Overview
The article highlights the emotional challenges healthcare providers face in their daily practice. It emphasizes how administrative burdens can weigh heavily on their ability to deliver compassionate care. By enhancing clinical documentation through SOAP narrative examples, we can ease these burdens and improve systematic patient record-keeping. Each component of the SOAP framework—Subjective, Objective, Assessment, and Plan—plays a vital role in fostering clear communication among healthcare providers. This clarity is essential for better patient outcomes.
Imagine the difference it could make if every healthcare provider felt supported in their documentation efforts. By streamlining these processes, we can alleviate stress and enhance collaboration within teams. This not only benefits the providers but also leads to improved experiences for patients, who deserve the best care possible.
Let’s consider the benefits of implementing SOAP narratives:
- They encourage thoroughness
- Improve information sharing
- Ultimately enhance patient safety
If we commit to these practices, we can transform our healthcare environment into one that prioritizes understanding and compassion.
I encourage you to reflect on your own experiences with clinical documentation. How might adopting SOAP narratives change your approach to patient care? Together, we can create a supportive atmosphere that values both providers and patients, ensuring that everyone receives the attention and care they need.
Introduction
In the realm of healthcare, effective documentation is crucial for delivering quality patient care. Have you ever felt overwhelmed by the demands of administrative tasks? Among the various methods available, SOAP notes emerge as a structured approach that allows healthcare providers to systematically capture comprehensive patient encounters. By breaking down information into four key components—Subjective, Objective, Assessment, and Plan—this method not only enhances communication among providers but also fosters better clinical decision-making.
As the healthcare landscape evolves, understanding the intricacies of SOAP notes becomes increasingly vital. This understanding ensures that patient care is both informed and compassionate. Imagine how streamlined documentation can alleviate some of the burdens you face, allowing you to focus more on what truly matters: your patients. This article delves into the significance of SOAP notes, exploring how they can transform clinical documentation and ultimately improve patient outcomes. Together, let’s embrace this powerful tool to enhance our practice and support the care we provide.
Understanding SOAP Notes: A Brief Overview
SOAP notes represent a vital recording method that healthcare professionals use to document client encounters systematically. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, each component playing a distinct and critical role in clinical documentation.
- Subjective: This section captures the individual's personal experiences, feelings, and concerns, offering insight into their perspective on their health condition. Understanding these narratives is crucial for tailoring support to meet their unique needs.
- Objective: In this section, measurable data is documented, including vital signs, physical examination findings, and laboratory results. This objective information lays the groundwork for informed clinical decisions.
- Assessment: Here, the clinician analyzes both subjective and objective data, leading to a diagnosis or clinical impression. This synthesis of information guides the next steps in patient care.
- Plan: The final section outlines the proposed next steps in treatment, such as further tests, therapies, referrals, or follow-up appointments. A well-organized strategy is essential for ensuring continuity of care and alignment among all medical team members.
The effective use of SOAP narrative examples is linked to improved patient outcomes. A study titled 'Impact of SOAP Notes on Medical Records' emphasized that using SOAP narrative examples significantly enhances medical record-keeping, fostering effective communication among providers. This standardized format promotes accuracy and ensures that critical information is easily accessible, which is essential for delivering high-quality care.
Recent statistics indicate that service providers utilizing SOAP narrative examples report notable improvements in record quality, with many observing enhanced outcomes for individuals and better clinical decision-making. The aim of rehabilitation is to assist patients in achieving a level of independence that facilitates discharge from care, underscoring the importance of accurate records in supporting this goal.
As medical services continue to evolve, the importance of precise and thorough records, such as SOAP narrative examples, cannot be overstated, particularly in primary treatment settings where effective communication is crucial. In 2025, the emphasis on SOAP notes in clinical practice remains strong, with ongoing trends focusing on integrating technology to simplify record-keeping processes. By adhering to SOAP narrative examples in their application, healthcare providers can enhance record quality and foster a more collaborative and informed approach to care.
As noted by AWD, "Ethics approval was obtained from the Institutional Review Committee of the health science college of Mettu University with reference number ARcsu/271/24," highlighting the ethical considerations that support effective documentation practices.
