Overview
This article highlights the emotional challenges healthcare providers face in documentation and patient care. The burden of administrative tasks can often overshadow the compassionate interactions that truly matter. By providing various examples of SOAP notes, we aim to enhance patient documentation across different healthcare disciplines.
Structured documentation is not just a requirement; it’s a lifeline for improving communication and continuity of care. Imagine how effective record-keeping can transform treatment outcomes! Specific examples from mental health, occupational therapy, and speech therapy illustrate this point, showing how thoughtful documentation leads to better patient management and support.
We invite you to reflect on your own experiences: How can improved documentation ease your daily challenges? By embracing these practices, you can foster a nurturing environment that prioritizes patient well-being. Let’s work together to enhance our documentation practices, ensuring that every patient receives the care they truly deserve.
Introduction
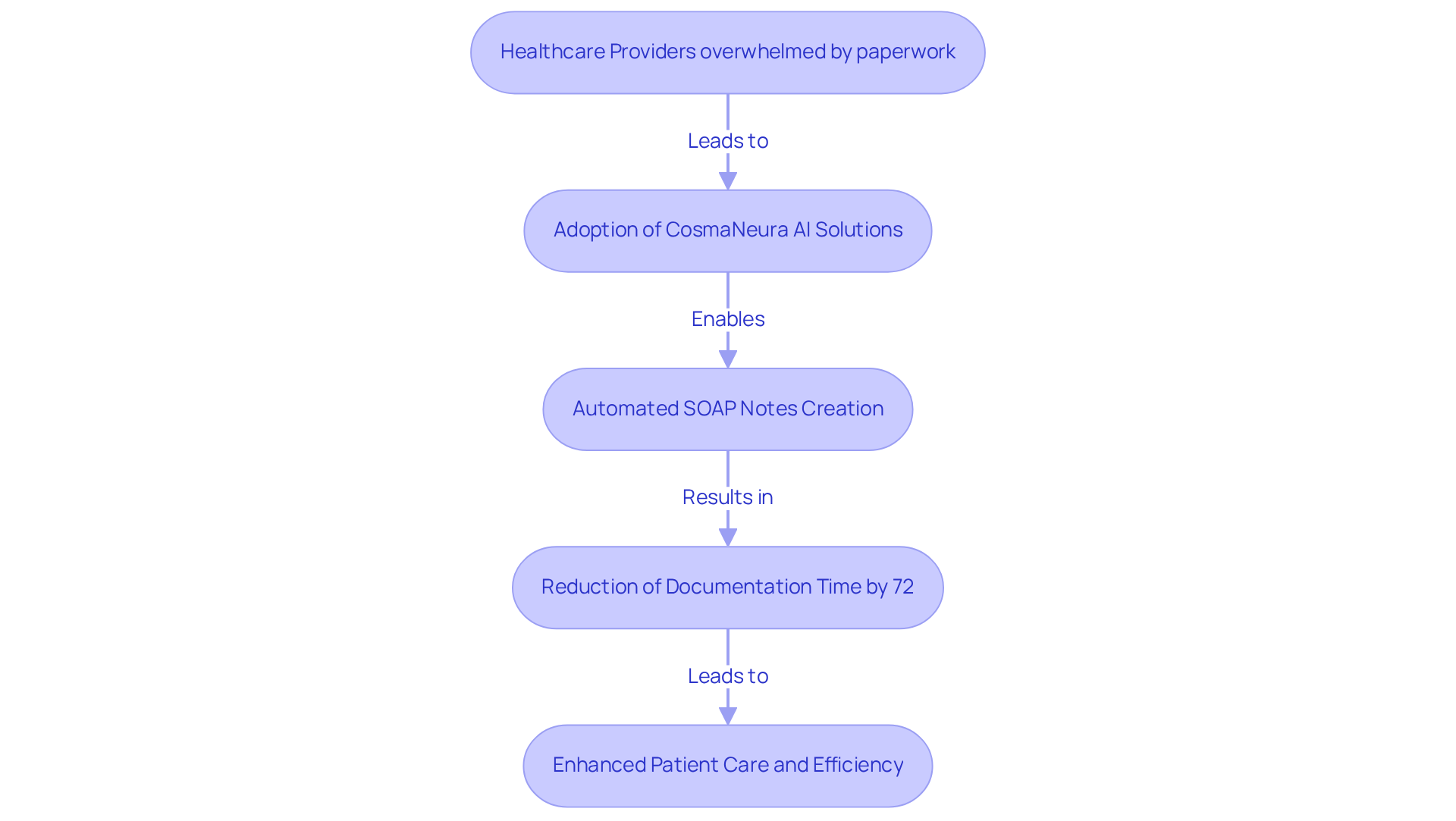
In the intricate landscape of healthcare, effective documentation is paramount. Yet, many providers feel overwhelmed by the demands of paperwork. This emotional burden can detract from the quality of care they provide. The integration of SOAP notes has emerged as a vital tool for streamlining patient interactions and enhancing care quality across various specialties.
Imagine a world where documentation becomes less of a chore and more of a streamlined process. This article presents ten compelling examples of SOAP notes that illustrate best practices and highlight the transformative potential of AI-powered solutions like CosmaNeura. These tools can alleviate administrative burdens, allowing healthcare professionals to focus more on what truly matters: their patients.
How can you, as a healthcare provider, leverage these insights to improve patient outcomes while navigating the complexities of documentation? Let's explore the possibilities together.
CosmaNeura: AI-Powered SOAP Note Automation for Healthcare Providers
In today's demanding healthcare environment, many providers face overwhelming administrative burdens that can detract from their ability to deliver compassionate care. CosmaNeura understands these challenges and harnesses cutting-edge AI technology to automate the creation of soap notes examples. This innovation significantly reduces the time healthcare providers spend on documentation, allowing them to focus more on supporting their clients.
Imagine having more time to connect with patients rather than being bogged down by paperwork. By seamlessly incorporating user data and clinical insights, CosmaNeura guarantees that notes are not only accurate but also tailored to each individual's specific needs. With nearly 41% of healthcare professionals reporting that they , this automation is essential for enhancing the quality of care.
The AI tools offered by CosmaNeura streamline charting processes and reduce time spent on record-keeping by an impressive 72%. This means healthcare providers can enhance their clinical experiences while upholding ethical standards. In a time when rising healthcare expenses weigh heavily on both individuals and providers, CosmaNeura's solutions not only boost operational efficiency but also help alleviate financial stress, ensuring that quality services remain accessible.
As the healthcare sector evolves, the integration of AI in documentation processes is set to transform both efficiency and care quality. By embracing this essential resource, primary care providers can navigate the complexities of their roles with greater ease and compassion. Are you ready to explore how CosmaNeura can support you in delivering the best care possible?
