Overview
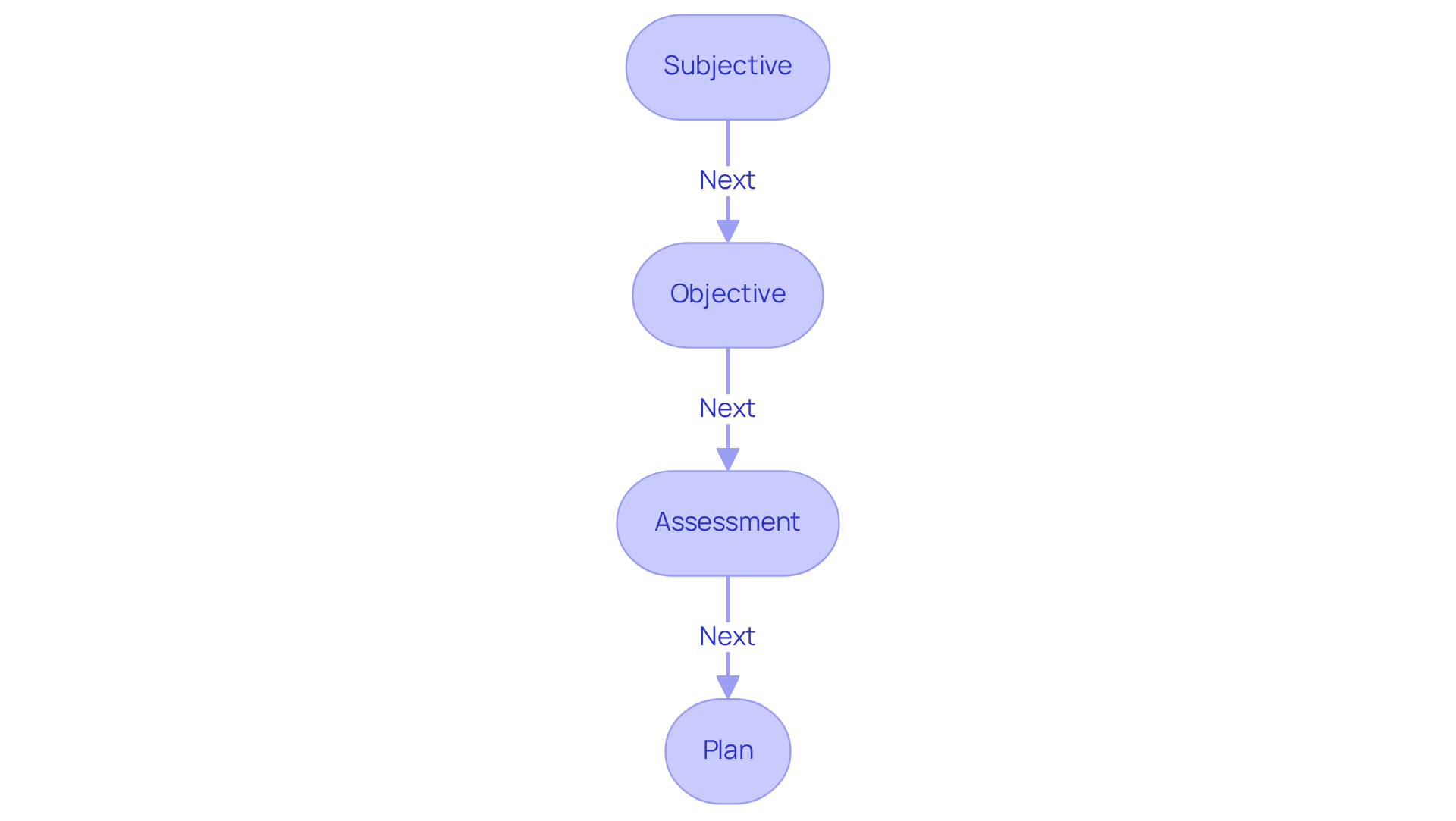
This article highlights seven examples of SOAP case notes designed to enhance effective patient documentation in healthcare settings. It begins by acknowledging the emotional challenges healthcare providers face, particularly the stress of managing administrative tasks that can detract from patient care. By detailing the structured format of SOAP notes—Subjective, Objective, Assessment, and Plan—it illustrates how these notes can streamline documentation and improve communication.
