Overview
The heart of this article lies in recognizing the vital SOAP note questions that can significantly enhance patient care. It compassionately underscores that structured documentation—comprising subjective, objective, assessment, and plan components—is not just a formality; it is essential for fostering effective communication, ensuring continuity of care, and ultimately improving patient outcomes. Evidence shows that this approach leads to greater precision and efficiency in clinical practices, which can alleviate some of the administrative burdens that healthcare providers often face.
Have you ever felt overwhelmed by the demands of documentation? You're not alone. Many healthcare professionals grapple with the challenge of balancing administrative tasks with the desire to provide the best care possible. By embracing the structured approach of SOAP notes, you can streamline your documentation process, allowing you to focus more on your patients and less on paperwork.
Imagine the impact of improved communication on your daily practice. When you utilize SOAP notes effectively, you not only enhance your own efficiency but also contribute to a more cohesive care experience for your patients. This, in turn, fosters trust and satisfaction, leading to better health outcomes.
We invite you to reflect on how implementing these essential SOAP note questions can transform your practice. Consider engaging with your peers or seeking additional resources to deepen your understanding. Together, we can navigate the complexities of healthcare documentation with empathy and purpose.
Introduction
In the intricate landscape of healthcare, effective communication and documentation are paramount. SOAP notes—structured records that encapsulate a patient's subjective experiences, objective findings, assessments, and plans—serve as essential tools for clinicians who are dedicated to delivering high-quality care. This article invites you to explore ten critical questions that can enhance the utility of SOAP notes, offering valuable insights into improving patient interactions and outcomes.
How can addressing these vital SOAP note questions transform the way clinicians document care and foster deeper connections with their patients? Together, let’s navigate this journey toward better communication and understanding in healthcare.
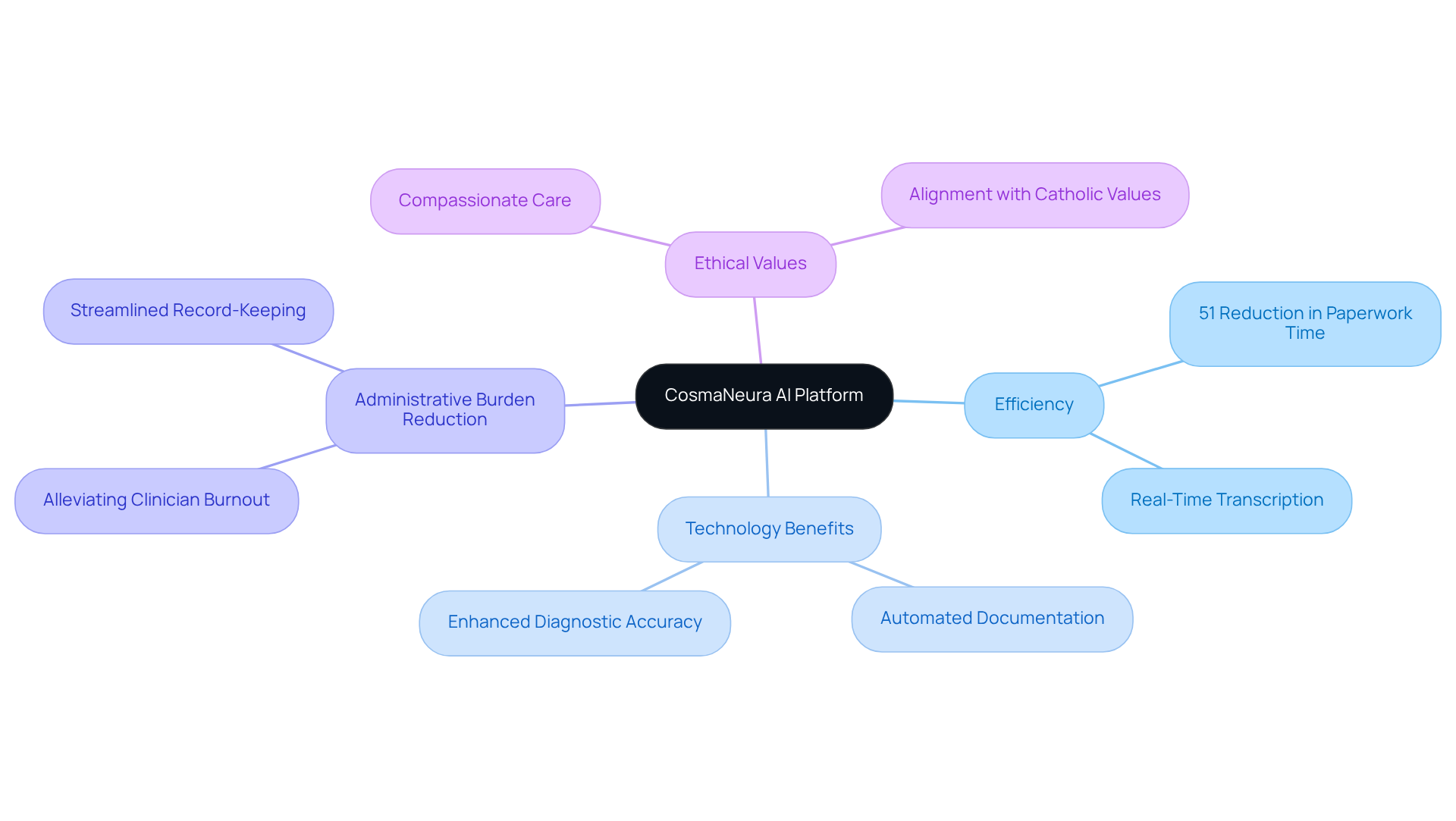
CosmaNeura: Streamline SOAP Note Documentation with AI
In today's fast-paced healthcare environment, providers often grapple with the emotional toll of administrative tasks. CosmaNeura's AI platform is designed to ease that burden by transforming the way they manage SOAP note questions through automating the documentation process. This innovation allows clinicians to dedicate more time to what truly matters: patient care.
Imagine the relief of having features like real-time transcription and summarization at your fingertips. CosmaNeura ensures that the answers to SOAP note questions are not just accurate but completed in a fraction of the time, enhancing overall efficiency in clinical settings. Recent advancements in AI technology have shown that these tools can reduce paperwork time by up to 51%. This significant reduction is crucial in alleviating the administrative pressures that often lead to clinician burnout.
