Overview
This article addresses the emotional challenges faced by healthcare providers in documenting patient care. It highlights how administrative burdens can weigh heavily on professionals, impacting their ability to deliver the compassionate care that patients deserve. By providing examples of effective charting notes, it emphasizes the importance of structured and clear records in enhancing patient care.
To support healthcare professionals, the article outlines various documentation methods, such as:
- SOAP notes
- Clinical notes
These approaches not only improve communication but also ensure legal compliance, ultimately leading to better patient outcomes. Accurate and timely record-keeping practices are essential for nurturing the patient-provider relationship.
Are you feeling overwhelmed by the demands of documentation? You're not alone. Many healthcare providers share this experience, and understanding how to streamline these processes can make a significant difference. By embracing effective charting techniques, you can alleviate some of the administrative burdens and focus more on what truly matters—your patients.
In summary, this article serves as a gentle reminder of the value of clear and structured documentation. By adopting these practices, you can enhance your ability to provide compassionate care while ensuring that your records support both you and your patients. Let’s take this step together towards improving patient care through thoughtful documentation.
Introduction
Effective healthcare documentation serves as the backbone of quality patient care. Yet, many providers feel overwhelmed by administrative tasks that pull them away from their primary mission: caring for individuals. This article delves into ten compelling examples of charting notes that not only enhance record-keeping but also streamline processes through innovative solutions, such as AI-powered tools.
How can healthcare professionals navigate the tension between thorough documentation and meaningful patient interaction? What strategies can they adopt to ensure their notes are both effective and compassionate? By exploring these questions, we aim to provide insights that resonate with your experiences and support your journey in delivering exceptional care.
CosmaNeura: AI-Powered Charting Solutions for Healthcare Providers
CosmaNeura introduces an innovative AI platform designed specifically for primary health providers who uphold Christian values. Are you feeling overwhelmed by administrative tasks? This platform automates essential processes such as client intake and triage, allowing healthcare professionals to dedicate more time to compassionate care.
Imagine a solution that not only improves operational efficiency but also aligns with ethical medical practices rooted in Catholic teachings. With advanced AI features, the platform serves as a charting notes example by enabling real-time transcription and summarization of telehealth sessions, ensuring careful record-keeping while maintaining the personal connection in interactions with individuals.
Recent advancements in AI demonstrate that such technologies can simplify healthcare records, significantly decreasing the time allocated to paperwork—up to two full days a week. This means clinicians can concentrate on what truly matters: the well-being of individuals. Embrace this essential resource and enhance your record-keeping processes today. You deserve to focus on your patients and the they need.
SOAP Notes: Essential Structure and Examples for Effective Documentation
SOAP notes serve as a cornerstone of effective healthcare documentation, comprising four essential components: Subjective, Objective, Assessment, and Plan. Each section plays a vital role in capturing a comprehensive view of the individual's condition and guiding their care, especially when enhanced by generative AI technologies.
- Subjective: This section captures the individual's reported symptoms, feelings, and experiences, providing crucial context for their condition. For instance, an individual might share, "I have been experiencing persistent headaches and fatigue." How can generative AI assist in documenting these subjective reports more efficiently? By allowing healthcare providers to focus on patient interactions rather than administrative tasks, we can create a more compassionate care environment.
- Objective: Here, measurable data is documented, including vital signs and physical examination findings. A clinician might note, "Blood pressure is 120/80, and heart rate is 72 bpm." Imagine the time saved when AI tools streamline the collection and entry of this data, reducing the burden of documentation and allowing for more meaningful patient engagement.
- Assessment: In this part, the healthcare provider synthesizes the subjective and objective information to formulate a diagnosis. For example, one might conclude, "The individual likely has tension headaches based on reported symptoms and examination results." With AI assisting in examining patterns in medical data, we can improve diagnostic precision and efficiency, ultimately .
- Plan: This outlines the next steps in the individual's treatment, detailing therapies, follow-up meetings, and any referrals. A plan might state, "Recommend stress management techniques and schedule a follow-up in two weeks." By automating reminders and follow-up scheduling, AI helps ensure that individuals receive prompt assistance, reinforcing our commitment to their well-being.
By following a charting notes example, healthcare professionals can enhance communication, ensure legal and ethical documentation, and ultimately improve care outcomes. The transparency offered by SOAP records not only assists in monitoring individual progress but also fosters a more systematic approach to clinical practice. Typically, a SOAP record spans two to four paragraphs, balancing thoroughness with conciseness. By incorporating generative AI into this process, we can reduce administrative burdens like scheduling appointments and handling medical records, enabling healthcare providers to concentrate more on delivering high-quality service to individuals. Together, let's embrace these tools to create a more nurturing and effective healthcare experience.

