Overview
In the realm of medical practice, chart notes are more than just documents; they are essential lifelines that capture vital information about a patient's health, treatment plans, and progress. These notes form the cornerstone of effective communication among healthcare providers, addressing the emotional challenges that often arise in patient care.
Have you ever felt overwhelmed by the administrative burdens that can detract from your focus on patient well-being? This article highlights how structured chart notes can not only improve care continuity but also reduce errors and enhance patient outcomes.
As we delve deeper, we recognize that the integration of AI technologies is transforming documentation practices, streamlining processes, and alleviating some of the administrative pressures that healthcare providers face. Imagine a world where your time is freed up to focus more on your patients and less on paperwork. The advancements in documentation are paving the way for a more efficient healthcare environment, ultimately benefiting both providers and patients alike.
We invite you to reflect on how these changes can impact your practice. By embracing structured chart notes and the innovations that accompany them, you can contribute to a system that prioritizes patient care and fosters better communication.
Let's work together to navigate these challenges and enhance the quality of care we provide. Your commitment to continuous improvement can make a significant difference in the lives of those you serve.
Introduction
In the intricate world of healthcare, chart notes are essential to patient documentation, encapsulating vital information that guides treatment and fosters communication among providers. These comprehensive records reflect not only a patient's health status and treatment plans but also play a crucial role in ensuring continuity of care, especially in complex cases involving multiple specialists.
As we navigate the evolving landscape of healthcare, the integration of technology—particularly artificial intelligence—offers promising solutions. These advancements revolutionize how chart notes are created and managed, alleviating administrative burdens and enhancing the quality of patient interactions. Yet, challenges such as time constraints and documentation complexity remain, making effective charting practices more important than ever.
This article delves into the significance of chart notes, explores best practices for their creation, and examines the transformative impact of technology on documentation processes. It emphasizes the ethical considerations that must guide these practices, all in pursuit of exceptional patient care. Together, let us embrace these changes and strive for a healthcare environment where every patient feels valued and understood.
