Overview
In the demanding world of healthcare, providers often face emotional challenges due to the overwhelming burden of documentation. It’s not just about keeping records; it’s about ensuring the best care for patients. That’s where essential therapy note templates come into play. These structured formats, such as SOAP, DAP, BIRP, and GIRP, are designed to enhance documentation efficiency.
Imagine a scenario where therapists can redirect their focus from administrative tasks to truly connecting with their clients. By streamlining record-keeping and improving communication, these templates support better patient care outcomes. They allow healthcare providers to spend more time on what truly matters—their patients.
We understand that every moment counts in therapy sessions. By utilizing these templates, you can alleviate some of the administrative pressures that weigh heavily on your shoulders. This not only enhances your workflow but also enriches the therapeutic relationship you cultivate with your clients.
Are you ready to transform your documentation process? Embrace these tools that not only simplify your tasks but also empower you to provide the compassionate care your patients deserve. Let’s make the journey of healing more focused and meaningful together.
Introduction
In the intricate landscape of healthcare, emotional challenges often intertwine with administrative demands. This reality makes the need for efficient documentation more pressing than ever. This article explores ten essential therapy note templates designed to streamline the documentation process. By doing so, it enables practitioners to focus on what truly matters: patient care. Yet, with a myriad of options available, how can therapists determine which templates will best enhance their practice and improve client outcomes? This inquiry sets the stage for a deeper exploration into the transformative power of structured documentation in therapy.
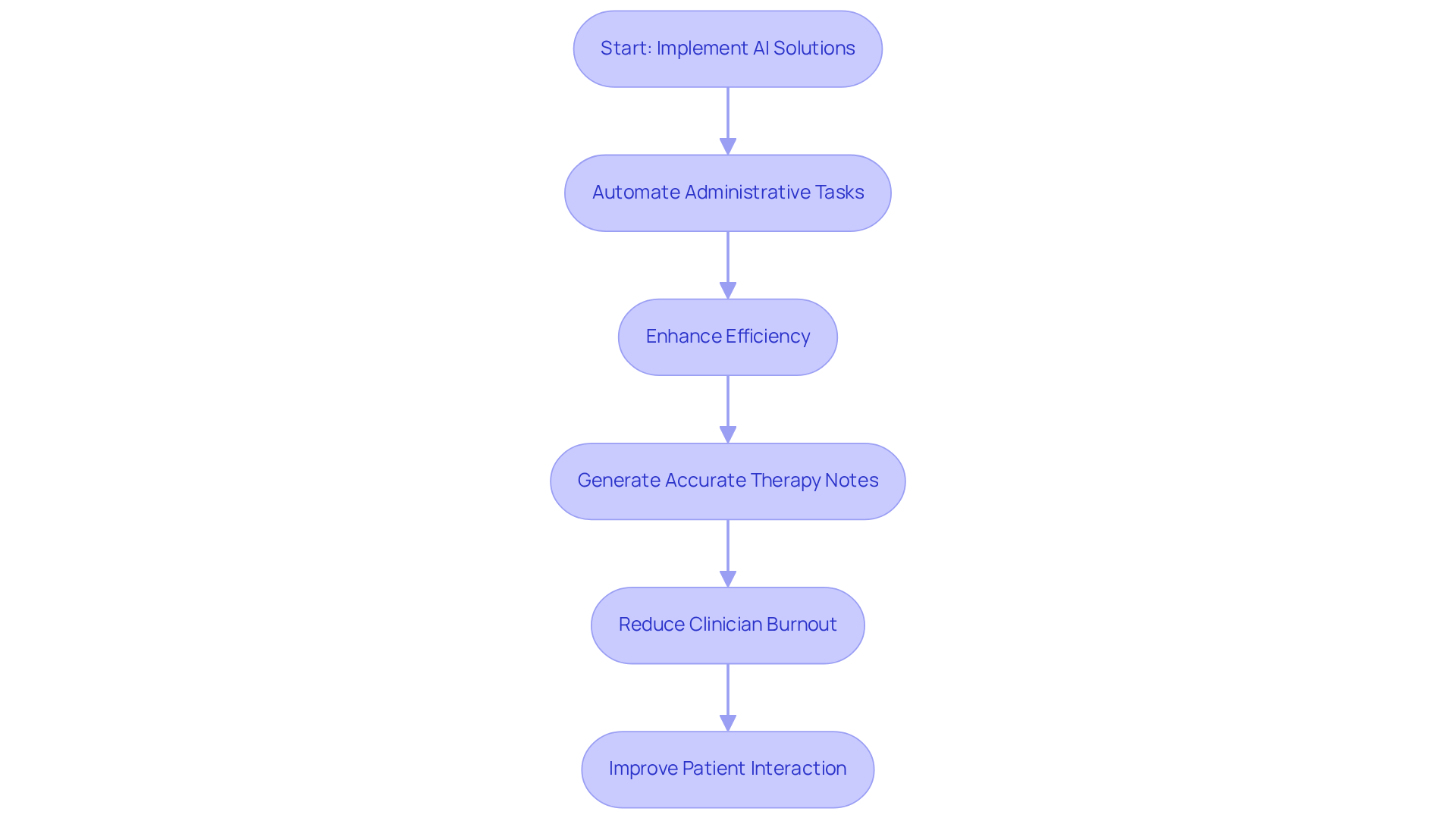
CosmaNeura: Streamline Therapy Note Management with AI-Powered Solutions
In the demanding world of healthcare, providers often face overwhelming emotional challenges, particularly in managing a therapy note template. CosmaNeura offers a compassionate solution with its cutting-edge AI platform, designed to alleviate these burdens and allow providers to focus on what truly matters—patient care. By automating administrative tasks like patient intake and record-keeping, CosmaNeura significantly enhances the efficiency of therapy practices, particularly through the use of a therapy note template, which is essential for healthcare startups navigating resistance to innovation.
