's observations but also incorporate best practices for clinical assessments. For instance, utilizing the APSO structure has demonstrated improvements in speed, task achievement, and usability for physician users compared to traditional documentation formats. This transition can lead to more efficient clinical workflows and better outcomes, especially as AI technologies foster seamless communication and collaboration among healthcare providers.
As we approach 2025, the significance of assessments in SOAP nursing notes remains critical. These assessments form the foundation for effective individual treatment, ensuring that clinicians can make informed decisions based on comprehensive evaluations, including examples from SOAP nursing notes. Cosmonaut's dedication to integrating Catholic values into its AI solutions reinforces the ethical framework guiding these assessments.
The case study titled 'Commitment to Catholic Values in Healthcare' exemplifies how CostaNera ensures that all recommendations and operations align with ethical guidelines, promoting morally responsible treatment and positioning the platform as a leader in .
The Plan Component: Outlining Next Steps in Care
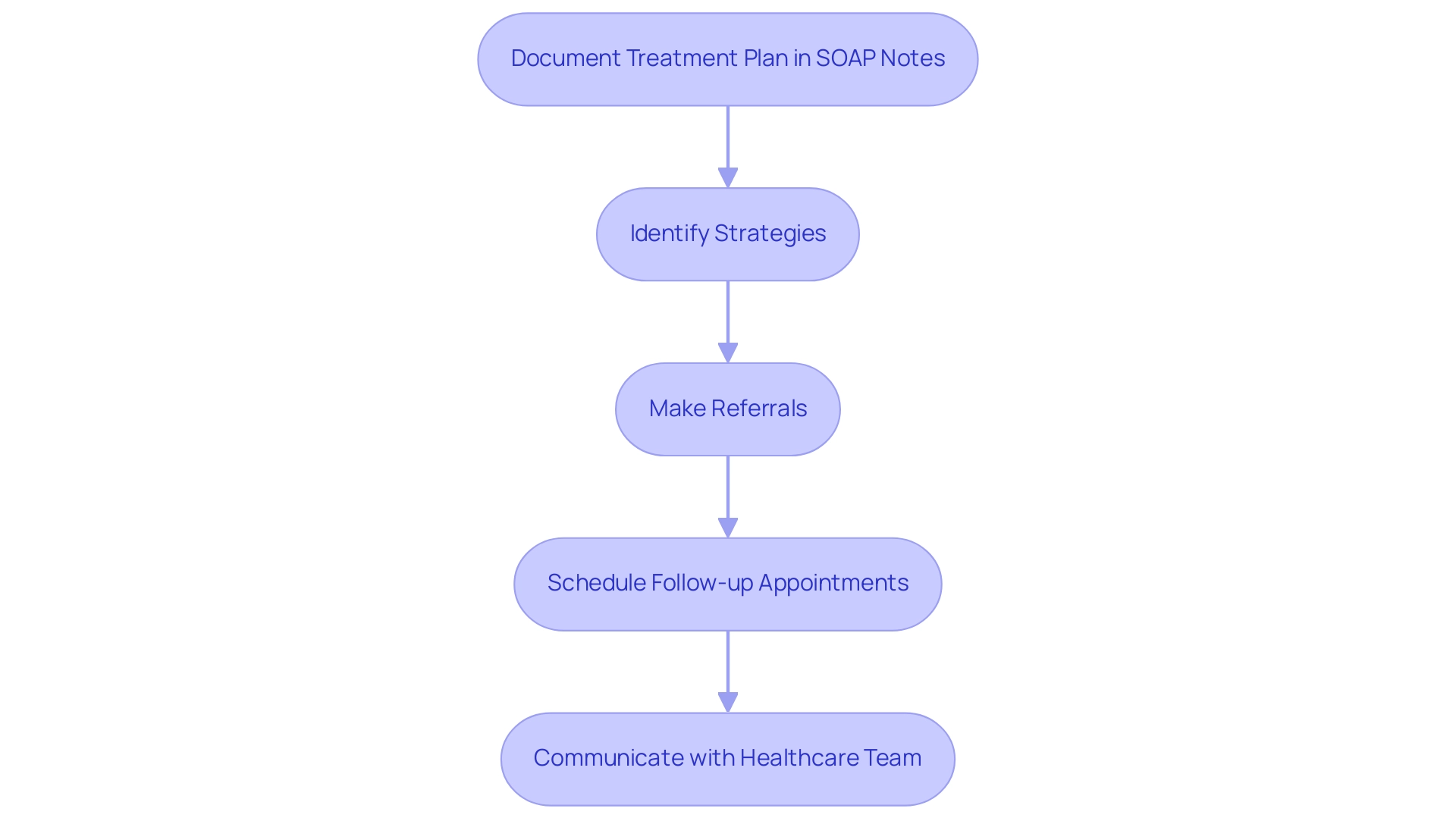
The plan section of SOAP notes is vital as it outlines the next steps in an individual's treatment journey, including strategies, referrals, and follow-up appointments. For instance, a clinician might document, 'Refer to a mental health specialist for further evaluation and initiate cognitive-behavioral therapy sessions.' This thoughtful plan ensures that all members of the healthcare team are aligned in their approach to the individual's care, ultimately enhancing the quality of service provided.
Current trends reveal that is essential for improving individual outcomes. Research shows that clear documentation in SOAP notes can significantly influence follow-up appointment adherence. Statistics indicate that individuals are more likely to attend follow-ups when their health plans are well-documented and communicated. In fact, studies suggest that up to 70% of patients adhere to follow-up appointments when they have a structured treatment plan in place.
However, in Singapore, only 0%-5% of healthcare providers initiate advance planning (ACP) during the dying phase. This statistic highlights the urgent need for structured plans to foster engagement and adherence.
