Overview
This article addresses the emotional challenges faced by healthcare providers, who often find themselves overwhelmed by administrative tasks. It offers essential SOAP note practice scenarios designed to enhance documentation efficiency and improve patient care. By introducing innovative platforms such as CosmaNeura and Kiroku, the article highlights how these tools can automate and streamline the SOAP note process. This ultimately allows clinicians to dedicate more time to meaningful patient interactions rather than getting bogged down by paperwork.
Have you ever felt that the administrative burdens of documentation impact the quality of care you provide? You're not alone. Many healthcare professionals share this concern, and that's why exploring solutions is so important. The tools discussed here not only alleviate these pressures but also enhance the overall patient experience, fostering a more compassionate healthcare environment.
Imagine spending less time on administrative tasks and more time connecting with your patients. These innovative platforms are designed to do just that, transforming the way you approach documentation. By embracing these solutions, you can improve your workflow and enrich the care you provide.
Take the first step toward a more efficient practice. Explore the benefits of these platforms and consider how they might help you reclaim precious time in your day. Your patients deserve your full attention, and with the right tools, you can make that a reality.
Introduction
In the fast-paced world of healthcare, the administrative demands on providers can often feel overwhelming, overshadowing their primary mission: to deliver exceptional patient care. As the weight of documentation continues to grow, innovative solutions like SOAP note practice scenarios emerge as vital tools that can enhance both efficiency and accuracy in record-keeping. How can healthcare professionals navigate the complexities of documentation while ensuring that patient interactions remain at the forefront?
This article explores seven critical SOAP note practice scenarios, revealing how these structured formats not only streamline the documentation process but also foster improved patient outcomes and satisfaction. By addressing the emotional challenges faced by healthcare providers, we can better understand the impact of administrative burdens on patient care. Let's delve into these scenarios together, and discover how they can support your efforts in providing the best possible care for your patients.
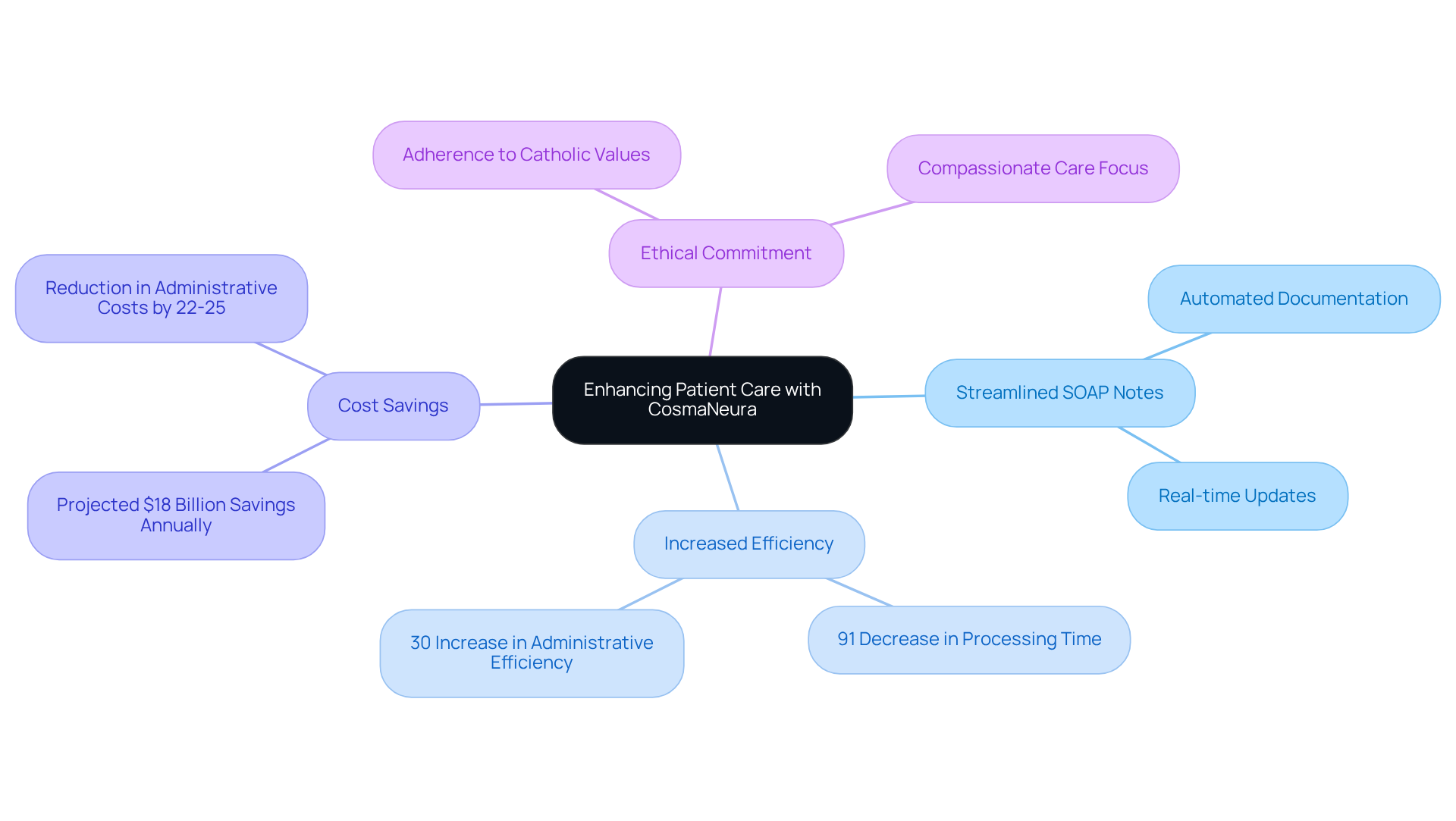
CosmaNeura: Streamline SOAP Note Documentation for Enhanced Patient Care
In the demanding world of healthcare, providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. CosmaNeura understands these challenges and transforms the SOAP note recording process in various SOAP note practice scenarios by automating it. This allows medical professionals to devote more time to rather than getting lost in paperwork.