Imagine the relief of conserving valuable time while upholding a compassionate approach to care, all in line with Catholic ethical standards. The platform’s advanced AI capabilities ensure real-time transcription and summarization of therapy sessions, creating a therapy note template that results in records that are not only accurate but also comprehensive. With the potential to save healthcare providers an estimated 200,000 hours daily through generative AI and automation, the impact on the efficiency of the therapy note template is truly profound.
Case studies reveal that organizations leveraging AI for documentation have experienced substantial improvements in workflow. This allows clinicians to dedicate their efforts to delivering high-quality care, effectively alleviating physician burnout. Moreover, it’s noteworthy that 81% of physicians believe generative AI will enhance interactions with patients. Thus, integrating such technology into therapy practices is not just beneficial; it’s essential for modern healthcare.
In addition, healthcare organizations are under significant financial pressure, making the efficiency gains from AI even more critical in addressing rising costs. By embracing these innovative solutions, we can ensure sustainable patient care while fostering an environment where compassion thrives. Are you ready to explore how CosmaNeura can transform your practice and enhance your patient interactions?
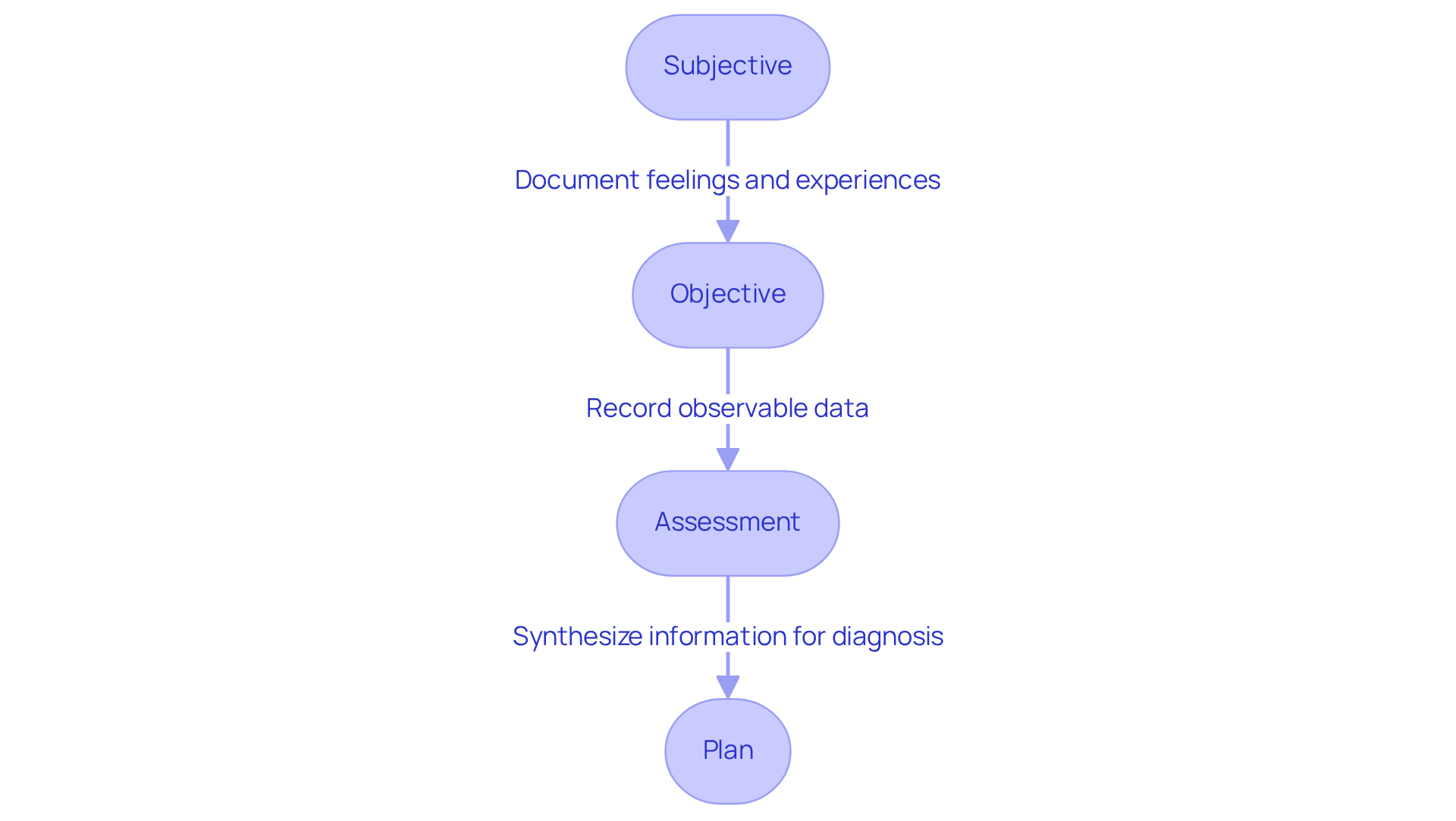
SOAP Note Template: A Structured Approach for Effective Therapy Documentation
The SOAP note template consists of four essential components: Subjective, Objective, Assessment, and Plan. This structured format empowers therapists to document their interactions with individuals in a thorough and organized way. Have you ever felt overwhelmed by the need to capture every detail? The Subjective section captures the individual's self-reported feelings and experiences, offering valuable insight into their emotional state. For instance, someone might express feelings of anxiety, stating, "He feels 'wound up' and angry much of the time," or report changes in sleep patterns, such as difficulty sleeping. These insights are crucial for understanding their condition.
The Objective section includes observable data, such as the individual's appearance and behavior during the session. This information can reveal important physical and emotional indicators. For example, a counselor might notice that an individual appears disheveled or struggles to maintain eye contact. These observations are vital in building a comprehensive understanding of the individual's experience.
Next, the Assessment section synthesizes information from both the Subjective and Objective components. This allows the therapist to make informed clinical judgments. If an individual reports heightened anxiety and exhibits fidgeting, the assessment may confirm a diagnosis of generalized anxiety disorder, as indicated by Michael's GAD-7 score of 14, which rose from 12. This connection between observations and assessments is key to effective treatment.