Example 1: Subjective Insights from a Patient Encounter
In a recent interaction, a 45-year-old female expressed, 'I've been feeling anxious and overwhelmed since my mother passed away last month.' This poignant statement not only reflects her emotional turmoil but also provides critical context for her current health challenges. Recording such personal insights is crucial for a thorough comprehension of her overall well-being and for customizing effective interventions.
Emotional health significantly influences outcomes, with anxiety disorders impacting a substantial segment of the population. The World Health Organization has developed brief psychological intervention manuals that effectively address multiple mental health issues, including anxiety and depression. Furthermore, studies indicate a strong connection between the occurrence of anxiety disorders and economic factors, such as GDP per capita and urbanization. This implies that socioeconomic circumstances can exacerbate mental health issues.
Incorporating subjective information into SOAP narrative examples allows healthcare providers to capture the nuances of an individual's emotional state. This practice is essential for developing a comprehensive treatment plan. For instance, when recording individual emotions, providers can use specific phrases that mirror the person's feelings, such as 'expressed feelings of sadness and anxiety related to recent bereavement.' This method not only enhances the clinical story but also aligns with optimal practices in mental health records.
Case studies demonstrate that efficient recording of emotional states can lead to better treatment outcomes. For example, one study revealed that individuals who received care recognizing their emotional experiences reported greater satisfaction and improved health results. Additionally, mindfulness meditation has proven beneficial for managing anxiety, even with just a few minutes of practice daily.
By prioritizing the recording of subjective insights, healthcare providers can deepen their understanding of individual experiences and foster a more compassionate approach to care.
As highlighted by Alia Al Ahbabi, the importance of capturing emotional health in clinical records cannot be overstated. Future studies might also focus on creating precise cross-cultural measures for evaluating anxiety, underscoring the ongoing need for enhanced comprehension and recording of emotional well-being among diverse groups.
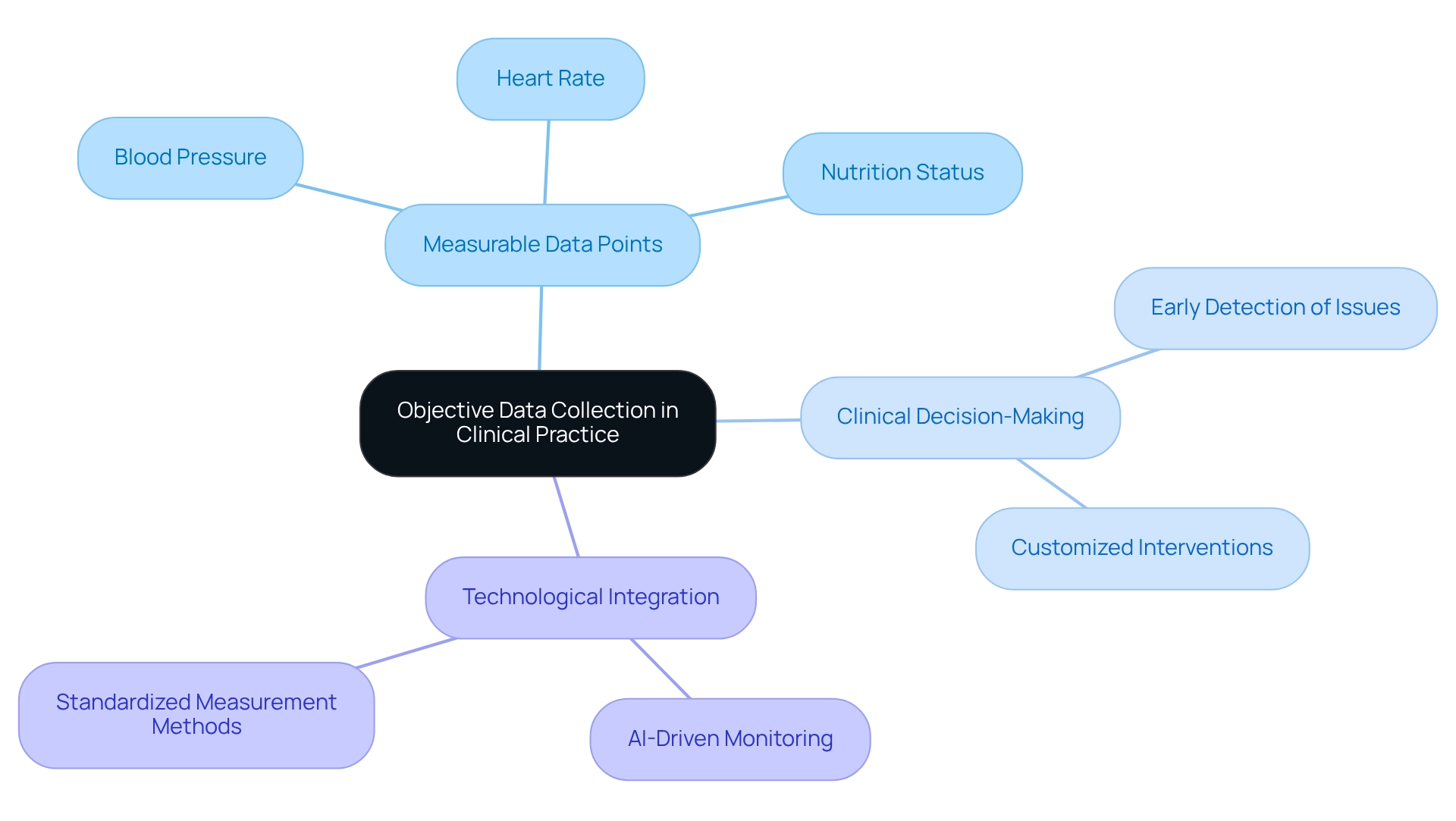
Example 2: Objective Data Collection in Clinical Practice
