Overview
In the demanding world of healthcare, providers often face significant emotional challenges. The weight of administrative tasks can feel overwhelming, detracting from the time and attention they wish to dedicate to patient care. This is where essential medical note templates come into play.
Templates like SOAP, DAP, and BIRP are not just tools; they are solutions designed to streamline documentation processes. By reducing administrative burdens, these templates empower healthcare professionals to focus more on what truly matters—caring for their patients. Imagine the difference this could make in service quality and patient outcomes.
Consider how much more time could be spent with patients, fostering relationships, and providing the compassionate care they deserve. With the right documentation tools, healthcare providers can transform their workflows and enhance their ability to serve.
We encourage you to explore these templates and see how they can support your practice. Together, we can improve the healthcare experience for both providers and patients alike.
Introduction
In the fast-paced world of healthcare, providers often feel overwhelmed by the weight of meticulous documentation. This burden can distract them from what truly matters: patient care. Fortunately, innovative medical note templates, powered by AI technology like CosmaNeura, offer a transformative opportunity to enhance both efficiency and the quality of care.
But as the healthcare landscape continues to evolve, we must ask ourselves: how can these templates not only ease administrative pressures but also cultivate deeper connections between providers and patients? By exploring essential medical note templates, we can uncover solutions that bridge the gap between operational efficiency and compassionate care.
Imagine a world where healthcare providers can focus more on their patients and less on paperwork. This is not just a dream; it can be a reality with the right tools in place. Let's delve into the possibilities that await us, fostering a more nurturing environment for both providers and patients alike.
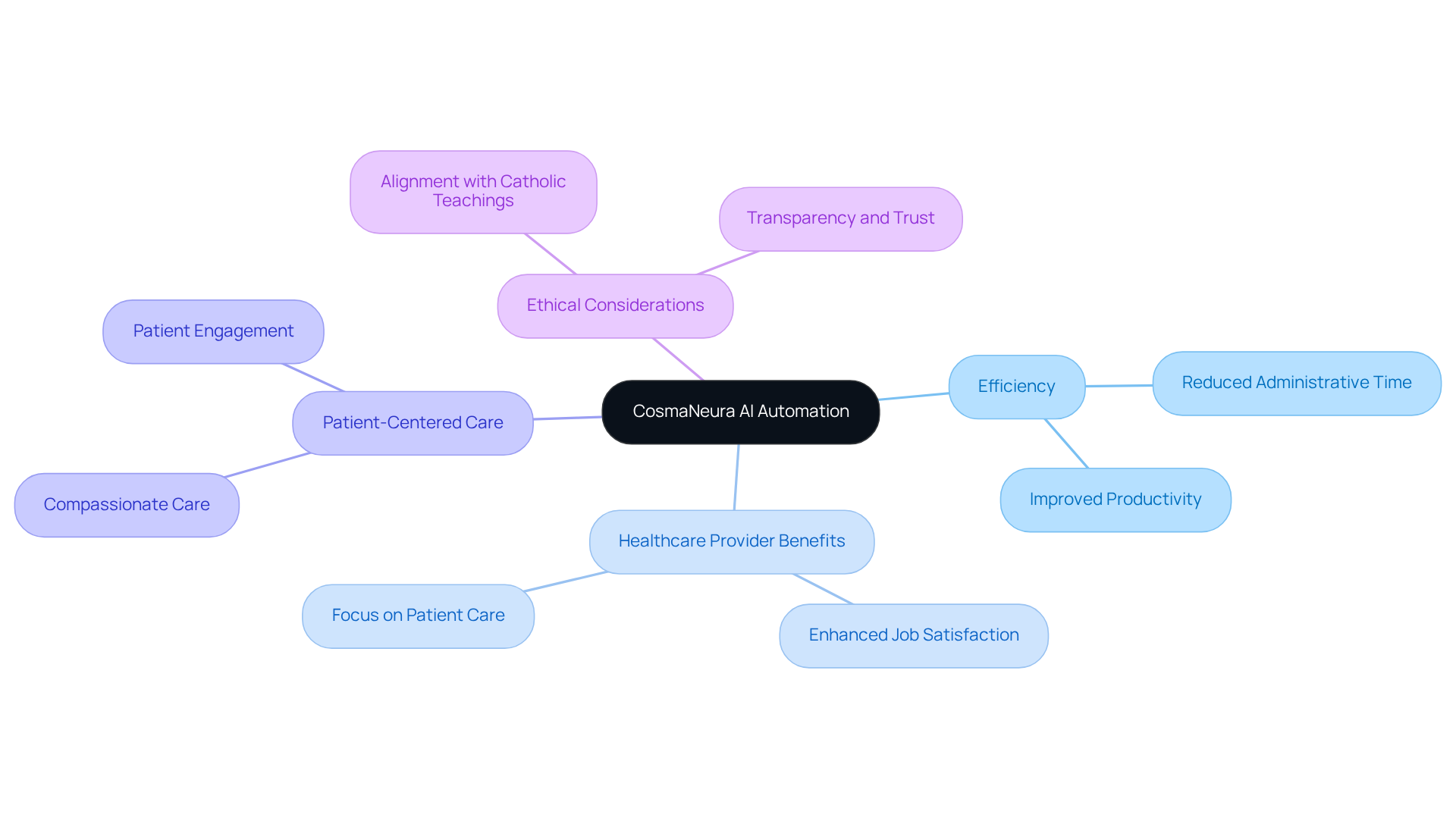
CosmaNeura: AI-Powered Medical Note Automation for Efficient Documentation
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to connect with patients. CosmaNeura recognizes this challenge and utilizes advanced AI technology to automate the creation of a medical note template for recording. By significantly decreasing the time spent on administrative tasks, this innovative solution allows healthcare professionals to focus more on meaningful patient interactions, fostering a compassionate and patient-centered atmosphere.
Imagine a world where the efficiency of record-keeping not only boosts productivity but also aligns with the ethical standards of Catholic teachings. CosmaNeura's automation reinforces a commitment to delivering high-quality care, ensuring that every patient feels valued and heard. Research indicates that AI can match or even surpass human precision in creating clinical summaries, enhancing the trustworthiness of medical records.