More and more medical organizations are recognizing the importance of AI-driven solutions to improve their record-keeping processes. This shift leads to in client records, ultimately benefiting everyone involved. As Jesse M. Ehrenfeld, AMA Immediate Past President, highlighted, "physicians are increasingly intrigued by the assistive role of health AI and the potential of AI-enabled tools to reduce administrative burdens, enhance diagnostic accuracy, and personalize treatments."
Furthermore, CosmaNeura's commitment to upholding Catholic values ensures that its AI solutions promote ethically responsible care for individuals. This alignment with the mission of delivering compassionate medical services is more important than ever.
Are you ready to explore how CosmaNeura can support you in your journey toward more compassionate care? Let us help you focus on what truly matters—your patients.
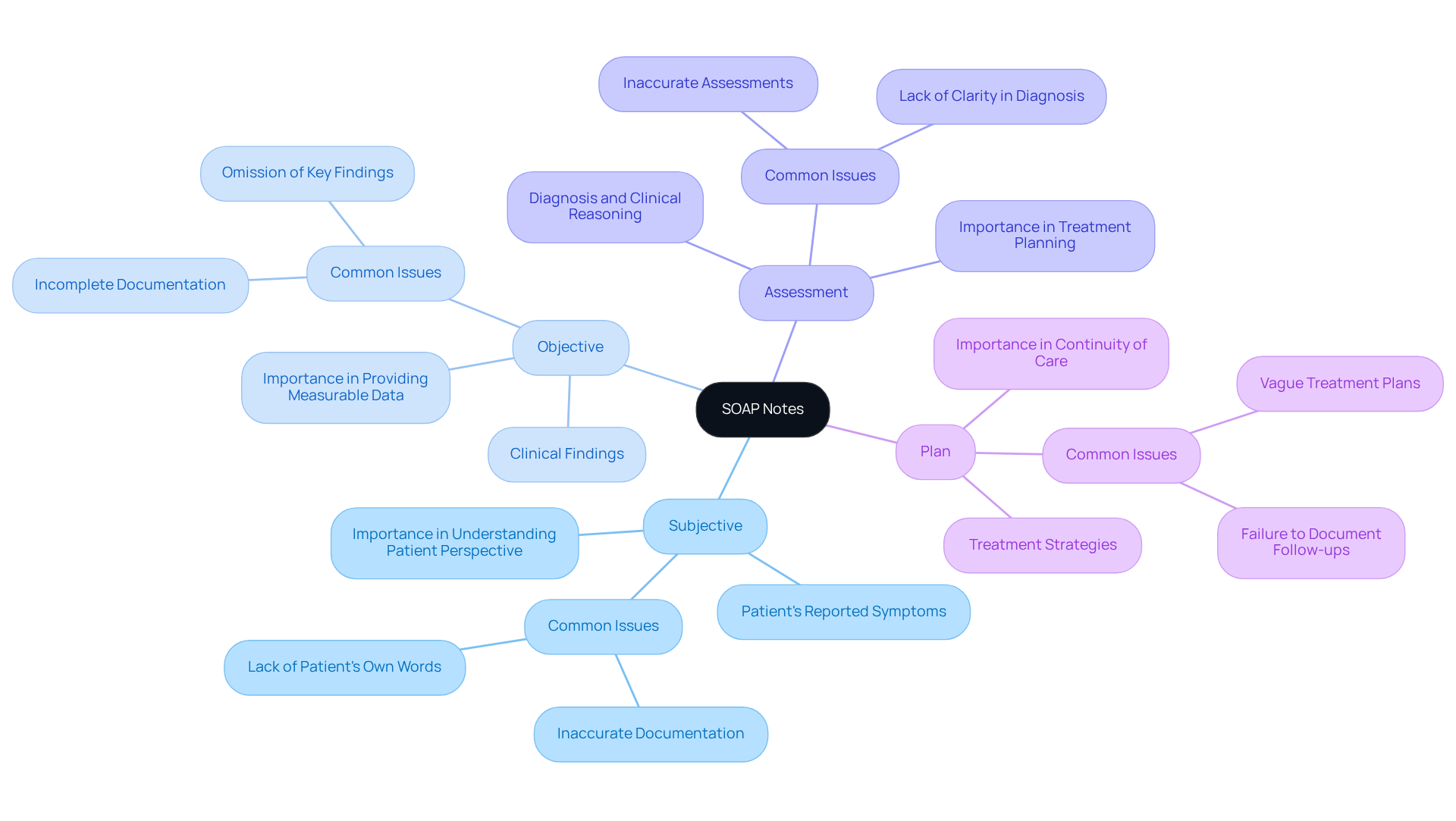
What Are SOAP Notes and Their Importance in Patient Care?
SOAP records—Subjective, Objective, Assessment, and Plan—serve as essential tools in the realm of medical documentation. They provide a structured format that not only helps clinicians capture vital details about a patient’s condition but also their treatment strategy. Have you ever felt overwhelmed by the administrative demands of your role? By maintaining clear and concise SOAP records, you can significantly improve communication and enhance safety for your patients. This approach ensures among different providers, allowing you to focus on what truly matters: your patients' well-being.
Incorporating SOAP records into your practice can alleviate some of the burdens you face daily. These records not only streamline your documentation process but also foster a collaborative environment among healthcare professionals. Imagine the peace of mind that comes with knowing that every detail of your patient’s care is accurately documented and easily accessible. By embracing this structured format, you're not just fulfilling a requirement; you're actively contributing to a safer and more effective healthcare system.
As you reflect on your current documentation practices, consider how addressing soap note questions can transform your approach to patient care. The benefits are clear: improved communication, enhanced safety, and a more cohesive treatment strategy. Let’s work together to ensure that every patient receives the care they deserve, with the support of well-organized documentation guiding the way.