Finally, the Plan outlines the next steps in treatment, detailing specific interventions and goals tailored to the client's needs. Utilizing the SOAP format in a therapy note template not only enhances clarity and organization but also ensures that all relevant information is documented. This documentation is vital for continuity of care. Consider how timely recording after every session, using clear and succinct language, and adhering to ethical guidelines can improve your practice.
By following these guidelines, therapists can elevate patient care outcomes. Structured documentation fosters better communication among healthcare providers and supports evidence-based practice. Overall, the SOAP format serves as a valuable therapy note template that enhances accountability and professionalism in clinical practice, acting as evidence of the care delivered to patients. Embrace this approach to enrich your therapeutic relationships and improve the well-being of those you serve.
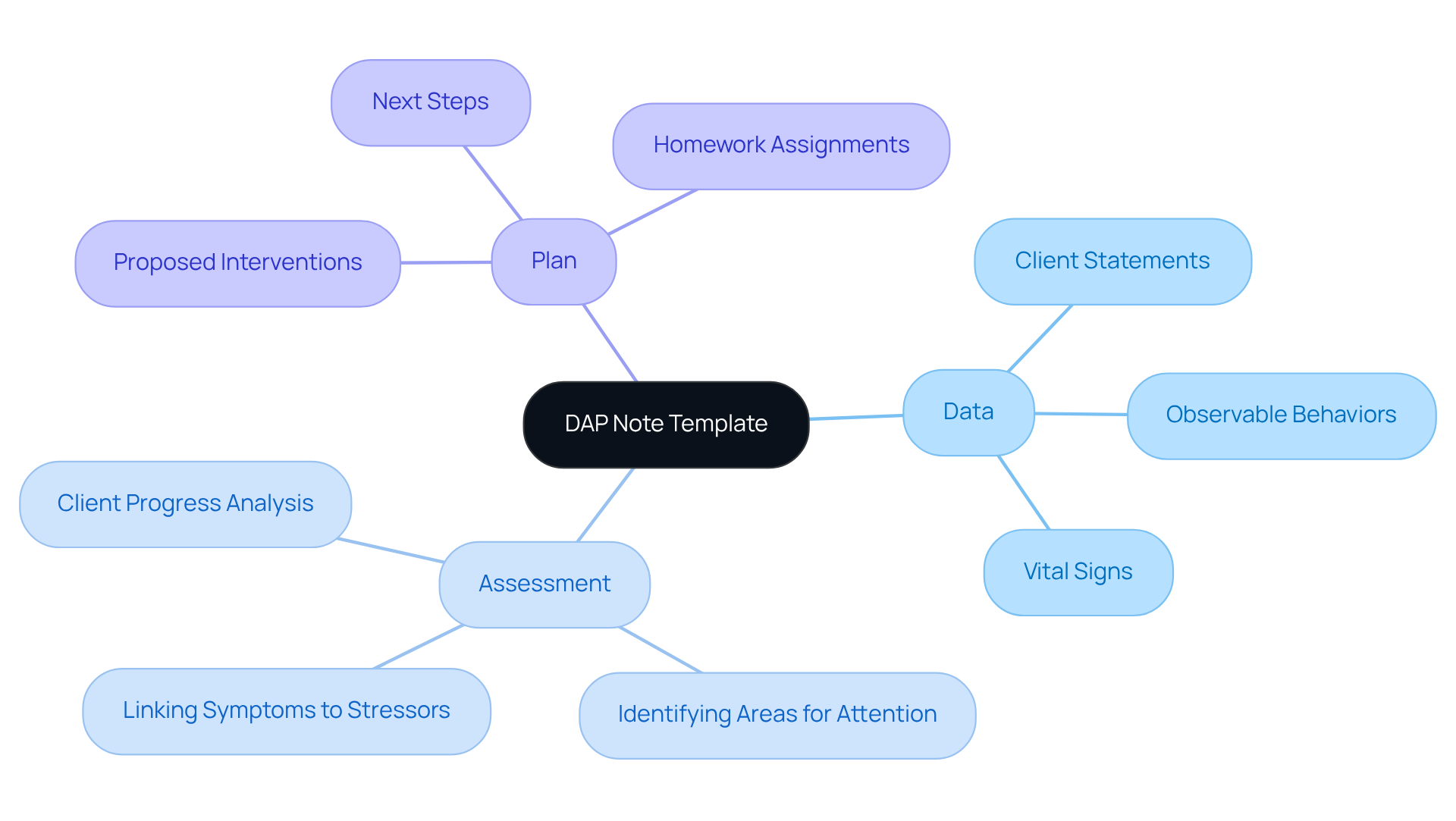
DAP Note Template: Documenting Data, Assessment, and Plan in Therapy
The DAP note template is thoughtfully structured into three essential components: Data, Assessment, and Plan. In the Data section, vital information from the session is captured, including direct statements from clients and observable behaviors. This meticulous record-keeping is crucial for understanding and supporting client needs. The Assessment section interprets this data, allowing professionals to analyze client progress and identify areas that may require additional attention. Finally, the Plan outlines proposed interventions or next steps, providing a clear direction for future sessions.
This therapy note template is especially advantageous for therapists aiming to improve their record-keeping efficiency. Have you ever felt overwhelmed by the time spent on documentation? Research indicates that clinicians can save 6-8 minutes per progress record when utilizing DAP formats, significantly easing the administrative burden associated with documentation. Furthermore, employing DAP records can lead to a 12% reduction in claim denials, underscoring their effectiveness in meeting payer requirements.
Real-world examples illustrate the practical application of DAP notes in therapy. For instance, a counselor might document a session with a patient experiencing anxiety by noting observable symptoms in the Data section, such as increased heart rate and restlessness. The Assessment could reveal that work-related stress has exacerbated the patient’s anxiety, while the Plan might recommend specific relaxation techniques to help manage these symptoms.
By embracing the therapy note template format, therapists can simplify their record-keeping process. This approach ensures that essential information is captured effectively, ultimately enhancing care and treatment planning for individuals. Are you ready to transform your documentation process and focus more on what truly matters—your clients?