Experts recommend outlining treatment plans with precision, utilizing [SOAP nursing notes examples](https://cosmaneura.com/newsroom1/-traditional-accelerators-arent-equipped-to-support-healthcare-startups). Healthcare professionals advocate for including specific details in these notes, such as timelines for follow-ups, the rationale behind referrals, and expected treatment outcomes. A specialist noted, "It should be the sort of thing where it’s right next to their allergies," emphasizing the practical importance of planning in individual management.
This level of detail not only aids in continuity of treatment but also builds trust in the patient-provider relationship.
Moreover, by leveraging AI to streamline administrative tasks like appointment scheduling and medical record management, healthcare providers can alleviate the burden of time-consuming processes. This automation allows clinicians to focus more on patient interactions and planning, ultimately enhancing satisfaction and reducing burnout. By integrating these automated processes into their workflows, healthcare providers can ensure that SOAP notes are comprehensive and efficiently managed, leading to better patient outcomes.
Real-world examples illustrate the effectiveness of documented treatment plans. A case study titled 'Facilitators and Recommendations for Improving ACP Practices' highlighted the positive impact of implementing standardized workflows in primary settings, which improved documentation of advance planning. The research revealed that when providers normalized conversations about treatment preferences, patient involvement increased, resulting in more thorough and practical assistance plans.
In summary, the planning aspect of documentation, including SOAP nursing notes examples, is not merely a procedural formality; it is a crucial factor that influences treatment and enhances service quality. By prioritizing clear and detailed documentation, alongside the integration of AI-driven efficiencies, healthcare providers can ensure that their patients receive the best possible outcomes while embodying the compassionate spirit of Catholic healthcare, as emphasized by CosmaNeura's mission.
10 Practical SOAP Nursing Note Examples Across Specialties
- Post-Operative Care: Subjective: 'I have pain at the incision site.' Objective: 'Incision clean, no signs of infection.' Assessment: 'Post-operative pain management needed.' Plan: 'Administer prescribed analgesics and monitor pain levels.'
- Diabetes Management: Subjective: 'I feel dizzy and my blood sugar is low.' Objective: 'Blood glucose: 60 mg/dL.' Assessment: 'Hypoglycemia due to missed meal.' Plan: 'Provide glucose tablets and educate on meal timing.'