For instance, in a recent pilot initiative, 3,442 doctors utilized during over 303,000 client interactions. This remarkable effort led to significant decreases in recording time and improved client engagement. By alleviating the administrative burden, CosmaNeura's platform, featuring a medical note template, empowers healthcare professionals to reclaim precious time, ultimately enhancing job satisfaction and the overall quality of care.
Are you ready to transform your practice and focus more on what truly matters? Embrace the future of healthcare with CosmaNeura, where technology and compassion come together to support your mission of providing exceptional care.
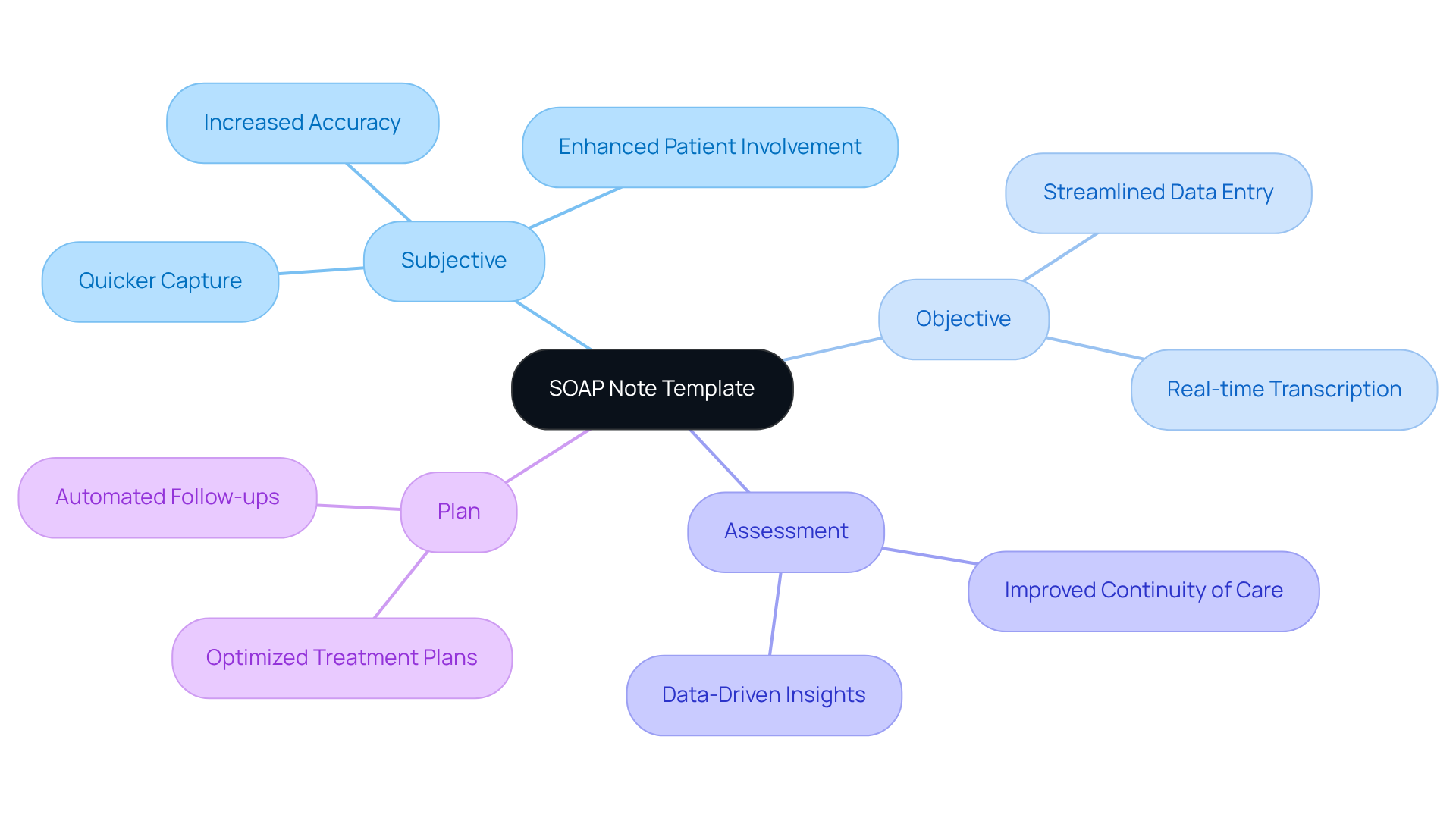
SOAP Note Template: Standardized Format for Patient Encounters
Healthcare providers often face emotional challenges, including burnout and overwhelming administrative tasks. The medical note template, specifically the SOAP (Subjective, Objective, Assessment, Plan) format, serves as a vital resource, helping to standardize records and ensuring that essential information is effectively captured during patient encounters.
How can we alleviate some of this burden? By leveraging generative AI, healthcare providers can enhance the efficiency of the documentation process. This allows for quicker and more accurate capture of subjective reports, objective findings, assessments, and planned interventions.
This organized method not only supports clinical decision-making but also improves continuity of care. It provides a clear record for future reference, which can be incredibly reassuring for both providers and patients. Additionally, AI can streamline regular administrative tasks, such as arranging appointments and overseeing medical records. This shift allows providers to focus more on client interactions and personalized care.
Incorporating AI into the medical note template for the SOAP documentation process can significantly enhance client involvement and optimize administrative efficiency. Ultimately, this leads to , addressing the pressing challenges that many healthcare professionals encounter today. Let’s embrace these advancements together to create a more supportive and effective healthcare environment.