Imagine a platform that not only ensures records are accurate and timely but also compliant with healthcare regulations. By streamlining these critical aspects of care, CosmaNeura significantly enhances efficiency, which is evident in the improved quality of service demonstrated in SOAP note practice scenarios for individuals. In fact, methods employing automated records have shown a remarkable 91% decrease in processing time, fostering greater engagement from those receiving care.
Furthermore, the integration of AI in medical documentation is projected to save organizations up to $18 billion annually by reducing administrative burdens. This aligns seamlessly with the ethical standards of Catholic teachings, reinforcing a commitment to compassionate and responsible care for individuals in need.
By addressing the financial pressures linked to rising medical expenses and the complexities of direct pay versus insurance, CosmaNeura's solutions empower providers to maintain in a cost-sensitive environment. How can we ensure that every patient receives the attention they deserve? With CosmaNeura, the answer is clear: by embracing innovation that prioritizes care over complexity.
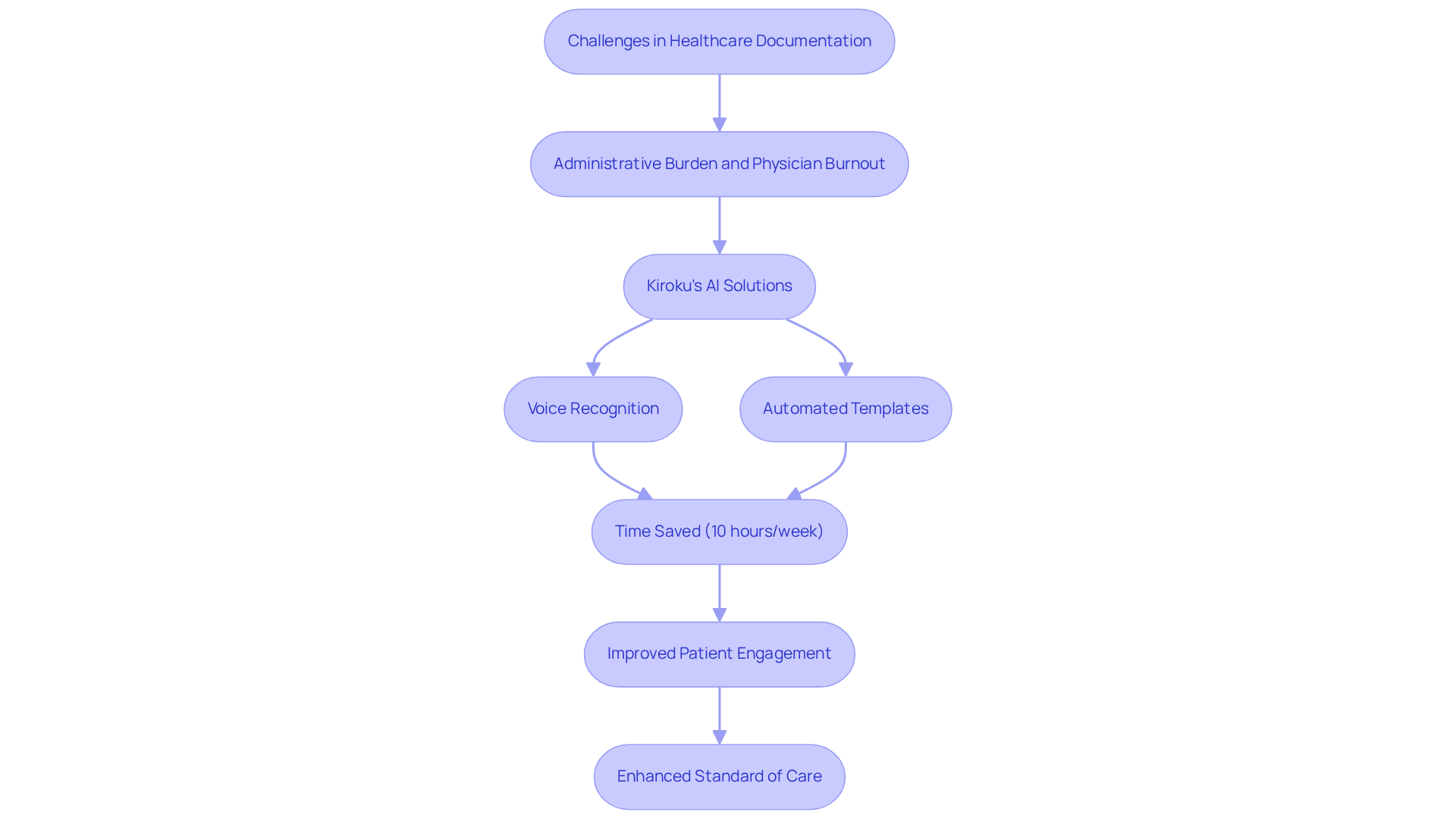
Kiroku: Simplify SOAP Note Creation with AI-Powered Tools
Healthcare providers often face overwhelming emotional challenges, especially when it comes to managing administrative tasks. The burden of record-keeping can detract from the precious time they have to care for their patients, contributing to the distressing issue of physician burnout.
Kiroku understands these struggles and utilizes cutting-edge AI technology to transform the generation of SOAP documentation. By leveraging advanced voice recognition and automated templates, Kiroku empowers clinicians to dictate their notes in real-time. This innovative approach significantly reduces the time spent on record-keeping, allowing providers to focus more on what truly matters—their patients.
Imagine saving about 10 hours each week! Statistics suggest that medical practitioners using AI recording tools experience this benefit, leading to improved patient engagement and satisfaction. Moreover, Kiroku seamlessly integrates with existing EHR systems, ensuring that documentation is both comprehensive and compliant.