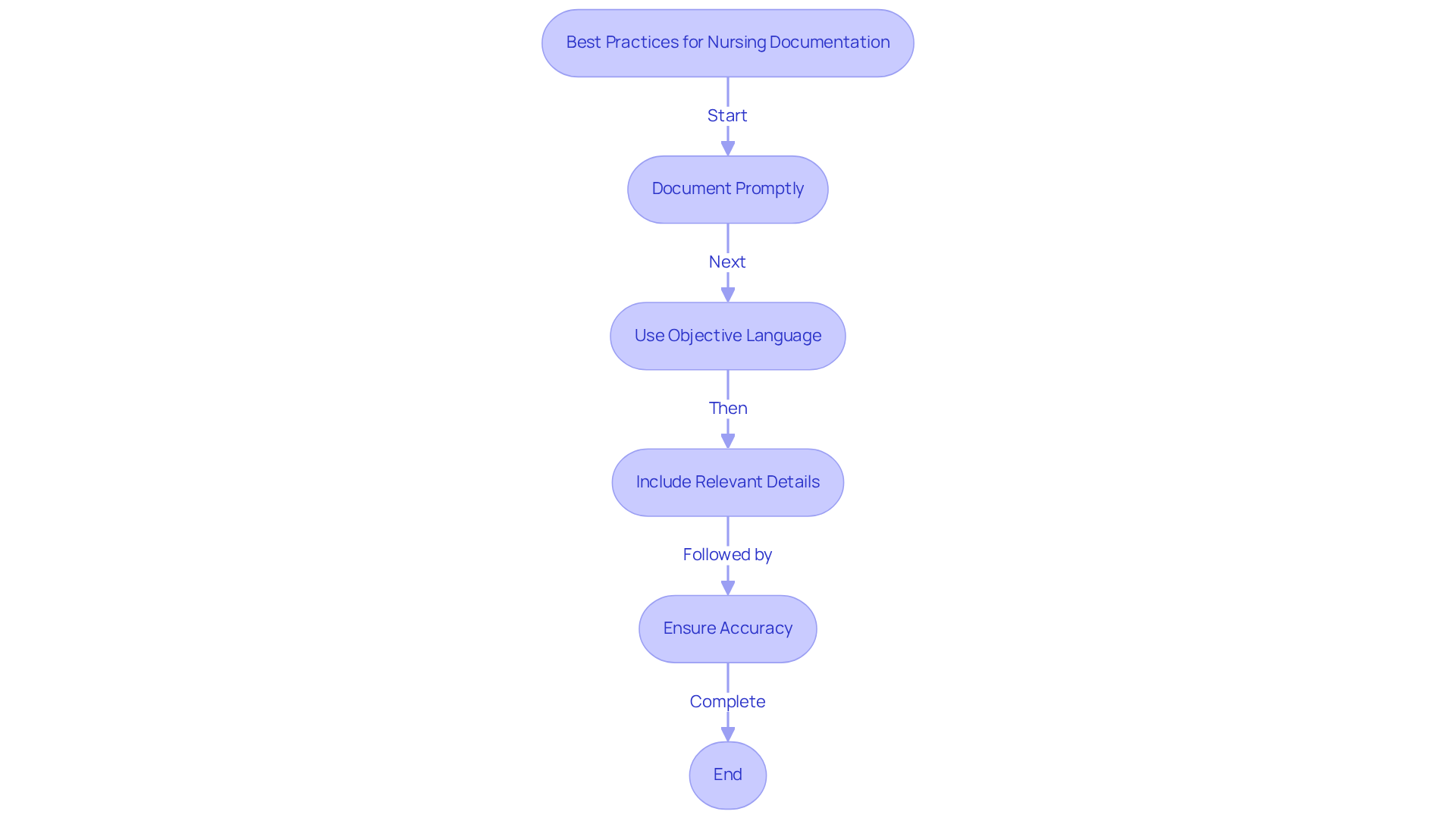
Nursing Notes: Key Examples and Best Practices for Accurate Patient Records
Nursing records must be clear, concise, and factual to ensure effective communication and high-quality care for individuals. It's essential to recognize the emotional challenges healthcare providers face in documenting patient interactions. Implementing best practices, including a charting notes example, can alleviate some of this burden and enhance patient outcomes.
- Documenting promptly after patient interactions is vital for maintaining accuracy and detail. For instance, a nursing note might state: 'Patient received pain medication at 10:00 AM; reports pain level decreased from 8 to 4 after administration. Vital signs stable. Educated individual on post-operative care.' This method not only captures the individual's response but also acts as a charting notes example, emphasizing the significance of prompt documentation and fostering a sense of trust and care.
- Utilizing objective language and avoiding personal opinions is crucial. Precise nursing records should represent observable behaviors and quantifiable information, such as vital signs and responses from individuals. For example, a note could read: 'Patient Smith, a 45-year-old female, presented with a temperature of 100.9°F and reported nausea. Administered APAP 325 mg; temperature decreased to 98.7°F after two hours, indicating a successful intervention.' This underscores the while offering a clear account of the individual's condition, reassuring both the patient and the healthcare team.
Including relevant details such as individual responses and interventions in a charting notes example enhances the quality of documentation. For example, a note might state: 'Patient Jones, an 81-year-old male, expressed feelings of fatigue and reported a productive cough. Vital signs recorded: B/P 150/88, P 74, R 26, T 98.2. Notified physician of changes in condition.' This guarantees that all healthcare providers engaged in the individual's treatment are aware of important updates, creating a collaborative approach to care.
Prompt and precise nursing records are crucial for enhancing health outcomes and maintaining continuity of care. As highlighted by nursing experts, comprehensive notes not only enhance communication among healthcare personnel but also serve an essential function in legal adherence and safety of individuals receiving care. Based on recent statistics, the average NCLEX pass rate is 73.26%, underscoring the significance of effective nursing education and record-keeping practices.
Furthermore, case studies, like that of Ms. Audra Jones, who was diagnosed with an asthma exacerbation, demonstrate how precise documentation leads to timely interventions and enhanced outcomes for individuals. As RN Jennifer Tomaselli expresses, 'Nurses learn early and often that treatment is the No. 1 priority — but charting is a close second.' By embracing these best practices, we can support each other in navigating the complexities of healthcare, ultimately prioritizing the well-being of those we serve.
