Overview
This article addresses the emotional challenges faced by healthcare providers, particularly in the realm of clinical documentation. It highlights the significance of SOAP notes in speech therapy, emphasizing how they can alleviate some of the administrative burdens that often detract from patient care. Structured SOAP notes not only enhance communication among healthcare providers but also ensure compliance with legal standards, ultimately leading to improved patient outcomes.
Consider this: when documentation is clear and organized, it fosters better collaboration among team members. The detailed capture of client progress and treatment plans allows for a more comprehensive understanding of patient needs. This clarity is essential for delivering the best possible care, as it empowers providers to make informed decisions based on accurate information.
Incorporating SOAP notes into your practice can be a transformative step. Not only do they streamline communication, but they also serve as a vital tool in documenting patient journeys. By embracing this structured approach, you can significantly enhance the quality of care you provide.
Let’s reflect on the benefits:
- Improved communication among healthcare providers.
- Compliance with legal standards.
- Enhanced patient care through detailed documentation.
As you consider these advantages, remember that implementing SOAP notes is not just about meeting requirements; it’s about fostering a supportive environment for both providers and patients. We encourage you to explore the integration of SOAP notes in your practice to experience these benefits firsthand.
Introduction
In the realm of speech therapy, effective documentation transcends a mere routine task; it stands as a cornerstone of quality care. Many healthcare providers face the emotional challenge of balancing meticulous record-keeping with the need to prioritize patient interactions. This dual burden can often feel overwhelming, impacting the quality of care provided.
This article explores ten essential SOAP note examples designed to streamline documentation and enhance the therapeutic process. How can these structured notes not only transform the way therapists communicate progress and treatment plans but also ensure compliance while fostering meaningful connections with clients? By embracing these strategies, therapists can alleviate some of the administrative pressures they face, allowing them to focus more on what truly matters—their patients.
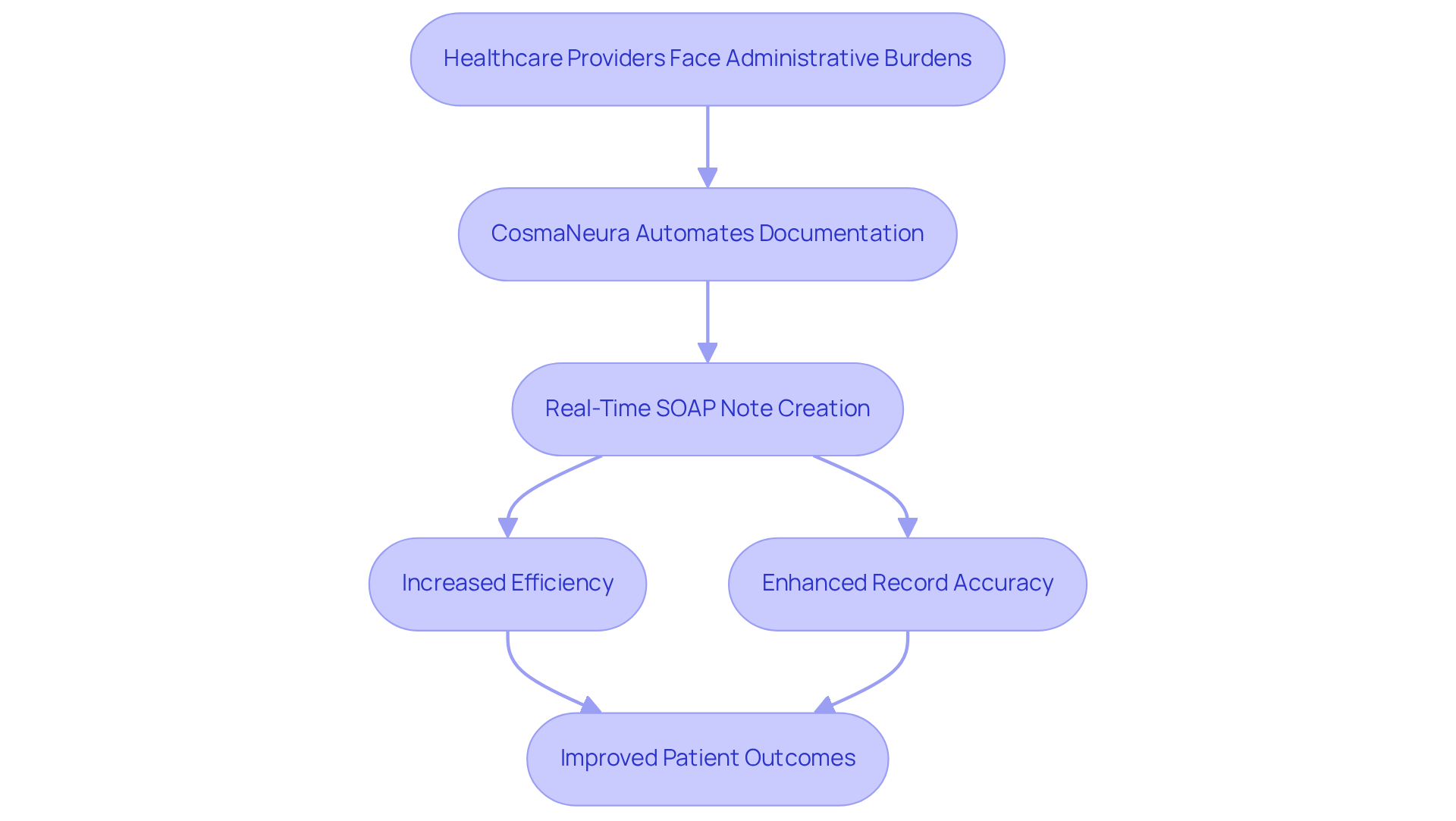
CosmaNeura: AI-Powered SOAP Note Automation for Speech Therapy
Healthcare providers often face overwhelming administrative burdens that can detract from the quality of patient care. CosmaNeura understands these challenges and utilizes advanced AI technology to automate the creation of documentation, including a speech therapy soap note example, for providers. By simplifying the record-keeping process, this innovative platform allows clinicians to focus more on what truly matters: meaningful interactions with their clients.
Imagine being able to create a speech therapy soap note example in real-time during therapy sessions. This approach captures essential details effortlessly, ensuring that continuous care is maintained. Not only does this increase efficiency, but it also enhances record accuracy, enabling providers to uphold exceptional care standards while adhering to ethical guidelines.
