Overview
This article highlights the vital role of SOAP charting in nursing, focusing on how this method fosters compassionate care through organized documentation of both subjective and objective patient information. Have you ever considered how much of an impact effective SOAP notes can have on clinical decision-making and patient outcomes? By emphasizing the need for empathetic record-keeping, we can address not just medical needs but also the emotional well-being of our patients.
As healthcare providers, we often face emotional challenges that can be exacerbated by administrative burdens. SOAP charting offers a solution, ensuring that we capture the complete picture of our patients' needs. Imagine the difference it could make in your practice if every note reflected not only the clinical facts but also the compassion that drives our work.
Incorporating this structured approach can enhance the quality of care we provide, leading to improved patient experiences and outcomes. Let's embrace this method together, recognizing that our documentation can be a powerful tool in delivering the empathetic care our patients deserve.
Are you ready to take the next step in your practice? Consider how implementing SOAP charting can transform your approach to patient care, ensuring that every aspect of their experience is thoughtfully recorded and addressed.
Introduction
In the realm of healthcare, effective communication and documentation are not just tasks; they are the foundation of quality patient care. Have you ever considered how SOAP charting—an acronym for Subjective, Objective, Assessment, and Plan—provides a structured framework that organizes critical patient information? More importantly, it fosters a compassionate approach to nursing, addressing the emotional needs of both patients and providers.
As our healthcare landscape evolves, the integration of technology, particularly AI solutions, is reshaping how providers document patient encounters. This shift enhances clarity and collaboration among teams, but it also brings challenges. Are we truly prepared to embrace these changes while ensuring that empathy remains at the forefront of our practice?
This article delves into the significance of compassionate SOAP charting, exploring its profound impact on patient outcomes. By examining real-world applications and best practices, we highlight the necessity of empathetic documentation in nurturing trust and understanding between providers and patients. Ultimately, this approach leads to improved care and satisfaction, fostering a supportive healthcare environment for all involved. Let’s explore together how we can make a difference in our documentation practices.
Understanding SOAP Charting: A Compassionate Approach
SOAP charting, which stands for Subjective, Objective, Assessment, and Plan, is an essential recording method in healthcare that fosters systematic logging of encounters with individuals. This organized approach not only gathers all relevant information but also allows nurses to maintain a caring focus on care. By utilizing SOAP charting, healthcare providers can enhance clarity and comprehensiveness in their records, which is vital for effective clinical decision-making.
As we look toward 2025, recent trends indicate a rise in the adoption of electronic nursing notes, significantly improving the record-keeping process. This shift facilitates better communication and collaboration among healthcare teams, aligning with the increasing emphasis on empathetic records. Such records are crucial for fostering trust and understanding between providers and individuals. CosmaNeura, the sole company developing AI solutions for the billion-dollar faith-oriented healthcare market, emphasizes that incorporating technology in record-keeping practices can further enhance these benefits.
AI algorithms have the capability to analyze large datasets, identifying genetic markers and biomarkers associated with specific diseases or treatment responses. This allows for more personalized medicine approaches, maximizing treatment effectiveness while minimizing adverse effects.
The impact of structured documentation on healthcare outcomes cannot be overstated. Studies have shown that implementing SOAP charting results in enhanced care by ensuring that all relevant information is readily accessible to the healthcare team. This accessibility empowers informed decision-making, ultimately leading to improved health outcomes for individuals.
Moreover, the transformative role of AI in personalized medicine has the potential to revolutionize healthcare by providing targeted therapies that align with individual needs, thereby enhancing overall outcomes. Additionally, AI can significantly reduce physician fatigue by simplifying the administrative duties linked to SOAP charting, allowing healthcare providers to focus more on care. Empathetic record-keeping is increasingly recognized as a fundamental aspect of quality healthcare.
By focusing on the individual's experience and needs, nurses can cultivate a more compassionate atmosphere that promotes healing and well-being. As healthcare evolves, the importance of maintaining a caring mindset in record-keeping practices remains paramount.
