Overview
This article highlights the emotional challenges faced by healthcare providers in documenting patient care. It recognizes that the administrative burdens often weigh heavily on their ability to focus on what truly matters—their patients. By providing essential assessment SOAP note examples, we aim to support healthcare providers in enhancing their documentation practices.
Effective SOAP notes are not just a formality; they are a vital tool that enhances patient care. When subjective and objective data are communicated accurately, it fosters better clinical decision-making and ultimately leads to improved patient outcomes. Imagine the difference it could make when every detail is captured with care and precision.
We encourage you to reflect on your current documentation practices. Are they serving your patients as well as they could? By adopting these SOAP note examples, you can transform your approach to patient care. Let’s work together to ensure that every patient receives the attention and care they deserve.
In summary, better documentation practices can significantly impact patient care. We invite you to explore these examples and consider how they can benefit your practice. Your commitment to improving documentation is a step towards nurturing better patient relationships and outcomes.
Introduction
In the intricate world of healthcare, many providers feel the weight of balancing patient care with administrative responsibilities. This delicate equilibrium can often seem precarious, especially as demands continue to rise. The challenge of maintaining accurate and effective documentation is not just an administrative task; it’s a vital component of quality patient care. What if the key to improving patient outcomes lies not only in treatment but also in how we record and communicate information? By exploring this idea, we can uncover the transformative power of structured documentation, which fosters better healthcare experiences for both patients and providers.
CosmaNeura: AI-Driven SOAP Note Automation for Healthcare Providers
In today’s fast-paced healthcare environment, providers often face overwhelming administrative burdens that can detract from their ability to deliver compassionate care. Have you ever felt that the time spent on paperwork takes away from your interactions with patients? CosmaNeura understands these challenges and offers a solution that can help.