The automation of clinical documentation can save healthcare professionals significant time, allowing them to reclaim hours that were once lost to paperwork. This recovery of time can lead to enhanced job satisfaction and improved overall patient outcomes. By addressing physician burnout and enhancing administrative efficiency, CosmaNeura is paving the way for a more patient-centric healthcare delivery model.
Are you ready to transform your practice? Embrace the opportunity to focus on your clients and elevate your care standards with CosmaNeura. Together, we can create a more compassionate and .
Medesk: Comprehensive Guide to Writing Speech Therapy SOAP Notes
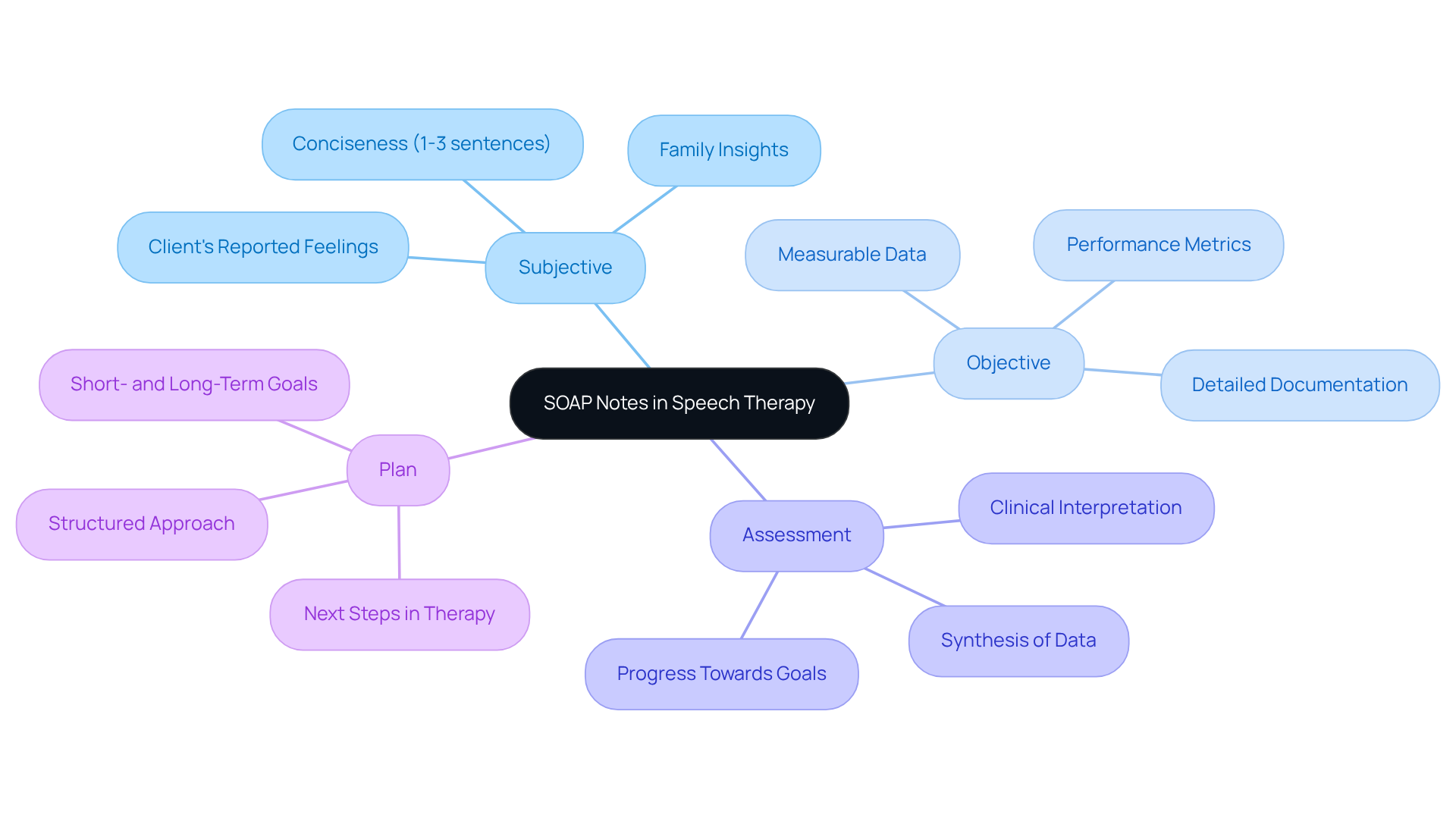
Effective clinical records, such as a speech therapy soap note example, are vital for speech therapy, fostering clarity and adherence to professional standards. Each component—Subjective, Objective, Assessment, and Plan—plays a crucial role in capturing the client's progress and treatment needs.
- Subjective: This section encompasses the client's reported feelings, symptoms, and any relevant insights from family members. Keeping it concise, ideally 1-3 sentences, helps maintain focus on the client's current state. How often do we find ourselves overwhelmed by the details?
- Objective: Here, measurable data is documented, such as performance metrics and specific behaviors observed during the session. This section should be the most detailed, providing quantifiable evidence of the client's progress, including percentages and accuracy levels. Isn't it reassuring to see tangible proof of improvement?
- Assessment: This component synthesizes information from the Subjective and Objective sections, offering a clinical interpretation of the client's status. It should reflect any changes in the treatment plan and highlight progress towards goals. Reflecting on this can be pivotal in understanding our clients' journeys.
- Plan: The Plan outlines the next steps in therapy, including short- and long-term goals. It should specify what will be addressed in future sessions, ensuring a structured approach to ongoing treatment. What can we do to ensure our clients feel supported in their progress?
Optimal methods for composing SOAP entries involve utilizing a speech therapy soap note example to , ensuring that writings are distinct for each session to prevent generic entries that could raise concerns during insurance evaluations. Furthermore, completing records right after sessions enhances precision and detail retention, aiding prompt reimbursement and efficient communication among healthcare providers. By following these guidelines, speech therapists can produce thorough and justifiable records that support quality patient care. Let’s embrace these practices together, ensuring our clients receive the best care possible.
Mentalyc: 15 SOAP Note Examples and Templates for Effective Documentation
In the demanding world of healthcare, providers often face emotional challenges, especially when it comes to documentation. Mentalyc understands these struggles and offers a comprehensive collection of 15 speech therapy SOAP note examples and templates, including a detailed speech therapy SOAP note example. These templates cover various scenarios, from initial assessments to progress notes, addressing the administrative burdens that can detract from patient care.