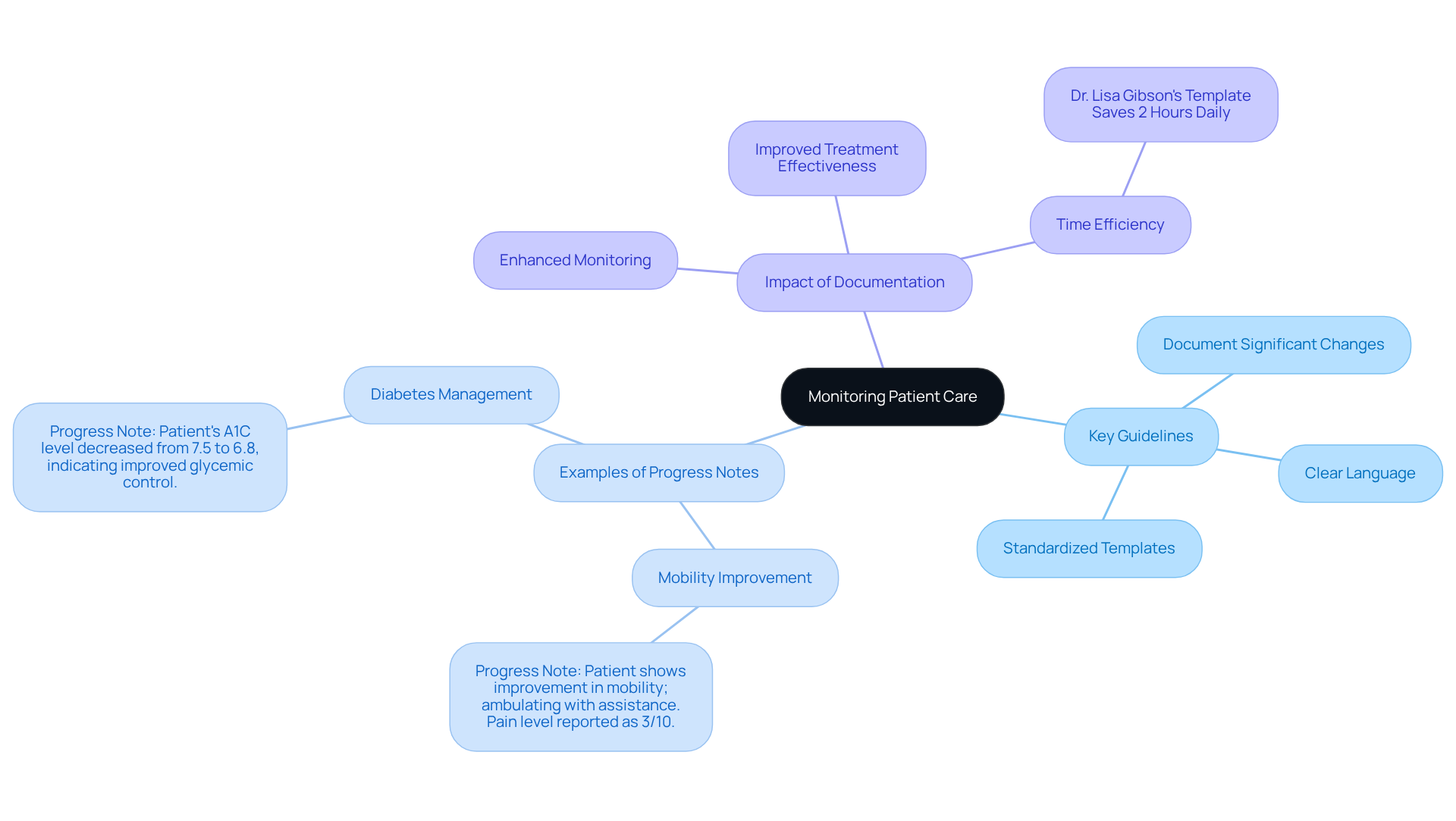
Progress Notes: Examples and Guidelines for Monitoring Patient Care
Progress records play a vital role in monitoring changes in a patient's condition, and it is essential that they are documented consistently. Healthcare providers often face emotional challenges, feeling the weight of administrative burdens that can impact patient care. To alleviate these concerns, here are some key guidelines for effective progress notes:
- Document significant changes in symptoms or treatment responses to ensure continuity of care.
- Use clear and specific language to describe observations, aiding accurate communication among healthcare providers.
- Utilize standardized templates to improve record-keeping efficiency and consistency.
For instance, an effective progress note might read:
- Progress Note: Patient shows improvement in mobility; ambulating with assistance. Pain level reported as 3/10. Continue physical therapy as planned.
Statistics suggest that well-organized progress records can greatly enhance monitoring of individuals. Research demonstrates that clinicians who employ standardized templates report better documentation timeliness and quality. In managing chronic illnesses, such as diabetes, progress records are essential for evaluating treatment effectiveness and making necessary modifications. For example, a progress note for a diabetic patient might include:
- Progress Note: Patient's A1C level decreased from 7.5 to 6.8, indicating improved glycemic control. Continue current medication regimen and schedule follow-up in three months.
Additionally, Ciba Health's last A1C check was 5.3, a non-diabetic level, showcasing the effectiveness of diligent monitoring through progress notes. The Ciba Health illustrates how organized records enhance chronic condition management. By consistently applying these guidelines and the charting notes example, healthcare providers can ensure thorough record-keeping that supports effective patient care and monitoring. Together, we can navigate the complexities of healthcare with compassion and diligence.
Charting Method: Techniques and Examples for Streamlined Note-Taking
An effective charting notes example is essential in enhancing record quality in healthcare. Healthcare providers often face emotional challenges due to administrative burdens that can detract from patient care. By addressing these concerns, we can improve both documentation and patient interaction.
- Utilizing Templates: Standardized templates streamline documentation, ensuring that all necessary information is captured consistently. For instance, a charting notes example can be an organized format for daily notes that includes sections for vital signs, medications, and comments from individuals, encouraging thorough record-keeping while minimizing repetition.
- Implementing Voice-to-Text Technology: This technology allows for real-time note-taking, significantly improving documentation efficiency. By transforming spoken words into text, clinicians can focus more on client interaction rather than manual data entry. Systems like ChatEHR enable healthcare providers to dictate notes during consultations, which are then automatically transcribed and organized within the individual's electronic health record.
