Overview
SOAP notes play a vital role for healthcare providers, offering a structured way to document patient encounters. By encompassing the subjective, objective, assessment, and plan components, they facilitate effective communication and ensure continuity of care. Have you ever felt overwhelmed by the demands of documentation? Mastering this format can significantly enhance patient outcomes while alleviating some of the administrative burdens you face daily.
Consider how this structured approach not only improves clarity but also fosters better relationships with your patients. By using SOAP notes, you can streamline your documentation process, allowing you to focus more on what truly matters—your patients' well-being. The benefits are clear: improved communication, better care coordination, and ultimately, happier patients.
We encourage you to explore this essential documentation format further. By embracing SOAP notes, you can enhance your practice and make a meaningful difference in the lives of those you care for. Remember, every step you take towards mastering this skill is a step towards better patient care.
Introduction
In the ever-evolving world of healthcare, the ability to document patient interactions effectively is not just important; it is essential. SOAP notes—a structured format that stands for Subjective, Objective, Assessment, and Plan—are foundational for accurate and comprehensive patient documentation. This systematic approach not only fosters clear communication among healthcare providers but also significantly enhances patient outcomes through careful record-keeping.
As technology advances, understanding the nuances of SOAP notes becomes increasingly crucial. How can we master each component and leverage AI to improve our documentation practices? The significance of SOAP notes in delivering high-quality patient care is profound.
This article explores the essential aspects of SOAP notes, offering insights into their structure, common pitfalls, best practices, and the transformative role of technology in enhancing documentation efficiency.
Understanding SOAP Notes: Definition and Importance
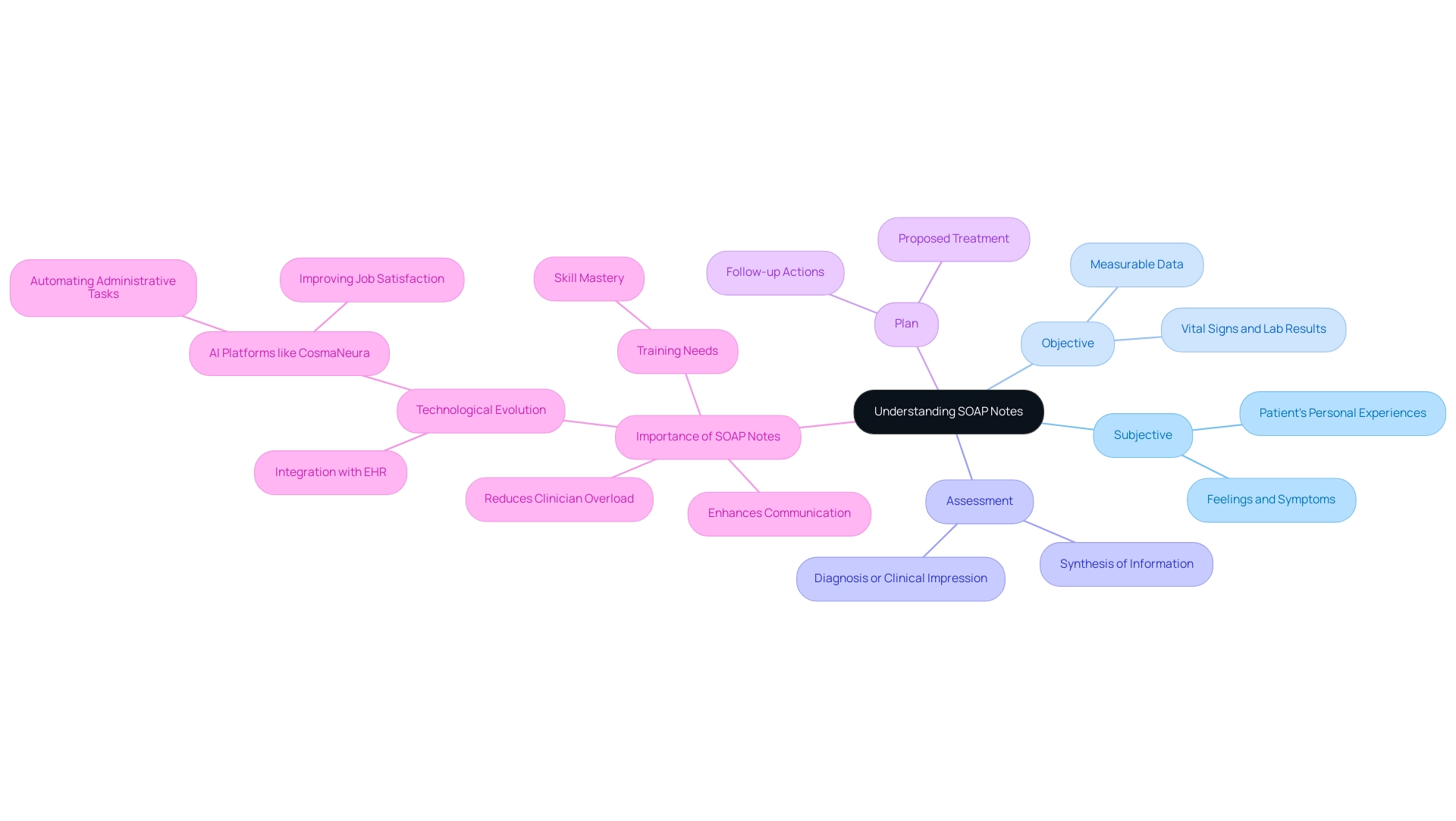
S O A P notes represent a compassionate approach to documenting patient encounters, serving as a structured method for providers to log their interactions effectively. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, with each component playing a vital role in the documentation process:
- Subjective: This section captures the patient's personal experiences, feelings, and symptoms articulated in their own words, providing valuable insight into their condition.