As healthcare providers increasingly embrace AI solutions, Kiroku stands out as a leader in simplifying SOAP note practice scenarios. This not only aids in achieving better clinical results but also lessens the workload for providers. In a medical environment where many doctors are understandably risk-averse and reluctant to adapt, Kiroku offers a vital solution. It reduces administrative burdens while enhancing the overall standard of care.
By choosing Kiroku, healthcare professionals can reclaim their time and energy, ultimately leading to a more fulfilling practice and through effective SOAP note practice scenarios. Isn't it time to embrace a solution that nurtures both providers and patients alike?
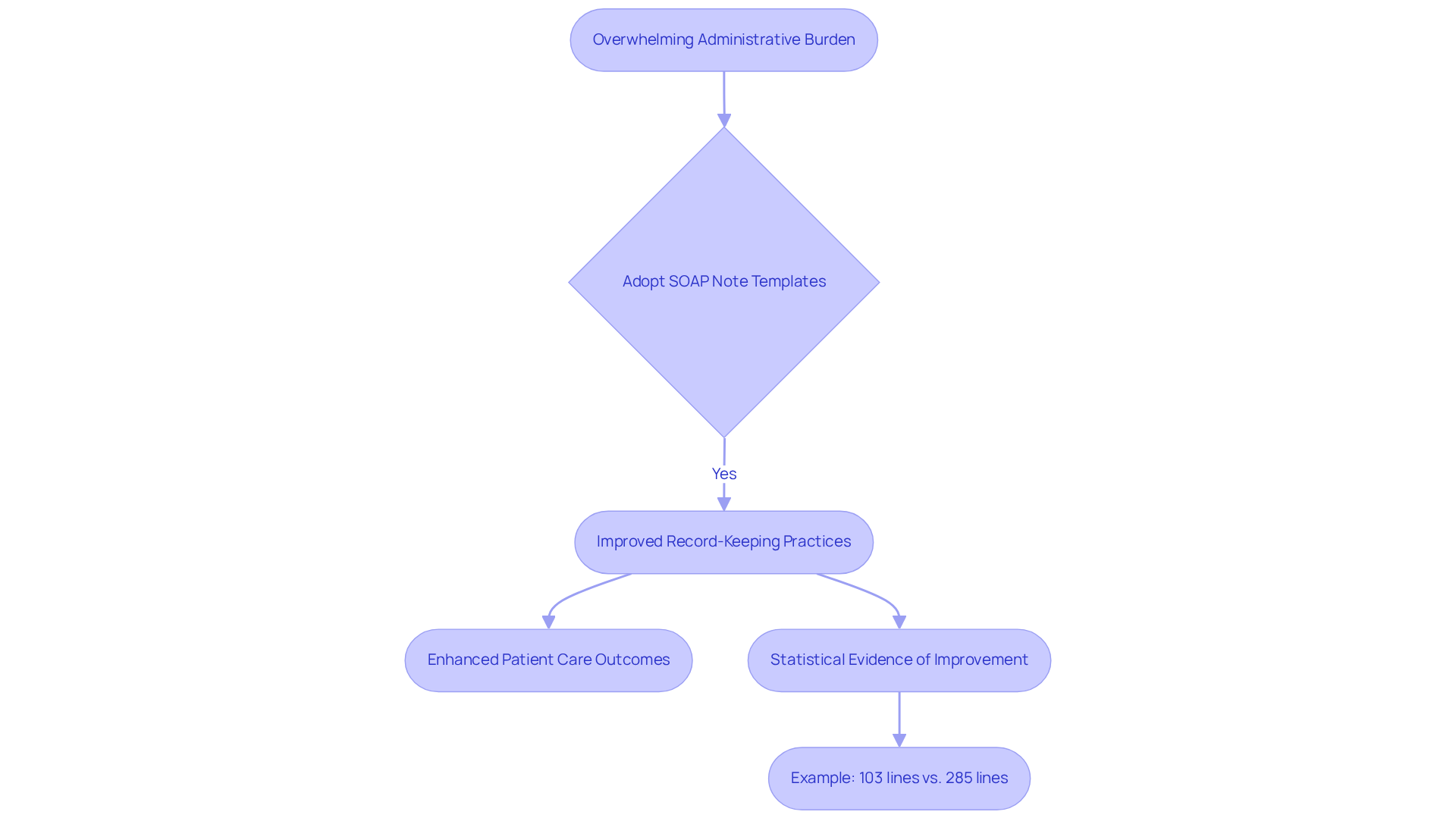
SimplePractice: Access SOAP Note Templates and Examples for Effective Documentation
Healthcare providers often face overwhelming administrative burdens that can detract from their primary mission: delivering compassionate care to patients. SimplePractice understands these challenges and provides an extensive range of practice scenarios and templates designed to ease the documentation process. By simplifying record-keeping, these templates ensure that essential information is captured clearly and organized effectively, allowing clinicians to focus more on their patients.
Imagine the difference it could make in your practice. By adopting these structured formats in soap note practice scenarios, you can significantly enhance your record-keeping practices, ultimately leading to improved patient care outcomes. Research shows that efficient record-keeping is vital for clinical effectiveness. For instance, a recent trial involving 36 residents demonstrated that a new template led to shorter records—103 lines versus 285 lines for the standard format (p < 0.001)—without compromising the quality of information presented. Faculty reviewers rated the standard notes as more accurate at 3.9 compared to 2.6 for the new notes (p = 0.003), underscoring the effectiveness of these templates.
This trend aligns with the growing inclination among medical providers to use soap note practice scenarios, which enhance communication within interdisciplinary teams and promote compliance with best practices in clinical records. As we look ahead to 2025 and the continued evolution of medical services, the importance of efficient record templates cannot be overstated. Resources like those provided by SimplePractice are essential for improving clinical workflows and ensuring that you can provide the best possible care to your patients.
