Overview
The article highlights the emotional challenges healthcare providers face in managing documentation, particularly the necessity of effective SOAP notes. It acknowledges that the administrative burdens can weigh heavily on professionals, diverting their focus from what truly matters: patient care. By introducing AI-driven solutions, the article illustrates how automating SOAP notes can significantly alleviate these pressures.
Imagine a world where healthcare professionals can devote their time to meaningful patient interactions rather than getting bogged down by paperwork. Automating SOAP notes not only reduces administrative burdens but also enhances the quality of patient care. This allows providers to concentrate on their patients, ultimately improving overall clinical outcomes.
As we reflect on these challenges, consider how embracing technology can lead to a more compassionate healthcare experience. By streamlining documentation, we can foster an environment where healthcare professionals feel supported and empowered. Let’s take a step towards this transformation together, prioritizing both provider well-being and patient care.
Introduction
In the fast-paced world of healthcare, it’s all too easy for the administrative demands on providers to overshadow the core mission of patient care. Many healthcare professionals feel the weight of these responsibilities, which can lead to stress and frustration. The introduction of AI-driven solutions, like CosmaNeura's automation tools, offers a glimmer of hope. These tools promise to alleviate that burden by streamlining the creation of SOAP notes, allowing providers to dedicate more time to their patients.
Yet, as these technologies gain traction, important concerns arise. How will they impact the quality of care? Can we ensure that empathetic communication remains at the forefront of our interactions? It’s vital for healthcare providers to find a way to balance the efficiency gained through automation with the essential human touch that defines compassionate care.
This balance is not just a goal; it’s a necessity. By embracing these innovations while remaining committed to the emotional and relational aspects of care, we can create a healthcare environment that truly supports both providers and patients. Together, let’s explore how we can integrate technology in a way that enhances our ability to connect with those we serve, fostering a culture of compassion and understanding.
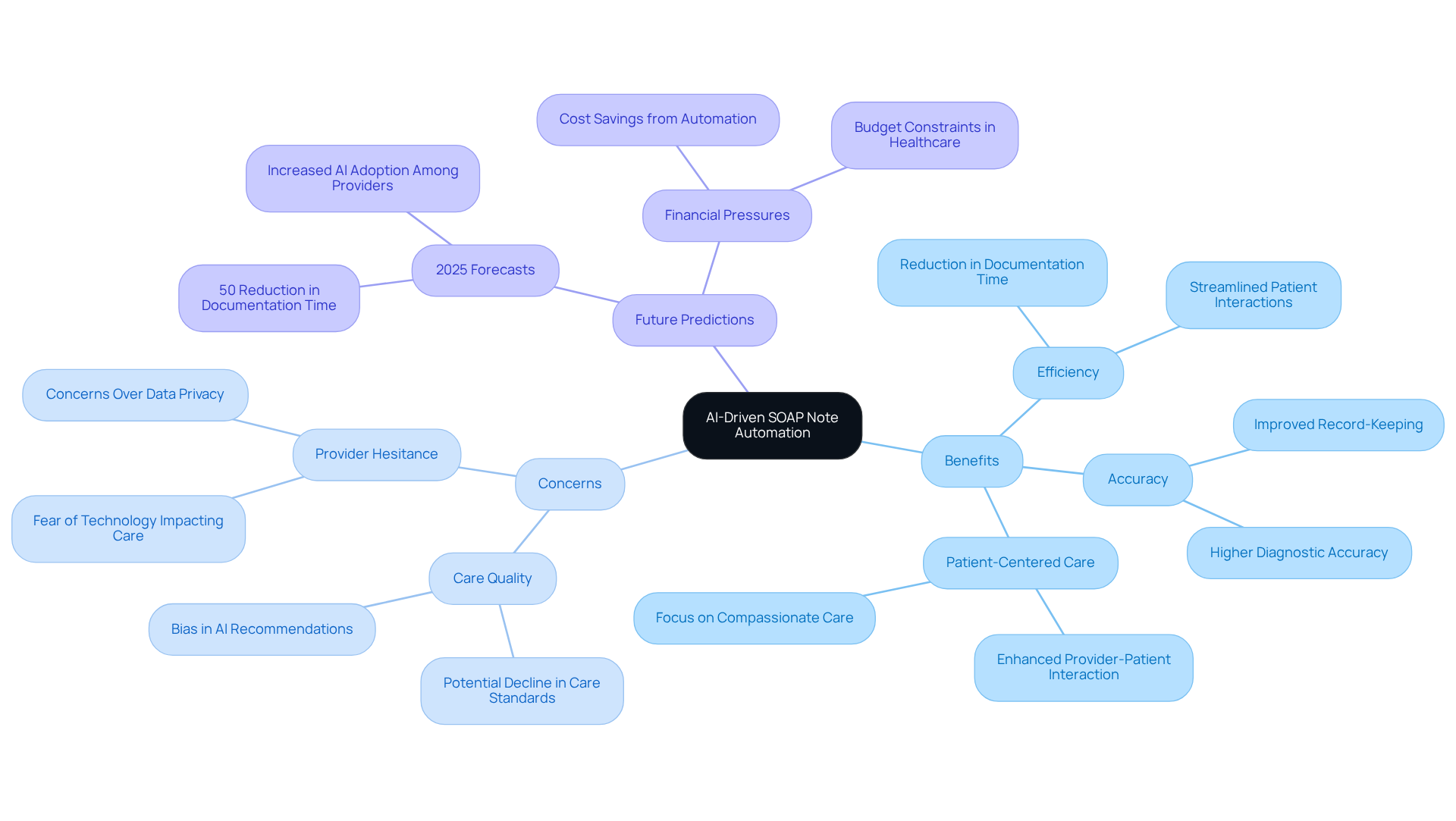
CosmaNeura: AI-Driven SOAP Note Automation for Healthcare Providers
Healthcare professionals often face overwhelming administrative burdens that can detract from their ability to provide the compassionate care their patients deserve. CosmaNeura offers a solution through advanced AI technology, automating the generation of SOAP notes. This innovation significantly reduces the time spent on documentation, allowing practitioners to prioritize meaningful client interactions. By ensuring that empathetic support remains central to their practice, healthcare providers can truly focus on what matters most—their patients.
The benefits of this optimization extend beyond efficiency; they align with the ethical principles of Catholic teachings, reinforcing a commitment to respectful and humane treatment of patients. However, it's understandable that many healthcare professionals may feel hesitant to embrace such innovative solutions due to concerns about the potential impact on care quality. As we look toward 2025, healthcare leaders recognize that AI can greatly enhance provider efficiency. Forecasts suggest that clinicians could reduce time spent on clinical record-keeping tasks by 50% through generative AI technologies integrated into electronic health records.
