Overview
The article titled "10 Clinical Documentation Examples for Effective Patient Care" addresses the emotional challenges faced by healthcare providers. It recognizes that the demands of clinical documentation can often feel overwhelming, impacting not only their workflow but also the quality of patient care.
In this context, effective documentation methods, such as SOAP notes and DAP notes, emerge as vital tools. These structured practices not only streamline administrative tasks but also enhance communication and continuity of care among healthcare providers. As a result, they contribute significantly to improved patient outcomes, fostering a nurturing environment for both patients and providers.
Consider the benefits of implementing these documentation strategies:
- Streamlined administrative processes that free up time for patient interaction.
- Enhanced communication that leads to a more cohesive care experience.
- Improved patient outcomes that reflect the quality of care provided.
By embracing these methods, healthcare providers can alleviate some of the burdens they face, ultimately leading to a more fulfilling practice and better patient experiences. We encourage you to explore these documentation techniques further and reflect on how they might support your journey in delivering compassionate care.
Introduction
In the intricate realm of healthcare, the weight of clinical documentation can often overshadow the essential mission of patient care. As healthcare providers work diligently to navigate this complex web of record-keeping, innovative solutions and structured approaches have emerged, aimed at streamlining the process. This ultimately enhances both efficiency and compassion in delivering care. Yet, with the swift advancement of technology and evolving regulatory standards, how can practitioners ensure they are not only compliant but also prioritizing their patients' well-being? This article explores ten practical clinical documentation examples that not only alleviate administrative burdens but also cultivate a more effective and empathetic healthcare experience.
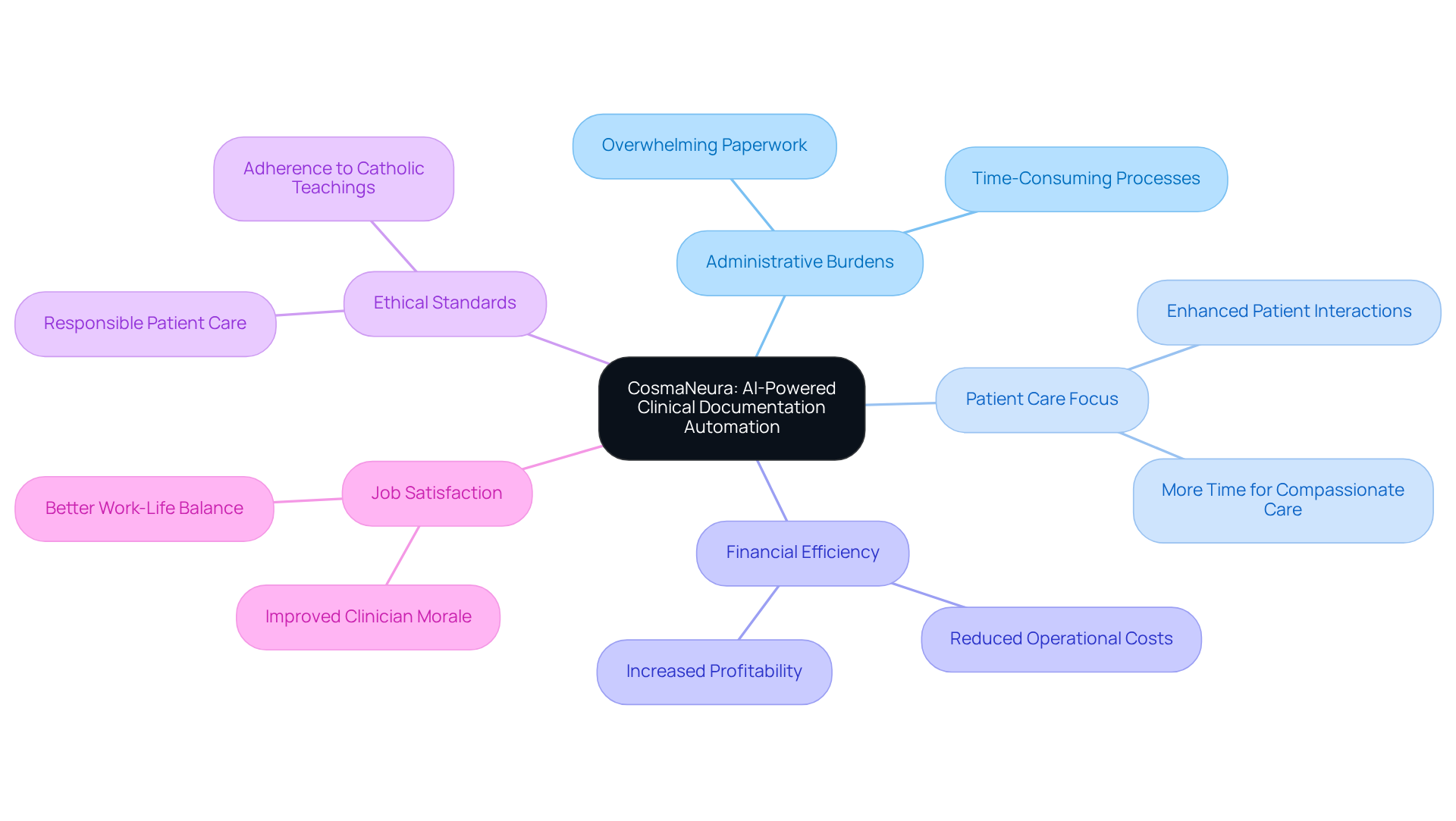
CosmaNeura: AI-Powered Clinical Documentation Automation
Healthcare providers often grapple with overwhelming administrative burdens that detract from their ability to deliver compassionate care. CosmaNeura understands these emotional challenges and utilizes advanced AI technology to transform clinical record-keeping processes. By significantly reducing the administrative load, it allows clinicians to focus more on patient care rather than paperwork, ultimately enhancing financial efficiency.