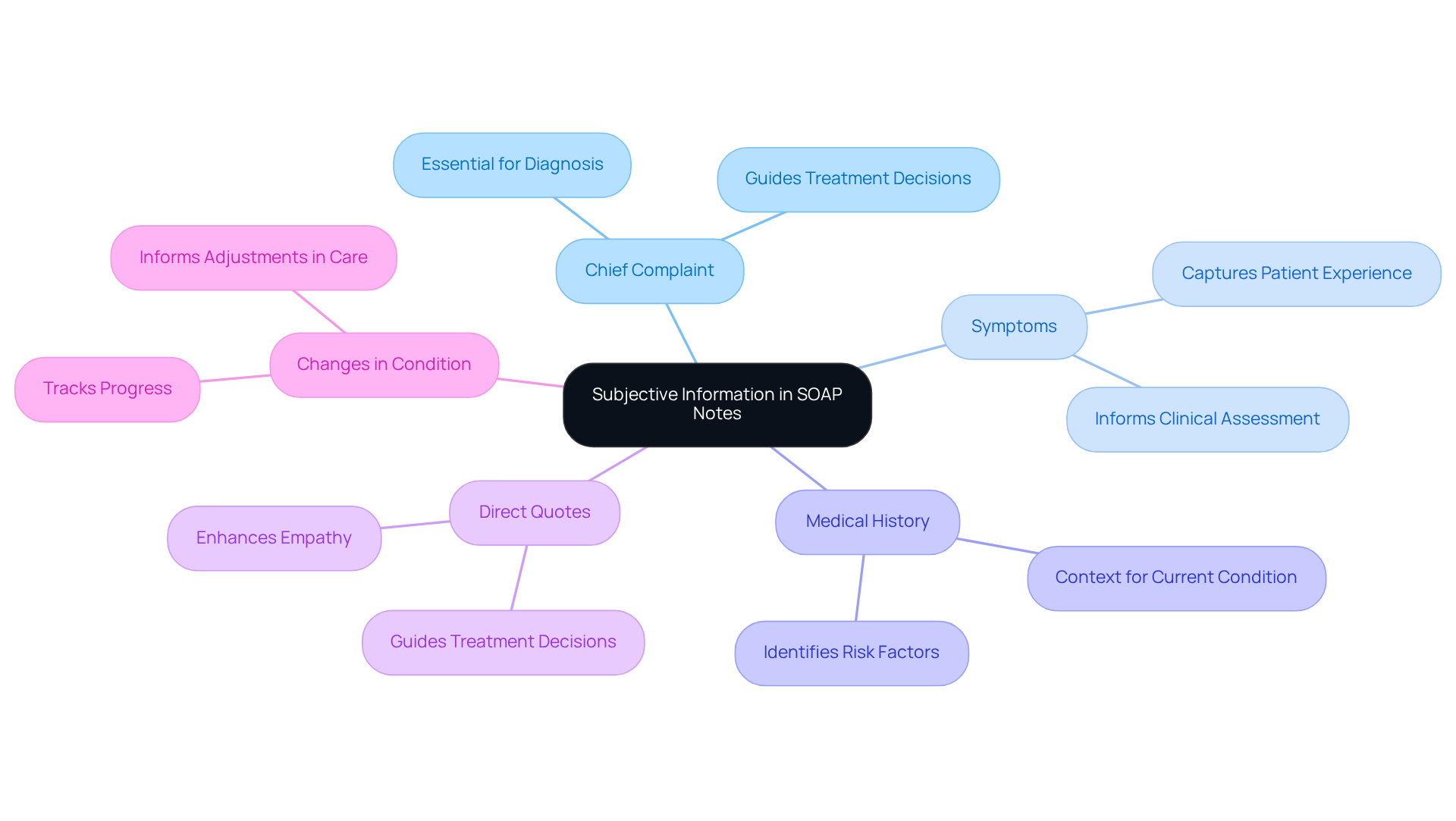
What Subjective Information Should Be Included in SOAP Notes?
In the subjective portion of soap note questions, it is essential for clinicians to document the individual's chief complaint, symptoms, and any relevant medical history. Have you ever considered how these details can shape the care you provide? Including direct quotes from the individual about their feelings or experiences, as well as any changes in their condition, can make a significant difference. This practice not only captures vital information but also fosters a deeper connection with the patient.
Accurate documentation through soap note questions is crucial for understanding the individual's perspective. By truly listening to their experiences, you can guide effective treatment decisions that resonate with their needs. Reflect on the impact this can have on your practice and the care you deliver. Engaging with patients on this level not only enhances their experience but also supports your role as a compassionate caregiver.
Ultimately, embracing this approach can . It's about creating a supportive environment where individuals feel heard and valued. As you document their stories, remember the power of empathy in your practice. Let this be a call to action to deepen your engagement with each patient, ensuring their voices are not just recorded but truly understood.
What Objective Measurements Are Necessary for Effective SOAP Notes?
In the demanding world of healthcare, answering soap note questions is essential for understanding the vital role of the objective section in patient care. It must encompass measurable data such as vital signs, physical examination findings, and diagnostic test results. These elements not only provide a factual foundation for the clinician's assessment but also enable the tracking of patient progress over time. How often do you find yourself wishing for clearer insights into a patient's condition? Recording objective measurements is crucial for informed clinical decision-making and empowers providers to modify treatment plans as necessary.
For instance, regular monitoring of vital signs—like blood pressure, heart rate, and temperature—can reveal significant health changes, guiding timely interventions. Healthy blood pressure is defined as a systolic reading of 120 or less and a diastolic reading of 80 or less. This emphasizes the importance of . Furthermore, individuals with a family history of heart disease are encouraged to check their blood pressure at least twice a year. Elevated blood pressure, often referred to as a 'silent killer' due to its lack of symptoms, highlights the importance of addressing soap note questions related to regular monitoring and recording.
Efficient documentation of these metrics not only improves care but also aids in compliance with ethical medical practices. This aligns with the compassionate spirit of healthcare, reminding us that every detail matters in the journey toward better health. Let’s commit to prioritizing these practices, ensuring our patients receive the attentive care they deserve.