Mental Health SOAP Note Example: Documenting Patient Interactions Effectively
Mental Health SOAP Note Example: Documenting Patient Interactions Effectively
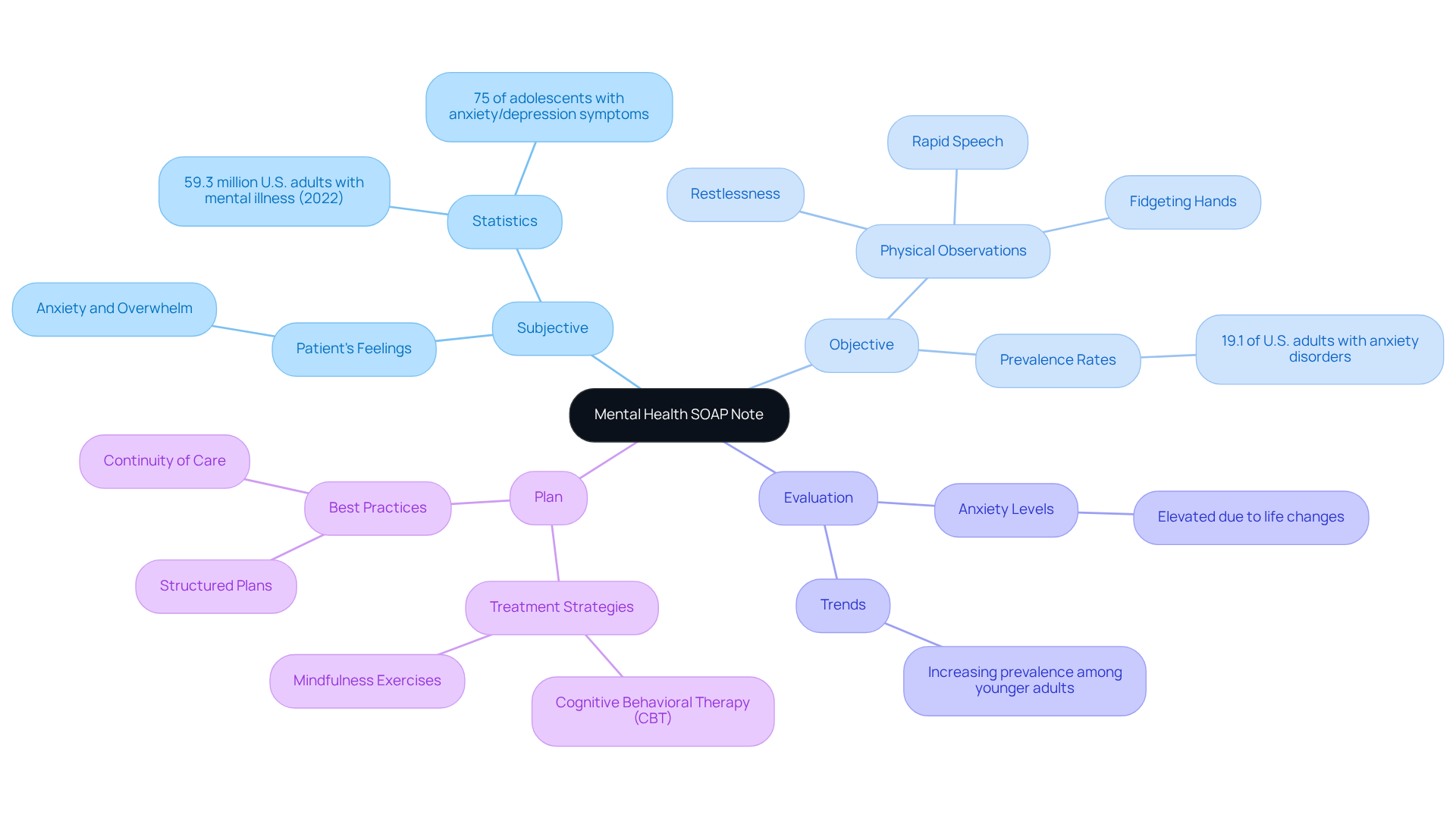
Subjective: The patient shares feelings of anxiety and being overwhelmed, expressing, 'I can't seem to manage my stress.' This statement reflects the emotional burden many individuals carry, especially in light of the rising mental health issues. In 2022, approximately 59.3 million U.S. adults experienced some form of mental illness, underscoring the importance of understanding these struggles.
Objective: Observations indicate that the individual appears restless, with a rapid speech pattern and fidgeting hands. These physical manifestations are common indicators of , affecting nearly 19.1% of U.S. adults each year. Recognizing these signs is crucial in providing compassionate care.
Evaluation: The individual's anxiety levels are assessed as elevated, likely intensified by recent life changes. Current trends reveal that mental health challenges are increasingly prevalent, particularly among younger adults. Alarmingly, nearly 75% of adolescents screen positive for moderate to severe anxiety or depression symptoms, highlighting the urgent need for support.
The treatment plan, which serves as soap notes examples, includes continuing cognitive behavioral therapy sessions on a weekly basis and introducing mindfulness exercises to help manage anxiety. This approach reflects best practices in mental health documentation by incorporating soap notes examples that emphasize the importance of structured plans addressing both immediate and long-term needs. By documenting these interactions effectively, healthcare providers can foster continuity of care and enhance outcomes for those they serve.
How can we further support our patients in navigating these challenges? Let's work together to ensure they feel heard and understood.
Occupational Therapy SOAP Note Example: Capturing Client Progress and Needs
Example of an Occupational Therapy SOAP Note:
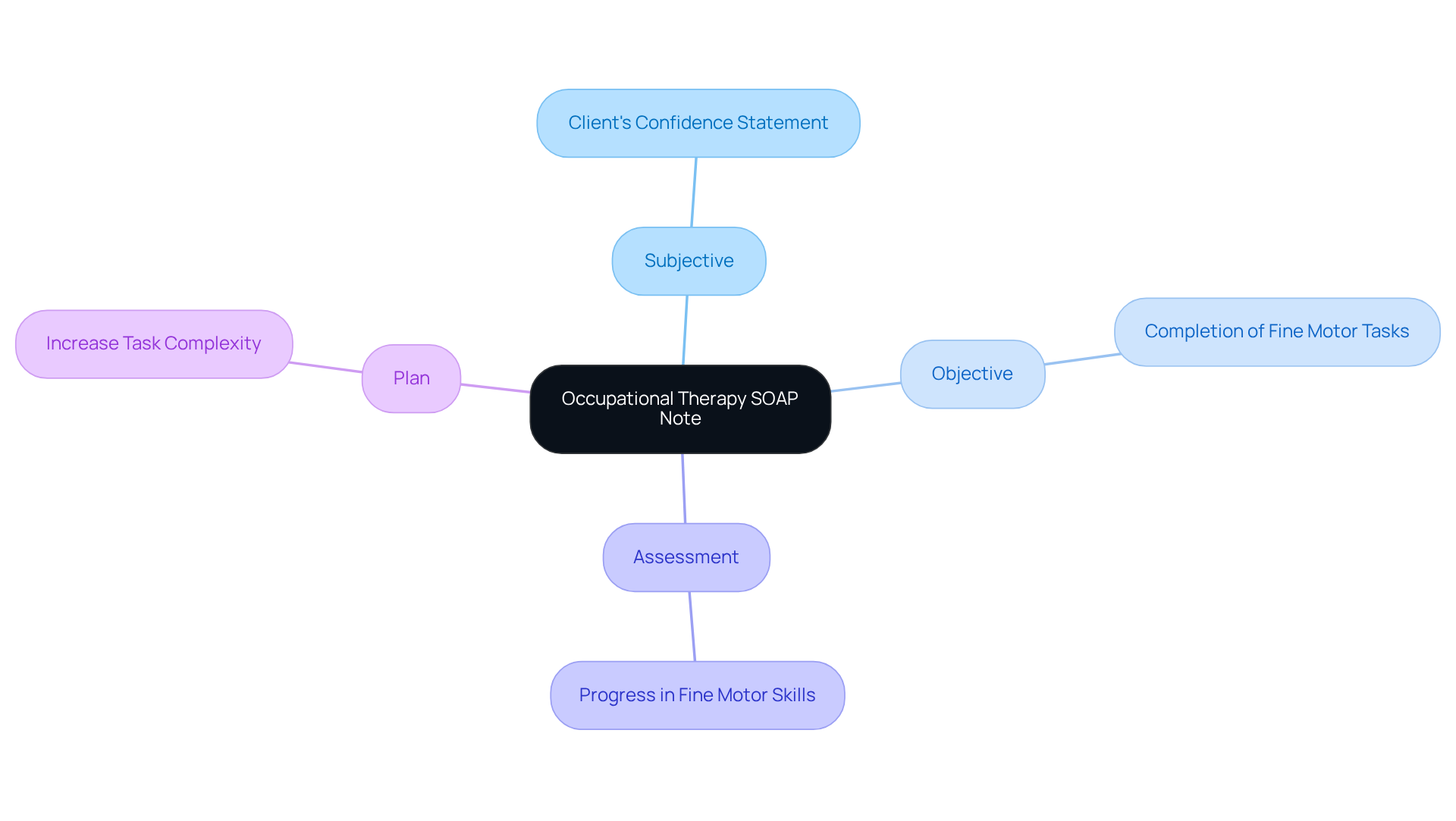
- Subjective: The client shares, 'I feel more confident using my left hand for daily tasks.' This statement highlights a significant in their journey.