- Prioritizing Key Information: Effective documentation requires an emphasis on essential details while avoiding unnecessary information. This approach not only enhances clarity but also ensures that crucial data is readily accessible for future reference.
The combination of these techniques not only enhances the precision of medical records but also boosts overall workflow efficiency. This enables healthcare providers to dedicate more time to supporting individuals, fostering a nurturing environment that .
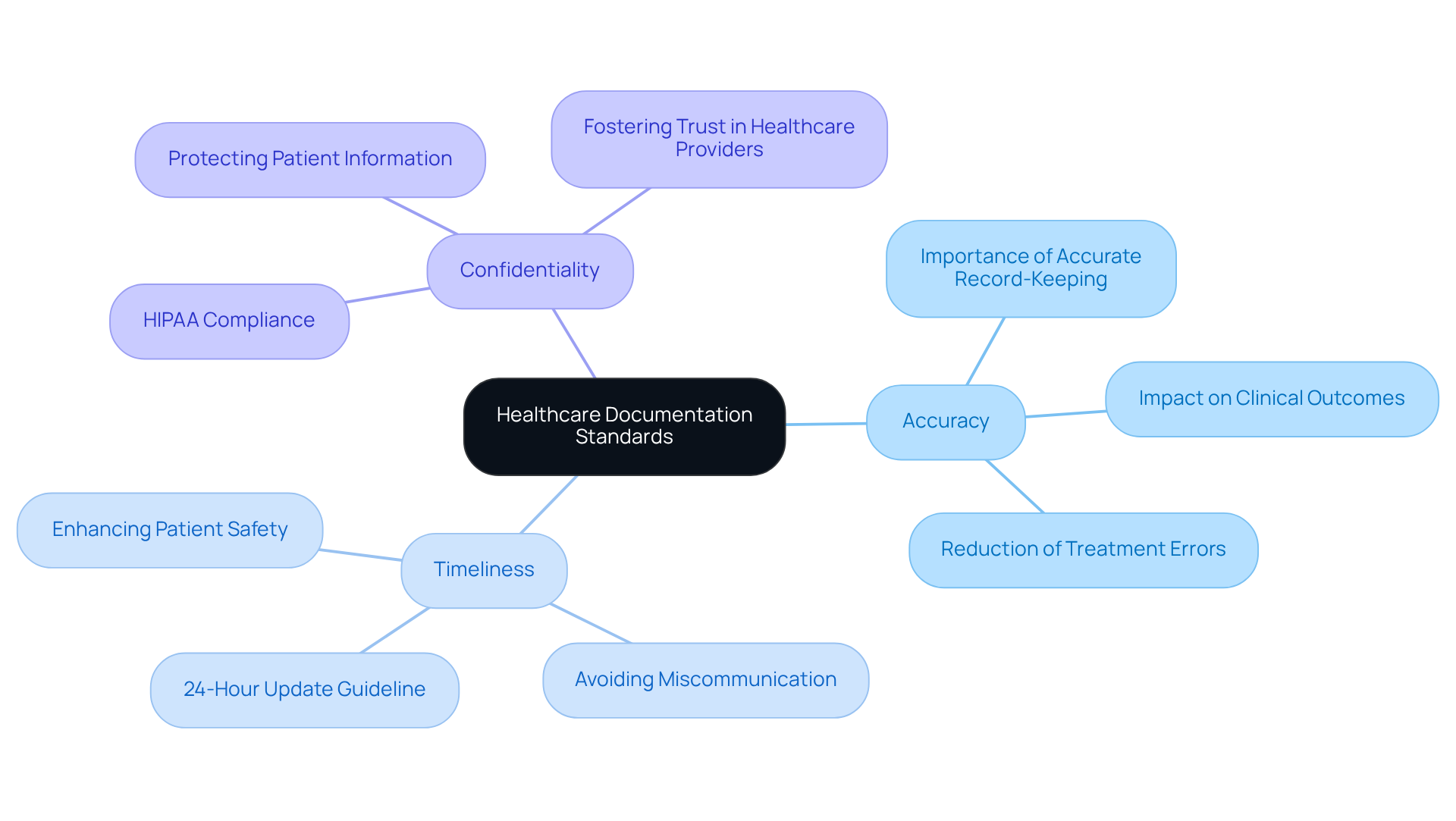
Documentation Standards: Examples Every Healthcare Provider Must Follow
Healthcare providers often face emotional challenges in delivering quality patient care while navigating administrative burdens. It’s essential to adhere to specific documentation standards that not only ensure compliance with regulations but also enhance the overall care experience for patients.
- Accuracy: Every entry should be factual and reflect the patient's true condition. Accurate record-keeping is vital; research shows that precise medical histories significantly improve clinical outcomes, reducing the risk of treatment errors. How might your documentation practices impact patient safety?
- Timeliness: Completing documentation promptly after client interactions is crucial. Records should ideally be updated within 24 hours of the visit to maintain accuracy and compliance. Delays can lead to miscommunication, which may compromise patient safety. Can you recall a time when timely updates made a difference in care?
- Confidentiality: Protecting patient information in accordance with is paramount. In 2023 alone, over 747 large data breaches affected more than 168 million records. Ensuring confidentiality not only safeguards patient privacy but also fosters trust in healthcare providers. How can enhancing confidentiality enrich the patient-provider relationship?
By following these standards, healthcare providers can not only improve the quality of care delivered but also ensure compliance with regulatory requirements. Let’s work together to create a supportive environment where both patients and providers thrive.
