Overview
The article titled "10 Examples of SOAP Notes for Effective Healthcare Documentation" seeks to address the emotional challenges healthcare providers face in their documentation practices. It emphasizes how structured SOAP notes can alleviate administrative burdens, ultimately allowing providers to focus more on patient care. By enhancing communication among healthcare providers and streamlining record-keeping, these notes not only improve documentation but also lead to better patient outcomes.
Imagine the relief of knowing that your documentation is comprehensive and compliant. This article highlights practical examples of SOAP notes that can transform your approach to healthcare documentation. Each example serves as a reminder of how effective documentation can foster a nurturing environment for both providers and patients.
Are you ready to enhance your documentation practices? Explore these examples and discover how they can support your commitment to providing exceptional care. Together, we can ensure that every patient receives the attention and care they deserve.
Introduction
In the intricate landscape of healthcare, where time is often a luxury, the challenge of effective documentation can feel overwhelming. Healthcare providers frequently grapple with administrative burdens that detract from their ability to connect with patients. As a solution, many are turning to structured frameworks like SOAP notes to help streamline their record-keeping processes. These frameworks ensure that vital patient information is captured accurately and efficiently.
This article explores ten compelling examples of SOAP notes, demonstrating how they enhance documentation practices and improve patient care across various specialties. However, we must ask ourselves: what happens when these notes become a burden rather than a tool? Striking a balance between thorough documentation and meaningful patient interaction raises critical questions about the future of healthcare practices. Let us reflect on how we can navigate these challenges together.
CosmaNeura: AI-Driven SOAP Note Automation for Healthcare Providers
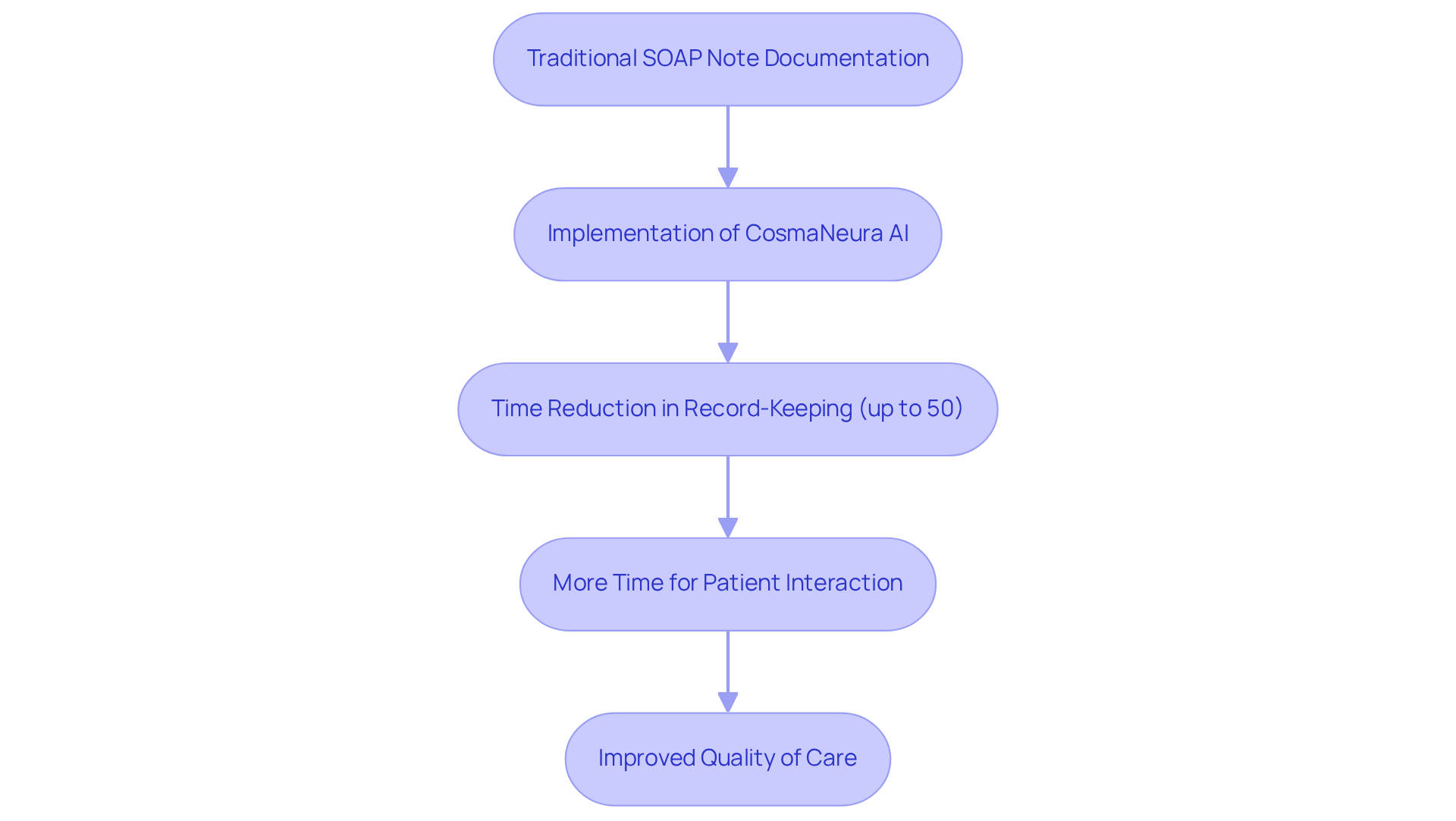
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from their ability to connect with patients. CosmaNeura understands this struggle and harnesses cutting-edge AI technology to automate the creation of examples of soap notes. By significantly reducing the time spent on paperwork, clinicians can focus more on meaningful interactions with individuals, ultimately improving the quality of care provided.
Imagine a scenario where the record-keeping process is simplified. CosmaNeura not only upholds high standards of care but also guarantees compliance with ethical guidelines, which is especially crucial in faith-oriented healthcare environments. The platform’s ability to incorporate individual values into the records enhances its significance, promoting a compassionate approach to care.
Consider this: case studies indicate that healthcare providers utilizing AI for record-keeping have experienced up to a 50% reduction in time spent on clinical records. This showcases the efficiency gains achievable through automation. As the healthcare landscape evolves, the use of automated clinical documentation is becoming more essential. In fact, 83% of doctors believe that AI can ease many administrative difficulties, thereby improving overall healthcare results.
Are you ready to embrace a solution that not only alleviates your administrative load but also enriches the care you provide? With CosmaNeura, you can and focus on what truly matters—your patients.
