Overview
This article addresses the emotional challenges that nurse practitioners face in patient care documentation. It highlights the overwhelming nature of administrative tasks and how they can detract from the compassionate care providers wish to deliver. By focusing on structured SOAP notes, the article illustrates a solution that not only enhances accuracy and clarity in clinical records but also fosters effective communication among healthcare providers.
Imagine a world where your documentation supports your patient interactions rather than hinders them. Structured SOAP notes can lead to better patient outcomes, allowing for personalized treatment plans tailored to individual needs. This approach not only alleviates some of the administrative burdens but also empowers you to focus on what truly matters—your patients.
Are you ready to transform your documentation practices? Embracing structured SOAP notes could be the first step towards a more fulfilling practice. By refining your documentation, you can enhance your ability to connect with patients and provide them with the care they deserve. Let’s explore how these tools can make a difference in your daily practice and ultimately improve the lives of those you serve.
Introduction
In the fast-paced world of healthcare, the weight of administrative tasks can often overshadow the essential mission of patient care. For nurse practitioners, mastering the art of SOAP notes is not merely a necessity; it is a pivotal opportunity to enhance clinical documentation and improve patient outcomes. Yet, with the complexities of modern medical practice, how can practitioners ensure their SOAP notes are both accurate and effective in conveying critical patient information? This article explores ten exemplary SOAP note formats tailored for nurse practitioners, offering insights and strategies to streamline documentation while nurturing compassionate care.
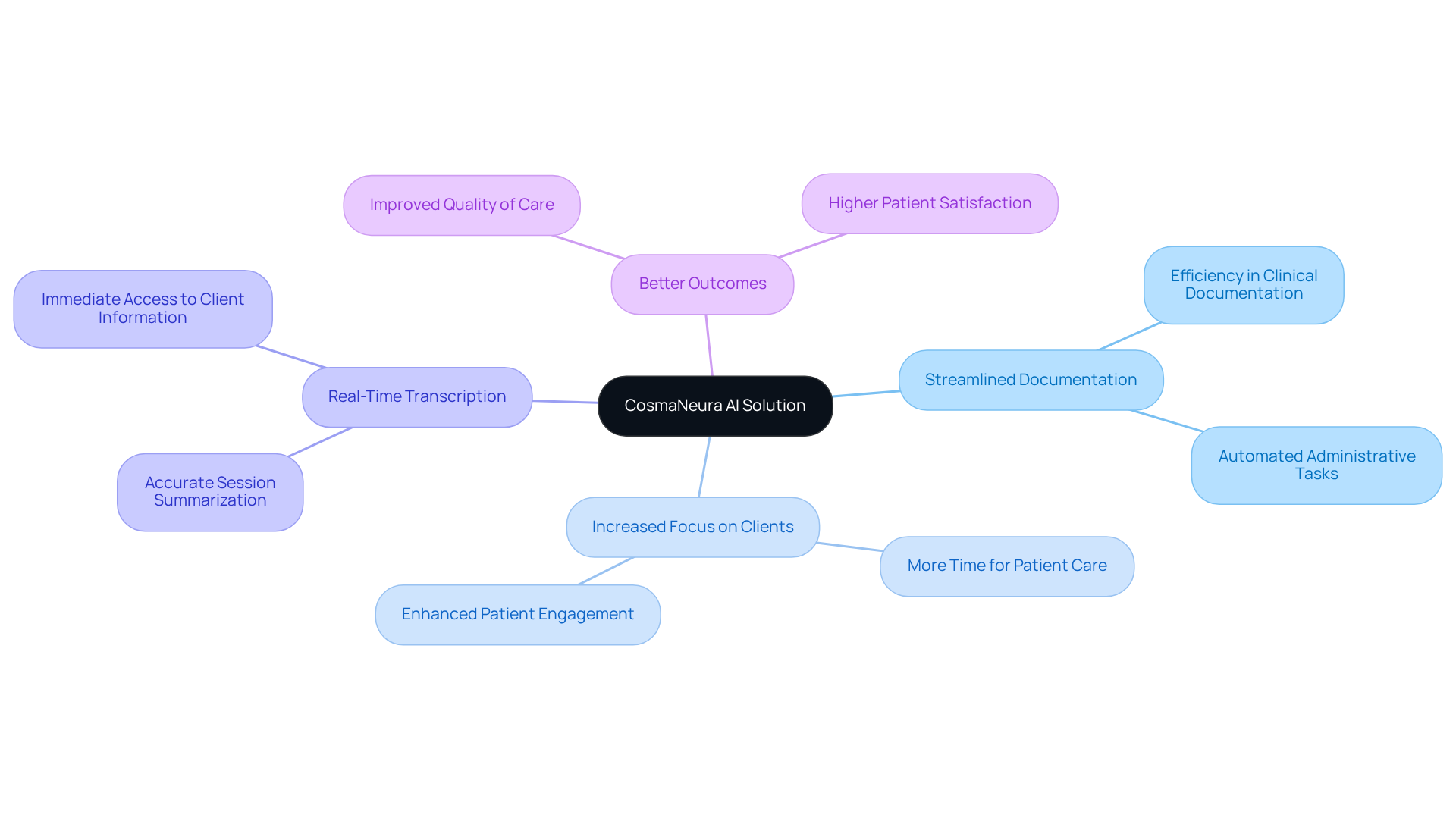
CosmaNeura: Streamline SOAP Note Documentation with AI Assistance
Healthcare providers often face overwhelming emotional challenges due to administrative burdens that detract from their ability to care for clients. CosmaNeura's AI platform is here to help transform this experience. By utilizing a soap note example nurse practitioner to automate the documentation process, providers can focus more on what truly matters—their clients.