Imagine a world where essential tasks like client intake, triage, and telehealth records are automated. This innovative platform not only streamlines operations but also ensures that all records adhere to ethical standards, particularly those rooted in Catholic teachings. As a result, medical practitioners can experience increased job satisfaction and foster better interactions with individuals.
of AI on clinical documentation examples is profound, easing the financial pressures faced by both individuals and practitioners. With CosmaNeura, healthcare providers can reclaim precious time, allowing them to nurture their relationships with patients. Wouldn't it be wonderful to have more time for what truly matters? Embrace this opportunity to enhance your practice and improve patient care today.
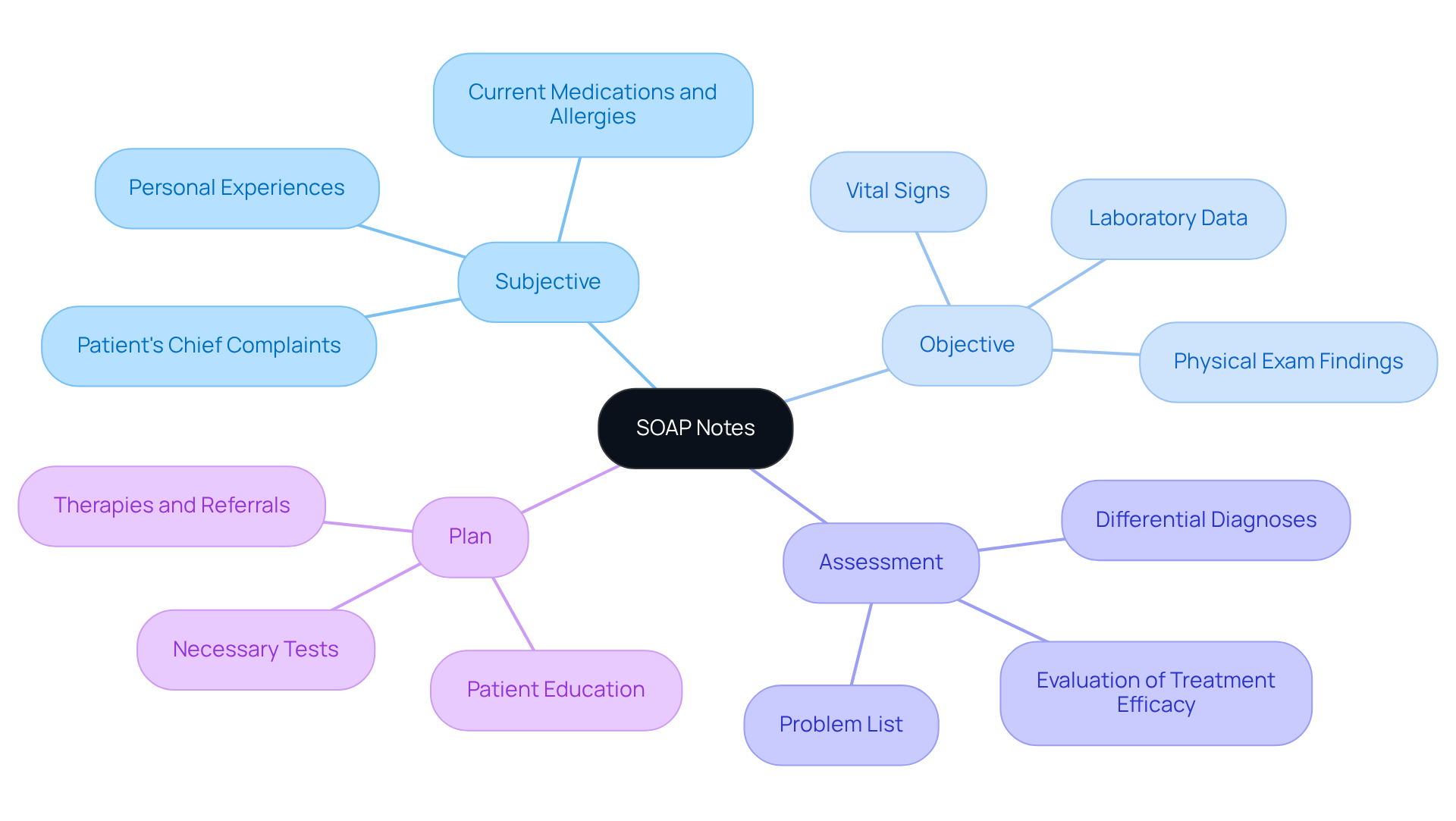
SOAP Notes: Structured Approach to Clinical Documentation
In the demanding world of healthcare, professionals often face emotional challenges that can weigh heavily on their ability to provide the best care. SOAP notes—standing for Subjective, Objective, Assessment, and Plan—serve as clinical documentation examples that provide a structured way to alleviate some of these burdens. By adopting this organized method, healthcare providers can systematically gather detailed client information, fostering a sense of clarity and support in their practice.