Psylio: Comprehensive SOAP Note Examples for Mental Health Counseling
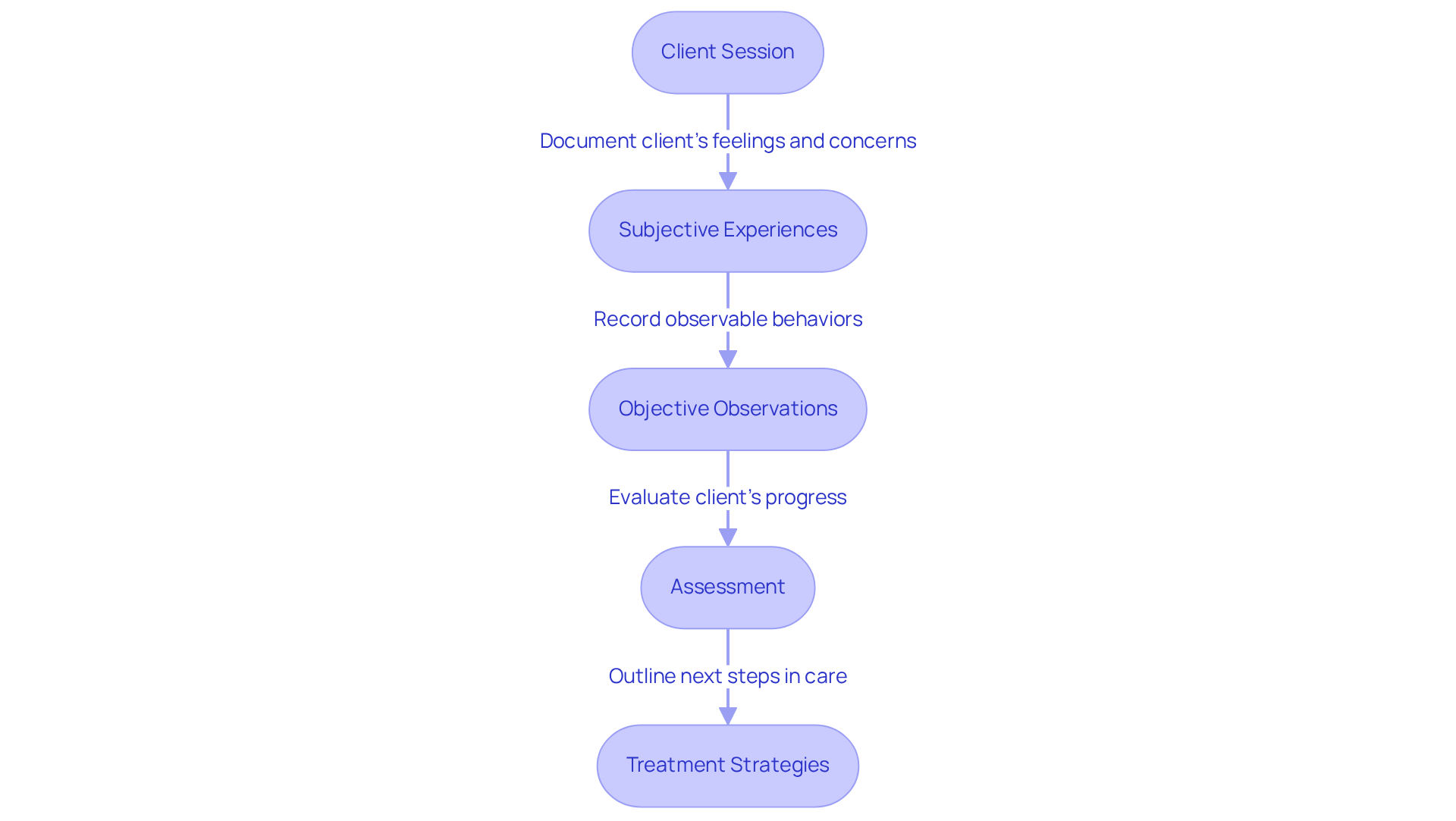
CosmaNeura understands the emotional challenges faced by mental health professionals. The various examples of clinical records designed for mental health counseling serve as an example of soap notes, highlighting the effective recording of subjective experiences, objective observations, assessments, and treatment strategies while aiming to alleviate some of the administrative burdens that can impact patient care. By utilizing these templates, mental health specialists can generate thorough and compliant records that serve as an example of soap notes, which are vital for enhancing care quality and ensuring adherence to industry standards.
Imagine a world where every detail of a client’s journey is captured seamlessly. By concentrating on the organized layout of clinical records, providers can reflect the individual's current condition and any changes since the previous session. This meticulous approach aids in tracking client progress over time and facilitates collaboration among healthcare providers, ultimately leading to improved mental health outcomes.
Including client quotations within therapy records can further enrich the written account. This practice provides insights into their emotional experiences and nurtures a deeper therapeutic relationship. As Vivian Chung Easton emphasizes, each piece of clinical documentation should represent the individual's current condition and pertinent alterations since the last session.
To enhance the in healthcare environments, providers are encouraged to consistently refine their recording methods and embrace technology. This commitment ensures precise records that adhere to legal requirements, allowing you to focus more on what truly matters—your clients' well-being. By taking these steps, you can make a significant difference in the lives of those you serve.