By utilizing cutting-edge AI technology, CosmaNeura automates the generation of clinical documentation, streamlining the record-keeping process for healthcare providers. This combines client intake and triage capabilities, ensuring that documentation is produced effectively and precisely. As a result, the time dedicated to administrative duties is greatly minimized, allowing you to focus more on what truly matters—your patients.
Imagine being able to allocate more time to client interactions, directly addressing concerns about innovation in healthcare. This automation not only boosts productivity but also alleviates the stress of administrative tasks. In doing so, CosmaNeura aligns with the mission of delivering compassionate care in a faith-focused environment.
Moreover, by enhancing financial efficiency through reduced operational costs and improved workflow, CosmaNeura empowers healthcare providers to thrive. Are you ready to embrace a solution that prioritizes both your wellbeing and that of your patients? Let’s explore how CosmaNeura can support you in your journey toward compassionate care.
Understanding SOAP Notes: Key Components and Their Importance
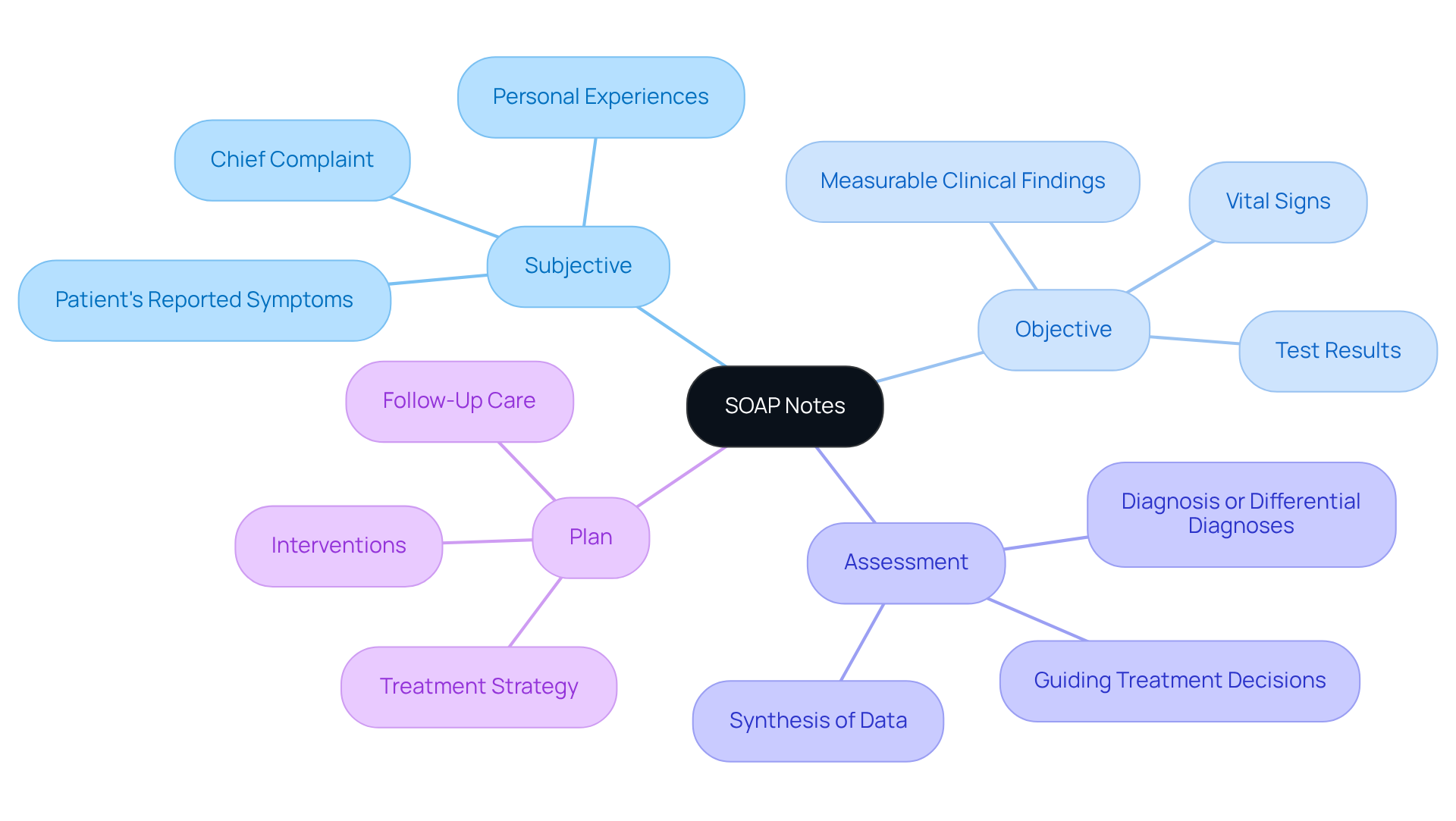
In the healthcare field, structured records, such as an assessment soap note example, are vital tools and consist of four main elements:
- Subjective
- Objective
- Assessment
- Plan
Have you ever felt overwhelmed by the sheer volume of information to capture? The Subjective section captures the individual's reported symptoms and experiences, providing essential context for the clinician. In contrast, the Objective section includes measurable clinical findings, such as vital signs and test results, which lend credibility to the assessment.
The assessment soap note example synthesizes subjective and objective data to formulate a diagnosis or differential diagnoses, guiding treatment decisions. This process can feel daunting, but it is crucial for effective patient care. Finally, the Plan outlines the treatment strategy, including interventions and follow-up care, ensuring continuity of care. Research shows that organized records, like structured notes, greatly boost clinical decision-making and enhance outcomes for individuals. This makes them essential in healthcare environments.