Defining Chart Notes: A Core Component of Medical Documentation
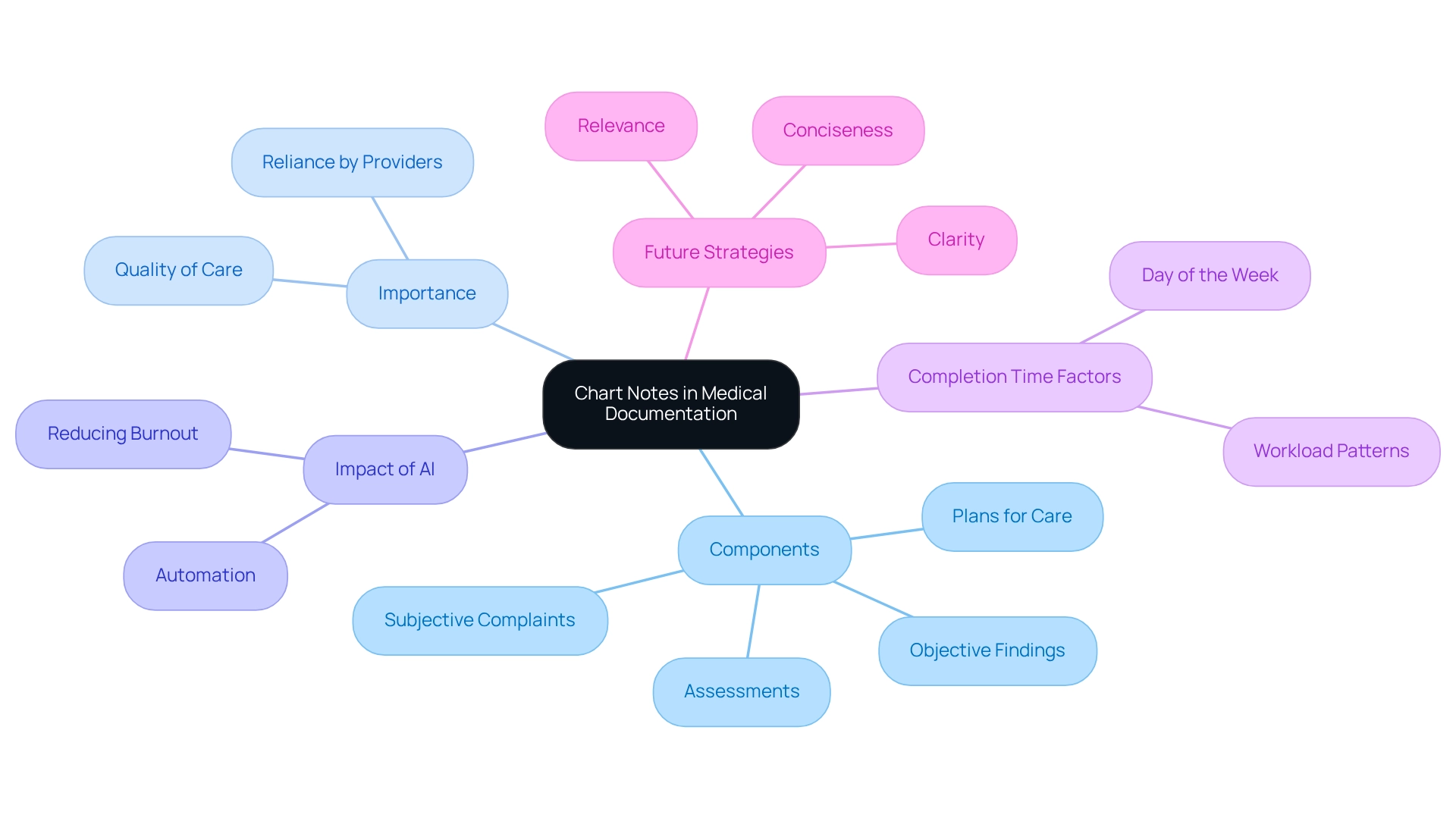
Chart records are not just documents; they are vital narratives created by medical professionals during or after client interactions, playing an essential role in medical documentation. These records encapsulate crucial details about an individual's health condition, treatment strategies, and progress over time. Typically, chart notes encompass various components, including subjective complaints from individuals, objective findings from examinations, assessments made by the provider, and plans for future care.
The importance of chart notes in medical practice is underscored by the fact that approximately 85% of medical providers rely on them as a fundamental aspect of care. Current statistics reveal that the average individual encounter demands 16 minutes and 14 seconds for electronic health record (EHR) documentation, illustrating the time-intensive nature of this process. As the medical landscape evolves, there is a noticeable shift toward intuitive, human-centered designs in medical charts that prioritize individual care over administrative burdens, reflecting ongoing advancements in medical documentation practices.
AI solutions from CosmaNeura are leading this transformation, streamlining administrative tasks such as charting and documentation. By automating repetitive processes, these AI-driven innovations alleviate the burden on healthcare professionals, enabling them to focus more on direct care for individuals. This not only enhances the quality of patient interactions but also addresses physician burnout, a pressing concern in the industry.
Have you ever considered how the day of the week impacts chart completion times? Recent studies reveal that encounters scheduled later in the week often result in compared to those earlier in the week, with charts finalized on weekends taking notably longer. This indicates that service behavior and workload patterns throughout the week affect documentation efficiency, highlighting the need for tailored training and tools to improve charting practices. The findings regarding the influence of the day of the week on chart completion further emphasize that documentation efficiency is closely linked to provider schedules.
Expert insights shed light on the significance of efficient chart records in medical documentation. Dr. Naheed Ali notes that while transitioning to an electronic health record system presents challenges, centralizing medical records digitally marks significant progress in medical services. This perspective aligns with the growing recognition of chart records as essential tools for enhancing care outcomes, particularly amid the difficulties faced during this transition.