Consider how these tools can transform your practice. By embracing these templates, you can alleviate some of the administrative load and refocus your energy on what truly matters—your patients. Let’s work together to create a more efficient and compassionate healthcare environment.
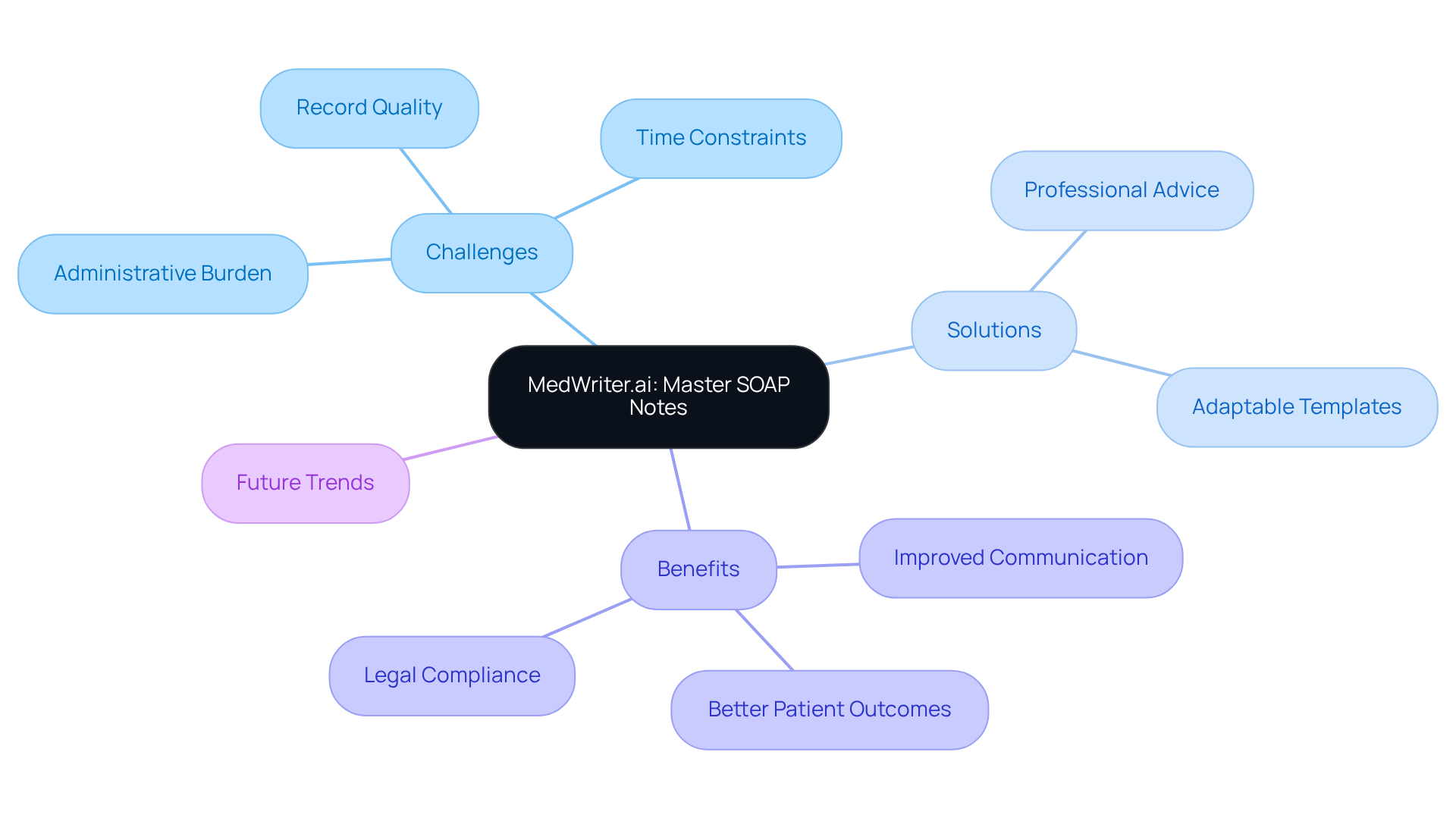
MedWriter.ai: Master SOAP Notes with Expert Guidance and Templates
Healthcare providers often face overwhelming administrative burdens that can detract from their primary focus: patient care. MedWriter.ai understands these challenges and offers a compassionate solution for creating SOAP records. By providing professional advice and adaptable templates, this innovative platform simplifies the note-taking process, allowing clinicians to craft thorough and accurate records that genuinely reflect their interactions with patients.
Imagine saving precious time while ensuring your records meet the highest standards of quality and compliance. With MedWriter.ai, you can enhance communication and coordination among , ultimately leading to better patient outcomes. Recent studies reveal that organized records significantly improve patient care results, underscoring the importance of efficient SOAP note practice scenarios in clinical practice.
Consider the impact of using a tool that not only streamlines your documentation but also fosters collaboration among healthcare professionals. Case studies have shown that platforms like MedWriter.ai lead to substantial improvements in SOAP note practice scenarios, ensuring legal compliance and promoting effective communication within medical teams.
As we move towards 2025 and beyond, the trend of customizable templates continues to grow. MedWriter.ai stands at the forefront, equipping healthcare professionals with the necessary tools for accurate and efficient documentation. Embrace this opportunity to enhance your practice and improve patient care by exploring what MedWriter.ai can do for you.
Blueprint.ai: Effective SOAP Note Examples for Therapy Practices
At Blueprint.ai, we understand the emotional challenges that therapy practices face in maintaining effective documentation. Our comprehensive selection of soap note practice scenarios serves as practical guides, helping therapists accurately capture essential information in various client situations. By utilizing these organized formats, clinicians can alleviate the administrative burdens that often detract from patient care, leading to improved clarity and consistency in medical files.
Imagine the relief of enhanced communication among healthcare professionals, which ultimately elevates the standard of care provided to individuals. Consistently using soap note practice scenarios empowers therapists to refine their record-keeping practices, benefiting their professional growth and positively impacting patient outcomes. As experts remind us, 'Quoting your clients directly in can be incredibly powerful.' This highlights the significance of structured documentation in fostering meaningful connections.