Current statistics reveal that implementing SOAP charting can lead to a substantial reduction in record-keeping errors, thereby enhancing safety for individuals. Expert insights from 2025 highlight that organized records not only improve workflow for nurses but also contribute to a more comprehensive understanding of healthcare. It is essential for nurses to protect individual privacy while documenting by remaining HIPAA compliant, ensuring that notes are secured and utilizing bed or room numbers instead of names.
In conclusion, the advantages of SOAP charting extend beyond mere compliance; they include enhanced service delivery, improved communication among healthcare providers, and a commitment to compassionate, ethical practices in nursing. As evidenced by several case studies, the integration of AI solutions from CosmaNeura into healthcare documentation can further streamline administrative tasks, reduce physician burnout, and ultimately lead to better outcomes for individuals.
Capturing the Subjective: Listening to Patient Voices
The subjective section of a SOAP note serves as a vital platform for nurses to document the individual's own words regarding their symptoms, feelings, and experiences. This aspect is essential for understanding the individual's perspective and tailoring care to their unique needs. For instance, a nurse might document, 'Patient reports feeling anxious about upcoming surgery, stating, 'I’m really scared about the anesthesia.'
By capturing such sentiments, nurses can effectively address emotional concerns and provide reassurance, thereby enhancing the overall experience of those receiving care.
In 2025, the significance of capturing individual voices in nursing has become increasingly acknowledged. Research indicates that 53.5% of women reported experiencing anxiety compared to 46.5% of men, underscoring the need for healthcare providers to be attuned to these emotional states. By integrating subjective information into individual treatment, nurses can cultivate a more compassionate atmosphere that recognizes and affirms individual emotions, aligning with CosmaNeura's mission to enhance the quality of service through ethical practices.
Case studies on patient-centered care illustrate the effectiveness of subjective documentation. For example, interventions aimed at reducing preoperative anxiety—such as pharmacological options like pregabalin and non-pharmacological methods like music therapy—have shown promising outcomes. These approaches not only lower anxiety levels but also contribute to improved postoperative results, highlighting the critical role of understanding individual experiences.
Moreover, expert insights emphasize the necessity of capturing subjective experiences in nursing. Özlem Ceyhan from the Department of Internal Medicine Nursing states, "Effective communication and psychological support can significantly enhance surgical outcomes," reinforcing the idea that subjective data is not merely supplementary but foundational to quality care.
To effectively capture individuals' subjective experiences, an example of SOAP charting nursing involves nurses focusing on open-ended questions that encourage patients to express their feelings and concerns. This practice not only enhances the records but also strengthens the therapeutic relationship, ultimately leading to improved outcomes for those receiving care.
Additionally, it is important to note that the research discussed was supported by open access funding organized by project DEAL, which adds context to the significance of these findings in nursing documentation.