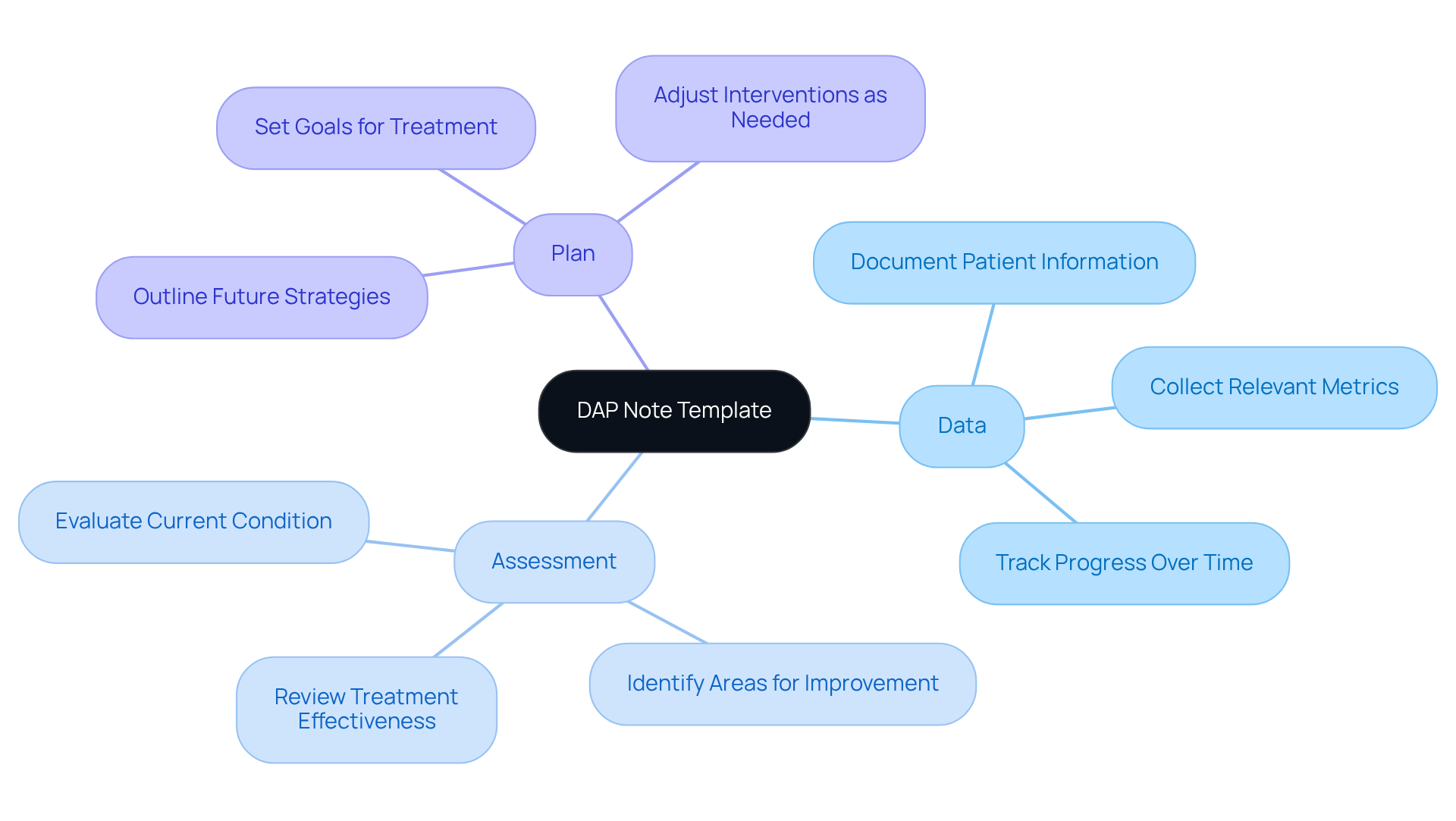
DAP Note Template: Focused Approach for Documenting Patient Progress
The medical note template is designed to ease the record-keeping burden of individual progress, focusing on three key components: Data, Assessment, and Plan. This medical note template not only assists providers in documenting essential information effectively but also enables them to evaluate the individual's current condition and outline a supportive strategy for the future.
Have you ever felt overwhelmed by administrative tasks? By incorporating generative AI, healthcare providers can automate parts of this documentation process. This not only reduces the administrative load but also frees up valuable time to focus on meaningful interactions with individuals.
Imagine a world where you can continuously monitor client progress and make informed decisions about treatment. This integration assures that providers can enhance the quality of service and deepen client engagement. Together, we can create a more .
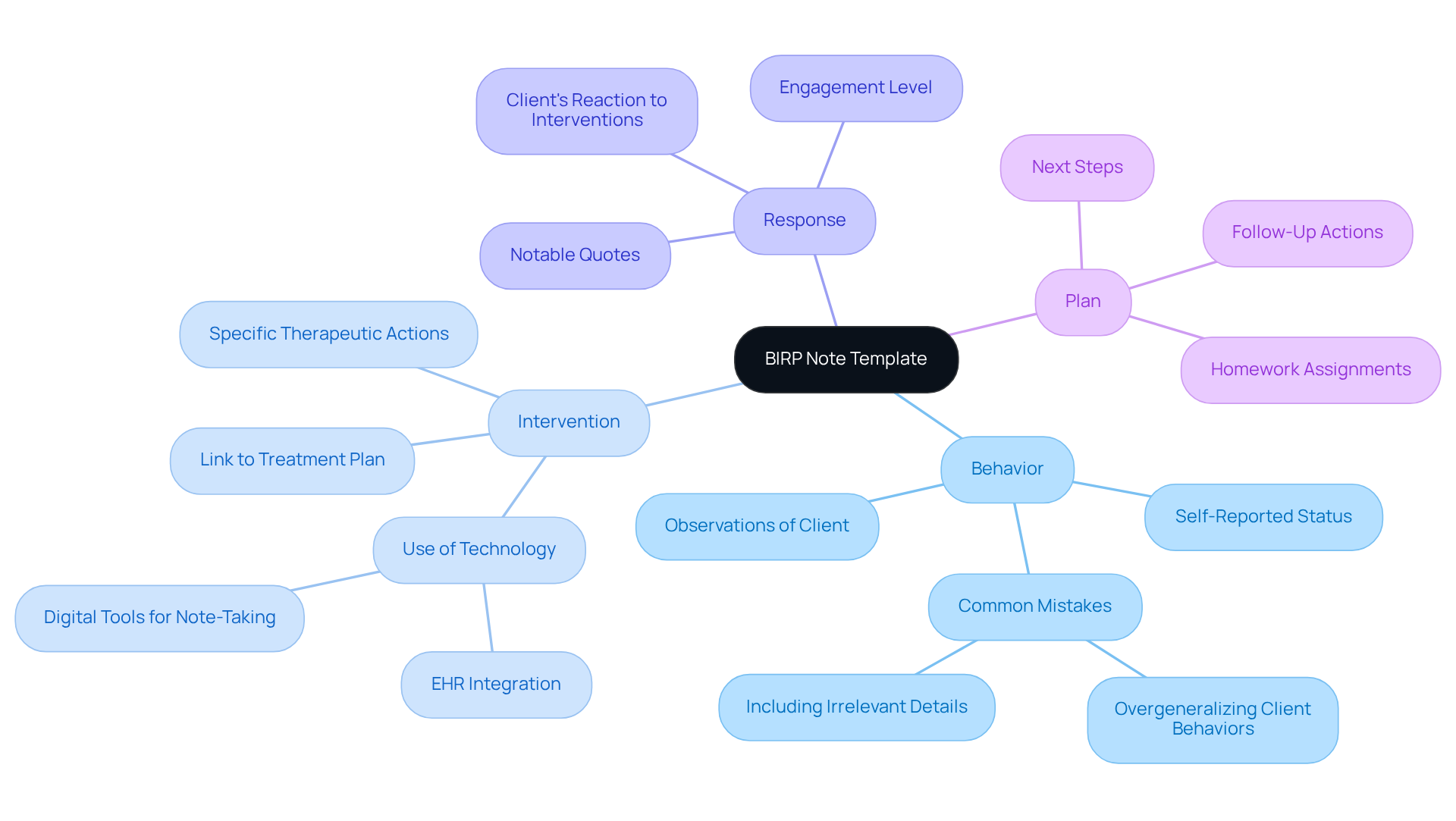
BIRP Note Template: Effective Documentation for Behavioral Health
In the demanding world of behavioral health, the BIRP template serves as a vital tool for documenting interactions, composed of four essential components:
- Behavior
- Intervention
- Response
- Plan
This organized format empowers providers to carefully document individual behaviors, the interventions applied, the responses observed, and the subsequent care plans. Timeliness is crucial; ideally, BIRP records should be finalized within 24-48 hours after each session to maintain accuracy and relevance.
