Overview
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver quality care. The article focuses on essential examples of SOAP notes, illustrating their vital role in standardizing clinical documentation. By utilizing structured SOAP notes, healthcare providers can improve communication, which is crucial in fostering trust and understanding with patients.
Imagine the relief of reducing administrative burdens—this not only enhances the quality of care but also allows providers to dedicate more time to what truly matters: patient care. The benefits of using SOAP notes extend beyond mere documentation; they create a supportive environment where healthcare professionals can thrive.
Are you ready to embrace a solution that can transform your practice? By implementing SOAP notes, you can alleviate some of the pressures of paperwork, ultimately enriching your interactions with patients. This approach not only streamlines your workflow but also nurtures a compassionate atmosphere in healthcare.
Let’s take a moment to reflect on the impact of these tools. Consider how much more fulfilling your day could be when you focus less on administrative tasks and more on the individuals you care for. The journey towards improved patient care begins with a single step—adopting structured SOAP notes can be that step.
Introduction
In the fast-paced world of healthcare, the pressure to maintain accurate and efficient documentation can often overshadow the primary goal: patient care. This can be overwhelming for many healthcare providers. The use of SOAP notes has emerged as a crucial tool, offering a structured method to capture vital patient information while alleviating some of the administrative burdens that can detract from patient focus.
Yet, how can providers ensure that these notes not only meet regulatory standards but also enhance the quality of care? This article delves into ten essential examples of SOAP notes, highlighting innovative solutions and best practices. These insights empower healthcare professionals to streamline their documentation processes, ultimately improving patient outcomes.
Together, let’s explore how we can navigate these challenges and foster a more compassionate approach to patient care.
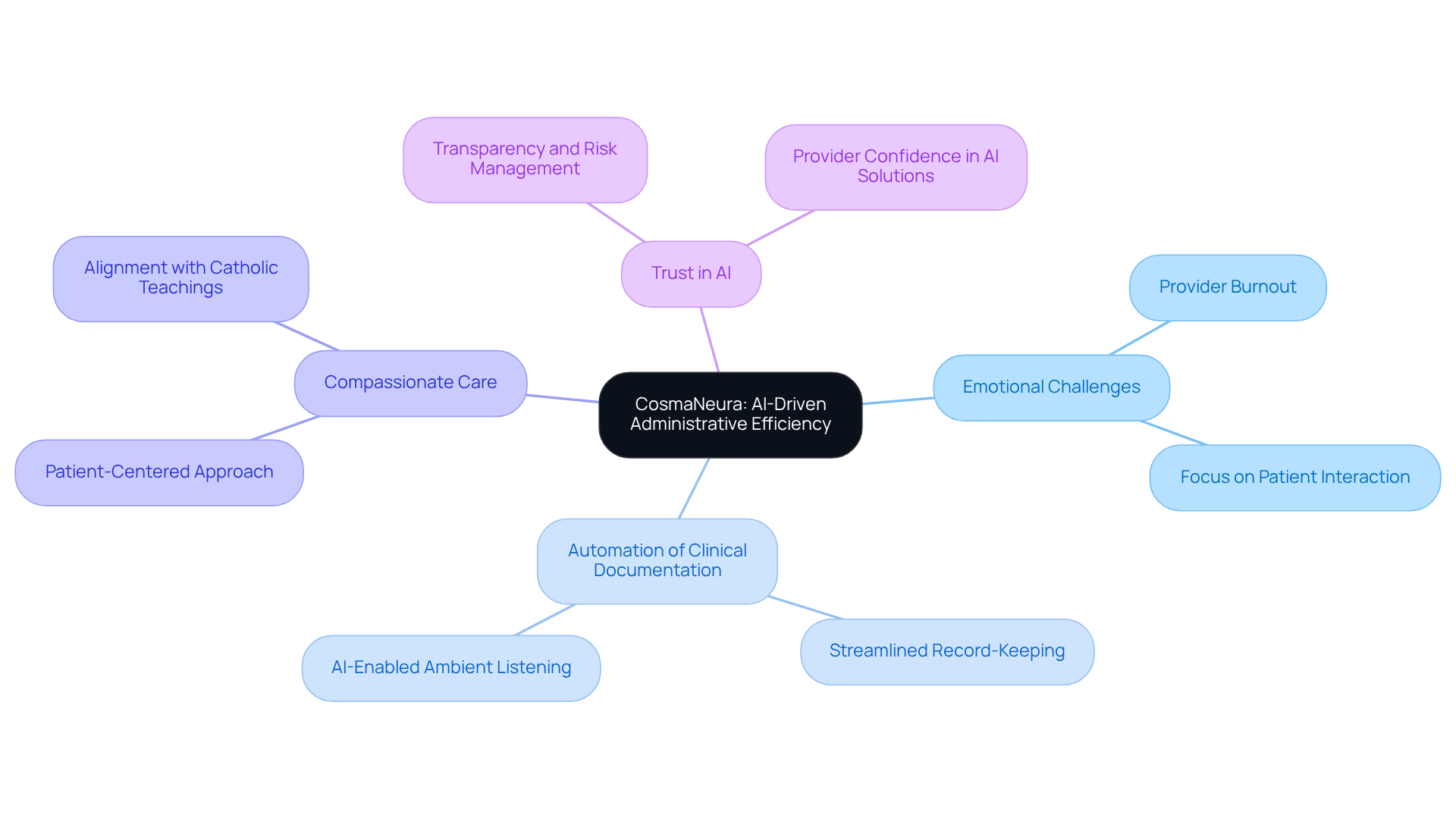
CosmaNeura: AI-Driven Administrative Efficiency for SOAP Notes
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to deliver compassionate care. CosmaNeura understands these emotional challenges and utilizes advanced AI technology to simplify the creation of clinical documentation. By significantly reducing the time spent on record-keeping, the platform allows providers to focus more on their interactions with patients.