- Objective: This part encompasses measurable data, including vital signs, physical examination findings, and laboratory results, which are crucial for an accurate clinical picture.
- Assessment: In this segment, the medical provider synthesizes the subjective and objective information to formulate a diagnosis or clinical impression, guiding the next steps in care.
- Plan: This section outlines the proposed treatment, additional tests, referrals, or follow-up actions, ensuring a comprehensive approach to managing individuals.
The significance of S O A P notes in medical care cannot be overstated. They foster efficient communication among medical professionals, promoting continuity of care and enhancing outcomes for patients. As we look towards 2025, the organized records provided by S O A P notes remain indispensable.
Have you ever felt overwhelmed by the administrative burdens of healthcare? Studies indicate that well-organized medical records can significantly reduce clinician overload and mitigate potential patient harm, underscoring the need for clarity in documentation. Furthermore, medical professionals may require training to correctly utilize S O A P notes, highlighting the importance of mastering this essential skill.
Expert opinions emphasize that mastering notes format is crucial for healthcare professionals. As noted by Kunal Sindhu, MD, "As with any skill, practice makes perfect." This sentiment reflects the ongoing need for training and practice in utilizing S O A P notes effectively.
Consider the transformative impact of structured documentation on patient outcomes. For instance, the integration of SOAP records within the CosmaNeura platform has led to increased job satisfaction among providers and improved service delivery by automating administrative tasks. This alignment with ethical medical practices, particularly in faith-centered medical environments, further underscores the importance of SOAP records in fostering a compassionate approach to care.
In summary, the advantages of utilizing S O A P notes for client records are numerous. They not only simplify the documentation process but also play a crucial role in ensuring high-quality care. As healthcare technology advances, the significance of S O A P records remains unwavering, emphasizing their essential function in effective patient management. Let us embrace this structured approach to enhance our care for those we serve.
The Structure of SOAP Notes: Breaking Down Each Component
Each component of a SOAP note plays a crucial role in delivering comprehensive patient care:
- Subjective: This section captures the patient's perspective, including their symptoms, concerns, and emotional state. For instance, an individual might say, "I feel fatigued and anxious," which provides insight into their mental and physical health.