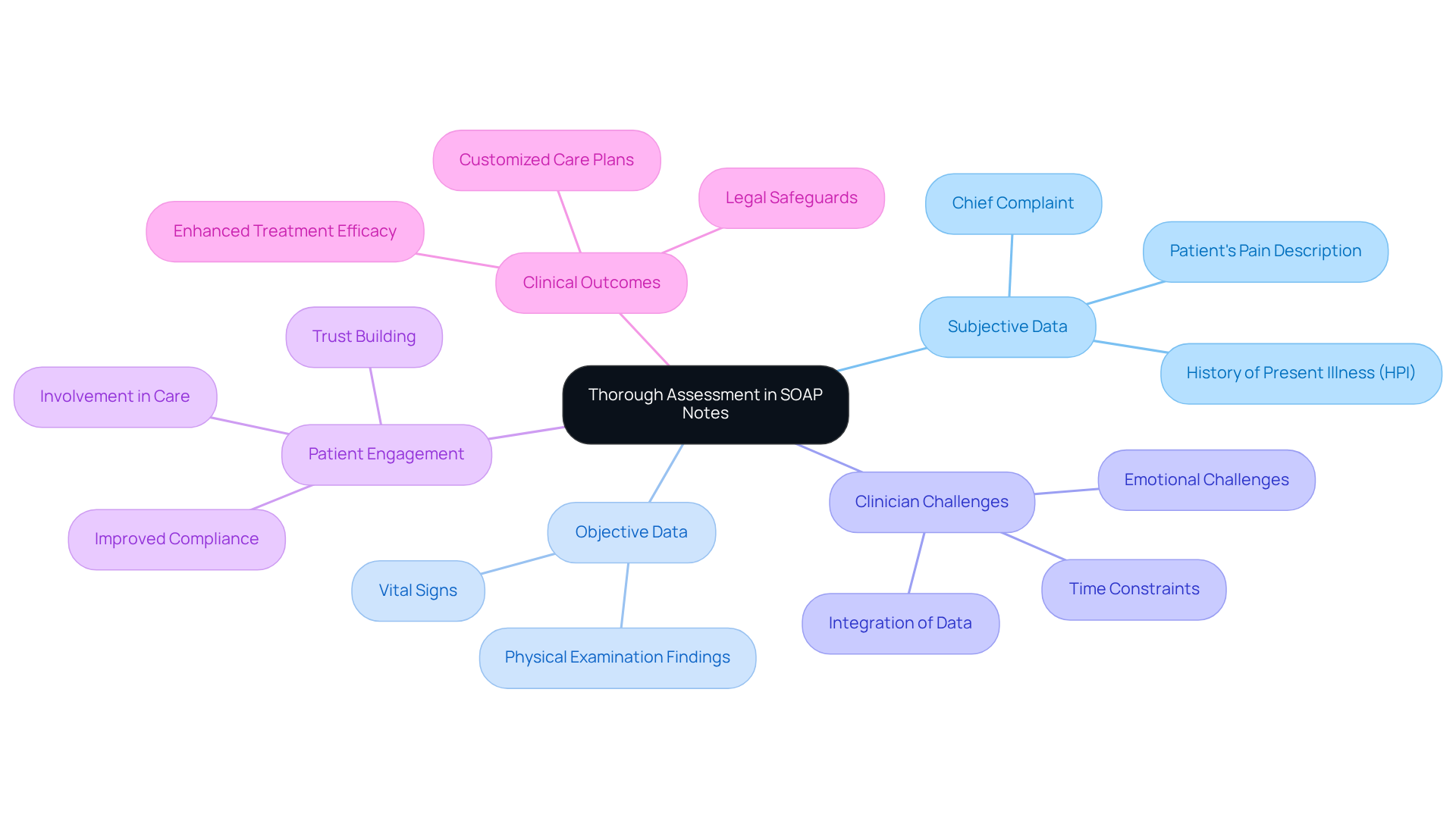
How to Conduct a Thorough Assessment in SOAP Notes?
Conducting a thorough assessment by answering soap note questions is not just a task; it’s an essential part of compassionate care. Clinicians often face emotional challenges when integrating information from both the subjective and objective sections. How do we ensure that we fully understand our patients' experiences through soap note questions? By carefully analyzing this data, we can identify patterns, potential diagnoses, and the individual's response to previous treatments.
For instance, when an individual presents with abdominal discomfort, the clinician should document the individual's description of the pain (subjective) alongside vital signs and physical examination findings (objective). This synthesis not only enhances but also informs the development of an effective treatment plan. Comprehensive evaluations are vital—they greatly influence medical outcomes by guaranteeing customized care suited to individual requirements.
Involving individuals in this process cultivates trust and enhances compliance with treatment plans. Have you noticed how this engagement can lead to improved health outcomes? Moreover, thoroughly recorded evaluations that address soap note questions offer legal safeguards for both individuals receiving care and medical practitioners, emphasizing the significance of careful record-keeping in clinical practice. By nurturing this approach, we can create a more supportive environment for everyone involved.
What Should Be Included in the Plan Section of SOAP Notes?
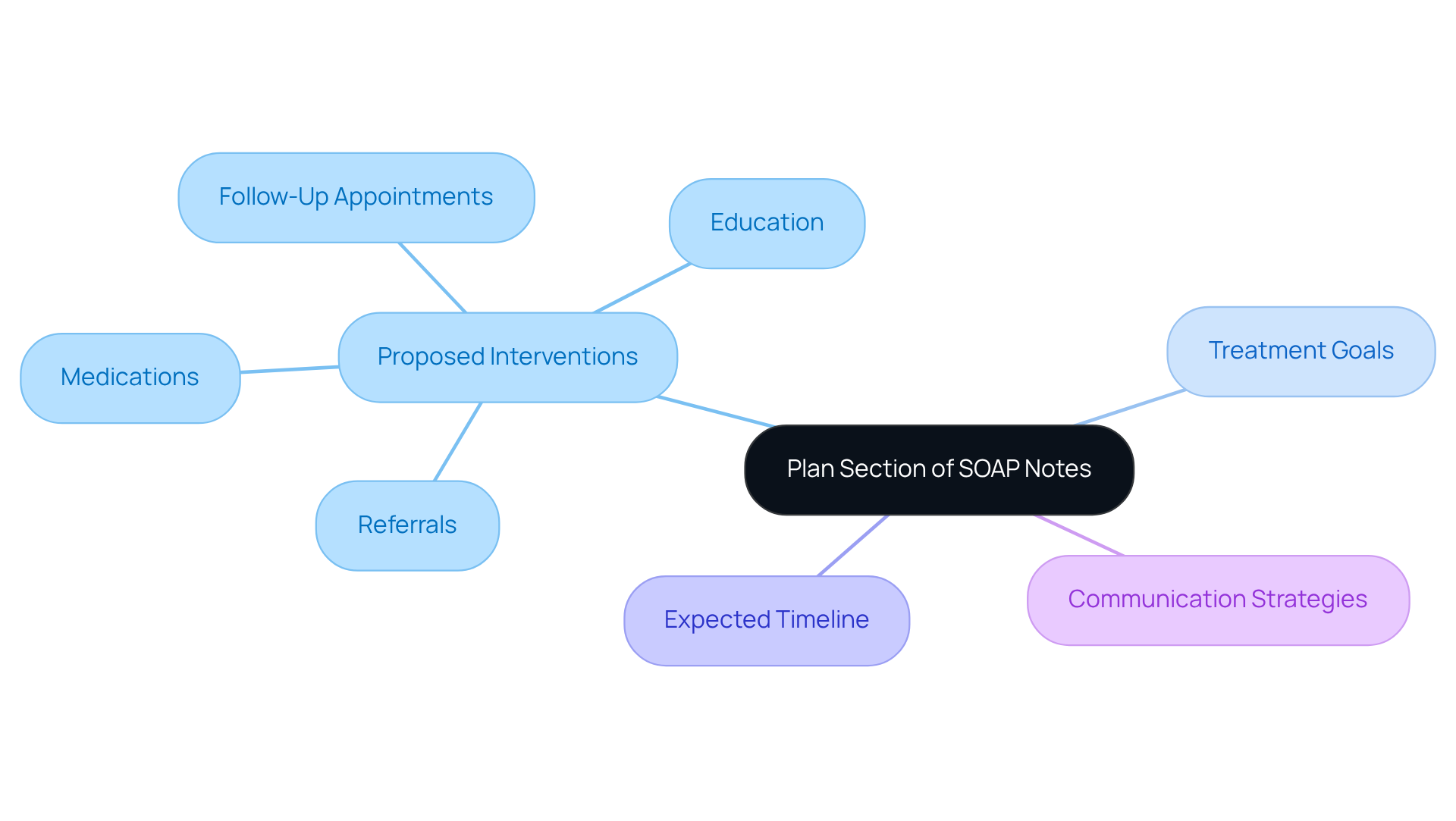