Imagine a world where client intake and triage are autonomously managed, ensuring that examples of soap notes are generated with both accuracy and efficiency. This automation not only enhances administrative efficiency but also fosters a deeper connection between providers and their patients, ultimately improving the quality of care.
CosmaNeura stands out by aligning its operations with the mission of delivering compassionate care rooted in Catholic teachings. The incorporation of AI in record-keeping represents a significant shift towards a more efficient healthcare model, promoting a patient-centered approach that truly values individual needs.
Moreover, CosmaNeura addresses the prevalent concerns among healthcare providers regarding the rapid adoption of AI technologies. By prioritizing trust and transparency in its solutions, CosmaNeura not only enhances administrative efficiency but also supports providers in navigating the complexities of innovation in care. How might your practice transform if you could focus more on your patients and less on paperwork? Engage with CosmaNeura today to explore how this compassionate approach can benefit your practice and enhance the care you provide.
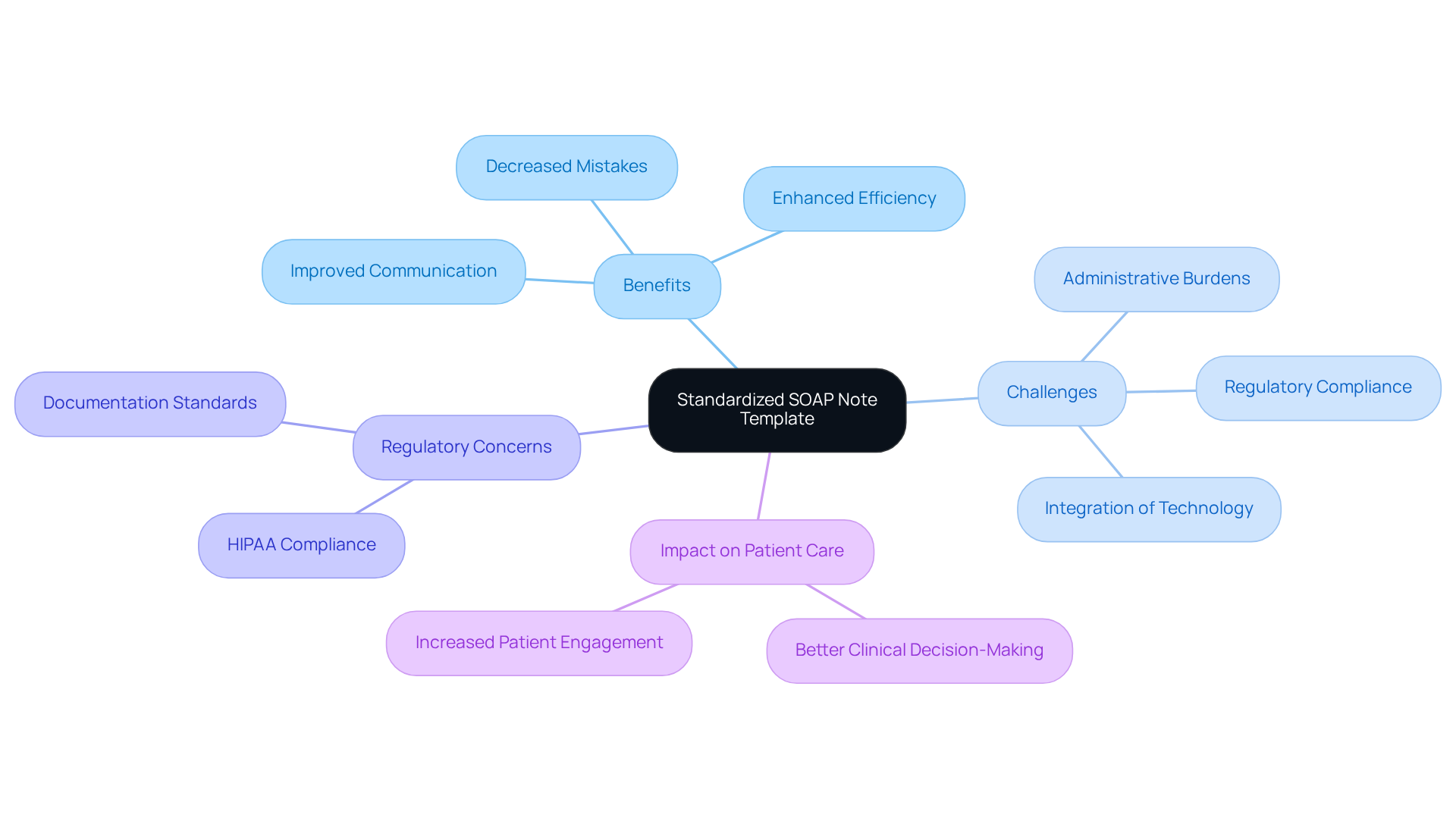
Heidi Health: Comprehensive SOAP Note Template for Standardization
Heidi Health understands the emotional challenges faced by healthcare providers, especially when it comes to managing documentation. The comprehensive SOAP note template offered serves as one of the examples of soap designed to standardize records across various healthcare settings, addressing the administrative burdens that can impact patient care. This template provides examples of soap that encompass all vital elements—Subjective, Objective, Assessment, and Plan—ensuring that healthcare providers consistently capture essential information about individuals.
By adopting such standardized documentation practices, providers can significantly enhance communication and continuity of care. This is especially important given regulatory concerns like HIPAA, which can create obstacles between individuals and providers. The result is improved outcomes for individuals, as clear and structured records promote better clinical decision-making and encourage teamwork among healthcare groups.
Moreover, the adoption of standardized documentation has been proven to decrease mistakes and enhance the overall quality of care for individuals. It serves as an essential resource for healthcare practitioners. Practices employing AI solutions have reported 75% quicker record-keeping, showcasing the efficiency achieved through standardized processes and helping to reduce physician burnout.