- Objective: Here, healthcare providers document observable and measurable data in their SOAP notes, including results from physical examinations, laboratory tests, and vital signs. An example could be, "Blood pressure: 120/80 mmHg; Heart rate: 72 bpm," which offers concrete evidence of the individual's current health status.
- Assessment: This component involves synthesizing the subjective and objective data to form a clinical judgment, which can be recorded in SOAP notes. For example, a provider might conclude, "Assessment: Generalized anxiety disorder," guiding the subsequent treatment plan.
- Plan: The final section outlines the next steps in care, including treatments, referrals, follow-up appointments, and SOAP notes. An example might be, "Plan: Refer to a psychologist for therapy; follow up in 4 weeks," ensuring a clear path forward for the individual's health journey.
In 2025, comprehending the format of SOAP notes is crucial for medical practitioners. It guarantees that all required information is recorded for efficient care of individuals. The focus on precise records is more essential than ever, particularly given the average frequency of reported data breaches in the medical field. This highlights the necessity for thorough record-keeping for safety and adherence to medical regulations.
As CosmaNeura targets the faith-focused medical sector with innovative AI solutions, mastering the SOAP notes format can significantly improve record-keeping practices. This not only enhances outcomes and satisfaction but also aligns with the increasing demand for specialized assistance in navigating regulatory frameworks.
Key Solutions:
- Automating records to ensure compliance with HIPAA and FDA guidelines.
- Streamlining processes to alleviate administrative burdens.
- Enhancing patient care through effective documentation.
Maulesh Shukla, an executive manager at Deloitte Services LP, highlights the significance of effective record-keeping in the medical field, stating, "Accurate and thorough records are essential for ensuring and compliance with regulatory standards."
Furthermore, insights from studies on regulatory changes affecting health plans underscore the importance for medical organizations to prioritize compliance strategies that incorporate record-keeping practices. By utilizing AI-powered advancements, like automated data input and real-time compliance evaluations, medical providers can improve their record-keeping processes, ultimately aiding in a more efficient and caring medical system. This specialized support is crucial for startups navigating the complex medical landscape, ensuring they meet compliance standards while delivering quality care.