- Respiratory Assessment: Subjective: 'I have a persistent cough.' Objective: 'Wheezing noted on auscultation.' Assessment: 'Possible asthma exacerbation.' Plan: 'Administer bronchodilator and schedule follow-up.'
- Wound Care: Subjective: 'The wound is itchy.' Objective: 'Wound healing well, no drainage.' Assessment: 'Normal healing process.' Plan: 'Continue current dressing and monitor for changes.'
- Mental Health: Subjective: 'I feel overwhelmed and anxious.' Objective: 'Patient appears restless.' Assessment: 'Increased anxiety symptoms.' Plan: 'Refer to counseling services and schedule follow-up.'
- Pediatric Care: Subjective: 'My child has a fever.' Objective: 'Temperature: 102°F.' Assessment: 'Fever likely due to viral infection.' Plan: 'Recommend fluids and monitor temperature.'
- Geriatric Care: Subjective: 'I feel weak and tired.' Objective: 'Patient has lost 5 lbs in the last month.' Assessment: 'Possible nutritional deficiency.' Plan: 'Refer to dietitian for assessment.'
- Cardiac Assessment: Subjective: 'I have chest pain when I exert myself.' Objective: 'ECG shows ST elevation.' Assessment: 'Possible myocardial infarction.' Plan: 'Immediate referral to cardiology.'
- Orthopedic Assessment: Subjective: 'My knee hurts when I walk.' Objective: 'Swelling noted in the knee joint.' Assessment: 'Knee sprain suspected.' Plan: 'Recommend rest, ice, and follow-up with orthopedic specialist.'
- Dermatology: Subjective: 'I have a rash on my arm.' Objective: 'Rash is red and raised.' Assessment: 'Contact dermatitis suspected.' Plan: 'Prescribe topical corticosteroids and advise on avoiding irritants.'
Including clients' own expressions in documentation not only enhances the records but also fortifies the therapeutic connection, ensuring that support is centered on the patient. For instance, a client describing their pain as 'a sharp, stabbing pain that feels like a knife' provides valuable insight into their experience.
The precision in these records is essential; ambiguous entries can lead to misunderstandings and mistakes in client support, highlighting the necessity for clear, actionable information. By following best practices in composing , healthcare providers can enhance communication, support continuity of treatment, and improve overall patient outcomes.