Imagine being able to dedicate more time to client care rather than getting bogged down in paperwork. The platform offers real-time transcription and summarization of telehealth sessions, capturing all relevant client information with precision and efficiency. This capability not only saves valuable time but also significantly enhances the quality of care provided to individuals.
As we prioritize compassionate healthcare, the benefits of this AI solution become clear. By alleviating administrative tasks, healthcare providers can anticipate increased efficiency in clinical documentation, which can be illustrated through a soap note example nurse practitioner. This shift ultimately leads to better outcomes and greater satisfaction for those receiving care.
Are you ready to embrace a solution that allows you to focus on your clients? With CosmaNeura, you can and enhance the care you provide. Let's work together to create a more compassionate healthcare experience.
Mental Health SOAP Note Example: Capturing Patient Insights Effectively
In a mental health environment, it's essential to begin with the Subjective section of a soap note example nurse practitioner, which captures the individual's self-reported feelings. For example, someone might say, 'I feel anxious and overwhelmed due to work stress.' This personal insight is vital as it reflects their emotional state and sets the context for the session.
Next, the Objective section should document observable behaviors, such as, 'Individual appeared restless and avoided eye contact during the session.' This provides concrete evidence of their condition. In the Assessment, clinicians synthesize this information, noting, 'Increased anxiety levels observed, likely related to the work environment.' This analysis helps us understand the individual's current challenges.
Ultimately, the Plan outlines actionable strategies, like 'Continue cognitive behavioral therapy sessions and introduce mindfulness techniques.' This ensures that treatment is tailored to the individual's needs. This organized approach, as seen in a , not only enhances record accuracy but also improves mental health outcomes by addressing all aspects of the patient's experience.
As Vivian Chung Easton wisely states, 'The primary objective of documentation is to facilitate high-quality, personalized care for your clients.' Moreover, therapists who utilized standardized templates for documentation accuracy saw an enhancement of 22% and a reduction in completion time by 31%.
Keeping thorough and precise clinical records is crucial for adhering to laws and regulations, ensuring ethical and effective care for individuals. How can we improve our documentation practices to better serve our clients? Let's strive for a compassionate approach that prioritizes their well-being.
Physical Therapy SOAP Note Example: Documenting Patient Progress
In the realm of physical therapy, a soap note example nurse practitioner serves as a vital tool for understanding patient experiences. The Subjective section reflects the individual's feelings, such as, 'I feel less pain in my knee but still have difficulty bending it.' This acknowledgment of personal struggle is crucial for building trust. The Objective section, presenting quantifiable data like, 'Patient demonstrates 90 degrees of flexion during assessment,' offers a clear view of progress.
The Assessment section synthesizes this information, noting, 'Improvement in pain levels observed, but further range of motion exercises are necessary.' This compassionate analysis highlights the ongoing journey towards recovery. Finally, the Plan outlines the next steps: 'Continue with physical therapy sessions twice a week, focusing on flexibility and strength training.' This organized approach, as illustrated in a soap note example nurse practitioner, not only aids in but also empowers therapists to make informed adjustments to treatment plans, ultimately enhancing patient outcomes.
Furthermore, adhering to HIPAA guidelines in record-keeping is essential for preserving patient confidentiality and ensuring legal compliance. Have you considered how efficient recording can impact your practice? Studies indicate that using organized formats can expedite documentation by up to 20%, significantly boosting productivity. Moreover, a uniform structure in clinical documentation fosters collaboration among practitioners, addressing common challenges in record-keeping. Together, we can create a more supportive environment for both patients and healthcare providers.
Family Medicine SOAP Note Example: Comprehensive Patient Care Records
In family medicine, the journey begins with the Subjective section of a soap note example nurse practitioner, where we capture the individual's narrative. Imagine someone sharing, 'I have been feeling fatigued and have a persistent cough.' This personal account is essential for truly understanding their experience and emotional state. Next, we move to the Objective section, which details measurable data such as vital signs and physical exam findings: 'Blood pressure 120/80, heart rate 72, lungs clear on auscultation.' These objective observations provide a solid foundation for clinical assessment, ensuring we base our decisions on facts.
The Assessment section synthesizes this information, stating, 'Possible viral infection; monitor symptoms.' This critical step combines both subjective and objective data, guiding the clinician's diagnostic reasoning towards a working diagnosis. Finally, the Plan outlines actionable steps: 'Advise rest, hydration, and follow-up in one week if symptoms persist.' This , which can be illustrated by a soap note example nurse practitioner, typically ranges from two to four paragraphs and ensures that all client concerns are documented and addressed. It helps avoid over-charting, enhancing continuity of care and supporting effective clinical decision-making.
By embracing this structured method, we not only streamline our processes but also nurture the patient-provider relationship, fostering an environment of care and understanding.