Lindy.ai: Step-by-Step SOAP Notes for Physical Therapy Practice
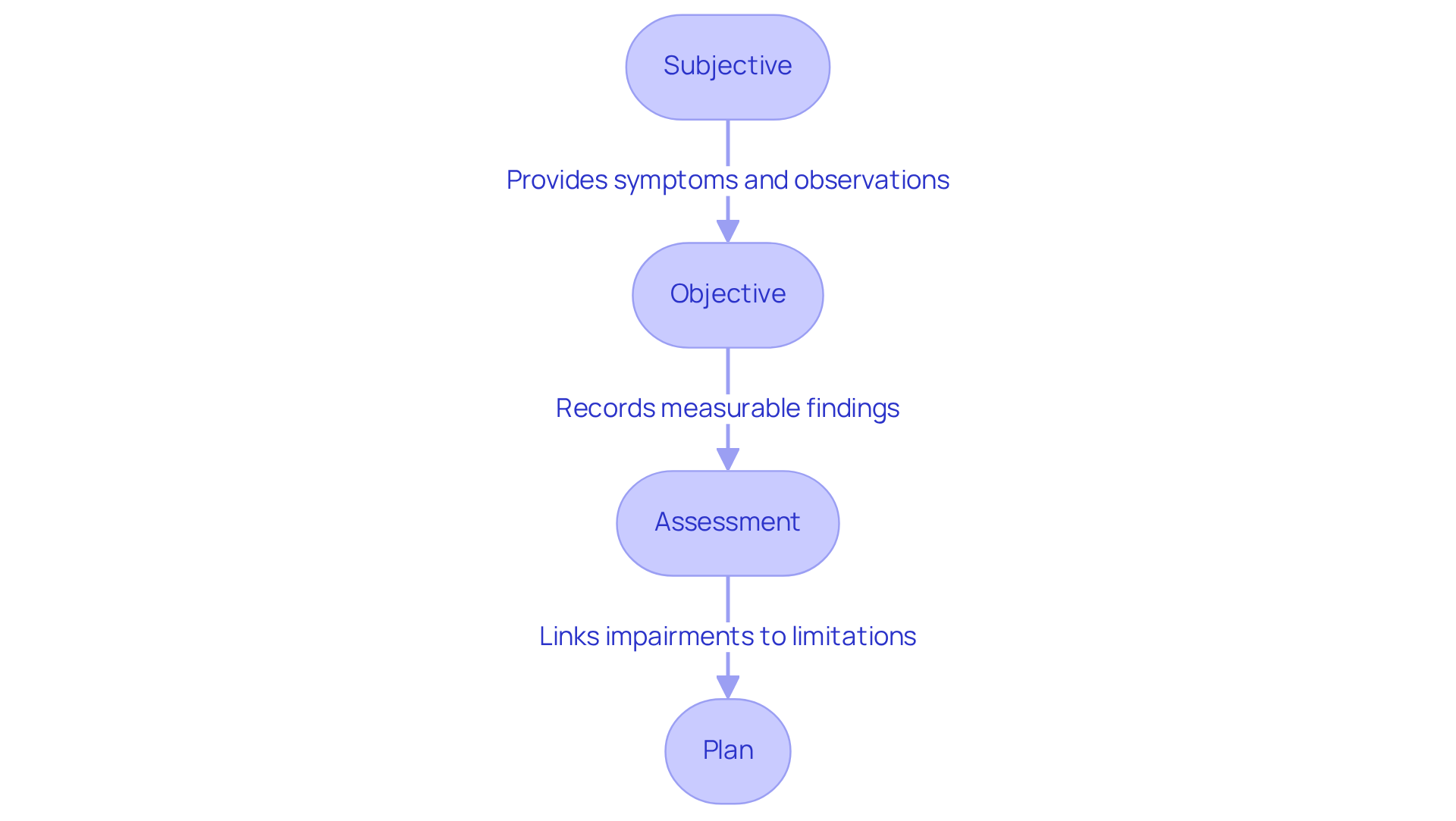
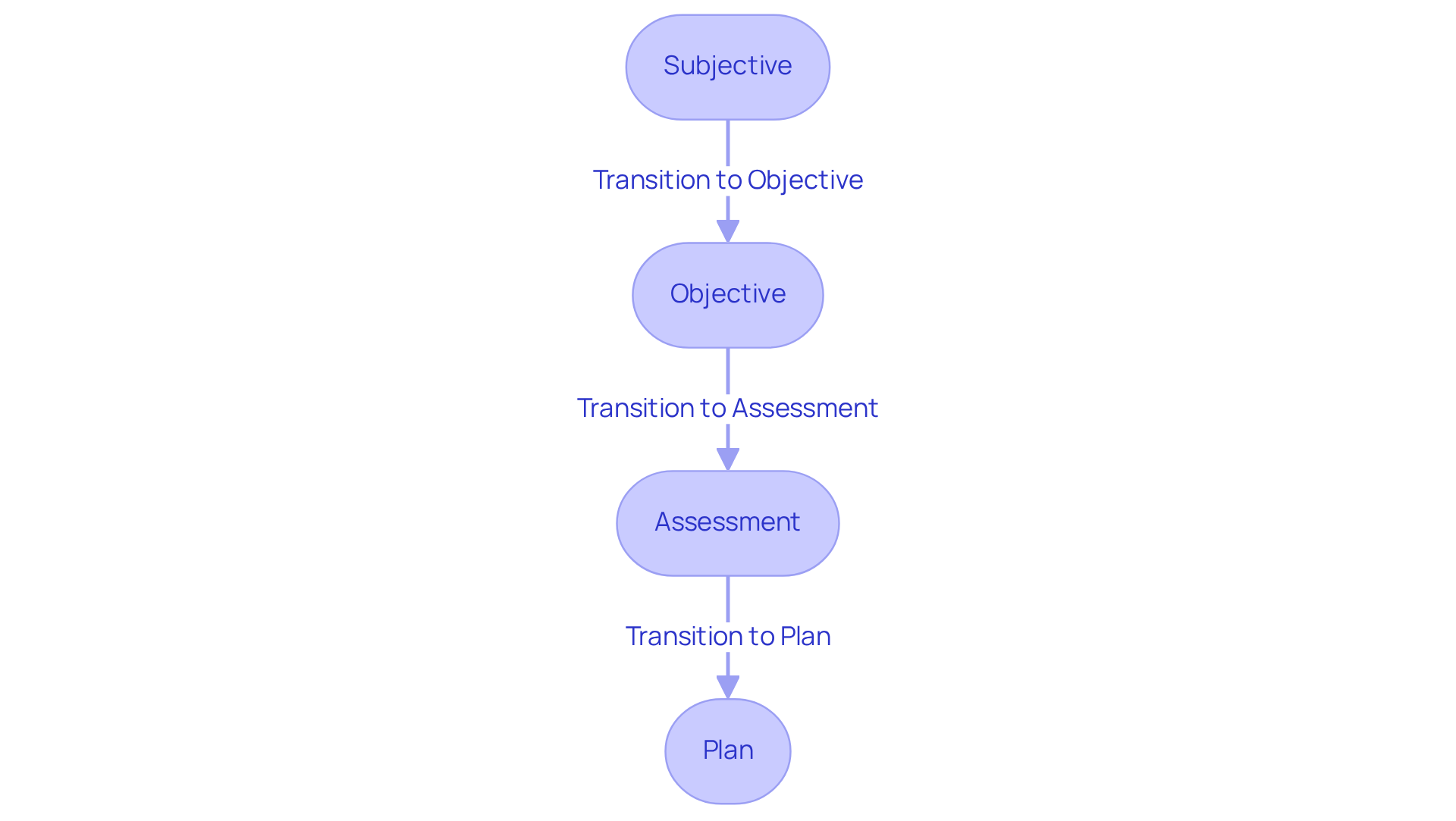
Effective SOAP notes are a vital example of soap notes for physical therapists, serving as a structured framework for documenting the care provided to individuals. Each component—Subjective, Objective, Assessment, and Plan—plays a crucial role in capturing both the individual’s progress and the efficacy of treatment.