This approach not only enhances communication among care teams but also nurtures a collaborative environment. When clinicians follow the , they create clinical documentation examples that ensure all relevant details are meticulously documented. This diligence is crucial for effective healthcare management and legal compliance, allowing providers to focus more on what truly matters: their patients.
Imagine the peace of mind that comes from knowing every detail is captured accurately. By embracing SOAP notes, you can streamline your documentation process, allowing more time for patient interaction and care. Let’s work together to create a healthcare experience that prioritizes both efficiency and compassion. How can you incorporate SOAP notes into your practice today?
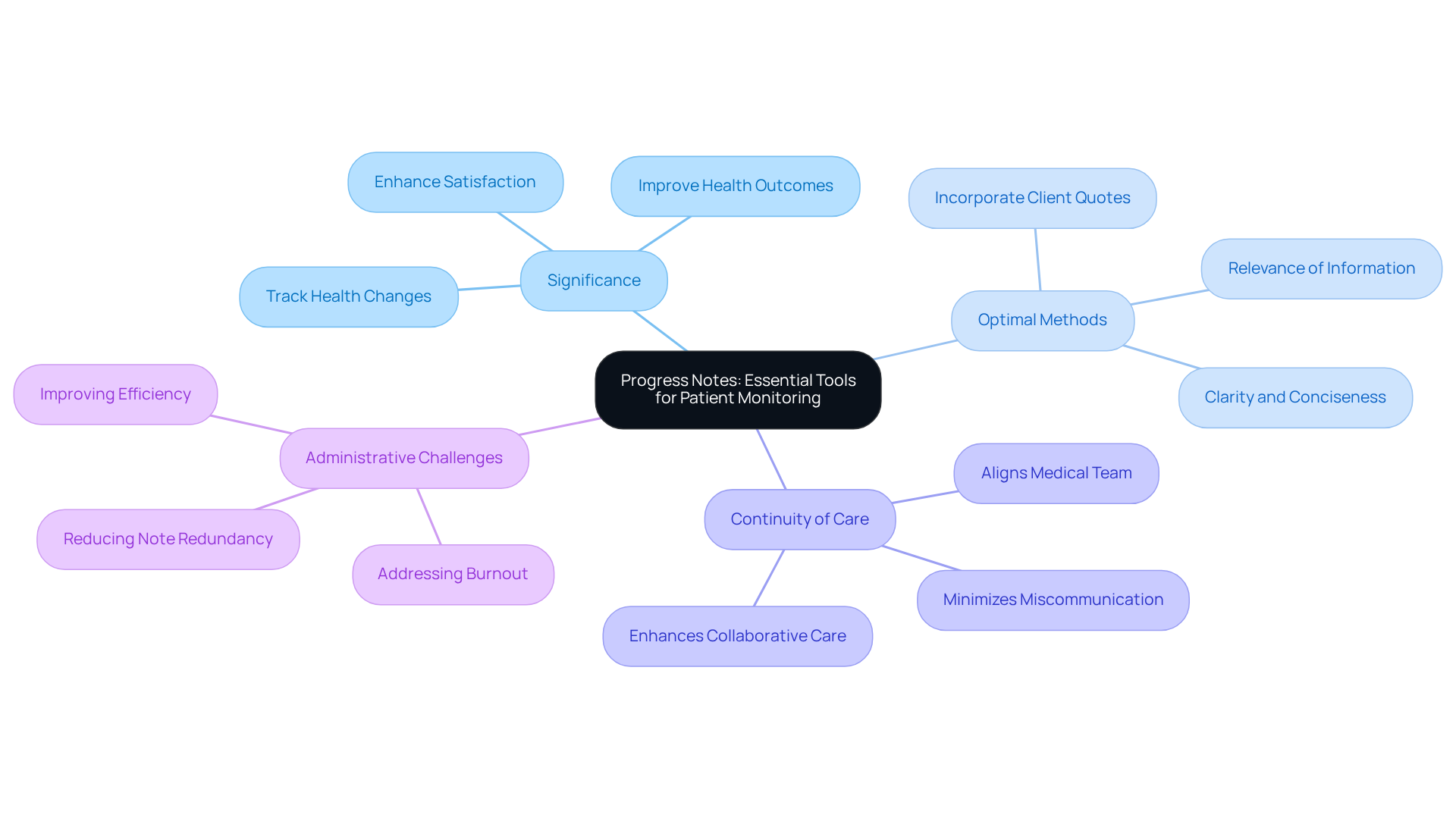
Progress Notes: Essential Tools for Patient Monitoring
Progress notes are vital records that capture the ongoing health status and treatment progress of individuals. They provide a comprehensive, chronological account of interactions, interventions, and outcomes, enabling healthcare providers to effectively track health changes and adjust treatment plans as necessary. In 2025, the significance of well-crafted progress notes is underscored by their direct impact on outcomes; studies reveal that thorough records can enhance satisfaction and health results.
Optimal methods for composing progress notes emphasize clarity, conciseness, and relevance. This ensures that all team members are informed about the individual's status. For instance, including direct quotes from individuals can enrich these records, offering valuable insights into their experiences and emotional states. This practice fosters a deeper connection between providers and individuals, which is essential for effective care.