As Larry Weed wisely observed, the structured format is crucial for efficient clinical reasoning. Prompt documentation—preferably within 24 hours following patient interactions—ensures precision and thoroughness. Addressing common pitfalls in documentation, such as incomplete records and non-standard abbreviations, is essential for maximizing the benefits of this standardized approach.
In embracing these solutions, healthcare providers can create a more supportive environment for themselves and their patients. How might adopting these practices transform your workflow and enhance patient care? Let's work together to foster a culture of clarity and compassion in healthcare documentation.
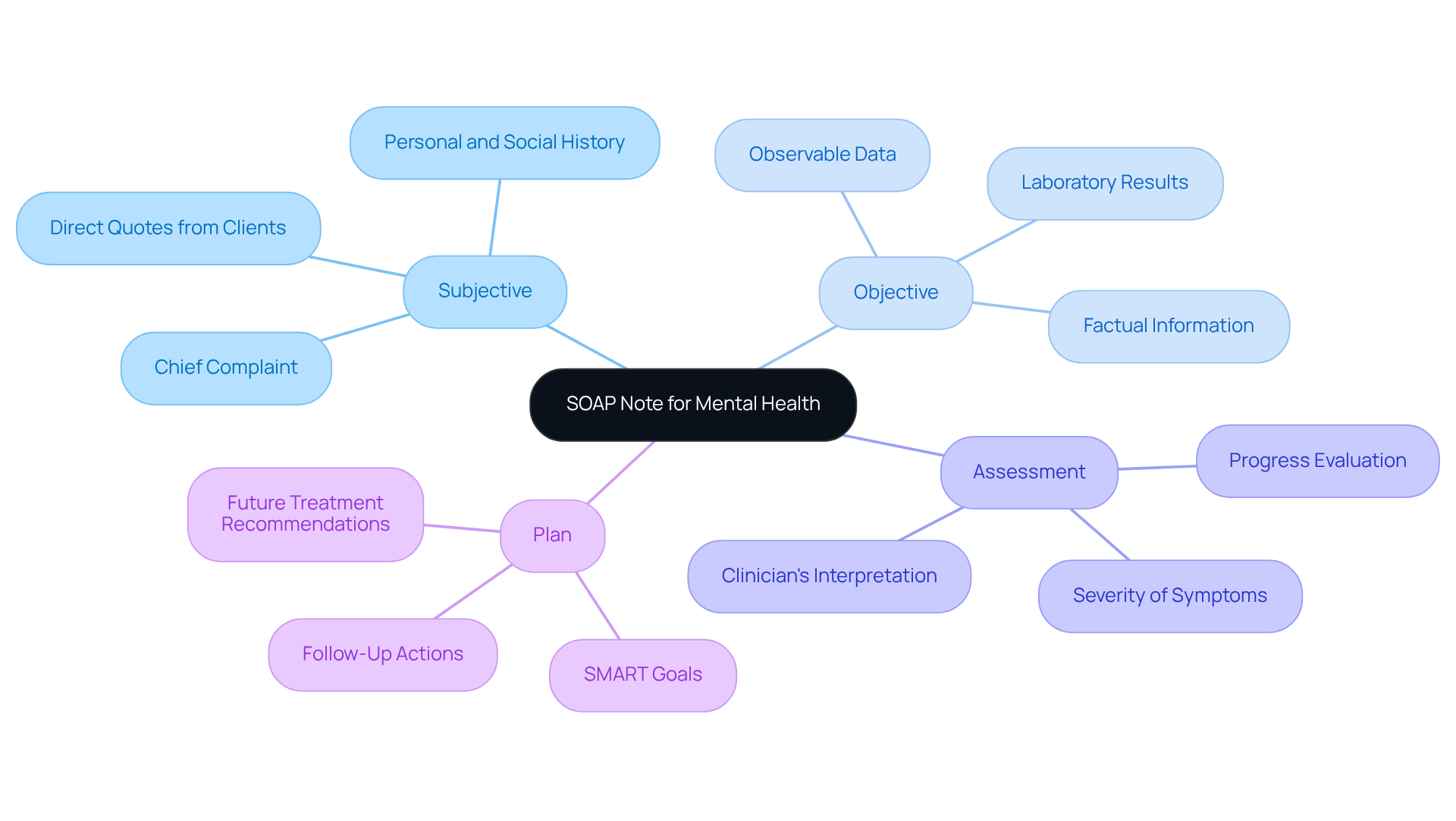
Mentalyc: Tailored SOAP Note Examples for Mental Health Practitioners
Mentalyc understands the emotional challenges that mental health professionals face daily. Customized documentation examples are specifically designed to address these needs, focusing on the nuances of mental health evaluations and interventions. By enabling providers to effectively record individual progress, these examples help alleviate some of the administrative burdens that can impact patient care.
Each SOAP record serves as examples of soap that include four essential elements:
- Subjective
- Objective
- Assessment
- Plan
The Subjective section features direct quotes from individuals, enhancing the accuracy of documentation and reflecting their unique experiences. How often do we find ourselves struggling to capture the true essence of our clients' feelings? Utilizing these tailored documents ensures that practitioners meet the specific requirements of their patients, promoting a more individualized approach to care.
It is advisable to finalize session summaries swiftly, ideally within 24-48 hours after meetings, to preserve precision. While structured records are invaluable for standardizing reports, it's crucial to recognize their limitations in capturing the complexities of mental health treatment. Have you considered how technology can aid in managing and organizing clinical records? Incorporating such tools can further enhance the documentation process, fostering accountability and transparency in the therapeutic journey.
Together, let’s embrace these solutions to not only improve our documentation practices but also to enrich the care we provide to those who trust us with their mental health.