Imagine how much simpler your record-keeping process could be. By adopting these structured formats, such as a speech therapy SOAP note example, you can ensure that all essential information is captured accurately and efficiently. This not only streamlines your workflow but also significantly enhances your documentation efficiency, leading to better outcomes for the individuals you serve.
Effective documentation is crucial. It fosters clear communication among healthcare teams, ultimately enhancing care and engagement for individuals. By embracing these tools, you can focus more on what truly matters—providing compassionate and effective care. We invite you to and see how they can support you in your important work.
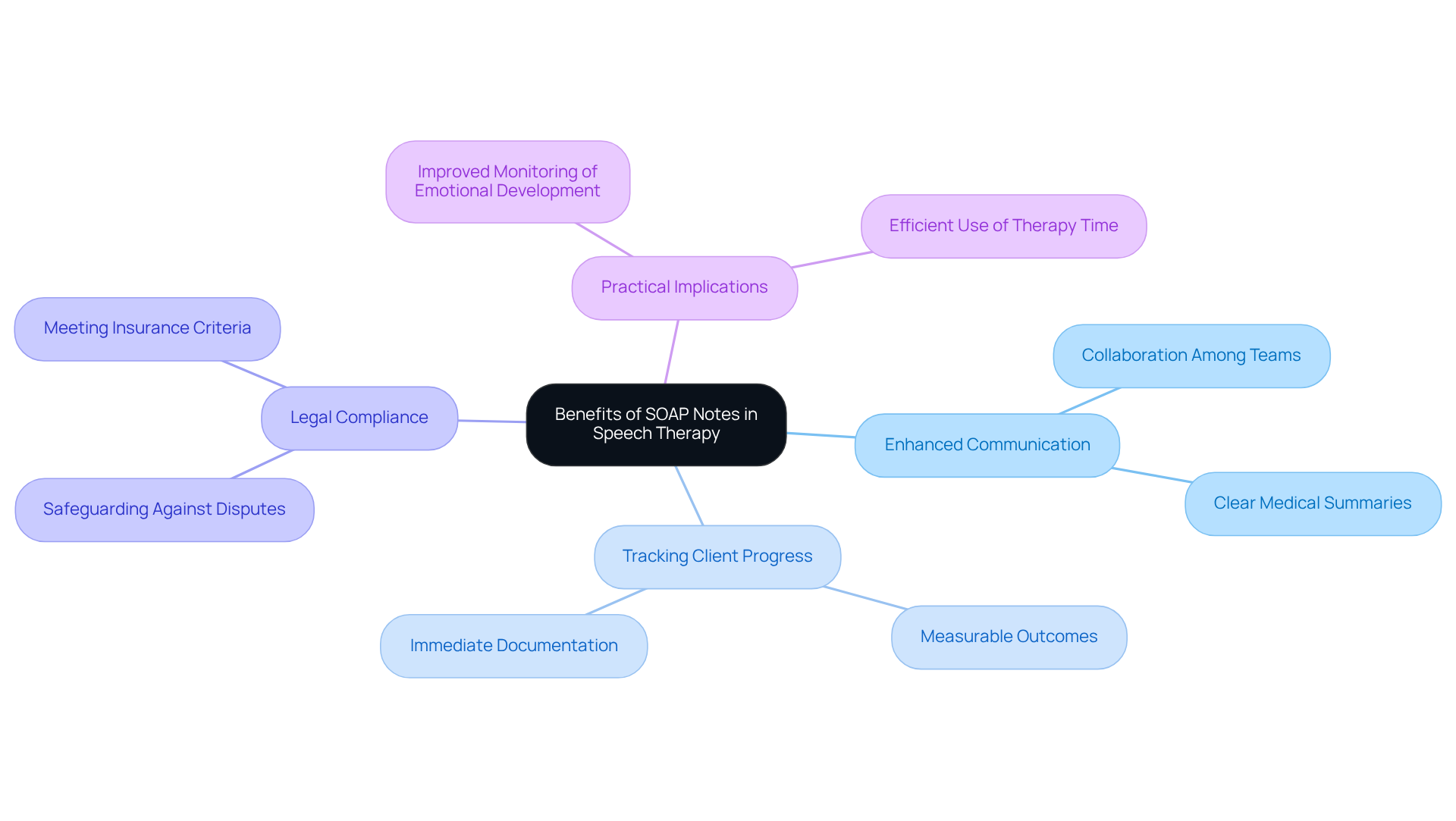
Quenza: Benefits and Examples of SOAP Notes in Speech Therapy
In the world of speech therapy, the use of a speech therapy soap note example offers profound benefits that can truly transform the way we communicate and care for our clients. Have you ever felt overwhelmed by the complexities of patient documentation? These structured notes, such as a speech therapy soap note example, not only enhance communication among healthcare providers but also improve the tracking of individuals and ensure adherence to legal standards. For example, when therapists create a speech therapy soap note example by documenting essential details about a client's progress—such as an increase in articulation accuracy or a decrease in anxiety symptoms—they create a clear picture that aids clinical decision-making. This clarity encourages , ensuring that everyone involved is informed about the individual’s treatment journey.
Consider the practical implications of this documentation approach. In one case, a client expressed feelings of sadness, rating their mood intensity as an 8 out of 10. This prompted the therapist to implement cognitive-behavioral strategies tailored to the client’s needs. The organized layout of therapy records, such as a speech therapy soap note example, allowed the practitioner to record this change efficiently, facilitating improved monitoring of the client's emotional development over time. Isn’t it reassuring to know that such structured documentation can lead to meaningful interventions?
Moreover, the impact of structured documentation extends beyond patient care; it also plays a vital role in compliance with legal standards. Precise documentation serves as a legal record of diagnoses and treatments, safeguarding both healthcare providers and individuals in disputes or insurance claims. Experts in the field emphasize that appropriate documentation, including a speech therapy soap note example, helps speech therapists meet insurance criteria while fostering transparent communication with clients and their families. This systematic approach not only enhances patient care but also allows therapists to devote more time to delivering effective interventions, rather than getting bogged down by administrative tasks. Let’s embrace this compassionate and organized method to ensure we are providing the best care possible.