Moreover, progress notes are crucial for continuity of care. They align all medical team members on the individual's treatment journey, minimizing the risk of miscommunication and enhancing collaborative care. Effective clinical documentation examples, such as progress notes, demonstrate how thorough records can improve care coordination, ultimately benefiting outcomes for individuals. By prioritizing comprehensive and meticulous records, healthcare professionals can significantly elevate the standard of care provided to those they serve.
Addressing the administrative challenges and inefficiencies in care provision, including physician burnout, is essential for refining the record-keeping process and enhancing overall healthcare. How can we support one another in tackling these challenges? Together, we can create a more .
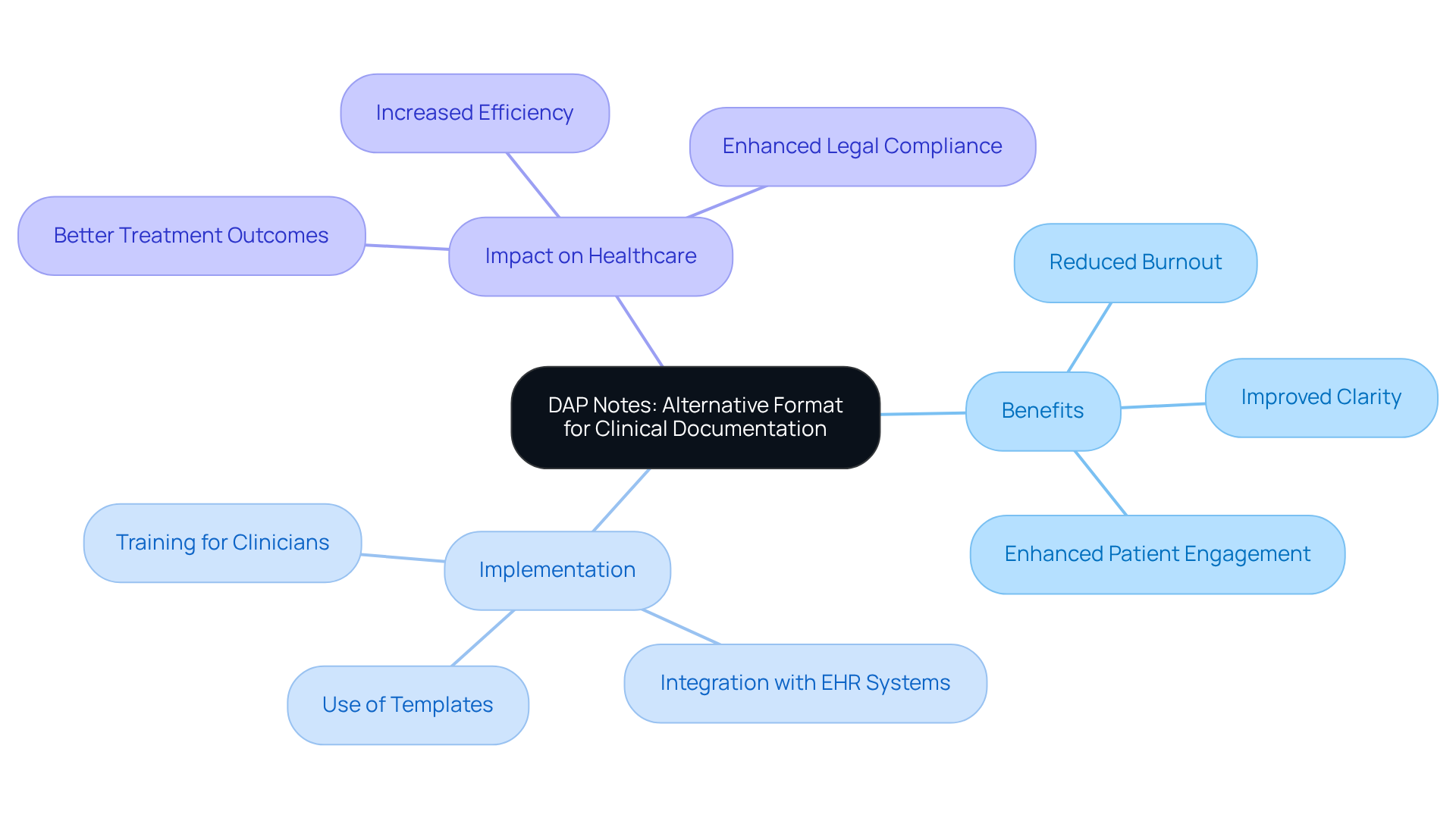
DAP Notes: Alternative Format for Clinical Documentation
In the demanding world of healthcare, many providers experience emotional challenges, including burnout. Statistics reveal that nearly half of medical workers face this issue, which can be alleviated through effective clinical documentation examples. DAP notes, representing Data, Assessment, and Plan, present a compassionate solution. This streamlined format captures essential data and assessments while outlining a clear plan for patient care, allowing clinicians to focus more on their interactions with clients.
Imagine the relief of minimizing time spent on documentation. By adopting clinical documentation examples like DAP notes, healthcare professionals can enhance clarity and efficiency in their record-keeping practices. Those who have embraced this format report significant improvements in their clinical documentation examples. This shift not only fosters better patient engagement but also promotes care continuity, addressing the core concerns of both providers and patients.