To enhance the efficiency of documentation, healthcare professionals should strive to following client interactions. By doing so, you not only improve your workflow but also contribute positively to the care you provide. Remember, your efforts in maintaining organized records can lead to better patient outcomes and a more fulfilling practice.
Real-World SOAP Note Examples: Practical Applications for Healthcare Providers
-
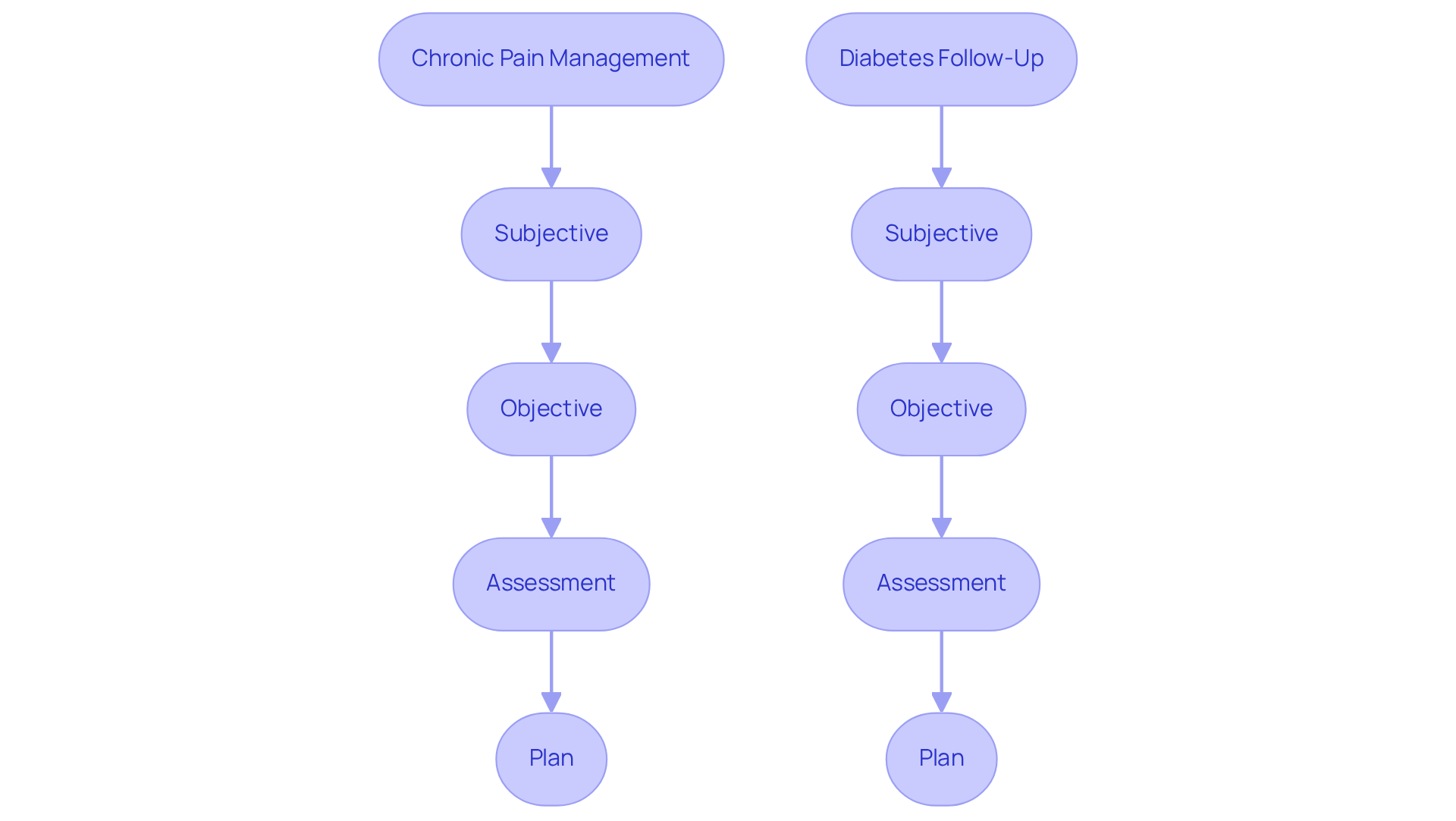
Example 1: Chronic Pain Management
- Subjective: The patient shares a pain level of 7/10 in the lower back, which worsens with prolonged sitting.
- Objective: A physical examination reveals limited range of motion and tenderness in the lumbar region.
- Assessment: This indicates chronic lower back pain, likely due to muscle strain.
- Plan: We recommend physical therapy and prescribe NSAIDs to help manage the pain effectively.
-
Example 2: Diabetes Follow-Up
- Subjective: The patient reports increased thirst and frequent urination, which may signal issues with blood sugar control.
- Objective: A blood glucose level of 250 mg/dL suggests that diabetes management needs improvement.
- Assessment: The patient is experiencing poorly controlled diabetes mellitus, requiring timely intervention.
- Plan: We will adjust the insulin dosage and schedule a follow-up appointment in one month to reassess management strategies.
Effective recording through an assessment soap note example is vital for providing quality care to individuals. Have you ever felt overwhelmed by the administrative burdens that can detract from patient care? Research shows that using like an assessment soap note example can enhance record quality by up to 30%, improving communication among healthcare teams. By integrating generative AI into the record-keeping process, healthcare providers can automate data entry, ensuring vital information is captured accurately and reducing the risk of errors. This technology not only simplifies record-keeping but also allows providers to focus more on client interactions. Prioritizing organized record-keeping techniques guarantees clarity and precision in medical files, ultimately leading to improved healthcare outcomes. Let's embrace these advancements together for a brighter future in patient care.