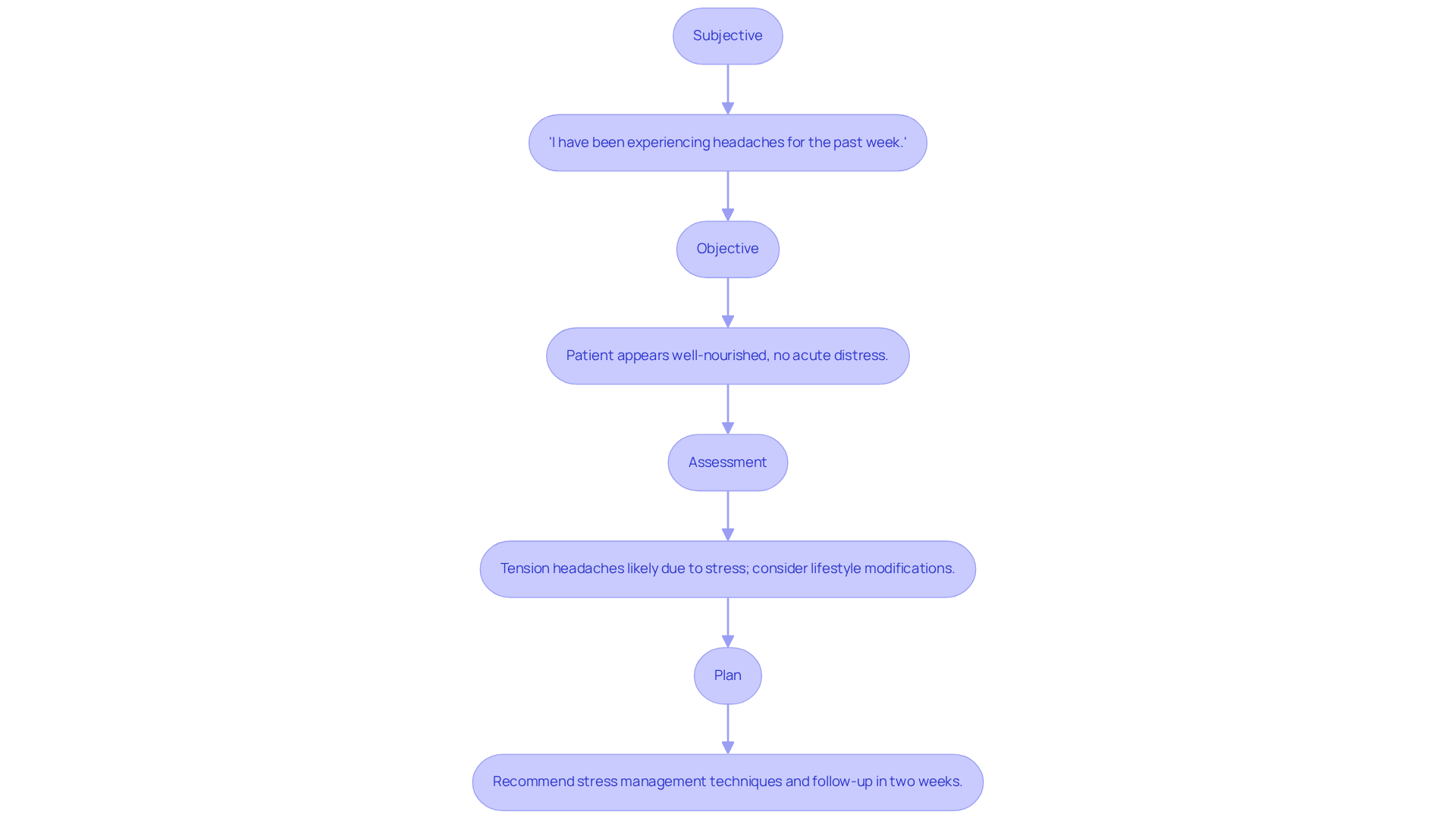
Primary Care SOAP Note Example: Ensuring Continuity of Care
In primary care, a [soap note example nurse practitioner](https://blog.cosmaneura.com/10-essential-features-of-dictaphone-medical-for-healthcare-providers) begins with the Subjective section, where an individual might express, 'I have been experiencing headaches for the past week.' This is a moment to connect with the patient’s experience.
In a soap note example nurse practitioner, the Objective section captures observable findings, such as 'Patient appears well-nourished, no acute distress.' Here, we document the physical state, providing a fuller picture of the patient’s health.
The Assessment could conclude with a soap note example nurse practitioner that states, 'Tension headaches likely due to stress; consider lifestyle modifications.' This insight allows us to address the root cause compassionately.
Finally, the Plan might specify, 'Recommend stress management techniques and follow-up in two weeks,' as illustrated in the soap note example nurse practitioner.
By utilizing generative AI, healthcare providers can simplify the record-keeping process, reducing the time spent on administrative tasks like scheduling and medical record management. This improvement enhances the quality of interactions with individuals seeking care.
Imagine the relief of having more time to focus on what truly matters—your patients. This organized documentation not only supports but also enables providers to monitor progress over time. It ensures that treatment strategies align with the individual’s evolving needs.
By embracing these tools, we can nurture our relationships with patients and provide the compassionate care they deserve.