Moreover, automating SOAP notes can enhance the review of systems SOAP note example, leading to improved accuracy and consistency in record-keeping—an essential component for effective patient management. Recent advancements in AI for healthcare documentation indicate that AI-generated reports demonstrate a 14.5% improvement in accuracy compared to traditional methods. This underscores the potential of AI to , ultimately benefiting both providers and patients alike.
By adopting these innovative solutions, healthcare professionals can alleviate administrative burdens and foster a more patient-centered approach to care. This shift not only addresses the increasing financial pressures that challenge healthcare organizations but also reaffirms a commitment to providing the highest quality of care. Are you ready to explore how these advancements can transform your practice and enhance the care you provide?
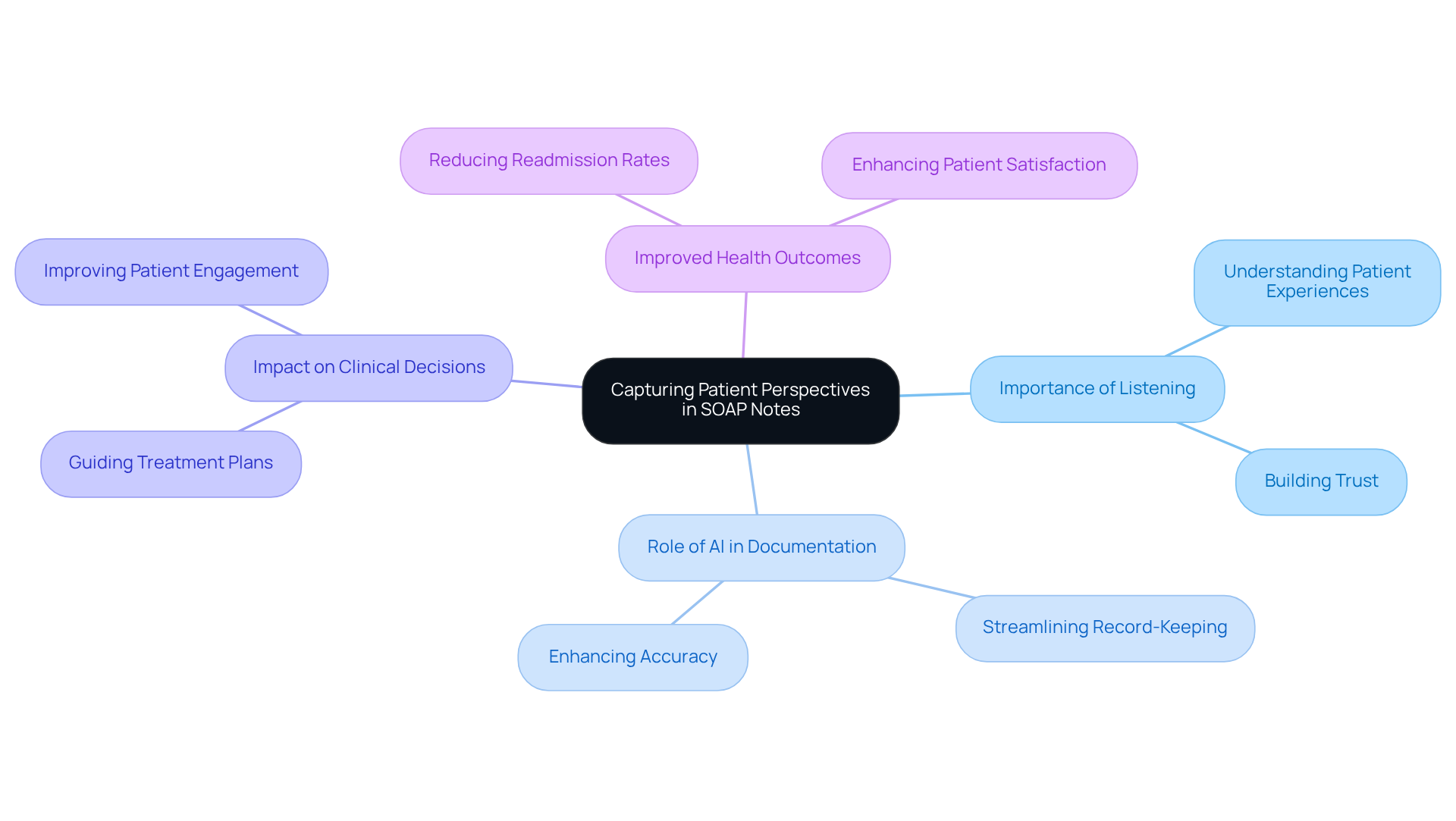
Subjective: Capturing Patient Perspectives in SOAP Notes
The subjective part of SOAP notes highlights the importance of understanding an individual's personal experiences, feelings, and concerns. Have you ever considered how vital it is for caregivers to actively listen and record these viewpoints? They provide essential context for the patient's condition and significantly guide clinical decisions.
By utilizing generative AI, healthcare providers can streamline the record-keeping process. This technology ensures that subjective data is captured efficiently and accurately. Imagine how much easier it would be for physicians if they could alleviate the administrative burden while fostering a stronger patient-provider relationship. With more time for meaningful interactions, the .
Effective documentation of subjective data, enhanced by AI tools, ultimately contributes to improved health outcomes. This compassionate approach not only addresses the challenges faced by healthcare providers but also emphasizes the importance of nurturing the patient experience. Let’s embrace these advancements together for a brighter future in healthcare.