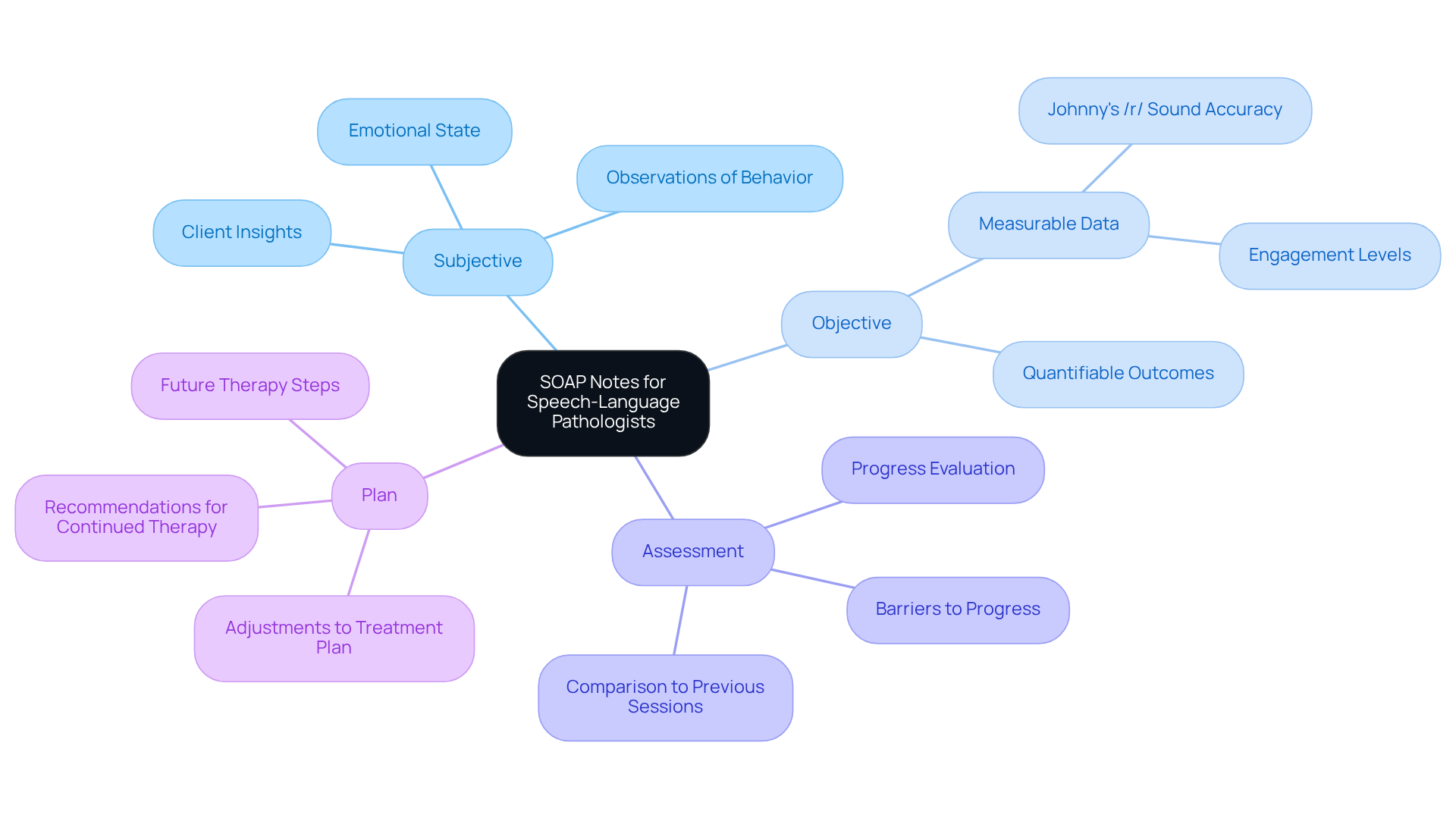
SimplePractice: SOAP Note Examples for Speech-Language Pathologists
SimplePractice provides a thoughtful selection of for speech-language pathologists, including a speech therapy soap note example, as well as assessments, treatment plans, and progress records. These resources are essential for practitioners, helping ensure that their documentation aligns with compliance standards while genuinely reflecting the high-quality care they provide. Effective clinical documentation not only fosters clear communication among healthcare professionals but also enhances treatment planning by capturing client progress and guiding future interventions. For example, when we document measurable outcomes—like 'Johnny improved his production of the /th/ sound by 15%'—we illustrate the effectiveness of therapy and reinforce accountability.
Expert Fiona Affronti highlights that each component of a clinical document, such as the speech therapy soap note example, has a unique role:
- The Subjective captures client insights
- The Objective presents measurable data
- The Assessment evaluates progress
- The Plan outlines future therapy steps
By embracing these organized record-keeping practices and utilizing EHRs, which streamline the recording process and ensure compliance, speech-language pathologists can improve their workflow and promote better outcomes for their clients. Furthermore, composing session records immediately after meetings is vital for maintaining accuracy and significance in reporting.
Have you considered how these practices can alleviate some of the administrative burdens you face? By implementing these strategies, you not only support your own efficiency but also enhance the care you provide to your clients.