Clear communication and accurate record-keeping are crucial for improving patient care outcomes. When healthcare providers can convey information effectively, it fosters a better understanding of patient needs and enhances the overall quality of care. This structured approach not only alleviates some of the administrative burdens but also empowers providers to focus more on their patients.
Consider how implementing these SOAP notes can transform your practice. By embracing this method, you can ensure that every patient interaction is documented with clarity and precision, ultimately leading to better health outcomes. We encourage you to explore these examples further and see how they can be integrated into your daily practice, fostering a nurturing environment for both patients and providers.
Introduction
In the intricate world of healthcare, effective documentation serves as a lifeline, supporting both patient care and provider efficiency. As innovative tools like AI emerge, particularly through platforms such as CosmaNeura, healthcare professionals are uncovering new ways to ease the burdens of writing SOAP case notes. Yet, what occurs when the very structure designed to enhance communication becomes a source of confusion or error? This article explores seven compelling examples of SOAP case notes, shedding light on best practices and common pitfalls that can profoundly affect patient outcomes and the quality of care delivered.
Are you feeling overwhelmed by the demands of documentation? You're not alone. Many healthcare providers grapple with the administrative burdens that can detract from the time spent with patients. By addressing these challenges head-on, we can foster an environment that prioritizes patient care. Join us as we delve into these examples, aiming to inspire and equip you with insights that will enhance your practice.
CosmaNeura: Streamline SOAP Note Documentation with AI
In today's fast-paced healthcare environment, many providers face the emotional challenge of overwhelming paperwork. CosmaNeura's AI platform provides a compassionate solution by automating the creation of SOAP case notes example, significantly reducing the time spent on administrative tasks. This allows healthcare professionals to devote more energy to patient interactions, enhancing the overall quality of care.
Imagine a world where notes are not only precise but also comply with healthcare regulations effortlessly. By integrating AI into the record-keeping process, providers can ensure that their documentation meets these essential standards. This not only alleviates stress but also for both clinicians and patients.
Moreover, the platform's ability to align with the principles of faith-oriented providers reinforces its commitment to ethical standards. By prioritizing compassion and understanding, CosmaNeura empowers healthcare professionals to focus on what truly matters—their patients.
Are you ready to transform your practice and enhance patient care? Embrace the future of healthcare with CosmaNeura's AI platform and experience the benefits of streamlined documentation firsthand.
Therapy SOAP Note Example: Best Practices for Clinicians
A well-structured SOAP case notes example is essential for effective documentation practices that truly support both clients and healthcare providers.
Subjective: "Client reports feeling anxious most days, particularly in social situations."
Objective: "Client appeared restless during the session, with a heart rate of 90 bpm."
Assessment: "The client's anxiety appears to be impacting their daily functioning, particularly in social settings. This assessment synthesizes both subjective and objective data to provide clinical judgment."
Plan: "Continue cognitive-behavioral therapy sessions weekly, introduce relaxation techniques, and monitor progress."
This soap case notes example highlights the necessity of using clear and concise language while documenting both subjective experiences and objective observations. Have you considered how effective record-keeping can enhance communication among healthcare providers? It not only ensures compliance with industry standards but also ultimately improves patient care.
Recognizing that the structured format has been utilized in healthcare records since the 1970s is crucial. Including direct quotes from clients in the Subjective section not only reflects their viewpoint but also significantly improves the quality of records. Moreover, adapting session records to various settings—such as personal therapy, group therapy, and telehealth appointments—is essential for thorough record-keeping.
Legal and ethical factors in progress documentation are also vital. They ensure compliance and safeguard both the provider and the client. Together, we can create a more compassionate and that truly serves the needs of our clients.