Practical Examples: SOAP Notes Across Healthcare Specialties
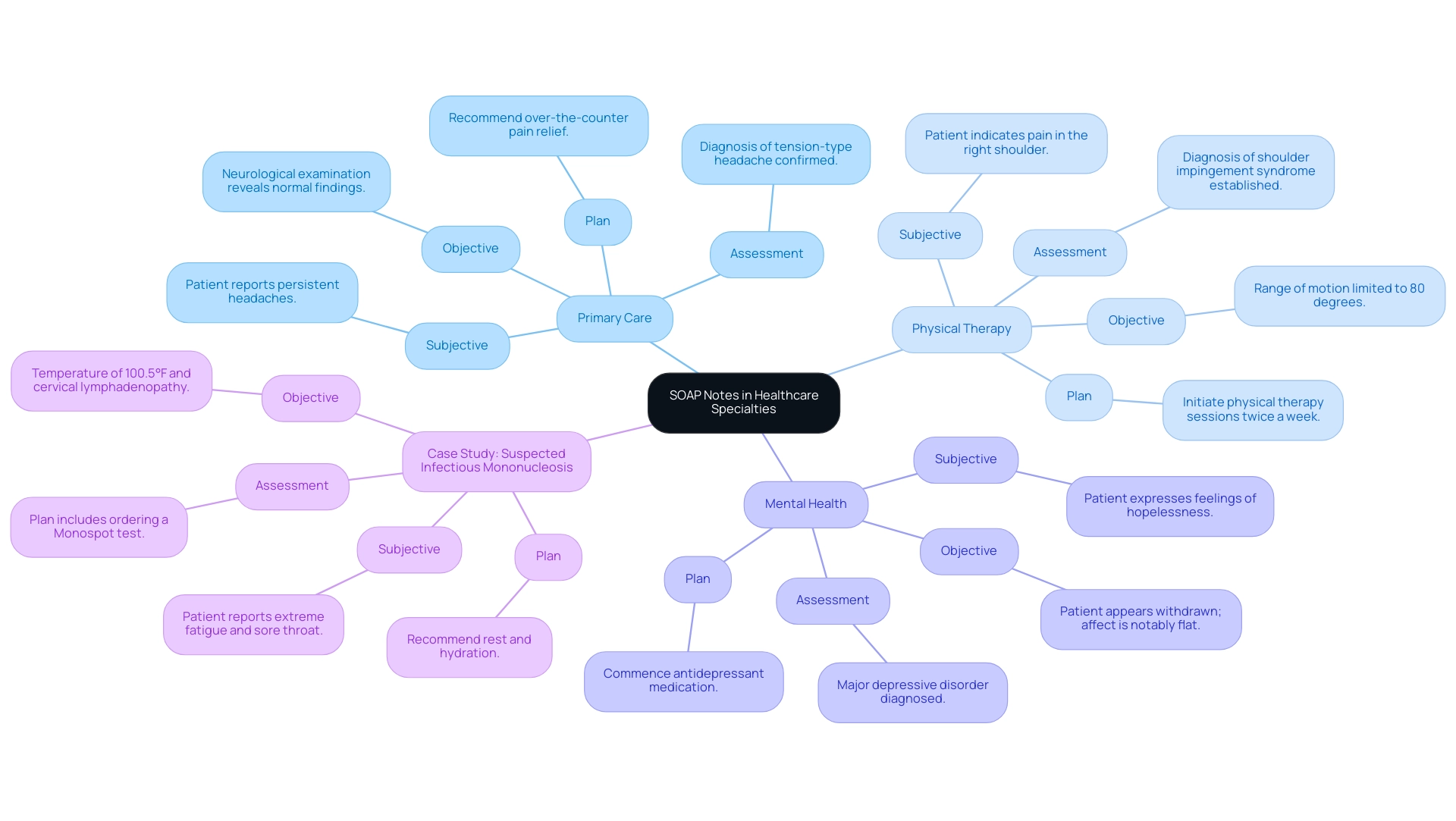
In the field of healthcare, effective documentation is not just a task; it is vital for providing compassionate care. SOAP notes serve as a standardized approach for capturing essential information that can significantly impact patient outcomes. Consider the following illustrative examples from various specialties:
-
Primary Care:
- Subjective: "Patient reports persistent headaches for the past week, describing them as moderate in intensity."
- Objective: "Neurological examination reveals normal findings; individual shows no signs of distress."
- Assessment: "Diagnosis of tension-type headache confirmed."
- Plan: "Recommend over-the-counter pain relief; advise follow-up if symptoms persist beyond one week."
-
Physical Therapy:
- Subjective: "Patient indicates pain in the right shoulder during overhead activities, rating it as 6/10."
- Objective: "Range of motion limited to 80 degrees; strength assessed at 4/5."
- Assessment: "Diagnosis of shoulder impingement syndrome established."
- Plan: "Initiate physical therapy sessions twice a week; provide education on home exercises to enhance recovery."
-
Mental Health:
- Subjective: "Patient expresses feelings of hopelessness and lack of motivation, stating, 'I just don’t feel like doing anything.'"
- Objective: "Patient appears withdrawn; affect is notably flat."
- Assessment: "Major depressive disorder diagnosed."
- Plan: "Commence antidepressant medication; schedule weekly therapy sessions to monitor progress."
These examples illustrate how SOAP notes can adapt across various healthcare environments, ensuring that records are both thorough and tailored to the unique needs of each individual. Effective SOAP notes prioritize relevant information while maintaining brevity and accuracy, which is essential for quality care. For instance, Bluedot's capability for transcription in over 17 different languages highlights the importance of effective documentation in diverse settings.
In a practical case study titled "," a patient reports extreme fatigue, sore throat, and swollen glands for one week, with a temperature of 100.5°F and cervical lymphadenopathy. The plan includes ordering a Monospot test, recommending rest and hydration, and advising against contact sports for 4–6 weeks. This case exemplifies how SOAP notes can be applied in real clinical scenarios, showcasing their role in ensuring patient safety and well-being.
