Overview
The article titled "10 SOAP Narrative Examples to Enhance Your Documentation Skills" addresses the emotional challenges faced by healthcare providers in their documentation practices. It offers practical examples and guidelines for writing effective SOAP notes, recognizing that the administrative burdens can weigh heavily on these dedicated professionals. By utilizing structured SOAP narratives, providers can significantly improve their record-keeping practices, fostering better communication and ultimately enhancing patient outcomes. This is not just a theoretical approach; various studies and expert opinions included in the content provide evidence of these benefits. We invite you to explore these examples and consider how they might alleviate some of the pressures you face, leading to a more fulfilling practice and better care for your patients.
Introduction
In the intricate landscape of healthcare, effective documentation transcends mere regulatory compliance; it stands as a vital component that profoundly influences patient care. As providers navigate the weight of administrative burdens, the pressing need for streamlined documentation methods becomes increasingly clear. This article delves into ten compelling SOAP narrative examples that not only refine documentation skills but also empower healthcare professionals to reclaim invaluable time for meaningful patient interactions. Yet, as the complexity of patient needs continues to evolve, how can practitioners ensure their documentation remains both efficient and comprehensive?
CosmaNeura: AI-Driven Patient Documentation for Healthcare Providers
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. CosmaNeura understands these emotional challenges and utilizes advanced AI technology to automate records, significantly lightening this load. By enhancing the documentation process, this platform allows clinicians to dedicate more time to their patients, ensuring that the vital human touch remains central to medical service delivery.
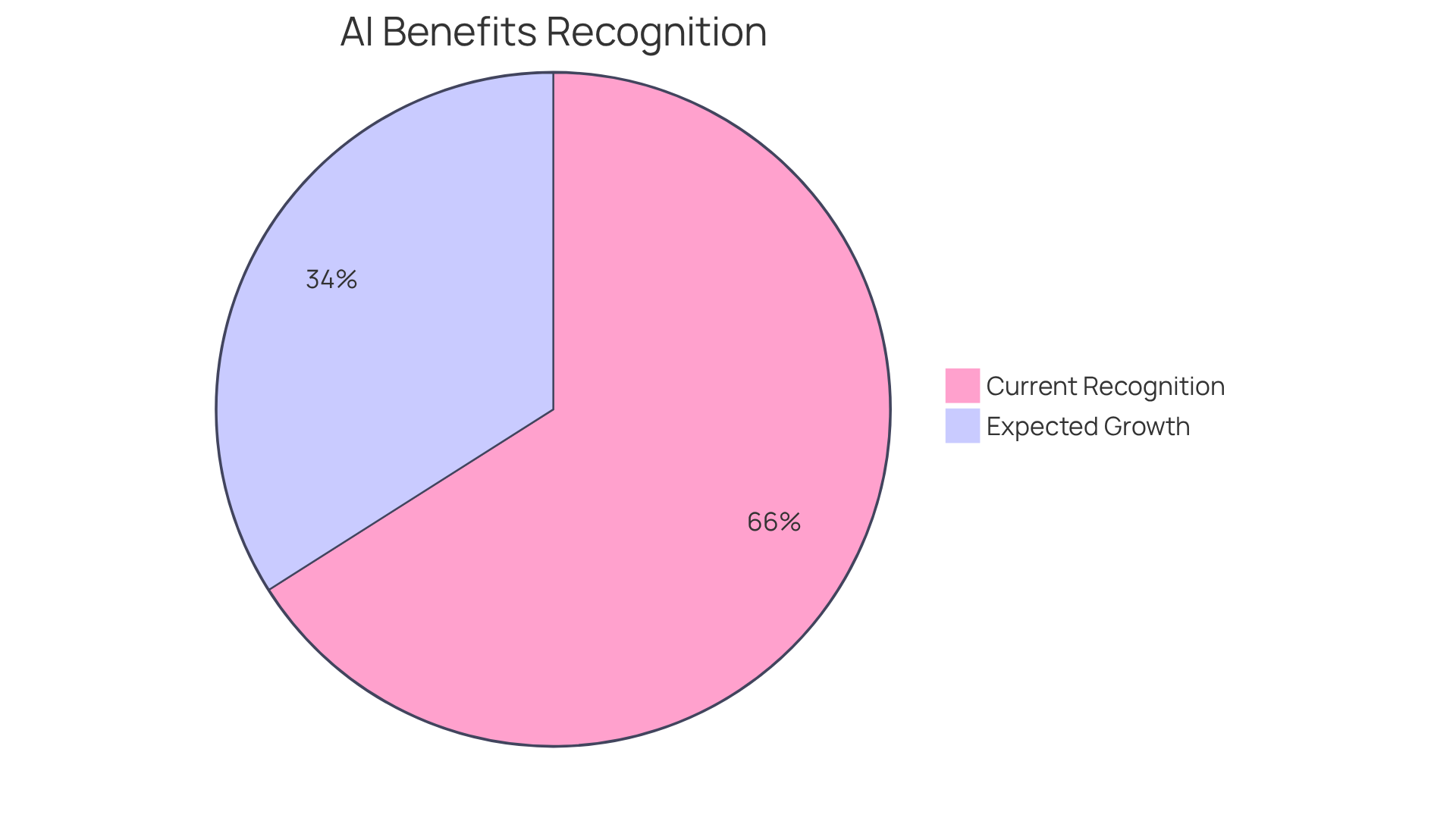
Imagine regaining precious hours each week to connect with those you care for. Medical leaders have noted that integrating AI can reduce administrative tasks by approximately 20%. This means more time for what truly matters—your patients. Case studies involving over 1,000 medical providers reveal that 57% of physicians see the alleviation of administrative burden as a significant opportunity for AI. With 66% of physicians expected to in 2024—a remarkable 78% increase from 38% in 2023—CosmaNeura stands out as an essential tool in the evolving landscape of medical services, enhancing both provider satisfaction and patient outcomes.
As healthcare costs continue to rise, there is an urgent need for solutions that improve financial efficiency without sacrificing the quality of care. Almost two-thirds—around 66%—of the 1,081 doctors surveyed by the AMA recognize the benefits of employing AI in medical services. This further underscores the platform's importance in transforming care delivery and addressing the challenges faced by providers.