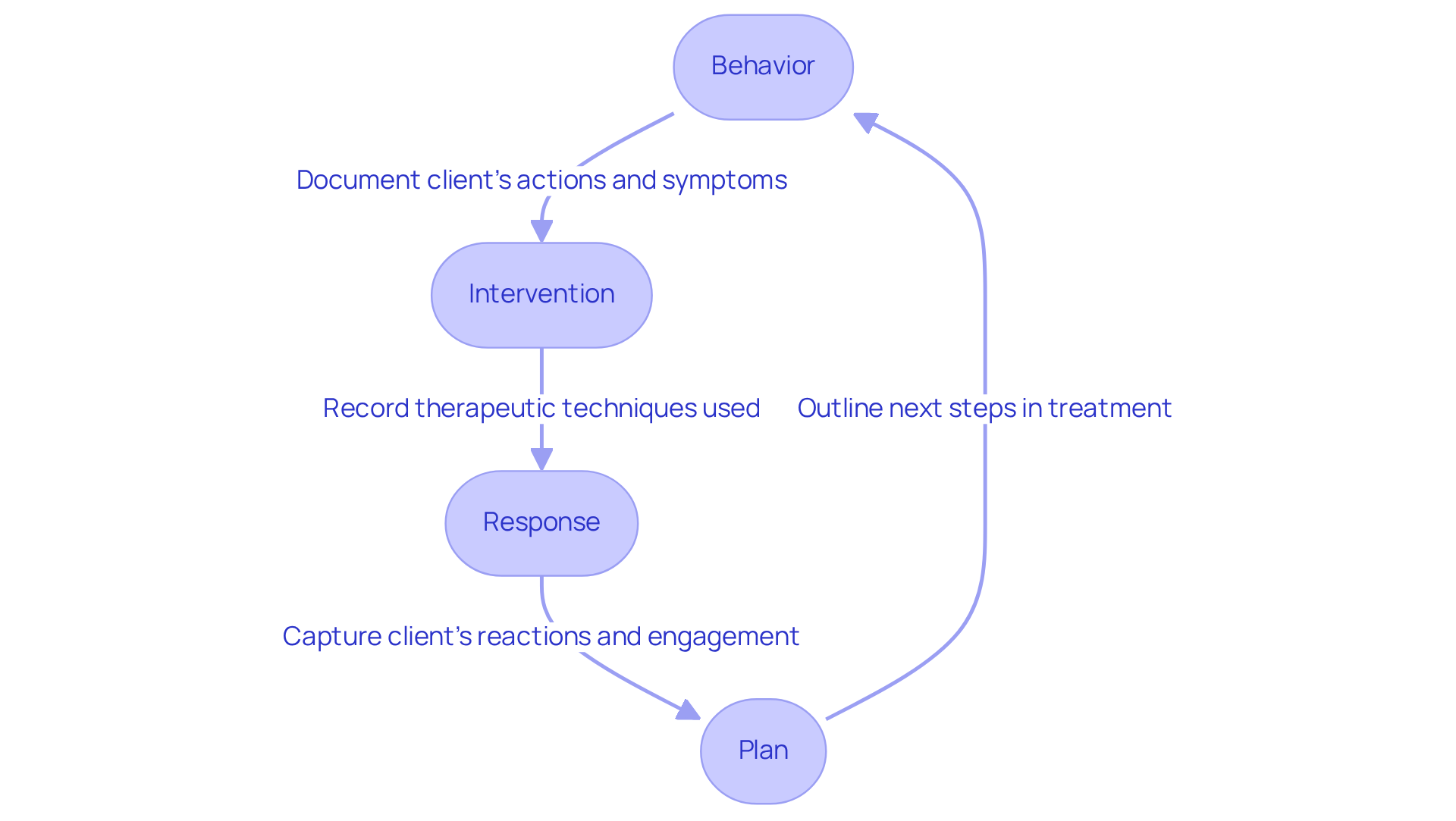
BIRP Note Template: Comprehensive Tracking of Client Interventions
The therapy note template known as BIRP serves as a crucial ally in therapy documentation, consisting of four key components: Behavior, Intervention, Response, and Plan. The Behavior section carefully records the individual’s actions, statements, and observable symptoms during the session, offering a clear insight into their current emotional state. For instance, if an individual shares that they experience panic attacks multiple times a week, documenting this can be invaluable for tracking their progress over time.
Next, the Intervention section outlines the specific therapeutic techniques utilized, such as cognitive behavioral therapy or relaxation exercises. This documentation is not just a formality; it links the therapist's actions directly to the individual's treatment goals, ensuring that interventions are tailored to their unique needs. For example, a therapist might introduce grounding techniques to help someone manage anxiety, and this would be reflected in the notes.
The Response component captures how the individual reacts to these interventions, including their engagement level and any notable quotes. This part is vital for assessing the therapy's effectiveness and making necessary adjustments. If a participant reports feeling immediate relief after practicing relaxation techniques, that feedback can significantly inform future sessions.
Finally, the Plan section details the next steps in treatment, encompassing goals, homework assignments, and scheduling future sessions. This organized approach not only fosters continuity of care but also enriches the overall therapeutic experience. Research indicates that counselors who effectively utilize BIRP records tend to achieve improved client outcomes, as these records simplify documentation and allow for more focused client interactions. By keeping a clear and structured record of each session, therapists can better monitor progress and adapt treatment plans as necessary, ultimately nurturing more successful therapeutic relationships.
In this way, the therapy note template not only streamlines the documentation process but also enhances the connection between provider and client, paving the way for more meaningful therapeutic journeys.
GIRP Note Template: Focusing on Goals and Client Responses in Therapy
The therapy note template serves as a structured documentation tool that includes four essential components: Goals, Interventions, Responses, and Plans. The Goals section thoughtfully outlines the objectives set for the individual, ensuring therapy aligns with their aspirations. Interventions detail the therapeutic techniques employed, offering insight into the methods used to facilitate progress. Responses capture the individual's feedback, documenting their journey toward achieving these goals, while the Plans section outlines the next steps in treatment, ensuring continuity and focus.
