Overview
The article highlights essential examples of medical notes that every healthcare provider should be familiar with, recognizing their crucial role in patient care and communication. Have you ever felt overwhelmed by the administrative burdens that can detract from your focus on patients? Understanding various types of medical documentation, such as SOAP notes, discharge summaries, and progress notes, can alleviate some of that stress. These records not only streamline communication but also enhance patient outcomes through thorough documentation practices.
By embracing effective documentation methods, you can foster clearer communication with your colleagues and patients alike. Imagine the peace of mind that comes from knowing your notes are contributing to improved patient care. This article serves as a supportive guide, encouraging you to explore these vital tools in your practice.
Incorporating these practices can lead to more meaningful interactions with your patients, ultimately benefiting their health and well-being. Let’s take a step together towards enhancing our documentation skills for the betterment of patient care. Your commitment to learning and improvement is a powerful tool in the healthcare field.
Introduction
In the intricate world of healthcare, medical notes are not just paperwork; they are the backbone of effective patient care. These notes encapsulate vital information that drives clinical decisions and enhances communication among providers. Have you ever considered how the landscape of healthcare is evolving? The significance of meticulous documentation is becoming increasingly pronounced, with studies showing a direct link between accurate medical notes and improved patient outcomes.
Each component of medical documentation, from the structured SOAP format to the nuanced capture of subjective experiences, plays a crucial role in fostering a collaborative relationship between patients and providers. As technology advances, integrating AI solutions offers a promising path to streamline documentation processes. This allows healthcare professionals to focus on what truly matters: delivering exceptional patient care.
This article delves into the critical elements of medical notes, exploring their impact on patient engagement, safety, and the overall quality of care in our rapidly changing healthcare environment. Together, we can navigate these challenges and enhance our approach to patient care.
Understanding Medical Notes: A Vital Component of Patient Care
An example of a medical note is an essential written document that captures vital information about an individual's health status, treatment plans, and progress. These notes play multiple crucial roles: they promote smooth communication among healthcare providers, ensure compliance with legal and regulatory standards, and enhance safety for individuals receiving care. Precise records of client interactions empower providers to make informed choices that significantly impact outcomes for individuals.
In 2025, the significance of is more critical than ever. Recent studies indicate that is directly linked to better health results. There is a significant correlation between comprehensive record management and improved care quality. For instance, a scoping review identified 37 records meeting inclusion criteria, underscoring the essential role of records in user engagement and satisfaction.
Moreover, real-world examples illustrate how effective can lead to better outcomes for individuals. One case study explored barriers to individual engagement with (PEHRs), revealing that concerns about data validity and complexity often hinder active participation. By addressing these issues through enhanced PEHR design and clinician involvement, greater individual engagement and satisfaction.
Jigar Patel, creator of Health-e, emphasizes, "Individuals must be enabled to engage in their own healthcare," highlighting the importance of proper records in achieving this goal.
Recent statistics reveal that only 5% to 9% of active portal users maintain their data for over a year. This statistic highlights the urgent need for improved record-keeping methods that encourage continuous user engagement. Additionally, individuals have expressed concerns about potential charges for portal access, which may further limit their involvement and exacerbate disparities in healthcare access.
Integrating AI solutions, such as those offered by CosmaNeura, can significantly improve the efficiency of medical documentation. can help identify individuals at higher risk of developing specific conditions, enabling healthcare providers to implement preventive measures early. This proactive approach not only enhances outcomes for individuals but also reduces the administrative burden on doctors, alleviating burnout and allowing them to focus more on individual support.
Ultimately, not only enhances patient safety but also ensures that all team members are aligned in their approach to care, improving the overall healthcare experience. As healthcare experts recognize the profound impact of precise medical records, they can more effectively support practices that prioritize comprehensive and efficient record-keeping.
Key Solutions:
- Improve PEHR design to address user concerns.
- Implement AI solutions for predictive analytics.
- Foster continuous engagement through .
By taking these steps, we can create a more supportive environment that empowers individuals in their healthcare journey.