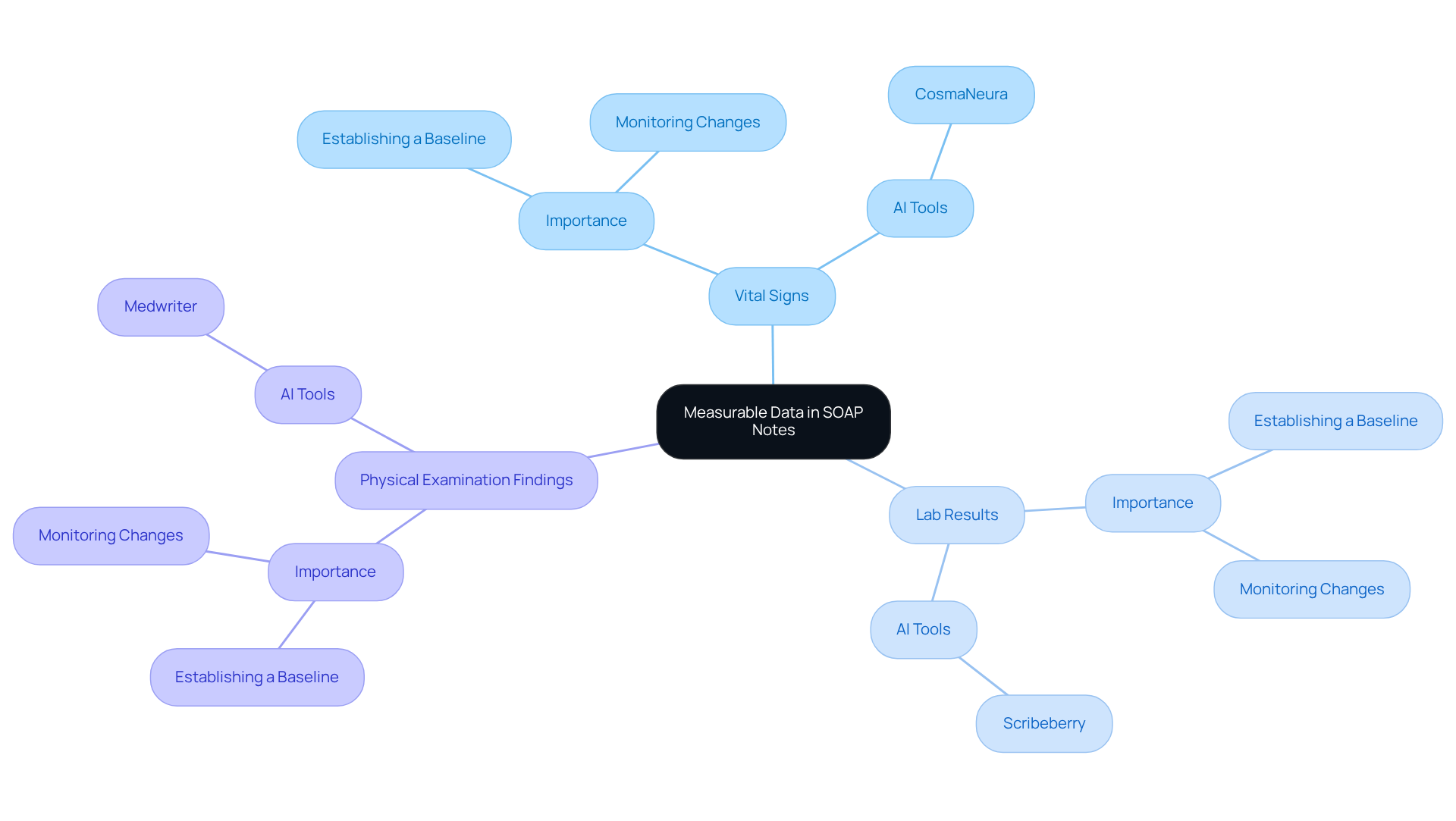
Objective: Documenting Measurable Data in SOAP Notes
In the demanding world of healthcare, the objective section of SOAP notes plays a vital role. It includes measurable data such as vital signs, lab results, and physical examination findings. This information is essential for establishing a baseline and in a patient's condition over time. Have you ever felt overwhelmed by the administrative tasks that take your focus away from patient care?
By utilizing AI tools like those offered by CosmaNeura, practitioners can ensure that objective data is accurately captured and easily accessible. This not only enhances clinical decision-making but also alleviates some of the burdens healthcare providers face. Imagine being able to spend more time on what truly matters—your clients' wellbeing—rather than getting lost in paperwork.
Generative AI technology simplifies the documentation process, allowing healthcare providers to concentrate on delivering quality care. This improvement in efficiency leads to better outcomes for individuals, fostering a more compassionate healthcare environment. Let's embrace these innovative solutions together, ensuring that every patient receives the attention and care they deserve.
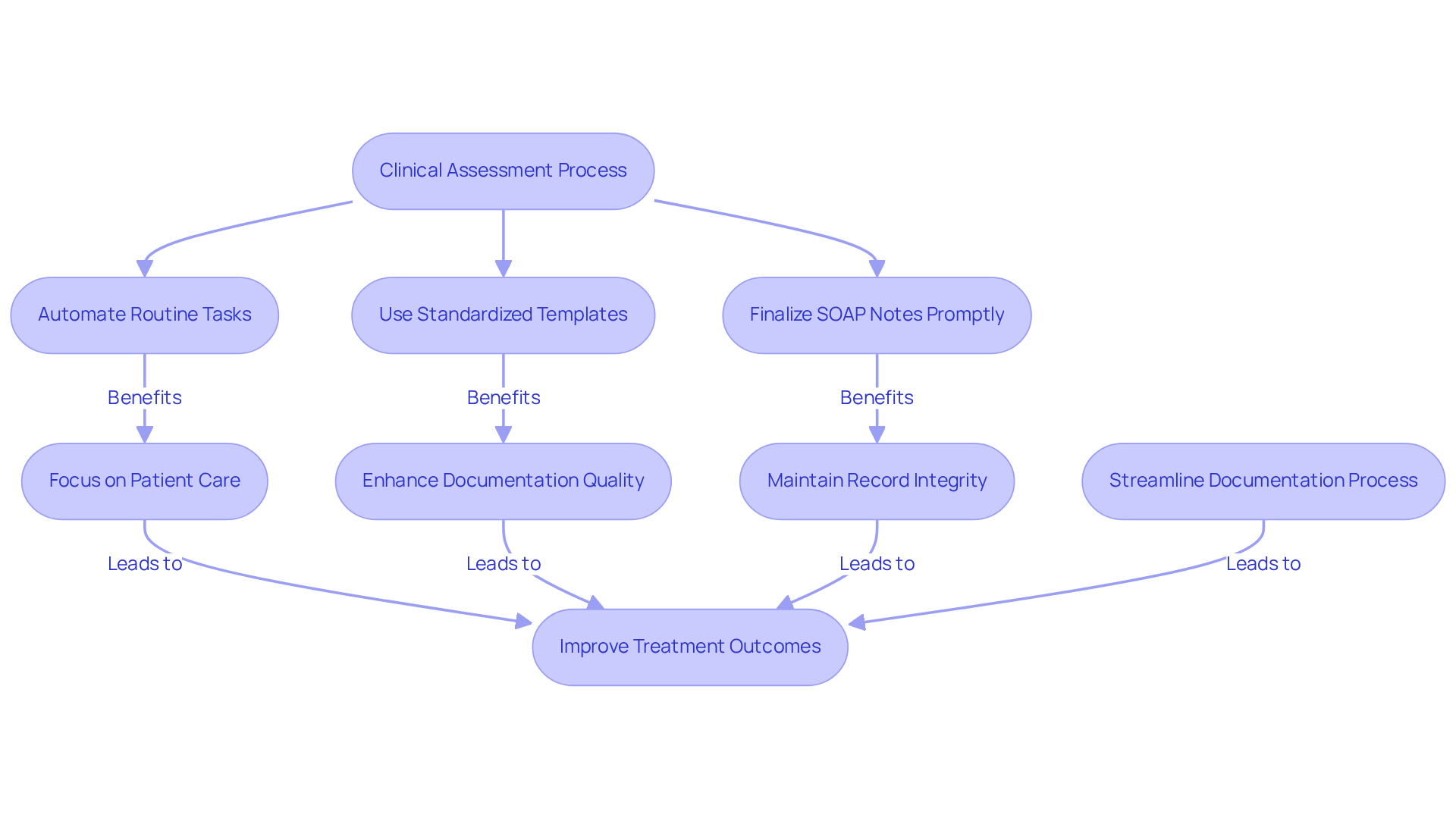
Assessment: Synthesizing Information for Clinical Judgment in SOAP Notes
The evaluation segment is vital in merging subjective and objective information to form a clinical judgment about the individual's condition. Practitioners face the emotional challenge of critically evaluating gathered information, striving to arrive at the most suitable diagnosis or problem list. Effective evaluations are essential, as they directly influence treatment strategies and ensure that support is tailored to meet the unique needs of each individual. By carefully analyzing the data, healthcare professionals can enhance the standard of service, ultimately improving outcomes for those receiving treatment. Recent research highlights the importance of clinical judgment in patient care, emphasizing that thorough assessments are foundational to effective treatment strategies.