- The Subjective section includes symptoms reported by the individual and observations from caregivers, offering valuable insight into their experiences.
- Meanwhile, the Objective section records measurable findings, such as vital signs and physical assessments, ensuring therapists gain a clear understanding of the individual’s condition.
- The Assessment component synthesizes the gathered information, linking impairments to functional limitations and justifying the ongoing need for care.
- Finally, the Plan outlines future interventions and goals, guiding the therapeutic process.
By adhering to these guidelines, therapists can create detailed records that not only enhance communication among healthcare providers but also support precise billing and compliance with payer requirements.
Organized clinical records have shown a significant improvement in health outcomes. Research indicates that effective record-keeping can enhance clinical decision-making and reduce medical errors by as much as 25%. Furthermore, efficient record-keeping can improve patient results by 20-30%. Establishments that adopt standardized formats report a 15-20% reduction in rejected insurance claims, illustrating the financial advantages of comprehensive record-keeping. By prioritizing best practices in documentation writing, physical therapists can ensure they deliver high-quality care while safeguarding their practice from potential legal and financial consequences.
Consider how these practices can alleviate the burden on your administrative duties. What if you could spend more time focusing on your patients rather than paperwork? By implementing effective documentation practices, such as an example of soap notes, you can not only streamline your documentation processes but also enhance the quality of care you provide. Embrace these best practices and witness the positive impact on both your practice and your patients.
MBLEX Guide: Effective SOAP Notes for Massage Therapy Documentation
The MBLEX Guide offers compassionate support for massage therapists with efficient templates that serve as an example of soap notes designed specifically for massage therapy records. These templates empower therapists to accurately document client sessions, capturing essential details about the client's condition, the treatment administered, and future plans. By embracing these organized records, massage therapists enhance the professionalism of their practice and ensure compliance with industry regulations.
Accurate documentation is vital. It fosters better communication among healthcare providers and aids in tracking client progress. An effective example of soap notes can lead to improved client outcomes, allowing therapists to tailor treatments based on recorded client responses and progress. This organized approach is essential for maintaining high standards in care and enhancing the therapeutic process.
Consider this: 91 percent of adult Americans believe massage can effectively reduce pain. This statistic underscores the necessity of documenting patient satisfaction and treatment efficacy. With 69,000 individuals succumbing to opioid overdoses each year, , including massage therapy, are more relevant than ever.
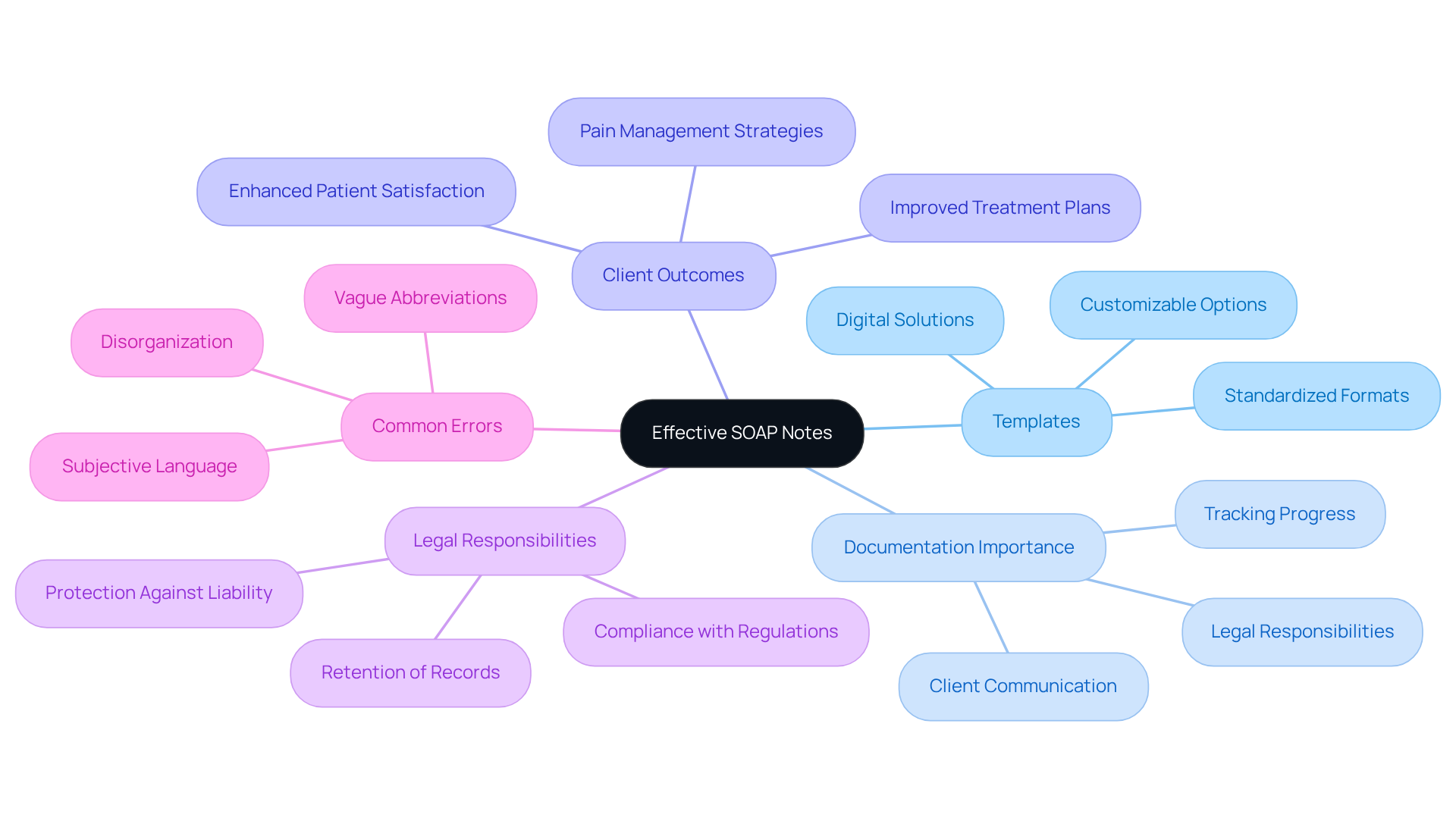
It’s important to remember that these records are legally enforceable documents, emphasizing the need for comprehensive records that safeguard legal responsibilities in practice. To ensure clarity and efficiency in reporting, frequent errors in clinical record-keeping—such as vague abbreviations and lack of structure—should be avoided.