Consider how CosmaNeura can transform your practice. Are you ready to embrace a solution that not only alleviates your administrative burdens but also enhances the care you provide? Together, we can navigate these challenges and create a more compassionate healthcare environment.
Headway: Comprehensive Guide to Writing Effective SOAP Notes
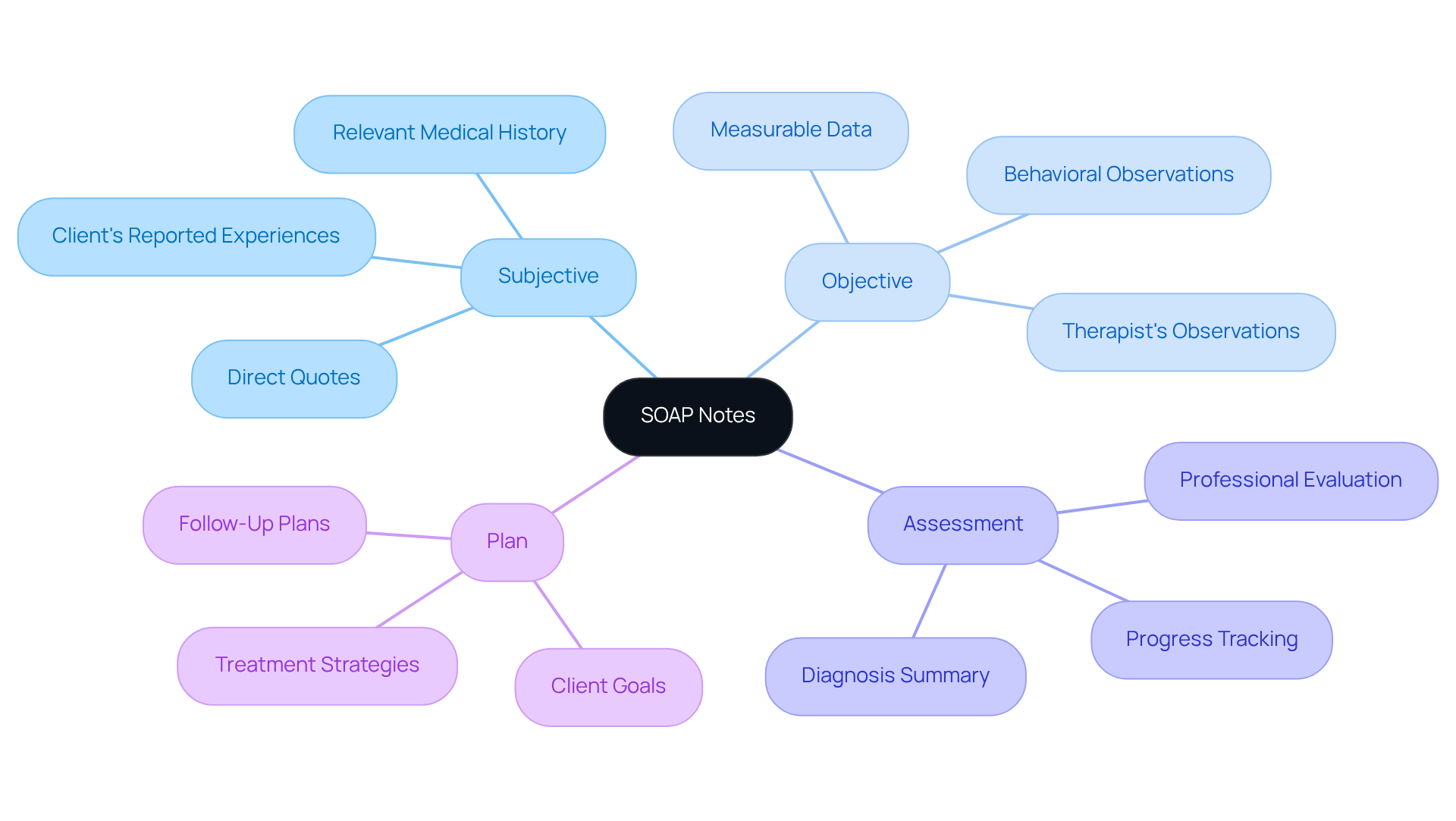
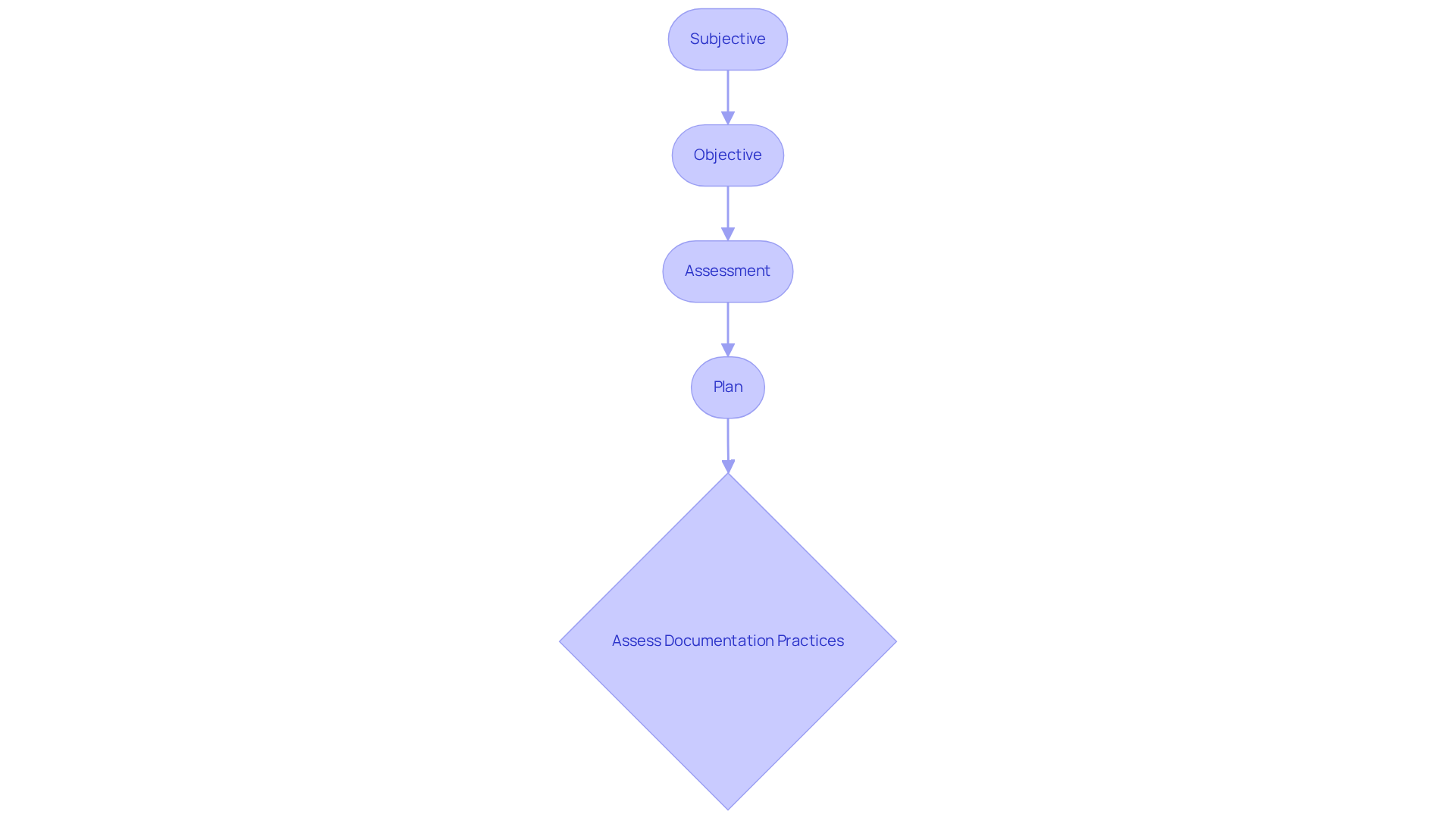
In the demanding world of healthcare, writing [effective SOAP narrative examples](https://headway.co/resources/soap-note) can often feel overwhelming. Headway provides a compassionate guide that breaks down each component: Subjective, Objective, Assessment, and Plan. This organized method not only ensures that all relevant individual information is gathered systematically but also fosters among medical providers. By embracing these guidelines, clinicians can enhance the quality of their records, ultimately leading to better health outcomes for their patients.
Imagine how much easier it would be to navigate patient care with clear and concise documentation. By utilizing this structured approach, healthcare providers can alleviate some of the