Overview
In the demanding world of healthcare, nurse practitioners often face emotional challenges, particularly when it comes to documentation. The weight of administrative burdens can detract from the quality of patient care, leaving providers feeling overwhelmed. This article highlights essential SOAP note templates designed to alleviate these pressures, ultimately enhancing both documentation efficiency and patient care.
Imagine a tool that streamlines record-keeping, allowing you to focus more on your patients. These templates incorporate features like automated data entry and specialty-specific customization, which not only improve the quality of care but also significantly reduce the administrative load on healthcare providers. By adopting these tools, you can reclaim valuable time and energy.
The benefits are clear: improved documentation leads to better patient outcomes and a more satisfying work experience. As you consider these solutions, reflect on how much easier your day-to-day tasks could be with the right support. We encourage you to explore these SOAP note templates further and discover how they can transform your practice, enabling you to provide the compassionate care your patients deserve.
Introduction
In the fast-paced world of healthcare, effective documentation transcends routine tasks; it stands as a cornerstone of quality patient care. Nurse practitioners often grapple with the emotional challenge of balancing comprehensive record-keeping with the need to devote ample time to their patients. This article delves into ten essential SOAP note templates, crafted to streamline the documentation process, enhance clinical accuracy, and ultimately improve patient outcomes.
Have you ever wondered how these templates can alleviate administrative burdens and elevate the standard of care across diverse medical settings? Let's explore this together.
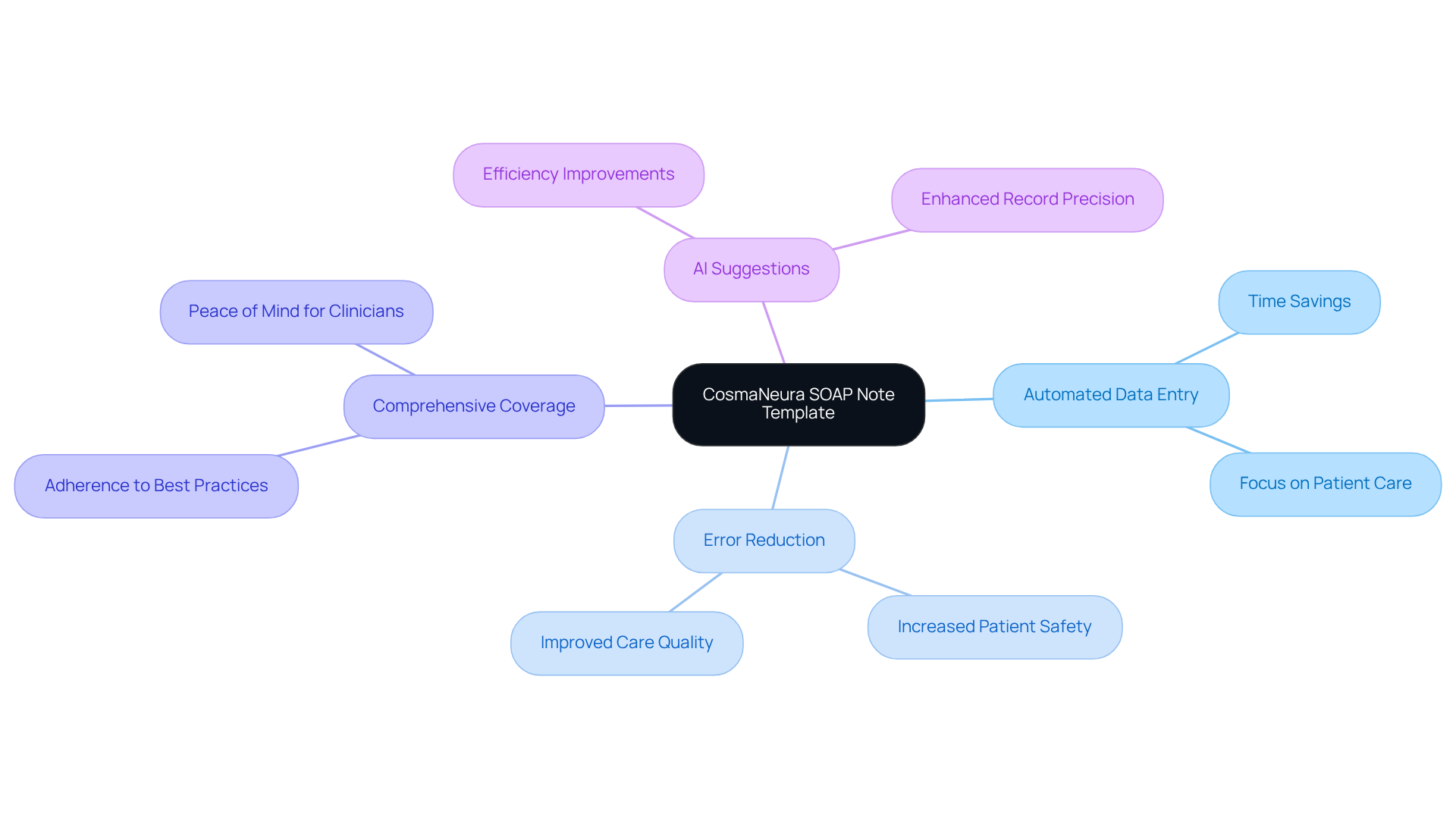
CosmaNeura SOAP Note Template: Streamline Documentation with AI
The soap note template nurse practitioner from CosmaNeura is here to transform the record-keeping process for healthcare providers, harnessing the power of AI to ease your burden. This innovative template automates data entry, ensuring that all essential information is captured with precision. By significantly reducing the time spent on records through the use of a soap note template nurse practitioner, it allows you to dedicate more attention to your patients, ultimately enhancing the quality of care you provide.
Key features of the template include:
- Automated Data Entry: Minimizing manual input, this feature leads to substantial time savings for clinicians, allowing you to focus on what truly matters—your patients.
- Error Reduction: By automating the record-keeping process, the template significantly decreases the likelihood of errors, promoting patient safety and improving overall care quality.
- Comprehensive Coverage: The soap note template nurse practitioner is structured to ensure that all necessary information is included, adhering to best practices in clinical record-keeping and providing you peace of mind.
- AI Suggestions: Utilizing historical data, the AI component proposes pertinent codes and notes, further improving the efficiency and precision of your records.