TheraPlatform: The Ultimate Guide to SOAP Notes for Speech Therapy
Effective record-keeping is essential in speech therapy, as it profoundly impacts and treatment outcomes. A comprehensive manual on clinical documentation includes a speech therapy soap note example that outlines each critical element—Subjective, Objective, Assessment, and Plan—while emphasizing their significance in practice. Consider these key insights to enhance your documentation:
-
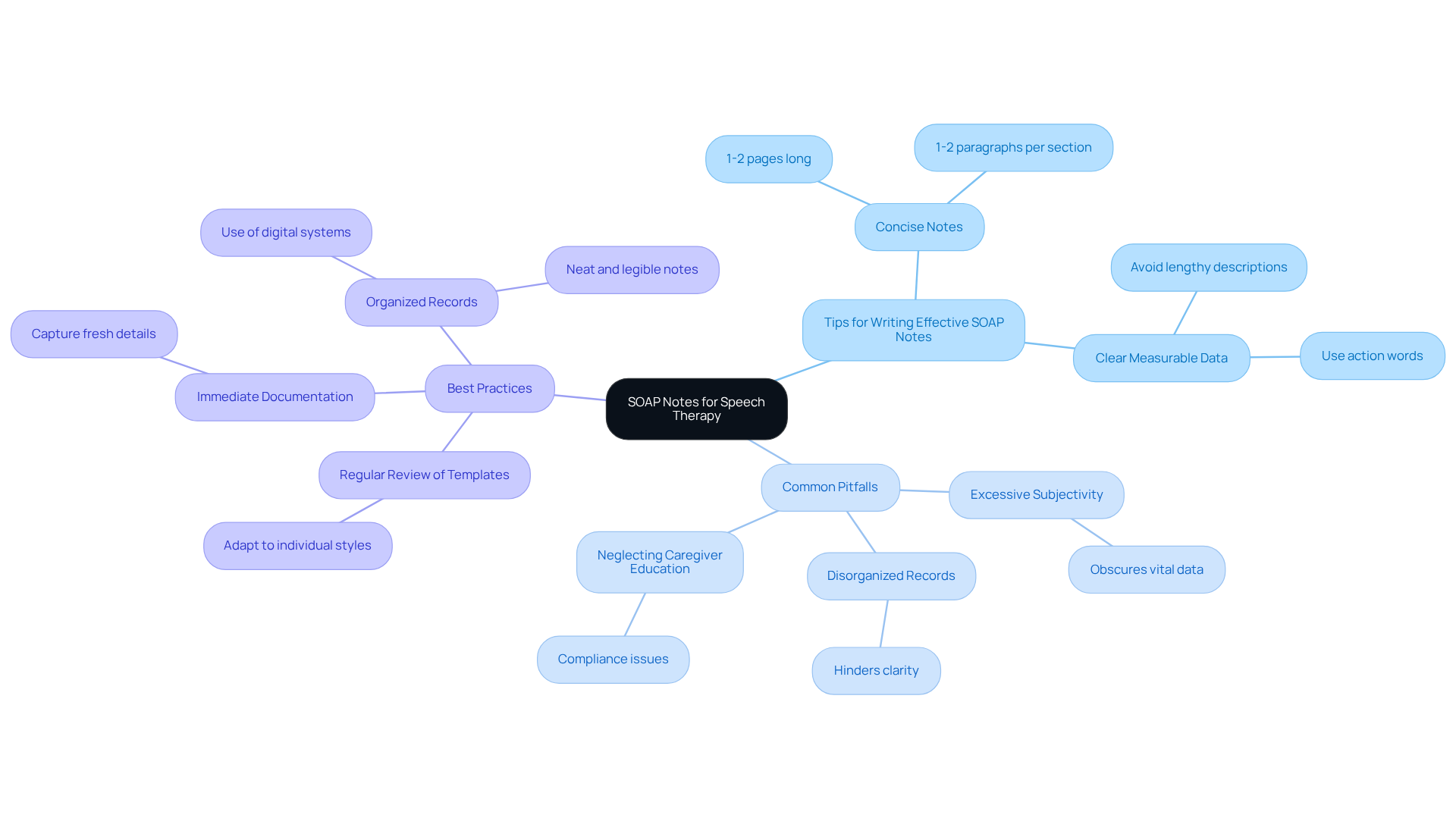
Tips for [Writing Effective SOAP Notes](https://ensorahealth.com/blog/how-to-write-excellent-soap-notes-for-speech-therapy-2):
- Aim for concise notes, ideally 1-2 pages long, with each section comprising 1-2 paragraphs.
- Utilize clear, measurable data in the Objective section, steering clear of lengthy descriptions of therapy activities.
- Incorporate action words to vividly illustrate challenges and progress, which can enhance clarity during insurance reviews.
-
Common Pitfalls in Speech Therapy Documentation:
- Be cautious of excessive subjectivity in the Objective section, as it can obscure vital data.
- Disorganized records may hinder clarity and complicate the review process.
- Neglecting to document caregiver education and home programs can lead to compliance issues with insurance requirements.
-
Best Practices for Effective SOAP Notes:
- Document each session immediately to capture fresh details and ensure accuracy.
- Maintain organized and clear records, whether using pen and paper or digital systems.
- Regularly review and adapt the speech therapy soap note example templates to suit individual note-taking styles, ensuring consistency and organization.
- Always verify records against templates and clinical guidelines for insurance reimbursement to meet necessary standards.
By following these guidelines, providers can significantly enhance their documentation practices, ensuring that all pertinent information is recorded while prioritizing compassionate care for individuals.
SoapNoteAI: Top 10 Common SOAP Note Examples for Speech Therapy
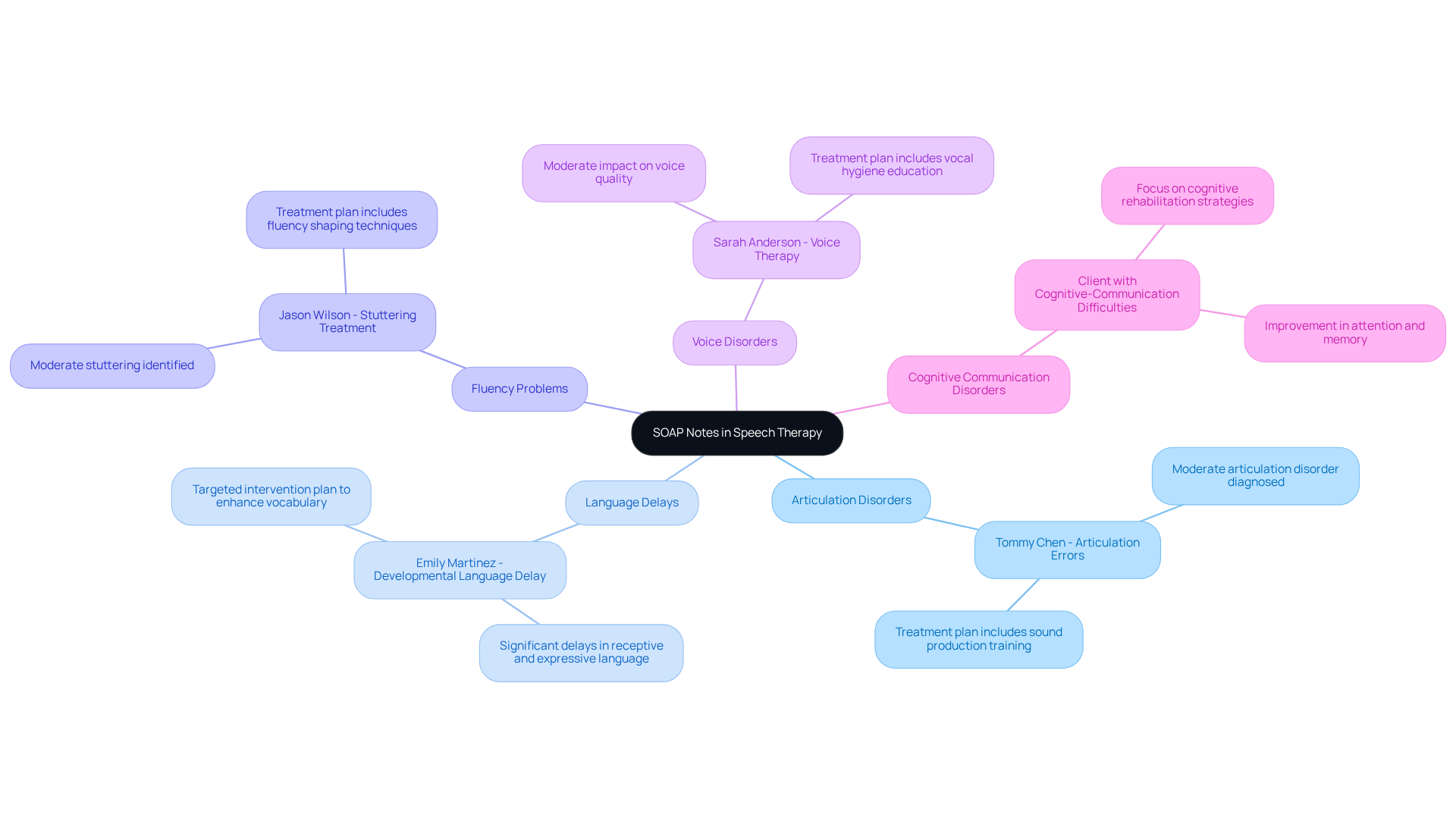
In the world of speech therapy, documentation can often feel overwhelming. Healthcare providers face emotional challenges as they strive to deliver the best care while managing administrative tasks. SoapNoteAI understands this struggle and offers a speech therapy soap note example, along with the top 10 typical documentation examples for situations like articulation disorders, language delays, and fluency problems.