Moreover, examining and modifying SOAP records before completion is crucial for ensuring clarity and legal compliance. By adopting these methods, therapists can reclaim valuable hours previously lost to administrative tasks, allowing them to focus more on what truly matters: client care. We encourage you to explore these resources and experience the transformative benefits they can bring to your practice.

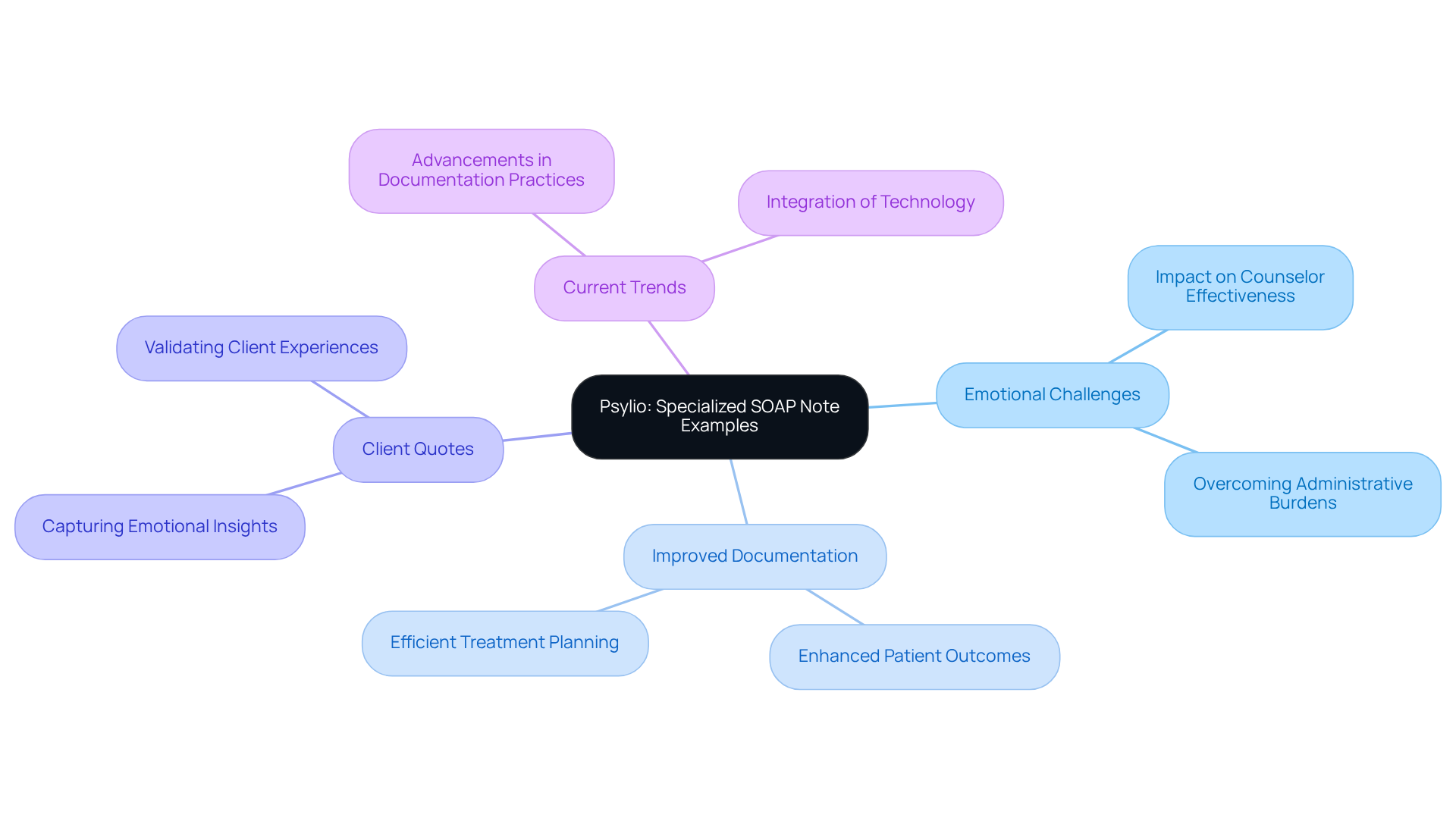
Psylio: Specialized SOAP Note Examples for Mental Health Counseling
In the demanding field of mental health counseling, professionals often face emotional challenges that can impact their effectiveness. Psylio recognizes this and provides specialized soap note practice scenarios that serve as vital resources designed to support counselors in precisely recording the nuances of client interactions within therapeutic environments. Have you ever felt overwhelmed by the administrative burdens that distract from patient care? These examples help ensure that critical details are not overlooked, allowing you to focus on what truly matters—your clients.
By utilizing these customized resources, mental health experts can greatly improve their soap note practice scenarios for record-keeping methods. Imagine the difference it could make in your practice—better documentation leads to improved patient outcomes and more efficient treatment planning. The incorporation of direct quotes from clients can offer deeper insights into , further enhancing the record-keeping process. As the field evolves, staying updated with current trends in documentation practices is essential for maintaining high standards of care.
Consider taking the next step in your professional journey. Engage with these resources to enhance your practice, ensuring that you provide the compassionate care your clients deserve. Together, we can navigate the complexities of mental health documentation, fostering an environment where both providers and clients thrive.