Acupuncturist SOAP Note Example: Integrating Alternative Therapies
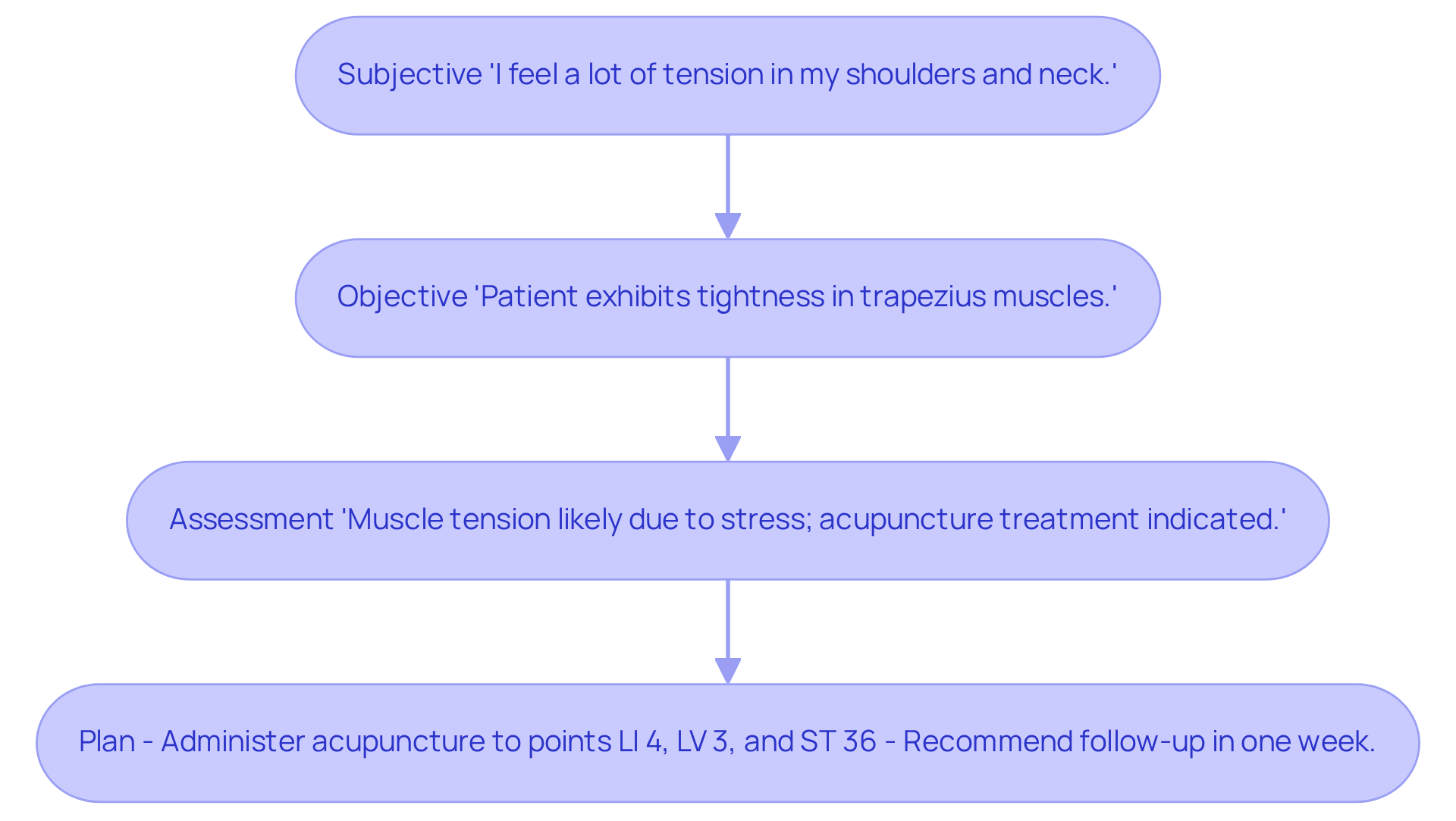
An acupuncturist's SOAP note compassionately integrates alternative therapies, beginning with the Subjective section where the individual may share, 'I feel a lot of tension in my shoulders and neck.' This personal account is crucial as it captures the and lays the groundwork for treatment.
In the Objective section, the practitioner notes observable findings, such as 'Patient exhibits tightness in trapezius muscles,' providing a factual basis for the assessment.
The Assessment might conclude with, 'Muscle tension likely due to stress; acupuncture treatment indicated,' effectively linking the subjective experience with clinical observations.
Finally, the Plan outlines specific actions:
- 'Administer acupuncture to points LI 4, LV 3, and ST 36'
- 'Recommend follow-up in one week.'
This organized approach not only ensures thorough records but also highlights the importance of alternative therapies in enhancing care outcomes. By carefully documenting these elements, practitioners can more effectively evaluate the success of alternative treatments and adjust care plans as needed.
Common SOAP Note Mistakes: Enhancing Documentation Accuracy
Frequent errors in the SOAP note example nurse practitioner records can significantly impact the care outcomes for individuals. Have you ever felt frustrated by vague language in the Subjective section, such as 'patient seems better'? This lack of specificity can lead to misunderstandings. Jess Barron emphasizes the importance of avoiding ambiguous language in records, as it undermines clinical clarity.
Moreover, incomplete data in the Objective section, such as omitted vital signs or relevant test results, compromises the quality of care provided. Neglecting to record an individual's blood pressure or lab results can obscure critical health information, potentially affecting treatment choices. To , it is essential for providers to ensure that each section of the soap note example nurse practitioner is detailed and specific, steering clear of generalizations and assumptions.
Establishing organized recording methods can lead to clearer, more succinct records. This practice ultimately enhances patient outcomes and promotes improved communication among healthcare teams. Consider utilizing tools like Yung Sidekick, which can produce progress records 90% quicker, improving efficiency in documentation.