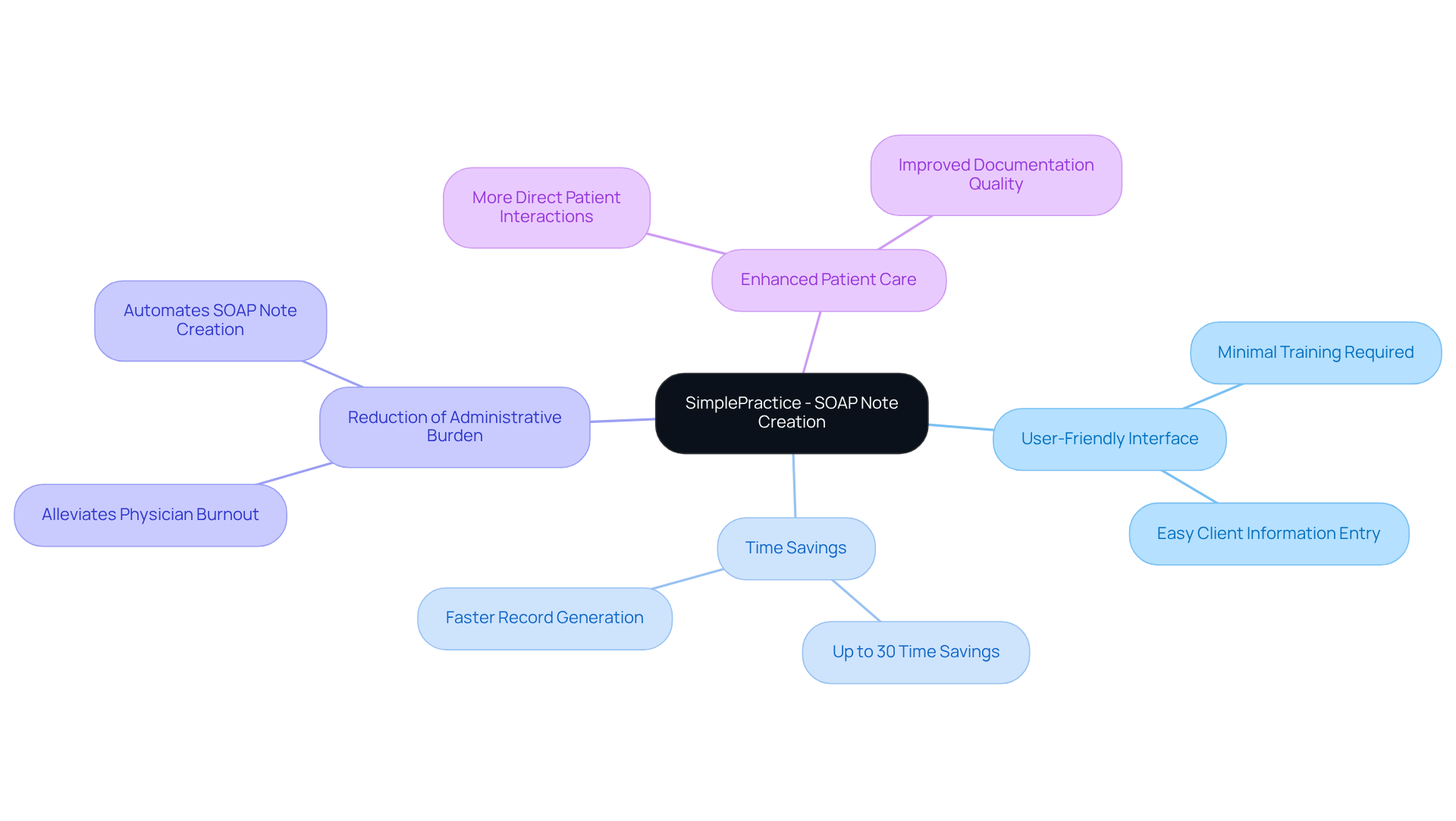
SimplePractice: User-Friendly SOAP Note Creation Platform
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to deliver quality patient care. SimplePractice stands out as a compassionate solution, offering an easy-to-use platform that simplifies the generation of examples of SOAP documents. With its user-friendly interface, professionals can quickly enter client information and produce detailed records with minimal training.
This simplicity not only saves precious time but also fosters more precise and comprehensive records, ultimately enhancing the quality of care for individuals. By automating the creation of SOAP notes, which are examples of SOAP, SimplePractice alleviates some of the administrative pressures that contribute to physician burnout. This allows healthcare providers to focus more on what truly matters: direct patient interactions.
Research suggests that platforms like SimplePractice can lead to significant decreases in record-keeping time. Independent evaluations have shown time savings of up to 30% in certain instances. Imagine how much more effective your practice could be with such intuitive record-keeping tools! By adopting these solutions, healthcare providers can experience enhanced workflow efficiency and greater job satisfaction, creating a more effective healthcare environment.
Furthermore, with the emergence of AI documentation tools offering features like coding suggestions and gap-closure prompts, providers can further enhance their documentation processes. To maximize these benefits, consider integrating user-friendly platforms like SimplePractice into your practice. Your patients—and your well-being—deserve it.
Headway: Specialized SOAP Note Templates for Therapists
Therapists often face emotional challenges in their practice, balancing the needs of their patients with the demands of documentation. Headway offers specialized templates that serve as examples of soap notes designed specifically for therapists, addressing these unique aspects of therapeutic practice. These templates serve as a guiding framework, helping therapists document treatment goals, interventions, and patient progress in a structured manner.
By utilizing these tailored templates, therapists can alleviate some of the administrative burdens that can impact patient care. This ensures that their documentation not only captures the intricacies of their work but also enhances the therapeutic relationship. Imagine the peace of mind that comes from knowing your notes reflect the depth of your practice.