Incorporating innovative AI solutions, such as CosmaNeura's Agentic Platform, can significantly ease the administrative burdens that often impede the assessment process. By automating routine record-keeping tasks and streamlining workflows, generative AI allows healthcare providers to focus more on critical clinical judgments rather than becoming overwhelmed by paperwork. This technology not only boosts the efficiency of SOAP note writing but also ensures that assessments are completed on time, maintaining the quality of records.
To avoid common pitfalls, it is crucial to sign and date SOAP note entries, ensuring accountability and accuracy. Additionally, finalizing SOAP notes within 24-48 hours is essential for preserving the integrity of the records. Providers should remain vigilant about potential challenges in SOAP note writing, such as incomplete records or excessive reliance on templates, which can undermine the quality of client treatment. Utilizing , particularly those enhanced by generative AI, can streamline the process of creating a review of systems soap note example, enhancing both efficiency and effectiveness in documentation.
Key Solutions to Consider:
- Automate routine tasks to focus on patient care.
- Finalize SOAP notes promptly to maintain record integrity.
- Use standardized templates to enhance documentation quality.
By embracing these strategies, healthcare providers can alleviate some of the burdens they face, ultimately leading to better patient care. How can you integrate these solutions into your practice today?
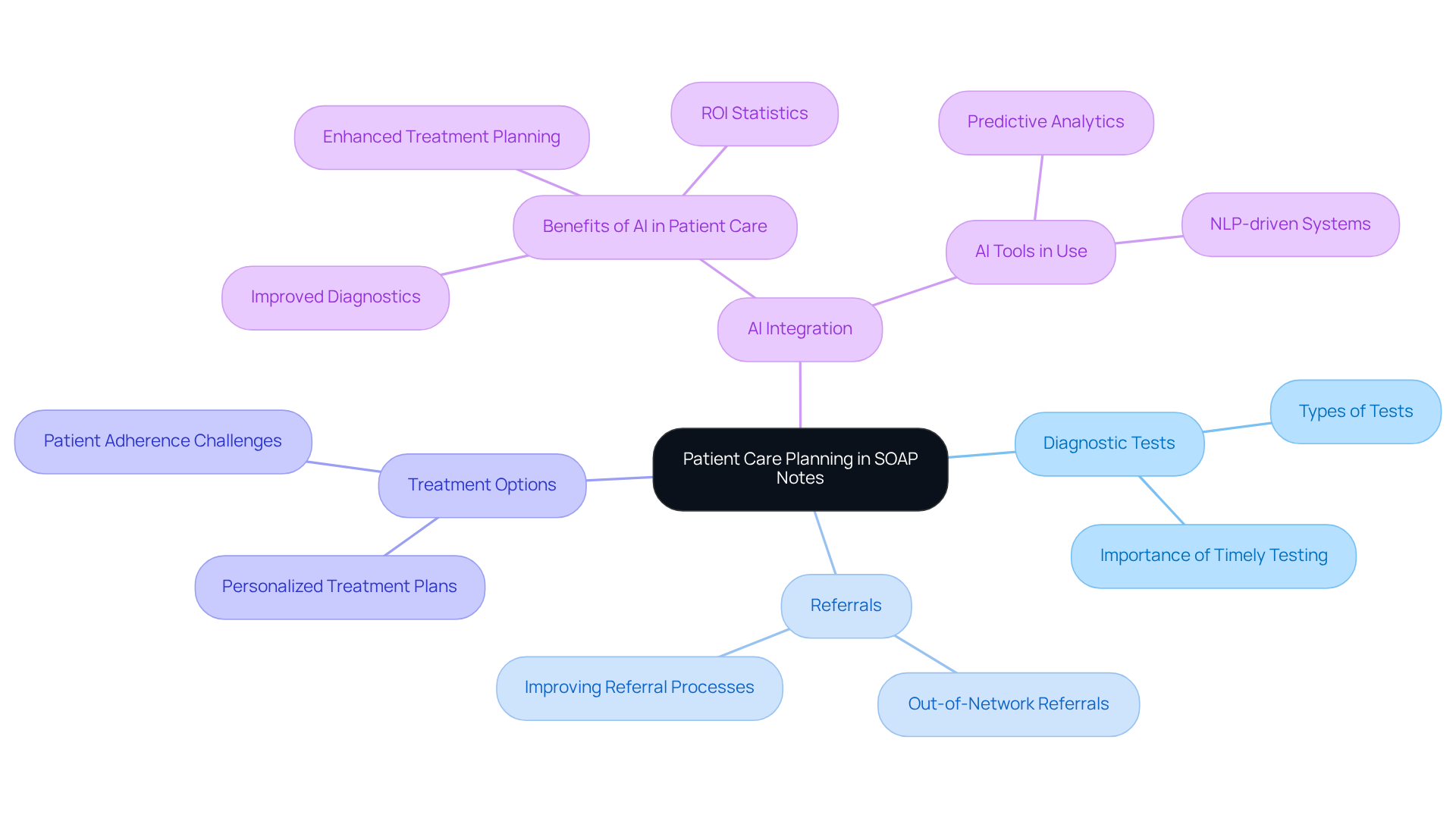
Plan: Outlining Next Steps in Patient Care within SOAP Notes
The plan segment of SOAP notes plays a vital role in outlining the next steps in client management, including diagnostic tests, referrals, and treatment options. This aspect is essential for ensuring continuity of support and effectively communicating the support strategy to other healthcare team members.
How often do you feel overwhelmed by the administrative burdens of patient care? Utilizing can alleviate some of that pressure, allowing providers to create detailed treatment plans that are guided by the most recent clinical guidelines and tailored to the unique situations of each individual.
For instance, AI-driven systems can analyze historical and current individual data to anticipate potential complications and recommend appropriate interventions. This not only enhances the quality of service but also fosters a deeper connection with patients. As the healthcare landscape evolves, the integration of AI in treatment planning is becoming increasingly important.