By embracing accurate and organized documentation, you not only support your clients but also uphold the integrity of your practice.
Blueprint.ai: SOAP Note Examples for Pediatric Healthcare Providers
Blueprint.ai provides an example of soap notes that includes customized documentation tailored specifically for [pediatric healthcare providers](https://cosmaneura.com/newsroom1/tag/Healthcare), addressing the unique needs of children and their families. These examples highlight the significance of age-appropriate documentation, which is essential for accurately capturing a child's health status and treatment progress. Effective pediatric documentation not only fosters communication among healthcare providers but also greatly enhances patient outcomes by providing a structured framework for recording interactions and treatment plans.
Healthcare providers often face emotional challenges when it comes to documenting pediatric cases. It's important to recognize that children may struggle to articulate their feelings and symptoms. For example, when documenting a 12-year-old girl with an unspecified anxiety disorder, including her mother's observations about her anxiety levels during various activities can offer a more comprehensive understanding of her condition.
Best practices for documenting pediatric healthcare interactions emphasize the need for balance—thoroughness paired with brevity. Utilizing ensures that each entry remains concise yet comprehensive. Involving caregivers during sessions can further enhance documentation quality, as they provide valuable insights into the child's behavior and symptoms outside of therapy.
The impact of well-structured example of soap notes on pediatric healthcare outcomes is significant. Quality records empower clinicians to monitor progress over time, identify trends, and make informed treatment decisions. For instance, a study revealed that pediatric practices using specialized EMR templates achieved a 50% reduction in record-keeping time, leading to improved efficiency and superior care for patients.
By embracing these best practices and focusing on the unique elements of pediatric care, healthcare providers can create effective documentation that not only meets clinical standards but also significantly contributes to better patient outcomes. How can you implement these strategies in your practice to enhance care for your young patients?
Quenza: Occupational Therapy SOAP Note Templates and Examples
Efficient record-keeping is not just a task; it’s a cornerstone of compassionate occupational therapy. These records are vital in enhancing client outcomes, ensuring that every detail of client interactions is captured with care. By utilizing organized structured templates, therapists can streamline the record-keeping process, allowing them to focus more on what truly matters—providing quality care to their clients.
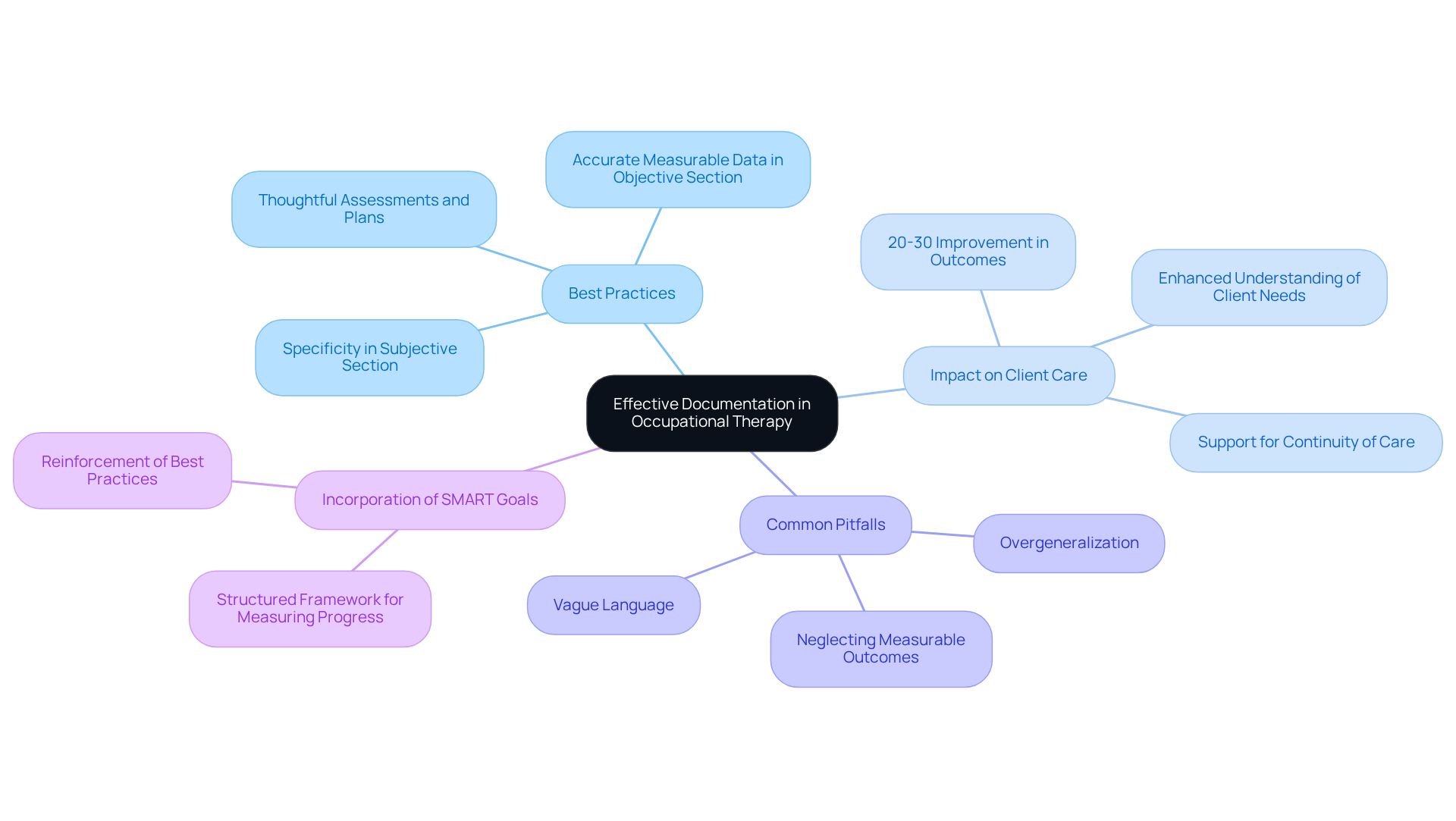
Best practices for documenting occupational therapy sessions are essential. Consider:
- Being specific and clear in the Subjective section.