When record errors occur, it is crucial to rectify them appropriately, maintaining the integrity of the medical record without misleading changes. For example, if a statement indicates, 'No visible swelling or bruising,' it should be corrected clearly and transparently if an error is identified. By adhering to these principles, healthcare providers can enhance their documentation practices, ultimately leading to better outcomes for those receiving care.
How can we ensure that our documentation practices truly reflect the care we provide? By embracing these guidelines, we can foster a supportive environment that prioritizes patient well-being and enhances our collective ability to deliver compassionate care.
Common Mistakes to Avoid When Writing SOAP Notes
When creating SOAP records, it’s essential to avoid common pitfalls to enhance care for individuals. Let’s explore some key mistakes to be mindful of:
- Vague Language: Ambiguous phrases like "feels better" can lead to misinterpretation. Instead, provide specific descriptions that clarify the patient's condition, such as "the patient reports a decrease in pain from 8 to 4 on a scale of 10."
- Inconsistent Format: A uniform structure for each SOAP record is crucial. Consistency aids clarity and ensures all pertinent information is easily accessible for any healthcare provider examining the records.
- Overly Lengthy Notes: Brevity is vital. Focus on including only pertinent information to prevent overwhelming readers with extraneous details. This not only saves time but also enhances the readability of the notes.
- Neglecting Follow-Up: Always incorporate a follow-up plan to ensure continuity of care. Clearly specify when the individual should return for a check-up or any additional assessments, which is vital for ongoing treatment.
- Ignoring Individual Input: The subjective section should accurately reflect the individual's voice and concerns. Involving individuals in their care fosters better communication and can lead to improved outcomes.
By recognizing and addressing these common errors, healthcare providers can significantly enhance the quality of their SOAP notes, ultimately leading to better care and safety. Research shows that effective communication and record-keeping practices are essential in minimizing medical errors, with interprofessional collaboration serving as a key component in improving patient outcomes. The OCR receives over 60,000 data breach notifications every year, underscoring the importance of accurate records in preventing mistakes that could result in data breaches.