The SOAP Note Format: Structure and Significance
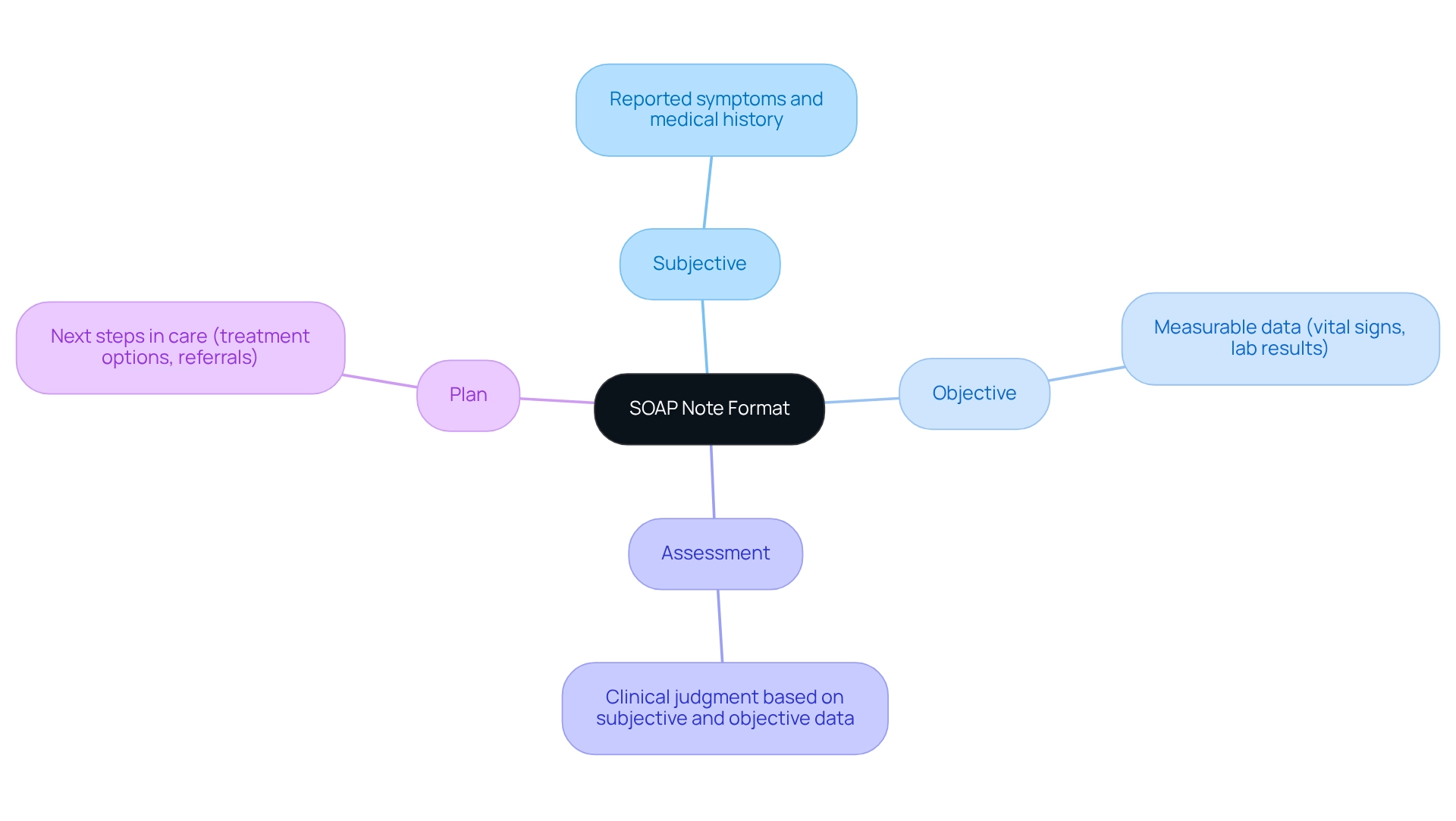
The is an essential instrument in clinical records, consisting of four main elements: Subjective, Objective, Assessment, and Plan. This organized method allows healthcare providers to systematically record client encounters, ensuring clarity and consistency in care.
- Subjective: This section captures the individual's reported symptoms, concerns, and medical history, providing insight into their experience and perspective.
- Objective: Here, measurable data such as vital signs, lab results, and physical examination findings are documented, offering a factual basis for clinical evaluation.
- Assessment: This component synthesizes the subjective and objective information to formulate a clinical judgment, allowing providers to identify the individual's condition and potential complications.