As we look to July 2025, the benefits of DAP notes in behavioral health are increasingly recognized. Numerous practitioners are incorporating this format into their methods, leading to more effective tracking of client progress. For example, therapists using DAP notes ensure that treatment plans remain relevant and responsive to individual needs. This compassionate approach not only enhances the quality of care but also helps professionals manage their administrative duties with greater ease.
Are you ready to explore how DAP notes can transform your practice? By embracing this method, you can alleviate some of the burdens of documentation and focus on what truly matters—your clients. Together, let’s for both providers and patients.
Legal and Ethical Considerations: Safeguarding Patient Documentation
Legal and ethical factors in clinical records are crucial for safeguarding individual information and ensuring adherence to medical regulations. Have you ever considered how these elements affect your practice and your patients? HIPAA requires that medical providers protect individual privacy, with recent statistics revealing that 70% of organizations faced a HIPAA incident in the past year. This reality can be daunting, especially when we learn that 32% of all from 2015 to 2022 occurred in the healthcare sector. The magnitude of this issue underscores the necessity for rigorous record-keeping practices.
Ethical documentation practices necessitate precise representation of individual information. Misrepresentation can lead to breaches of trust, which no healthcare provider wants to experience. For instance, improper disposal of protected health information (PHI) can result in significant violations. It's concerning to note that negligent insiders account for over 60% of insider incidents. This highlights the importance of being vigilant in our documentation practices.
Moreover, the majority of HIPAA enforcement activities focus on non-compliance with individuals' rights standards of the HIPAA Privacy Rule. Are you aware of the specific areas where practitioners often fall short? Furthermore, 60% of medical professionals are not fully confident they would pass a HIPAA audit, illustrating a lack of readiness among practitioners. By adhering to these legal and ethical standards, medical providers not only comply with regulations but also foster trust and maintain the integrity of care for individuals. This ultimately enhances the overall experience for both providers and patients.
Consider the financial implications as well; the typical expense of a healthcare data breach is $7.13 million. This figure highlights the serious consequences of non-compliance and the urgent need for strong record-keeping practices. Let’s work together to create a safer, more trustworthy healthcare environment for everyone.
Telehealth Documentation: Best Practices for Remote Care
Navigating telehealth documentation can be challenging for healthcare providers, as they strive to ensure that remote client interactions are accurately recorded and meet regulatory standards. It’s essential to recognize the emotional weight of these responsibilities. Key practices, such as:
- Documenting the patient's location
- The technology used for the visit
- Obtaining informed consent
serve as foundational steps in this process.
Moreover, capturing all relevant clinical information during the session is vital for maintaining continuity of care. This not only supports the but also reassures patients that their care remains consistent and thorough. By adhering to these best practices, healthcare providers can enhance the quality of telehealth services, ensuring that records not only meet legal standards but also reflect the compassionate care that patients deserve.
Imagine the peace of mind that comes from knowing you are providing the best possible care, even in a virtual environment. By embracing these practices, you can foster a supportive atmosphere for your patients and alleviate some of the administrative burdens that can weigh heavily on your shoulders. Let's work together to improve our telehealth services, ensuring that every interaction is meaningful and compliant.
Patient-Generated Health Data: Integrating Insights into Documentation
Individual-generated health data (PGHD) represents valuable health information created and recorded by individuals beyond the confines of traditional clinical settings. This data holds the potential to transform clinical documentation examples by offering into a person's health status, lifestyle choices, and adherence to treatment plans. Imagine how, by harnessing this information, medical professionals can craft more personalized care plans that not only enhance client engagement but also elevate satisfaction levels.
Consider this: studies reveal that 57.9% of healthcare integrations actively utilize biometric and individual activity data. Such information can significantly inform clinical decisions, leading to better outcomes for patients. However, effective integration of PGHD requires clear communication with individuals, highlighting the importance of their contributions to health records. This approach fosters a cooperative care environment, empowering individuals to take an active role in managing their health.
Are we truly leveraging the insights that PGHD offers? By recognizing the emotional challenges faced by healthcare providers and patients alike, we can pave the way for a more supportive and collaborative healthcare experience. Let’s embrace the potential of PGHD together, enriching our understanding of health and enhancing the quality of care we provide.