Additionally, maintaining audit-ready documentation safeguards against compliance issues, highlighting the legal significance of precise records. Continuous education is vital for improving documentation quality through regular training sessions, ensuring that healthcare providers remain informed about best practices. Let’s work together to create a more effective documentation process that supports both providers and patients alike.

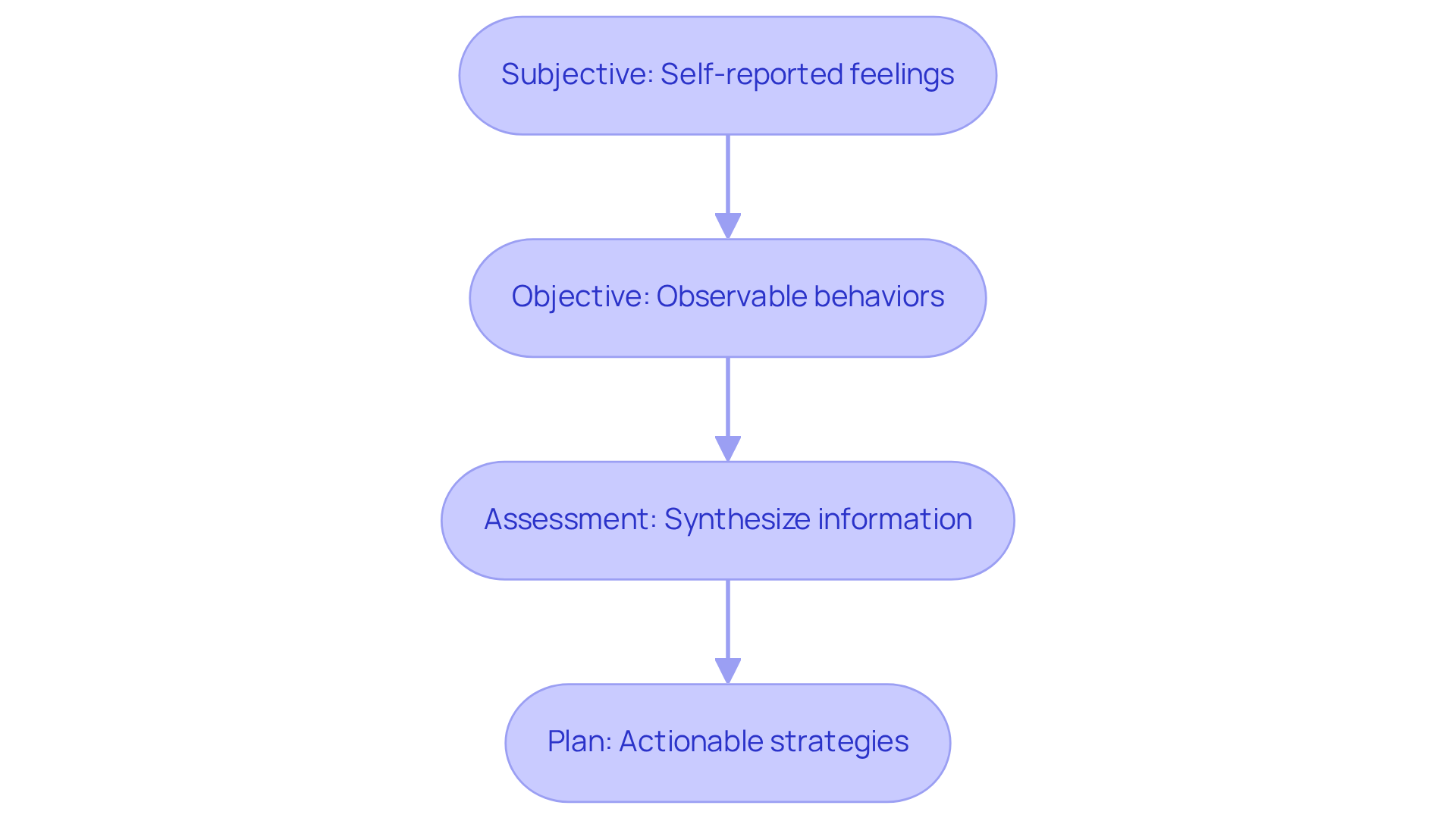
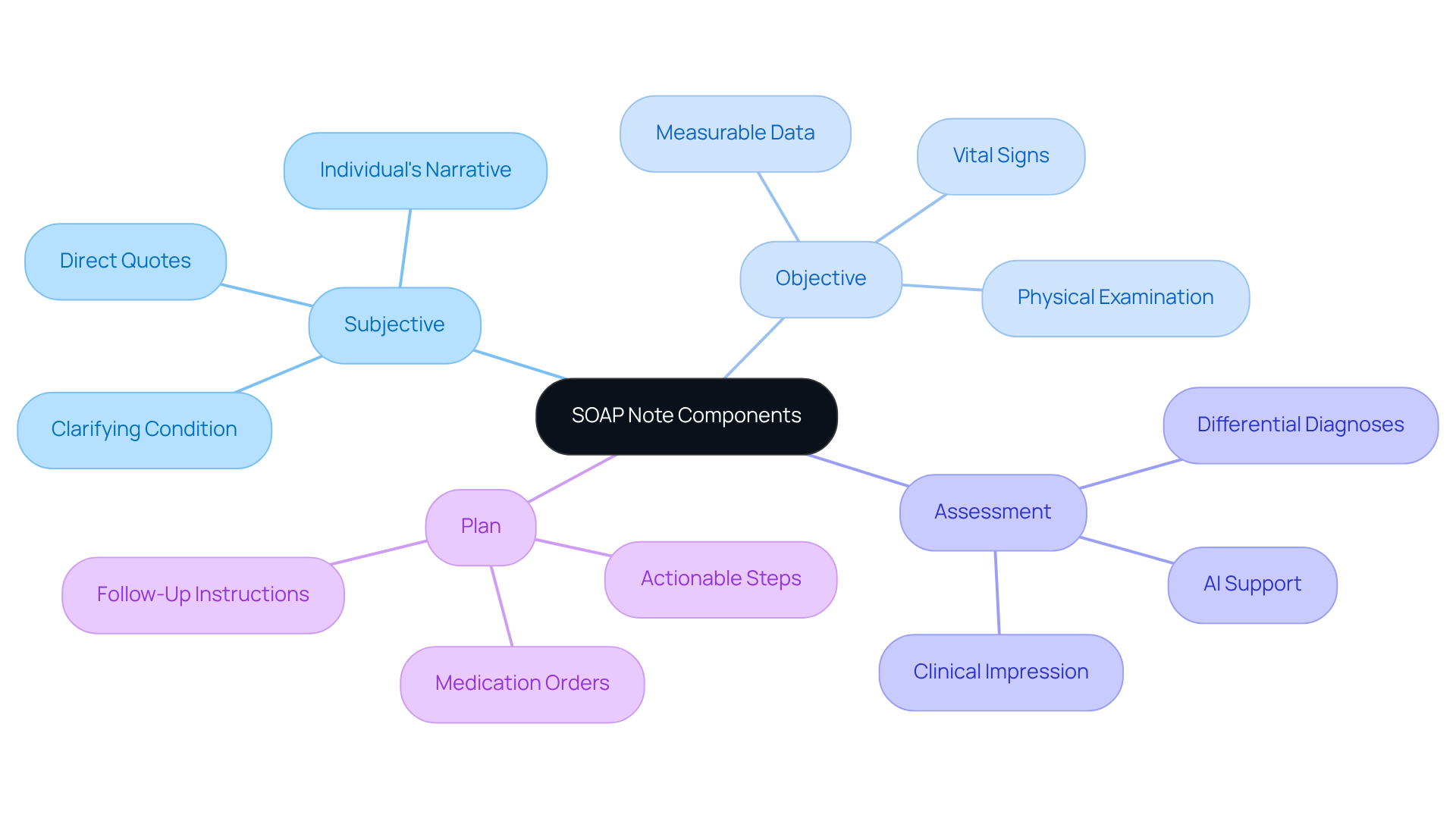
Key Components of a SOAP Note: Structuring Effective Documentation
An example of a soap note for a nurse practitioner is structured around four essential components: Subjective, Objective, Assessment, and Plan. The Subjective section captures the individual's narrative, detailing their symptoms, concerns, and experiences, which are vital for understanding their perspective. Have you ever considered how incorporating direct quotes from individuals can improve the credibility of the records? This approach not only clarifies their condition but also honors their voice.
The Objective section presents measurable data, such as vital signs and physical examination findings. These details are crucial for establishing a factual basis for clinical decisions. Precise documentation of these observations plays a significant role in the overall evaluation of the individual's health, ensuring that every aspect is considered.
In a soap note example nurse practitioner, the Assessment component synthesizes information from both the Subjective and Objective sections. This allows clinicians to formulate a clinical impression and prioritize differential diagnoses, which is essential for effective treatment planning. With the assistance of AI algorithms, healthcare providers can analyze vast amounts of medical data, including medical history and test results. This support aids in making precise diagnoses and developing , ultimately enhancing diagnostic accuracy and improving outcomes for individuals.
Finally, the Plan section serves as a soap note example nurse practitioner by outlining actionable steps for care, including immediate interventions, medication orders, and follow-up instructions. By utilizing generative AI, physicians can simplify administrative tasks such as appointment scheduling and billing. This enables them to focus more on meaningful interactions with clients. Clear and measurable plans not only enhance participant engagement but also ensure accountability in follow-up actions. By mastering the format of clinical documentation and incorporating AI tools, healthcare professionals can significantly improve record quality and operational efficiency, ultimately leading to better care outcomes for individuals. What steps can you take today to integrate these practices into your routine?