This goal-oriented method is vital for effective therapy, as it encourages therapists to remain centered on the individual's needs and aspirations. For example, an individual striving to learn coping skills for depression might establish specific, measurable goals within the GIRP framework, allowing for clear tracking of progress. As noted by an Anonymous Psychotherapist, 'Effective documentation not only safeguards you as a clinician but also fosters meaningful advancement for those you assist by clearly outlining key points in their therapeutic journey.'
Practical examples illustrate the positive impact of GIRP documents on client outcomes. Therapists utilizing GIRP documentation have reported enhanced clarity in treatment plans and improved communication among providers, as highlighted in various case studies. By focusing on patient objectives, therapists can cultivate stronger therapeutic relationships, ultimately leading to heightened engagement and success in therapy. One specialist remarked, 'The therapy note template found in GIRP documents is an essential resource for mental health practitioners, offering a structured framework for recording sessions, monitoring advancement, and making informed decisions regarding future therapy.' This organized approach not only streamlines the record-keeping process but also underscores the importance of goal-oriented therapy, ensuring that clients remain at the heart of their treatment.

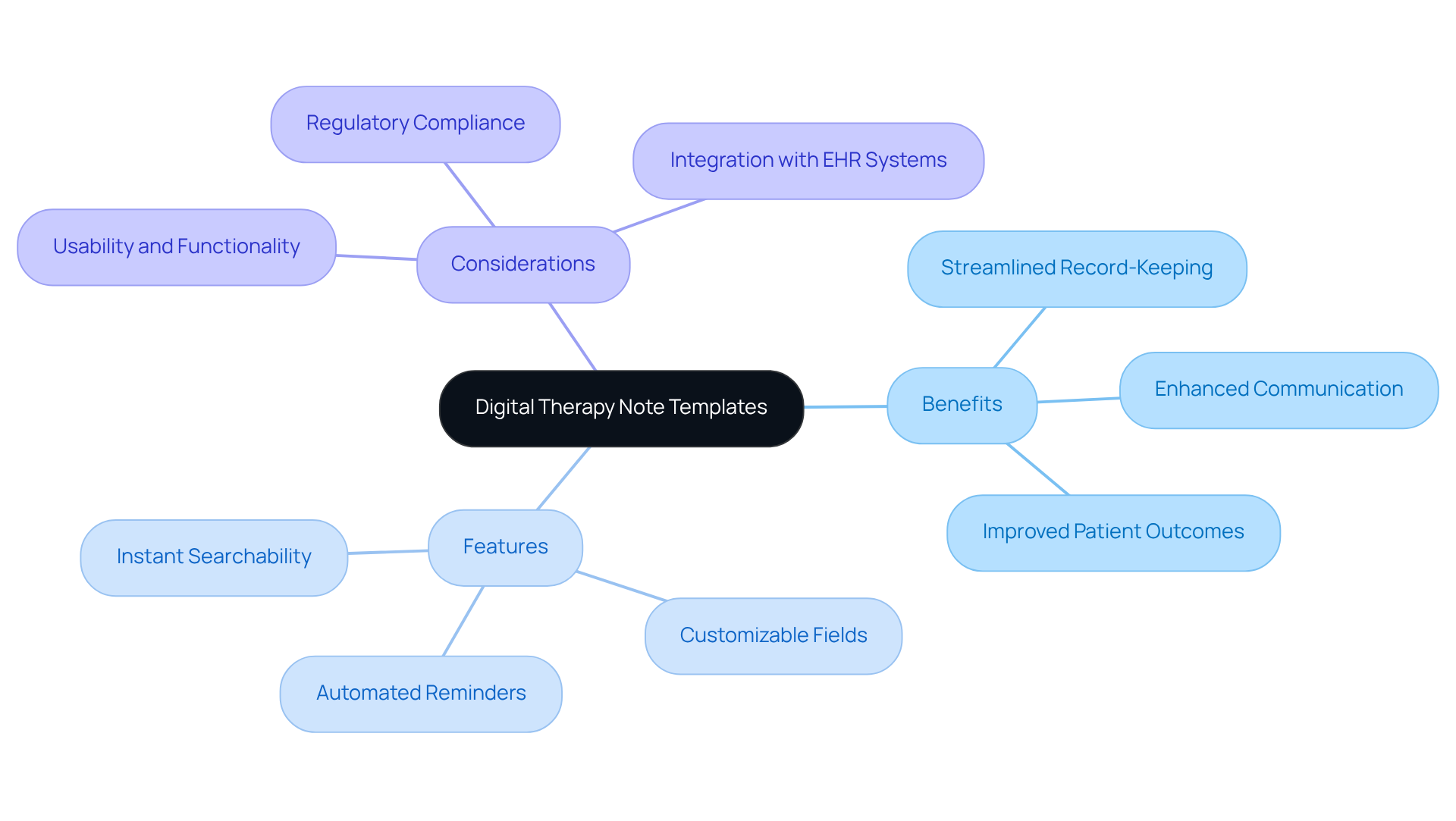
Digital Therapy Note Templates: Leveraging Technology for Enhanced Documentation
Digital therapy note templates provide a compassionate solution for practitioners dealing with the pressing challenge of fragmented care in healthcare. These adaptable tools seamlessly integrate with electronic health record (EHR) systems, streamlining record-keeping and fostering better communication among providers. Have you ever felt overwhelmed by the administrative burdens that detract from patient care? With digital templates, you can experience instant searchability, allowing for quick access to patient information while significantly reducing the risk of errors from manual entry.
Furthermore, the ability to generate reports swiftly not only aids in maintaining accurate records but also enhances coordination with other healthcare providers—an essential aspect in a fragmented system. It’s important to recognize that regulatory concerns, like those from HIPAA, can create barriers to effective patient care. By embracing technology, practitioners can refine their record-keeping methods, ultimately allowing more time to focus on what truly matters: patient care. This shift not only elevates the quality of care provided but also plays a vital role in improving patient outcomes, as thorough documentation is key to informed clinical decision-making.