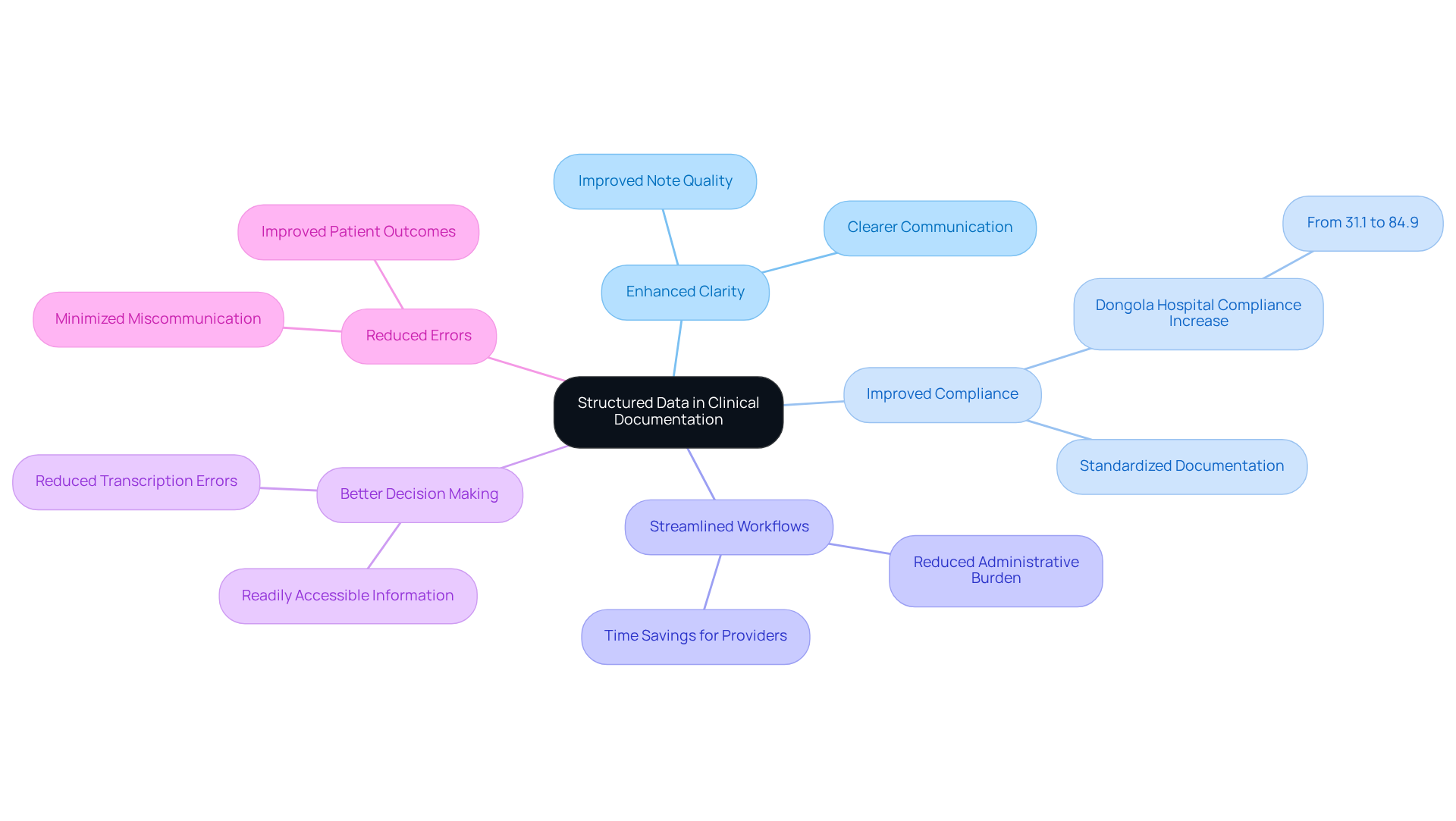
Structured Data: Enhancing Clarity in Clinical Documentation
Structured data in clinical records plays a vital role in ensuring that information is organized in a standardized format. This organization significantly enhances data accuracy and retrieval efficiency, which can alleviate some of the administrative burdens that healthcare providers often face. By adopting structured data practices, medical providers not only enhance the clarity of client records but also streamline workflows and facilitate compliance with regulatory requirements. For instance, a clinical audit at Dongola Specialised Hospital revealed that implementing structured documentation templates led to a remarkable increase in compliance from 31.1% to 84.9%. This showcases the effectiveness of structured methods in improving documentation quality.
Moreover, structured data supports better clinical decision-making by ensuring that essential information is readily accessible. Have you ever experienced the frustration of searching for critical data? This method not only decreases the likelihood of transcription mistakes but also improves communication among medical teams, ultimately resulting in better outcomes for individuals. As we look ahead to 2025, the medical field will continue to evolve, highlighting the growing significance of data standardization. This will empower practitioners to while delivering high-quality care. For medical professionals seeking to improve their operational effectiveness and patient care standards, the incorporation of clinical documentation examples through organized record-keeping methods is crucial. Let’s embrace these practices together for a brighter future in healthcare.