Looking ahead to 2025, optimal strategies for chart records emphasize clarity, conciseness, and relevance, ensuring that documentation not only meets regulatory standards but also elevates the quality of care. These best practices are increasingly important as medical providers encounter variability in documentation completion, underscoring the necessity for provider-specific training and tools. Numerous instances exist where well-organized chart documentation has led to better outcomes for individuals, highlighting their crucial role in the service delivery process.
As the field continues to evolve, the significance of chart records in medical documentation remains paramount, serving as the foundation for effective care for individuals. Furthermore, CosmaNeura's AI solutions address the challenges of fragmented communication and administrative burdens, empowering care professionals to navigate the complexities of care more efficiently.
The Importance of Chart Notes in Patient Care and Communication
Chart notes are essential in healthcare, ensuring that every member of the team has access to accurate and up-to-date information about an individual's condition and treatment. This meticulous documentation promotes effective communication among healthcare professionals, which is crucial for continuity of care, especially in complex situations involving multiple specialists. Have you ever considered how communication breakdowns can affect patient outcomes? A study on sign-out communication in emergency medical services revealed that, although signouts occurred 99% of the time, only 8.6% included all essential components for optimal care.
This statistic underscores the significance of detailed chart notes, enabling a new provider to quickly grasp an individual's history and treatment strategy during transitions. This understanding is vital in reducing the risk of mistakes and improving outcomes for those receiving care. Furthermore, the World Health Organization defines safety for individuals in care as a framework aimed at reducing risks and avoidable harm, emphasizing the importance of accurate documentation in preventing adverse events and medical errors.
In fact, the UK health ombudsman reported that poor communication contributes to approximately 48,000 avoidable sepsis deaths annually. This statistic illustrates the dire consequences of notes. As Jeremy Howick poignantly asked, 'How does communication influence safety for individuals receiving care?' This question highlights the essential role that effective communication plays in ensuring safety and quality care.
Thoroughly recorded chart entries also serve as legal documents, protecting both individuals receiving care and practitioners in case of disagreements related to treatment. By utilizing templates for handovers, medical professionals can ensure that all essential information is included. For instance, templates can be prepared using text messaging platforms to facilitate the inclusion of all necessary information, thereby improving communication and continuity of care.
Ultimately, the function of chart records transcends simple documentation; they are a fundamental aspect of efficient care and communication among healthcare professionals. Let us work together to enhance our charting practices, ensuring that every detail counts in providing the best possible care.
Key Elements of Chart Notes: Structure and Content Requirements
are essential for quality patient care, serving as a cornerstone for understanding and supporting individuals' needs. They typically encompass several key elements that ensure compassionate care:
- Individual Identification: Fundamental details such as the individual's name, date of birth, and medical record number are crucial for accurate tracking and management of information.
- Date and Time: Recording when the note was created is vital for tracking the individual's progress over time, enabling a clearer understanding of their healthcare journey.
- Subjective Information: This section captures individual-reported symptoms and concerns, often articulated in the individual's own words. It provides valuable insights into the patient's experience and perspective, which are critical for effective diagnosis and treatment.
- Objective Findings: Clinical observations made by the professional are recorded here, including vital signs, results from physical examinations, and outcomes of diagnostic tests. This objective data forms the foundation for informed clinical decision-making.
- Assessment: This element reflects the provider's interpretation of both subjective and objective data, leading to a diagnosis or clinical impression. It combines collected information to guide the next steps in care.
- Plan: A comprehensive outline of the subsequent steps in the individual's care is detailed here, including proposed treatments, referrals to specialists, and follow-up appointments. This organized method not only guarantees that all pertinent information is recorded but also enhances communication among medical professionals.
The SOAP note method exemplifies this structured approach by organizing individual information into four categories: Subjective, Objective, Assessment, and Plan. This method facilitates better communication and improves clinical reasoning among healthcare providers. However, adaptations like the SOAPE model have emerged to address limitations, such as the need for ongoing updates to individual information.