Moreover, the incorporation of AI-driven solutions from CostaNera can simplify the documentation process, enabling clinicians to recover several hours each day that were formerly taken up by routine administrative tasks. This ultimately improves the quality of service provided, allowing healthcare professionals to focus on what truly matters—their patients.
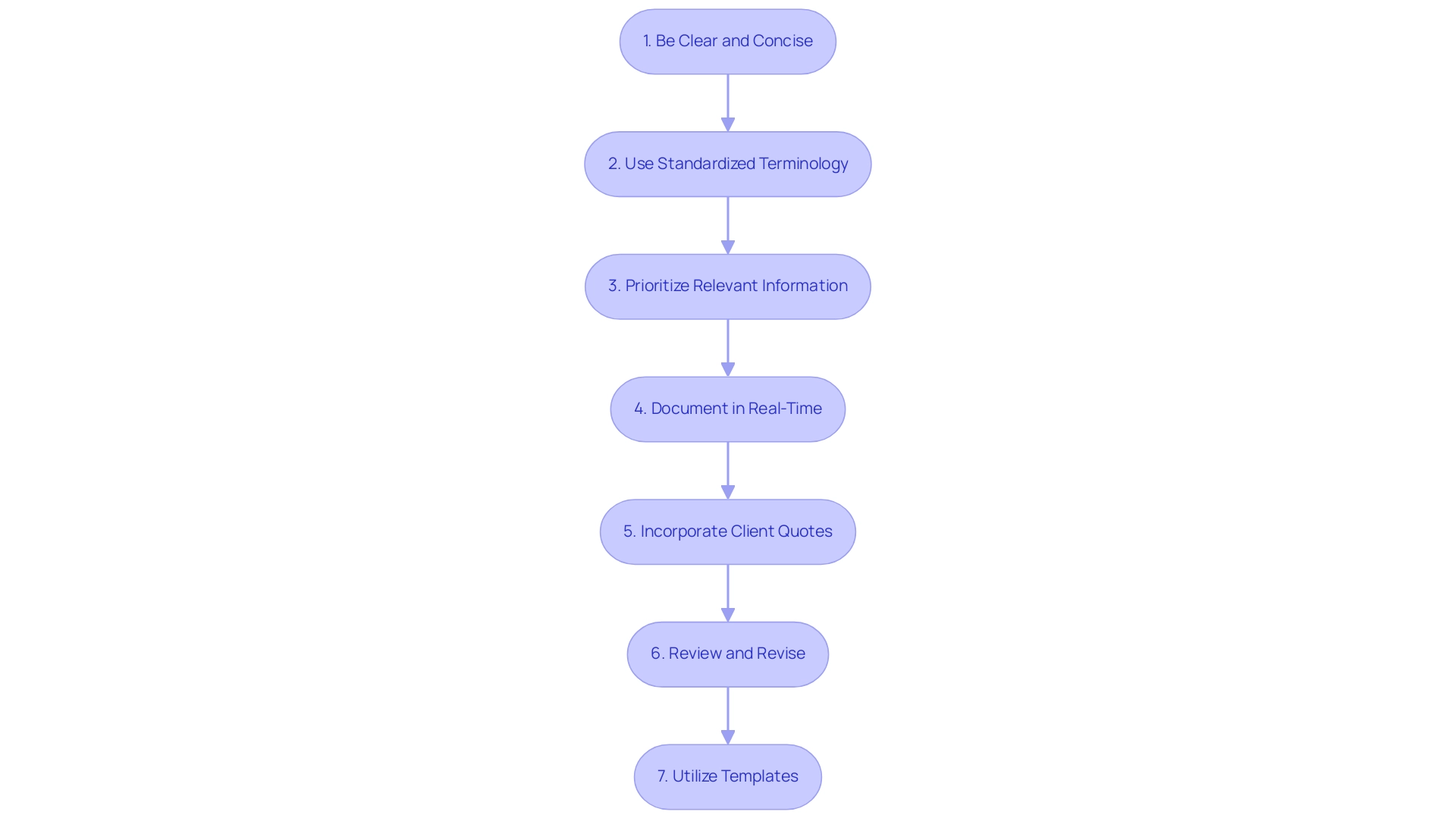
Tips for Crafting Effective SOAP Notes
- Be Clear and Concise: Utilize straightforward language to ensure your written materials are easily understood by all healthcare providers. This approach not only enhances communication but also fosters collaboration in patient care.
- Use Standardized Terminology: Consistency in language is essential for preserving clarity and reducing the chance of misinterpretation. This is crucial for protecting client wellbeing and ensuring everyone is on the same page.
- Prioritize Relevant Information: Concentrate on the most pertinent details that directly impact individual wellbeing. Avoid extraneous information that may dilute the focus of your records, allowing for a clearer understanding of client needs.
- Document in Real-Time: Aim to write your observations right after the client encounter. This practice ensures accuracy and completeness, enhancing the overall efficiency of care delivery and supporting better outcomes.
- Incorporate Client Quotes: Including the individual’s own words enhances the subjective aspect of the SOAP record. For example, when a client mentioned that she’d ‘had enough’ of her brother’s taunts, it emphasized the importance of recording sentiments in documentation.
- Review and Revise: Dedicate time to examine your records for clarity and completeness before finalizing them. This step is vital for ensuring that all relevant information is accurately captured and easily retrievable.
- Utilize Templates: Implement standardized templates to streamline . This method guarantees that all essential elements are incorporated and fosters consistency across medical records, crucial for continuity of treatment. For efficiency and consistency in recording, using SOAP nursing notes examples through a structured documentation template is suggested.