- Objective: The client successfully completed 10 repetitions of fine motor tasks with minimal assistance, which can be documented in soap notes examples. This achievement reflects their dedication and progress.
- Assessment: The client demonstrates improvement in fine motor skills, which is reflected in the soap notes examples, indicating a positive trajectory towards therapy goals. Such progress is truly encouraging.
- Plan: In the next session, we will increase the complexity of tasks to further challenge the client. This approach aims to foster continued growth and confidence.
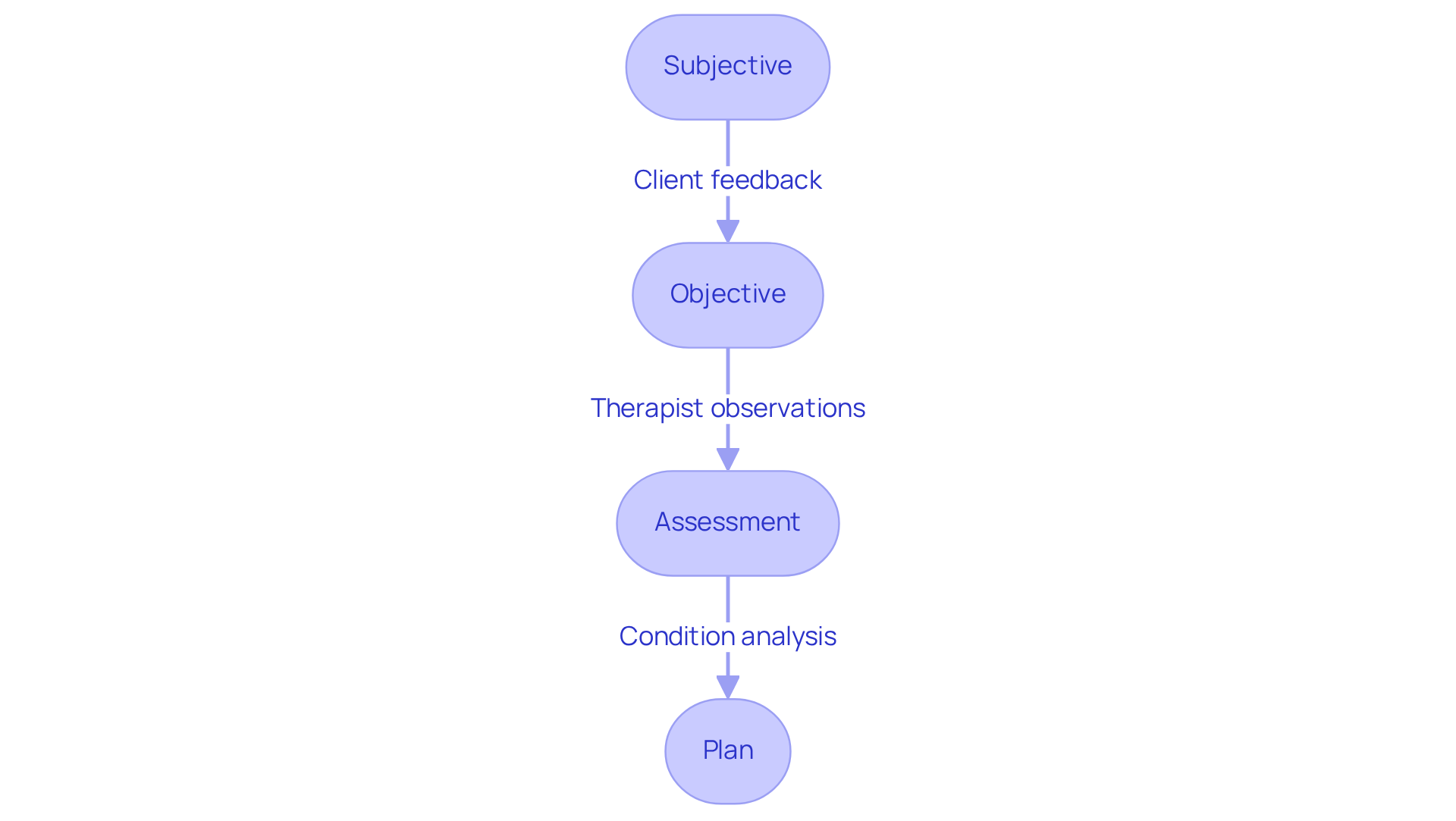
Speech Therapy SOAP Note Example: Structuring Effective Communication Records
Subjective: The patient shares, 'I feel like I'm improving, but I still struggle with certain sounds.' This statement reflects an important level of self-awareness and engagement in the therapeutic journey, which is vital for effective treatment. As noted by Patricia Prelock, Ph.D., CCC-SLP, 'Communication is not just about speaking; it’s also about listening and understanding.' This highlights the dual role of records in capturing both clinician observations and individual experiences, fostering a collaborative atmosphere.
Objective: The individual articulated 80% of target sounds correctly during practice. This measurable data is crucial for tracking progress and adjusting treatment plans accordingly. Notably, statistics reveal that 22.9% of individuals did not exhibit clinically significant progress in any domain, underscoring the importance of thorough documentation in monitoring outcomes in speech therapy.
Evaluation: The individual is making commendable progress but requires ongoing focus on specific phonemes. This analysis helps identify areas needing additional intervention, ensuring therapy remains tailored to the individual's unique needs. A case analysis on the significance of organized records, such as soap notes examples, demonstrated that well-arranged notes greatly enhance comprehension among team members, promoting improved outcomes for individuals.
Plan: Introduce targeted exercises for challenging sounds in the next session. A clearly defined plan is essential for maintaining clarity in treatment objectives and ensuring alignment between the therapist and individual on next steps. Timely record-keeping is vital; using soap notes examples immediately after therapy sessions aids in capturing details while they are fresh in the clinician's mind, reducing the risk of omitting important information.