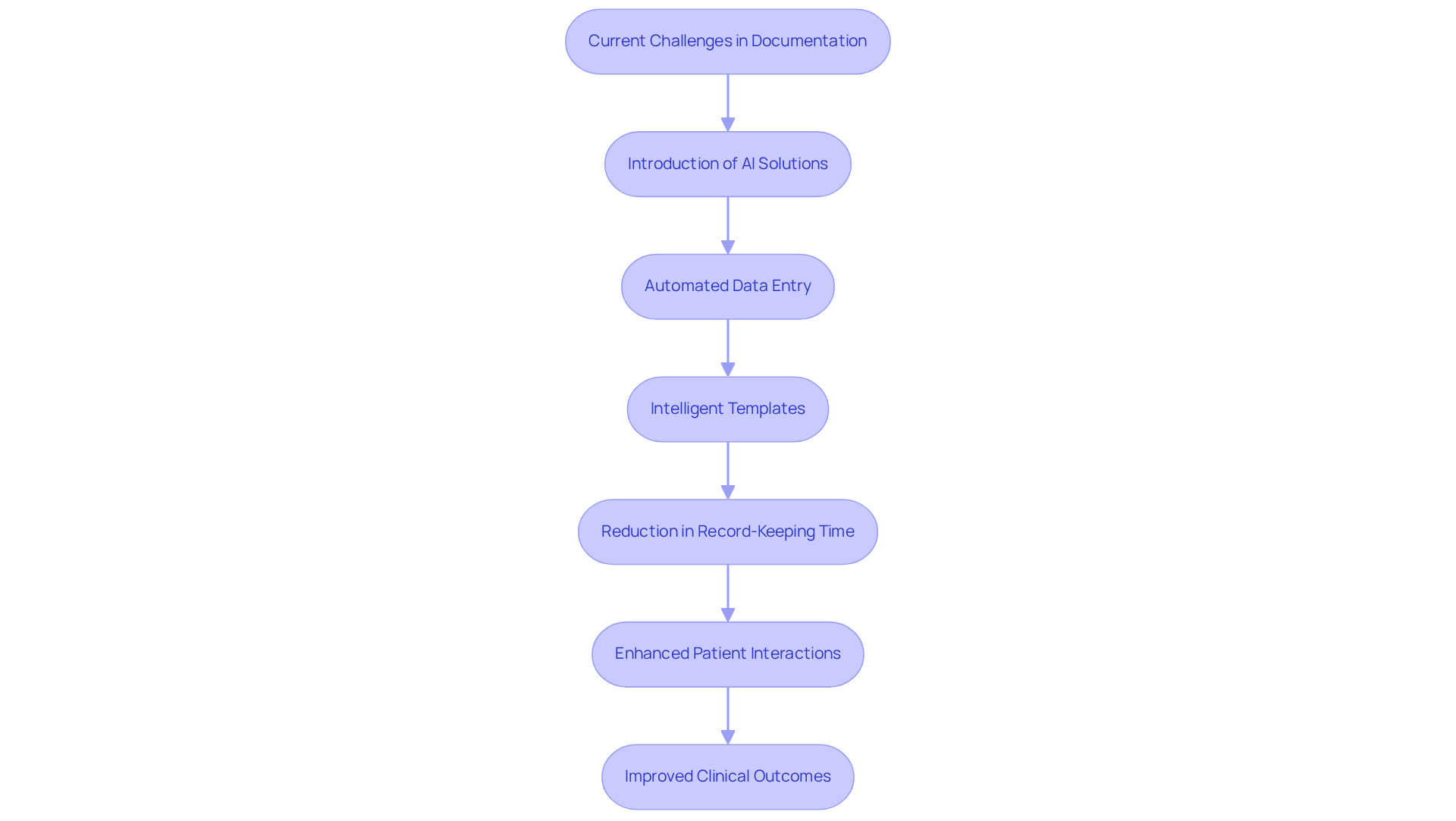
TryTwoFold: AI Solutions for Efficient SOAP Note Writing
Healthcare providers often face emotional challenges when it comes to documentation. The reluctance to embrace innovation can feel overwhelming, especially when it impacts the quality of patient care. TryTwoFold understands these concerns and offers innovative AI-powered solutions that significantly improve the soap note practice scenarios in the documentation writing process. By automating data entry and utilizing intelligent templates, TryTwoFold enables clinicians to generate accurate and comprehensive notes swiftly.
Imagine the relief of reducing the administrative load. With this automation, providers can focus more on delivering high-quality care to individuals. Hospitals that have adopted report up to a 40% decrease in record-keeping time. This has led to enhanced patient interactions and satisfaction, demonstrating the positive impact of innovation on healthcare delivery.
As we look ahead to in 2025, incorporating AI tools like TryTwoFold becomes crucial. These solutions streamline record-keeping processes in soap note practice scenarios, ultimately leading to improved clinical outcomes and increased job satisfaction among medical professionals. By directly addressing physician concerns about quality of care and efficiency, TryTwoFold aids in transforming medical delivery.
Are you ready to embrace innovation while reducing burnout? Let TryTwoFold support you in making this transition easier, ensuring that your focus remains on what truly matters—caring for your patients.