- Accurately recording measurable data in the Objective section.
- Providing thoughtful assessments and plans.
This structured approach not only fosters better communication among healthcare providers but also supports , which is crucial for effective treatment.
The impact of well-prepared clinical records extends far beyond mere documentation; they significantly influence client interactions and treatment efficacy. In fact, well-organized examples of soap notes can lead to a remarkable 20-30% enhancement in outcomes through effective treatment modifications. By clearly articulating client concerns and progress, therapists deepen their understanding of each individual's unique needs, ultimately paving the way for improved therapeutic outcomes.
However, it is important to be mindful of record-keeping pitfalls such as overgeneralization and vague language, which can undermine the quality of patient care. Documentation, therefore, serves as an essential resource for occupational therapists, ensuring that every aspect of client care is recorded with accuracy and clarity. Additionally, incorporating SMART goals into documentation can further structure measurable progress, reinforcing best practices in occupational therapy.
Are you ready to enhance your documentation practices? Embrace these strategies to not only improve your record-keeping but also to elevate the care you provide to your clients.
Positive Psychology: SOAP Notes for Counseling and Therapy Practices
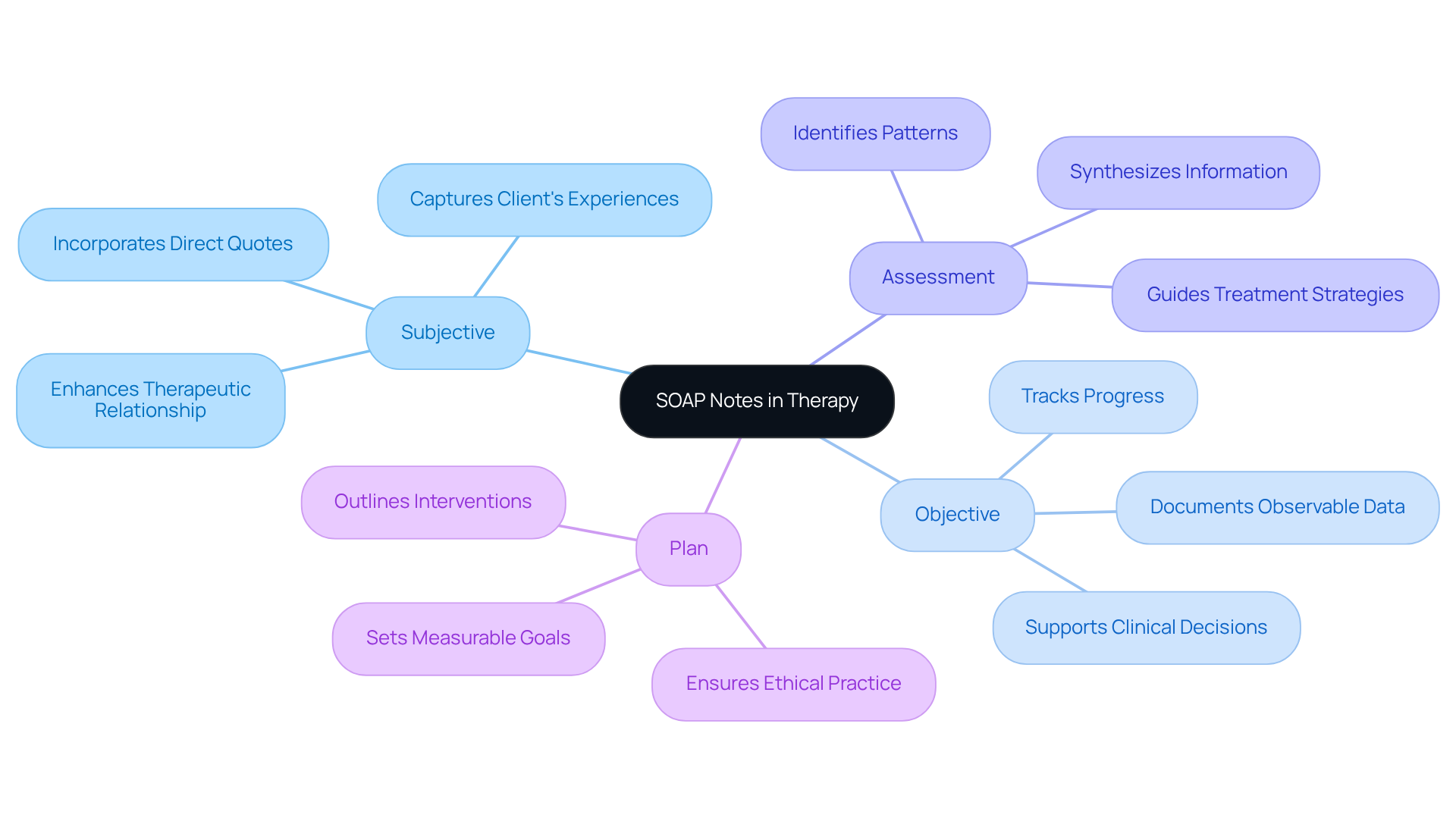
Positive Psychology recognizes the vital role of documentation in counseling and therapy practices. Have you ever felt overwhelmed by the administrative tasks that come with providing care? These notes are an example of SOAP notes, serving as a structured framework for documenting client interactions, which allows therapists to effectively track progress and adapt treatment plans as needed.
By consistently utilizing the SOAP format, which is an example of SOAP notes comprising Subjective, Objective, Assessment, and Plan, therapists can create records that are not only clear and concise but also adhere to industry standards. This structured approach enhances communication among healthcare providers, ultimately leading to and ensuring compliance with legal and ethical requirements.
It's important to note that healthcare professionals spend an average of 35% of their time on record-keeping. This statistic highlights the pressing need for effective practices. Thankfully, the integration of technology in clinical documentation is transforming record-keeping. Platforms like Supernote enable therapists to save 3-4 hours weekly while ensuring a 99% accuracy rate in transcription services.
Additionally, documenting informed consent is crucial for maintaining ethical practice and supporting client autonomy in mental health care. Overall, organized clinical documentation, which includes an example of SOAP notes, significantly influences therapy results, establishing it as a vital resource for effective client care. How can we continue to improve these practices together?
Social Work Portal: Best Practices for Writing SOAP Notes in Social Work
The Social Work Portal recognizes the emotional challenges social workers face in documenting client interactions. Effective documentation is crucial, yet it can often feel overwhelming. The guidelines provided by the portal serve as a nurturing solution, helping social workers capture all relevant information with ease.