administrative burdens that often detract from patient interactions. This not only helps in maintaining comprehensive records but also allows for more meaningful connections with patients.
Let’s take a moment to reflect: how often have you felt that time spent on paperwork could have been better used in direct patient care? By prioritizing effective SOAP narrative examples, you can transform your practice. Engage with these guidelines, and witness the positive impact on your documentation and patient relationships.
MedWriter.ai: Templates and Best Practices for SOAP Notes
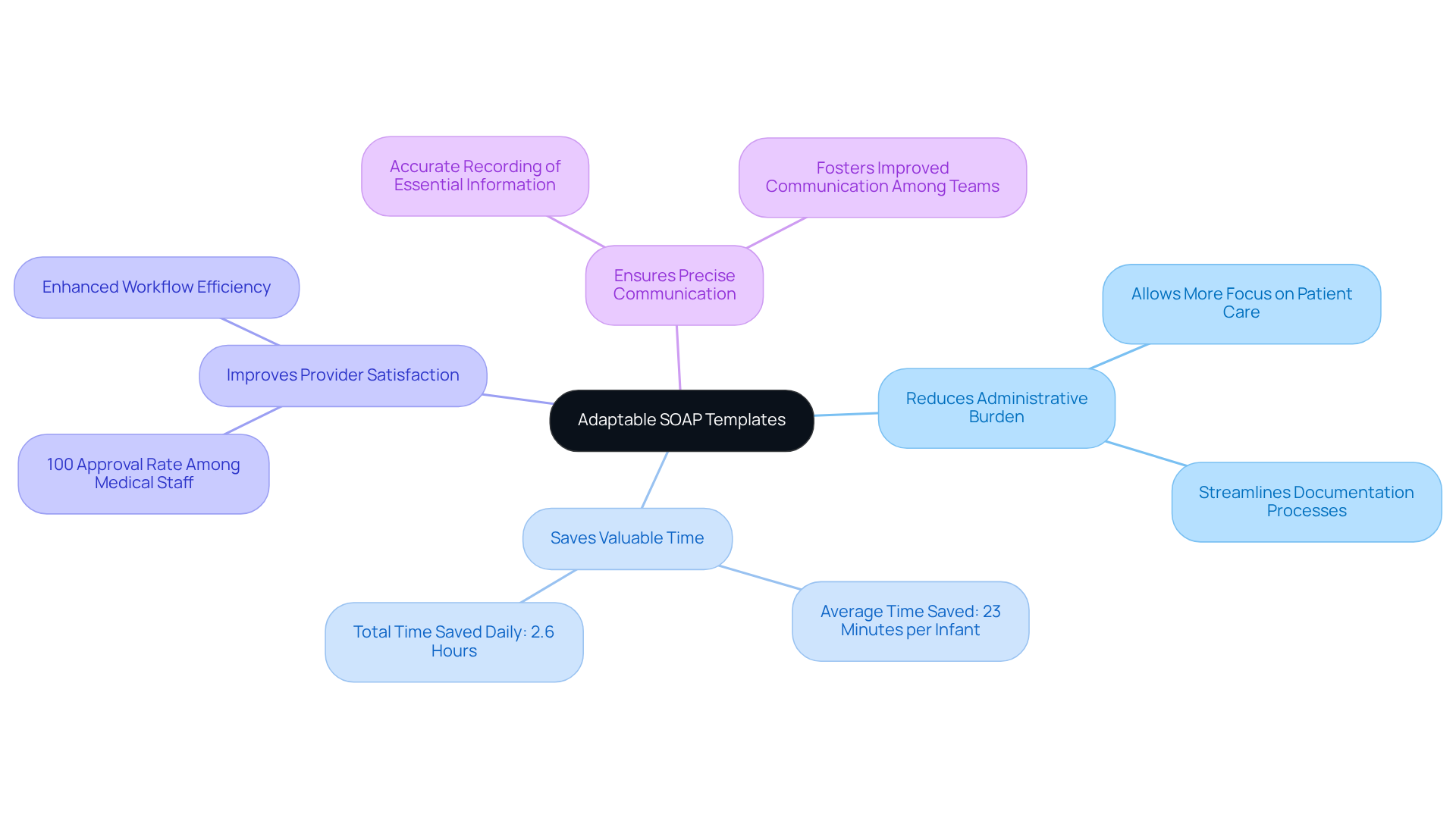
In the demanding world of healthcare, employing [adaptable templates for a SOAP narrative example](https://quenza.com/blog/soap-note) can significantly alleviate the strain on providers. These templates are thoughtfully designed to capture vital information effectively, allowing caregivers to focus more on what truly matters—patient care. By applying optimal techniques for a SOAP narrative example, such as clarity, conciseness, standardized language, and incorporating patient quotes, medical professionals can elevate the quality of their records.