In 2025, the emphasis on effective communication records in speech therapy continues to grow. Therapists are encouraged to document communication progress meticulously, ensuring that every session's details are captured promptly. This practice not only supports clinical decision-making but also empowers patients by keeping them informed about their progress. Progress in at least one area of Therapy Outcome Measures occurred in 77.1% of cases involving 16,356 individuals, highlighting the effectiveness of speech therapy and the significance of record-keeping in monitoring such advancements.
Including direct quotes from clients can further enrich notes, offering a vivid depiction of their journey. As highlighted in a recent case study, 'The words you struggle to say today will come more easily tomorrow—keep going.' This sentiment encapsulates the essence of speech therapy, where every small victory is worth celebrating. Additionally, the quote, 'Every time you speak, you claim your space in the world,' emphasizes the importance of communication in speech therapy.
Ultimately, in speech therapy go beyond administrative requirements; they foster a collaborative environment that prioritizes care and progress. The journey of communication is filled with steps, pauses, and breakthroughs, and as noted, 'Communication is a journey, and every small step forward is worth celebrating.
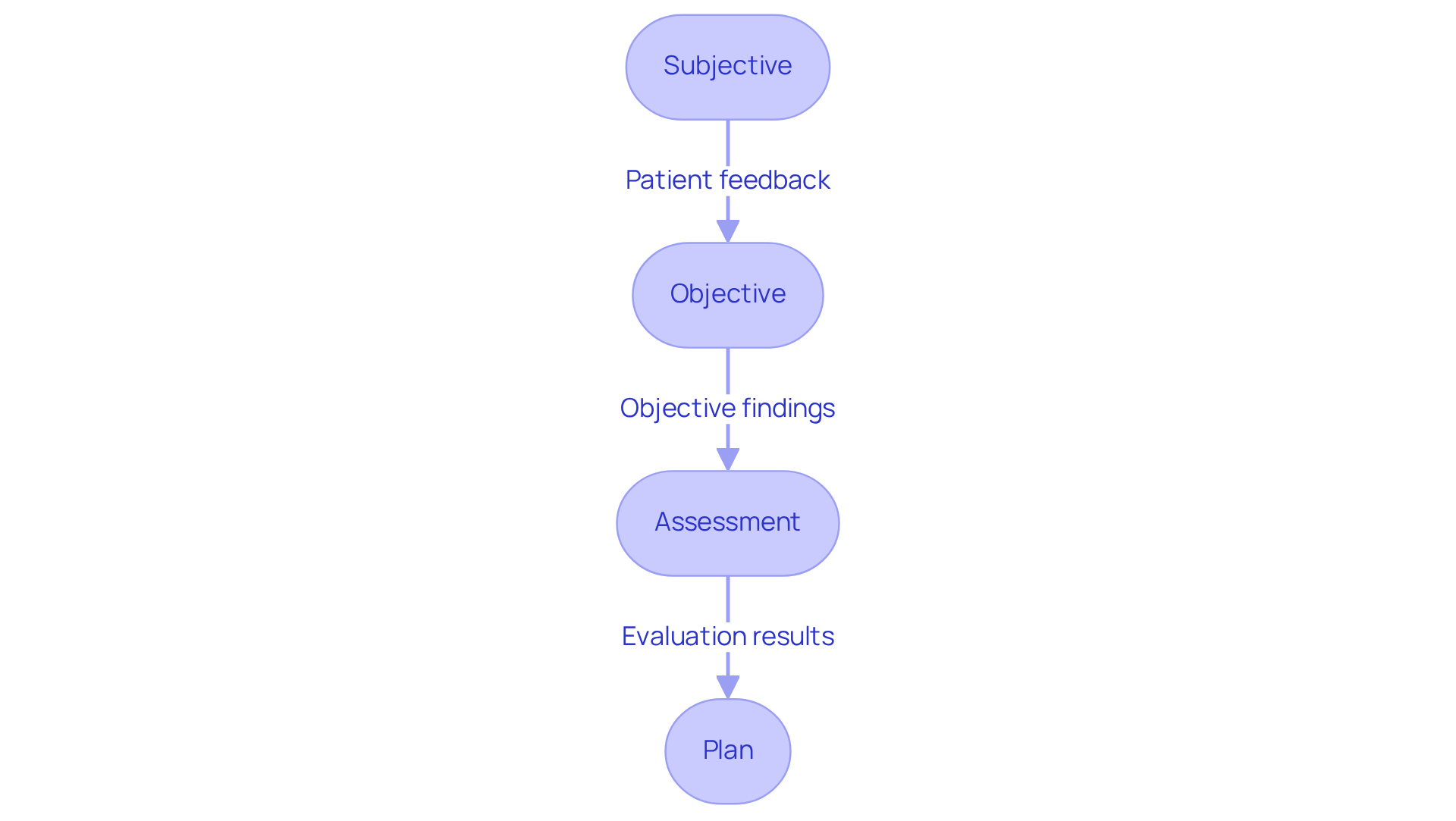
Primary Care SOAP Note Example: Comprehensive Patient Assessment
Primary Care SOAP Note Example: Comprehensive Patient Assessment
Subjective: The patient expresses feeling significant fatigue and occasional headaches, sharing, 'I haven't been sleeping well.' This heartfelt account is crucial for grasping the individual’s condition and guiding clinical decisions. By leveraging generative AI tools, such as engagement applications, physicians can enhance the collection of subjective data, fostering a deeper understanding of personal experiences.
Objective: Vital signs remain stable, and the physical examination shows no abnormalities. Recording objective data, like vital signs, is vital for a thorough assessment and assists clinicians in swiftly locating essential information. AI-driven tools can automate the documentation of these objective findings, allowing healthcare providers to focus more on patient interaction and less on administrative tasks.
Evaluation: The evaluation indicates a possible sleep disruption contributing to the individual's fatigue. This section to inform a diagnosis, which is crucial for guiding future treatment decisions. Generative AI can identify patterns in medical data, supporting physicians in making more accurate assessments and enhancing diagnostic capabilities, thereby addressing the challenges of physician burnout and administrative pressures.
Plan: It is recommended to provide sleep hygiene education and schedule a follow-up appointment in two weeks. A well-defined treatment strategy ensures continuity of support and directs the future management of patients. By utilizing AI-driven scheduling systems, physicians can streamline appointment management, alleviating administrative burdens and enhancing patient engagement.
In primary care, effectively documenting patient fatigue and sleep issues is essential, as highlighted in various [soap notes examples](https://herzing.edu/blog/write-it-right-soap-notes-back-your-practice). These soap notes examples not only facilitate clear communication among healthcare professionals but also assist with legal and billing responsibilities. The structure of these notes was proposed by Larry Weed nearly 50 years ago, underscoring its significance in clinical practice. Additionally, under the 2021 Cures Rule, all U.S. hospitals and clinicians must ensure clinical notes are accessible to patients, fostering transparency and empowering individuals. As Imran Shaikh emphasizes, maintaining accurate clinical records, including structured notes, is vital for a successful healthcare practice. Furthermore, documentation supports billing codes and clarifies the complexity of appointments, highlighting their financial implications. As healthcare evolves, upholding high standards in record-keeping practices is crucial for delivering safe, high-quality care. Regular evaluations of record-keeping methods are necessary to stay aligned with optimal procedures and regulatory standards.
Massage Therapy SOAP Note Example: Recording Treatment Sessions Accurately
Massage Therapy SOAP Note Example: Recording Treatment Sessions Accurately
Subjective: The client shares, 'I feel tightness in my shoulders and neck.' This personal insight is essential, reflecting the client's experience and concerns, which guides the therapist's focus with empathy.