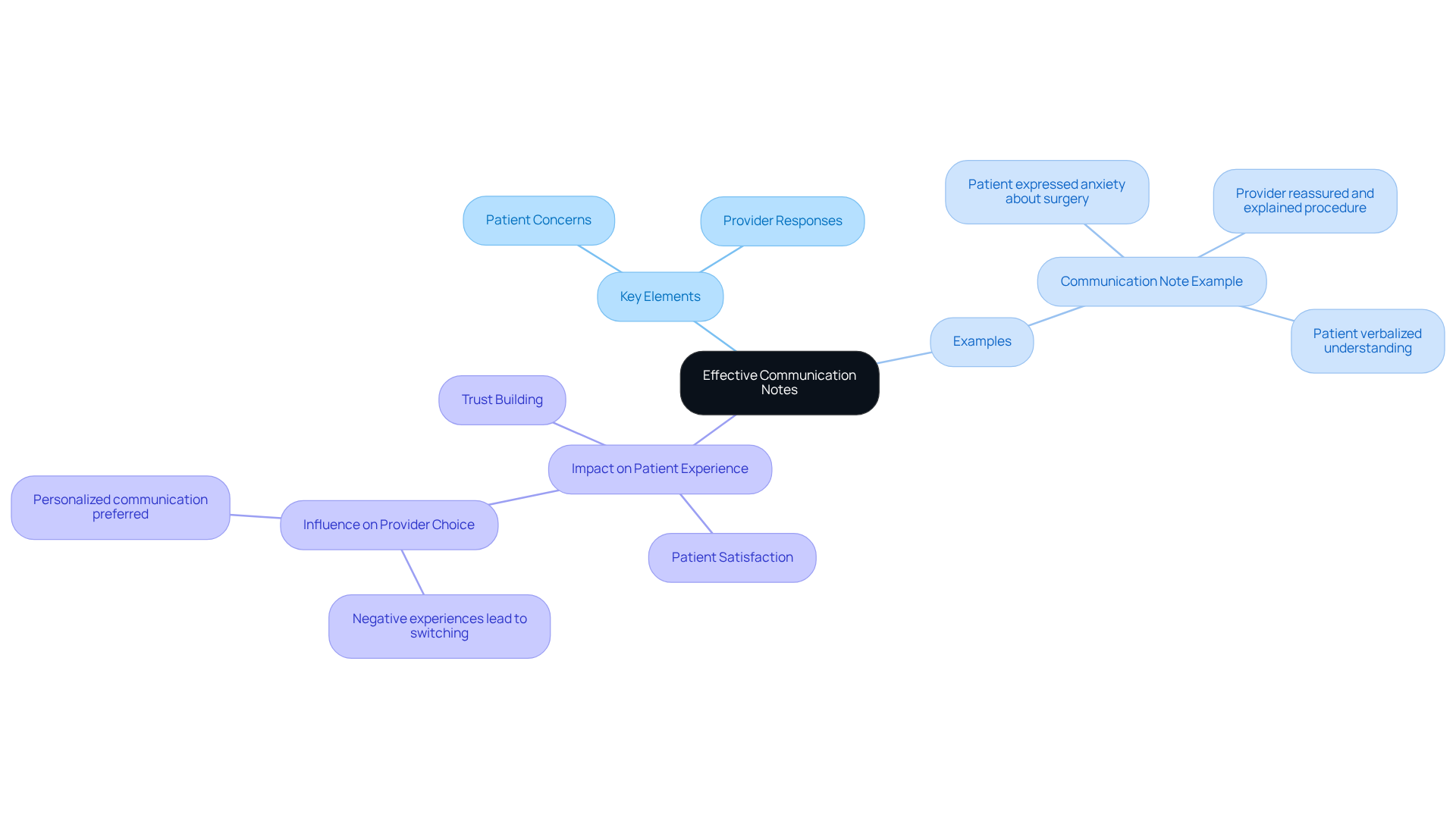
Communication Notes: Examples for Enhancing Patient-Provider Interactions
Effective communication records are vital for capturing the nuances of patient-provider interactions. These notes should encompass key elements such as:
- Patient concerns and questions.
- Provider responses and educational efforts.
For instance, a well-crafted communication note might read:
- Communication Note: Patient expressed anxiety about upcoming surgery; provided reassurance and explained the procedure in detail. Patient verbalized understanding and agreed to proceed.
The importance of documenting these interactions cannot be overstated. Clear and concise notes not only enhance the quality of care but also significantly influence satisfaction among individuals receiving care. Have you considered how your documentation practices affect patient experiences? Research indicates that individuals with negative experiences are three times more likely to change providers compared to those who report excellent interactions. Additionally, 80% of healthcare consumers favor digital communication with their providers, emphasizing the necessity for prompt and customized records.
By employing effective communication techniques in records, healthcare providers can build trust and enhance client involvement. For instance, adding interactive features in written materials can enable individuals, making them feel more engaged in their treatment choices. This approach aligns with the growing expectation for a communication experience akin to that of online retail, where clarity and responsiveness are paramount.
Ultimately, improving interactions between healthcare providers and individuals through careful record-keeping not only results in but also fosters a more satisfying healthcare experience for individuals. How can you enhance your communication practices to better meet the needs of your patients?