With 83% of doctors believing that AI can by reducing administrative burdens, the CosmaNeura Note Template stands out as a vital tool for contemporary healthcare practices. By using a soap note template nurse practitioner to streamline documentation, it not only enhances operational efficiency but also fosters a more patient-centered approach to care. We invite you to explore how this tool can support you in your daily practice and elevate the care you provide.
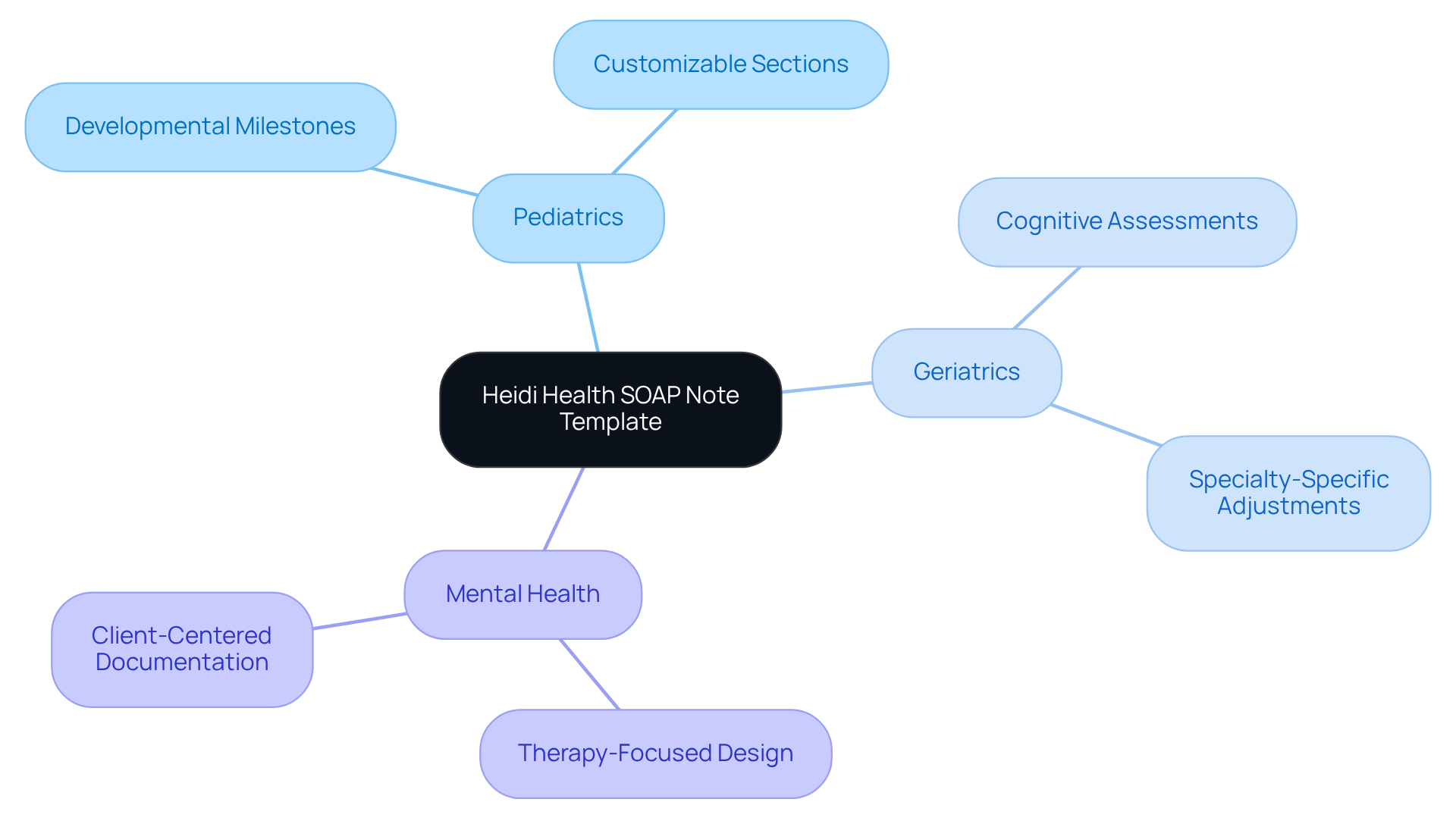
Heidi Health SOAP Note Template: Versatile Examples for Every Specialty
The Heidi Health soap note template nurse practitioner offers a compassionate framework that can be adapted to meet the diverse needs of various medical specialties, such as pediatrics, geriatrics, and mental health. Each part of the template is thoughtfully crafted to capture the unique aspects of client interactions that matter most in different fields. For instance, the Subjective section may include developmental milestones for children or cognitive assessments for elderly individuals. This level of flexibility not only facilitates comprehensive and relevant records using the soap note template nurse practitioner but also significantly enhances the provided to individuals.
The soap note template nurse practitioner features customizable sections that allow for adjustments to align with specialty-specific needs, ensuring that all vital information is captured, thus reducing administrative burdens for healthcare providers.
- Comprehensive Examples: It features examples tailored to various demographic groups, assisting healthcare providers in effectively documenting a range of clinical scenarios with a soap note template nurse practitioner, which is essential for improving efficiency and accessibility in care.
- Enhanced Relevance: By ensuring that records are closely tied to the individual's condition, the soap note template nurse practitioner enhances better clinical decision-making and outcomes. As Dr. Lawrence L. Weed emphasized, "this record cannot be separated from the concern for that individual," underscoring the importance of detailed records in healthcare.
- Impact on Patient Care: The use of a soap note template nurse practitioner is essential for specialty-specific documentation, enabling the delivery of personalized care that meets the unique needs of patient populations, ultimately leading to improved health outcomes. Statistics reveal that utilizing organized templates, specifically the soap note template nurse practitioner, can elevate compliance rates to 95%, showcasing the effectiveness of the Heidi Health Note Template in enhancing patient-centered care and streamlining administrative processes.