Documenting the Objective: The Facts Matter
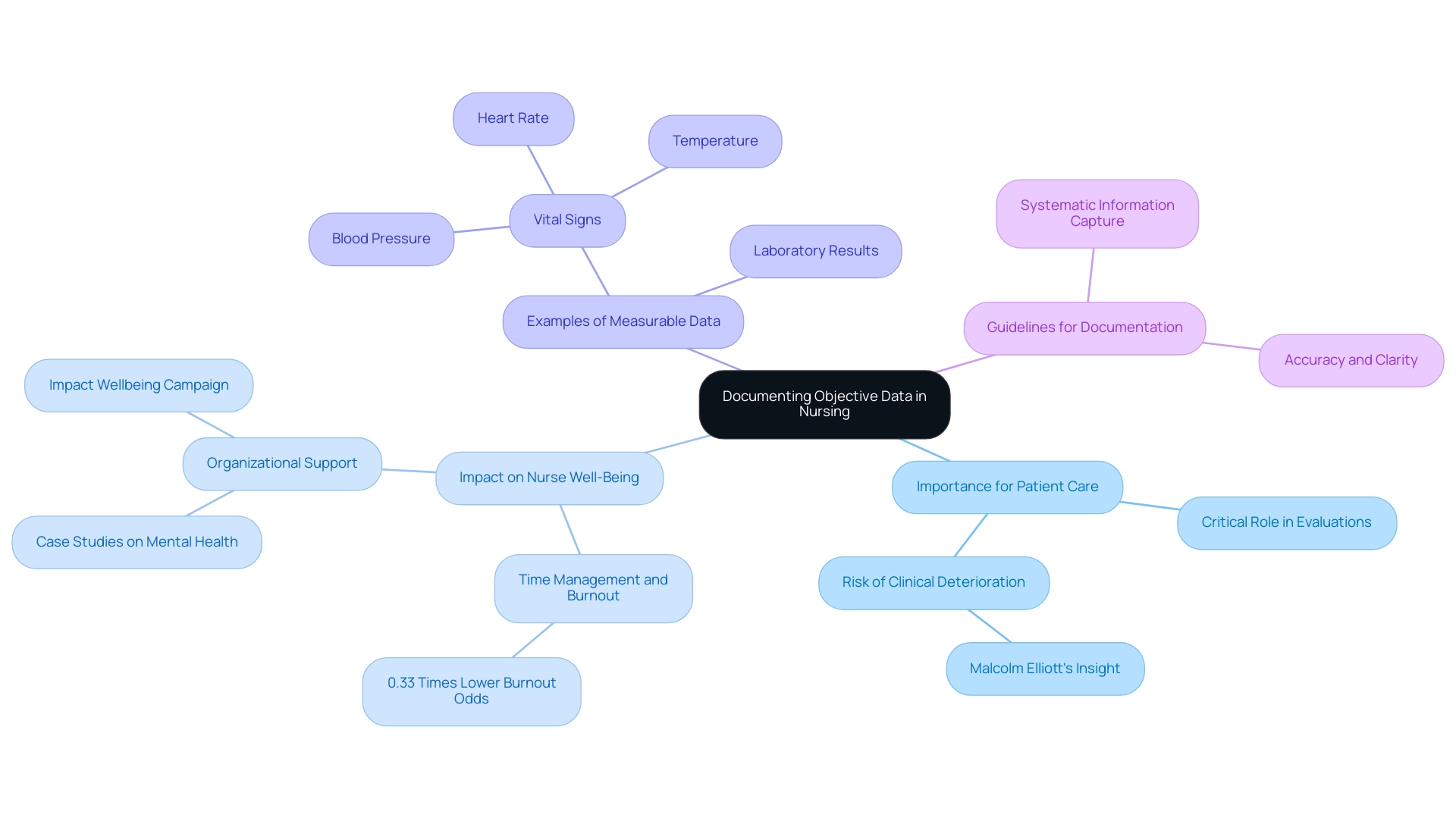
The objective part of a SOAP note serves as a vital example of soap charting nursing, playing a crucial role in capturing measurable data that informs evaluations. This encompasses vital signs, physical examination findings, and laboratory results. For instance, a nurse might document: Blood pressure 120/80, heart rate 72 bpm, and temperature 98.6°F. Such factual information is essential for evaluating an individual's condition and making informed treatment decisions.
Have you ever considered how the time constraints faced by healthcare workers can impact their well-being? Research indicates that those who feel they have sufficient time to complete their tasks are 0.33 times less likely to report burnout compared to their peers. This underscores the importance of comprehensive records in effectively managing workload and supporting mental health.
Incorporating objective data alongside subjective insights is a powerful example of soap charting nursing. This approach enables nurses to develop a holistic understanding of an individual's health status, which is vital for effective planning. Recent guidelines for documenting objective data in nursing highlight the necessity for accuracy and clarity, ensuring that all relevant information is captured systematically. For example, organizing vital signs not only aids in immediate clinical decision-making but also contributes to long-term health strategies for individuals.