Did you know that hospitals that adopt AI report an impressive return on investment of $3.20 for every dollar spent, often within just 14 months?
This statistic highlights the significant benefits of embracing advanced technologies to improve patient outcomes and streamline care processes. By incorporating AI into your practice, you can not only enhance the efficiency of your work but also ensure that your patients receive the highest level of care.
Let’s explore how these tools can support you in your mission to provide compassionate and effective healthcare.
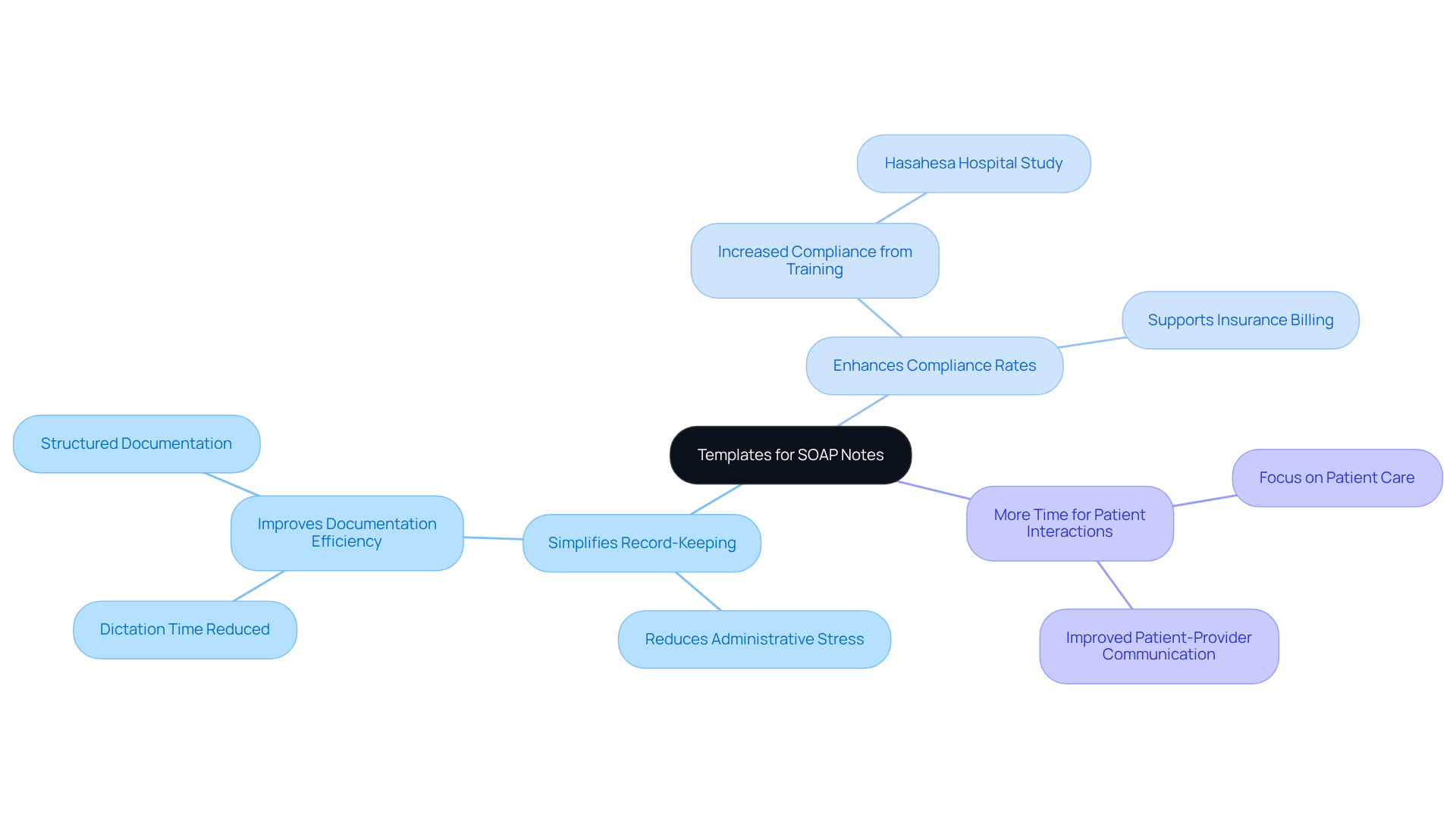
Templates: Streamlining SOAP Note Documentation for Consistency
In the demanding world of healthcare, administrative burdens can often weigh heavily on providers, leading to stress and burnout. Utilizing templates for a can significantly ease this burden, ensuring that all essential information is consistently captured. Imagine if generative AI could automate data entry and compliance checks within these templates. This not only alleviates the administrative load but also allows healthcare professionals to focus more on what truly matters: patient care.
Templates can be customized to meet the specific needs of various specialties or groups, making them a versatile resource. Research shows that organized record-keeping methods can lead to a remarkable increase in compliance. For instance, a study at Hasahesa Hospital revealed an improvement from 38.2% to 87.2% after focused training. This shift simplifies record-keeping and empowers professionals to dedicate more time to supporting their clients.
Moreover, standardized records have been linked to enhanced healthcare efficiency. By reducing the time spent on administrative tasks, providers can engage more meaningfully with their patients. By adopting these practices, healthcare professionals can create a review of systems soap note example that ensures their records are both thorough and efficient, ultimately improving the quality of care they provide.
Key Benefits of Using Templates for SOAP Notes:
- Simplifies record-keeping, reducing administrative stress.
- Enhances compliance rates, leading to better patient outcomes.
- Allows more time for meaningful patient interactions.
By embracing these solutions, you can foster a more compassionate and effective healthcare environment. How might these changes impact your daily practice and patient relationships?