The plan section of soap note questions plays a vital role in outlining proposed interventions, including medications, referrals, follow-up appointments, and education for individuals. Have you ever considered how crucial it is to specify treatment goals and the expected timeline for achieving them in your soap note questions? Efficient record-keeping in this section is essential for addressing soap note questions, ensuring that all members of the healthcare team are informed and can collaborate seamlessly in the individual's care.
As highlighted by the WHO, increasing adherence may have a greater impact on health than any enhancement in specific medical treatments. This underscores the importance of in improving outcomes for individuals. Remember the words of former Surgeon General C. Everett Koop: "Drugs don't work in patients who don't take them." This statement emphasizes the critical nature of adherence and the role of clear communication in achieving it.
By prioritizing clear communication and addressing potential gaps among healthcare teams, we can significantly reduce misunderstandings and enhance the overall quality of care. Let’s work together to create an environment where everyone feels supported and informed, ultimately leading to better health outcomes for those we serve.
What Are Common Mistakes to Avoid When Writing SOAP Notes?
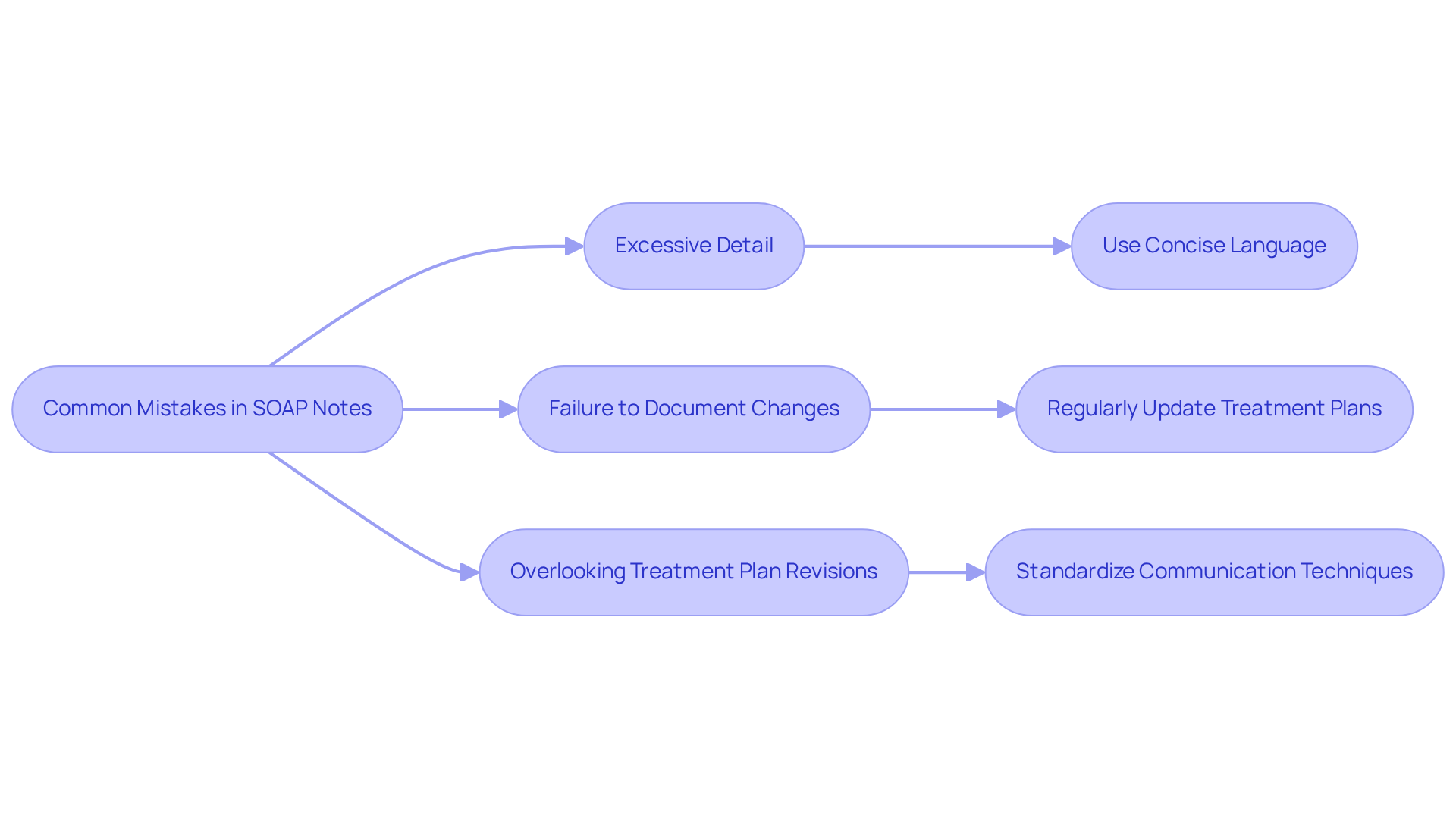
When writing SOAP notes, clinicians often encounter soap note questions that highlight emotional challenges, potentially compromising clarity and effectiveness. It’s crucial to be aware of common pitfalls related to soap note questions, such as providing excessive detail that obscures vital information or failing to document changes in a patient’s condition. Have you ever overlooked the need to revise a treatment plan based on new findings? This can lead to misunderstandings among healthcare professionals, ultimately affecting patient care. Given that medical mistakes rank as the third leading cause of death, precise record-keeping becomes essential.