During the visit, the clinician documented crucial objective findings: 'Patient's blood pressure is 130/85 mmHg, heart rate is 78 bpm, and she appears well-nourished and in no acute distress.' These measurable data points are vital for evaluating the individual's physical health and guiding clinical decision-making. Objective measurements, such as blood pressure and heart rate, provide a foundation for precise evaluations. This allows healthcare providers to recognize potential health issues early and customize interventions accordingly.
Statistics indicate that only around 20.7% of adults with hypertension succeed in keeping their blood pressure below the advised limit of 130/80 mmHg. This highlights the significance of careful monitoring and record-keeping in clinical practice. Moreover, specialist viewpoints consistently emphasize that objective data is essential in assessments, as it improves diagnostic precision and treatment effectiveness. For example, the hazard ratio for a 10 bpm higher resting heart rate in Black women is 1.02, underscoring the importance of heart rate in clinical evaluations.
To efficiently gather objective data in clinical environments, practitioners should follow the most recent guidelines, which stress standardized measurement methods and comprehensive record-keeping practices. Incorporating vital sign records in SOAP narrative examples not only simplifies health records but also ensures that essential health indicators are readily available for continuous care. The integration of AI-driven remote health monitoring technologies, such as those developed by CosmaNeura, can further enhance this process. These technologies allow medical professionals to monitor individuals' vital signs in real-time, enabling timely interventions when needed.
The case study titled 'Trends in Hypertension Characteristics' shows a stagnation in hypertension management, emphasizing the need for renewed efforts in tracking and documentation. By prioritizing objective measurements and leveraging AI innovations, clinicians can significantly enhance outcomes and foster a more effective healthcare environment. This aligns with CosmaNeura's mission to improve healthcare delivery through innovative solutions, ultimately supporting healthcare providers in their vital roles.
Example 3: Assessment Techniques in SOAP Documentation
In the assessment section, the clinician noted: 'The individual exhibits signs of generalized anxiety disorder, likely exacerbated by recent bereavement.' This observation highlights the emotional challenges faced by many individuals. It is recommended to consider cognitive behavioral therapy (CBT) and possibly refer to a mental health specialist. Such a statement effectively synthesizes both subjective observations and objective findings, guiding thoughtful clinical decisions.