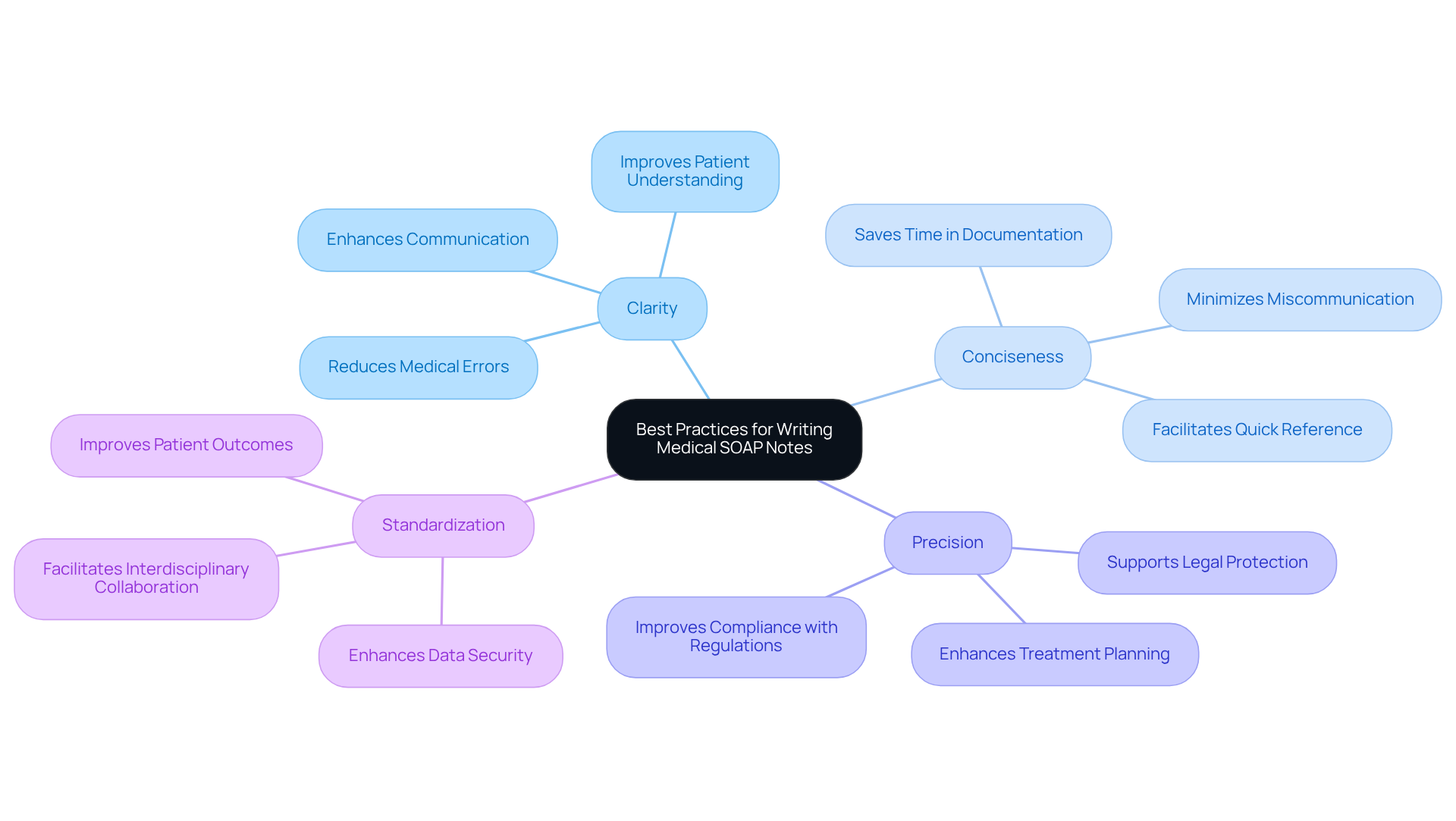
EHS Insight: Best Practices for Writing Medical SOAP Notes
EHS Insight recognizes the emotional challenges faced by healthcare providers in creating soap note practice scenarios. Clarity, conciseness, and precision in reporting are not just best practices; they are essential for alleviating the administrative burdens that can impact patient care. By adhering to these guidelines, medical providers can develop documentation that not only meets industry standards but also fosters compliance with regulations.
Have you considered can significantly reduce medical errors? Studies indicate that it can decrease such errors by up to 25%, enhancing outcomes for individuals by 20-30%. By applying these optimal methods, you raise the standard of documentation and promote better communication among healthcare experts, ultimately improving care for individuals.
For instance, soap note practice scenarios serve as invaluable resources for tracking individual progress, ensuring that treatment plans are easily understood. This clarity is vital for maintaining adherence and satisfaction. Moreover, real-world examples illustrate that effective soap note practice scenarios can greatly minimize misunderstandings between providers and patients, leading to stronger therapeutic relationships and improved outcomes.
As we look toward 2025, the emphasis on clarity in medical documentation remains paramount. It directly influences the quality of care delivered in clinical settings. Let’s continue to prioritize these practices, fostering an environment of understanding and support for both providers and patients alike.
Lindy.ai: SOAP Note Examples for Chest Pain Management
In the demanding world of healthcare, managing chest pain can be an emotionally charged experience for both providers and patients. Lindy.ai recognizes the challenges you face and offers soap note practice scenarios specifically tailored for chest pain management. These examples not only guide you in documenting this critical condition but also help you gather essential client information effectively.
Imagine the peace of mind that comes from knowing you have all pertinent details incorporated into your records. By utilizing soap note practice scenarios, you can enhance your record-keeping practices, ultimately improving safety for the individuals you care for. This is not just about documentation; it's about fostering a supportive environment where every detail matters.
We invite you to explore how these resources can lighten your administrative burdens, allowing you to focus more on what truly matters—your patients. Together, we can improve the and ensure that every individual receives the attention they deserve.