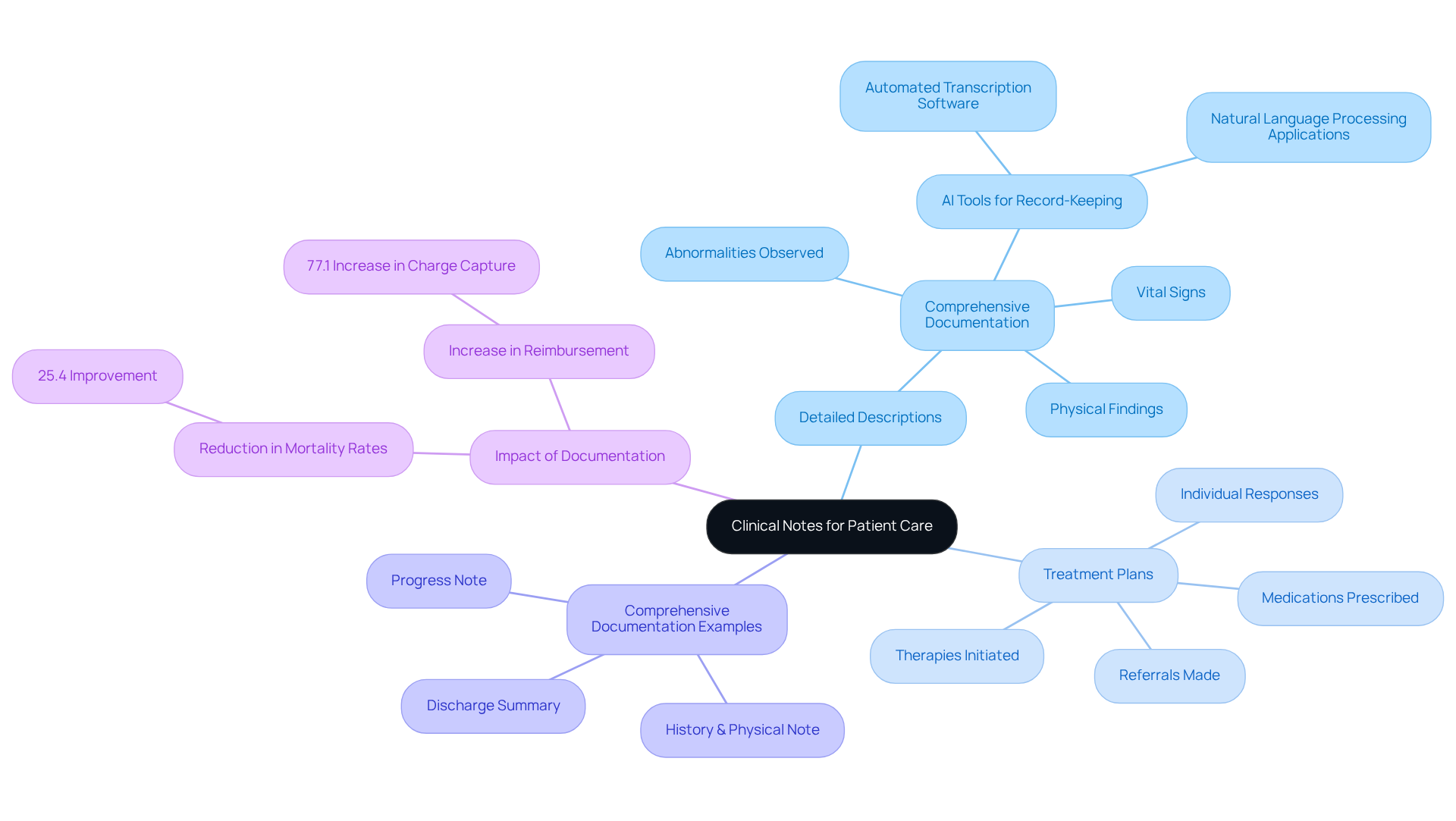
Clinical Notes: Essential Examples for Comprehensive Patient Care
Clinical notes are essential for delivering high-quality patient care, and they should encompass several key elements:
- Detailed Descriptions: Comprehensive documentation of examinations and assessments is crucial. This includes noting vital signs, physical findings, and any abnormalities observed during the examination. Have you considered how generative AI tools, such as automated transcription software and natural language processing applications, can simplify your record-keeping process? By utilizing these technologies, physicians can ensure that all pertinent details are captured efficiently and accurately.
- Treatment Plans: It is vital to clearly outline the treatment strategies employed, including medications prescribed, therapies initiated, and any referrals made. Recording individual responses to these interventions is equally important for monitoring progress and modifying care as necessary. AI tools can assist in creating standardized treatment plans, enhancing consistency and clarity in documentation.
Example of a Clinical Note:
Clinical Note: Patient examined for respiratory distress; auscultation revealed wheezing. Initiated nebulizer treatment; patient reported improvement in breathing after 15 minutes.
Incorporating detailed clinical notes not only enhances communication among healthcare providers but also supports continuity of care, legal defense, and reimbursement processes. Did you know that precise clinical records significantly enhanced quality metrics, resulting in a 25.4% reduction in observed mortality rates? Moreover, the application of standardized record templates has been demonstrated to enhance charge capture rates by 77.1%, highlighting the financial advantages of meticulous record-keeping.
Current trends in clinical documentation practices emphasize the importance of integrating client quotes into notes. This practice can provide into their experiences and foster a stronger therapeutic relationship. For example, direct citations from individuals can demonstrate their emotional conditions and highlight significant instances in their treatment journey, ultimately leading to more tailored planning. As one health expert remarked, "Recording standard procedures is crucial for the continuity of care, legal protection, reimbursement, communication among healthcare providers, and improved diagnoses and treatments."
Examples of Comprehensive Clinical Documentation:
- History & Physical Note: Records the individual's medical history and current conditions, establishing a foundation for diagnosis and treatment.
- Progress Note: Records the individual's status during multiple healthcare interactions, monitoring changes over time and guiding ongoing treatment strategies.
- Discharge Summary: Offers a summary of the individual's hospital admission and progress, ensuring continuity of care after discharge.
By prioritizing detailed clinical documentation and leveraging AI technologies, healthcare providers can enhance individual outcomes, improve operational efficiency, and ensure compliance with regulatory standards. Let’s work together towards a future where compassionate care is supported by efficient documentation.