Objective: Notable tension is observed in the upper trapezius and levator scapulae muscles. Documenting these objective findings is vital for establishing a baseline and tracking progress over time, ensuring the client feels understood.
Assessment: The assessment reveals that muscle tension likely contributes to the client's discomfort. This thoughtful analysis aids in formulating a targeted treatment plan that addresses the client's needs.
Plan: The plan is to continue with deep tissue techniques and reassess in the next session. Clear planning fosters alignment between the therapist and client on treatment goals, nurturing a supportive environment.
Effective record-keeping in massage therapy transcends mere regulatory requirements; it enhances communication between practitioners and clients. As Jeff Levin, a respected expert in the field, emphasizes, 'Licensed massage therapists ought to be respected as mainstream practitioners, whose profession provides a therapeutic approach not just to address pain and functional challenges, but to foster wellness and overall wellbeing.' This underscores the importance of comprehensive records in promoting a holistic approach to patient support.
In 2025, the accuracy of recording treatment sessions is more critical than ever. With the , expected to expand by 18% from 2023 to 2033, proper record-keeping can significantly enhance client outcomes and satisfaction. Notably, 88% of study participants reported massage as beneficial to their overall health and wellness. By utilizing soap notes examples, therapists can ensure they capture essential details of each session, which facilitates better continuity of care and strengthens the therapeutic relationship.
Integrating efficient record-keeping methods into your massage therapy routine not only aids in compliance but also promotes a culture of professionalism and responsibility. Furthermore, adopting improved record-keeping methods can lead to substantial financial savings, with potential decreases of $7,000 annually in software and payment processing expenses. As the industry evolves, staying informed about best practices in documentation will be key to thriving in a competitive market.
Consider how these practices can enhance your approach to care. By prioritizing accurate record-keeping, you not only support your clients but also foster a more fulfilling and effective therapeutic practice.
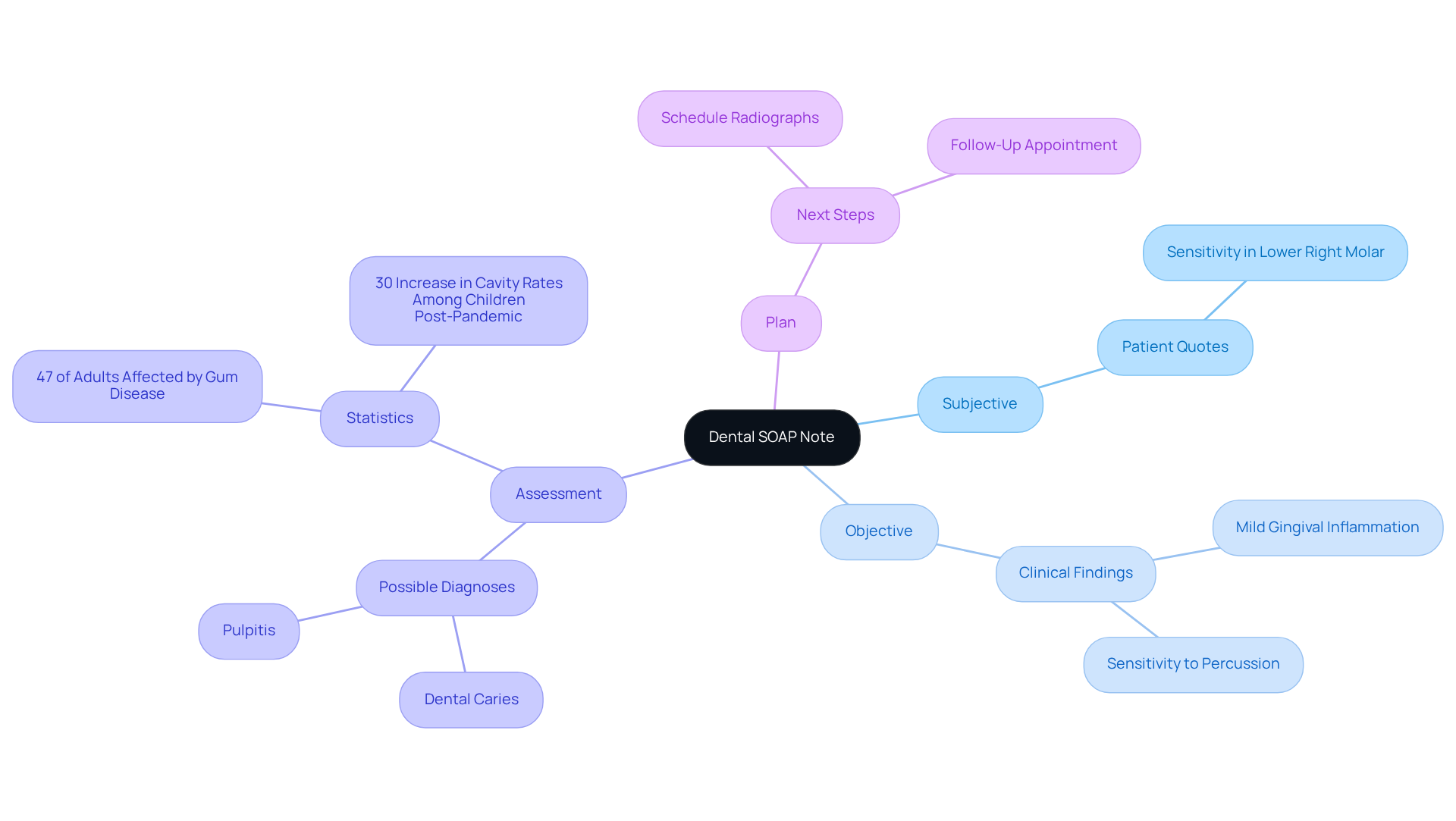
Dental SOAP Note Example: Documenting Oral Health Assessments
Dental SOAP Note Example: Documenting Oral Health Assessments
Subjective: The patient shares, 'I have been experiencing sensitivity in my lower right molar.' This heartfelt input is essential, as it reflects the patient's personal experience and concerns, guiding the assessment process with compassion.
Objective: A clinical examination reveals mild gingival inflammation and sensitivity to percussion. Documenting these objective findings is vital for establishing a baseline and supporting the diagnosis, ensuring we address the patient’s needs effectively.
Assessment: The findings suggest possible dental caries or pulpitis, indicating the need for further investigation. Accurate assessments are crucial, as they inform treatment decisions and ensure continuity of care. It's significant to note that gum disease impacts 47% of adults over 30, underscoring the commonality of dental issues that require thorough records.
Plan: Schedule radiographs and a follow-up appointment for treatment. A well-defined plan is essential for effective management of individuals, demonstrating our commitment to addressing their needs.
Efficient record-keeping methods in dentistry are fundamental. Precise examples of SOAP notes not only facilitate communication among healthcare professionals but also enhance safety and quality of treatment. For instance, consider that nearly 40% of adults skipped dental visits during the pandemic, leading to a 30% increase in cavity rates among children. This highlights the necessity for and treatment results, especially during times of interrupted services.
Dental professionals emphasize the importance of accurately documenting oral health assessments. As one specialist noted, 'Thorough records are the foundation of efficient care for individuals.' Furthermore, as highlighted by Humble Memorial Dental, 'Oral health plays a critical role in overall health.' By adhering to best practices in documentation, we can ensure that we meet both clinical and ethical standards, ultimately enhancing outcomes for our patients.