The integration of CBT, which has demonstrated a response rate of 77% for panic disorder without agoraphobia, underscores the importance of evidence-based practices in treatment planning. Mental health professionals emphasize that accurate diagnosis and timely intervention are crucial for effectively managing anxiety disorders. For instance, a study on CBT for anxiety in the elderly revealed mixed outcomes. Some studies showed significant decreases in anxiety symptoms, while others indicated no enhancement over relaxation training alone. This variability emphasizes the need for customized strategies tailored to individual requirements and situations.
SOAP narrative examples highlight that evaluation methods are crucial in healthcare decisions. Clinicians are encouraged to utilize structured assessments that encompass both clinical observations and patient-reported symptoms. Present referral rates to mental health professionals in primary health settings suggest an increasing acknowledgment of the necessity for collaborative models, which can improve outcomes for individuals.
Furthermore, the incorporation of AI algorithms, like those created by CosmaNeura, can examine individual data to recognize patterns, genetic markers, and biomarkers linked to particular treatment responses. This allows providers to customize treatments more efficiently. Such methods not only enhance the quality of service but also align with the ethical principles maintained in faith-based medical practices. This ensures that individual well-being remains at the forefront of clinical decision-making. CostaNera, being the sole company developing AI solutions for the faith-based healthcare sector, strengthens these ethical principles, assisting providers in offering compassionate and responsible support.
Example 4: Crafting Effective Treatment Plans in SOAP Format
The treatment plan for the individual was thoughtfully designed to provide comprehensive care that addresses her unique needs. It encompasses several key components:
- Initiate Cognitive Behavioral Therapy (CBT) sessions once a week for the next six weeks.
- Schedule a follow-up appointment in one month to assess progress and make necessary adjustments.
- Encourage participation in support groups for grief management, fostering a nurturing community environment.
This organized approach is crucial, as research indicates that structured treatment plans significantly enhance adherence to follow-up appointments, with compliance rates improving by up to 30% when clear plans are established. Furthermore, the effectiveness of these strategies in improving outcomes for individuals is well-documented; studies show that those with structured plans experience better health results and higher satisfaction levels.
It's important to note that thirty-six percent of studies included in recent reviews were classified as low-quality, highlighting the need for robust treatment plans in clinical practice. A significant case study, 'The Evolution of Clinical Data Use in Healthcare,' illustrates the transformative impact of organized record-keeping. It emphasizes how the shift from paper-based records to electronic health records (EHRs) has improved data accessibility and care coordination among providers. This evolution underscores the importance of effective treatment planning in medical documentation, as it not only streamlines processes but also enhances safety and outcomes for individuals.
The case study demonstrates that organized treatment plans lead to improved clinical decision-making and client engagement. Medical providers, incorporating expert insights, stress the necessity of structured treatment plans for delivering high-quality service. One provider shared, 'Having a clear, structured plan enables us to focus on what truly matters—our clients' well-being.'
Additionally, a study published in the Journal of Clinical Oncology Clinical Cancer Informatics reveals how a tool called TransPRECISE can 'guide pathway-based personalized medical decision making,' further reinforcing the significance of structured approaches in treatment planning. CosmoNauts, the sole company developing AI solutions for the faith-oriented healthcare sector, enhances this organized method by providing tools that elevate service quality while adhering to Catholic teachings. Through AI-driven innovations, CosmaNeura is revolutionizing care with tailored treatments and improved outcomes, illustrating how meticulous documentation can foster enhanced clinical decision-making and engagement.
Example 5: Comprehensive SOAP Note for a Complex Case
Consider an individual facing multiple health challenges. This situation can be overwhelming, and the SOAP note might reflect their experience as follows:
- Subjective: The individual shares feelings of increased fatigue and difficulty concentrating, attributing these struggles to their ongoing health challenges.
- Objective: While vital signs remain stable, lab results reveal mild anemia, which could be influencing their symptoms.
- Assessment: The fatigue and cognitive difficulties likely stem from chronic illness and nutritional deficiencies—common issues for those with complex health profiles. It's concerning that research shows at least 54% of American children have a diagnosed chronic condition, illustrating the widespread nature of these multifaceted health issues. In Ohio, the statistics are particularly alarming, ranking 39th for cancer deaths, 42nd for cardiovascular deaths, and 40th for diabetes deaths among U.S. states. This underscores the urgent need for effective management of chronic conditions within this population.