By adhering to these best practices, social workers can not only enhance the quality of their records but also improve client outcomes. Imagine the positive impact on your clients when every detail is accurately documented. These methods empower you to focus more on your clients and less on administrative burdens.
We encourage you to explore these optimal methods and see how they can . Together, we can ensure that every client interaction is meaningful and impactful.
SimplePractice: Common SOAP Note Mistakes to Avoid for Better Documentation
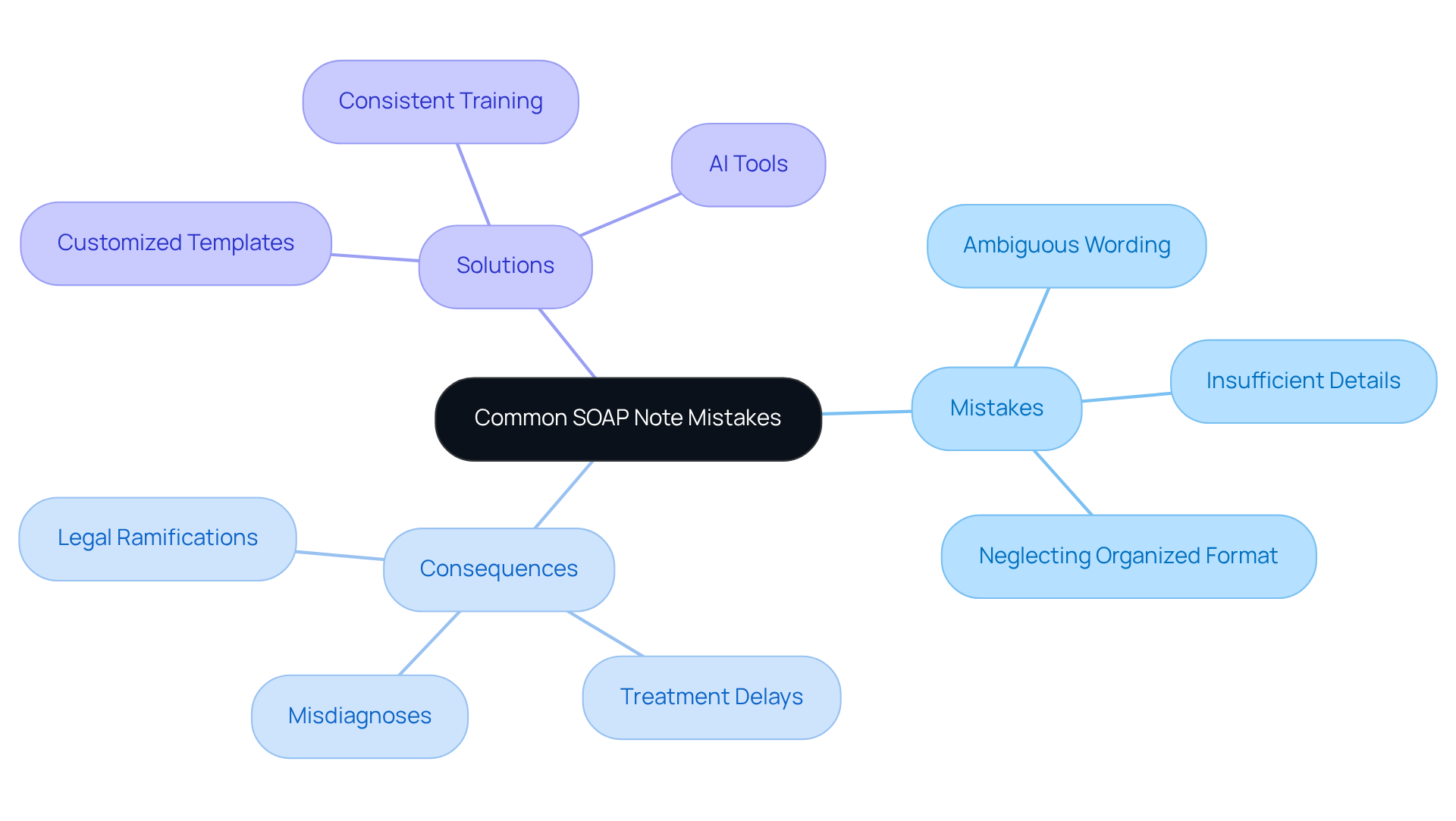
Effective clinical note recording is essential for guaranteeing high-quality patient care and reducing risks linked to record-keeping mistakes. Have you ever felt overwhelmed by the demands of accurate documentation? Frequent mistakes, such as ambiguous wording, insufficient details, and neglecting to follow the organized format, can lead to significant consequences. These include misdiagnoses, treatment delays, and even legal ramifications for healthcare providers. According to a study published in the Journal of Patient Safety, record-keeping errors contribute to a staggering percentage of adverse events in healthcare, with studies indicating that up to 72% of risks associated with electronic health records stem from inaccuracies in nursing records.
To enhance practices related to the example of SOAP notes, healthcare providers should prioritize clarity and completeness. Utilizing can ensure that all pertinent information is gathered effectively during client interactions. Consistent training and evaluations can strengthen best practices, while the incorporation of AI tools can simplify data entry and offer real-time notifications for essential records, significantly minimizing mistakes. Consider how AI tools can automatically correct errors in datasets, enhancing the reliability of EHR information.
By steering clear of typical mistakes found in the example of SOAP notes, healthcare professionals can enhance their record-keeping methods, ultimately resulting in improved care coordination and outcomes for individuals. As emphasized by industry experts, "Documentation acts as a legal shield during malpractice lawsuits by providing evidence of the care delivered." Promoting a culture that appreciates high-quality records is crucial for protecting client safety and improving the overall integrity of healthcare systems. The financial effects of record mistakes are also substantial—did you know that the United States expends over $40 billion annually for individuals affected by medical errors?
In summary, let’s work together to foster a supportive environment where accurate documentation is prioritized. By doing so, we can ensure that our patients receive the best possible care and that we, as healthcare providers, can feel confident in our practices.