To , practitioners should focus on using concise, specific language. Each section of the SOAP note questions—Subjective, Objective, Assessment, and Plan—should clearly convey the relevant information required. For instance, instead of stating 'the individual feels better,' a more precise note would be 'the individual reports a decrease in pain from 8/10 to 4/10.' Implementing standardized communication techniques can further improve clarity.
By steering clear of these frequent errors, healthcare providers can significantly enhance the quality of their records. This not only leads to better patient outcomes but also reduces the financial repercussions of record-keeping errors, which contribute to an estimated $68 billion in mistakes on medical bills each year.
Here are some key solutions to consider:
- Use concise language that captures the essence of the patient’s condition.
- Regularly update treatment plans based on new insights.
- Standardize communication techniques to foster clarity.
By embracing these practices, you can navigate the complexities of record-keeping with greater confidence and compassion.
How Can Templates Improve SOAP Note Efficiency?
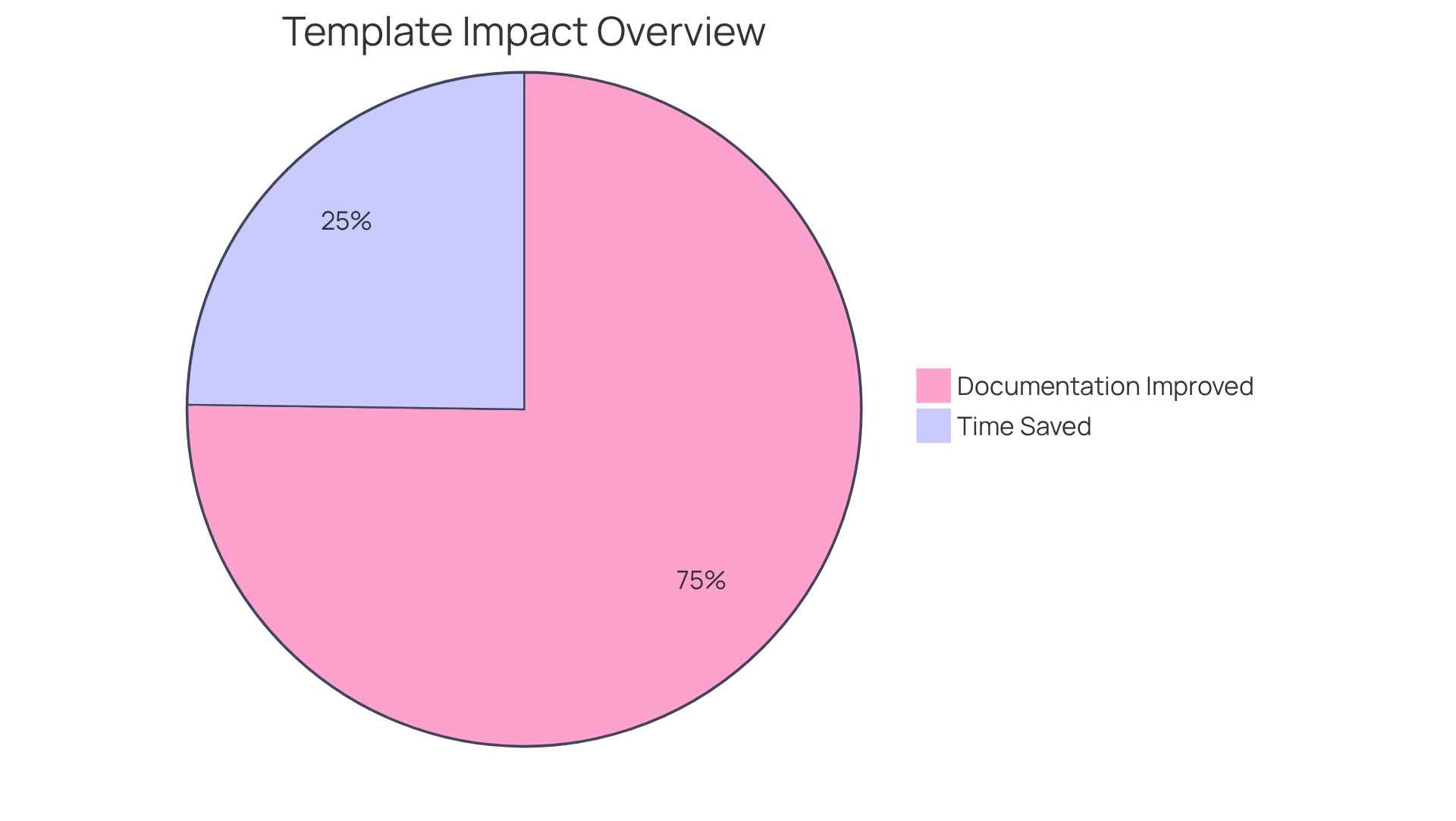
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to deliver compassionate patient care. Utilizing offers a structured format that not only streamlines documentation but also alleviates some of this stress. Research shows that standardized documentation practices can lead to significant time savings. For instance, after implementing templates, the average total admission record time decreased from 97.9 minutes to 71.0 minutes, a remarkable 28% reduction. This newfound efficiency allows healthcare providers to dedicate more time to their clients, enhancing the quality of care.