- Plan: The final section outlines the next steps in care, including treatment options, referrals, and follow-up appointments.
Utilizing the SOAP format not only enhances the clarity and conciseness of records but also improves the overall quality of care. Have you ever considered how organized records can lead to better outcomes for individuals receiving care? Research shows that is critical, ensuring that essential information is easily accessible.
In 2025, optimal practices for SOAP records stress the significance of precision and thoroughness. Aiming for a 99% or higher accuracy rate is vital to prevent legal complications and ensure the safety of individuals receiving care. Choosing a is essential for healthcare providers to uphold these standards. Providers who implement SOAP records effectively often report increased job satisfaction and improved experiences for those they serve, as these records streamline workflows and reduce administrative burdens.
CosmaNeura, as the sole company developing for the billion-dollar faith-focused healthcare market, exemplifies how technology can . By automating and offering AI-driven services, CosmaNeura not only enhances record-keeping efficiency but also supports aligned with Catholic teachings. Case studies show that organizations , especially those using CosmaNeura's platform, have observed .
For instance, a primary health clinic that incorporated SOAP records into their practice reported a 30% decrease in record-keeping time. This change enabled clinicians to allocate more time to direct interactions with individuals, fostering stronger connections.
The healthcare sector encounters many obstacles, including broken communication, regulatory hurdles, and increasing expenses, which can impede effective service delivery. Have you felt the weight of these challenges? Expert opinions underscore the , serving as a model for medical documentation that supports clinical decision-making while aligning with ethical practices. By following the SOAP format, healthcare professionals can ensure their documentation is thorough and indicative of their dedication to high-quality service.
Moreover, the incorporation of AI solutions into this process tackles essential challenges in healthcare delivery, improving individual service and provider efficiency through streamlined administrative workflows.
Subjective Notes: Capturing the Patient's Voice
Subjective notes are essential in capturing an individual's perspective on their health, forming a vital part of the SOAP note. This section reflects the individual's own descriptions of symptoms, feelings, and concerns, which are crucial for effective clinical care. For example, one might say, 'I have been feeling more anxious lately and have trouble sleeping.'
By documenting these , can tailor their assessments and interventions to meet the . This prioritization not only enhances the but also fosters a collaborative and trusting relationship between individuals and providers.
Research indicates that when clinicians actively incorporate into their practice, it strengthens the clinician-client relationship and places individuals at the heart of the healthcare process. Studies reveal extremely high correlations (greater than 0.95) between various methods of related to , highlighting the reliability of these insights.
Furthermore, the Journal of the American Medical Association noted, "Results were very positive in favor of the accuracy of reported data," reinforcing the importance of capturing the individual's voice.
Real-world examples illustrate the profound impact of . For instance, focus group studies involving individuals with glaucoma identified ten distinct domains of importance, shedding light on psychosocial impacts like emotional well-being and social concerns. These qualitative insights complement quantitative findings, emphasizing the multifaceted challenges faced by individuals and the necessity of addressing their subjective experiences.
Moreover, may fall short in capturing the quality of life effects of glaucoma treatments, signaling a need for more sensitive and specific assessment tools.
The significance of personal observations extends beyond individual interactions; they greatly enhance communication between provider and client. By effectively recording client concerns, providers can ensure treatment plans align with the individual's values and preferences, ultimately leading to improved satisfaction and adherence to treatment.
As we approach 2025, the emphasis on personal observations in healthcare is growing, indicating a shift towards more individualized and compassionate medical practices. By integrating these insights into medical records, healthcare providers can enhance clinical outcomes while embodying the .