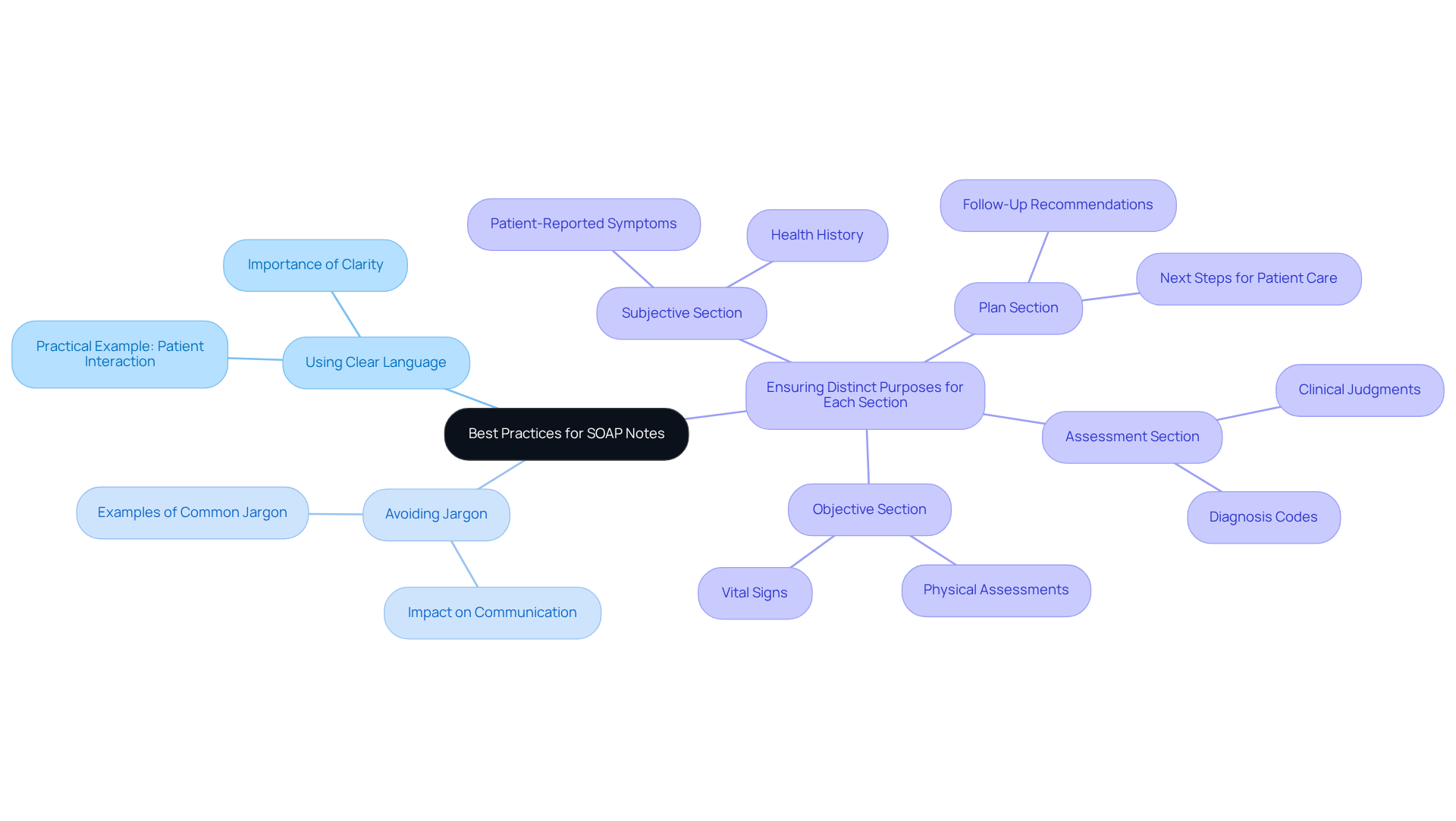
Nurse.org SOAP Note Guide: Best Practices and Practical Examples
The Nurse.org guide for clinical documentation compassionately outlines best practices for writing effective notes, focusing on clarity, conciseness, and relevance. Have you ever felt overwhelmed by the demands of documentation? This guide offers key recommendations for the soap note template nurse practitioner, such as:
- Using clear language
- Avoiding jargon
- Ensuring that each section serves a distinct purpose
Practical examples illustrate how to document various patient scenarios, utilizing a soap note template nurse practitioner, which helps them understand how to apply these principles in real-world situations. By enhancing documentation skills, you can improve patient-provider communication, ultimately leading to better care for those you serve. This guide stands as a , inviting you to engage with its insights and support your journey in providing compassionate care.
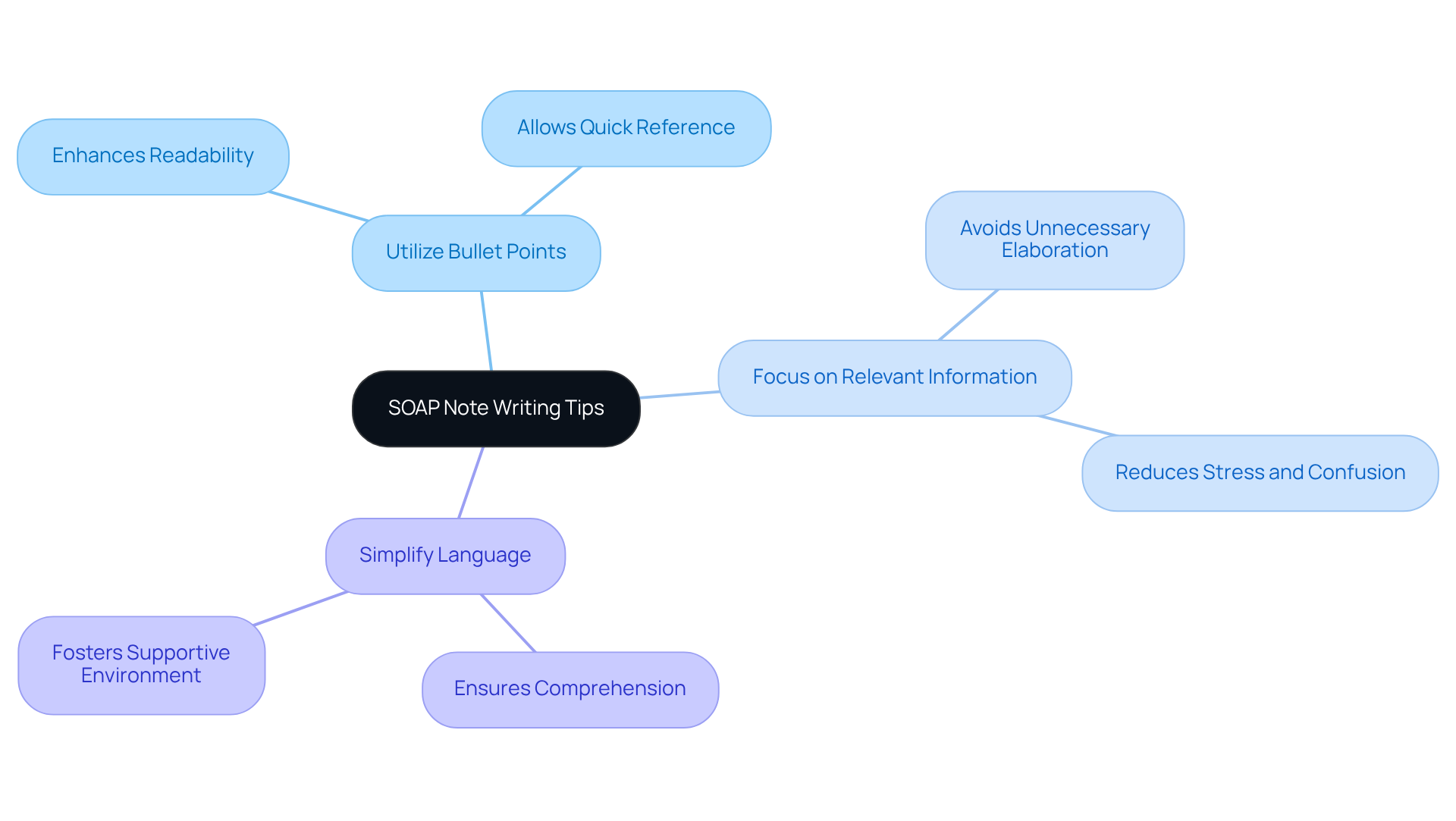
NP Charting School SOAP Note Writing Tips: Clarity and Conciseness
The NP Charting School offers vital strategies for crafting effective SOAP notes that prioritize clarity and conciseness, addressing the emotional challenges healthcare providers often face:
- Utilize Bullet Points: This format enhances readability and allows for quick reference, making it easier for busy professionals to find the information they need.