These examples serve as a quick reference, designed to ease the documentation process for providers. By streamlining the way patient interactions are recorded, SoapNoteAI helps ensure that all necessary information is captured efficiently. Imagine the relief of having a reliable tool that allows you to focus more on your patients and less on paperwork.
By utilizing these documentation examples, providers can enhance their workflow and ultimately improve patient care. This not only saves time but also allows for more with patients. Are you ready to transform your documentation experience and reconnect with the heart of your practice? Engage with SoapNoteAI today and discover how it can support you in your vital role.
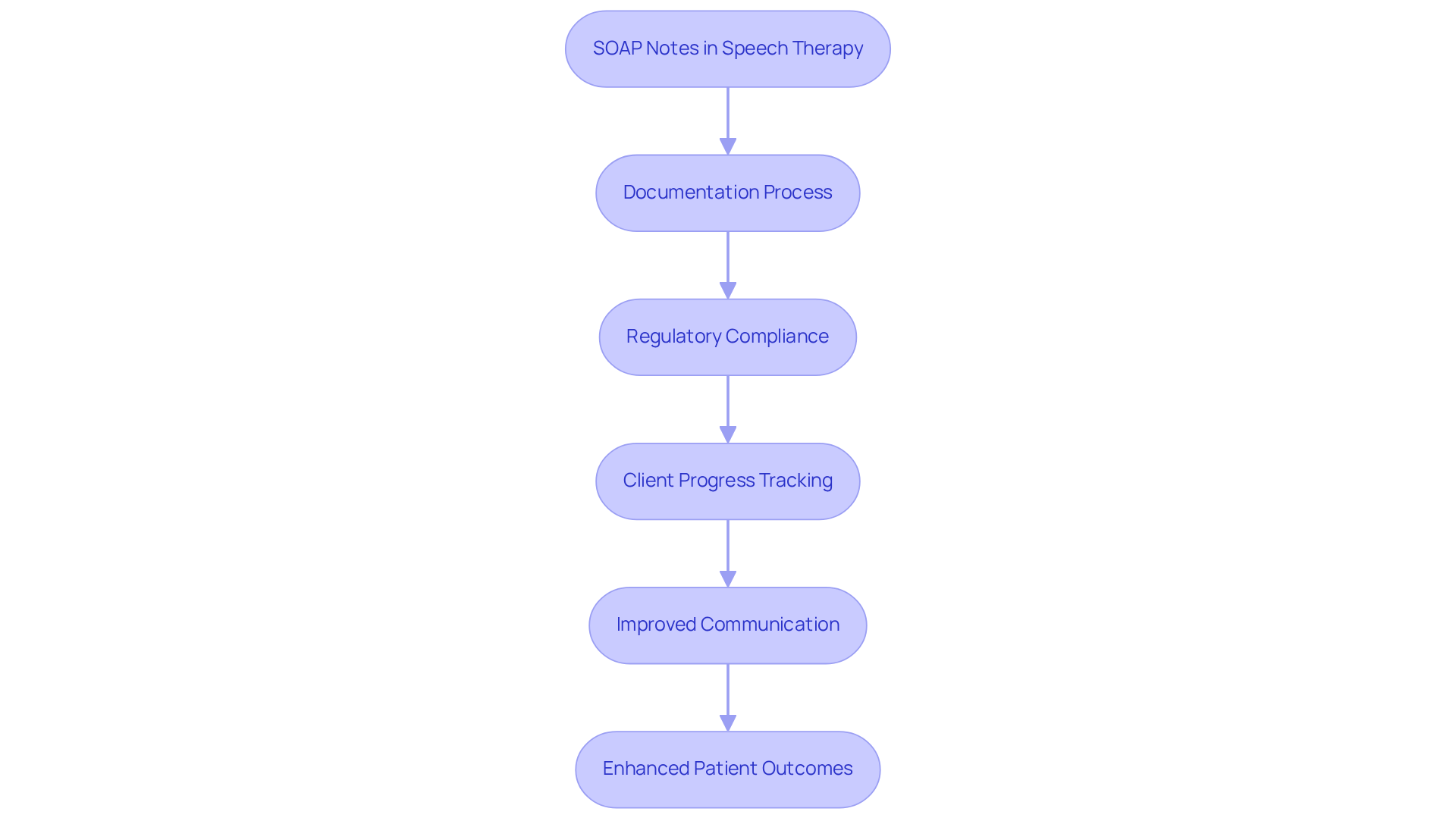
Headway: Compliance Benefits of SOAP Notes in Speech Therapy
Organized records through therapeutic logs, including a speech therapy soap note example, play a vital role in ensuring adherence within speech therapy. Have you ever felt overwhelmed by the administrative demands of your practice? By carefully keeping precise and thorough documentation, providers not only protect themselves from potential legal issues but also align their practices with industry standards. Regulatory requirements for documentation in speech therapy are stringent, and a speech therapy soap note example is necessary to ensure clear records that reflect client progress and treatment plans. For instance, a speech therapy soap note example must include measurable data in the objective section, while the subjective section captures the client's self-reported symptoms, providing a comprehensive view of their condition.