Research highlights that enhancing document templates can lead to remarkable time savings. For instance, in a Mother-Baby Unit, the implementation of new templates resulted in an average time saving of 23 minutes per infant, translating to about 2.6 hours saved daily across the unit. This increased efficiency not only streamlines documentation but also , with surveys revealing 100% approval of the new templates among medical staff.
Moreover, the organized layout of the SOAP narrative example ensures that essential information is recorded accurately, fostering improved communication among medical teams and enhancing patient outcomes. By embracing these best practices and leveraging technology, healthcare providers can create effective SOAP records that serve as crucial legal documents while simultaneously enriching the overall quality of care.
- Key Benefits of Using Adaptable SOAP Templates:
- Reduces administrative burdens, allowing more focus on patient care.
- Saves valuable time, enhancing overall efficiency.
- Improves provider satisfaction through streamlined processes.
- Ensures precise communication among healthcare teams.
As we navigate the complexities of healthcare, let’s embrace these solutions and continue to improve our practices for the benefit of both providers and patients alike.
SimplePractice: User-Friendly SOAP Note Management for Therapists
Therapists often face overwhelming emotional challenges in their work. SimplePractice understands this and provides an intuitive platform designed specifically for them to manage their SOAP narrative example effectively. With , the record-keeping process becomes not just easier but also more supportive of their needs.
Imagine quickly entering and retrieving client information without the usual hassle. This intuitive interface allows therapists to maintain precise records effortlessly. By automating administrative tasks related to paperwork, therapists can reclaim precious time—time that can be devoted to nurturing relationships with their clients and delivering personalized care.
This simplicity of use transforms not just record-keeping practices but also empowers therapists to provide high-quality care. It's about enhancing client interactions and improving health outcomes. Are you ready to experience a change that prioritizes your well-being and that of your clients? Let SimplePractice be your partner in this journey toward more compassionate and effective care.
Mentalyc: Automated SOAP Note Generation for Enhanced Efficiency
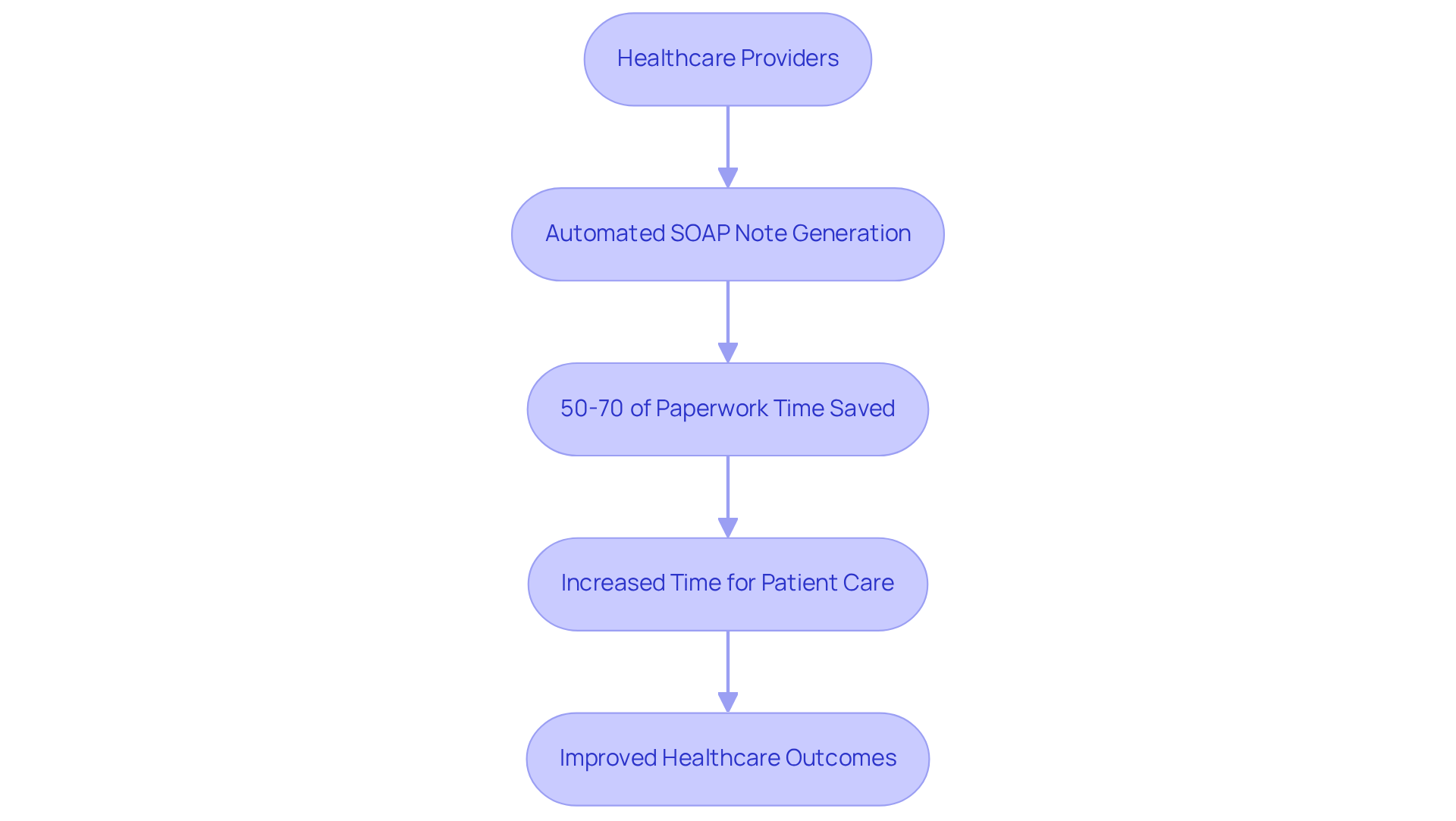
Healthcare providers often find themselves overwhelmed by administrative tasks, which can detract from their primary focus: patient care. Mentalyc understands these challenges and utilizes advanced AI technology to automate the creation of a soap narrative example. This innovation significantly simplifies the , allowing clinicians to reclaim 50-70% of their paperwork time. Imagine the valuable hours that can be redirected towards patient interactions and care.