Objective Notes: Documenting Clinical Findings
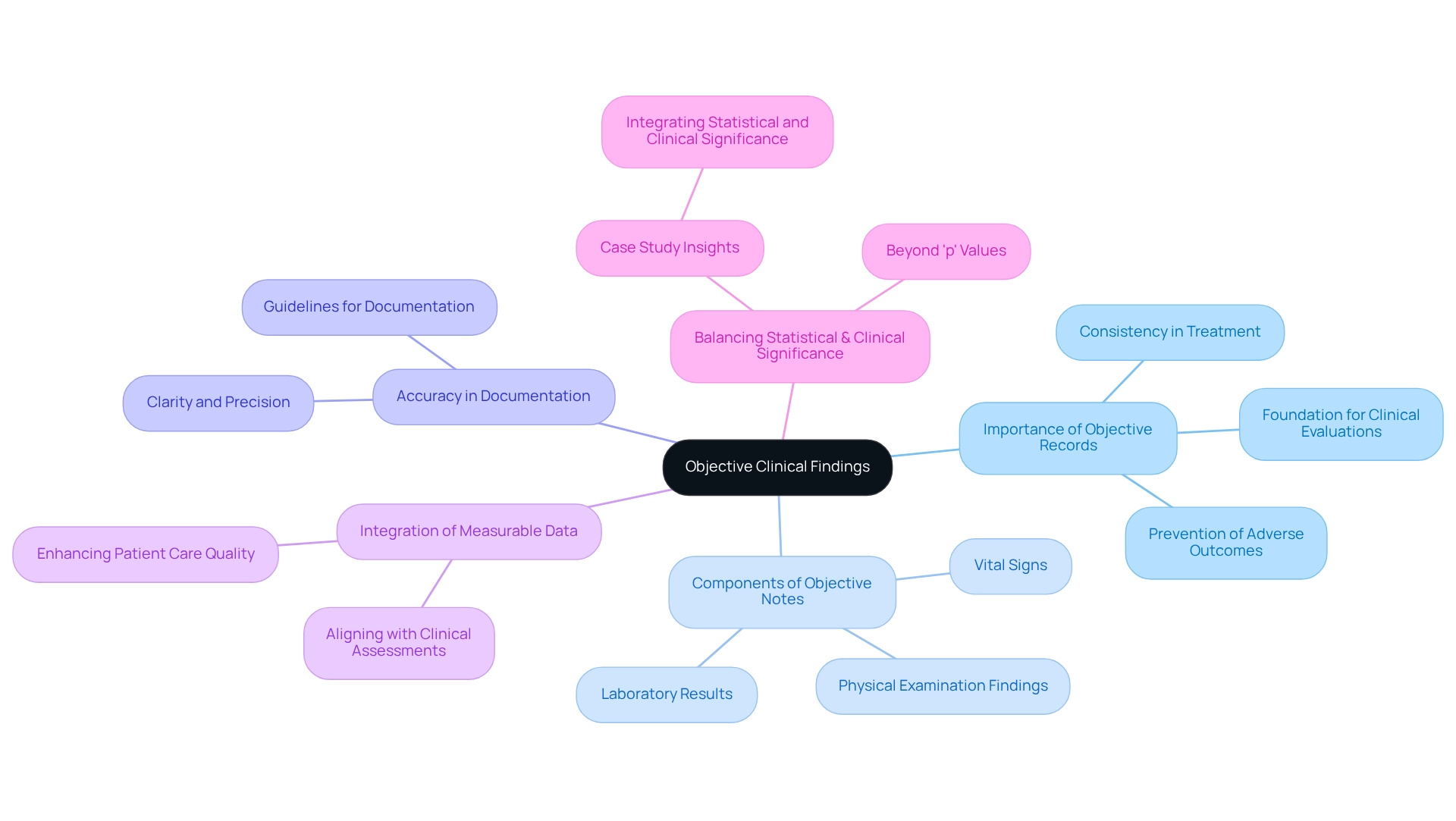
Objective records play a crucial role in , serving as the backbone of measurable and observable information gathered during client interactions. These records include vital signs, physical examination findings, and laboratory results. For instance, a medical note might document: Blood pressure 120/80, heart rate 72 bpm, and temperature 98.6°F.
Such provide a factual foundation for , essential for monitoring changes in an individual's condition over time. Have you ever considered how vital these details are in your daily practice?
The importance of cannot be overstated. They ensure that all involved in an individual's treatment have access to consistent and reliable information, which is vital for effective therapy planning. Each year, 16 billion injections are administered worldwide. Unfortunately, unsafe practices can lead to , underscoring the critical need for precise documentation to prevent adverse outcomes.
Moreover, integrating measurable data into clinical assessments aligns with the latest guidelines for documenting objective clinical findings. These guidelines stress clarity and precision, reinforcing the role of unbiased records in enhancing quality. As Hunny Sharma from the Department of Community and Family Medicine notes, "It is high time now that the researchers, journal editors, and readers should take a keen interest in looking beyond the threshold 'p' value and also rather than just assessing the worth of research by considering the 'p' values."