Consider how these specialized templates can transform your documentation process. They provide clarity and focus, allowing you to dedicate more time to what truly matters—your patients. Embrace the opportunity to enhance your practice and foster deeper connections with those you serve.
Bluedot HQ: Diverse SOAP Note Examples Across Specialties
Access to a varied collection of documentation examples across different healthcare specialties is essential for healthcare providers. Have you ever felt overwhelmed by the administrative tasks that can take time away from patient care? In dermatology, for instance, the examples of SOAP records detail skin conditions and treatments, while pediatric SOAP records monitor developmental milestones and immunization status. By exploring various record styles and formats, providers can customize their notes to better suit their specific practice requirements.
This approach not only enhances record-keeping abilities but also significantly elevates the overall standard of care for individuals. Varied documentation styles foster clarity and organization, which are essential for effective communication among multidisciplinary teams. Furthermore, specialist perspectives highlight that employing different examples of SOAP can lead to more thorough patient evaluations and improved treatment strategies.
As one expert observed, "Utilizing templates based on your preferred models simplifies progress records and guarantees consistency throughout all your documents." Imagine the peace of mind that comes from knowing your documentation is both efficient and effective.
Ultimately, consider integrating templates from different specialties into your practice to refine your documentation practices. This ensures they meet both clinical and regulatory standards, allowing you to focus more on what truly matters—providing compassionate care to your patients.

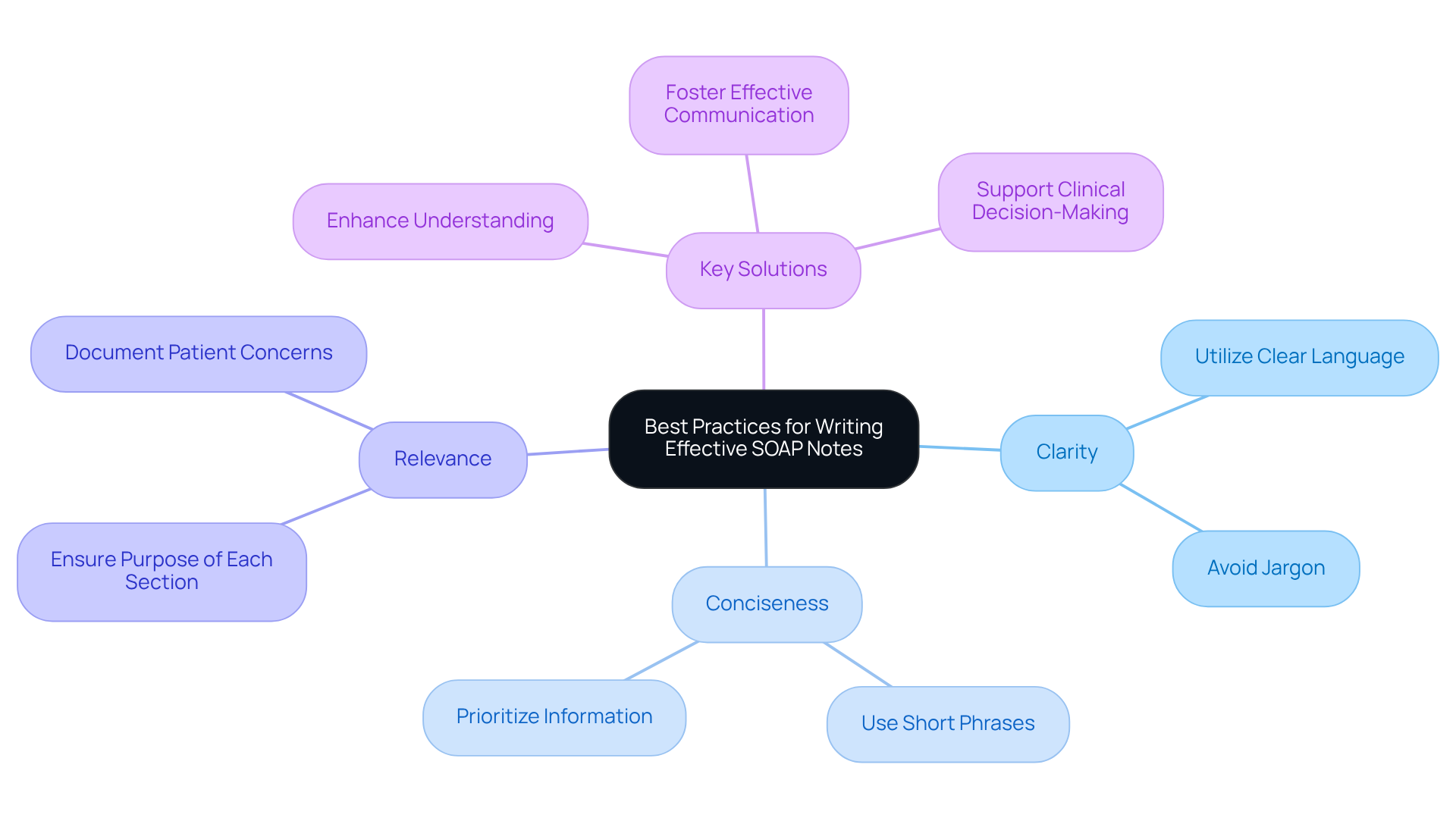
Psylio: Best Practices for Writing Effective SOAP Notes
In the demanding world of healthcare, providers often face emotional challenges that can impact their ability to deliver optimal patient care. Psylio outlines best practices for crafting effective documentation, emphasizing clarity, conciseness, and relevance. By utilizing clear language and steering clear of jargon, every part of the document can serve a distinct function, alleviating some of the administrative burdens that can weigh heavily on professionals.