Physiotherapy SOAP Note Example: Tracking Patient Recovery Progress
Physiotherapy SOAP Note Example: Tracking Patient Recovery Progress
Subjective: The patient expresses a sense of relief, stating, 'I can walk longer distances without pain now.' This positive feedback is not just words; it reflects a significant shift in their journey toward recovery. Understanding these personal experiences is essential as they highlight the emotional challenges faced by individuals on this path.
Objective: Observations reveal an enhanced range of motion in the affected joint, measurable through specific assessments. Using to document these objective findings is crucial for establishing a baseline and tracking progress over time. This attention to detail reassures patients that their recovery is being closely monitored and supported.
Assessment: Notable progress suggests that the current rehabilitation plan is effective. Research indicates that maintaining efficient records can lead to improved recovery outcomes, with approximately 79% of patients reporting significant pain reduction after physical therapy. Regular evaluations are vital, as they allow for adjustments based on the individual's evolving needs, which can be documented through soap notes examples. Additionally, referencing case studies on the effectiveness of physical therapy for chronic pain underscores the importance of comprehensive documentation, including soap notes examples, in fostering recovery.
Plan: We will increase the intensity of exercises and schedule a reassessment in one month. This plan will be tailored to align with the individual's specific goals and capabilities, ensuring it remains realistic and attainable. By regularly using soap notes examples to record progress, we not only enhance clinical decision-making but also nurture patient engagement and motivation. It's noteworthy that physical therapy can reduce healthcare costs by up to 72% compared to surgical interventions, highlighting the numerous advantages of diligent record-keeping.
Incorporating insights on the importance of monitoring recovery can further emphasize the value of documentation. For example, the statement, 'Progress monitoring provides essential feedback on treatment effectiveness,' can be seamlessly integrated into the Assessment section, reinforcing how systematic documentation can lead to improved patient outcomes and satisfaction.
Pediatric SOAP Note Example: Tailoring Documentation for Young Patients
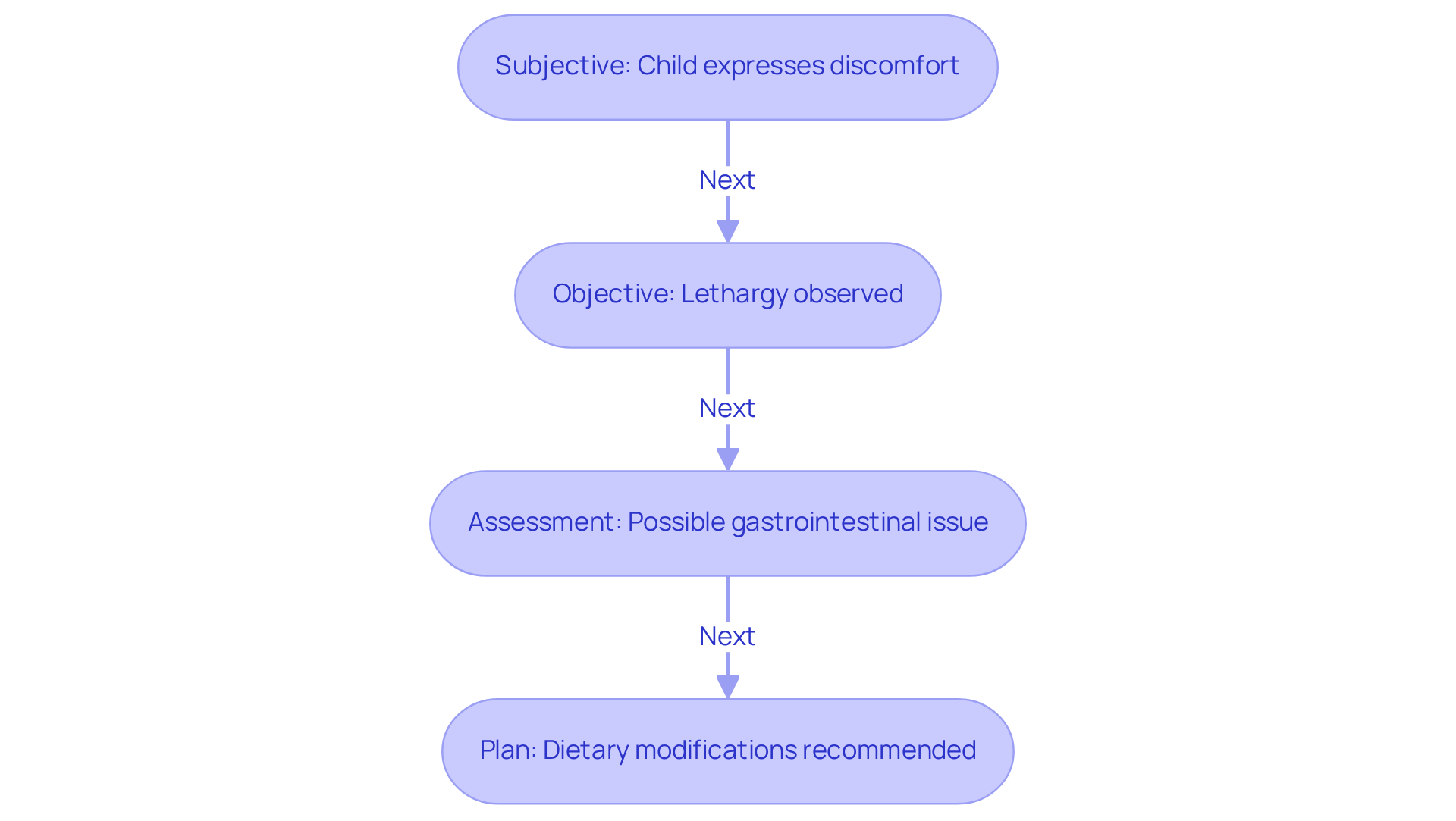
Pediatric SOAP Note Example: Tailoring Documentation for Young Patients
Subjective: The child expresses discomfort, stating, 'My tummy hurts.' The parent notes a decrease in appetite, which raises potential health concerns that deserve our attention. How often do we see children struggle to articulate their feelings?
Objective: Observations reveal that the child appears lethargic, and an abdominal examination shows tenderness—critical indicators for further assessment. It’s essential that pediatric documentation includes vital signs and physical examination results to provide a comprehensive view of the child's health.
Assessment: These findings suggest a possible gastrointestinal issue, highlighting the need for additional evaluation to confirm the diagnosis and determine appropriate interventions.
Plan: Recommended actions include dietary modifications to alleviate symptoms and scheduling a follow-up appointment in one week to monitor progress and reassess the child's condition.
Precise record-keeping in pediatric care is crucial for effective treatment planning and continuity of care. SOAP notes examples for pediatrics should reflect the unique communication styles of children, often requiring input from caregivers to capture a complete view of the child's health. Effective record-keeping practices, such as SOAP notes examples, include using clear, simple language and incorporating direct quotes from both the child and their guardians to enhance understanding and engagement.
Pediatricians emphasize the importance of capturing both subjective experiences and objective findings. This dual approach aids in forming a . For instance, a pediatrician observed, 'Recognizing functional limitations is essential to pediatric evaluation.' This highlights the necessity for comprehensive records that consider developmental stages and family dynamics.
Furthermore, studies indicate that record-keeping time decreased by 50% after transitioning to specialized pediatric templates. This underscores the efficiency achieved through appropriate record management practices. By customizing records to the needs of young individuals, healthcare providers can ensure that their notes are not only precise but also significant in guiding treatment choices.