By alleviating the burden of documentation, Mentalyc not only boosts efficiency but also ensures that records remain consistent and reliable across various medical fields. This consistency is crucial in a sector where every detail matters. Medical leaders recognize this transformative potential, with 89% believing that AI can expedite processes within healthcare.
As we navigate an environment marked by challenges such as restricted access to care and rising costs, the use of a soap narrative example through automated document creation emerges as a vital resource. It enhances clinician efficiency and ultimately improves healthcare outcomes. If you’re ready to explore how this solution can benefit your practice, consider taking the next step towards a more efficient future in patient care.
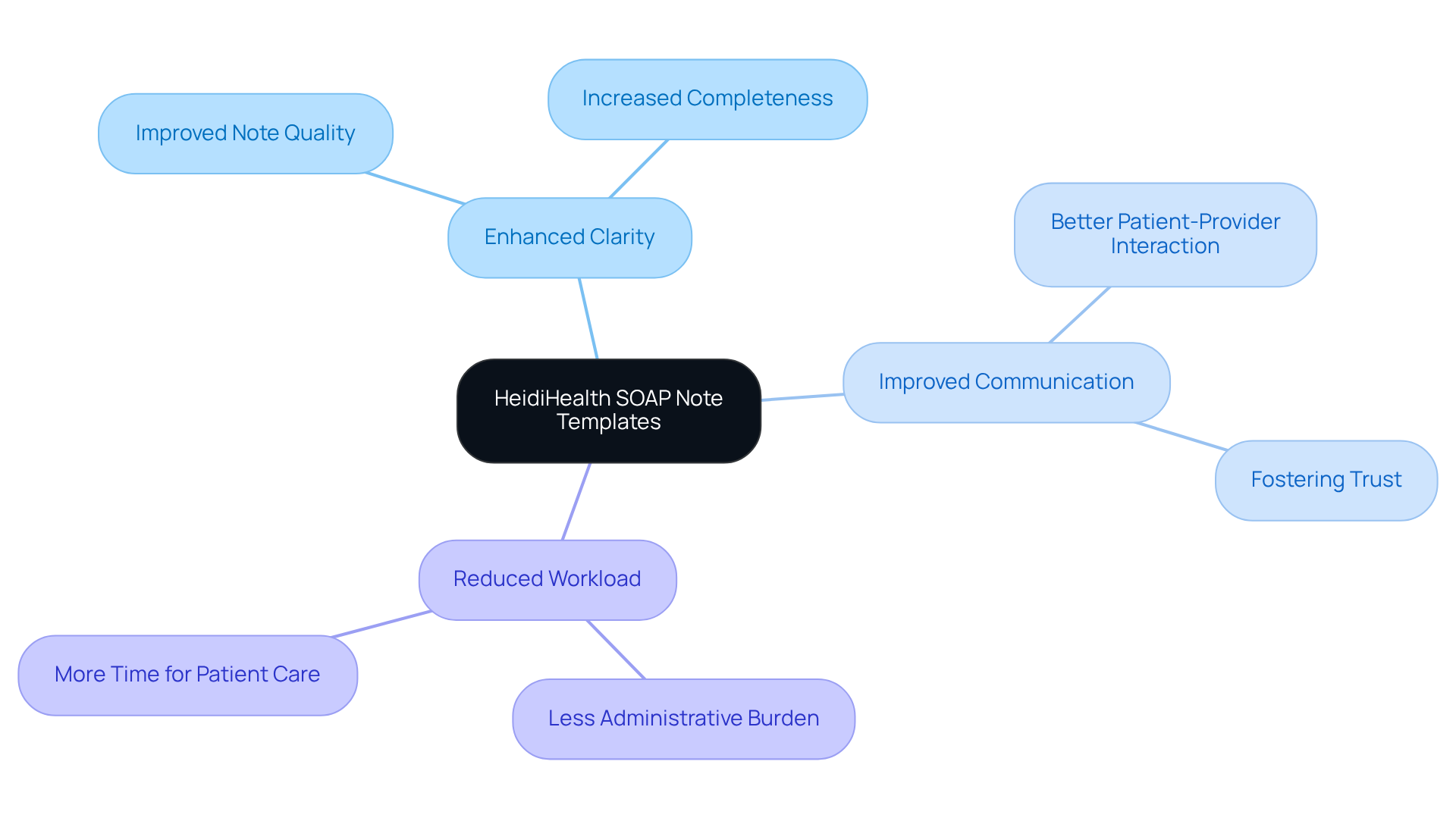
HeidiHealth: Customizable SOAP Note Templates for Various Medical Fields
HeidiHealth understands the emotional challenges that healthcare providers face. The adjustable SOAP narrative examples, designed for various medical specialties, enable practitioners to customize their records according to their specific needs. This flexibility is essential for capturing all relevant information efficiently, which is crucial for maintaining amidst the complexities of disjointed medical systems.
Did you know that organized records can significantly enhance the quality of Electronic Health Record (EHR) entries? A study revealed that the Qnote quality score improved from 64.35 to 77.2 (p < 0.001), showcasing remarkable advancements in clarity and brevity. By streamlining workflows, these customizable templates enable healthcare providers to focus more on their interactions with patients, fostering better communication and coordination.