This perspective highlights the necessity of balancing statistical significance with clinical relevance in record-keeping practices. Additionally, a case study titled " emphasizes achieving this balance to ensure findings are both statistically robust and clinically meaningful. As healthcare continues to evolve, the emphasis on objective records will remain paramount, ensuring that clinical decisions are informed by robust and reliable data.
The ongoing encouragement for researchers and healthcare providers to consider both statistical and clinical significance when evaluating research results further aligns with the emphasis on accurate documentation in clinical assessments. How can we ensure that our documentation practices reflect the compassion and care we strive to provide to our patients?
Assessment Notes: Formulating Clinical Judgments
The Assessment section of the represents a crucial juncture where healthcare providers synthesize insights from the Subjective and Objective sections to form . This synthesis is vital for diagnosing conditions, recognizing potential complications, and assessing the effectiveness of ongoing treatments. For instance, a medical note might state, 'Patient presents with symptoms consistent with generalized anxiety disorder, requiring further evaluation and management.'
Such careful analysis not only influences timely care decisions but also shapes future treatment strategies, ensuring a comprehensive approach to patient needs.
The significance of extends beyond immediate clinical assessments; they play an essential role in guiding . Research indicates that effective relies heavily on well-organized assessment records. Notably, studies reveal that 74% of healthcare providers utilizing (CDSS) still face challenges related to , underscoring the need for clarity and accuracy in records. CDSS functions—ranging from diagnostics to prescription support—manifest as alerts, guidelines, and workflow tools that enhance clinical decision-making.
Moreover, the transition to has introduced complexities that can overwhelm clinicians if not managed appropriately. A case study titled 'Challenges of Electronic Medical Documentation' illustrates how the shift to electronic records, while improving data availability, can result in excessive information that burdens providers. This situation emphasizes the necessity for concise and clinically relevant data presentation in evaluation records, as the risk of errors can potentially jeopardize patient safety.
Acknowledging expert perspectives, it is crucial to recognize that the assessment component of SOAP records is not merely a formality; it is a vital element that influences clinical outcomes. As Reed T. Sutton notes, 'Extra precautions and conscientious design must be taken when building, implementing, and maintaining CDSS.' This highlights the importance of ensuring that the information within evaluation records is both actionable and relevant.
Therefore, the Assessment section is essential not only for immediate but also for fostering long-term health outcomes through informed clinical decision-making. How can we ensure that our records serve as effective tools in this process? Let’s continue to strive for clarity and compassion in our documentation.
Plan Notes: Outlining Future Care Strategies
The Plan segment of the SOAP note plays a crucial role in outlining the next steps in an individual’s treatment journey, encompassing diagnostic tests, referrals, medications, and . For instance, a provider might document: 'Refer to a mental health specialist for further evaluation; initiate cognitive behavioral therapy; schedule follow-up in four weeks.' This organized approach ensures that all members of the healthcare team are aligned with the agreed-upon strategies, significantly enhancing patient involvement in their treatment process.
Research shows that effective treatment plans lead to improved outcomes. Organizations that incorporate social determinants of health data are projected to achieve an additional 12-17% enhancement in results. Furthermore, a study on outpatient follow-up services revealed that significantly improves compliance. Regina R Nelson, RN, noted, 'Despite these limitations, we believe it is reasonable to conclude that emergency department individuals who have their at the time of discharge are more likely to adhere to outpatient follow-up treatment.'
This highlights the importance of in .
Incorporating examples of medical notes into medical records is essential for , serving as a roadmap for both providers and patients. Optimal approaches for drafting these assistance plans in 2025 involve clearly outlining , using concise language, and ensuring that all relevant information is easily accessible. The case study titled 'Challenges in Ensuring Outpatient Follow-Up Support' discussed obstacles to follow-up support, emphasizing that arranging follow-up appointments at the time of ED discharge significantly enhances compliance.
By prioritizing , healthcare professionals can create medical notes that foster improved patient involvement and ultimately enhance the quality of services provided. Additionally, the Patient Protection and Affordable Care Act has incorporated measures for , underscoring the significance of within the broader healthcare policy framework.