To fully harness these advantages, therapists should thoughtfully evaluate EHR systems based on usability and functionality, ensuring they select tools that align with their practice needs. Consider the specific characteristics of a therapy note template—customizable fields and automated reminders are just a few features that illustrate their value in overcoming fragmentation. By choosing the right tools, you can create a more nurturing environment for your patients, enhancing both your practice and their care journey.
Customizable Therapy Note Templates: Tailoring Documentation to Provider Needs
Customizable therapy note template empower providers to adapt their records to meet the unique needs of their practice and patients. Have you ever felt overwhelmed by the demands of documentation? Therapists can modify sections of the therapy note template, incorporate unique fields, or adjust formats to align with their therapeutic methodologies. This flexibility not only ensures that all pertinent information is captured but also enhances user-friendliness.
By customizing a therapy note template, professionals can significantly enhance their efficiency, allowing them to focus on what truly matters—providing compassionate care. As a licensed therapist observes, maintaining clear and personalized records fosters a collaborative environment where both therapist and individual can monitor progress and adjust goals as necessary. This approach not only streamlines the documentation process but also reinforces the therapeutic relationship, ultimately leading to better patient outcomes.
Imagine the difference it could make if your documentation felt less like a burden and more like a supportive tool in your practice. By using a therapy note template, you can transform your workflow and prioritize the emotional well-being of your patients.
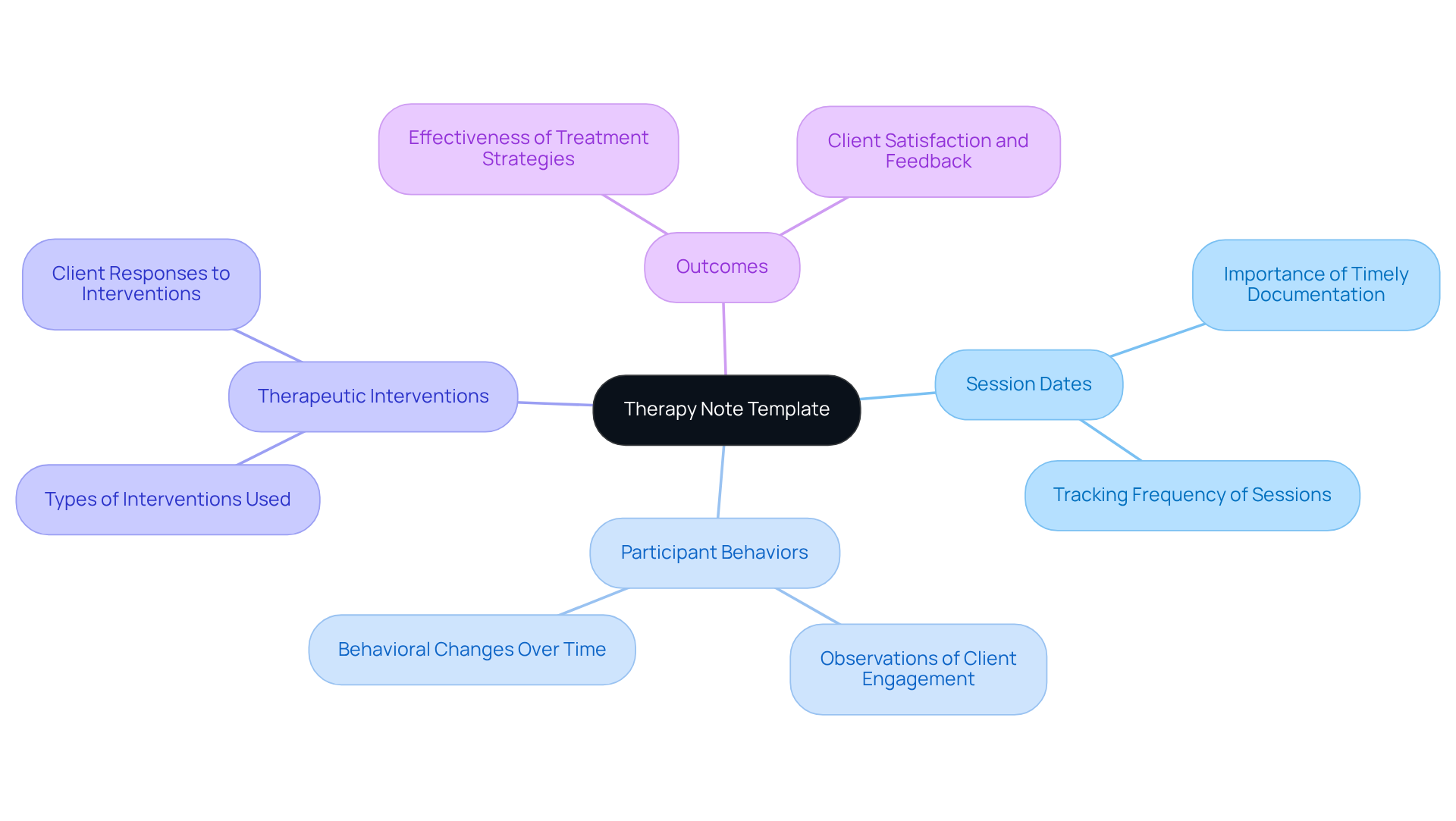
Progress Note Template: Essential for Monitoring Client Development
The therapy note template serves as a vital resource for documenting the significant details of an individual's growth over time. A therapy note template typically includes sections for recording session dates, participant behaviors, therapeutic interventions, and outcomes. By consistently refreshing these records, professionals can assess the efficacy of treatment strategies and make necessary adjustments. Have you ever noticed how a counselor might observe a participant's progress in managing anxiety through specific coping techniques? This insight can guide future sessions and interventions, ensuring that care remains tailored to the individual's needs.