- Focus on Relevant Information: Including only the most pertinent details that directly impact patient care helps avoid unnecessary elaboration, reducing stress and confusion.
- Simplify Language: Using accessible terminology ensures that all healthcare team members can easily comprehend the documentation, fostering a supportive environment.
Incorporating these strategies is crucial, especially considering that studies have shown the variability of FK scores decreased overall after the EHR transition, indicating improved readability in clinical documentation. By applying these methods, nurse practitioners can create documentation using a soap note template nurse practitioner that is not only informative but also enhances understanding among other healthcare providers. This practice significantly boosts collaboration and ensures effective coordination of patient care. As Dr. Lawrence Weed pointed out, "Structured records offer a systematic approach for documenting client details clearly and succinctly in mental health counseling." This historical context emphasizes the , reminding us of the profound impact our documentation can have on patient outcomes.
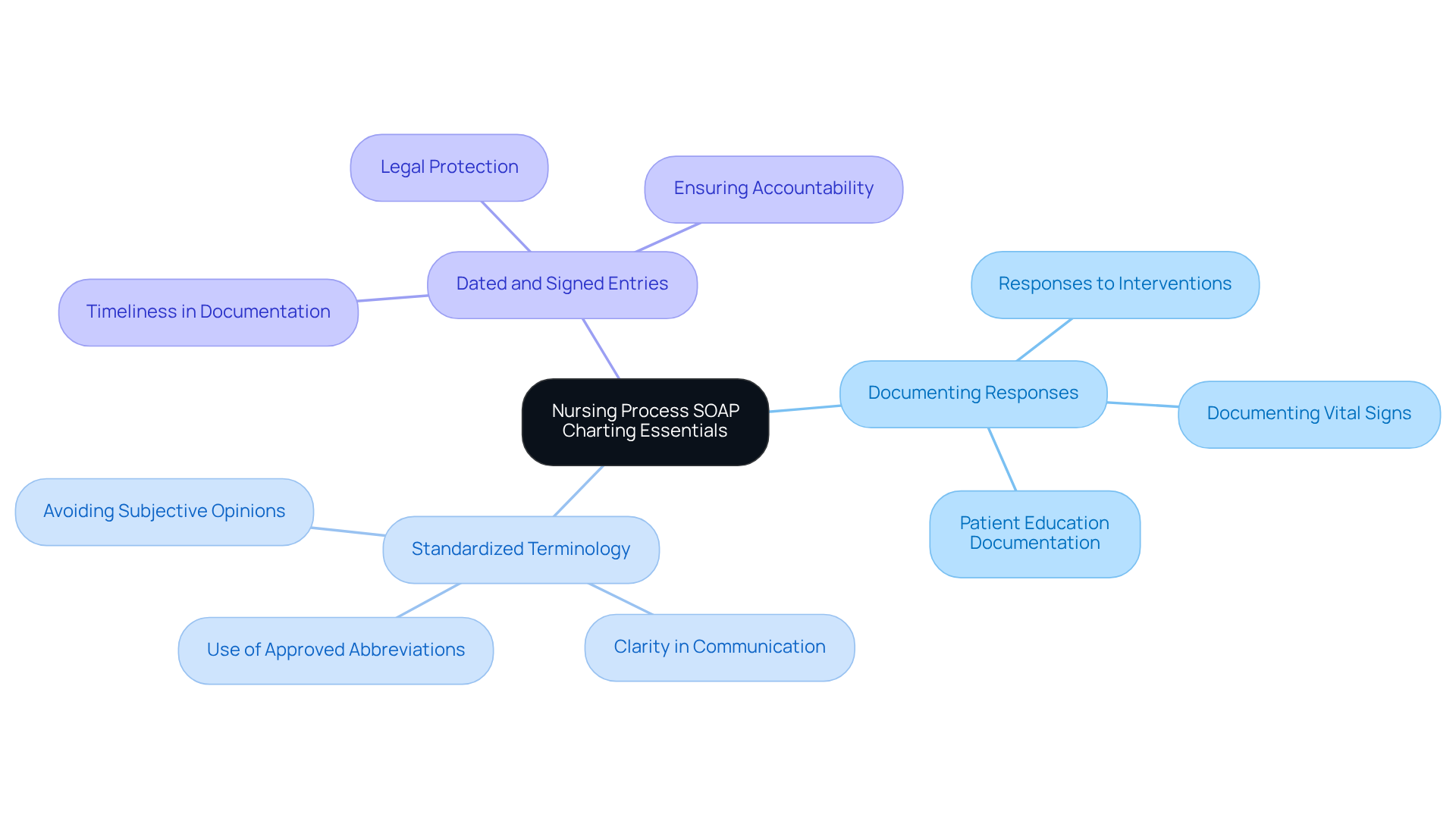
Nursing Process SOAP Charting Essentials: Accurate Documentation Guidelines
Accurate documentation is not just a task; it’s a vital part of nurturing effective nursing practice. The Nursing Process provide compassionate guidelines to help ensure that the soap note template nurse practitioner is both comprehensive and precise.