By utilizing this template, behavioral health professionals can achieve thorough documentation that not only supports ongoing treatment but also nurtures patient engagement. Effective BIRP records become a guiding light for future care, enabling clinicians to reflect on progress and adjust strategies as needed. Moreover, the adaptability of BIRP records across various mental health environments, including outpatient and inpatient settings, enhances their versatility.
It’s essential to adhere to HIPAA regulations for the secure storage and access of BIRP records, underscoring the importance of legal compliance in record-keeping. To maintain the integrity of these records, providers should avoid frequent errors, such as overgeneralizing client behaviors or including irrelevant details. Additionally, embracing technology can simplify the BIRP record process, boosting efficiency in reporting.
Ultimately, the improve communication among providers, leading to better outcomes for individuals and continuity of services. How can you ensure your documentation practices foster a supportive environment for your patients? Consider the benefits of a well-structured BIRP approach and the positive impact it can have on your practice.
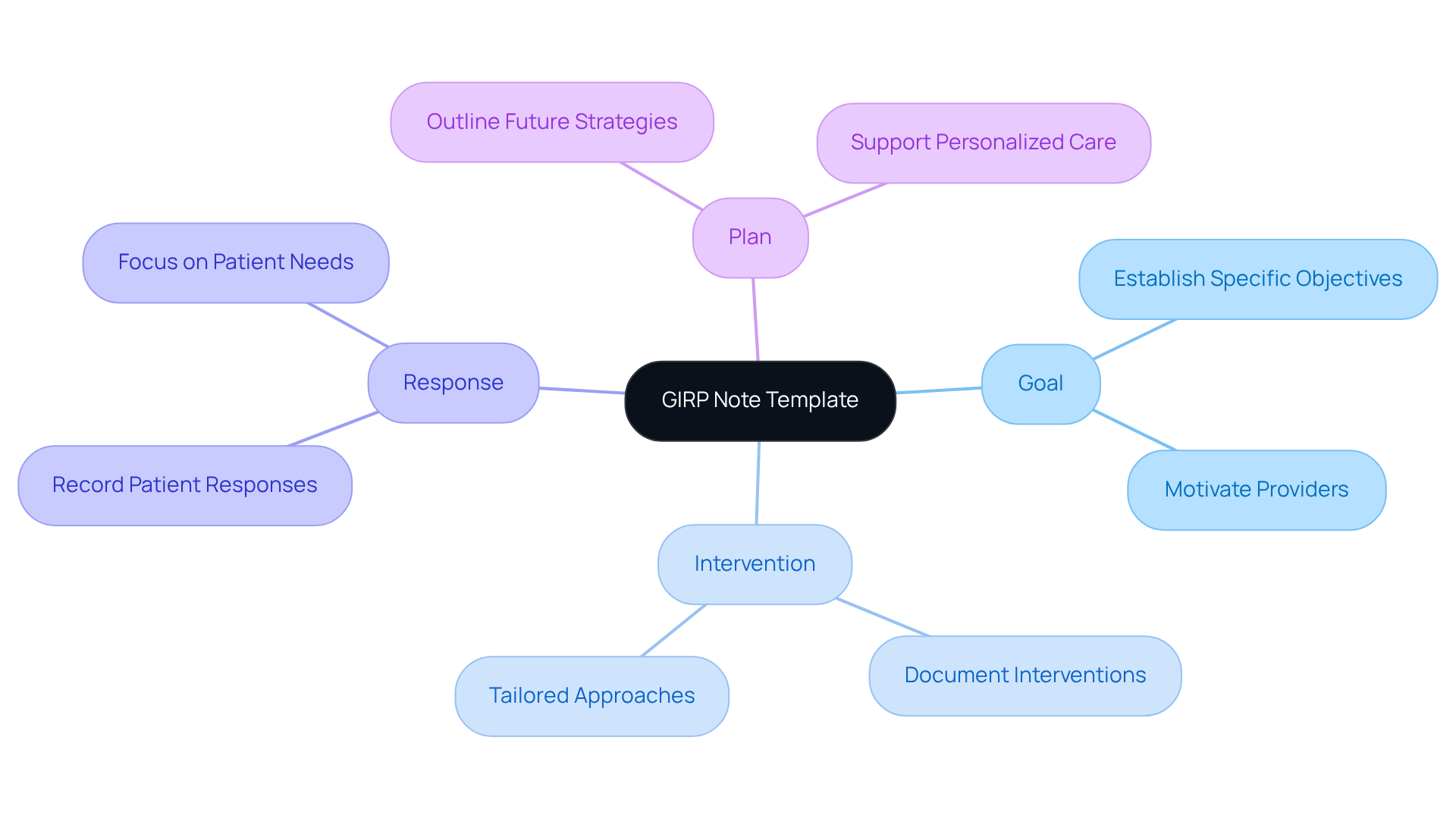
GIRP Note Template: Goal-Oriented Documentation for Patient Care
The medical note template is designed with the intent to enhance goal-oriented documentation in healthcare. It consists of four essential components:
- Goal
- Intervention
- Response
- Plan
This format not only motivates providers to establish specific objectives for treatment but also encourages them to document the interventions employed to achieve those goals. Have you considered how this approach could transform your practice? By recording individuals' responses and outlining strategies for future support, healthcare professionals can genuinely focus on what matters most—their patients.