This continuous record-keeping, facilitated by a therapy note template, is essential for guaranteeing that individuals receive optimal care and support throughout their therapeutic journey. By utilizing a therapy note template to maintain clear and concise progress records, therapists can enhance communication with clients and other healthcare providers, ultimately leading to improved treatment results and client satisfaction. It’s crucial to finalize records promptly after each session to avoid overlooking details, as specialists in the field often emphasize.
Moreover, health experts who are well-versed in standard practice records tend to record more efficiently. This highlights the importance of progress records in therapy. Utilizing a therapy note template like Quenza Notes can significantly streamline the documentation process, making it easier for therapists to maintain accurate and timely records. By embracing these practices, we can collectively enhance the quality of care provided to those we serve.
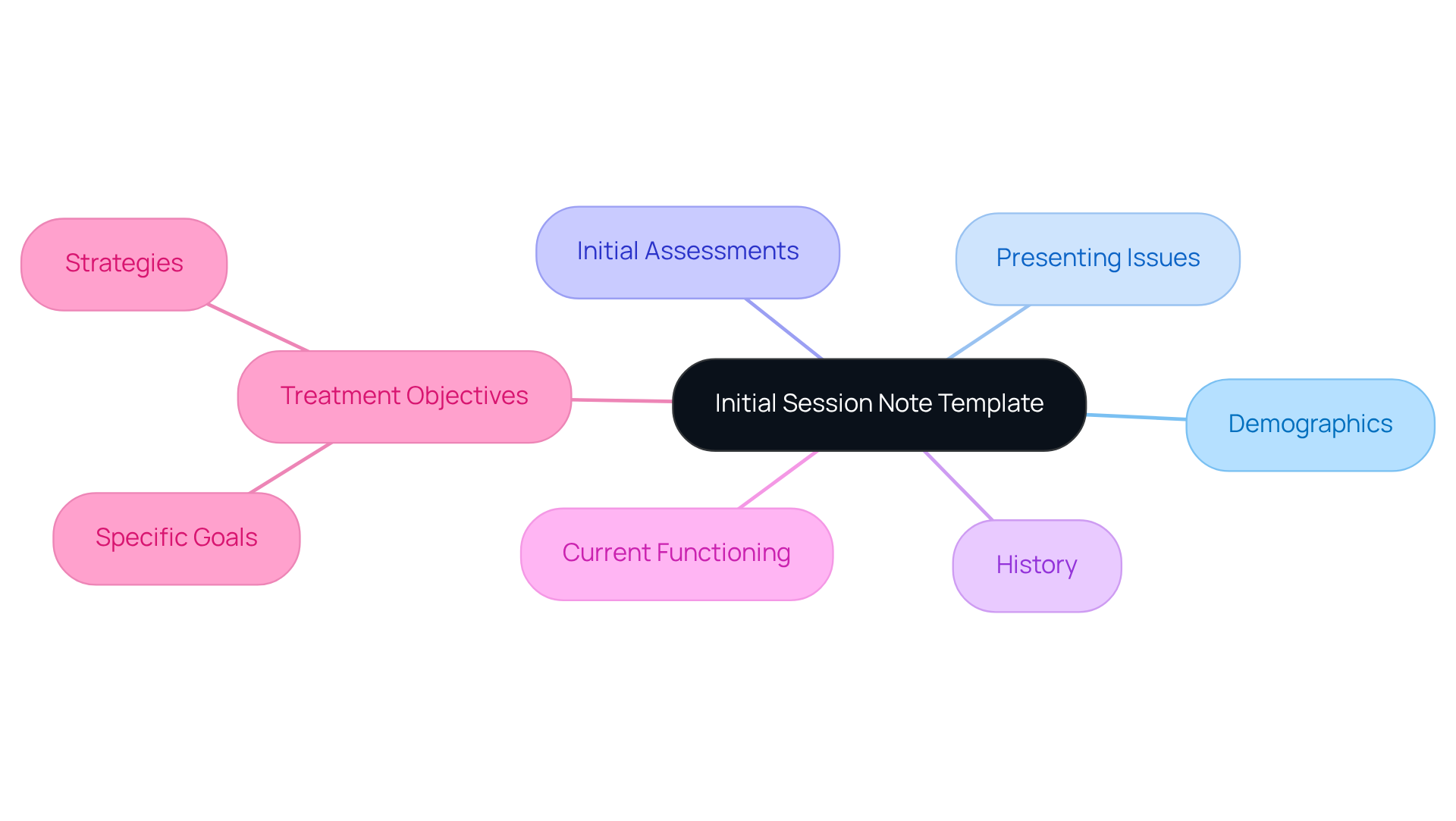
Initial Session Note Template: Establishing Baselines for Effective Therapy
The therapy note template plays a vital role in capturing an individual's baseline information, such as demographics, presenting issues, and initial assessments. Have you considered how essential this is for understanding your clients? This therapy note template usually includes sections for the individual's history, current functioning, and treatment objectives. By establishing a comprehensive baseline in the therapy note template, therapists can effectively track changes and progress throughout the therapeutic process.
This initial record not only serves as a reference point for future sessions but also ensures that treatment remains focused and relevant to the client's needs. It’s crucial to complete records promptly; preventing delays of more than 3 to 5 days in finishing entries helps preserve memory accuracy, which is key for efficient treatment planning. Additionally, utilizing secure, HIPAA-compliant software for writing and storing therapy notes is critical to uphold ethical and legal standards.
Incorporating direct quotes from clients, such as 'I just felt so overwhelmed and alone,' can offer deeper insights into their emotional states, enhancing the relevance and accuracy of the material. Overall, prompt and accurate foundational records not only promote a stronger therapeutic relationship but also lead to improved outcomes for those receiving services. How can you ensure that your documentation supports your clients’ journeys? Reflect on the ways you can enhance your practice today.