Key Solutions:
- Clearly outline support strategies.
- Use concise language for clarity.
- Ensure accessibility of all pertinent information.
By implementing these strategies, we can create a more compassionate and effective healthcare environment.
Beyond SOAP: Exploring Other Essential Medical Notes
While the SOAP format is common in clinical practice, it's essential for healthcare providers to be well-versed in other vital types of medical documentation. History and Physical (H&P) records exemplify this, offering a along with current physical examination results. These records are fundamental in healthcare, aiding thorough evaluations and ensuring continuity of support.
Alongside H&P records, formats like progress reports and discharge summaries are crucial for documenting . Progress records monitor an individual's condition over time, while discharge summaries provide a brief overview of treatment and follow-up plans when leaving a healthcare facility.
Understanding the nuances of these different types of records enables providers to select the most appropriate format for each encounter, ultimately . For instance, a study examining data from 391 health systems revealed that and satisfaction.
Real-world examples further illustrate the impact of various medical documentation formats on quality of service. In one case study, the implementation of H&P notes in a primary care setting led to improved communication among healthcare teams and more informed clinical decisions. This showcases the importance of comprehensive record-keeping. Additionally, the case study titled 'Disparities in ' highlights ongoing inequalities in accessing medical records, emphasizing the need for thorough documentation in addressing these issues.
As the healthcare landscape evolves, providers must adapt to diverse reporting styles beyond SOAP to effectively meet the needs of those they serve. This adaptability not only fosters better client-provider relationships but also aligns with the growing emphasis on comprehensive and ethical care for individuals. As Wesley Barker, Chief of the Data Analysis Branch, noted, "Although most at least once in the past year via a web-based portal, a growing number reported using a smartphone health app to access their information."
This trend underscores the necessity for efficient record-keeping methods that cater to varying individual preferences.
In this context, CosmaNeura's pioneering role in providing is vital. Features like , streamlined data entry, and intelligent reminders significantly alleviate the administrative burdens that contribute to physician burnout. By enhancing service standards through , CosmaNeura's solutions empower healthcare providers to focus more on delivering exceptional client support.
This commitment to ethical standards not only addresses the challenges faced by healthcare providers but also ensures that the well-being of individuals remains the top priority.
Progress Notes: Monitoring Patient Progress
are a cornerstone of efficient healthcare, serving as essential documentation of an individual's ongoing health condition and the effectiveness of treatment measures. These observations include updates on the individual's condition, their reactions to different therapies, and any alterations to the treatment plan. For example, a provider might document, 'Patient reports reduced anxiety levels following therapy sessions; continue current treatment plan.'
Consistently refreshing progress records not only keeps healthcare providers aware of the individual's changing requirements but also enables prompt modifications to care approaches.
The importance of progress records extends beyond simple recording; they are crucial in tracking individual health. A recent study indicates that organizations incorporating into their population health models can achieve an additional 12-17% improvement in outcomes. This highlights the significance of thorough and precise progress documentation in capturing the complete context of an individual's health.
According to a recent survey by Deloitte, 87% of healthcare executives now rank among their top three strategic priorities—up from just 42% in 2018. This shift underscores the critical role of .
Furthermore, professional insights emphasize that effective progress documentation can greatly influence treatment results. Consistent revisions in these records enable providers to , ensuring that interventions stay aligned with the individual's needs. Clinicians who consistently document exemplify a medical note that has been associated with enhanced involvement and satisfaction among individuals.
Practical instances illustrate the advantages of careful progress record keeping. In one case study, mental health clinicians who utilized demonstrated , particularly among those with cognitive-behavioral orientations. This indicates that organized documentation can lead to more favorable outcomes for individuals receiving care.
The study explored professional and practice characteristics that predict attitudes toward monitoring and feedback, revealing that clinicians with cognitive-behavioral orientations held more positive attitudes toward standardized measures.
To enhance the effectiveness of progress notes, providers should follow , such as:
- Being concise yet comprehensive
- Using clear language
- Ensuring that notes are updated promptly after each client interaction.
By documenting treatment effectiveness clearly, providers can create a robust record that not only aids in but also enhances overall client support.