By concentrating on objectives, the medical note template empowers healthcare providers to improve patient involvement. This approach ensures that treatment is not just a one-size-fits-all solution but is instead tailored to meet personal requirements. Imagine the positive impact this could have on your interactions with patients! With a that acknowledges the unique challenges faced in healthcare, the medical note template provided by GIRP stands as a supportive tool that can facilitate a more personalized and effective treatment journey.
PIRP Note Template: Structured Documentation for Interventions
The PIRP note template serves as a vital, organized format for recording individual treatment interventions, encompassing four essential elements: Problem, Intervention, Response, and Plan. This structured approach empowers healthcare providers to identify the issues they face, document the interventions applied with care, capture individual responses, and outline a thoughtful future treatment plan. By employing the PIRP template, providers not only ensure comprehensive records but also facilitate the assessment of interventions, leading to improved outcomes for those they serve.
In a rapidly evolving healthcare environment, the importance of organized records like the PIRP template becomes increasingly clear. It strengthens the commitment to delivering high-quality care for individuals. Have you ever felt overwhelmed by administrative tasks, wishing to devote more time to your patients? Incorporating generative AI into these record-keeping practices can significantly enhance workflows, allowing healthcare providers to focus more on meaningful interactions with individuals and less on paperwork.
This shift not only alleviates the burden of administrative duties but also nurtures a more compassionate approach to patient care. Imagine a scenario where your time is spent fostering relationships rather than managing records. By embracing tools that streamline documentation, you can create a more supportive environment for both yourself and your patients. Together, let’s .
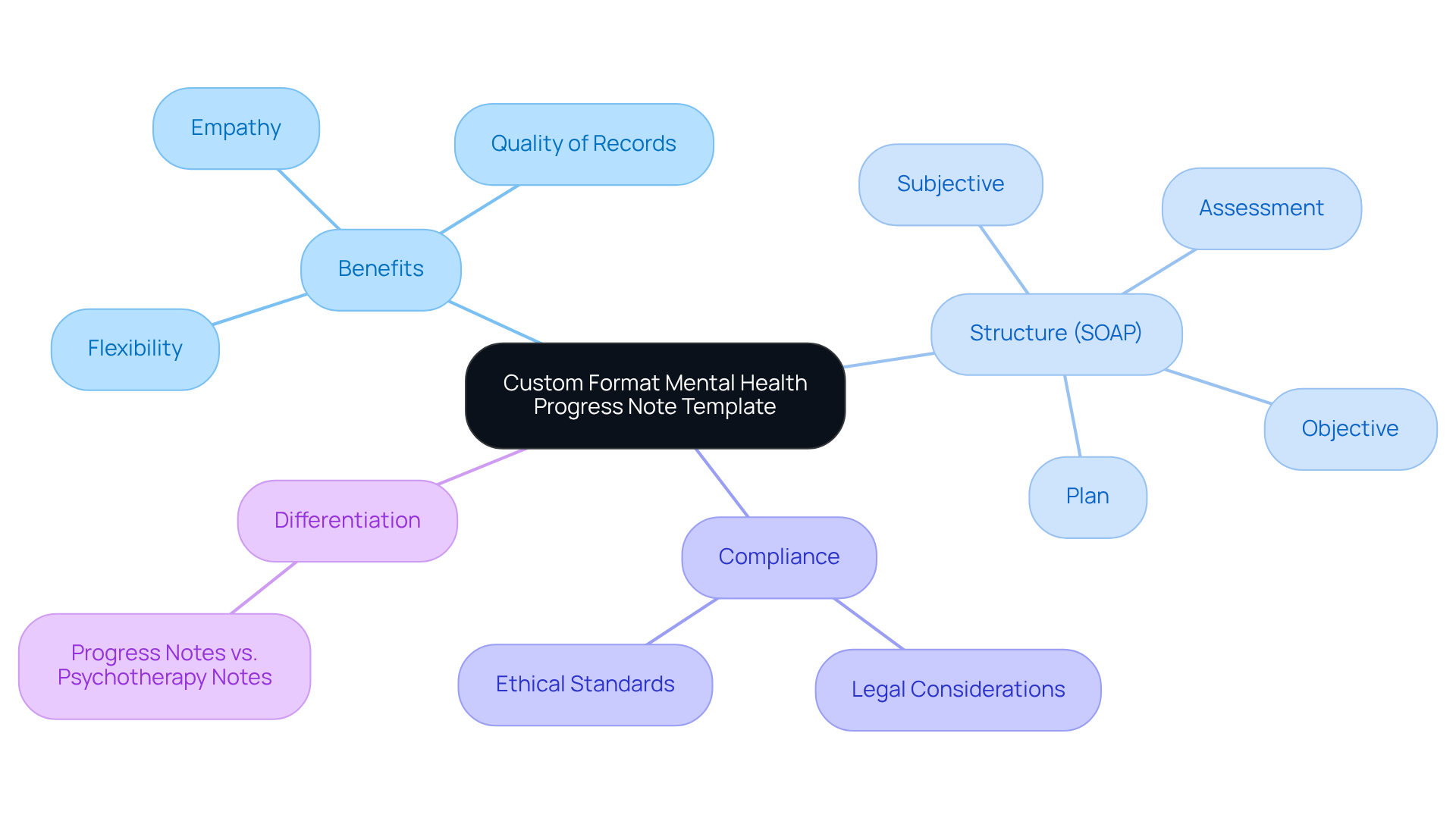
Custom Format Mental Health Progress Note Template: Tailored Documentation Solutions
Mental health providers often face emotional challenges as they navigate the complexities of patient care. The administrative burdens can weigh heavily, impacting the quality of attention given to each client. Custom format medical note templates for mental health progress offer a compassionate solution, providing considerable flexibility in recording. They allow practitioners to tailor their notes to meet the specific needs of their practice and patient demographic.