Statistics suggest that the percent agreement for therapeutic needs in chart notes can vary from 68.3% to 100%, underscoring the inconsistency in reliability across different documentation practices. This variability highlights the significance of adhering to current guidelines for chart notes medical structure and content requirements, which are essential for upholding high standards in medical documentation and ultimately resulting in enhanced outcomes for individuals.
As medical documentation has evolved into electronic formats, healthcare providers face challenges such as data overload if not managed properly. Structured chart reviews, as noted by Murray M Pollack, MD, emphasize that "structured chart reviews with clear objectives by knowledgeable primary reviewers followed by a brief secondary review by an appropriate expert can be valid and reliable and applied to research, quality assessments, and process improvement activities." This underscores the necessity for effective documentation practices that enhance care for individuals.
Moreover, the integration of AI-driven predictive analytics from CosmaNeura can significantly improve outcomes by analyzing data to identify individuals at higher risk of developing certain conditions. By offering early alerts and facilitating preventive actions, AI not only simplifies administrative tasks but also aids providers in making informed choices that lead to improved management of individuals and reduced expenses related to advanced treatments. However, it is important to consider potential challenges in implementing AI solutions, such as data privacy concerns and the need for proper training for healthcare staff to effectively utilize these technologies.
Types of Chart Notes: Understanding Different Documentation Practices
In medical practice, various types of chart notes play a vital role in patient care and documentation, each serving a unique purpose:
- Progress Records: These records are crucial for capturing ongoing care and updates regarding an individual’s condition. Typically following a standardized format like SOAP (Subjective, Objective, Assessment, Plan), they promote clear communication among healthcare professionals. The integration of AI-driven tools from CosmaNeura can streamline this process, ensuring updates are efficiently recorded and easily accessible.
- Initial Evaluation Records: Compiled during the first interaction with an individual, these records provide a comprehensive summary of the individual’s medical history, presenting issues, and preliminary treatment strategies. They serve as a foundational document guiding subsequent care. With AI innovations from CosmaNeura, the analysis of initial assessments can be enhanced, allowing for quicker identification of critical health issues and tailored treatment plans.
- Consultation Records: When a specialist assesses an individual referred by another practitioner, consultation records are generated. These encapsulate the expert’s conclusions and suggestions, ensuring that all practitioners involved in the individual’s care are coordinated on the treatment strategy. AI can assist in synthesizing these notes, making it easier for professionals to access relevant information and collaborate effectively.
- Discharge Summaries: Compiled at the time of an individual’s discharge from a medical facility, discharge summaries outline the treatment received during their stay, , and any necessary referrals. This documentation is essential for ensuring continuity of care as the individual transitions back to their primary healthcare provider. AI-driven solutions from CosmaNeura can automate the creation of these summaries, reducing the administrative burden on medical professionals and allowing them to focus more on patient interactions.
Each type of chart note in medicine is critical for ensuring clear communication and continuity of care across various settings. Statistics indicate that approximately 62.5% of healthcare professionals have prior experience with chart notes, underscoring the importance of effective documentation practices. As Dr. Steven Stack, president of the American Medical Association, noted, "There are individuals who feel that their health care providers aren’t able to pay full attention to them because the doctor is absorbed by this technology."
This highlights the challenges of maintaining focus on individuals amidst documentation demands.
Moreover, the medical sector is recognizing that technology should enhance usability rather than complicate it. The case study titled 'Smarter Tech for Clinicians' illustrates this shift, envisioning a future where medical charts are more human-centered, fostering enhanced interaction and improved management of care. Additionally, the organized chart review approach is designed to be applicable and can be utilized in various research and quality enhancement efforts in healthcare, further emphasizing the significance of chart notes in broader healthcare scenarios.
By embracing AI-driven innovations from CosmaNeura, the documentation process can be transformed, ultimately enhancing care and efficiency for healthcare professionals. How might these advancements change your experience in patient care?
Challenges in Chart Note Documentation: Navigating Administrative Burdens
Healthcare professionals encounter significant obstacles in chart documentation, largely stemming from administrative burdens that can hinder both efficiency and accuracy. These challenges are not just procedural; they deeply affect the emotional well-being of providers and the quality of care patients receive.