Integrating these optimal methods can greatly improve the quality of documentation, resulting in enhanced patient care efficiency. Research indicates that the APSO arrangement is superior to the conventional documentation sequence regarding speed, task success, and usability for physician users. Furthermore, the format of documentation serves as a checklist and cognitive support, assisting in information retrieval for learning.
A real-world example is the "Hypoglycemia Case," where a 45-year-old female with Type 1 diabetes was effectively documented and treated using SOAP nursing notes examples based on a structured SOAP note approach. By concentrating on clear documentation, healthcare professionals can better support outcomes and streamline their workflow.
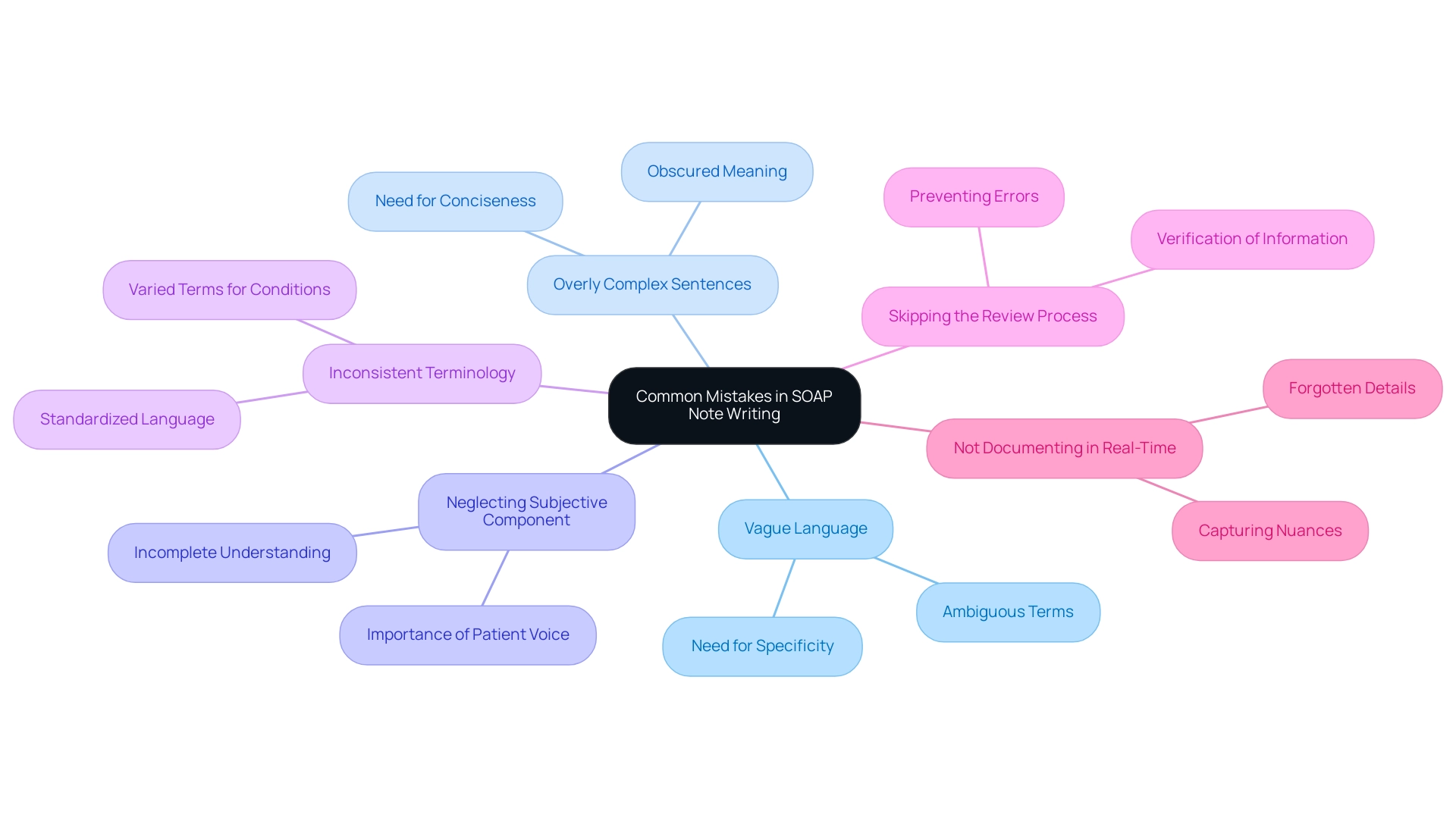
Common Mistakes to Avoid in SOAP Note Writing
- Vague Language: The use of ambiguous terms can lead to significant misinterpretations in care. Specificity in descriptions is crucial; for instance, instead of stating 'the individual seems better,' specify 'the individual reports a reduction in pain levels from 8 to 4 on a scale of 10.' This clarity helps ensure that all healthcare providers understand the individual's condition accurately. Vague or ambiguous entries in SOAP nursing notes can lead to miscommunication and errors in client care, emphasizing the need for specificity in documentation.