These templates can include various elements designed for different therapeutic strategies, ensuring that records remain relevant and effective. By utilizing a medical note template, mental health practitioners can significantly enhance the quality of their records, which is essential for monitoring a client's treatment journey and ensuring continuity of care. Progress records serve as both clinical instruments and legal documents, requiring meticulous attention to detail and precision.
For instance, structured formats such as SOAP notes promote thorough record-keeping by organizing information into Subjective, Objective, Assessment, and Plan sections. This organization not only among healthcare providers but also fosters a sense of clarity in the care process. Additionally, prompt and precise record-keeping aids in billing compliance and legal responsibility, ultimately leading to improved outcomes for individuals receiving care.
The use of customized records addresses varied patient needs while cultivating a more empathetic and efficient therapeutic setting. Moreover, CosmaNeura's AI-driven billing suggestions can further enhance billing compliance, improving the overall value of the record-keeping process. It is also crucial to differentiate between progress records and psychotherapy records to uphold client confidentiality and understand the legal implications of documentation.
In this way, we can create a supportive environment that not only meets the administrative needs but also prioritizes the emotional well-being of both practitioners and clients alike.
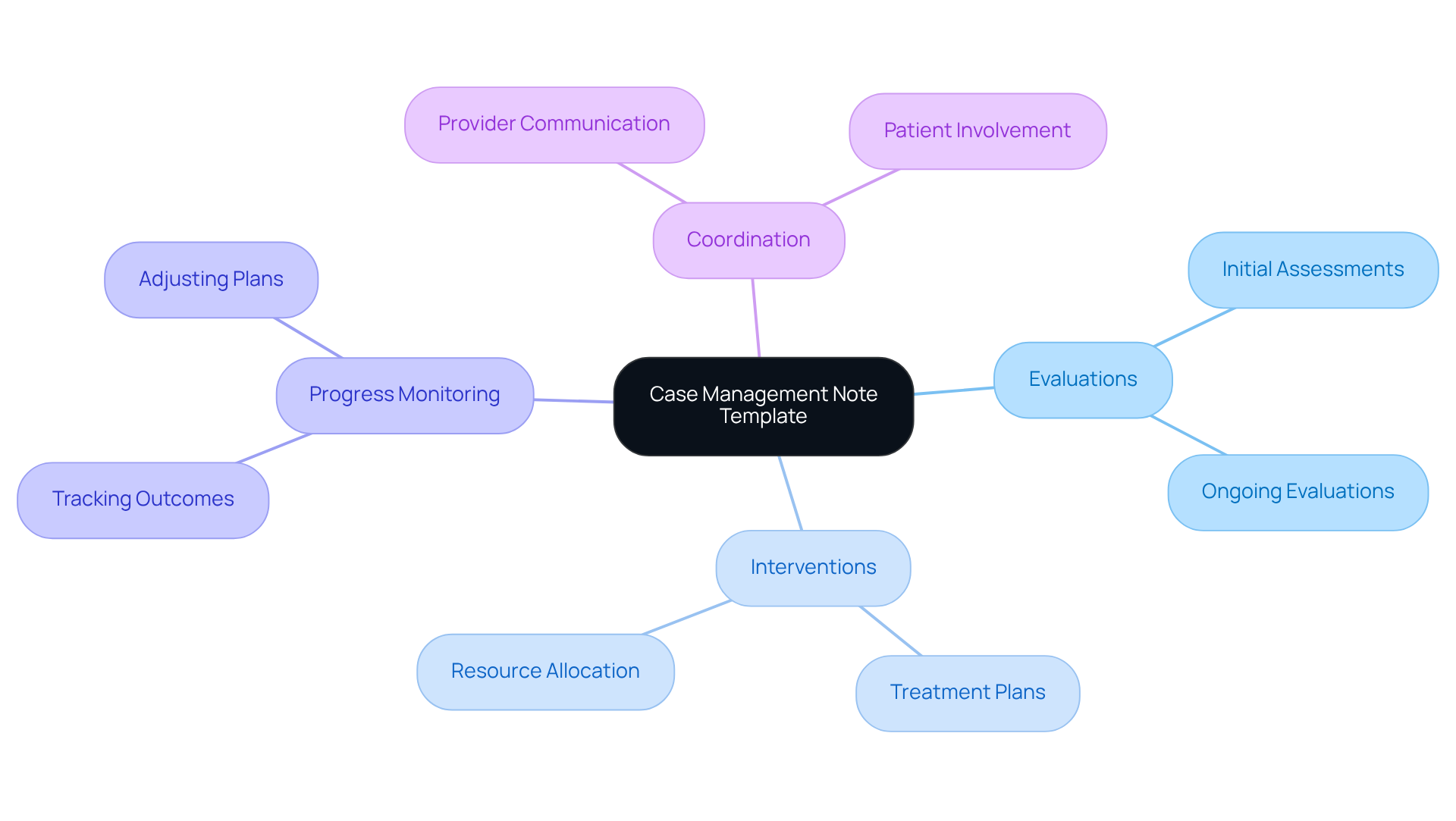
Case Management Note Template: Comprehensive Care Documentation
The case management note template plays a vital role in providing comprehensive support for individuals, especially those facing complex needs. This features sections for evaluations, interventions, progress monitoring, and coordination among various providers. By utilizing this template, case managers can ensure that every aspect of an individual's treatment is meticulously documented, fostering effective communication and collaboration within the healthcare team.
Have you ever considered how thorough health records can significantly enhance patient outcomes? Research reveals that nearly 90% of health system leaders recognize the positive impact of digital tools on their strategies for 2025. Furthermore, efficient record-keeping is linked to improved service coordination, which is essential in addressing challenges like clinician burnout and staff shortages. As healthcare systems increasingly focus on operational efficiencies, the importance of diligent record-keeping in case management becomes even more apparent. It not only streamlines workflows but also cultivates a culture of accountability and quality service, ultimately benefiting both providers and clients alike.