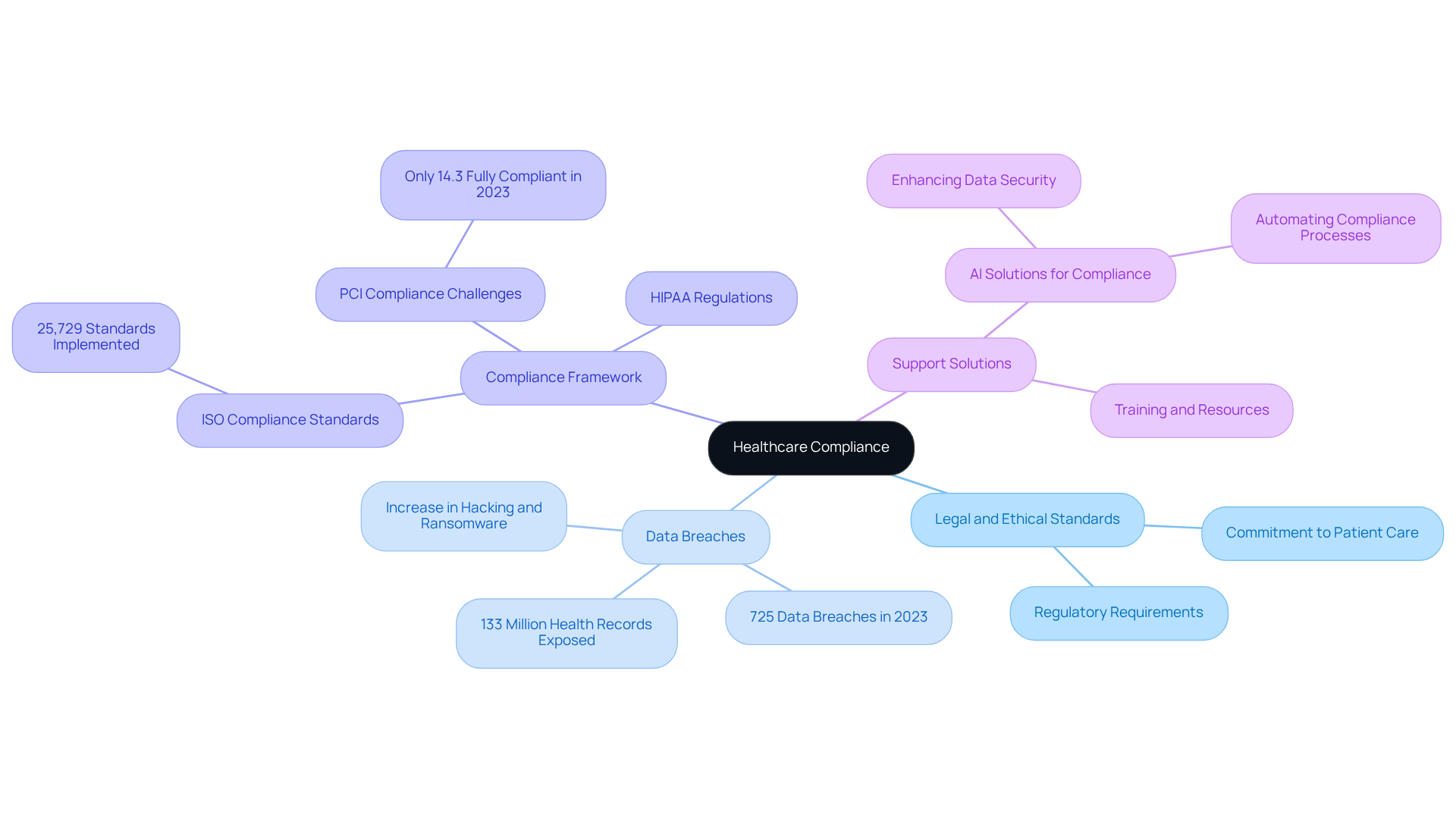
Compliance: Ensuring Legal and Ethical Standards in SOAP Notes
In the demanding world of healthcare, compliance with legal and ethical standards is not just a requirement; it’s a commitment to patient care. Providers often face emotional challenges when ensuring the accuracy, completeness, and security of their review of systems soap note example. The stakes are high, as protecting patient confidentiality is crucial in meeting regulatory requirements.
Consider the urgency of this issue: in January 2023, the HIPAA Journal reported 725 data breaches, exposing over 133 million health records. This alarming statistic highlights the pressing need for compliance in safeguarding sensitive information. Furthermore, the ISO has established an extensive framework of 25,729 international compliance standards, underscoring the complexities healthcare practitioners navigate daily.
To support professionals in upholding compliance, CosmaNeura offers AI solutions designed to protect sensitive information while promoting ethical record-keeping practices. With 85% of companies acknowledging that in the past three years, the need for effective solutions is more critical than ever.
This dedication to ethical standards in documentation reflects a broader commitment to responsible healthcare. It resonates deeply with the values upheld by faith-based organizations, reminding us of our shared responsibility to protect those we serve. How can we, as a community, ensure that our practices not only meet regulatory requirements but also nurture trust and compassion in our patient relationships? Let’s engage in this vital conversation together.
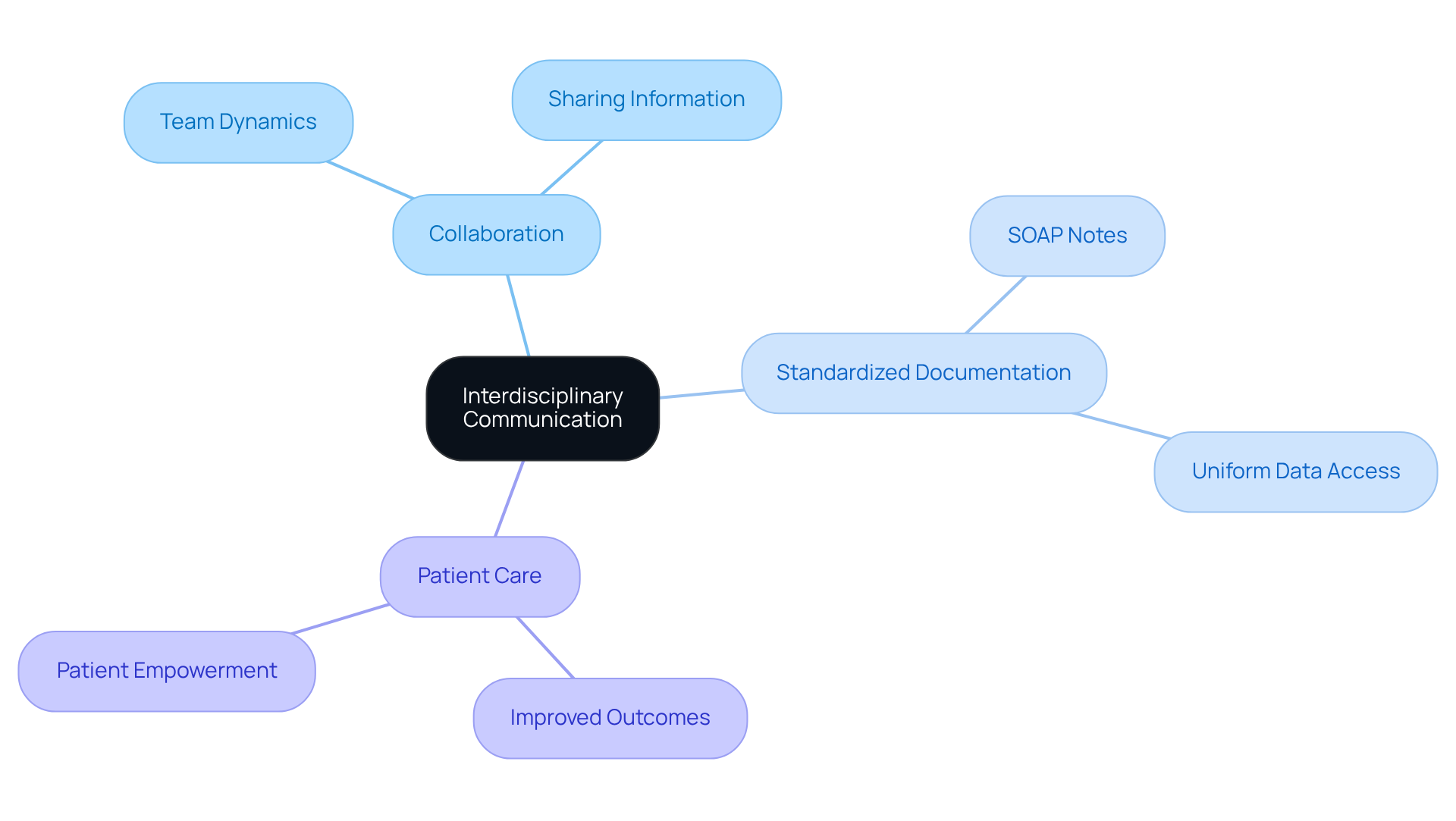
Interdisciplinary Communication: Enhancing Collaboration through SOAP Notes
In the demanding world of healthcare, communication can often feel overwhelming. The review of systems SOAP note example serves as an essential tool that not only enhances collaboration among interdisciplinary teams but also alleviates some of that burden. By recording vital information in a standardized format, providers ensure that every team member has access to uniform and precise data, crucial for delivering coordinated support.