Common SOAP Note Mistakes: What Healthcare Providers Should Avoid
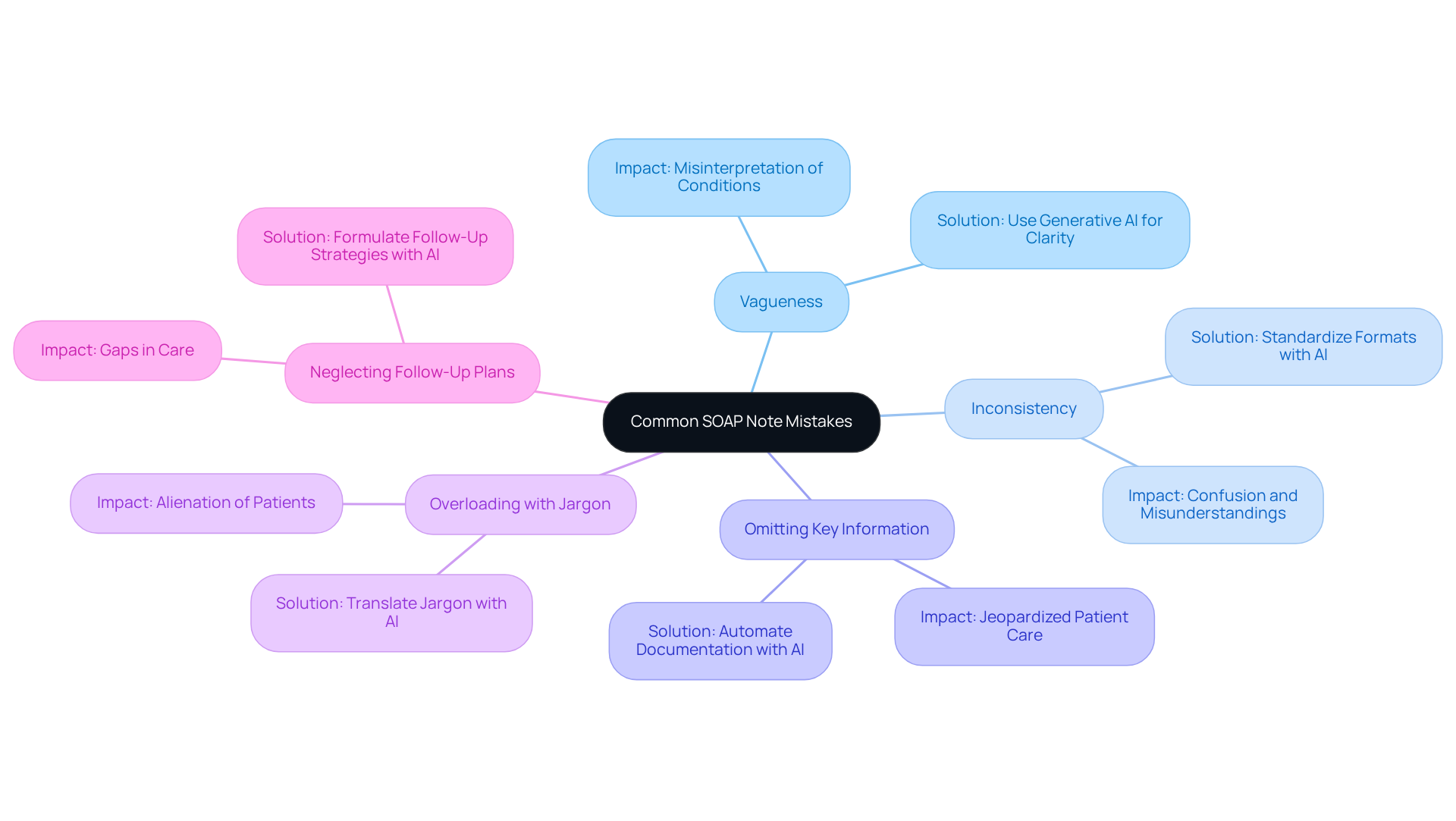
- Vagueness: Ambiguous language can lead to misinterpretation of individual conditions, which may compromise patient care. Have you ever wondered how often unclear descriptions affect outcomes? Research indicates that nearly 30% of record errors stem from vagueness, underscoring the need for clarity. Generative AI can support healthcare professionals in crafting clear and concise records, reducing the likelihood of ambiguity by prompting for specific details and ensuring thorough descriptions.
- Inconsistency: A lack of a consistent format can confuse readers and hinder effective communication. How often do inconsistent records lead to misunderstandings? Ensuring uniformity in the assessment SOAP note example is crucial, as discrepancies can lead to misinterpretations of patient status and treatment strategies. AI tools can assist in standardizing formats, applying templates and guidelines to ensure consistency across records.
- Omitting Key Information: Neglecting to include critical details can jeopardize patient care and follow-up. Have you considered the impact of insufficient records on client outcomes? Research shows that missing information is a significant factor in negative results, highlighting the . Generative AI can automate the documentation process by providing an assessment SOAP note example that prompts providers to include all necessary information, thereby minimizing the risk of omissions.