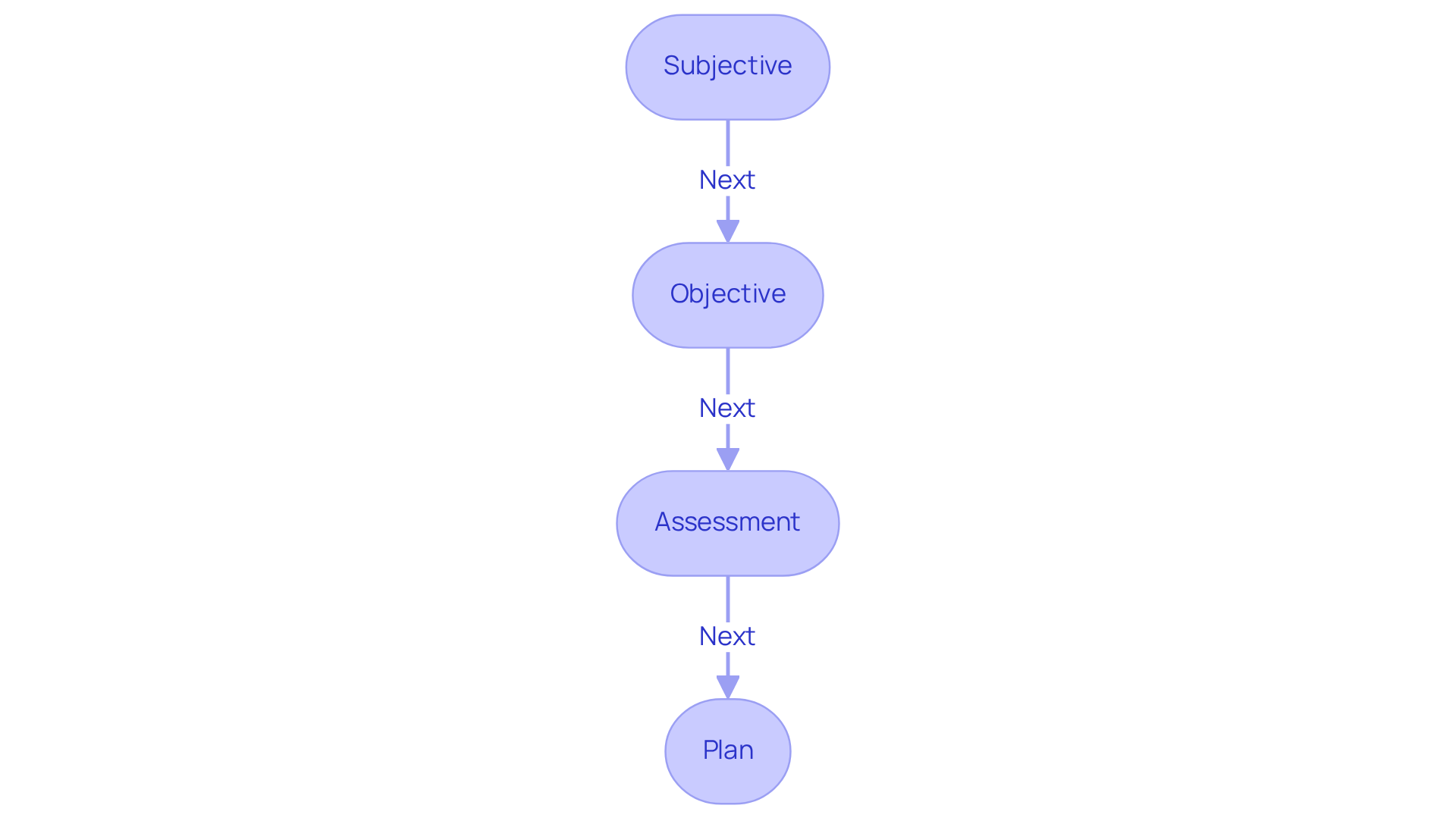
Mentalyc: Understanding SOAP Notes in Mental Health Practice
Mentalyc underscores the vital role of SOAP records in mental health practice, illustrating how these organized entries can significantly improve the documentation of client interactions. By following the SOAP format—Subjective, Objective, Assessment, and Plan—mental health professionals can systematically capture essential information that not only informs treatment decisions but also tracks patient progress.
Have you ever felt overwhelmed by the administrative tasks that can distract from patient care? Real-world examples highlight the effectiveness of soap note practice scenarios in various situations. For instance, a client experiencing severe depression may share feelings of hopelessness and difficulty concentrating, which can be documented in the Subjective section. The Objective section would then encompass observable data, such as the client's disheveled appearance and lack of eye contact, offering a comprehensive view of their condition.
Expert opinions emphasize the importance of precise records in mental health treatment. Dr. Lawrence Weed, a pioneer in SOAP note creation, noted that "SOAP notes have become the standard approach for recording progress and enhancing communication between healthcare providers." This structured method not only aids in treatment planning but also ensures compliance with regulatory standards, fostering a sense of security in your soap note practice scenarios.
As we look towards the future, current trends in record-keeping reveal a growing reliance on technology. Tools like Mentalyc are automating the note-taking process, allowing mental health professionals to dedicate more time to patient care while ensuring that documentation remains accurate and compliant with HIPAA regulations. Moreover, integrating SMART objectives into SOAP records can clarify expectations and enhance accountability in treatment planning.
In 2025, the focus on SOAP records continues to grow, as they remain essential for effective communication and continuity of care in mental health environments. By mastering soap note practice scenarios, clinicians can enhance the quality of care they provide, ultimately leading to better patient outcomes. Additionally, a retrospective billing analysis can uncover areas for revenue recovery, highlighting the financial benefits of thorough documentation in mental health practice.
Together, let’s embrace these practices to improve not only our documentation but also the we offer to our clients.
Conclusion
In the realm of healthcare, we understand that effective documentation is essential for ensuring quality patient care. SOAP notes emerge as a vital tool in this process. Have you ever felt overwhelmed by administrative tasks? By embracing innovative solutions like those offered by CosmaNeura, Kiroku, and others, healthcare providers can streamline their documentation practices. This shift allows for more meaningful patient interactions and less time spent on paperwork.
Imagine reducing your documentation time significantly while improving communication among your healthcare team. The article highlights several essential SOAP note practice scenarios that showcase the benefits of utilizing advanced tools and templates. Each platform discussed, whether it be SimplePractice's templates or MedWriter.ai's guidance, illustrates the importance of adopting best practices in SOAP note documentation. This approach not only enhances the accuracy and efficiency of record-keeping but also fosters a supportive environment for both providers and patients.
As the healthcare landscape evolves, the significance of efficient and accurate documentation cannot be overstated. By prioritizing innovative SOAP note solutions, providers can alleviate administrative burdens. This ultimately leads to better care for patients. Embracing these advancements enhances the quality of care and nurtures a more compassionate healthcare environment. It is time to take action—explore these tools and transform your documentation practices for the betterment of both providers and patients alike.