This organized approach fosters a cooperative atmosphere where the focus remains on individual patient needs. Imagine how empowering it is for healthcare providers to have streamlined communication that simplifies the sharing of essential information. This ultimately strengthens team dynamics and provided.
By embracing standardized documentation, we can create a nurturing environment that enhances outcomes for individuals. Let’s reflect on how the review of systems SOAP note example can transform our practice, encouraging a culture of collaboration and care. Together, we can ensure that our patients receive the compassionate support they deserve.
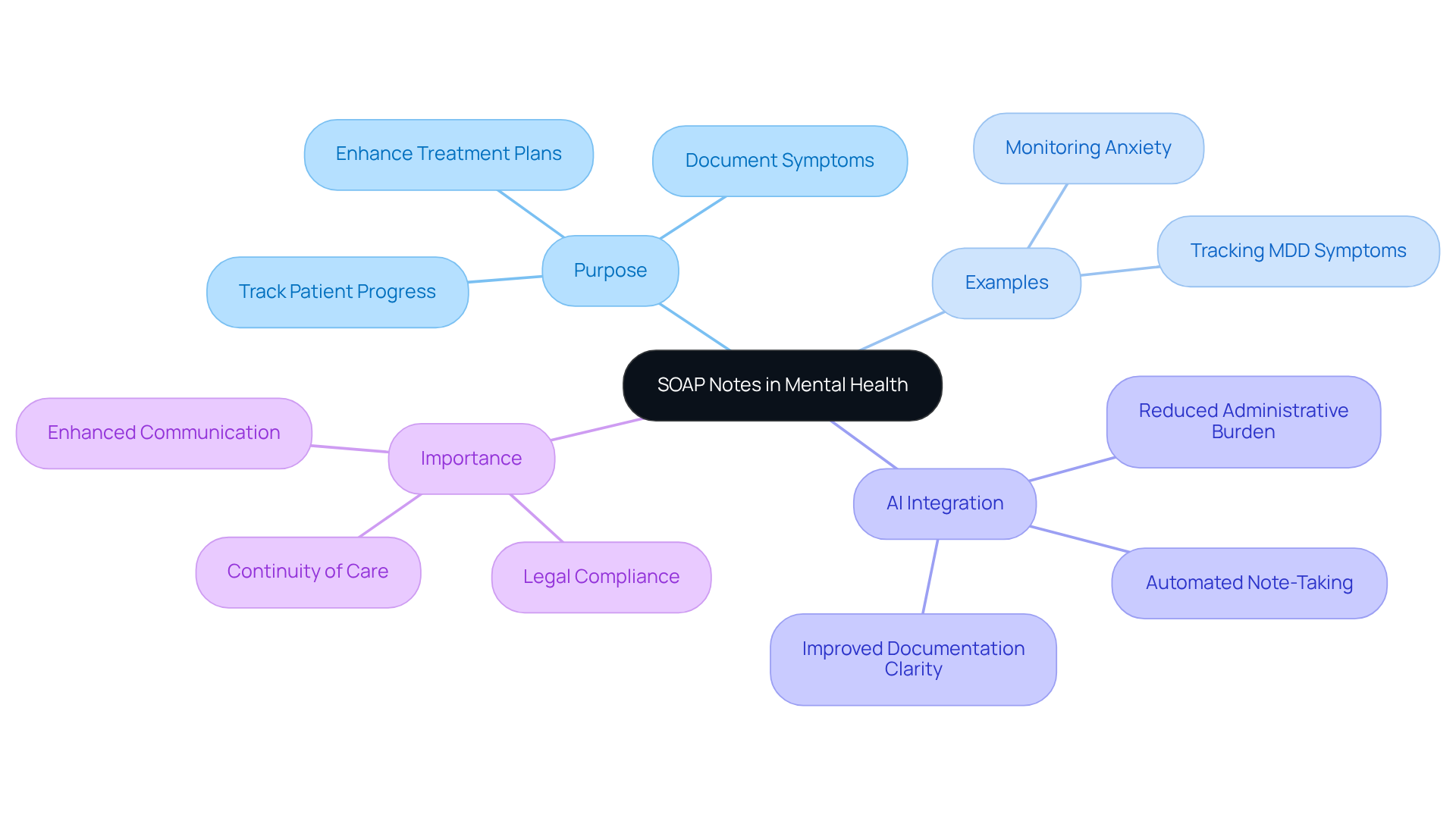
Mental Health Applications: Utilizing SOAP Notes for Patient Progress Tracking
In the realm of mental health support, the review of systems SOAP note example serves as a vital tool for tracking individual progress over time. They empower providers to document changes in symptoms, treatment responses, and feedback from individuals—elements that are essential for making informed adjustments to care plans. For instance, when a patient diagnosed with Major Depressive Disorder (MDD) shares feelings of hopelessness and fatigue, these insights can be carefully recorded in the subjective section of the SOAP note. This organized documentation allows clinicians to and the effectiveness of interventions.
Moreover, integrating AI tools can significantly enhance documentation practices, easing the administrative burdens that often accompany scheduling and managing medical records. By automating the note-taking process, mental health professionals can capture the nuances of client experiences and progress without the weight of manual entry. This not only saves time but also improves the clarity and consistency of records, ultimately leading to better outcomes for those receiving care. For example, an individual with a 6-month history of escalating anxiety symptoms can have their progress effectively tracked through well-organized SOAP notes, facilitating timely interventions.