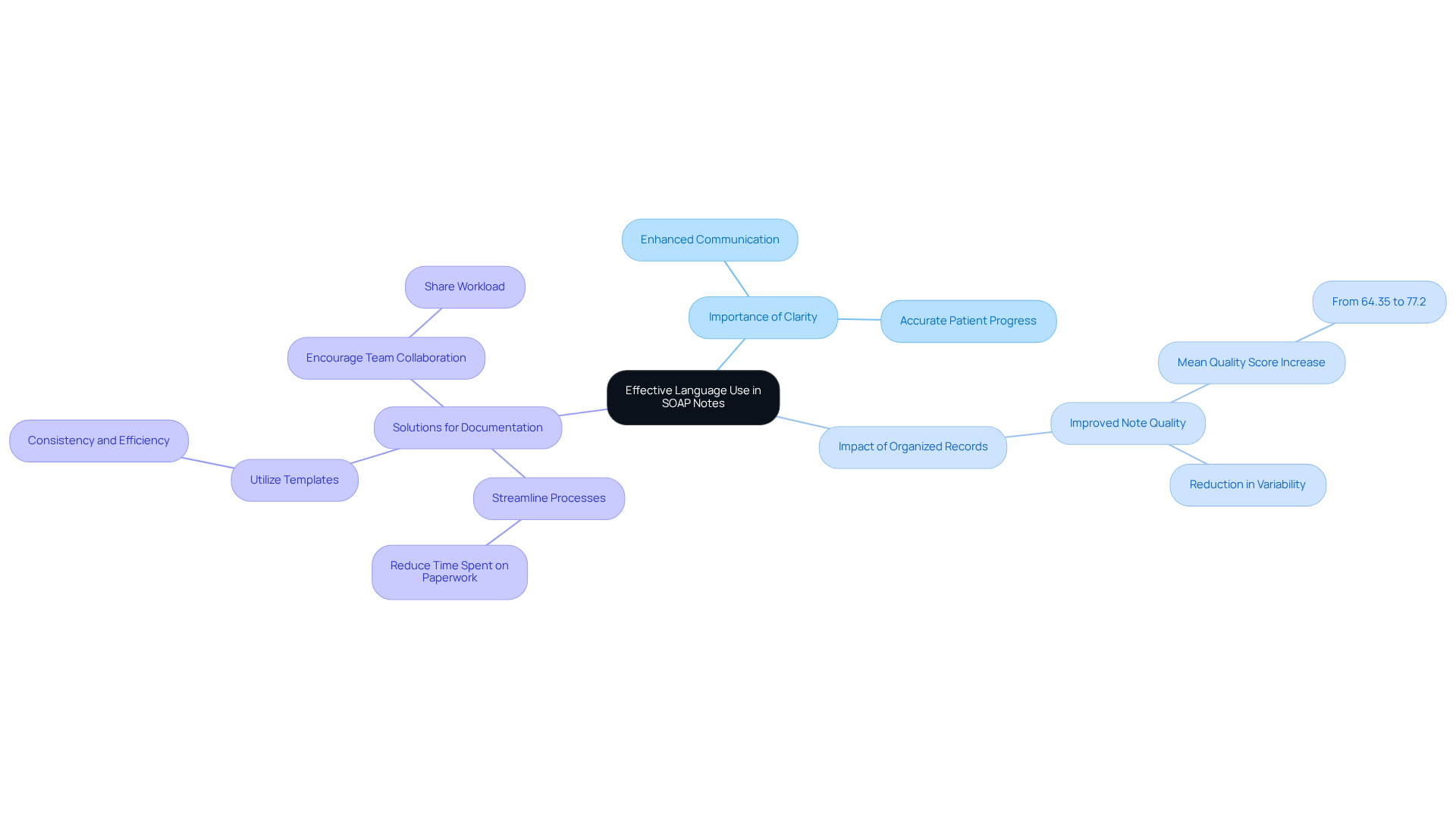
Effective Language Use in SOAP Notes: Clarity and Precision
Effective language use in a soap note example nurse practitioner is crucial for enhancing clarity and precision in patient care. Have you ever felt overwhelmed by the jargon and vague terms that can cloud communication? Instead, let’s focus on using clear and specific descriptions that truly reflect the individual’s condition. For instance, instead of saying 'patient is better,' specify 'patient reports a decrease in pain from 8/10 to 4/10.' This degree of detail not only enhances communication among healthcare professionals but also ensures an accurate recording of the individual’s progress in a soap note example nurse practitioner context.
Research shows that organized records can significantly improve note quality, with average scores rising from 64.35 to 77.2 following implementation. This highlights the importance of clarity in healthcare records. Transparent records greatly improve communication with individuals, allowing for and better health outcomes. By focusing on precise language, clinicians can effectively convey critical information, ultimately leading to better care and increased patient satisfaction.
However, it’s important to recognize that implementing structured documentation may introduce an administrative burden. Here are some key solutions to consider:
- Streamline documentation processes to reduce time spent on paperwork.
- Utilize templates for consistency and efficiency.
- Encourage team collaboration to share the workload.
By managing these challenges, we can maintain efficiency in clinical practice while providing the compassionate care our patients deserve. Let’s continue to strive for clarity in our records and communication, ensuring that every individual receives the best possible care.