Have you ever felt overwhelmed by the administrative demands of your role? Key elements of this practice include:
- Documenting responses to interventions
- Using standardized terminology
- Ensuring that all entries are dated and signed
By embracing these practices, you not only enhance the quality of care you provide but also protect yourself legally, creating a clear record of patient interactions. Remember, each note you take is a step towards better patient care.
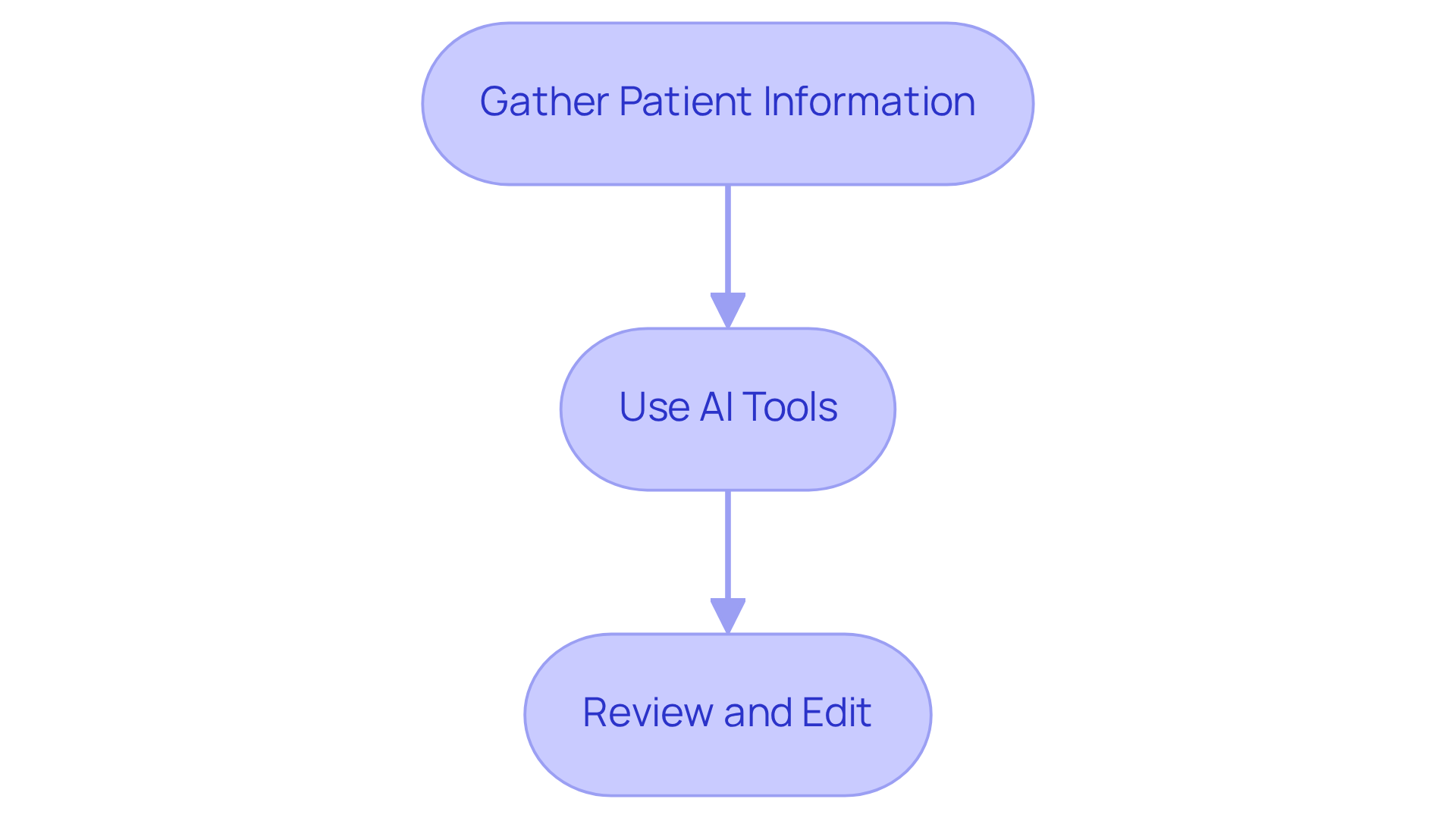
SoapNoteAI Step-by-Step SOAP Note Writing Guide: Enhance Your Skills
The SoapNoteAI Step-by-Step Writing Guide offers a compassionate approach to creating clinical documentation, empowering healthcare professionals with AI tools. This guide serves as a supportive resource, helping practitioners navigate each part of the SOAP document with the use of a while providing practical advice for efficient data entry and analysis. By embracing this guide, healthcare providers can significantly improve their record-keeping abilities with the use of a soap note template nurse practitioner, ensuring that their documentation is both accurate and aligned with the unique needs of their patients and treatment goals.
- Step 1: Gather Patient Information: Before you begin, take a moment to collect all relevant data. This preparation ensures that you can report thoroughly and with confidence.
- Step 2: Use AI Tools: Leverage AI for streamlined data entry and receive coding suggestions that enhance billing accuracy. It's inspiring to note that practices utilizing AI medical scribes have reported a remarkable 30% increase in revenue, underscoring the financial benefits of integrating these tools into your workflow.
- Step 3: Review and Edit: Prior to finalizing your documentation, conduct a careful review to confirm both accuracy and clarity. This step is vital in minimizing errors and omissions. As Dr. Claire Dave wisely notes, "Effective documentation is essential in healthcare for delivering high-quality care to individuals." Strive to finalize your documentation within 24 hours of client interactions to maintain precision and relevance.