Malcolm Elliott from Monash Nursing & Midwifery poignantly states, "Failure to assess these signs puts individuals at risk, as their clinical deterioration might not be detected or is recognized far too late for medical intervention to be effective." This emphasizes the critical role of objective information in nursing evaluations, enhancing individual support while also benefiting the well-being of healthcare providers. Case studies illustrate that organizations prioritizing objective data collection and management can significantly improve health worker mental health outcomes, especially during high-stress periods, as discussed in the report 'Organizational Interventions for Health Worker Mental Health.'
Furthermore, the National Institute for Occupational Safety and Health has initiated the 'Impact Wellbeing' campaign to assist employers in enhancing working conditions and supporting the mental health of health workers. This initiative adds relevance and timeliness to our discussion. By embracing these practices, nurses can ensure their documentation is not only effective but also aligned with the latest standards in healthcare. Let's work together to create a supportive environment that prioritizes both patient care and the well-being of healthcare providers.
Thoughtful Assessments: Bridging Data and Compassion
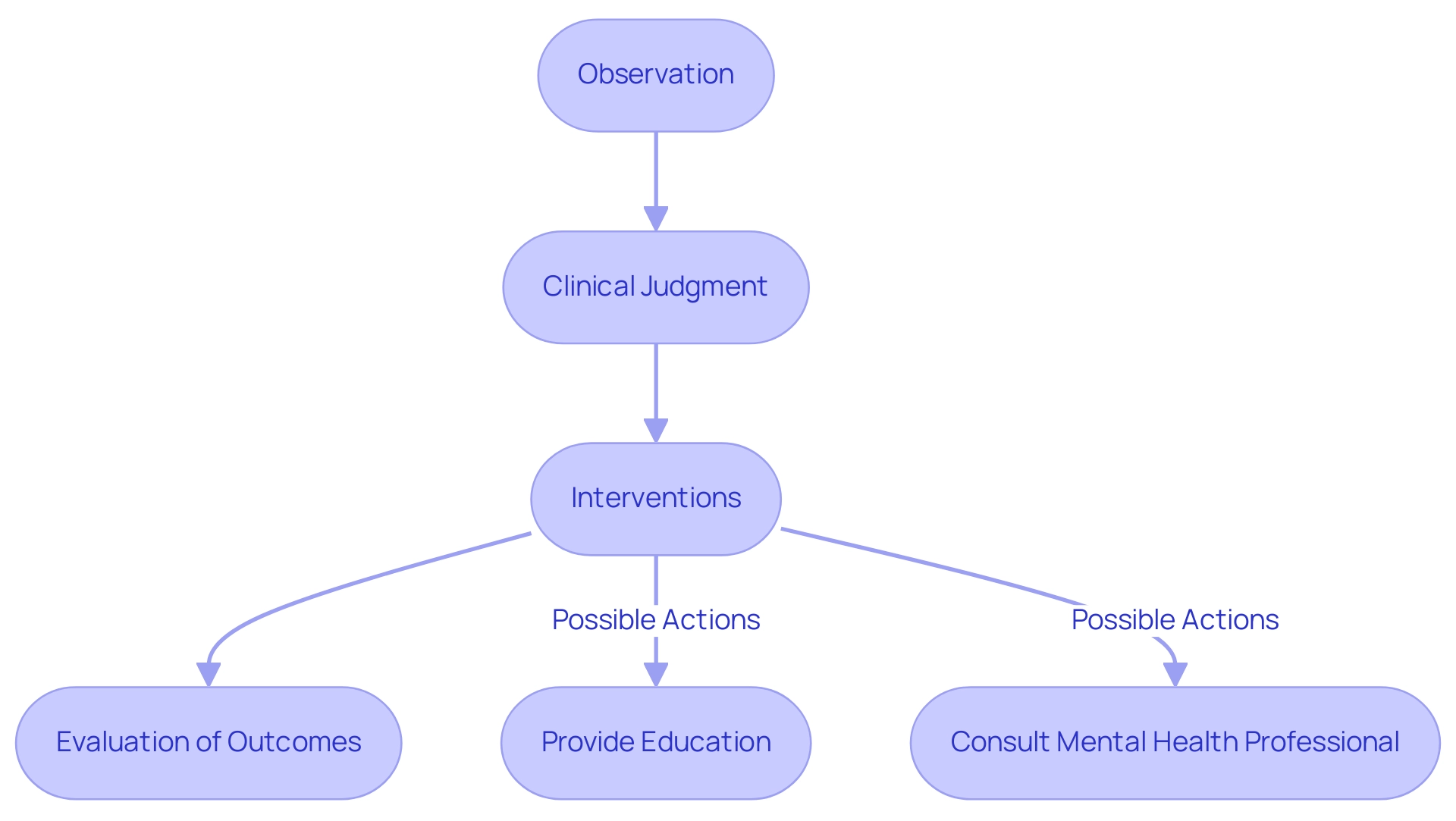
An example of SOAP charting in nursing illustrates how nurses play a crucial role in synthesizing subjective and objective data to form a comprehensive clinical judgment in the assessment section. For instance, after observing an individual's expressed anxiety alongside stable vital signs, a nurse might document, 'Individual exhibits signs of anxiety related to surgery, but vital signs are stable.' This thoughtful evaluation acknowledges the individual's emotional state and informs the development of tailored interventions.
Such interventions could include providing additional education about the procedure or involving a mental health professional to address the individual's concerns.
The significance of compassionate assessments in nursing practice is paramount, as demonstrated in the example of SOAP charting. Research indicates that effective assessments lead to improved outcomes, with a notable increase in the completion of nursing assessments from 28.01% in 2020 to 58.73% in 2021, as shown in the VALENF Project. This multifaceted approach not only enhanced the quantity of assessments but also improved their quality, with adequately completed evaluations rising from 63.4% to 71.8%.