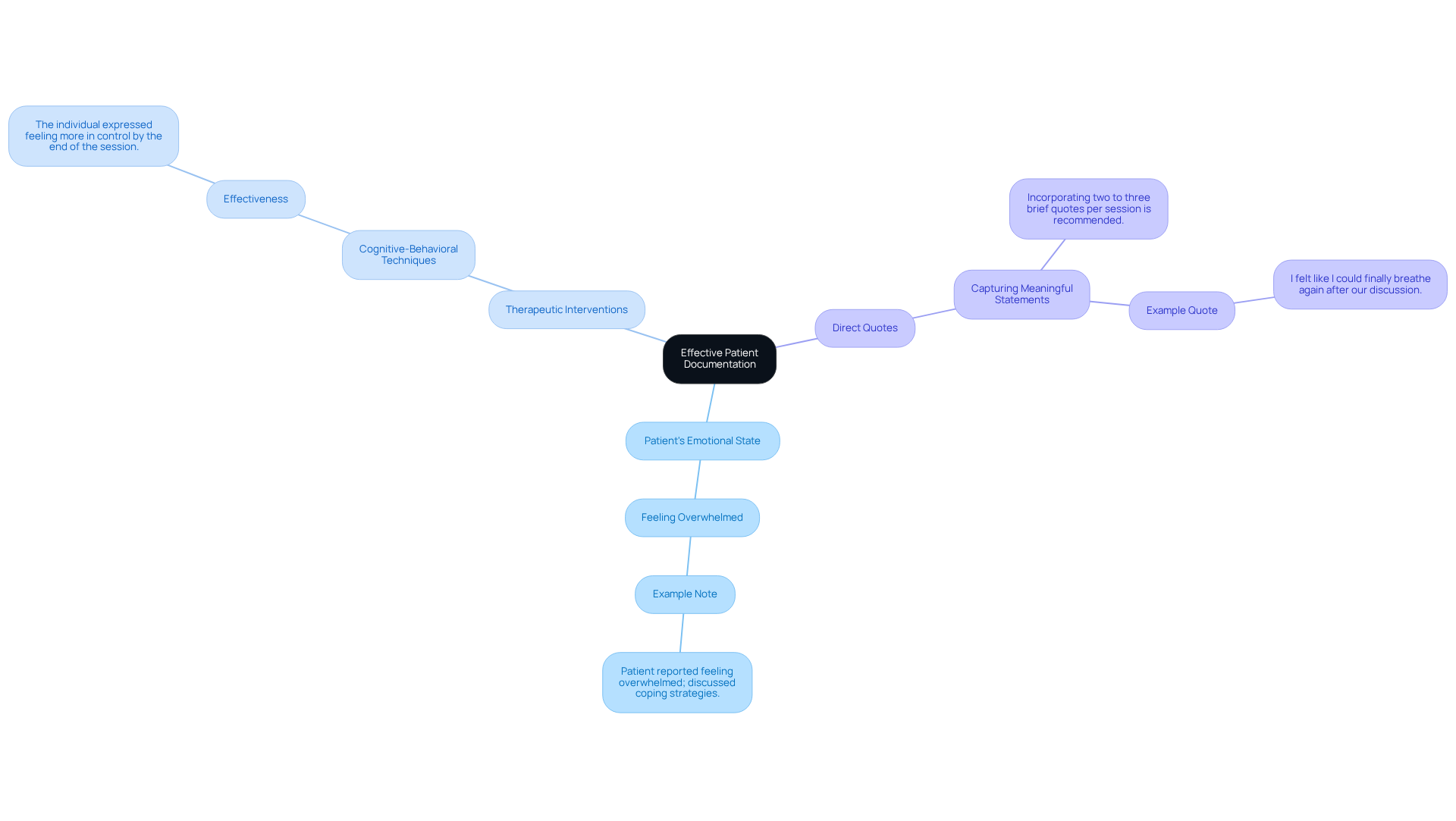
Mental Health Notes: Key Examples for Effective Patient Documentation
Mental health notes should prioritize the following elements:
- Patient's Emotional State: Documenting the patient's emotional state and behavior during sessions is essential for understanding their progress and challenges. For instance, a note might read: "Patient reported feeling overwhelmed; discussed coping strategies."
- Therapeutic Interventions: Clearly outlining the interventions used and their effectiveness not only tracks the treatment process but also informs future sessions. An example could be: "Engaged in cognitive-behavioral techniques; the individual expressed feeling more in control by the end of the session."
Effective documentation serves multiple purposes. It captures the nuances of the individual's experience, provides context for therapeutic goals, and enhances the overall quality of care. By incorporating direct quotes from individuals, therapists can further enrich their notes, reflecting genuine emotions and fostering deeper connections. For instance, incorporating an individual's reflection such as, "I felt like I could finally breathe again after our discussion," can emphasize significant moments in therapy and clarify the impact of interventions. It is recommended to include two to three brief quotes per session for effective note-taking.
In summary, comprehensive mental health records not only assist in monitoring progress but also strengthen the therapeutic relationship, ultimately resulting in better outcomes for patients. To ensure , it is advisable to write down meaningful quotes as soon as possible.