By following these steps, you not only enhance your documentation skills but also contribute to better patient care. How can you integrate these practices into your daily routine to make a meaningful difference?
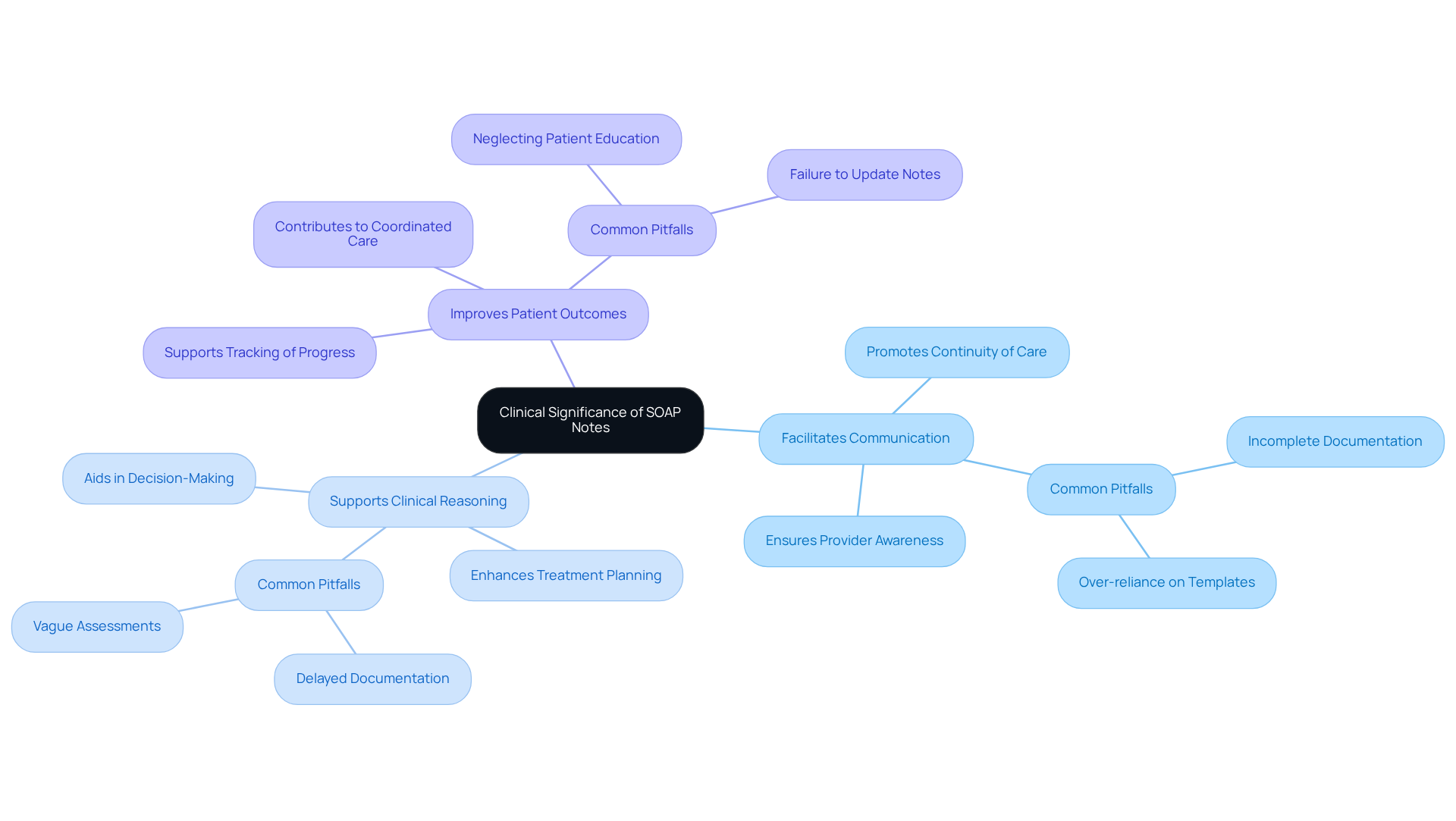
NCBI Clinical Significance of SOAP Notes: Foundation for Effective Care
The NCBI highlights the clinical importance of structured documentation as a vital resource for efficient healthcare. This documentation not only aids effective communication among healthcare professionals but also ensures that every team member is aware of an individual's condition and treatment strategy. By adopting an organized record-keeping approach, clinical reasoning and decision-making are enhanced, ultimately leading to improved patient outcomes. Recognizing the significance of clinical records empowers healthcare professionals to refine their record-keeping methods, contributing to the delivery of superior care.
However, it is essential to recognize that incomplete or erroneous records can cause misunderstandings and lead to inappropriate treatment. To enhance the , providers should avoid common pitfalls such as over-reliance on templates and delays in recording. Maintaining clarity and precision in each section is crucial, as emphasized by Vivian Chung Easton, to ensure that the information remains understandable and actionable for all healthcare professionals involved. Moreover, the adaptability of clinical documentation allows it to be effectively utilized across various therapeutic environments, further underscoring its importance in providing holistic care for individuals.
- Facilitates Communication: Ensures all providers are informed about patient status.
- Supports Clinical Reasoning: Aids in decision-making and treatment planning.
- Improves Patient Outcomes: Contributes to coordinated and effective care.
Nursing Process Common SOAP Note Examples: Practical Applications
Efficient documentation is essential for ensuring high-quality care for individuals. As healthcare professionals, we understand the emotional challenges that come with managing patient information. Typical , such as the soap note template nurse practitioner, provide a practical structure that can alleviate some of these burdens, helping you capture essential information accurately across various scenarios.
- Routine Check-Up: When documenting vital signs, individual complaints, and follow-up plans, remember that each detail matters. For example, during a routine check-up, you might record a pulse of 74 beats per minute, a temperature of 36.7 degrees Celsius, and a weight of 174 lbs 8 oz. In the subjective section, an individual may report feeling well, while the assessment could highlight any necessary follow-up tests. How can this structured approach help you feel more confident in your notes?