These statistics highlight the vital importance that considerate evaluations have in nursing strategies, ensuring they reflect the individual's comprehensive needs. Furthermore, an example of SOAP charting underscores the importance of connecting information with empathy in nursing evaluations. By integrating subjective insights—such as an individual's emotional responses—with objective findings like vital signs, nurses can create care plans that genuinely resonate with the person's experience.
This synthesis is essential in promoting a caring healthcare atmosphere, ultimately resulting in improved clinical outcomes and greater satisfaction among individuals. As Sarfraz Masih observed, a notable difference was identified in nurses' usability scores before and after interventions, emphasizing the influence of effective assessment tools on nursing practice.
Moreover, evaluating functional capacity, the risk of pressure injuries, and the risk of falls in hospitalized individuals is crucial, as these are sensitive nursing outcomes that empathetic assessments aim to address. As the landscape of nursing continues to evolve in 2025, the focus on empathetic evaluations will remain a cornerstone of effective treatment. CosmaNeura's AI solutions can further enhance these assessments by providing clinical decision support that aligns with the compassionate approach in nursing, ensuring that plans are not only data-driven but also empathetic and patient-centered.
This integrated approach reflects the critical role of specialized understanding in healthcare, particularly in the context of evaluating healthcare startups and leveraging AI for improved patient-physician interactions.
Compassionate Planning: Tailoring Care to Individual Needs
The planning stage of soap charting nursing plays a crucial role in crafting a personalized treatment strategy that meets the unique needs of each individual. For example, when a patient expresses anxiety about an upcoming surgery, a thoughtful soap charting plan could incorporate pre-operative counseling sessions and relaxation techniques specifically designed to alleviate their concerns. This personalized approach not only fosters greater engagement from participants but also significantly enhances their satisfaction levels.