Moreover, the Institute of Medicine (IOM) emphasizes that fatigue during shift work raises error rates, highlighting the necessity for medical providers to remain vigilant and precise in their record-keeping. Therefore, refining the quality of SOAP notes is not merely a matter of record-keeping; it is toward ensuring patient safety and satisfaction.
Best Practices for Writing Effective SOAP Notes
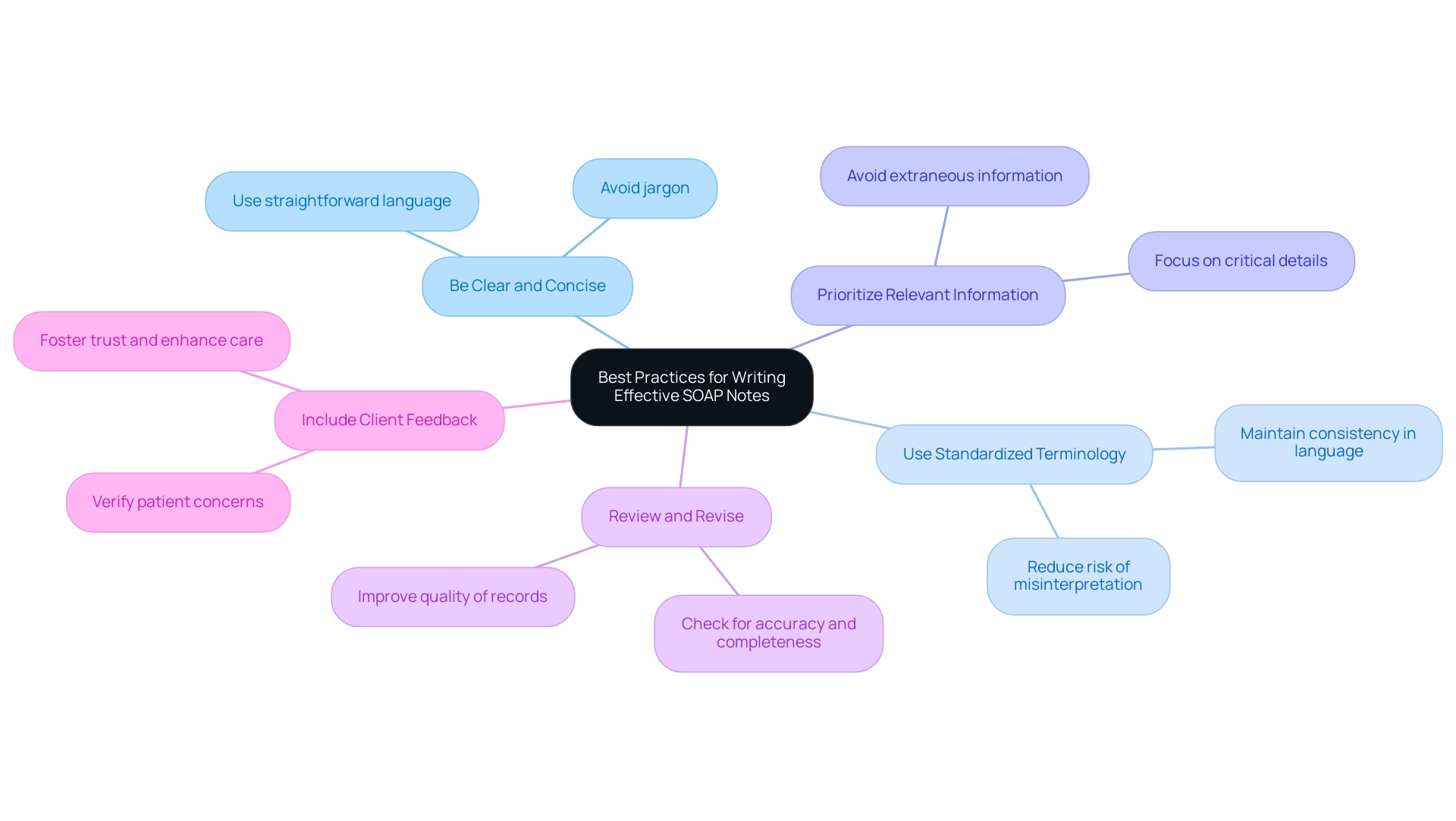
To write effective SOAP notes, healthcare providers should embrace the following best practices:
- Be Clear and Concise: Use straightforward language that avoids jargon, ensuring that your notes are easily understood by all members of the healthcare team. This clarity is essential for effective communication and continuity of care.
- Use Standardized Terminology: Consistency in language is crucial. Employing standardized medical terminology helps maintain clarity and reduces the risk of misinterpretation, which is vital in a fast-paced healthcare environment.
- Prioritize Relevant Information: Focus on the most critical details that directly impact patient care. By avoiding extraneous information, you can ensure that the records remain relevant and actionable.
- Review and Revise: Before finalizing your notes, take a moment to review them for accuracy and completeness. This practice not only improves the quality of records but also reduces the likelihood of mistakes that could impact outcomes for individuals.
- Include Client Feedback: Involve individuals in the recording process by verifying that their concerns are accurately represented in the subjective section. This inclusion fosters trust and enhances the quality of care by ensuring that patient perspectives are considered.
In today's rapidly evolving medical environment, effective documentation is more critical than ever. With the global Internet of Medical Things market projected to reach $286.77 billion by 2025, the importance of accurate record-keeping cannot be overstated. As Dmytro Tymofiiev, Delivery Manager at SPD Technology, wisely notes, 'Sometimes it makes sense to help your medical professionals obtain additional education in data science, machine learning, or informatics to gain a deeper understanding of the intricacies of analytics.' This understanding is essential, as acts as a transformative influence that enhances care and operational efficiency.