This structured approach, developed in the 1950s, has become a fundamental component of medical records. It offers healthcare professionals a systematic way to capture, arrange, and convey patient information. By following these best practices, healthcare providers can create documentation that is not only informative but also enhances communication with other members of the care team.
Effective clinical records act as a legal and professional safeguard. They ensure adherence to recording standards and protect against audits, providing peace of mind. Integrating clear and concise records can greatly enhance individual care and clinical decision-making, ultimately leading to improved health outcomes.
Consider the following key solutions to improve your documentation practices:
- Utilize clear language to enhance understanding.
- Avoid jargon to ensure accessibility for all team members.
- Ensure each section of the document serves a clear purpose.
By embracing these best practices, healthcare providers can foster a more supportive and effective environment, ultimately benefiting both themselves and their patients. How can you start implementing these strategies today?
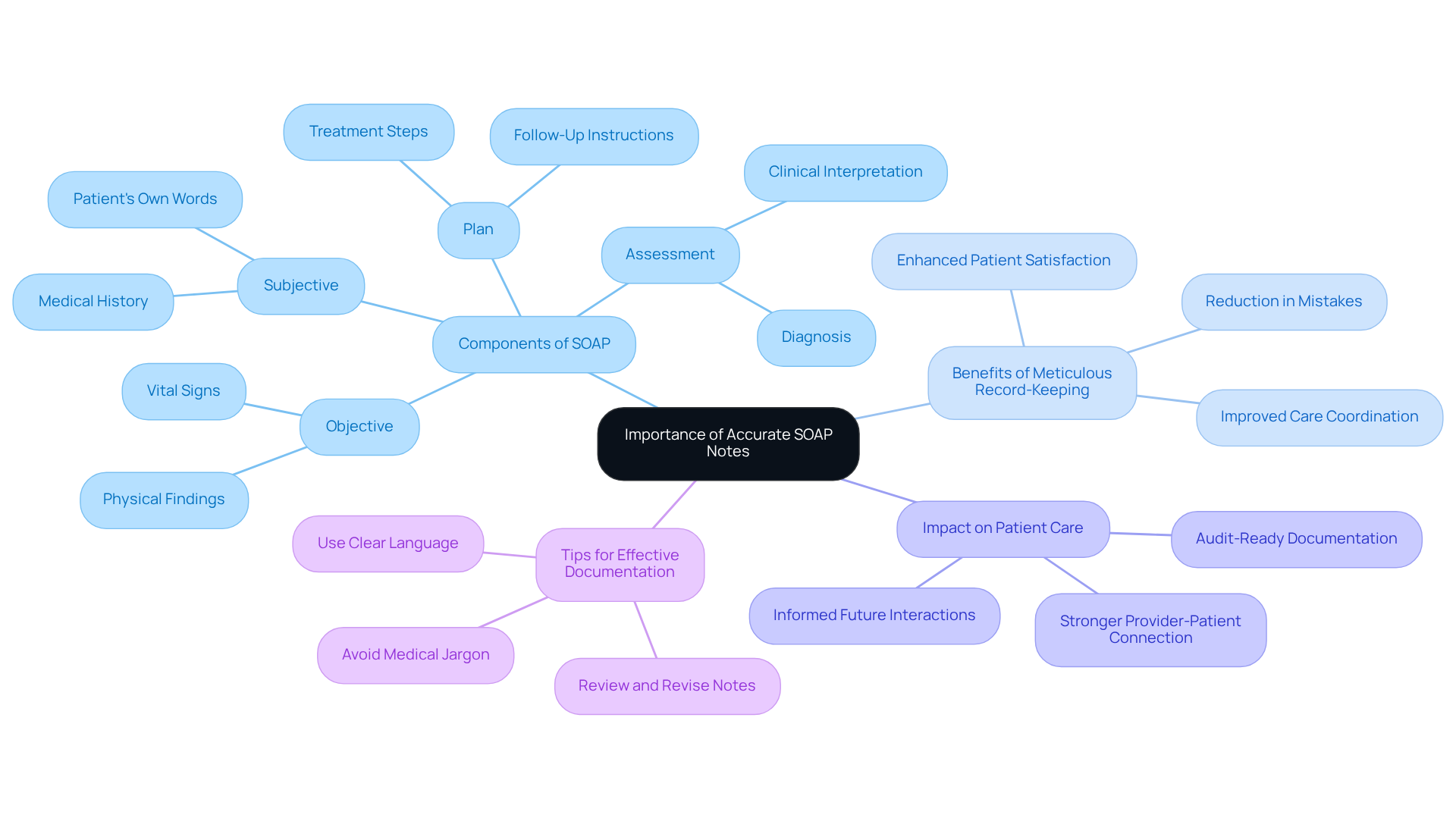
NP Charting School: Tips and Examples for Accurate SOAP Notes
In the demanding world of healthcare, providers often face emotional challenges that can weigh heavily on their ability to deliver care. The NP Charting School recognizes this struggle and offers vital assistance for creating accurate SOAP notes, providing examples of SOAP to emphasize the importance of comprehensive record-keeping. Thorough medical histories and precise evaluations are not just administrative tasks; they are essential components that directly influence patient care and outcomes.
Research shows that meticulous record-keeping can lead to enhanced satisfaction among patients and a decrease in mistakes. This reinforces the necessity for healthcare providers to prioritize careful documentation. By embracing best practices, providers can create records that not only reflect the patient's current condition but also serve as valuable references for future interactions.
Imagine the difference it can make when documentation is clear and comprehensive. It ultimately enhances the quality of care delivered, fostering a stronger connection between providers and patients. We encourage healthcare providers to engage with these resources and take proactive steps towards improving their record-keeping practices. Together, we can elevate the standard of care and ensure that every patient feels valued and understood.