Research indicates that facilities that prioritize employee involvement see improved client satisfaction ratings. This underscores the importance of a considerate treatment strategy that addresses both the medical and emotional dimensions of care. Notably, statistics reveal that the AHA region 2 (New Jersey, New York, and Pennsylvania) experienced a year-over-year increase of 1.8 points in patient experience, illustrating the positive impact of compassionate planning. Furthermore, 42% of Americans are more likely to adhere to treatment plans when they receive support and guidance from their healthcare professionals, highlighting the critical role of customized treatment strategies in boosting adherence and satisfaction in 2025.
Moreover, the case study titled 'The Interconnection of Employee and Client Experience' demonstrates how high employee satisfaction is linked to improved service outcomes. This emphasizes the necessity for a holistic approach in nursing that addresses both psychological and physical health needs.
As we reflect on these insights, it becomes clear that a compassionate, tailored approach in healthcare not only benefits patients but also enhances the overall experience for everyone involved.
Real-World Examples: Compassionate SOAP Notes in Action
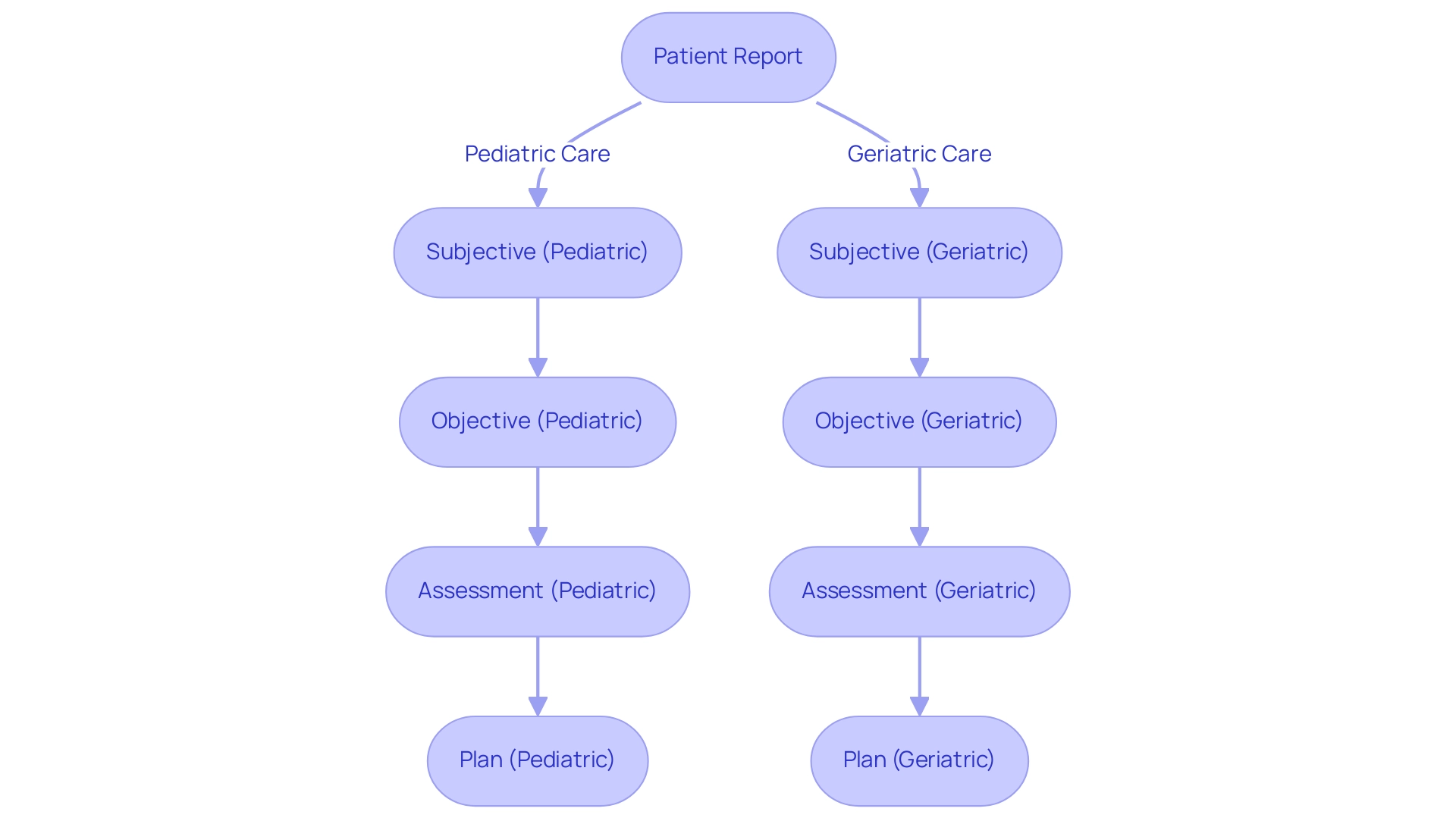
Compassionate SOAP notes are essential for delivering patient-centered care. They not only document clinical information but also address the emotional needs of patients. Consider these examples that illustrate how this documentation style can effectively meet the unique needs of individuals:
- Pediatric Care:
Subjective: A child reports pain at a level of 8/10, expressing distress.