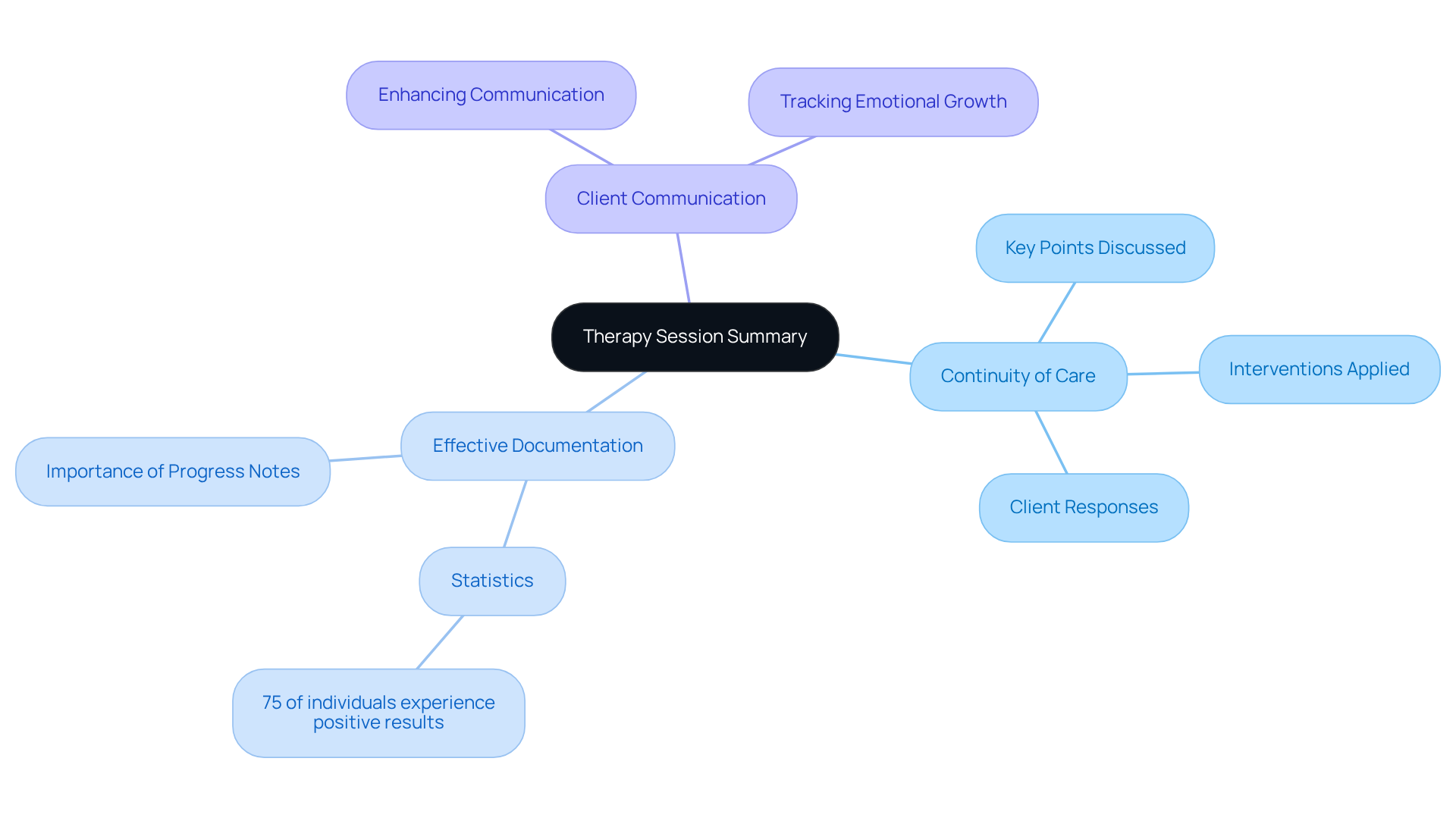
Therapy Session Summary Template: Ensuring Continuity of Care
The therapy note template serves as an invaluable resource for capturing a concise overview of each session, highlighting key points discussed, interventions applied, and client responses. The therapy note template serves as essential documentation that not only ensures continuity of care but also allows professionals to revisit previous sessions with ease, aligning with treatment goals. As Vivian Chung Easton, Clinical Product Lead at Blueprint, insightfully notes, "Creating clear and concise progress records is essential for maintaining continuity of care and showcasing the effect of therapeutic interventions."
By diligently maintaining thorough session summaries, professionals can enhance communication with clients, ensuring that both parties remain informed about progress and the next steps in the therapeutic journey. Have you ever considered how vital these records are for tracking emotional growth? For instance, a therapist might document a client's expressed feelings of inadequacy during a session, which can be referenced in future discussions to adjust treatment strategies accordingly.
Statistics reveal that approximately 75% of individuals who undergo psychotherapy experience positive results. This underscores the importance of effective documentation in achieving these outcomes. By adopting a structured approach, we not only foster a collaborative environment but also reinforce the therapeutic alliance, ultimately leading to more effective outcomes.
Isn't it reassuring to know that clear documentation can significantly impact the therapeutic process? Let's commit to enhancing our practices for the benefit of our clients.
Conclusion
Embracing various therapy note templates discussed in this article is essential for enhancing documentation efficiency and improving patient care. These structured formats—SOAP, DAP, BIRP, GIRP, and customizable templates—streamline the documentation process and ensure that critical information is captured accurately. By utilizing these tools, therapists can focus on delivering compassionate care while maintaining comprehensive records that support effective treatment planning.
Have you ever felt overwhelmed by administrative tasks? Key insights reveal that implementing AI-powered solutions like CosmaNeura can significantly alleviate these burdens, allowing healthcare providers to dedicate more time to their patients. The benefits of structured documentation extend beyond mere record-keeping; they foster better communication among providers, enhance accountability, and ultimately lead to improved patient outcomes. As highlighted, integrating technology in therapy documentation is not just a trend but a necessity for modern healthcare practices.
In conclusion, the significance of adopting effective therapy note templates cannot be overstated. By prioritizing structured documentation, therapists can ensure that their practices are both efficient and compassionate. It is crucial to explore and implement these tools, as they play a vital role in nurturing therapeutic relationships and enhancing the overall quality of care. The journey towards better documentation is a step towards better patient outcomes—are you ready to take that step?