- Overly Complex Sentences: Clarity is paramount in healthcare documentation. Overly complex sentences can obscure meaning and hinder readability. Aim for straightforward language that conveys information effectively, such as breaking down lengthy explanations into concise statements.
- Neglecting the Subjective Component: Capturing the individual's voice is essential for a complete assessment. Failing to document subjective data can lead to an incomplete understanding of the individual's experience. Always prioritize the patient's perspective by including their descriptions of symptoms and feelings.
- Inconsistent Terminology: Using varied terms for the same condition can create confusion among healthcare providers. To avoid this, adhere to standardized language and terminology. This practice not only enhances communication but also aligns with best practices in healthcare documentation.
- Skipping the Review Process: A thorough review of SOAP records is vital for ensuring accuracy and completeness. Before completing documentation, take the time to verify that all relevant information is included and accurately recorded. This step can prevent potential errors that may affect care.
- Not Documenting in Real-Time: Delaying documentation can result in forgotten details and inaccuracies. To uphold the accuracy of medical records, document observations in real-time whenever feasible. This practice aids in capturing the nuances of patient interactions and ensures that vital information is not missed.
Integrating and other best methods into your clinical note writing can greatly improve the quality of documentation. For example, a case study named 'Conclusion on Effective Documentation Practices' emphasizes that implementing creative solutions can improve the precision and efficiency of records, ultimately resulting in better treatment outcomes and enhanced client assistance. Furthermore, a statistic shows that clients' progress on the /ch/ production objectives improved from 50% accuracy in the last session to 80% accuracy when clear and specific documentation was utilized.
By following these guidelines, healthcare providers can enhance treatment outcomes and ensure high-quality client support.
The Importance of SOAP Notes in Patient Care
Clinical records are essential for documenting client interactions and ensuring continuity of care. They provide a structured format that significantly enhances communication among healthcare providers, fostering better coordination of treatment plans. Over the past fifty years, the evolution of medical documentation has led to longer and more detailed entries, emphasizing the need for clarity and accessibility in clinical records.
Precise clinical records serve as legal documents that protect both individuals and providers during conflicts, while also playing a vital role in improving health outcomes. Research shows that well-maintained documentation correlates with enhanced continuity of care, offering a comprehensive view of a patient's history and treatment progress.
Moreover, specialists emphasize that the integrity of documentation is crucial for sustaining effective healthcare practices. Imran Shaikh, a Content Marketing Expert and SEO Specialist at Augnito AI, highlights, "It’s essential that these basic aspects of the documentation are clearly stated and accurate to maintain the integrity of the record." By ensuring clarity and accuracy in these records, healthcare professionals can promote better communication and collaboration among providers.
Practical examples illustrate how efficient documentation can lead to improved healthcare communication, ultimately enhancing the quality of service provided. Consider CosmaNeura's innovative AI platform, which automates administrative tasks and enhances clinical decision-making. This platform supports the effective use of SOAP nursing notes in patient care. With predictive analytics, CosmaNeura's AI can identify patterns in individual data, allowing healthcare providers to anticipate disease progression and identify those at greater risk of developing certain conditions.