Moreover, templates ensure that all vital elements of the SOAP document are consistently recorded, which is essential for addressing soap note questions and maintaining high-quality patient records. A study revealed that introducing standardized templates improved compliance with quality metrics without increasing the time spent on notes. For example, the percentage of complete neurovascular examinations documented soared from 3.6% in the pre-template group to an impressive 85.0% in the template group. This improvement not only reflects better record-keeping but also fosters a culture of thoroughness and consistency in patient care.
Experts in the healthcare field underscore the importance of standardization in record-keeping. Nancy H. Miller, MD, noted that standardized EMR templates can elevate the quality of clinical records and enhance communication among providers. This sentiment resonates with many healthcare professionals who have found that templates simplify the completion of clinic records and encourage inquiries about significant issues, ultimately leading to better care for clients.
In conclusion, incorporating templates into SOAP practices while addressing soap note questions not only streamlines the recording process but also cultivates an environment of meticulousness and consistency, which can significantly improve patient outcomes. However, it's important to recognize that while templates enhance efficiency, challenges such as time constraints and incomplete records still exist in achieving optimal reporting. By addressing these obstacles together, we can continue to strive for excellence in patient care.
How Can Technology Enhance SOAP Note Documentation?
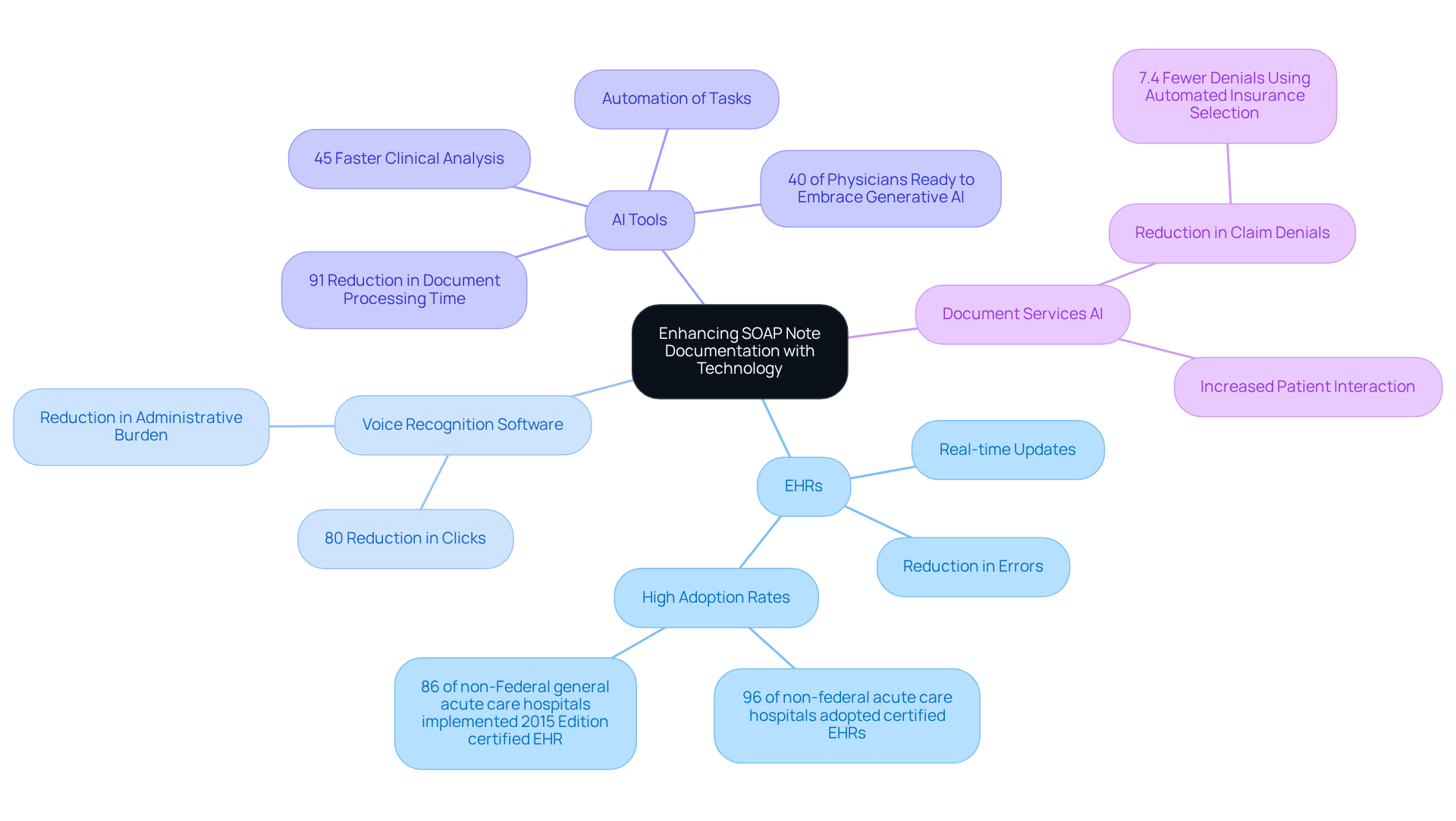
In the demanding world of healthcare, technology serves as a vital ally in enhancing SOAP note recording. The integration of electronic health records (EHRs), voice recognition software, and AI-driven tools addresses the emotional challenges faced by providers, simplifying data entry and reducing errors. These innovations allow for real-time updates to medical records, which can alleviate the stress of administrative tasks and improve patient care.
Consider this: as of 2021, nearly 96% of non-federal acute care hospitals had adopted certified EHRs, with 86% of non-Federal general acute care hospitals implementing a 2015 Edition certified EHR. This widespread reliance on digital documentation underscores the collective movement towards more . AI tools, in particular, can automate repetitive tasks, enabling medical providers to focus on what truly matters—caring for individuals.
In fact, practices utilizing Document Services AI have reported an impressive 91% reduction in document processing time. Imagine the relief and increased capacity for patient interaction that such efficiency can bring. Furthermore, 40% of U.S. physicians are ready to embrace generative AI in their interactions with patients this year, highlighting a growing acceptance of these supportive technologies.