Time constraints are a major concern. Providers often find it difficult to complete chart notes promptly due to overwhelming patient volumes. A staggering 22.1% of individuals with public insurance report experiencing notable administrative burdens, exacerbating these time pressures. This reality is echoed by Albert J Heuer, who highlights the serious consequences of such burdens on healthcare delivery.
The complexity of documentation requirements adds another layer of difficulty. The myriad regulations governing documentation can feel daunting, leading to inconsistencies and errors in medical chart notes. This administrative complexity indirectly impacts patient access to care, creating a ripple effect that can compromise overall service delivery.
Technological barriers also pose significant challenges. Many healthcare professionals struggle with electronic health record (EHR) systems that are often cumbersome and unintuitive. These obstacles complicate the documentation process, making it harder for professionals to maintain precise and effective records.
Moreover, the relentless pressure to produce accurate and timely chart notes significantly contributes to provider burnout. This not only affects their well-being but also undermines the quality of care provided to individuals. Research indicates that administrative burdens are a prevalent issue, with serious implications for .
Insights from the case study titled "Engagement and Administrative Burden" shed light on the relationship between engagement and the administrative challenges individuals face. This underscores the need for better measurement and understanding of these tasks. Addressing these challenges requires a united effort to simplify documentation processes, enhance EHR usability, and provide adequate support for medical professionals.
By enhancing our understanding of administrative tasks, we can improve the quality and value of medical services. This, in turn, benefits both practitioners and patients. Together, let’s advocate for a system that alleviates these burdens and fosters a healthier work environment for our dedicated healthcare providers.
Key Solutions to Consider:
- Simplifying documentation processes.
- Improving EHR usability.
- Offering sufficient support for healthcare professionals.
Let’s engage in a conversation about how we can tackle these challenges together.
Leveraging Technology: Enhancing Chart Note Documentation with AI
The incorporation of technology, especially artificial intelligence (AI), is fundamentally transforming medical chart notes documentation in the medical field. CosmaNeura's AI-powered tools offer numerous benefits for healthcare specialists:
- Automated Transcription: CosmaNeura's AI can transcribe client encounters in real-time, drastically reducing the time clinicians spend on manual note-taking. This efficiency enables caregivers to devote more time to interaction and care, ultimately improving outcomes for those receiving treatment.
- Smart Templates: AI-driven templates from in organizing their documentation efficiently, ensuring that all essential elements are included. This reduces the risk of omissions and enhances the overall quality of documentation, which is crucial for maintaining high standards of patient care.
- Data Analysis: Advanced algorithms can analyze historical chart notes to identify patterns and suggest pertinent information for current documentation. This capability not only improves accuracy but also simplifies the documentation process, making it more efficient and decreasing the administrative burden on medical providers.
- Interoperability: CosmaNeura's AI enables smooth data exchange between different electronic health record (EHR) systems, enhancing communication among medical providers. This guarantees that all pertinent individual information is easily accessible, promoting a more unified approach to individual care.
The influence of AI on chart documentation is highlighted by recent statistics showing that AI can improve diagnostic precision considerably. For example, a study with 80,000 women showed that AI-assisted diagnostics could identify 20% more cases of breast cancer without raising false positives, while simultaneously decreasing professionals' workloads by 44%. This demonstrates how AI not only enhances outcomes for individuals but also reduces the administrative load on professionals, tackling the problem of physician burnout.
Furthermore, AI digital consults enable clinicians to assess the effectiveness and safety of interventions in a virtual setting prior to real-world implementation, further highlighting AI's transformative role in medical documentation.
Nevertheless, it's crucial to recognize that there is a rising distrust in AI among certain demographics, with 30% of millennials and 32% of baby boomers expressing skepticism towards AI-generated information in 2024. This underscores the necessity for medical professionals to tackle these issues as they incorporate AI into their routines, especially in overcoming opposition to innovation.