As Dr. Glen Stream wisely notes, "Effective record-keeping is crucial for enhancing health outcomes and satisfaction." By embracing these customizable templates, clinicians can refine their documentation practices, leading to improved patient outcomes and satisfaction. This approach also helps alleviate some of the administrative burdens that contribute to physician burnout.
Consider the benefits of adopting these templates:
- Enhanced clarity in records
- Improved patient-provider communication
- Reduced administrative workload
By taking this step, you can create a more compassionate healthcare environment that prioritizes patient care and provider well-being. Let’s work together to overcome these challenges and enhance the healthcare experience for everyone involved.
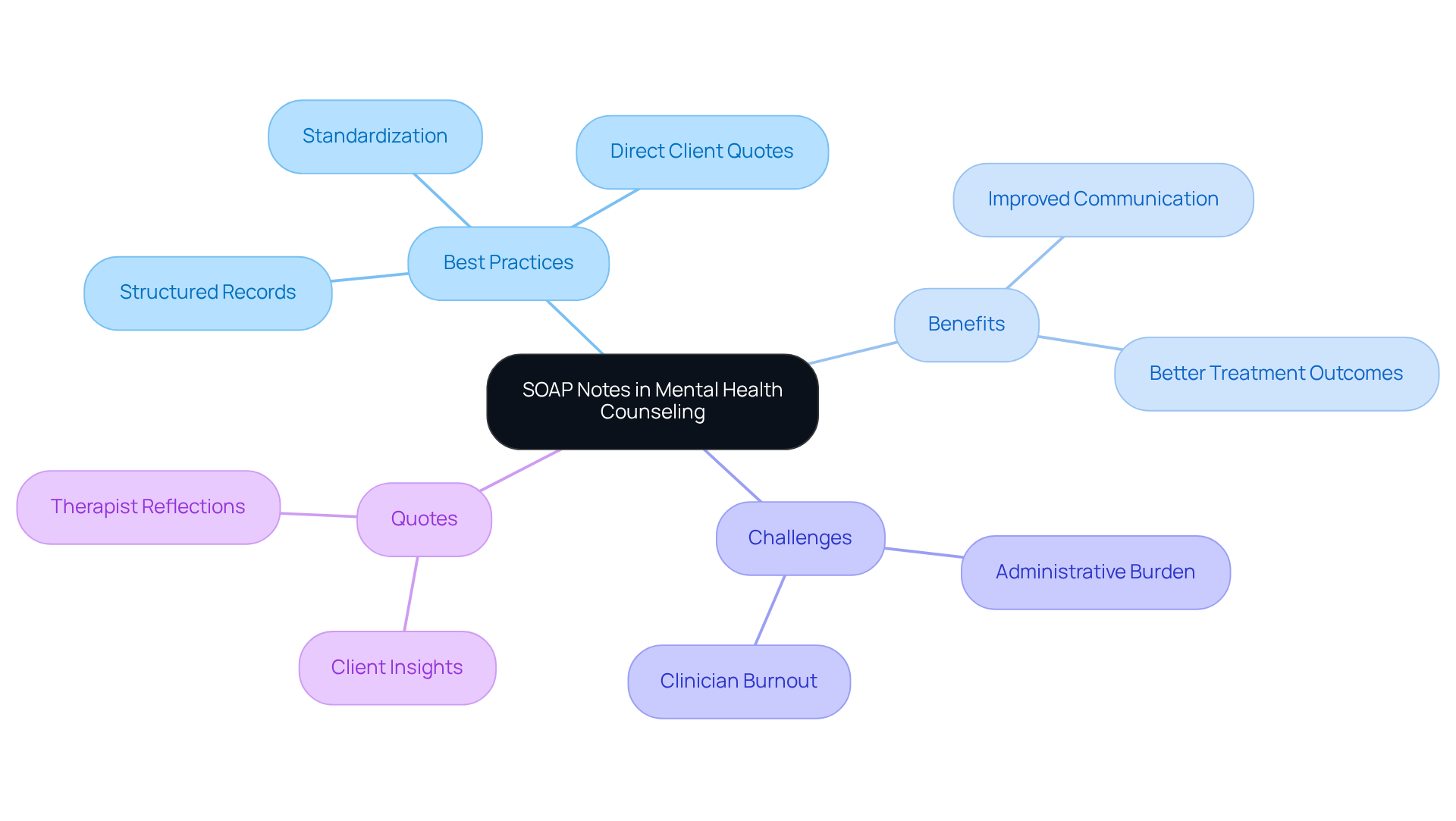
Psylio: SOAP Note Examples for Mental Health Counseling
At Psylio, we understand the emotional challenges that mental health professionals face, especially when it comes to documenting client interactions. Our comprehensive collection of soap narrative examples is designed with your needs in mind, showcasing best practices that not only capture all pertinent information but also enhance communication among healthcare providers. Have you ever felt overwhelmed by the administrative burdens that can detract from patient care? Effective record-keeping is crucial, and studies show that structured and standardized records can significantly improve the quality of mental health care, leading to better treatment outcomes.
We encourage mental health professionals to adopt these practices, as they can and alleviate the administrative burden that often contributes to clinician burnout. By including direct quotes from clients within SOAP records, you can add depth and clarity, capturing the nuances of their experiences. As one specialist wisely noted, "Investing effort into creating clear, concise, and clinically pertinent records can result in improved treatment outcomes and a more fulfilling practice experience."
By utilizing soap narrative examples, mental health practitioners can enhance their recording skills, ultimately improving the quality of care they provide. Remember, every step you take towards better documentation is a step towards a more rewarding practice and better outcomes for your clients. Let's embrace these tools together and foster a supportive environment for both clinicians and clients.
Social Work Portal: SOAP Note Writing Guide for Social Workers
The Social Work Portal offers a specialized guide for writing a soap narrative example, designed specifically for social workers to address the unique challenges that arise in documenting client interactions. Effective record-keeping is essential; unclear notes can become liabilities, particularly regarding insurance reimbursement. This guide provides practical advice and relatable examples that empower social workers to . Have you ever considered how your documentation reflects your clients' strengths? A recent study revealed that only 1% of students recorded client strengths, highlighting a significant gap in effective record-keeping.