Heidi Health: Legal Requirements and Compliance for SOAP Notes in Healthcare
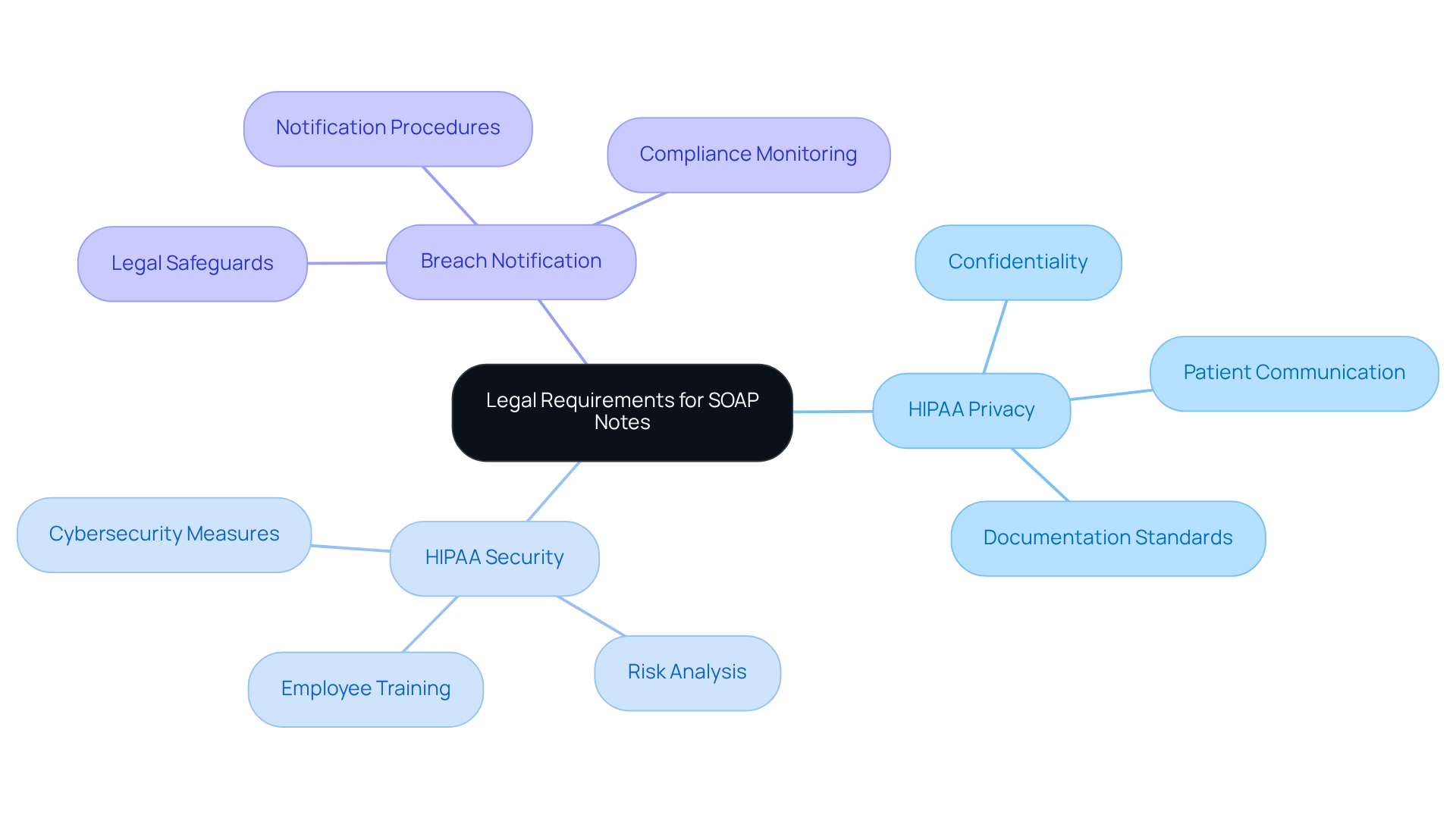
Heidi Health highlights the essential legal requirements and compliance considerations for an example of soap notes in healthcare, emphasizing the importance of adhering to HIPAA regulations. Maintaining precise, thorough, and secure records is not just a best practice; it is crucial for protecting both healthcare providers and individuals. Compliance with HIPAA is vital, encompassing three main rules:
- Privacy
- Security
- Breach Notification
These rules dictate how patient information is managed. A well-documented medical history is key for efficient revenue cycle operations, speeding up payments and ensuring appropriate reimbursement, with effective record-keeping methods contributing to 95% of reimbursement success. Additionally, 94% of compliance officers agree that if a clinician's action is not documented, it is not recognized as completed, underscoring the necessity of detailed records in healthcare environments.
Healthcare providers must ensure that their documentation, such as an example of soap notes, aligns with current standards, including the confidentiality and security of individual information. This is particularly important as healthcare institutions are prime targets for cyberattacks, making robust record-keeping practices essential for mitigating risks associated with breaches. Furthermore, adherence to HIPAA not only protects individual privacy but also serves as a safeguard against potential legal issues, as comprehensive records can significantly reduce the chances of successful malpractice claims.
When it comes to SOAP records, an example of soap notes involves accurately logging all client interactions and ensuring that the notes reflect the provided. This is vital for maintaining a permanent record of treatment, which supports ongoing care and fosters communication among healthcare providers. By grasping and implementing these legal requirements, including the necessity for annual employee HIPAA training, healthcare providers can enhance their documentation practices, ultimately leading to improved patient outcomes and greater organizational efficiency.
Conclusion
In the realm of healthcare, effective documentation through SOAP notes is not just a procedural necessity; it’s a vital aspect of enhancing patient care and ensuring compliance with industry standards. Have you ever felt overwhelmed by the administrative burdens that can take time away from your patients? The integration of technology, particularly AI-driven solutions like CosmaNeura, has revolutionized how healthcare providers manage their documentation processes. By automating SOAP note creation, clinicians can significantly reduce the time spent on paperwork, allowing them to prioritize meaningful interactions with their patients.
Throughout this article, we have explored various examples of SOAP notes across different healthcare disciplines, illustrating the importance of structured documentation. From mental health counseling to pediatric care, each section of the SOAP format—Subjective, Objective, Assessment, and Plan—plays a vital role in capturing essential patient information. The insights shared highlight not only the efficiency gains achievable through automation but also the profound impact that meticulous record-keeping has on clinical decision-making and patient outcomes.
As the healthcare landscape continues to evolve, embracing best practices for SOAP note documentation becomes increasingly essential. Are you ready to refine your recording methods? Healthcare providers are encouraged to utilize technology and prioritize clarity to enhance the quality of care they deliver. By committing to effective documentation, practitioners not only safeguard their practices against potential legal issues but also foster a more compassionate and efficient healthcare environment for their patients. Together, let’s embrace these changes to ensure every patient receives the attentive care they deserve.