- Chronic Condition Management: Managing chronic conditions requires capturing ongoing treatment responses and adjustments. For instance, if an individual with diabetes reports fluctuations in blood sugar levels, it’s crucial to review their medication regimen in the plan section. This reflection not only aids in better care but also fosters a deeper connection with your patients.
- Acute Care Situations: In acute care scenarios, detailing immediate interventions and individual reactions is critical. For example, if someone presents with acute pain after an injury, documenting their pain level and any immediate treatments provided, such as pain relief measures, can make a significant difference. Are you equipped to handle these urgent situations with clarity?
By examining these examples, practitioners can gain insights into best practices for utilizing a soap note template nurse practitioner to record routine check-ups and other scenarios involving individuals. This ultimately enhances your record-keeping skills and improves outcomes. Remember, appropriate documentation through structured notes not only reduces mistakes but also promotes effective communication among healthcare providers. Together, we can ensure that care is both comprehensive and coordinated, fostering an environment where patients feel supported and understood.

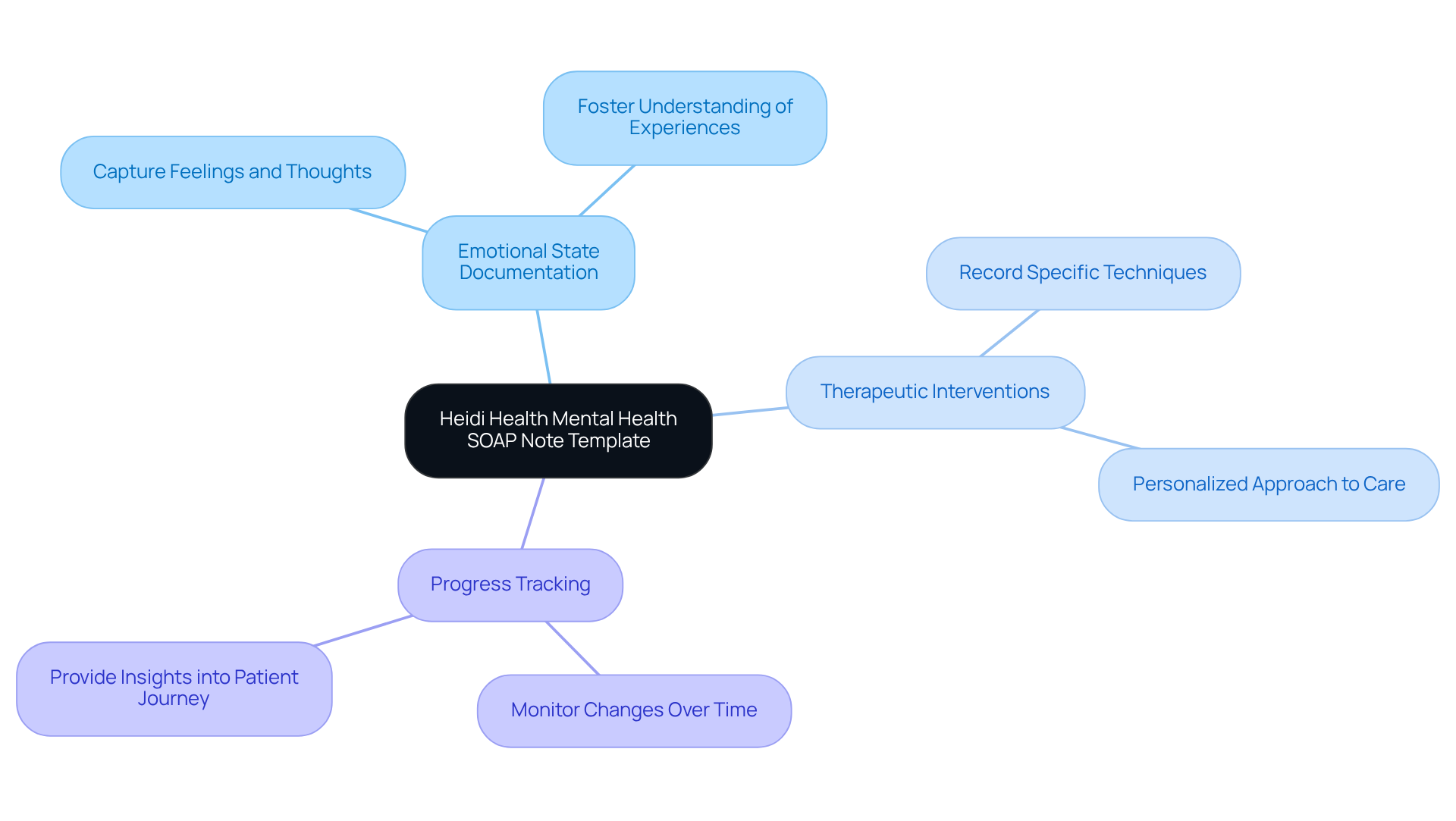
Heidi Health Mental Health SOAP Note Template: Tailored for Practitioners
The Heidi Health Mental Health SOAP Note Template is thoughtfully crafted for mental health practitioners, focusing on the unique challenges of mental health assessments and interventions. This template provides essential sections for documenting emotional states, therapeutic interventions, and over time. By utilizing this tailored approach, mental health providers can ensure that their documentation truly reflects the complexities of mental health care, ultimately enhancing treatment outcomes.
- Emotional State Documentation: Capture the feelings and thoughts of your patients, fostering a deeper understanding of their experiences.
- Therapeutic Interventions: Record the specific techniques employed during sessions, allowing for a more personalized approach to care.
- Progress Tracking: Monitor changes in individual status over time, providing valuable insights into their journey.
By recognizing the emotional challenges faced by healthcare providers and addressing the administrative burdens that can impact patient care, this template serves as a supportive tool. It encourages mental health professionals to engage with their documentation in a way that prioritizes patient well-being, ultimately leading to more effective treatment outcomes.