The incorporation of AI-driven predictive analytics from CosmaNeura can significantly enhance this process. By identifying individuals at greater risk of developing specific conditions, we can enable early interventions that improve outcomes and reduce medical expenses. Additionally, addressing challenges like physician burnout and fragmented care is crucial for improving the overall healthcare experience.
- Plan: It is recommended to refer the individual to a nutritionist for dietary counseling to address potential nutritional deficiencies. A follow-up appointment in two weeks is suggested to monitor progress. This comprehensive SOAP narrative effectively captures the complexity of the individual's condition while outlining a clear path forward.
The importance of thorough record-keeping in addressing complex health challenges cannot be overstated. It not only supports clinical decision-making but also enhances communication among medical professionals. By incorporating insights from healthcare providers and leveraging AI innovations from CostaNera, we can better navigate the intricacies of chronic disease management. Ultimately, this approach aims to improve patient outcomes and enhance quality of life.
How can we further support individuals facing similar challenges? Together, we can create a more compassionate and effective healthcare environment.
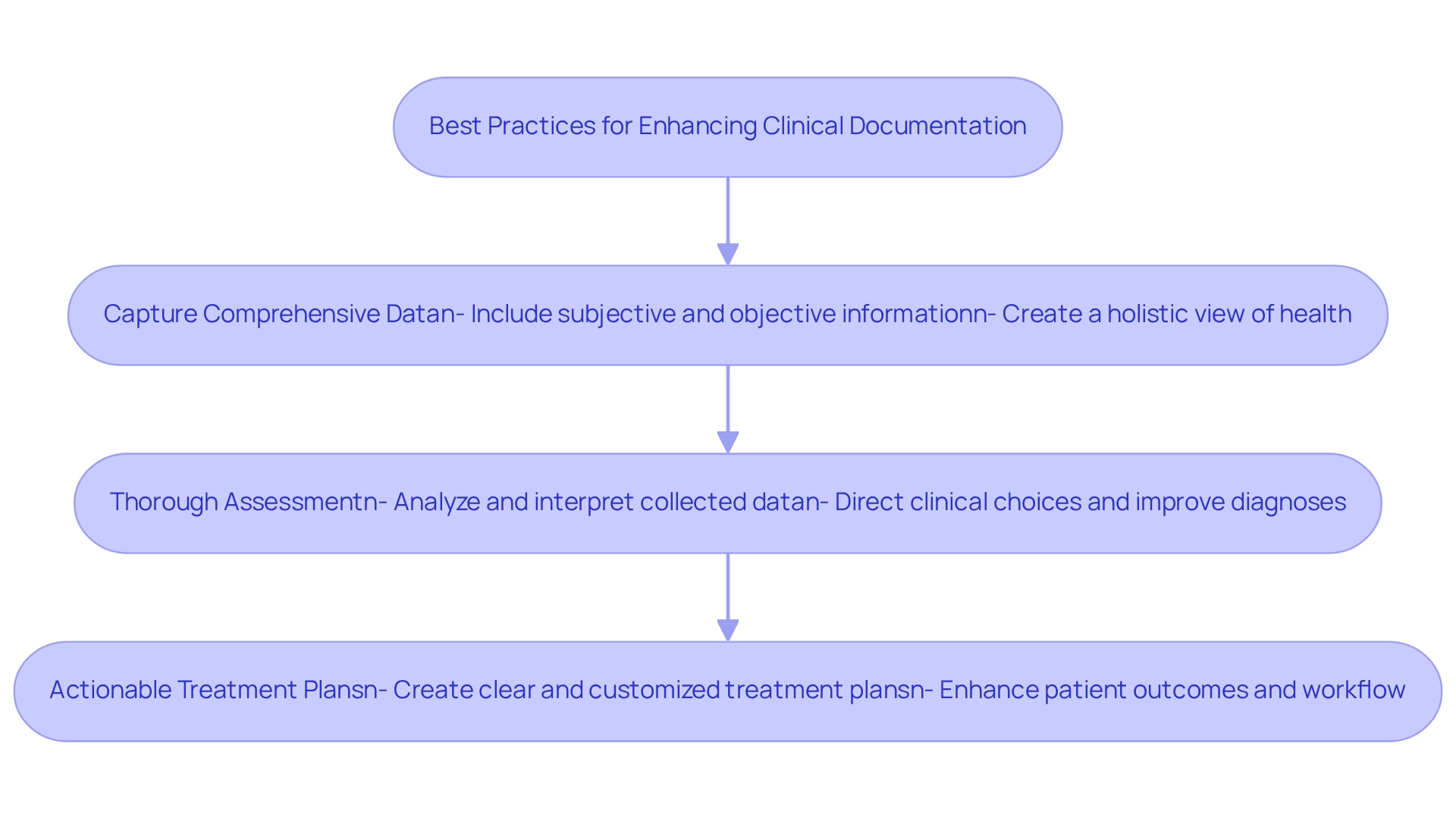
Key Takeaways: Enhancing Clinical Documentation with SOAP Notes
Effective SOAP notes are essential for providing high-quality clinical records, and we understand the emotional challenges you face in this demanding field. Here are some key principles to enhance your documentation practices:
- Capture Comprehensive Data: Always include both subjective and objective information to create a holistic view of the individual's health. This dual approach ensures that all relevant information is considered, leading to more informed clinical decisions.