As Enola Proctor wisely states, "Social work’s future, its very survival, depends on our ability to deliver services with a solid base of evidence and to document their effectiveness." By adhering to the SOAP narrative example—Subjective, Objective, Assessment, and Plan—social workers can create notes that are not just clear and concise, but also impactful in conveying essential information. Incorporating strengths-based records is crucial; it fosters a more holistic view of clients and their needs, ultimately leading to improved social work outcomes.
To implement these practices effectively, consider regularly assessing your record-keeping methods. Are you seeking feedback to ensure your documentation meets professional standards? By doing so, you can enhance your practice and better support your clients. Remember, your notes are not just administrative tasks; they are vital tools in your compassionate mission to serve those in need.
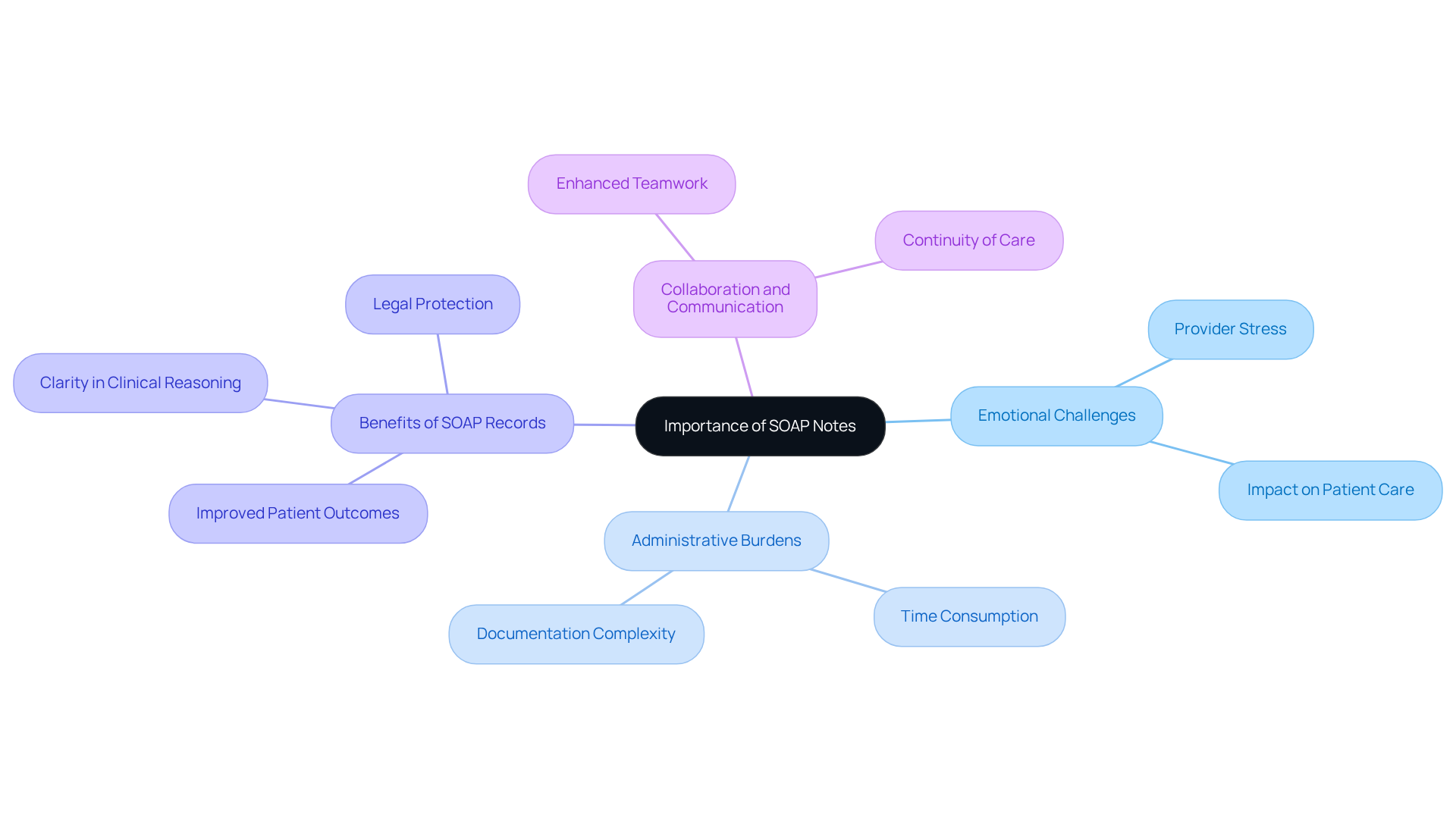
NCBI: Educational Resource on the Importance of SOAP Notes
Healthcare providers often face emotional challenges in their daily practice. The administrative burdens can weigh heavily, impacting the quality of patient care. The NCBI offers a valuable educational resource that highlights the significance of a SOAP narrative example in clinical settings. By utilizing SOAP records as a SOAP narrative example, medical professionals can efficiently capture individual interactions, fostering better communication and ensuring continuity of care, particularly in fragmented medical systems.
Imagine the difference it can make when healthcare providers enhance their understanding of the SOAP narrative example. This knowledge leads to , ultimately benefiting patient outcomes. Organized records through a SOAP narrative example not only clarify clinical reasoning but also promote collaboration among care teams. This collaborative spirit is essential in today’s medical landscape.
By embracing these educational tools, healthcare professionals can navigate their roles with greater confidence and efficiency. Consider how streamlined documentation can alleviate stress and enhance teamwork. Let’s take action together to prioritize effective communication and patient-centered care. Engage with the resources available and witness the positive impact on your practice and your patients.