Documentation Templates: Streamlining Clinical Processes
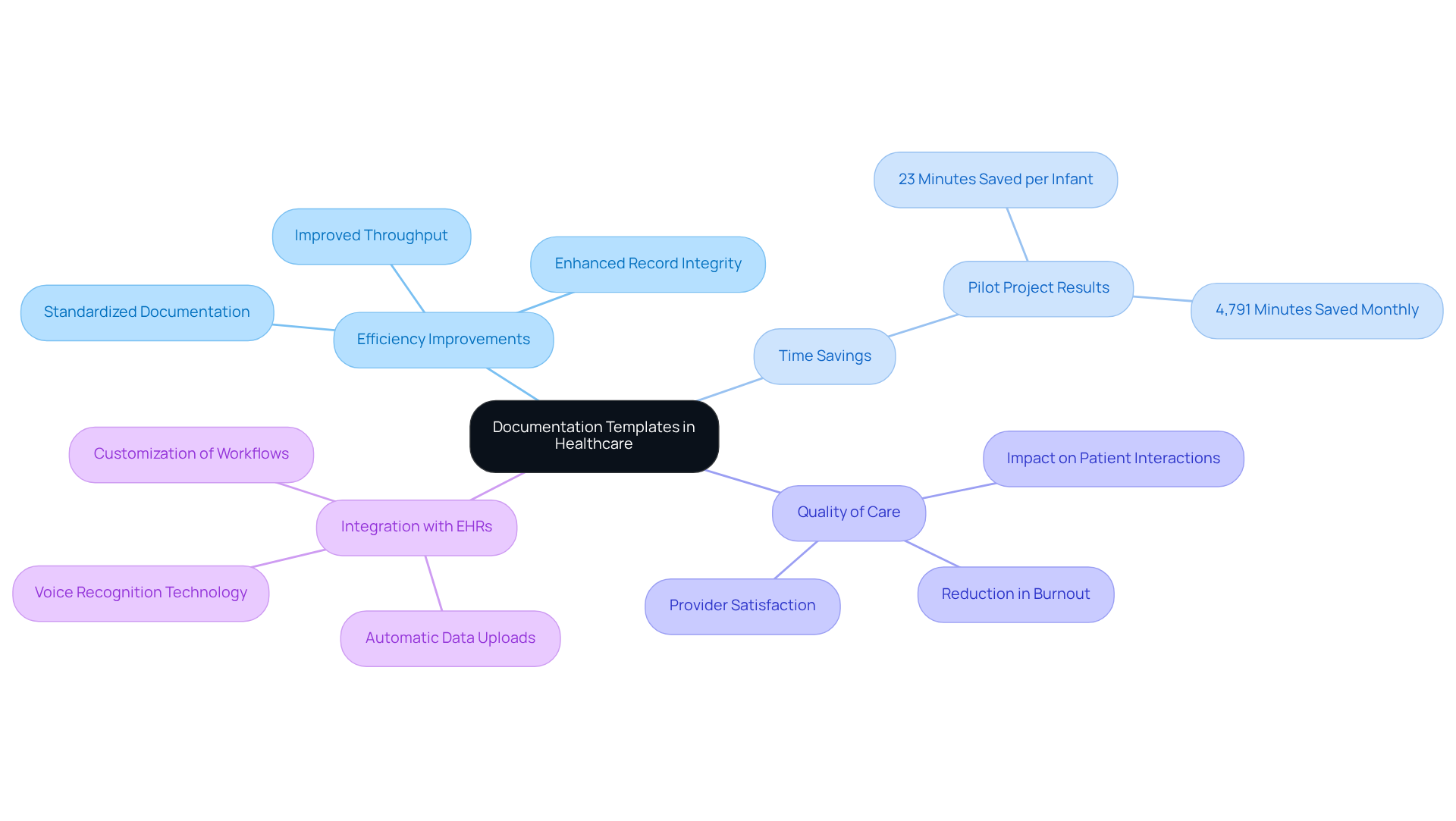
Healthcare professionals often face overwhelming administrative burdens that can detract from the quality of patient care. Templates serve as pre-designed forms that help standardize clinical documentation examples, significantly improving the efficiency of record-keeping processes. By implementing these templates, clinicians can save valuable time while ensuring that all essential information is consistently captured. Customized for particular specialties or visit types, these templates not only enhance usability but also maintain high standards of record quality.
Consider a pilot project in a Maternal and Baby Unit, where optimizing physician note templates saved an average of 23 minutes per infant during their hospital stay. This led to a remarkable total of 4,791 minutes saved monthly across the unit. Such efficiency translates into enhanced direct client care time, allowing caregivers to focus more on meaningful interactions with individuals rather than administrative duties.
Moreover, nearly 75% of medical professionals believe that record-keeping demands adversely affect care quality. This highlights the urgent need for efficient procedures. By standardizing clinical documentation examples with templates, medical professionals can enhance record integrity, improve throughput, and ultimately foster a more effective delivery system. Additionally, integrating these templates with Electronic Health Records (EHRs) can further decrease record-keeping time and enhance overall efficiency.
Imagine the possibilities when generative AI is utilized to automate the creation and management of template files. Medical practitioners can regain precious time for direct patient care, significantly improving the overall patient experience. Enhanced billing methods can also lead to higher income for medical providers, underscoring the necessity for effective record-keeping strategies.
In light of these insights, how can your practice begin to implement these changes? Together, we can .