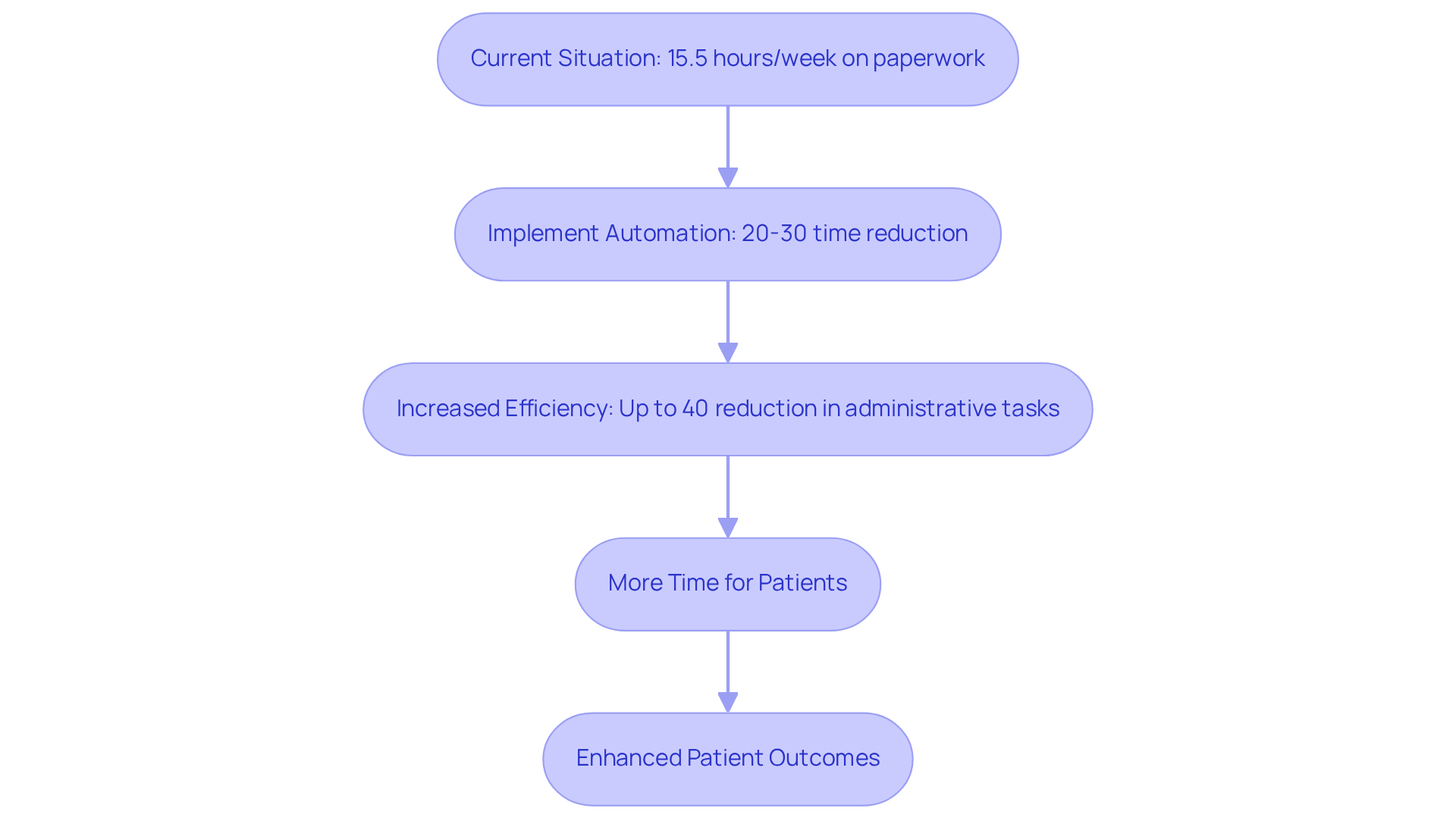
Upheal: Streamlined Documentation Solutions for SOAP Notes
Healthcare providers often face overwhelming emotional challenges due to the extensive administrative tasks that accompany their vital work. Upheal understands this struggle and offers creative documentation solutions tailored specifically for clinical records. By automating various aspects of record-taking, healthcare professionals can produce structured documentation quickly and accurately, significantly reducing the time spent on administrative duties by up to 40%. This newfound efficiency allows clinicians to refocus their efforts on delivering exceptional care, ultimately leading to improved outcomes for patients in need.
Imagine dedicating approximately 15.5 hours each week to paperwork. This burden can be alleviated through automation. With AI-powered tools, the time required for documentation can be reduced by 20-30%. This means providers can either attend to more patients or spend additional quality time with each individual. Furthermore, automated records help ensure adherence to healthcare standards, minimizing errors that could lead to liability concerns. As the healthcare landscape evolves, embracing automation in clinical documentation is not just a trend; it is essential for enhancing operational efficiency and clinician satisfaction.
Now is the time to consider how these solutions can transform your practice. By reducing the administrative load, you can focus on what truly matters: your patients. Let’s explore how embracing these innovative tools can not only lighten your workload but also enrich the quality of care you provide.