- Overloading with Jargon: Excessive medical terminology can alienate patients and obscure essential information. Is your language accessible to those you serve? Clear communication is vital for ensuring that individuals understand their conditions and care plans. AI-powered tools can help translate complex medical jargon into patient-friendly language, fostering better understanding and engagement.
- Neglecting Follow-Up Plans: Failing to outline clear next steps can create gaps in care. How can we ensure continuity of care for our patients? A well-defined follow-up strategy is essential, as it guarantees that individuals receive the necessary attention and interventions after their visit. Generative AI can assist in formulating comprehensive follow-up strategies by suggesting specific timelines and responsibilities, ensuring that all necessary steps are documented and communicated effectively.
Best Practices for Writing Effective SOAP Notes in Healthcare
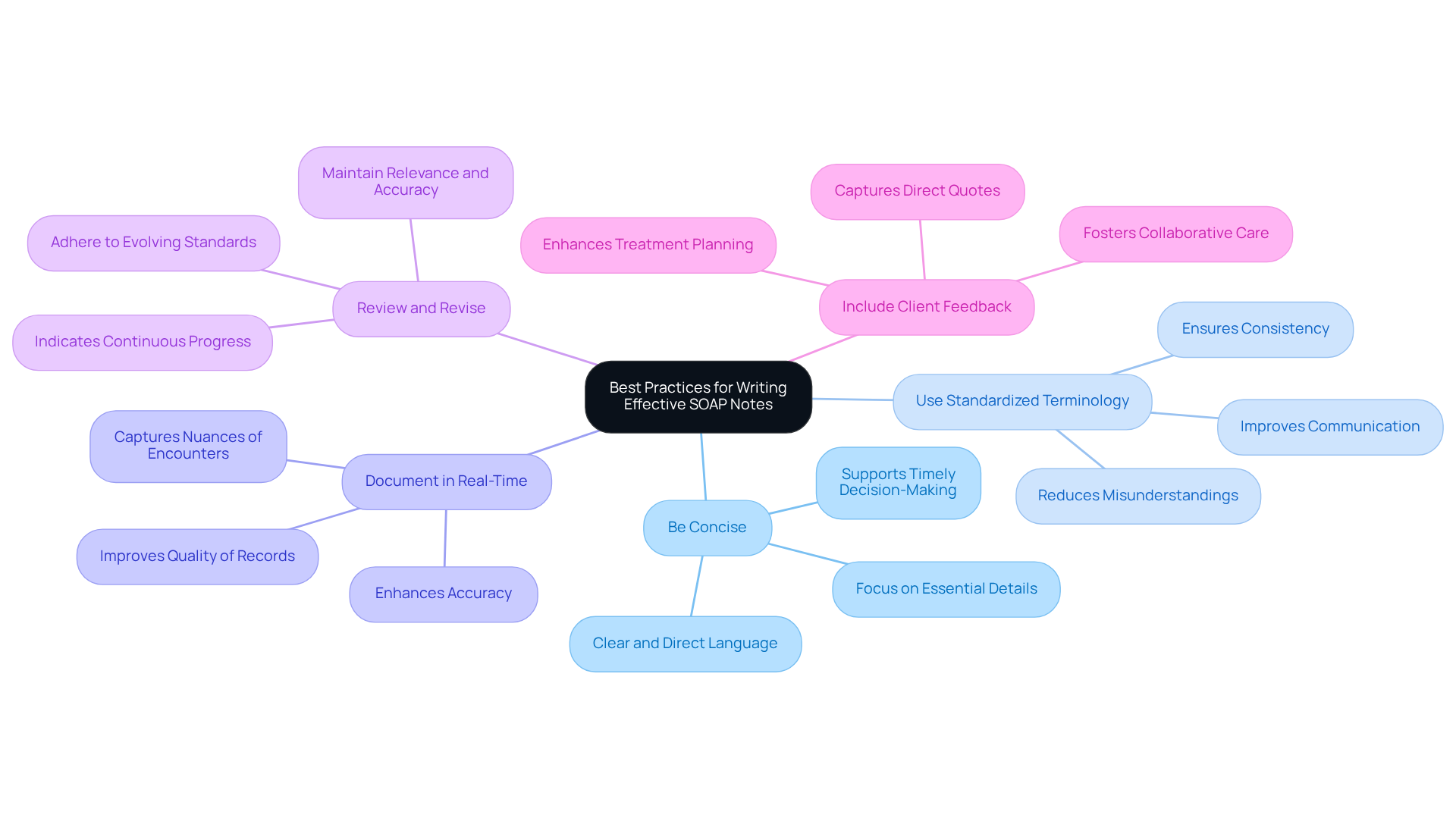
- Be Concise: Clear and direct language is essential for conveying information efficiently. Each note should capture the essential details without unnecessary elaboration. This approach not only enhances clarity but also supports timely decision-making in healthcare, allowing providers to focus on what truly matters.