As the medical field continues to progress, the advantages of utilizing technology for chart notes become more apparent. By utilizing CosmaNeura's AI solutions, medical providers can simplify their documentation processes, ultimately enabling them to concentrate more on providing outstanding care. According to the Keragon Team, in December 2023, only 25% of medical executives had implemented generative AI solutions, indicating that while the potential is recognized, adoption is still in its early stages.
Ethical Considerations in Chart Notes: Ensuring Compliance and Confidentiality
Ethical considerations in chart notes medical documentation are vital for fostering trust and ensuring compliance with legal standards. These principles are not just rules; they resonate deeply with the emotional challenges faced by healthcare providers and patients alike.
- Confidentiality: Protecting client information is a fundamental responsibility of healthcare providers. Chart records should be accessible only to authorized staff, which is essential for safeguarding individual confidentiality and complying with laws like HIPAA. Did you know that breaches of (EMR) accounted for 195 incidents, representing 5.99% of total breaches? This statistic underscores the importance of robust confidentiality measures to prevent unauthorized access to sensitive information.
- Precision: Providers carry a moral obligation to ensure that chart records accurately reflect the individual's condition and treatment. Flawed documentation can lead to misdiagnoses and inappropriate treatment plans, potentially jeopardizing safety and care quality. The ongoing challenges related to the loss and theft of protected health information (PHI), especially unencrypted electronic devices, highlight the necessity for meticulous documentation practices. Although protections have improved, incidents of theft and loss still occur frequently, stressing the importance of comprehensive security measures.
- Informed Consent: Patients deserve to know how their information will be used and have the right to access their medical chart notes. This transparency not only builds trust but also empowers individuals in their healthcare journey, reinforcing their role in decision-making processes concerning their health.
- Compliance with Regulations: Adhering to legal and regulatory requirements for documentation is crucial for protecting both patients and professionals. Non-compliance can lead to legal consequences, treatment delays, and damage the reputation of healthcare professionals. Covered entities and business associates have distinct HIPAA compliance obligations based on their activities, emphasizing the need for a thorough understanding and adherence to these regulations.
By prioritizing these ethical considerations, medical providers can enhance the quality of care reflected in their chart notes and maintain the integrity of the patient-provider relationship. Implementing comprehensive security measures, including encryption and secure handling of both electronic and paper records, is essential to prevent unauthorized access to sensitive information. This commitment to ethical documentation practices not only safeguards patient confidentiality but also strengthens the overall healthcare system.
As R.A.K. noted, "A.A. and R.A.K. supervised the study," highlighting the collaborative effort in addressing these critical issues.
Conclusion
Chart notes are the backbone of effective patient care, serving as vital records that encapsulate a patient's health status, treatment plans, and progress. In complex cases involving multiple specialists, clear communication is essential for continuity of care. However, the administrative burdens associated with charting can weigh heavily on healthcare providers, detracting from the time they can spend with patients. Fortunately, the integration of AI technology, particularly solutions from CosmaNeura, offers a promising avenue to alleviate these pressures, allowing providers to focus more on meaningful patient interactions.
Best practices for creating chart notes emphasize clarity, conciseness, and relevance. These practices not only meet regulatory standards but also enhance patient care outcomes. By leveraging structured approaches like the SOAP method and incorporating AI-driven tools, healthcare providers can improve the efficiency and accuracy of their documentation. Yet, challenges such as time constraints, complexity of requirements, and provider burnout persist. This highlights the ongoing need for innovation and support in documentation practices.
Ethical considerations surrounding confidentiality, accuracy, informed consent, and regulatory compliance are paramount in maintaining patient trust and safeguarding sensitive information. As the healthcare landscape continues to evolve, embracing technological advancements while adhering to ethical standards is crucial for fostering an environment where every patient feels valued and understood. Ultimately, a commitment to effective charting practices and the integration of AI technology will lead to improved patient outcomes, demonstrating the indispensable role of chart notes in modern healthcare. How can we continue to support each other in this journey toward better care?