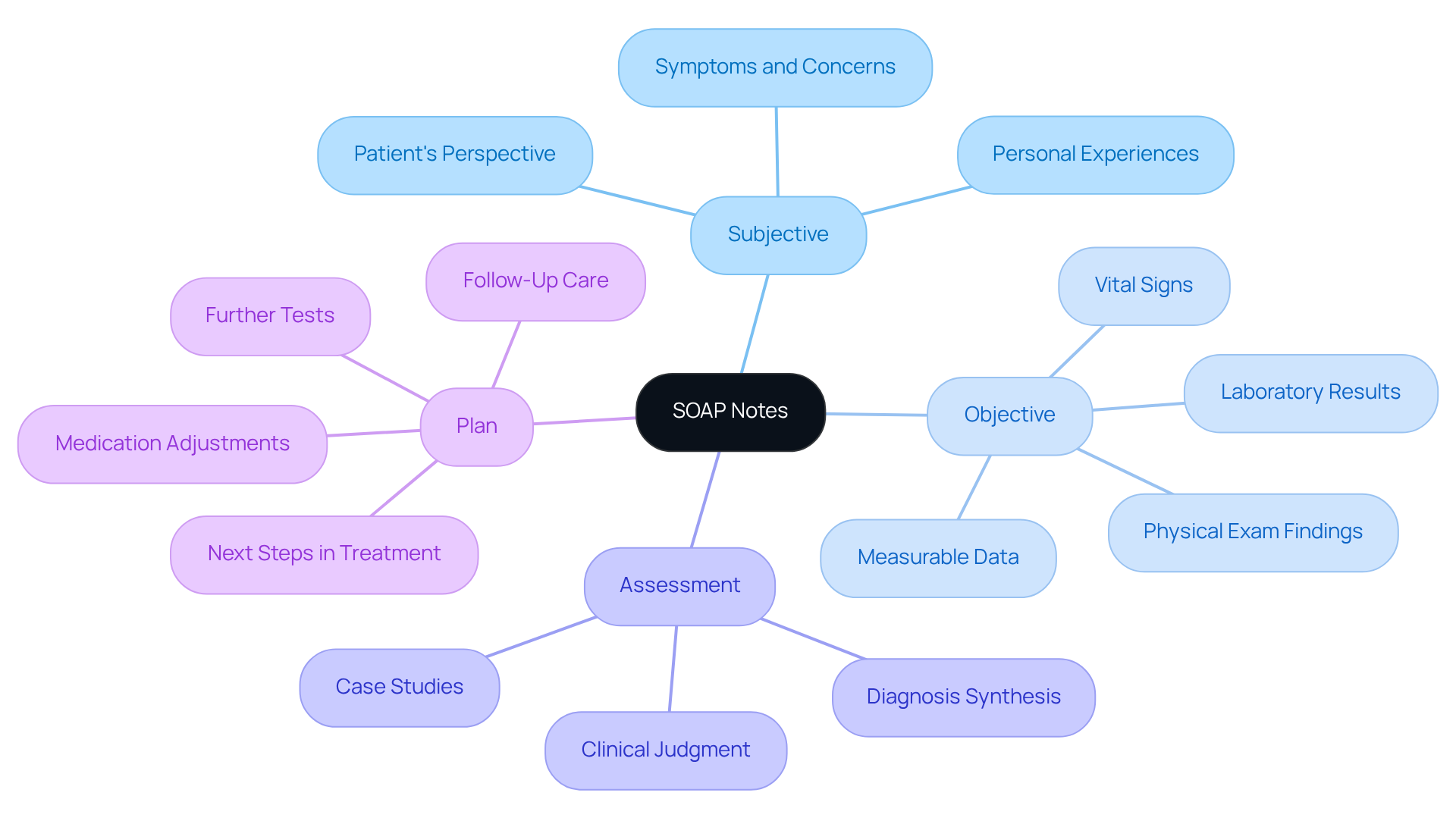
Nursing Process Components of SOAP Notes: Understanding Each Section
Understanding the [components of the soap note template nurse practitioner](https://sigmamd.com/blog/soap-notes) is vital for effective documentation in healthcare. Each section—Subjective, Objective, Assessment, and Plan—plays a crucial role in enhancing patient care and communication among providers.
- Subjective: This section captures the patient's perspective, detailing symptoms, concerns, and personal experiences. It is essential for understanding the individual's narrative and context, which informs clinical reasoning. As highlighted by HealthOrbit AI, "When documentation is applied consistently, care teams can swiftly comprehend the individual's condition, what has been attempted, and what is scheduled next."
- Objective: Here, measurable data is documented, including vital signs, physical exam findings, and laboratory results. This factual information offers a solid basis for clinical evaluations and aids in monitoring the individual's condition over time. Well-written serve as essential legal documents for audits, billing checks, or legal reviews.
- Assessment: This component synthesizes the subjective and objective data to arrive at a diagnosis. It reflects the clinician's interpretation and clinical judgment, guiding the subsequent treatment plan. A case study involving Mr. Johnson's hypertension management demonstrates how each section contributes to care and decision-making.
- Plan: The Plan outlines the next steps in treatment, including further tests, medication adjustments, and follow-up care. It ensures that both the clinician and individual are aligned on the care strategy moving forward.
By mastering each component of a soap note template nurse practitioner, healthcare providers can significantly enhance their documentation practices. Statistics show that structured documentation offers a systematic approach for clinical reasoning, assisting healthcare professionals in evaluating, diagnosing, and managing individuals effectively. Well-structured SOAP notes not only improve communication among care teams but also serve as essential legal documents, ensuring clarity and continuity in patient care.
How can you ensure that your documentation practices are as effective as possible? By embracing the SOAP format, you can alleviate some of the administrative burdens and focus more on what truly matters—providing compassionate care to your patients.
Conclusion
The utilization of SOAP note templates is essential for nurse practitioners who are striving to enhance their documentation processes and improve patient care. Have you ever felt overwhelmed by the administrative tasks that take time away from your patients? By embracing structured documentation, healthcare providers can streamline their record-keeping, reduce errors, and dedicate more time to delivering compassionate care.
Throughout the article, we've explored various SOAP note templates, each showcasing unique features and benefits. From the innovative CosmaNeura template that harnesses AI for efficiency, to the versatile Heidi Health template tailored for diverse specialties, these options provide valuable tools to enhance clinical documentation. Best practices for writing effective SOAP notes, such as clarity and conciseness, have been highlighted, offering practical insights for healthcare professionals.
Ultimately, adopting these templates is not just about compliance; it cultivates a culture of effective communication and collaboration among healthcare teams. By prioritizing accurate and comprehensive documentation, practitioners can ensure that every patient receives the highest quality of care. Engaging with these resources can truly make a meaningful difference in your daily practice, empowering nurse practitioners to navigate the complexities of patient care with confidence and compassion.