Discharge Summaries: Ensuring Continuity of Care
serve as vital records that encapsulate a patient's hospital experience and outline the necessary follow-up treatment. These summaries typically include crucial elements such as the reason for hospitalization, treatments provided, discharge diagnoses, and recommendations for ongoing support. A well-crafted discharge summary, an example of a medical note, might state, 'Patient discharged after treatment for pneumonia; follow up with primary care physician in one week.'
The is deeply intertwined with . Research reveals that the rate of is significantly lower for individuals receiving comprehensive discharge summaries, with only 31% requiring readmission compared to 44% in the control group. This underscores the importance of and readmissions.
To create effective discharge summaries, . Each summary should narrate the individual's journey clearly, highlighting essential information that promotes . For instance, a study analyzing readmission rates found that 71% of readmissions were avoidable, primarily due to premature discharge before conclusive therapy.
This illustrates how comprehensive discharge records can profoundly influence follow-up treatment and reduce . Including specialist perspectives in the discharge process can further enhance the effectiveness of these summaries. As Dr. Leora I. Horwitz states, 'The quality of discharge summaries is crucial in ensuring a smooth transition from hospital to home, ultimately promoting better outcomes for individuals.' By adhering to these guidelines and emphasizing the importance of thorough records, healthcare providers can significantly improve patient transitions and decrease readmission rates.
This commitment to quality aligns with , ensuring that all records reflect the values of compassion and responsibility inherent in Catholic teachings.
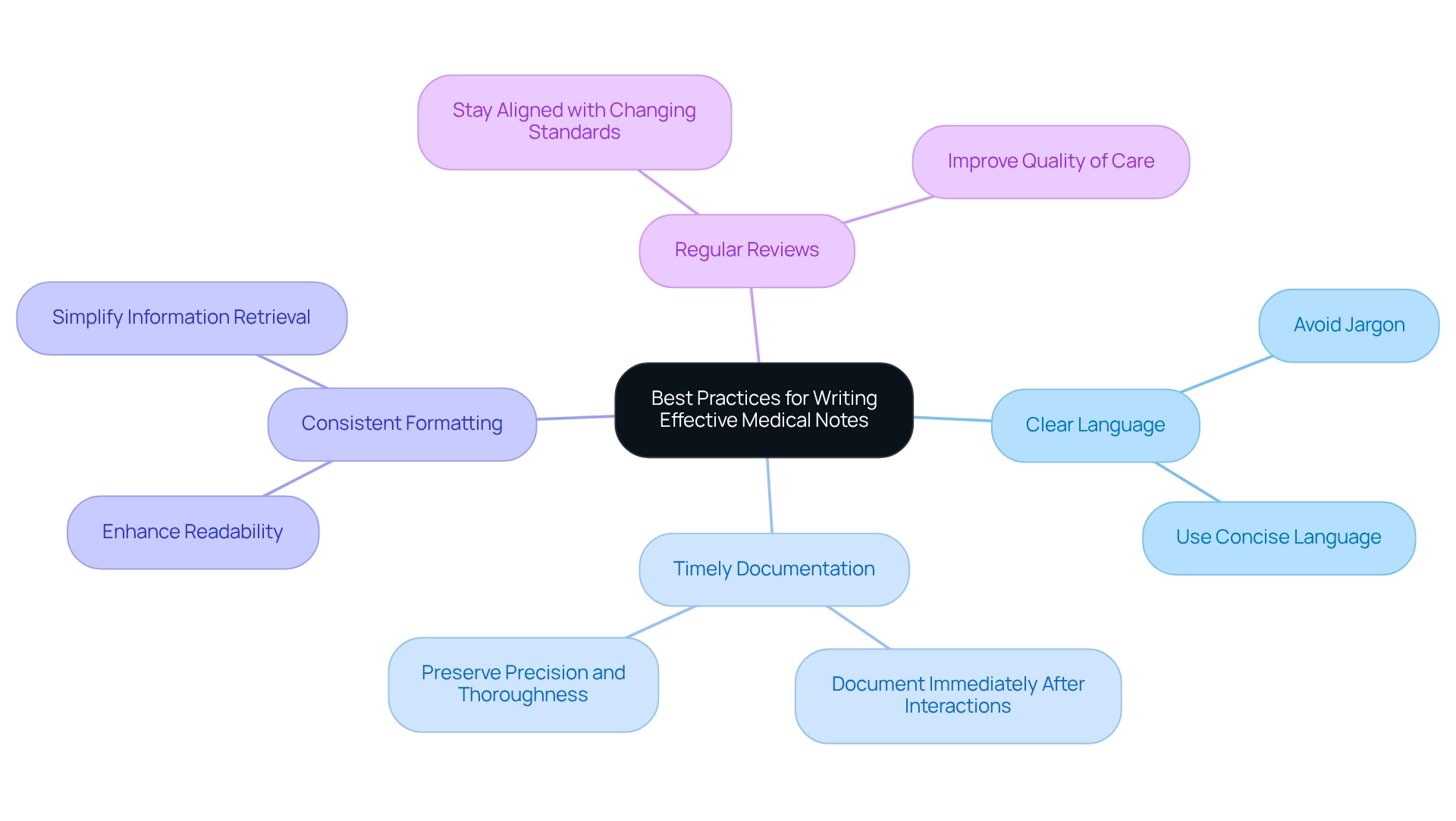
Best Practices for Writing Effective Medical Notes
Healthcare providers often face emotional challenges when creating medical notes. It can be overwhelming to ensure clarity while managing the demands of patient care. By utilizing clear and concise language, providers can ease their burden; this not only aids in understanding but also minimizes the risk of misinterpretation. Steering clear of jargon guarantees that all members of the healthcare team can comprehend the records, regardless of their specialty.
Prompt record-keeping is vital. Documenting pertinent information right after interactions with individuals helps preserve precision and thoroughness, which is essential for . Consistency in formatting further enhances readability, making it simpler for team members to find and understand essential details swiftly.
Have you considered how regularly reviewing and updating record-keeping practices can benefit you? This proactive strategy enables providers to stay aligned with changing standards and , ultimately enhancing the quality of care. For instance, a study examining almost 3 million outpatient progress records revealed that the average , and average redundancy grew by 10.9 percentage points over a decade. This shift toward lengthier and possibly more repetitive records highlights the significance of to improve their usefulness in patient care.