To implement these practices effectively, providers should consider using standardized templates that facilitate comprehensive and efficient record-keeping. How can we make our documentation more effective while ensuring we remain connected to our young patients?
Geriatric SOAP Note Example: Ensuring Comprehensive Care for Older Adults
In the realm of elderly support, effective documentation is not just a task; it is a cornerstone for ensuring comprehensive management of individuals. A well-organized medical note serves as an invaluable resource for healthcare professionals, fostering clear communication and continuity of care. Consider this example of a Geriatric SOAP note:
Subjective: The patient shares, 'I feel more tired than usual and have trouble sleeping.' This expression highlights the individual's perception of their health, which is crucial for understanding their unique needs.
Objective: While vital signs remain stable, the physical examination reveals decreased mobility. Documenting these objective observations allows for a clear evaluation of the individual's current health status.
Assessment: The assessment suggests possible sleep disturbances and mobility issues, indicating a need for further evaluation. This section synthesizes both subjective and objective data, guiding .
Plan: The proposed plan includes sleep hygiene education and a physical therapy evaluation. This proactive approach ensures that the patient receives tailored interventions to address their specific concerns.
Incorporating insights from elderly health experts can further illuminate the importance of detailed records. For instance, experts emphasize that 'thorough records are essential for providing quality support to elderly individuals,' underscoring the critical role of [soap notes examples](https://blog.cosmaneura.com/10-essential-md-548-instructions-for-healthcare-providers) in geriatric practice. Additionally, with health and long-term support expenses for individuals living with dementia projected to reach $384 billion in 2025, efficient record-keeping becomes increasingly vital in managing assistance for older adults. By committing to effective documentation practices, healthcare providers can significantly enhance the quality of care for older adults, ensuring that their unique needs are met with compassion and precision.