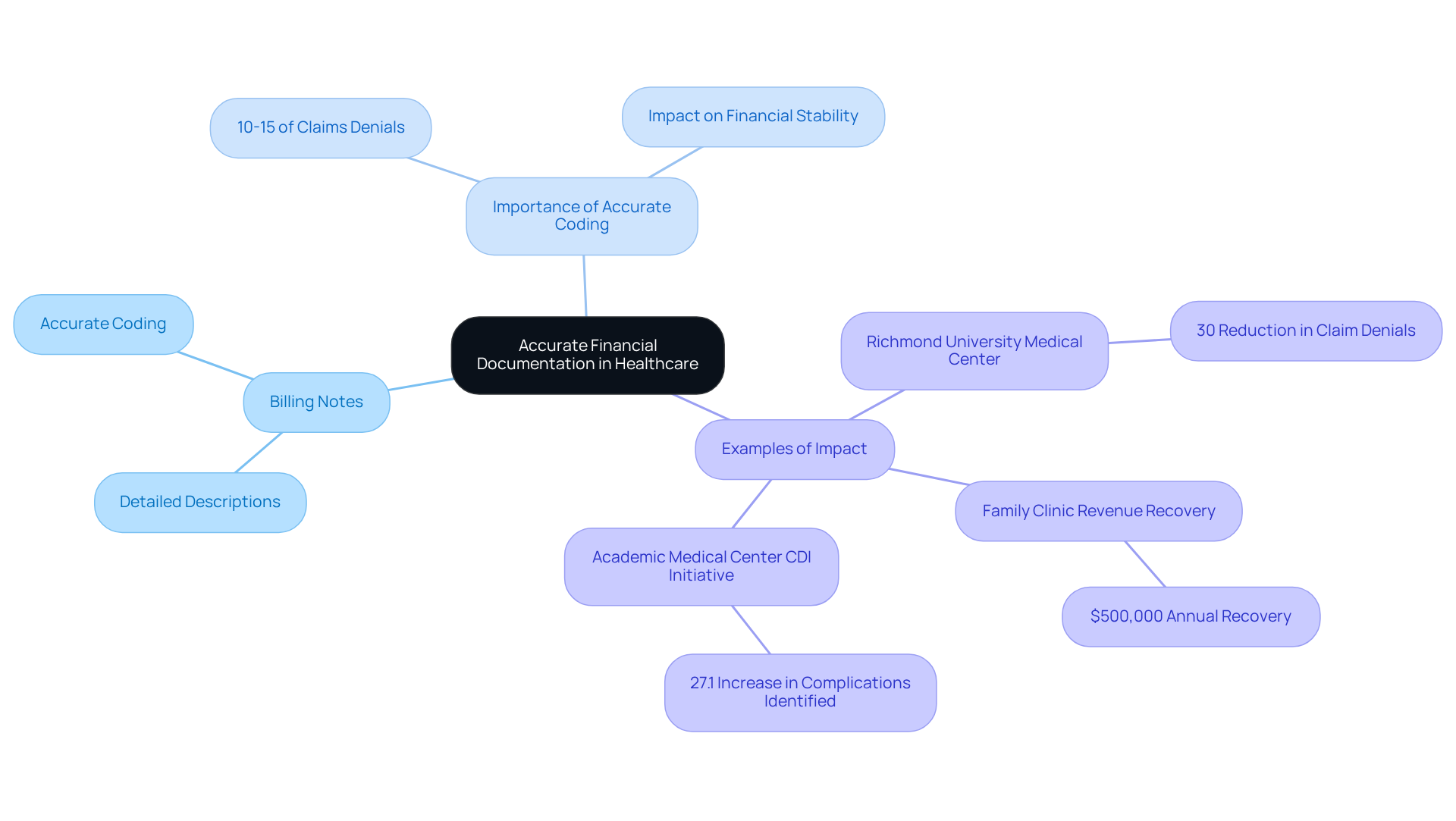
Billing Notes: Examples for Accurate Financial Documentation in Healthcare
Billing notes should encompass:
- Detailed descriptions of services provided.
- Accurate coding for billing purposes.
Example:
- Billing Note: Patient received a comprehensive evaluation and treatment plan; billed for initial consultation and follow-up visit. Ensure all codes are verified against services rendered for accurate reimbursement.
Precise billing records are vital in healthcare, as they directly affect revenue recovery and operational efficiency. Have you ever considered how administrative burdens can impact patient care? For instance, Richmond University Medical Center's Clinical Documentation Improvement (CDI) program led to a 30% reduction in claim denials, significantly enhancing their revenue cycle. This enhancement demonstrates how efficient record-keeping methods can directly relate to financial stability. Similarly, a family clinic that improved its preventive health records regained almost $500,000 each year in lost income, illustrating the financial impact of thorough record-keeping.
The importance of cannot be overstated; it ensures that healthcare organizations maintain financial stability while delivering quality services. Did you know that record errors contribute to 10-15% of claims denials, jeopardizing the viability of smaller practices? By implementing robust billing practices, providers can not only secure appropriate reimbursements but also foster trust in the physician-patient relationship, ultimately improving health outcomes. Furthermore, an academic medical center's CDI initiative resulted in a 27.1% increase in identifying significant complications, reinforcing the necessity of accurate documentation and coding in enhancing care delivery.
Conclusion
Effective healthcare documentation is not just a task; it’s a vital part of delivering compassionate, high-quality patient care. The insights shared throughout this article highlight the emotional challenges healthcare providers face, emphasizing the importance of structured and precise record-keeping. By utilizing charting notes examples such as SOAP notes, nursing notes, and communication records, healthcare providers can enhance their documentation practices. This ensures a comprehensive and accurate representation of patient interactions and treatment plans, allowing for a deeper connection with those they serve.
The transformative role of AI-powered tools like CosmaNeura cannot be overlooked. These tools streamline documentation processes, freeing healthcare professionals to focus more on what truly matters—patient care—rather than getting bogged down by administrative tasks. Best practices for various types of notes are essential, especially regarding timeliness, accuracy, and confidentiality. These elements are crucial for maintaining effective communication and compliance with healthcare standards, fostering trust between patients and providers.
In conclusion, diligent documentation impacts far beyond mere compliance; it builds a foundation of trust and enhances overall care outcomes. As the healthcare landscape continues to evolve, embracing these best practices and leveraging innovative technologies will be essential. This will create a compassionate and efficient environment where both patients and providers can thrive. The call to action is clear: let us prioritize effective documentation together, ensuring that the focus remains on the well-being of every individual receiving care.