This capability enables early interventions that significantly improve outcomes for individuals. As healthcare continues to advance, the importance of comprehensive documentation—especially through structured formats—remains a fundamental aspect of quality care. Additionally, selecting with high accuracy rates is crucial to avoid legal issues and ensure safety, further underscoring the importance of precise documentation.
The Future of SOAP Notes: Innovations and Adaptations
The future of SOAP nursing notes is on the brink of significant transformation, driven by technological advancements. As healthcare providers, we understand the emotional toll that administrative burdens can take on your ability to connect with patients. The integration of artificial intelligence and electronic health records offers a promising solution. Innovations like voice recognition and automated documentation tools from CosmaNeura are set to revolutionize the note-taking process, allowing you to dedicate more time to what truly matters—patient interactions.
Imagine a world where appointment scheduling and medical record management are streamlined through AI solutions. This can significantly ease the burden of time-consuming tasks, enabling you to focus on delivering high-quality care. However, it's essential to recognize that studies indicate healthcare professionals may need additional training to effectively utilize these new tools. Education plays a vital role in maximizing the benefits of AI in documentation.
As telehealth continues to grow, clinical records must evolve to meet the needs of virtual appointments. This ensures that documentation remains comprehensive and efficient across all service environments. The integration of AI into clinical documentation not only boosts efficiency but also enhances the accuracy of medical records—an essential factor for patient safety and satisfaction. New technologies, such as machine learning and blockchain, are expected to further refine documentation practices, enhancing clinician productivity while preserving the crucial human empathy in healthcare.
Furthermore, the ongoing development of medical records aims to improve patient care through better documentation methods and technology integration. Expert insights suggest that fostering a deeper understanding of analytics among medical professionals can significantly enhance documentation capabilities. As Dmytro Tymofiiev, Delivery Manager at SPD Technology, notes, "Sometimes it makes sense to help your medical professionals obtain additional education in data science, machine learning, or informatics to gain a deeper understanding of the intricacies of analytics."
It's important to acknowledge the limitations of the traditional SOAP model, particularly regarding its ability to document changes over time. Extensions like SOAPE could address these challenges, providing a more comprehensive framework for documentation that aligns with the goal of improving administrative efficiency. Looking toward 2025, the integration of AI in healthcare documentation is anticipated to yield substantial improvements, paving the way for a more streamlined and effective approach to care.
Prioritizing clarity and consistency in documentation practices can lead to improved workflows, , and enhanced safety. This is a crucial aspect of the future of healthcare documentation that deserves our attention and commitment.
Conclusion
Implementing SOAP notes effectively is crucial for enhancing patient care and ensuring seamless communication among healthcare providers. By breaking down patient encounters into the structured components of Subjective, Objective, Assessment, and Plan, healthcare professionals can create clear and concise documentation that captures critical information and supports informed clinical decision-making. The importance of accurate SOAP notes extends beyond documentation; it directly influences billing accuracy, compliance, and ultimately, patient outcomes.
As the healthcare landscape evolves, innovative technologies like AI and electronic health records promise to refine the documentation process even further. These advancements allow healthcare providers to focus more on patient interactions and less on administrative tasks, potentially improving both efficiency and satisfaction. Capturing patient-reported outcomes and fostering clear communication remain vital in nurturing a patient-centered approach to care.
In summary, embracing the structured framework of SOAP notes and adapting to new trends and technologies is essential for optimizing patient experiences and outcomes. By prioritizing accurate and comprehensive documentation, healthcare providers can enhance the quality of care and be well-prepared to meet the challenges of an ever-changing medical environment. The journey toward improved patient care begins with mastering the art of SOAP notes—a fundamental skill that will continue to shape the future of healthcare. How can we ensure that our documentation not only meets standards but also reflects our commitment to compassionate care?