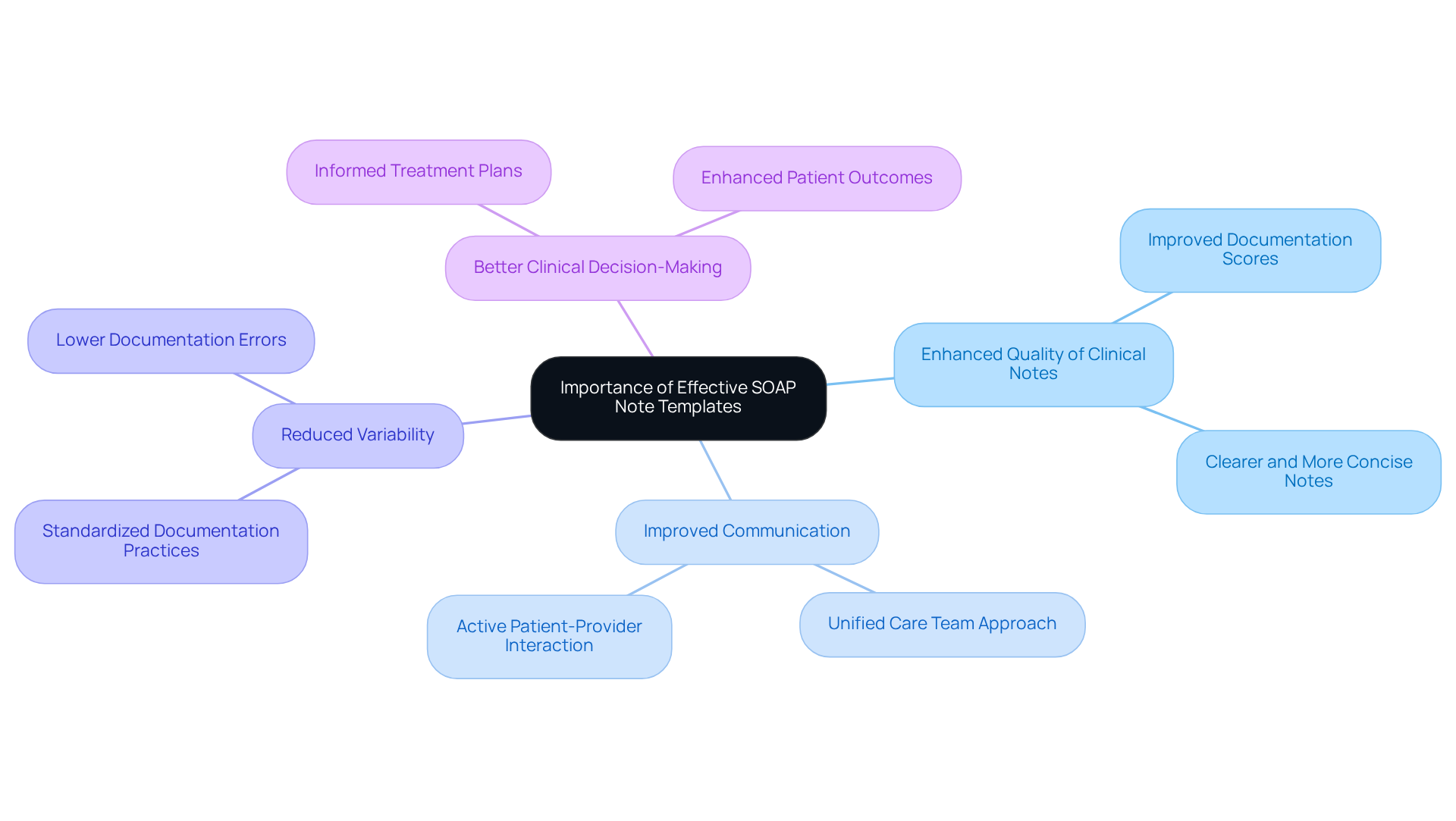
Heidi Health: Importance of Effective SOAP Note Templates in Healthcare
In the demanding world of healthcare, the emotional challenges faced by providers can be overwhelming. The administrative burdens often distract from what truly matters: the care of individuals. This is where examples of soap templates become essential for efficient use. They not only standardize records but also ensure a thorough capture of client information, alleviating some of the stress healthcare providers experience.
Studies reveal that organized records significantly improve the quality of clinical notes, leading to better outcomes for those receiving care. For instance, one study found that utilizing structured templates raised quality scores from 64.35 to 77.2. This clear link between systematic record-keeping and enhanced care underscores the importance of adopting such practices in daily routines.
Moreover, effective templates foster better communication among care teams, promoting a unified approach to managing individuals' health. By embracing standardized templates, healthcare providers can simplify their record-keeping processes. This ultimately results in more precise and effective care, supporting not only the providers but also the individuals they serve.
Consider the following key benefits of using efficient SOAP templates:
- Enhanced quality of clinical notes.
- Improved communication within care teams.
- Reduced variability in documentation quality.
- Better clinical decision-making.
These advantages positively impact patient outcomes, allowing healthcare providers to focus more on their patients and less on paperwork. It’s time to embrace this systematic approach and take a step towards reducing administrative burdens. By doing so, we can ensure that every individual receives the compassionate care they deserve.
Conclusion
The integration of effective SOAP notes in healthcare is essential for enhancing both administrative efficiency and the quality of patient care. By utilizing structured documentation, healthcare providers can significantly alleviate the burdens associated with record-keeping, allowing them to focus more on their interactions with patients. This shift not only improves operational workflows but also reinforces the compassionate care that is central to the healthcare mission.
Throughout this article, we have explored various platforms and strategies, showcasing how tools like CosmaNeura, Heidi Health, and SimplePractice contribute to the creation of high-quality SOAP notes. From standardized templates that ensure consistency and clarity to AI-driven solutions that streamline documentation processes, the insights presented highlight the transformative potential of adopting best practices in SOAP note writing. Each example demonstrates how tailored documentation can enhance communication among care teams, reduce errors, and ultimately lead to better health outcomes for patients.
Embracing these innovative approaches to SOAP notes is not merely about reducing paperwork; it is about fostering a healthcare environment where providers can prioritize patient care over administrative tasks. As the landscape of healthcare continues to evolve, integrating effective documentation practices will be crucial for delivering compassionate, efficient, and high-quality care.
It is time for healthcare professionals to reflect on their current documentation strategies. Consider how adopting these solutions can enhance your practice, improve patient relationships, and elevate the standard of care provided. Together, we can create a healthcare environment where compassion and efficiency coexist, ultimately benefiting both providers and patients.