In light of these insights, how can we better support our healthcare teams? Embracing structured documentation practices like the medical note template can pave the way for improved patient care and a more sustainable work environment. Let’s prioritize these essential tools to nurture a compassionate and efficient healthcare system.
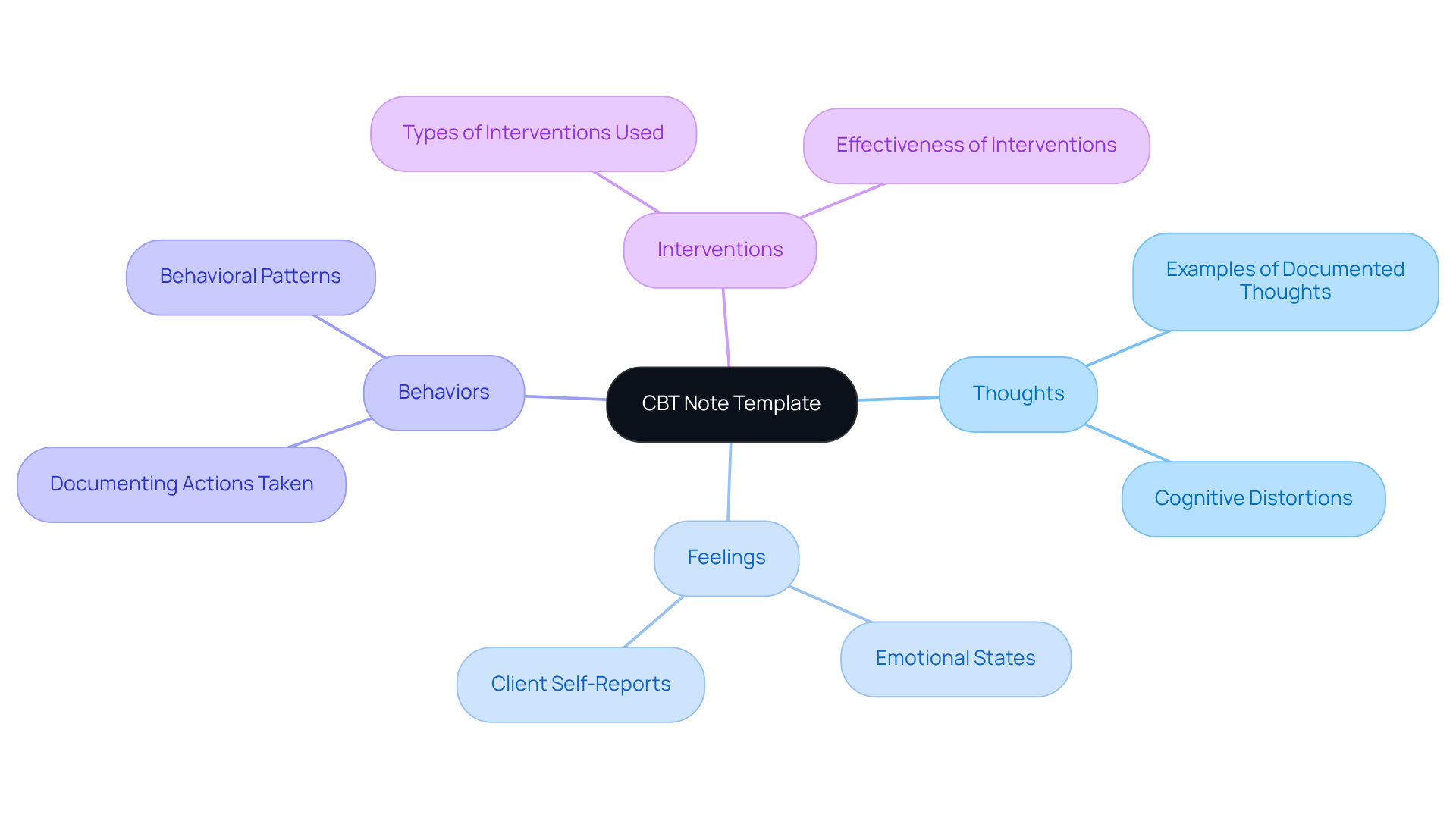
CBT Note Template: Structured Documentation for Therapy Sessions
The CBT note template is thoughtfully designed to support the documentation of therapy sessions within Cognitive Behavioral Therapy. It features dedicated sections for capturing an individual’s thoughts, feelings, behaviors, and the specific interventions used during each session. This organized approach not only aids therapists in monitoring client progress over time but also allows for timely adjustments to treatment plans based on recorded insights. By utilizing this template, therapists can significantly enhance the quality of their records, fostering effective patient engagement and ensuring adherence to best practices.
Have you ever felt overwhelmed by the administrative demands of your practice? Research reveals that organized record-keeping practices in CBT lead to improved outcomes, with a notable increase in compliance rates among therapists who adopt standardized templates. For instance, a recent study found that using CBT note templates resulted in a remarkable 65% compliance rate in record-keeping practices, underscoring their effectiveness in streamlining clinical workflows. Furthermore, 74% of providers report an increase in daily working hours due to the use of EHR, highlighting the vital role of effective record-keeping strategies in alleviating clinician workload.
Case studies further demonstrate the advantages of structured documentation. One example highlighted a therapist who, by consistently using a CBT template, was able to identify patterns in a client’s anxiety reactions, leading to more targeted interventions. This not only strengthened the therapeutic relationship but also contributed to the client’s overall progress. Additionally, documenting collateral contacts, such as interactions with other specialists involved in a client’s support, is essential for providing a comprehensive view of treatment and ensuring coordinated care.
Integrating organized recording methods, like those provided by CBT templates, is crucial for maintaining clarity and continuity in therapy. As experts in the field remind us, "If it’s not documented, it didn’t happen." This practice not only supports the therapeutic process but also , ensuring that records serve their intended purpose of delivering quality care. How can you enhance your documentation practices to better support your clients?