Moreover, investing in scalable and interoperable technology is vital for medical organizations to manage increasing data volumes, directly impacting the record-keeping process. Efficient record-keeping techniques can also streamline compliance procedures, as emphasized in the case study 'Closing Thoughts on Healthcare Compliance,' ultimately fostering trust in care for individuals.
By implementing these best practices, medical providers can significantly enhance the effectiveness of their SOAP notes. Clear and concise records not only improve patient care but also contribute to greater patient satisfaction levels, which are increasingly recognized as a crucial measure of quality in 2025. As the medical landscape evolves, the ability to document effectively will remain a cornerstone of successful patient-provider interactions.
Leveraging Technology: Enhancing SOAP Note Documentation with AI
The incorporation of technology, especially AI, is transforming the process of SOAP notes in medical care.
- Automated Data Entry: Imagine a world where AI tools capture client interactions in real-time, significantly decreasing the time healthcare providers spend on manual record-keeping. This efficiency allows clinicians to focus more on what truly matters—patient care—rather than getting bogged down by administrative duties.
By utilizing advanced voice dictation technology, providers can efficiently record information as SOAP notes during patient encounters. This not only simplifies the record-keeping process but also enhances the precision of the entries, as they are produced in real-time.
- Standardized Templates: AI can create uniform templates that guide providers in following the SOAP notes format. This guarantees that all essential elements—Subjective, Objective, Assessment, and Plan—are included, fostering consistency and completeness in records. Furthermore, AI systems can analyze historical SOAP notes to identify trends and areas for improvement in record-keeping practices. This analytical capability empowers providers to refine their approach, leading to better outcomes.
can be seamlessly integrated into electronic health record (EHR) systems. This integration ensures that patient information is not only easily accessible but also current, promoting improved clinical decision-making.
The influence of AI on medical record-keeping is profound. By 2025, statistics indicate that automated record-keeping solutions are becoming increasingly vital, with many healthcare providers recognizing the need for AI-driven tools to enhance their workflows. Importantly, 91% of physicians must be aware that GenAI-sourced materials were developed by doctors and medical experts before utilizing them in clinical decisions, highlighting the importance of trust in AI-generated records.
Moreover, as noted by Wolters Kluwer, 68% of physicians have shifted their perspectives over the past year and are now more inclined to believe that GenAI could be beneficial to healthcare. Additionally, the market for AI-integrated medical imaging is projected to expand at a 26.5% CAGR from 2021 to 2028, indicating a strong trend towards AI adoption in diagnostics, paralleling the enhancements observed in SOAP records. Regular auditing of payer payments is also essential for ensuring accurate reimbursement in medical practices, underscoring the importance of precision in records.
As the market for AI-integrated solutions continues to grow, healthcare providers can anticipate improved efficiency and accuracy in their SOAP notes, ultimately leading to enhanced patient care. How might embracing these innovations transform your practice and the care you provide?
Conclusion
In today's healthcare landscape, effective documentation through SOAP notes is not just a task—it's essential for delivering high-quality patient care. Understanding the structured components of SOAP—Subjective, Objective, Assessment, and Plan—allows healthcare providers to capture comprehensive patient information. This approach enhances communication and continuity of care, ultimately leading to better patient outcomes.
However, common pitfalls in writing SOAP notes, such as vague language and neglecting follow-up plans, can create misunderstandings and compromise patient safety. By embracing best practices—being clear, concise, and incorporating patient feedback—providers can significantly elevate the quality of their documentation. Moreover, the integration of technology, particularly AI, is revolutionizing the documentation process. Automated data entry and real-time note creation not only enhance efficiency but also improve accuracy.
As the healthcare industry evolves, the importance of effective SOAP note documentation remains a cornerstone of successful patient-provider interactions. Prioritizing clarity and consistency in documentation practices can lead to improved workflows and heightened patient satisfaction and safety. By adopting these strategies, we can ensure that the art of documentation thrives, fostering a more effective and compassionate healthcare system.
What steps will you take today to enhance your documentation practices and support your patients better?