- Use Standardized Terminology: Adopting common medical terms is crucial for improving communication among healthcare providers. By using standardized terminology, we can reduce misunderstandings and ensure that all team members interpret records consistently. This consistency is vital for effective collaboration and ultimately improves patient care.
- Document in Real-Time: Writing notes during or immediately after patient interactions significantly enhances accuracy. This practice captures the nuances of each encounter, reducing the risk of forgetting critical details and improving the overall quality of records. As we see, 100,000 providers are changing the way healthcare is delivered, highlighting the importance of effective documentation practices.
- Review and Revise: Regularly revisiting and updating documentation is essential for maintaining relevance and accuracy. This practice guarantees adherence to evolving clinical standards and indicates continuous progress in treatment modifications. Following institutional policies concerning the assessment soap note example is vital for upholding high standards in record-keeping, ensuring we provide the best care possible.
- Include Client Feedback: Integrating client perspectives into documentation fosters a collaborative approach to care. By capturing direct quotes and insights from individuals, we can create a more comprehensive understanding of their experiences. This understanding is essential for . For instance, recording client self-reported experiences illustrates the importance of including patient input in medical records, ultimately enhancing the care we provide.
Leveraging Technology: Enhancing SOAP Note Documentation with Digital Tools
Healthcare providers often face emotional challenges due to overwhelming administrative tasks. Digital tools like electronic health records (EHRs) and specialized recording software can ease this burden. By utilizing features such as templates, voice recognition, and automated prompts, record-keeping becomes simpler, reducing errors and saving precious time.
Imagine having access to AI-driven solutions like CosmaNeura, which offer real-time suggestions for documentation. This not only ensures accurate capture of necessary information but also enhances efficiency. CosmaNeura’s intelligent, HIPAA-compliant AI solutions align with compassionate care that reflects Catholic values, fostering a nurturing environment for both providers and patients.
Consider the positive impact these tools can have on your practice. By streamlining documentation, you can focus more on what truly matters—your patients. For practical implementation, explore our API examples to see how these solutions can seamlessly integrate into your existing systems. Together, we can for both providers and those they care for.
Legal and Ethical Considerations in SOAP Note Documentation for Providers
Healthcare providers often face emotional challenges while navigating the complex landscape of legal and ethical considerations in documenting SOAP notes. It’s crucial to maintain the confidentiality of individuals and secure informed consent before sharing any information. Adhering to regulations like HIPAA is not just a requirement; it protects medical data and fosters trust in the healthcare system.
Consider this: nearly 10% of individuals in healthcare settings encounter medication mistakes. This statistic underscores the necessity of precise records in preventing such issues. Moreover, the ethical consequences of record-keeping practices are significant; providers must accurately portray client interactions, ensuring their records reflect honesty and integrity.
This commitment to ethical record-keeping not only enhances care for individuals but also nurtures a culture of accountability within healthcare environments. By employing an organized format for clinical records, we can improve record-keeping procedures, facilitating clearer communication and ultimately leading to better patient outcomes.
Expert insights reveal that effective record-keeping practices are essential for building trust and ensuring quality care. Let’s work together to create a supportive environment that prioritizes both patient safety and ethical standards. Your makes a difference in the lives of those you serve.
Training Opportunities: Enhancing SOAP Note Writing Skills for Healthcare Providers
Healthcare providers often face emotional challenges when it comes to managing documentation effectively. The burden of administrative tasks can detract from the vital care they provide to individuals. However, focused training options such as workshops, online courses, and mentorship initiatives can significantly enhance their documentation skills. Numerous organizations offer specialized training that emphasizes efficient record-keeping methods, legal aspects, and the integration of digital tools.
Engaging in these educational initiatives not only sharpens individual skills but also nurtures a culture of excellence within healthcare teams. For instance, the case study 'Benefits of SOAP Notes' acts as an assessment soap note example, illustrating how effective record-keeping practices can enhance care and communication among healthcare providers. Moreover, workshops have shown the ability to improve record precision and efficiency, leading to better outcomes for individuals.