Insights from experts emphasize that efficient documentation aids in meeting payer requirements and legal standards. These records serve as a , documenting all relevant patient information and justifications for services rendered. This structured approach enhances communication among healthcare providers and ensures that therapy goals are clearly defined and tracked over time.
Consider how structured documentation can influence regulatory adherence. Therapists who utilize this method can easily reference previous sessions, aiding in the assessment of client progress and identifying barriers to achieving therapy goals. Moreover, regular application of structured documentation fosters enhanced cooperation with caregivers and insurance companies, ultimately leading to better patient outcomes and satisfaction.
In summary, the adherence advantages of documentation in speech therapy can be illustrated with a speech therapy soap note example, which is considerable. By following organized record-keeping practices, providers can ensure they meet regulatory requirements while delivering high-quality care that aligns with industry standards. Are you ready to embrace these practices and enhance your therapy sessions?
Mentalyc: Importance of Specificity in Speech Therapy SOAP Notes
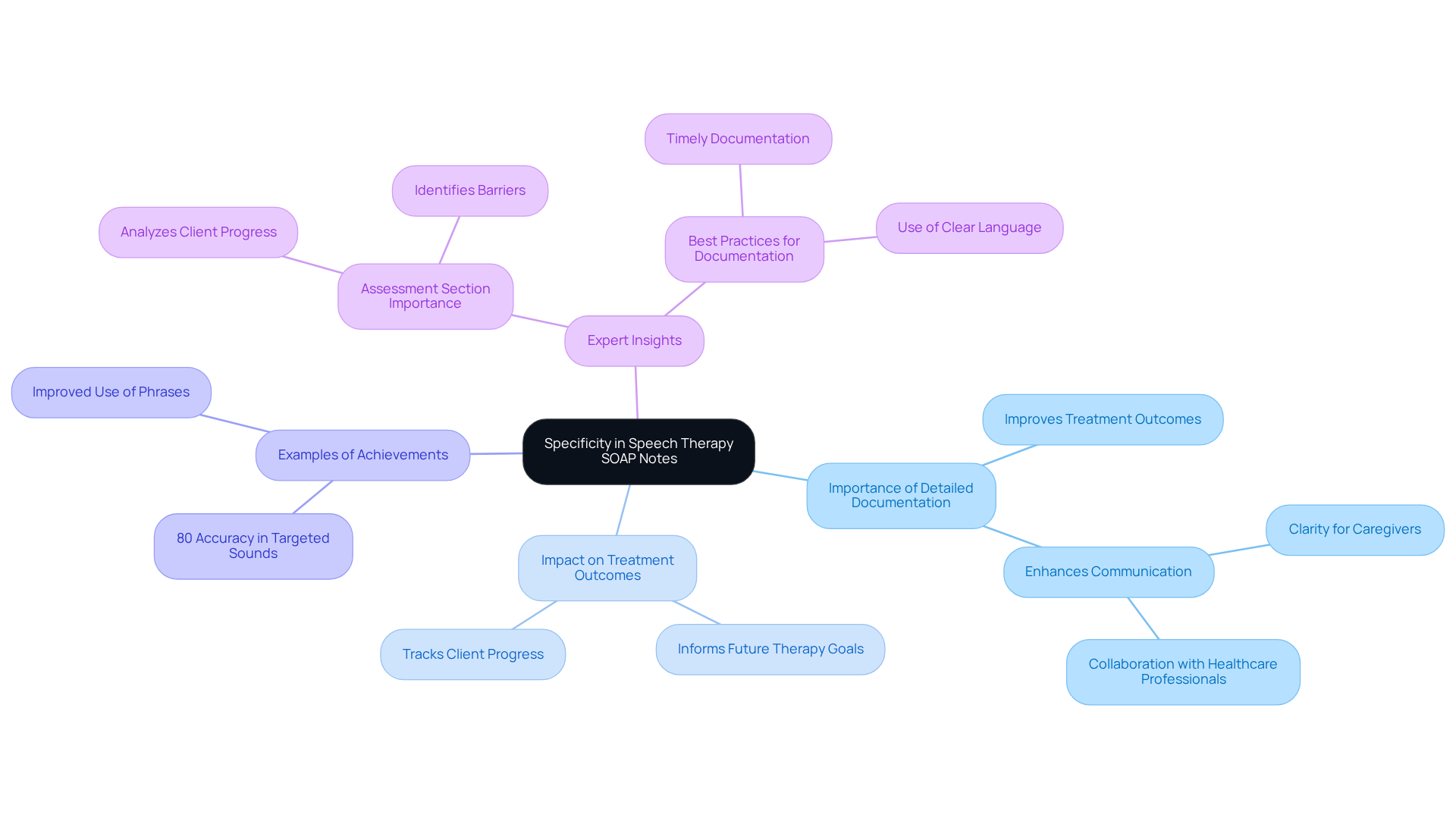
The significance of specificity in a speech therapy SOAP note example is profound, as detailed documentation plays a crucial role in improving treatment outcomes. Have you ever considered how meticulous documentation of individual behaviors and responses can create a comprehensive view of a person's progress? This understanding is vital for and collaboration with other healthcare professionals.
For example, when therapists record specific achievements—like an individual demonstrating 80% accuracy in producing targeted sounds—it not only highlights progress but also informs future therapy goals. This level of detail fosters clearer communication among caregivers and therapists, ensuring that everyone involved understands the individual’s journey.
Experts in the field, including seasoned speech-language pathologists, emphasize the importance of the Assessment section in a speech therapy SOAP note example. This section serves as an opportunity to analyze client progress and identify barriers, ultimately guiding the therapeutic approach. By concentrating on thorough and practical documentation, therapists can significantly enhance the quality of care provided. This leads to improved outcomes and greater satisfaction for those receiving treatment.
In light of these insights, how might you refine your documentation practices to better support your clients? By embracing detailed and empathetic note-taking, you can foster a more collaborative and effective treatment environment.