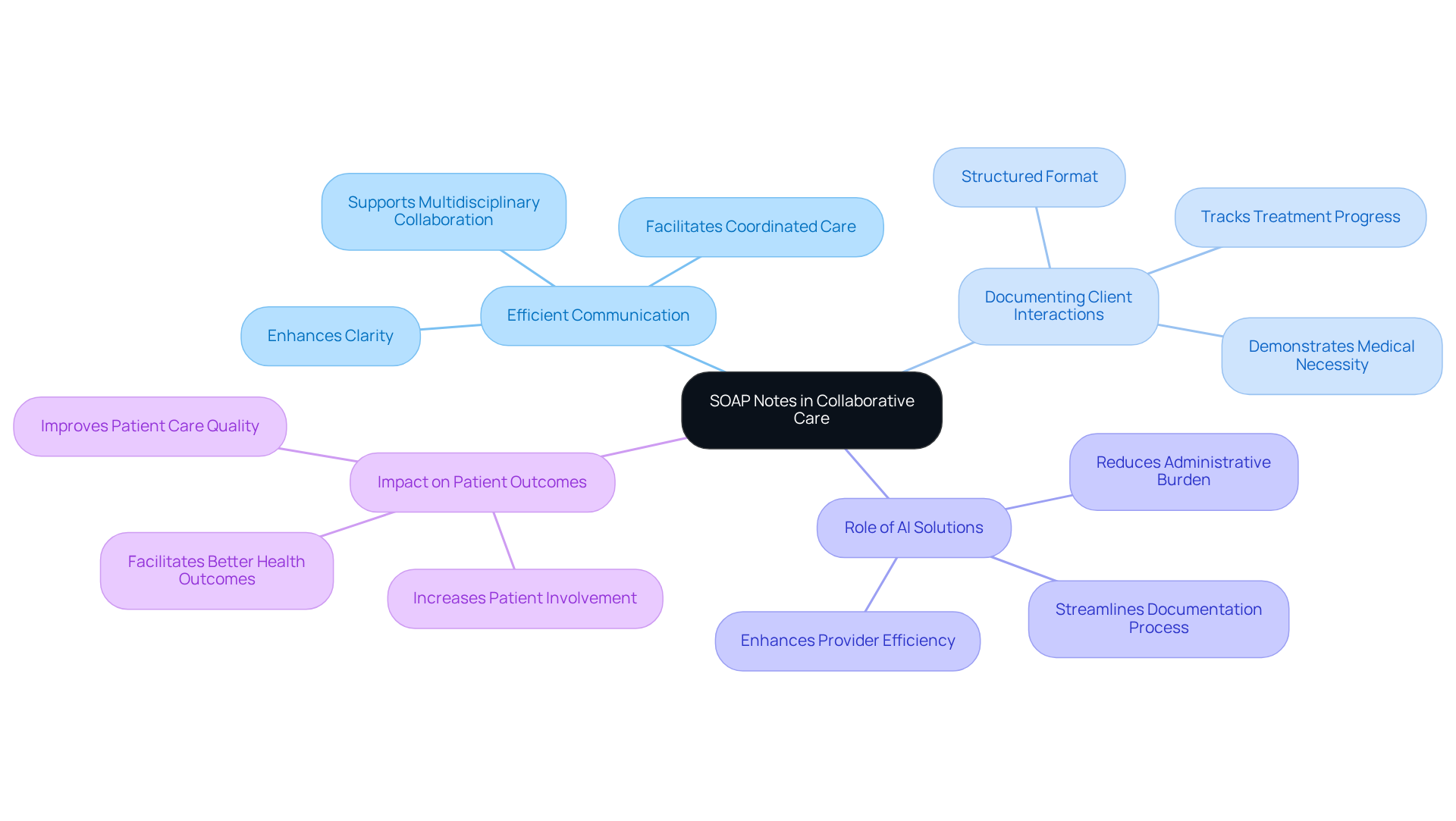
SOAP Notes in Collaborative Care: Enhancing Team Communication
In cooperative care environments, documentation plays a vital role in fostering efficient communication among team members. Have you ever considered how a [SOAP note example nurse practitioner](https://cosmaneura.com) can serve as a standardized format for documenting client interactions and transform your practice? By sharing critical information seamlessly, healthcare providers can monitor progress more effectively. For example, when a mental health professional documents an individual's therapy session using structured formats, this record becomes easily accessible to the primary care doctor. This transparency not only aligns all team members regarding the patient's condition and treatment plan but also facilitates coordinated care, ultimately enhancing patient outcomes.
The organized format of clinical documentation enhances clarity and nurtures a cooperative atmosphere where multidisciplinary groups can collaborate more effectively. Yet, we understand that can weigh heavily on healthcare providers, impacting the quality of patient care. This is where innovative AI solutions, like CosmaNeura's Agentic Platform, come into play. By streamlining SOAP note documentation, these tools specifically address the administrative challenges that arise from a SOAP note example nurse practitioner, which contribute to physician burnout and resistance to innovation.
Imagine a scenario where you can focus more on patient care, with less time spent on paperwork. By embracing these advancements, you can not only alleviate stress but also improve the overall experience for your patients. Let’s work together to explore how such solutions can enhance your practice and ultimately lead to better health outcomes for those you care for.
Conclusion
The integration of structured SOAP notes into healthcare practices significantly enhances patient care. By streamlining documentation processes and fostering effective communication among providers, we address the emotional challenges healthcare practitioners face daily. Focusing on the four essential components—Subjective, Objective, Assessment, and Plan—allows healthcare practitioners to capture each patient's narrative accurately. This leads to more personalized and compassionate care.
Throughout the article, various examples illustrate how SOAP notes can be effectively applied across different healthcare settings, from mental health to physical therapy and family medicine. The benefits of utilizing these notes are clear:
- Improved documentation accuracy
- Enhanced collaboration among multidisciplinary teams
- Ultimately, better health outcomes for patients
Moreover, incorporating AI tools like CosmaNeura can alleviate administrative burdens, allowing providers to dedicate more time to direct patient care.
As the healthcare landscape continues to evolve, embracing structured documentation methods and technological advancements will be crucial. By prioritizing clarity and precision in SOAP notes, practitioners not only improve their workflow but also reinforce the importance of compassionate, patient-centered care. This commitment to effective documentation is essential for building trust and ensuring that each individual's unique needs are met in the healthcare system. Let us continue to support one another in this journey towards improved patient care.