Objective: Observations reveal the child grimacing and holding their abdomen tightly.
Assessment: The symptoms suggest severe abdominal pain, likely due to appendicitis.
Plan: Prepare the child for surgery while implementing comfort measures, such as providing a favorite toy or distraction techniques to alleviate anxiety. - Geriatric Care:
Subjective: An elderly patient expresses a fear of falling, indicating a sense of vulnerability.
Objective: The individual demonstrates an unsteady gait and requires assistance to move safely.
Assessment: This situation presents a high risk for falls, necessitating immediate attention.
Plan: Implement fall precautions, such as removing obstacles in the individual's environment, and schedule physical therapy to enhance strength and stability.
These examples highlight the importance of empathetic SOAP notes in directing effective interventions tailored to individual care requirements. In a landscape where the pandemic has exacerbated moral injury and exhaustion among healthcare providers, focusing on empathetic support is more vital than ever. A grounded theory investigation has identified essential supporters and obstacles to empathetic support, leading to the creation of a Nursing Assistance Model aimed at improving client outcomes.
Furthermore, real-world statistics reveal that patients in intensive care units endure considerable pain and suffering, underscoring the need for compassionate support. As noted by Saechao et al., "Patients in intensive care units endure significant pain and distress and they require empathetic assistance." This statement emphasizes the necessity for healthcare providers to prioritize empathy in their documentation practices.
Additionally, the case study titled 'Artful Nursing in Pakistan' illustrates how artful nursing, which emphasizes humane responsiveness and healing power, can be integrated into empathetic support practices. As nursing practices evolve, the incorporation of effective SOAP records remains crucial in ensuring that assistance is not only clinically sound but also compassionate and responsive to the emotional and physical needs of individuals. By prioritizing compassionate care in documentation, healthcare providers can foster a more humane and supportive environment for all individuals.
Avoiding Common Mistakes: Ensuring Compassionate Documentation
In the realm of SOAP charting nursing, it's important to recognize that common mistakes often arise from vague language, incomplete data, and a failure to capture the individual's voice. These challenges can be overwhelming, but by adopting best practices, nurses can alleviate some of the administrative burdens that impact patient care.
- Utilize Clear and Specific Language: Employing precise terminology that accurately reflects the patient's condition is crucial. This clarity not only aids in effective communication among healthcare providers but also enhances individuals' understanding of their medical records. It serves as a reminder of how technical jargon can create barriers to comprehension.
- Document Comprehensive Information: It's vital to ensure that all relevant details are captured, including the emotional and psychological aspects of the individual's experience. This thorough method of documentation greatly enhances the quality of treatment by offering a more complete view of the individual's needs and progress.
- Incorporate Perspectives of Individuals: Actively listening to individuals and integrating their concerns into the notes confirms their experiences. This practice nurtures a compassionate atmosphere, which is essential for effective support.