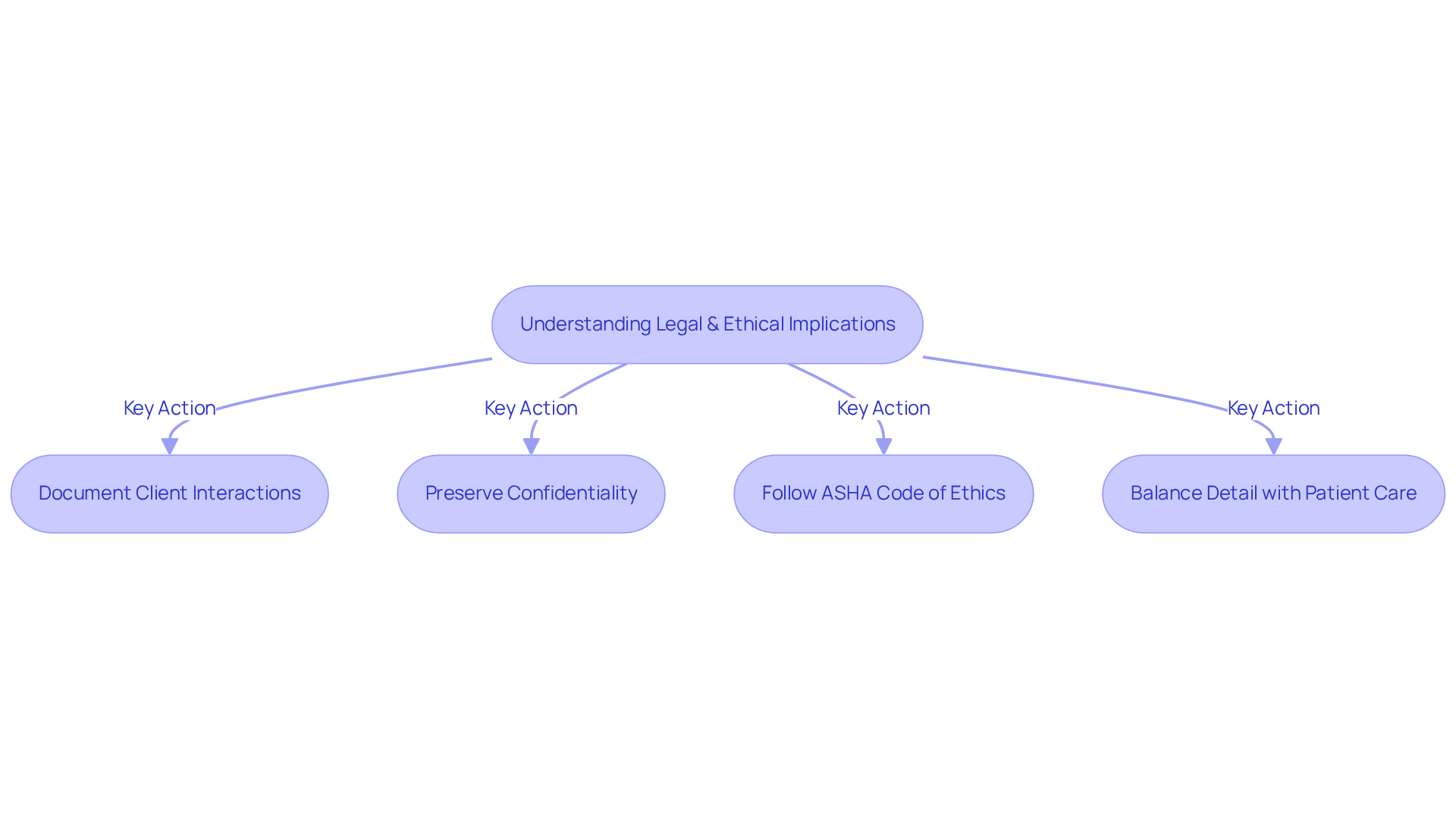
Quenza: Legal and Ethical Implications of SOAP Notes in Speech Therapy
In the field of speech therapy, understanding the [legal and ethical consequences of a speech therapy SOAP note example](https://forensicnotes.com/importance-of-documentation-expert-and-influential-leader-quotes) is incredibly important. These notes not only document interactions with clients but also serve as a protective measure for both providers and clients. Preserving confidentiality is essential; providers must navigate the complexities of legal standards regulating records to protect sensitive patient information. Recent revisions to the ASHA Code of Ethics emphasize the significance of ethical record-keeping practices, reinforcing that all disclosures must be legally authorized. This shift underscores the necessity of understanding ethical guidelines in clinical documentation, as failure to comply can lead to serious repercussions.
Real-world examples shed light on the impact of ethical considerations on SOAP note practices. For instance, during the Ebola virus disease outbreak, ethical dilemmas arose regarding the confidentiality of individuals and the need for accurate care documentation in high-stress situations. The outbreak resulted in over 11,000 deaths and highlighted disparities in healthcare standards, illustrating the critical role of ethics in clinical settings. Speech-language pathologists faced challenges in balancing the need for detailed records with the urgency of patient care, demonstrating the importance of meticulous record-keeping in safeguarding both providers and patients.
Insights from experts further highlight the importance of ethical standards in record-keeping. Experts emphasize that careful documentation not only supports clinical decision-making but also serves as a legal safeguard. As Stuart Rudner states, "To establish a robust legal stance, record-keeping is essential. Otherwise, you expose yourself to unnecessary liability and cost." Inadequate records can lead to misunderstandings and potential liability issues. Therefore, adhering to ethical guidelines in practices such as the speech therapy SOAP note example is crucial for building trust and ensuring high-quality client care.
To implement these ethical standards in daily practice, providers should regularly review their documentation processes, ensuring they align with the and prioritize patient confidentiality.
Conclusion
The significance of effective documentation in speech therapy is profound. Recognizing the emotional challenges healthcare providers face, structured formats like SOAP notes can alleviate some of the administrative burdens that often detract from patient care. By integrating comprehensive examples and best practices, providers can ensure their documentation meets the high standards of care that clients truly deserve.
Throughout this article, we have shared important insights about the components of SOAP notes—Subjective, Objective, Assessment, and Plan. Each section is vital in capturing client progress, guiding treatment decisions, and ensuring compliance with legal and ethical standards. Innovative tools like CosmaNeura and Mentalyc can help ease the administrative load, allowing therapists to devote more time to the compassionate care their clients need.
Ultimately, embracing effective documentation practices is crucial for enhancing patient outcomes and cultivating a collaborative healthcare environment. Speech therapists are encouraged to explore the resources available to them, refine their documentation strategies, and prioritize structured notes in their practice. By taking these steps, they can transform their interactions with clients, ensuring that every session is documented with clarity and precision. How might these practices change your approach to patient care?