Furthermore, efficient record-keeping methods not only aid in recovery but also illustrate the medical necessity of interventions. This reinforces the importance of . As emphasized by UCLA researchers, restricting efficiency tools can ironically lead to more effective writing, indicating that simplicity in records can produce better outcomes.
Moreover, the constraints of the conventional SOAP format have prompted the creation of extensions such as SOAP, which fulfill the requirement for recording changes over time. This evolution in documentation practices is particularly relevant in the context of CosmaNeura, the only company creating AI solutions for . Here, is crucial for aligning with ethical standards and enhancing patient care.
In summary, adhering to these best practices—, , consistent formatting, and regular reviews—can significantly enhance the quality of medical notes. By doing so, you not only benefit your practice but also provide better care for your patients, exemplifying what excellence in medical note-taking truly means.
Conclusion
Effective medical notes are not just essential; they are the heart of patient care, forming the bedrock for clinical decision-making and fostering communication among healthcare providers. Have you ever considered how structured documentation can alleviate some of the emotional burdens you face? The SOAP note format stands out as a beacon, enabling comprehensive patient assessments by capturing subjective experiences, objective data, clinical judgments, and future care plans. By prioritizing meticulous documentation, you can significantly enhance patient engagement, safety, and overall care quality.
The integration of technology, especially AI-driven solutions, emerges as a transformative ally in enhancing documentation efficiency. These advancements not only lighten administrative loads but also empower you to focus on what truly matters: delivering compassionate and personalized care. As the healthcare landscape evolves, the significance of accurate and thorough medical notes will only increase, underscoring the need for ongoing adaptation and adherence to best practices.
In conclusion, your commitment to effective medical documentation is vital for nurturing a collaborative healthcare environment that prioritizes patient needs. By embracing structured formats, leveraging technological innovations, and capturing the patient's voice, you can significantly improve clinical outcomes and ensure that every patient receives the highest standard of care. As we move forward together, enhancing documentation practices will be pivotal in shaping a more efficient, equitable, and compassionate healthcare system.
- Embrace structured documentation to enhance clarity and communication.
- Leverage technology to reduce administrative burdens and focus on patient care.
- Capture the patient’s voice to foster engagement and improve outcomes.
Together, let’s commit to a future where effective documentation transforms patient care.