Conclusion
In the realm of healthcare documentation, SOAP notes are essential for fostering accurate and effective communication between providers and patients. This structured approach not only enhances the quality of care but also alleviates administrative burdens, allowing healthcare professionals to devote more time to meaningful patient interactions. Have you considered how AI-powered solutions like CosmaNeura can help? By significantly reducing the time spent on documentation, providers can maintain the integrity and accuracy of their notes while focusing on what truly matters—their patients.
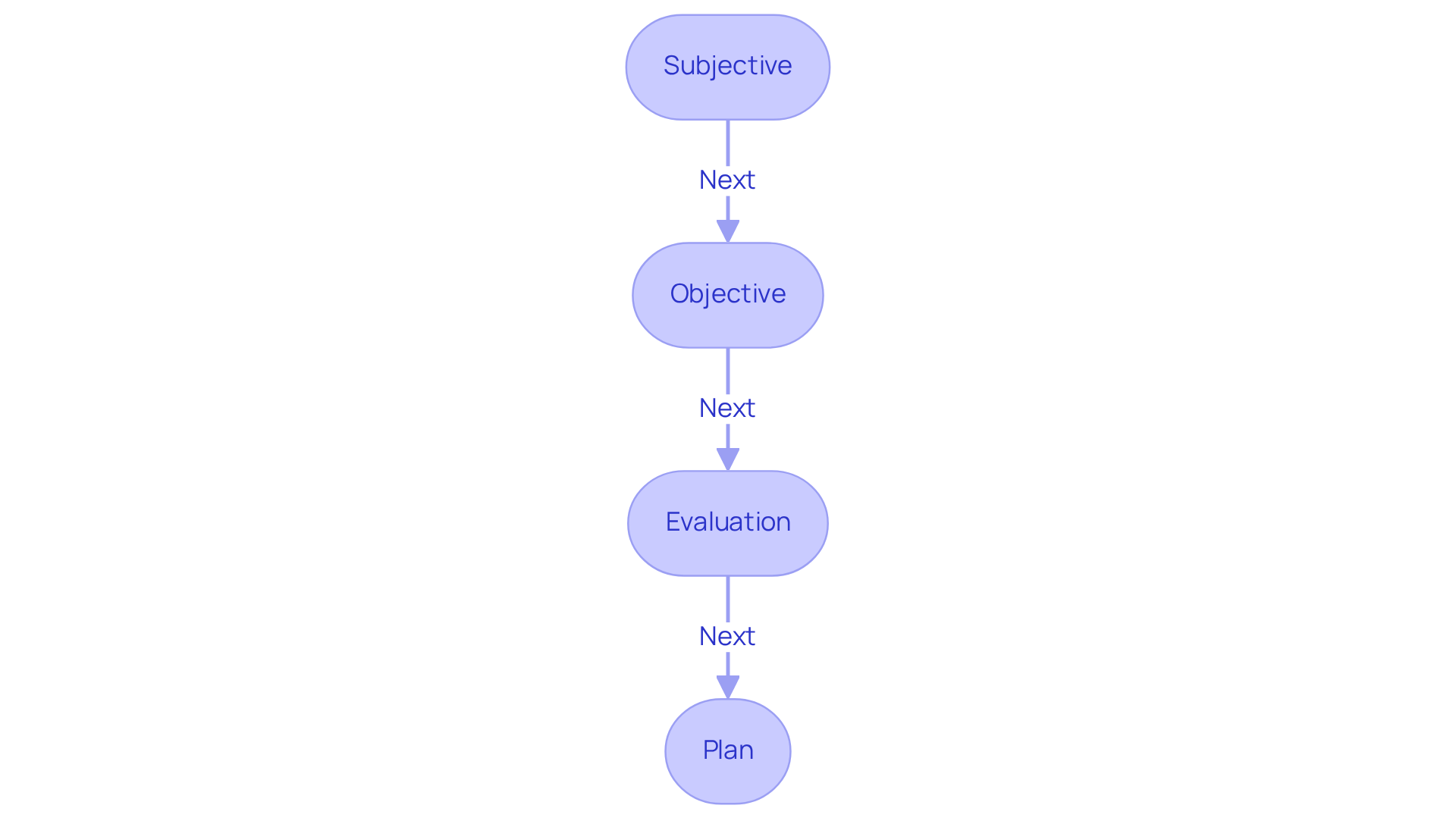
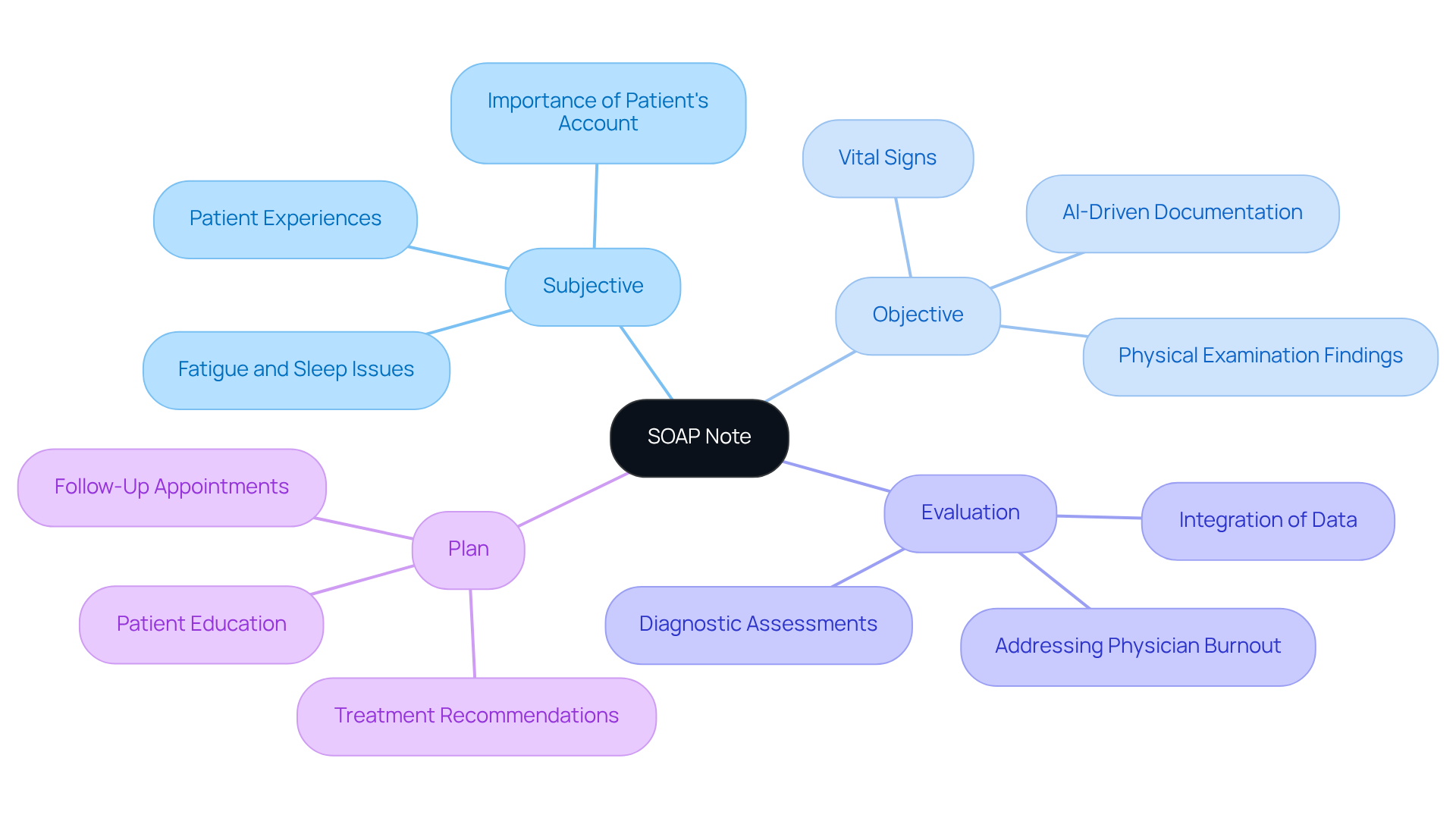
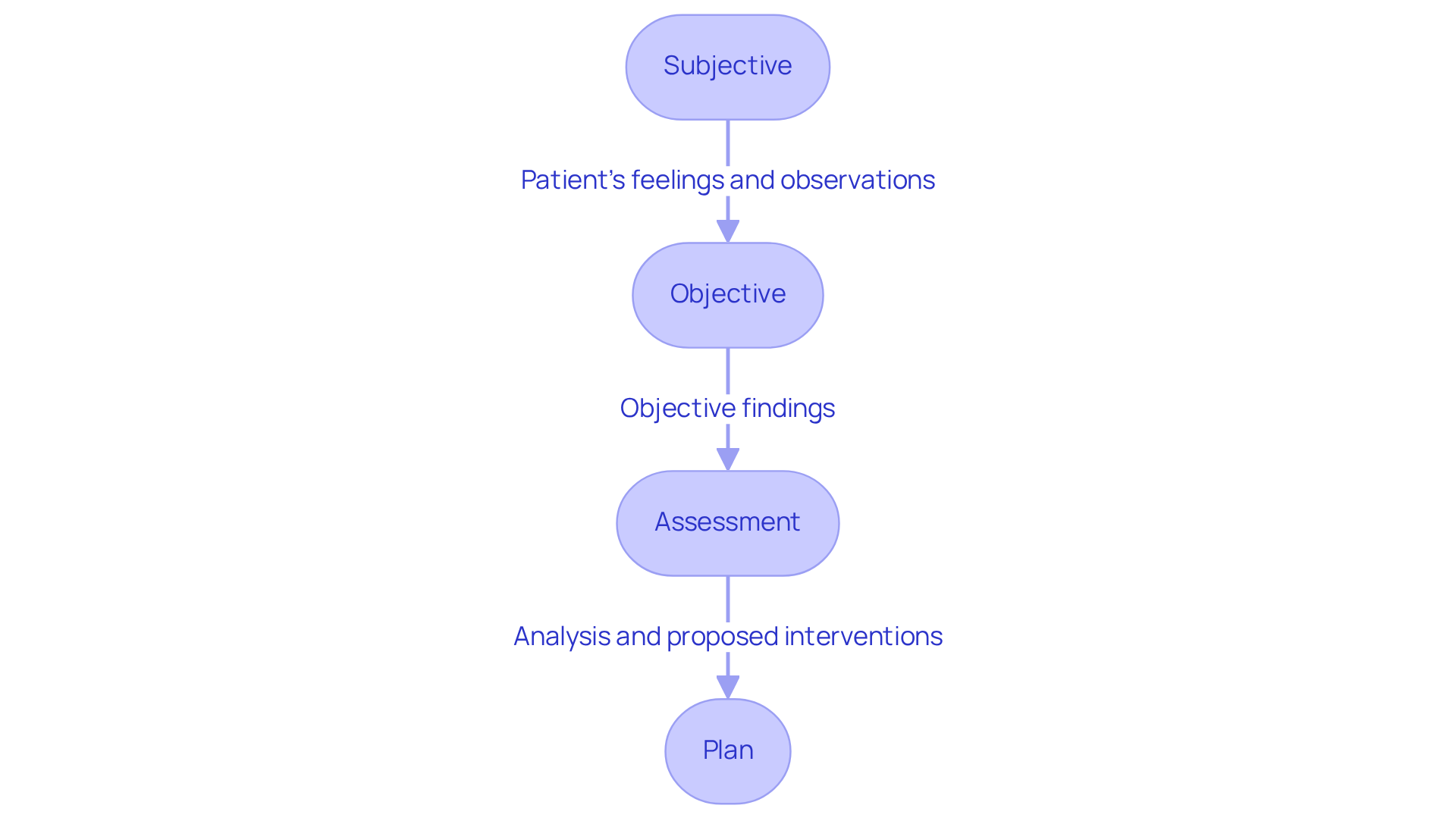
Throughout this article, we've explored various SOAP note examples across different healthcare fields, illustrating how each component—Subjective, Objective, Assessment, and Plan—contributes to a comprehensive understanding of patient needs. From mental health to geriatric care, the significance of precise documentation is clear. Each example underscores the necessity of capturing both the patient's experiences and clinical observations, ultimately informing treatment plans and promoting continuity of care. How might your practice benefit from such clarity?
As the healthcare landscape evolves, embracing effective documentation practices is more crucial than ever. By prioritizing accurate and timely SOAP notes, healthcare providers not only enhance patient outcomes but also cultivate a culture of professionalism and accountability. The integration of AI tools can elevate these practices even further, ensuring that quality care remains at the forefront while easing the administrative burdens that often hinder healthcare delivery. Embrace these insights and consider how implementing robust SOAP note strategies can transform your practice and improve the lives of those you serve.