By embracing these advancements, medical professionals can significantly enhance the precision and effectiveness of SOAP note questions. This ultimately leads to improved outcomes and greater satisfaction for individuals. As Maury Brown insightfully noted, "more small practices are adopting AI-powered tools to streamline the administrative tasks that hinder them." This observation emphasizes the transformative potential of AI in the medical field, inviting healthcare providers to explore how these tools can support their mission of delivering compassionate care.
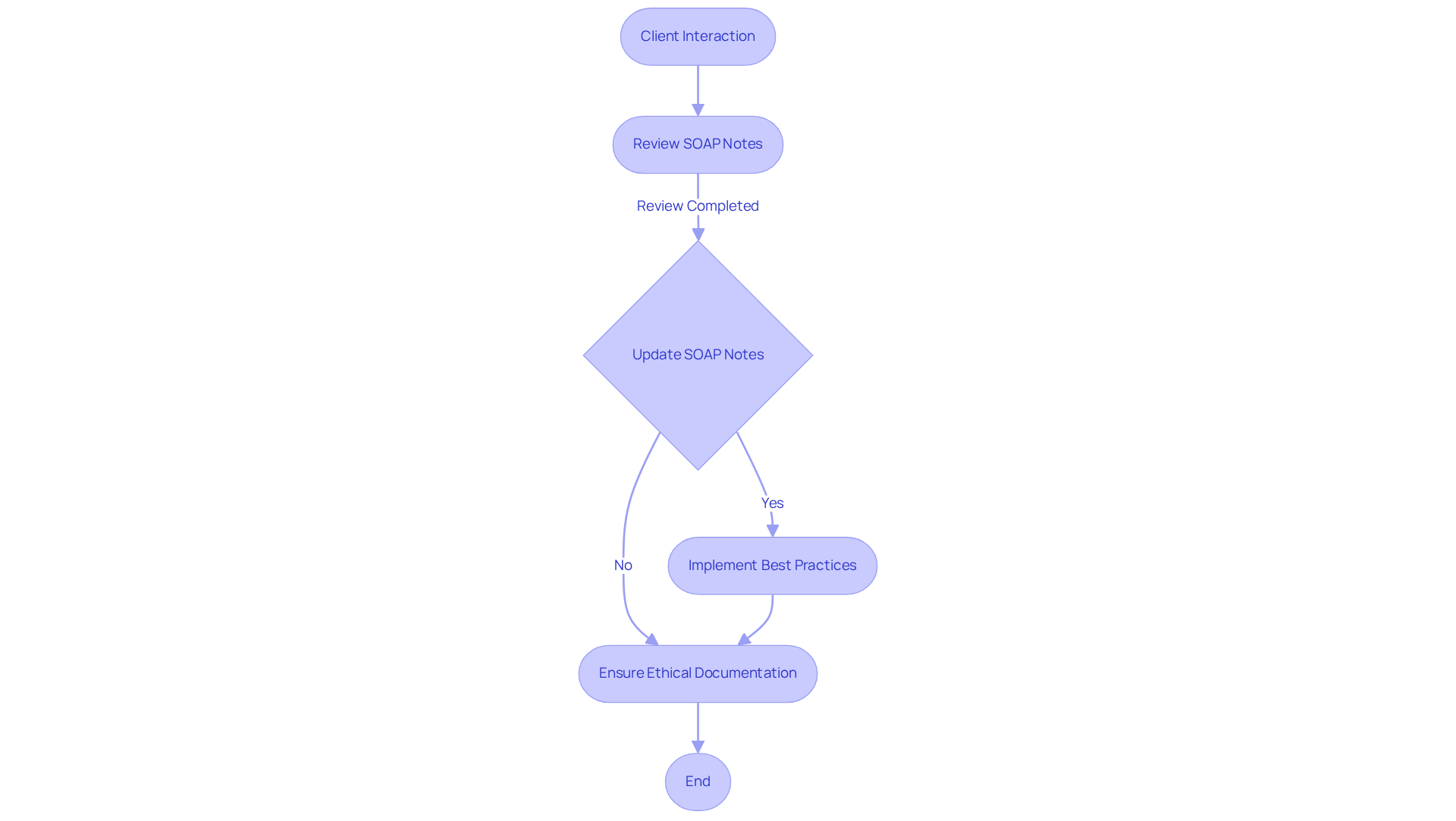
How Often Should SOAP Notes Be Reviewed and Updated?
Consistently reviewing and updating soap note questions is crucial, ideally after each client interaction or whenever there is a notable change in the individual's condition. Have you considered how answering soap note questions not only guarantees that records accurately reflect the individual's condition and treatment strategy but also enhances communication among healthcare professionals? Statistics reveal that can lead to increased reimbursement rates and improved outcomes for individuals. For instance, health professionals utilizing electronic systems are 2.2 times more likely to effectively document their routine practices.
Moreover, routine record evaluations help identify missing details, fostering a culture of continuous improvement in healthcare. Documentation practices should center around the patient and adhere to ethical standards, aligning with the mission of providing compassionate care. By embracing these best practices, healthcare providers can ensure that their documentation remains current, comprehensive, and ethically aligned, ultimately enriching the quality of care delivered to patients. How might you implement these strategies to enhance your practice and support your patients better?
Conclusion
Integrating effective SOAP note practices is not just a procedural necessity; it’s a vital step towards enhancing patient care and improving clinical outcomes. Have you felt the weight of administrative burdens impacting your time with patients? By focusing on structured documentation, healthcare providers can streamline their processes, allowing more time for meaningful patient interactions. Advances in technology, especially through platforms like CosmaNeura, can significantly alleviate the documentation load, reducing the administrative strain that often leads to clinician burnout.
Throughout this article, we’ve explored the key aspects of SOAP notes—from the importance of subjective and objective data to conducting thorough assessments and formulating clear treatment plans. Each section plays a pivotal role in ensuring that patient records are comprehensive, facilitating seamless communication among healthcare professionals. Recognizing common mistakes and implementing standardized templates can further enhance clarity and effectiveness in documentation.
Ultimately, embracing these practices fosters a more compassionate healthcare environment and reinforces our commitment to delivering high-quality care. As the healthcare landscape evolves, leveraging technology and adhering to best practices in SOAP note documentation will be crucial in ensuring that patients receive the attentive and informed care they deserve. It’s time for healthcare providers to prioritize these strategies, transforming their documentation approach and leading to improved patient outcomes and satisfaction. Let’s take this journey together, nurturing our commitment to excellence in patient care.