As seen in various case studies, efficient training initiatives can streamline the record-keeping process, allowing healthcare workers to focus more on patient care rather than administrative duties. Continuous learning is essential; as Helen Hayes wisely stated, 'The expert in anything was once a beginner.' This underscores the importance of to refine skills and adapt to the ever-evolving demands of healthcare.
Furthermore, John Dewey's insight, 'Education is not preparation for life; education is life itself,' highlights the critical role of ongoing education in enhancing record-keeping methods. Healthcare professionals are encouraged to explore accessible workshops and online classes to improve their clinical record skills. By doing so, they can ultimately enhance the care they provide to individuals, fostering a more compassionate and effective healthcare environment.
Impact of SOAP Notes on Patient Care: Enhancing Outcomes Through Effective Documentation
An assessment soap note example illustrates how effective documentation is essential for enhancing patient care, ensuring that all relevant information is accurately recorded and communicated among healthcare providers. Have you ever felt overwhelmed by the administrative burdens that can distract from patient interaction? Thorough records, such as those in an assessment soap note example, not only aid improved clinical decision-making but also significantly lower the risk of mistakes, thereby enhancing continuity of care. Research shows that healthcare professionals who engage in organized documentation training observe a remarkable 37% decrease in ambiguous or unreadable records compared to those relying on traditional recording techniques. This enhancement in clarity is directly linked to increased satisfaction and better outcomes for individuals.
Furthermore, the careful integration of subjective and objective data within an assessment soap note example allows for a more nuanced understanding of individual needs. For instance, have you considered how actively listening and employing open-ended questions during client interactions can yield richer subjective data? This approach is crucial for accurate diagnoses and personalized treatment plans. An assessment soap note example during a well-organized evaluation stage can enhance health outcomes by as much as 50%, underscoring the significance of efficient record-keeping in clinical practice.
In real-world applications, healthcare professionals who prioritize detailed clinical documentation report greater satisfaction levels among clients. Individuals feel more understood and involved in their care. By utilizing advanced diagnostic technologies and voice recognition software, clinicians can enhance the accuracy and efficiency of their record-keeping. Ultimately, this leads to improved patient experiences and outcomes. Thus, by dedicating themselves to , healthcare providers can significantly elevate the standard of care they deliver.
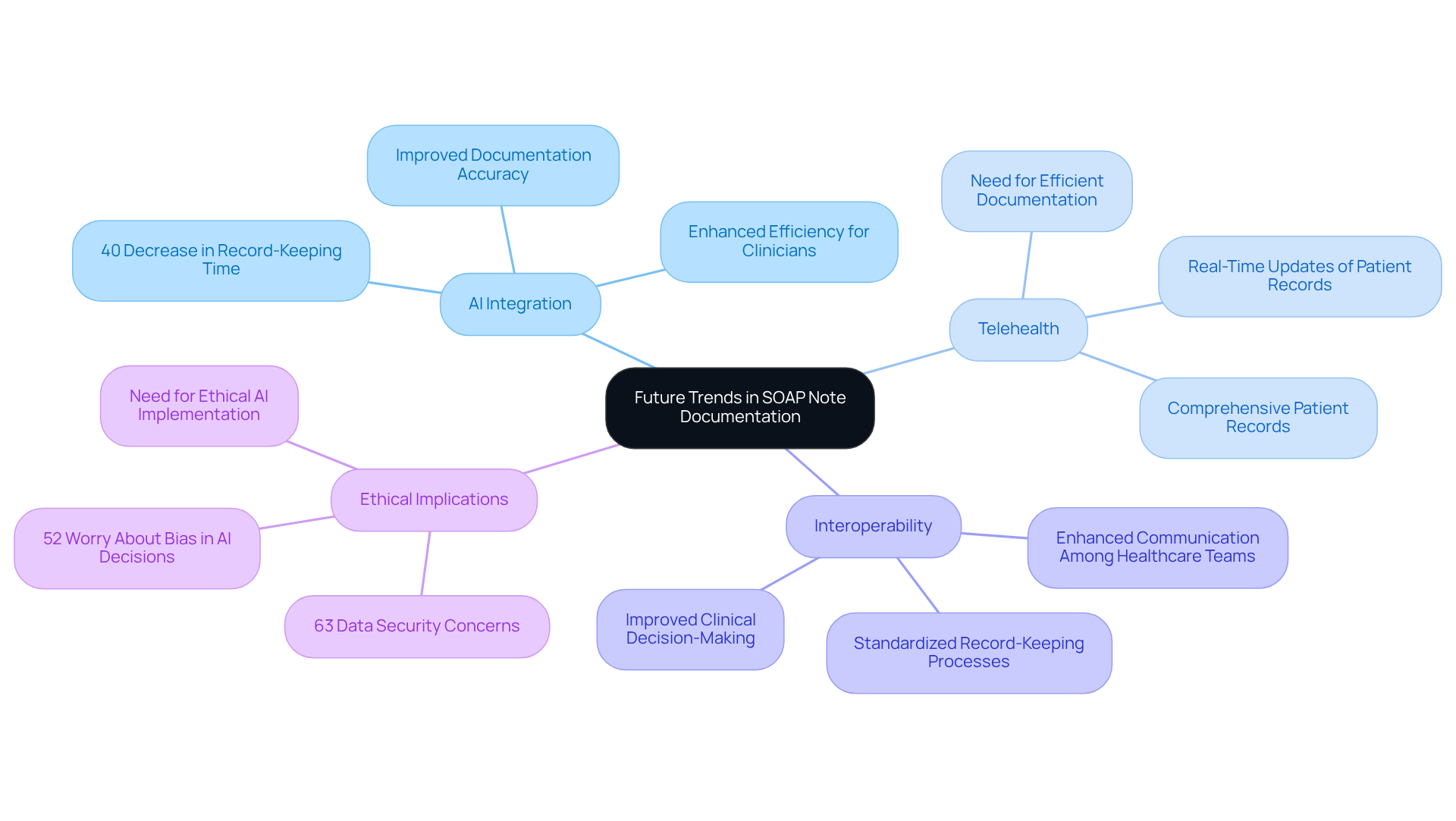
Future Trends in SOAP Note Documentation: What Healthcare Providers Need to Know
The terrain of clinical record writing is evolving rapidly, shaped by significant trends that impact healthcare providers. Many professionals face emotional challenges as they navigate the complexities of record-keeping, often feeling overwhelmed by administrative burdens. The integration of AI and machine learning offers a compassionate solution, transforming how records are managed and alleviating some of these pressures. For instance, hospitals adopting AI-driven SOAP note solutions have reported a remarkable 40% decrease in record-keeping time. This allows clinicians to dedicate more time to patient interactions, ultimately .