Upheal: Practical SOAP Note Examples for Healthcare Providers
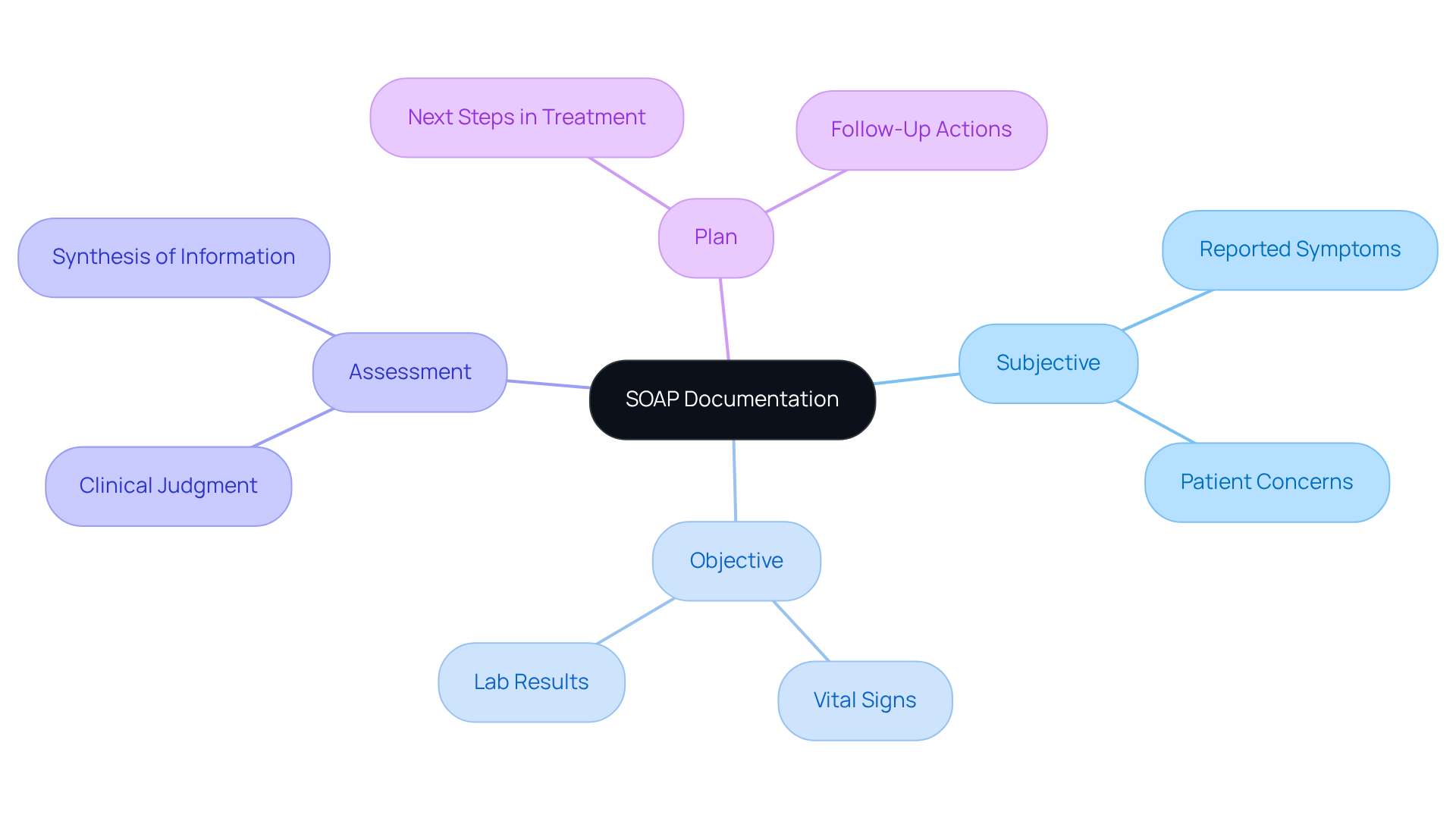
Thorough recording of client interactions is essential for healthcare professionals, especially when facing challenges like physician burnout and resistance to innovation. Have you considered how structured documentation can alleviate some of these burdens? Utilizing the SOAP format—Subjective, Objective, Assessment, and Plan—can significantly enhance this process. By adopting these structured practices, providers can ensure that all relevant information is captured accurately, leading to improved care and safety.
Practical examples serve as a SOAP narrative example that illustrates how to document interactions effectively. For instance:
- In the Subjective section, a provider might note an individual's reported symptoms and concerns.
- The Objective section could include measurable data such as vital signs or lab results.
- The Assessment section synthesizes this information to provide a clinical judgment.
- The Plan outlines the next steps in treatment.
Incorporating these examples into daily practice not only enhances the quality and consistency of records but also and improves revenue cycle management. Healthcare experts emphasize that comprehensive record-keeping methods lead to increased reimbursement levels and reduced legal risks, ultimately benefiting both providers and patients. By focusing on structured data entry, clinicians can streamline their workflows and derive actionable insights from patient data, ensuring a more effective healthcare delivery system.
Furthermore, leveraging innovative AI solutions like CosmaNeura's Agentic Platform can enhance these documentation practices, addressing administrative burdens and fostering a more [patient-centered approach to care](https://blog.cosmaneura.com/10-medical-software-systems-examples-for-enhanced-healthcare-delivery). Imagine the relief of having more time to focus on what truly matters—your patients.
Conclusion
In the realm of healthcare, effective documentation is not merely a task; it is a vital component that enhances patient care and provider efficiency. Have you ever felt overwhelmed by administrative burdens? This article emphasizes the significance of utilizing structured SOAP narratives, demonstrating how various platforms and tools, such as CosmaNeura and SimplePractice, can alleviate these pressures. By adopting these practices, healthcare providers can redirect their focus towards what truly matters—building meaningful connections with patients.
Key insights reveal that integrating AI-driven solutions can significantly reduce the time spent on documentation. Imagine studies indicating up to a 70% decrease in paperwork time! Furthermore, customizable templates and best practices in SOAP note writing not only streamline the documentation process but also improve communication among healthcare teams. This structured approach fosters better patient outcomes and enhances overall provider satisfaction, underscoring the transformative potential of effective record-keeping.
As the healthcare landscape continues to evolve, embracing these innovative documentation strategies is crucial. Providers are encouraged to prioritize efficient and compassionate care by leveraging technology and structured methodologies. By doing so, they can navigate the complexities of patient interactions with greater confidence. Ultimately, this leads to improved health outcomes and a more rewarding practice experience for both clinicians and patients alike. Let’s take this step together towards a brighter future in healthcare.