The importance of recording changes in mental health services cannot be overstated. Regularly updated SOAP notes serve as a review of systems SOAP note example, providing a clear view of a patient's journey and enabling adjustments in treatment strategies based on documented evidence. As specialists often highlight, proper record-keeping supports legal adherence and enhances communication among healthcare professionals, ensuring continuity of care. By mastering the use of SOAP notes and leveraging generative AI, clinicians can foster a culture of comprehensive record-keeping that greatly improves therapeutic progress tracking and the overall quality of care.
How can you enhance your practice today? Embrace the power of effective documentation and AI integration to alleviate your workload and focus more on what truly matters—your patients' well-being.
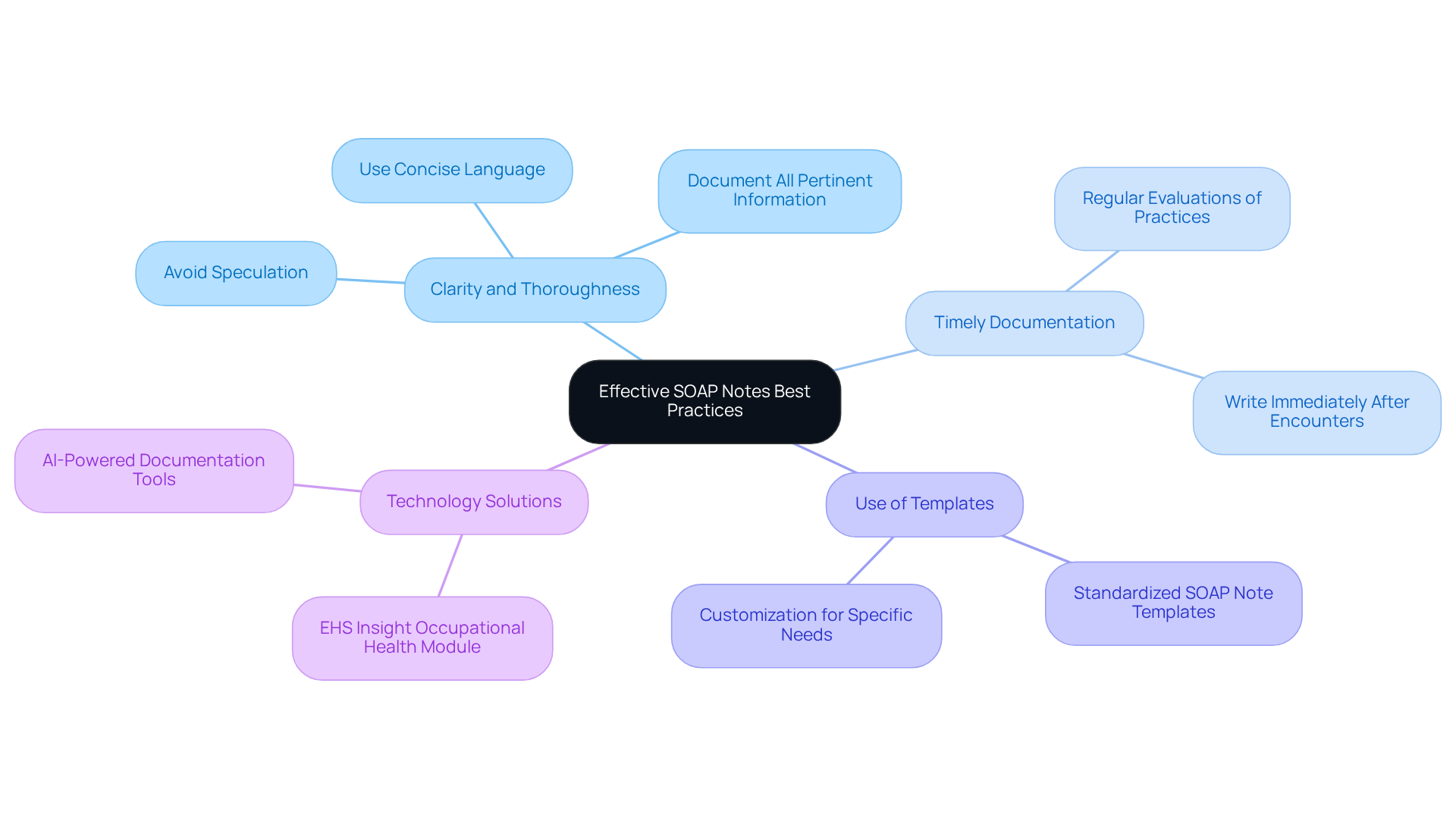
Best Practices: Writing Effective SOAP Notes for Optimal Patient Care
Crafting effective SOAP notes can be a challenge for many healthcare providers, often leaving them feeling overwhelmed. To address these emotional burdens, it's essential to prioritize . By using concise, objective language and ensuring all pertinent information is documented, you can alleviate some of this stress. Regular evaluations and updates of record-keeping practices are crucial for maintaining high-quality SOAP notes.
Have you ever noticed how composing SOAP notes right after encounters with individuals can significantly improve accuracy? This simple practice lowers the chance of leaving out essential details, making your job easier. Additionally, utilizing organized templates can simplify the record-keeping process, helping you consistently capture vital information without added strain.
Recent trends show an increasing reliance on technology-driven solutions to enhance record-keeping efficiency. This not only promotes better healthcare outcomes but also aligns with industry standards. Imagine how implementing these best practices could enhance your documentation efficiency, leading to improved patient care and satisfaction. By taking these steps, you can create a more nurturing environment for both yourself and your patients.
Conclusion
The integration of AI-driven solutions like CosmaNeura into the healthcare documentation process signifies a transformative shift in the utilization of SOAP notes. By automating the generation of these essential documents, healthcare providers can alleviate significant administrative burdens, allowing them to devote more time to patient care. This enhancement not only boosts the efficiency of clinical practices but also aligns with ethical commitments to compassionate treatment, ultimately fostering a more patient-centered approach.
Throughout this article, we have shared key insights into the multifaceted applications of SOAP notes in clinical settings. From capturing subjective patient experiences to documenting objective data, synthesizing assessments, and outlining treatment plans, each component plays a vital role in ensuring comprehensive patient care. The advantages of utilizing standardized templates and AI tools are evident, as they promote consistency, accuracy, and improved communication among interdisciplinary teams.
As the healthcare landscape continues to evolve, embracing these innovative practices becomes essential for enhancing the quality of care provided to patients. By prioritizing effective documentation and leveraging advanced technologies, healthcare professionals can cultivate a more efficient and compassionate environment. The call to action is clear: how can we explore these advancements to not only alleviate administrative stress but also enrich the patient experience and outcomes?