As remote consultations become increasingly common, telehealth emerges as another vital factor reshaping record-keeping practices. The need for efficient and precise documentation has never been more crucial. AI tools are being utilized to improve telehealth record-keeping, ensuring that individual records are both thorough and current—essential elements for effective care delivery. The incorporation of SOAP Note AI into telehealth services has proven beneficial, contributing to comprehensive patient records during remote consultations.
Moreover, the emphasis on interoperability among electronic health records (EHRs) is paramount. Standardized record-keeping processes enabled by AI not only enhance communication among healthcare teams but also improve clinical decision-making. With 80% of hospitals now leveraging AI to boost workflow efficiency, staying informed about these advancements is essential for providers seeking to optimize their documentation practices. However, it's important to acknowledge the ethical implications of AI in healthcare. Many providers express concerns, with 63% citing data security risks and 52% worried about potential bias in AI-powered medical decisions.
As healthcare continues to embrace these innovations, understanding the implications of AI and telehealth on the assessment SOAP note example will be vital for enhancing patient care and operational efficiency. How can we ensure that these advancements serve to support both healthcare professionals and their patients? By engaging with these technologies thoughtfully, we can create a more compassionate and efficient healthcare environment.
Conclusion
The significance of effective SOAP note documentation in healthcare is profound. Recognizing the emotional challenges faced by healthcare providers, it is essential to adopt structured formats and leverage innovative technologies to alleviate administrative burdens. This approach not only enhances documentation practices but also fosters better communication among teams, ultimately leading to improved patient care and outcomes.
Throughout this article, we explored the key components of SOAP notes, including:
- The subjective elements
- The objective elements
- Assessments
- Treatment plans
Real-world examples illustrated how these notes can guide clinical decisions, while common mistakes underscored the necessity for clarity and consistency. Moreover, the integration of AI-driven tools like CosmaNeura was emphasized as a means to streamline documentation processes, allowing providers to dedicate more time to patient interactions.
Looking ahead, embracing advancements in technology and training will be crucial for healthcare providers. By prioritizing effective documentation and continuous learning, professionals can ensure they meet the evolving demands of patient care. Engaging with these tools and practices not only enhances individual skills but also contributes to a healthcare environment that prioritizes compassion and efficiency. The commitment to high-quality SOAP notes ultimately paves the way for better healthcare experiences for both providers and patients alike.