Additionally, utilizing tools like SPRY can significantly enhance the efficiency of charting and record-keeping. Therapists can complete SOAP notes in under 5 minutes, which helps reduce the administrative burden on healthcare providers.
A case study titled "Assessment Section Blunders" illustrates the importance of synthesizing information in the assessment section. By improving this section, therapists were able to produce more useful records that supported treatment planning, showcasing how careful charting positively affects client care.
Furthermore, a quote from Michael Reider highlights the effectiveness of clear records:
"Client's progress on the /ch/ production objectives improved from 50% accuracy in the last session to 80% accuracy using visual cues. Without visual cues, performance decreased significantly."
This underscores the importance of maintaining clear and specific records to monitor individual progress.
Statistics indicate that the average claim amount is $150.00, emphasizing the financial implications of thorough and accurate documentation. By navigating away from common pitfalls in SOAP charting nursing, nurses can enhance the quality of service while contributing to the overall efficiency and effectiveness of healthcare delivery.
Embracing Compassionate SOAP Charting: A Call to Action
Adopting empathetic SOAP charting is essential for enhancing treatment standards. By prioritizing the subjective experiences of individuals and accurately documenting objective data, nurses can synthesize this information into comprehensive assessments and plans. This approach enables the delivery of care that is both effective and compassionate. Have you ever considered how your documentation practices might influence patient expectations? Studies reveal a significant negative relationship between individuals' expectations and nurses' behaviors, highlighting the importance of empathetic record-keeping to bridge this gap (r=-0.900).
This method not only fosters a stronger bond with individuals but also improves overall outcomes for those receiving care. To implement caring documentation practices in 2025, healthcare providers should focus on training programs that emphasize empathy and communication skills. As noted by Hanan Elzeblawy Hassan, extensive in-service training can greatly enhance nurses' confidence and practices related to empathetic support. Furthermore, case studies, such as the one conducted at Shiraz University of Medical Sciences, demonstrate a statistically significant correlation between compassion competence and safety competency among psychiatric nurses.
This underscores the importance of integrating empathy into nursing education, as enhancing these skills can lead to improved safety outcomes for individuals. Effective execution of empathetic support in healthcare environments is evident in numerous instances where nurses actively engage with individuals, resulting in heightened satisfaction and safety. By adopting a model of SOAP charting, healthcare providers can improve their documentation while also contributing to a more fulfilling practice. This aligns with CosmaNeura's goal to revolutionize healthcare by automating administrative tasks, allowing providers to focus on empathetic care for individuals.
The benefits of this approach are manifold: increased job satisfaction for nurses and better health outcomes for patients, reinforcing the compassionate spirit central to Catholic healthcare values. Are you ready to embrace these practices and foster a more empathetic healthcare environment?
Conclusion
Effective SOAP charting serves as a cornerstone of compassionate healthcare, merging the systematic documentation of patient information with a profound understanding of their emotional and psychological needs. This structured approach not only enhances clarity and communication among healthcare teams but also cultivates a nurturing environment where patients feel genuinely heard and valued. By integrating subjective patient experiences with objective data, nurses can craft comprehensive assessments that inform personalized care plans, ultimately leading to improved patient outcomes.
The rise of technology, particularly AI solutions, further bolsters this compassionate framework by streamlining documentation processes and alleviating administrative burdens. This shift allows healthcare providers to dedicate more time to direct patient care, reinforcing the crucial role of empathy in clinical interactions. As the healthcare landscape continues to evolve, the emphasis on compassionate SOAP charting becomes increasingly vital, ensuring that quality care remains at the forefront of nursing practice.
In conclusion, embracing compassionate SOAP charting is not merely a best practice; it is a vital commitment to enhancing patient care and satisfaction. By prioritizing the holistic needs of patients and nurturing a culture of empathy, healthcare providers can significantly improve both individual experiences and overall health outcomes. The call to action is clear: integrate compassion into every facet of documentation, paving the way for a more humane and effective healthcare system.