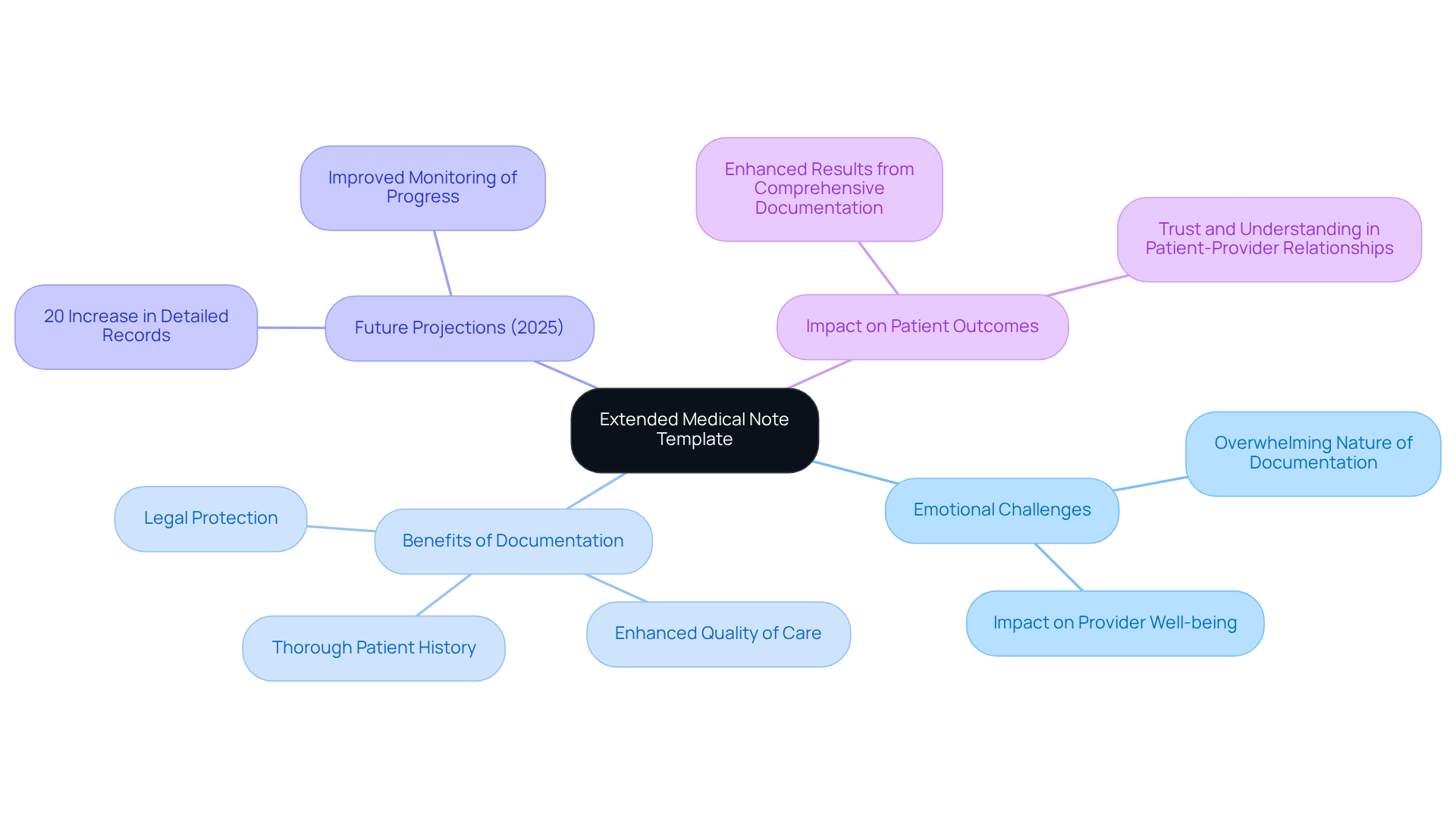
Extended Progress Note Template: Detailed Documentation for Patient Care
In the complex world of healthcare, the emotional challenges faced by providers can feel overwhelming. The extended medical note template is not just a tool; it’s essential for thorough documentation in complicated cases. This organized format allows healthcare providers to gather , current condition, interventions, and future treatment plans. By utilizing the medical note template, providers can ensure that all relevant details are recorded, supporting thorough care and enhancing the quality of interactions between individuals and providers.
As we look ahead to 2025, data suggest a significant shift in practice. Healthcare establishments report a 20% increase in the fulfillment of detailed records, highlighting the growing importance of extended progress records. This enhancement is vital for handling intricate cases, as it enables improved monitoring of progress and more informed clinical decision-making. Have you considered how thorough records can directly impact patient outcomes? Research shows that comprehensive documentation leads to enhanced results, illustrating the relationship between extensive accounts and efficient service delivery.
Comprehensive documentation is not merely a regulatory necessity; it is an essential element of patient-focused support that fosters trust and understanding. In today’s healthcare landscape, where complexity is the norm, the importance of using a medical note template for detailed progress notes cannot be overstated. They play a pivotal role in ensuring high-quality patient care. Let’s embrace the power of thorough documentation together, recognizing its potential to transform our interactions and improve patient experiences.
Conclusion
Recognizing the emotional challenges faced by healthcare providers, the importance of efficient medical documentation comes into focus. The exploration of various medical note templates reveals their transformative potential in healthcare practices. These templates not only streamline the documentation process but also enable providers to dedicate more time to patient care, fostering a compassionate and effective environment.
Administrative burdens can weigh heavily on healthcare professionals, impacting their ability to deliver quality care. Throughout the article, key templates such as:
- SOAP
- DAP
- BIRP
- GIRP
- PIRP
have been discussed, showcasing structured approaches to capturing essential patient information. The integration of AI, exemplified by CosmaNeura, illustrates how technology can alleviate these burdens, enhance accuracy, and ultimately improve patient outcomes. Each template serves a unique purpose, whether focusing on behavioral health, goal-oriented documentation, or comprehensive care coordination, reinforcing the notion that organized records are vital for quality healthcare delivery.
Ultimately, embracing these medical note templates transcends mere compliance or efficiency; it nurtures a healthcare system that prioritizes patient well-being and provider satisfaction. By leveraging structured documentation practices and AI-driven solutions, healthcare professionals can create a more supportive, engaging, and effective environment. This ensures that every patient receives the high-quality care they deserve. The call to action is clear: let us prioritize the adoption of these essential tools to transform healthcare practices for the better.