Evolving Demands: Adapting Clinical Documentation Practices
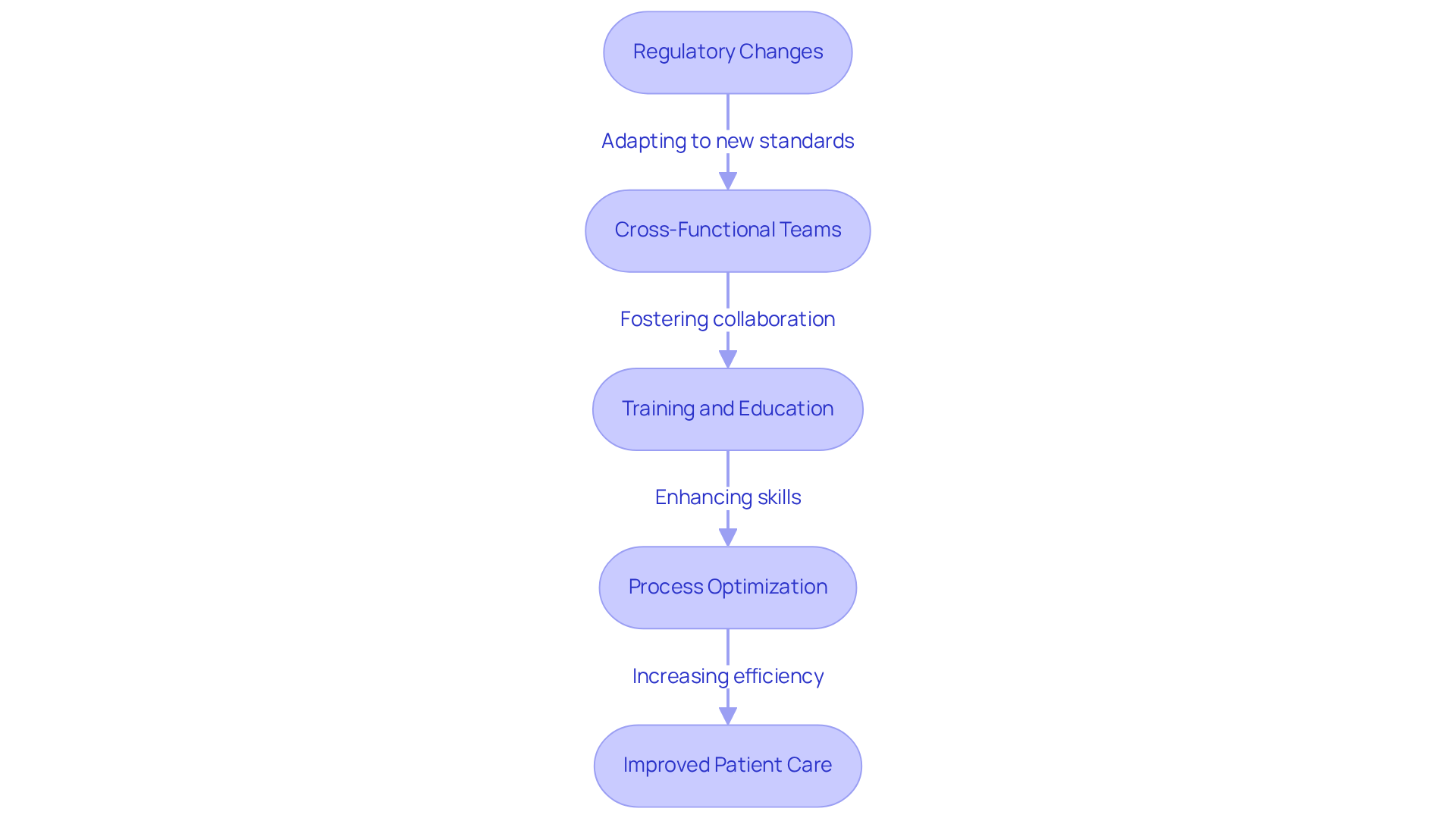
The medical environment is undergoing constant change, and this evolution can feel overwhelming for healthcare providers. As new demands arise, clinical documentation examples must adapt to keep pace. Regulatory changes, like the introduction of new coding standards in 2025, aim to enhance the precision and specificity of medical service documentation. This increased granularity in diagnostic and procedural codes may raise concerns about compliance and billing errors, prompting the need for healthcare professionals to invest in training and technology. How can we ensure that these changes lead to improved patient care rather than added stress?
Healthcare providers are already responding positively to these regulatory changes. By establishing cross-functional teams that include members from billing, compliance, IT, and clinical departments, they foster collaboration and innovation. This teamwork ensures that clinical documentation examples are aligned with regulatory expectations. Organizations that prioritize continuous education and training for their billing professionals are better positioned to navigate the complexities of updated coding guidelines and compliance requirements. This proactive approach not only improves billing efficiency but also reduces errors, ultimately benefiting patient care.
However, challenges remain. The increased administrative burdens and potential disruptions in billing workflows due to regulatory updates can be daunting. To address these challenges, medical organizations must adopt and process optimization strategies. Regular audits and the use of data analytics can significantly enhance billing efficiency and adherence. How can we monitor compliance and identify areas for improvement before issues escalate?
By embracing these changes and adapting their strategies based on clinical documentation examples, healthcare professionals can maintain compliance while enhancing patient care and outcomes. For instance, implementing regular training sessions on new coding standards empowers staff to stay informed and proficient. This positions providers as leaders in operational efficiency and quality care. Let’s work together to navigate these changes and ensure that we continue to provide the best possible care for our patients.
Conclusion
Embracing effective clinical documentation practices is essential for enhancing patient care and improving the overall healthcare experience. Have you ever felt overwhelmed by administrative tasks? By utilizing innovative tools like CosmaNeura and structured methods such as SOAP and DAP notes, healthcare providers can significantly reduce these burdens, allowing them to focus more on their patients. This shift not only promotes efficiency but also nurtures a compassionate environment where patient interactions can thrive.
Throughout this article, we've explored various clinical documentation examples, highlighting their importance in improving communication, ensuring legal compliance, and fostering better patient-provider relationships. The integration of patient-generated health data and structured documentation emphasizes the need for a collaborative approach in healthcare, where both providers and patients play active roles in the documentation process.
As the healthcare landscape continues to evolve, it is crucial for professionals to adapt their documentation practices to meet new demands and regulatory changes. By prioritizing effective record-keeping strategies, healthcare providers can enhance care quality, streamline operations, and ultimately create a more supportive environment for both patients and practitioners. The call to action is clear: it is time to embrace these advancements and commit to transforming clinical documentation for a brighter future in patient care.