- Thorough Assessment: Utilize the assessment section to analyze and interpret the collected data. This essential analysis not only directs clinical choices but also improves the precision of diagnoses. As you may have noticed, there is an increasing dependence on real-time clinical decision support systems that provide medical professionals with pertinent insights at crucial moments.
- Actionable Treatment Plans: Create clear and actionable treatment plans customized to the individual's unique needs. This specificity not only enhances patient outcomes but also promotes a more effective workflow for healthcare professionals.
Research shows that efficient clinical records greatly influence patient treatment. For instance, a research project at the Radboudumc Center for Head and Neck Oncology demonstrated that establishing organized treatment pathways enhanced record quality and efficiency. Implementing organized formats for electronic health records (EHR) resulted in clearer and more concise notes, ultimately improving the quality of service offered.
Furthermore, as the volume of inquiries for data obtained from EHRs is anticipated to increase, the significance of thorough record-keeping becomes even more evident. The Office of Inspector General observed that there is no substantial difference in coding mistakes between doctors recording in paper files and those utilizing EHRs, highlighting the efficiency of electronic record-keeping methods.
By following these best practices, you can enhance your records and improve overall client outcomes, leading to greater job satisfaction and professional well-being. Additionally, leveraging AI technology from CosmaNeura to streamline administrative tasks such as appointment scheduling and medical record management can alleviate the burden of time-consuming duties. This allows you to focus more on patient care, ultimately reducing burnout.
Ongoing research is needed to identify best practices for improving clinical documentation, emphasizing the evolving nature of this critical aspect of healthcare. Together, we can navigate these challenges and foster a supportive environment for both healthcare providers and patients.
Conclusion
Effective documentation through the use of SOAP notes is crucial in enhancing patient care in today’s healthcare landscape. Have you ever felt overwhelmed by the demands of capturing both subjective experiences and objective data? By systematically organizing this information, healthcare providers can create a comprehensive picture of their patients' health. This structured approach not only fosters informed clinical decision-making but also facilitates clear communication among team members, ensuring that everyone is aligned in their understanding of the patient's needs.
The assessment and planning phases within SOAP notes are vital in tailoring interventions that cater to individual patient circumstances. Imagine developing actionable treatment plans based on thorough analysis—this is how healthcare professionals can significantly improve patient outcomes and satisfaction. Moreover, the integration of technology, such as AI-driven solutions, enhances this process by streamlining documentation, allowing providers to focus more on meaningful patient interactions rather than administrative burdens.
In summary, mastering the art of SOAP note documentation is essential for delivering high-quality care. As healthcare continues to evolve, embracing effective documentation practices will not only support better clinical outcomes but also promote a more compassionate approach to patient care. By prioritizing structured documentation, healthcare providers can ensure they are well-equipped to meet the complexities of patient needs in an ever-changing environment. Let’s commit to refining our documentation practices together, fostering a healthcare experience that is both efficient and empathetic.