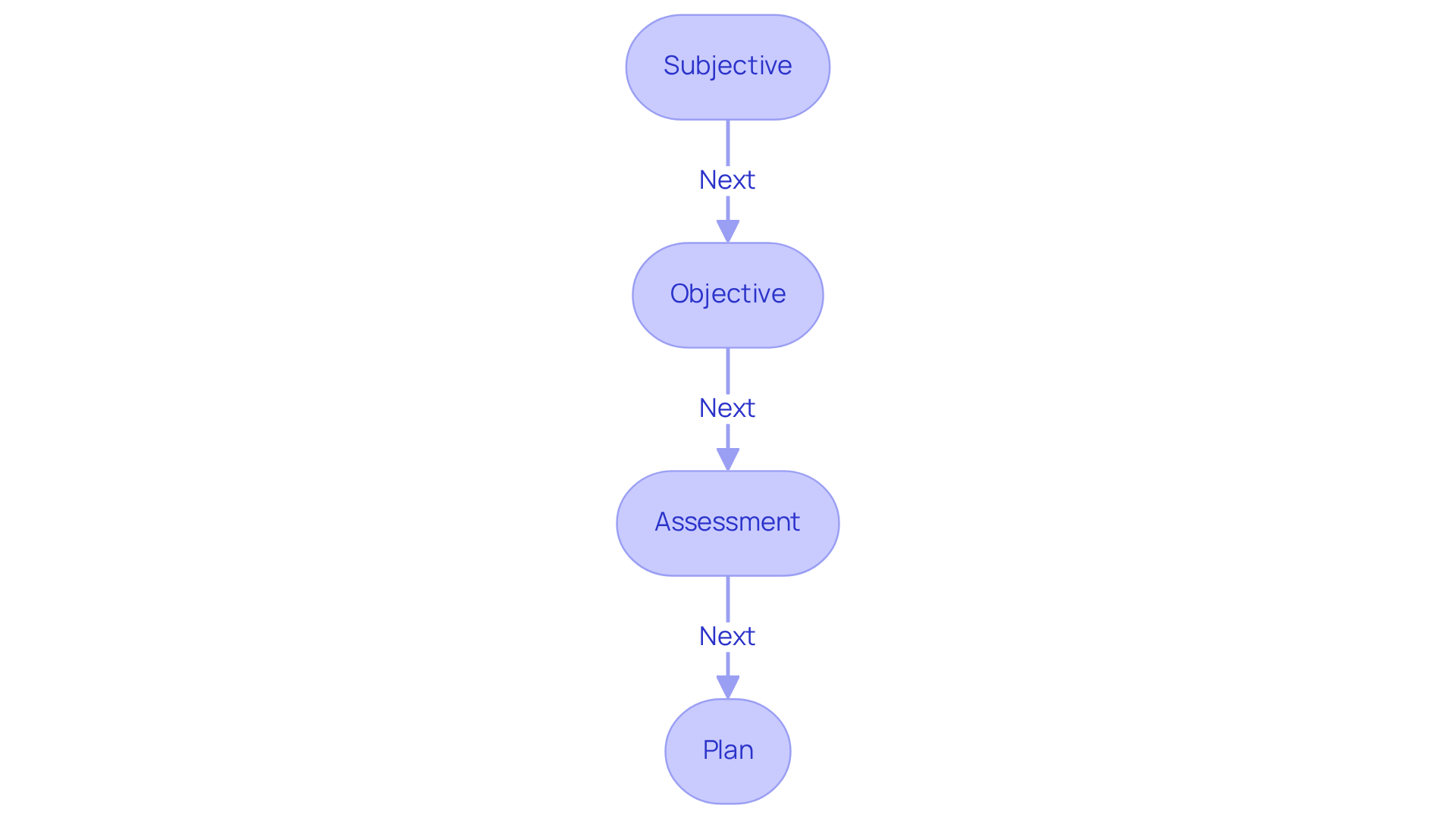
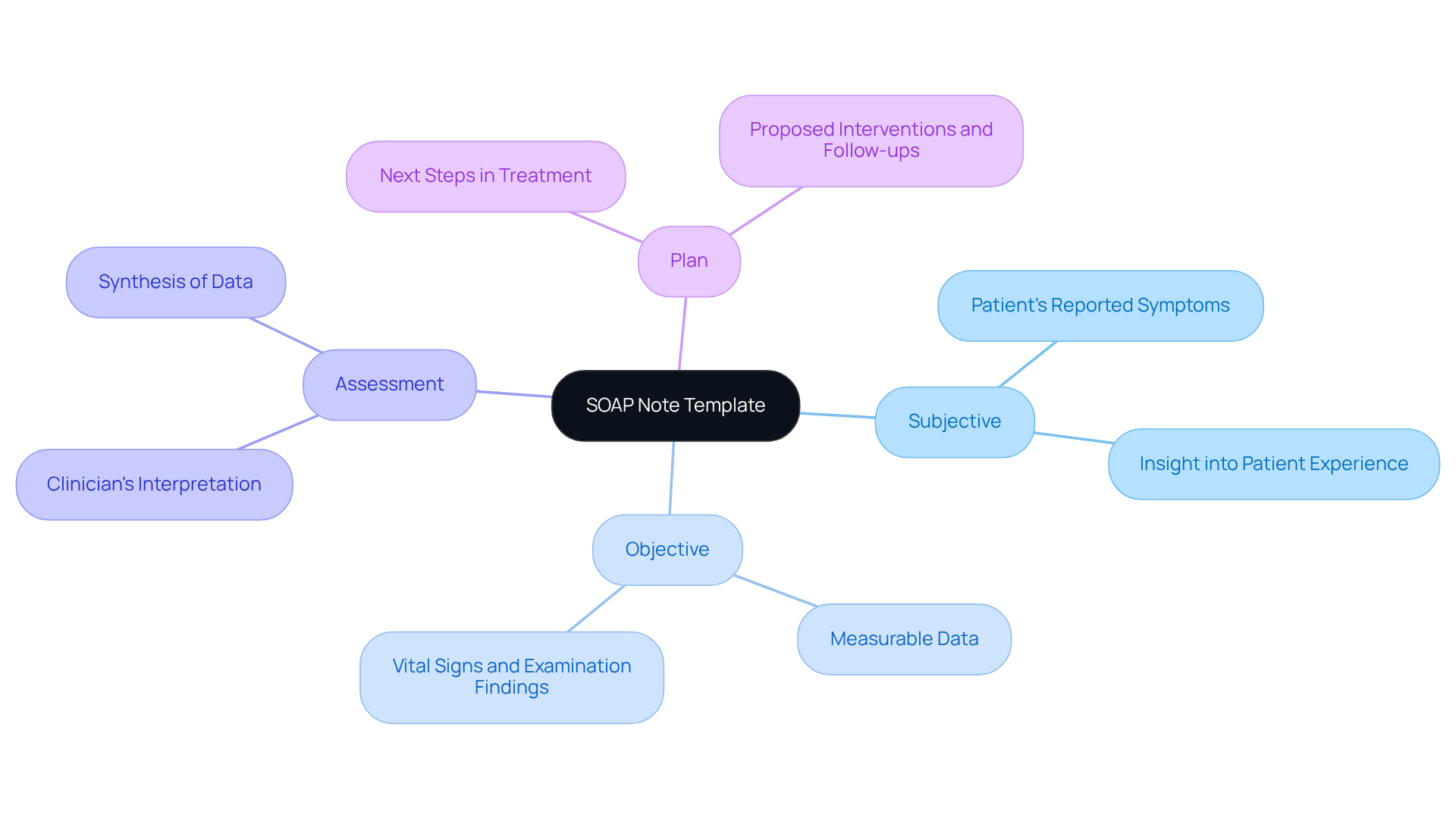
SOAP Note Template: Ensuring Consistency in Patient Records
Using a can significantly ease the recording process, ensuring that essential information is consistently captured. Have you ever felt overwhelmed by the administrative demands of healthcare? A well-structured template addresses this concern, including the following components:
- Subjective: This section captures the patient's reported symptoms and concerns, providing insight into their experience.
- Objective: In the soap case notes example, measurable data such as vital signs and physical examination findings are documented, offering a factual basis for assessment.
- Assessment: Clinicians interpret the subjective and objective data in this section, synthesizing information to form a clinical judgment, as illustrated in a soap case notes example.
- Plan: This outlines the next steps in treatment, including proposed interventions, follow-up appointments, and a soap case notes example to document the process.
Research indicates that without structured templates, medical records can suffer from significant errors. In fact, studies show that record quality can improve by up to 30% when using standardized formats. By following a structured documentation format, healthcare professionals can systematically gather all essential information, thus reducing the chance of missing vital details. It’s heartening to note that specialist views support the uniformity of SOAP case notes example, emphasizing that consistent recording practices not only enhance communication among healthcare teams but also improve overall care results.
Integrating AI tools, like natural language processing software for data entry and machine learning algorithms for analyzing health data, can further enhance these advantages. Imagine being able to focus more on your interactions with clients instead of getting bogged down by paperwork. Moreover, clinical records offer legal safeguarding through precise recording, which is crucial in healthcare environments, ensuring that both care for individuals and administrative effectiveness are emphasized. To truly enhance these benefits, healthcare providers are encouraged to adopt AI-powered documentation solutions alongside standardized clinical records. Together, we can make a difference in patient care.
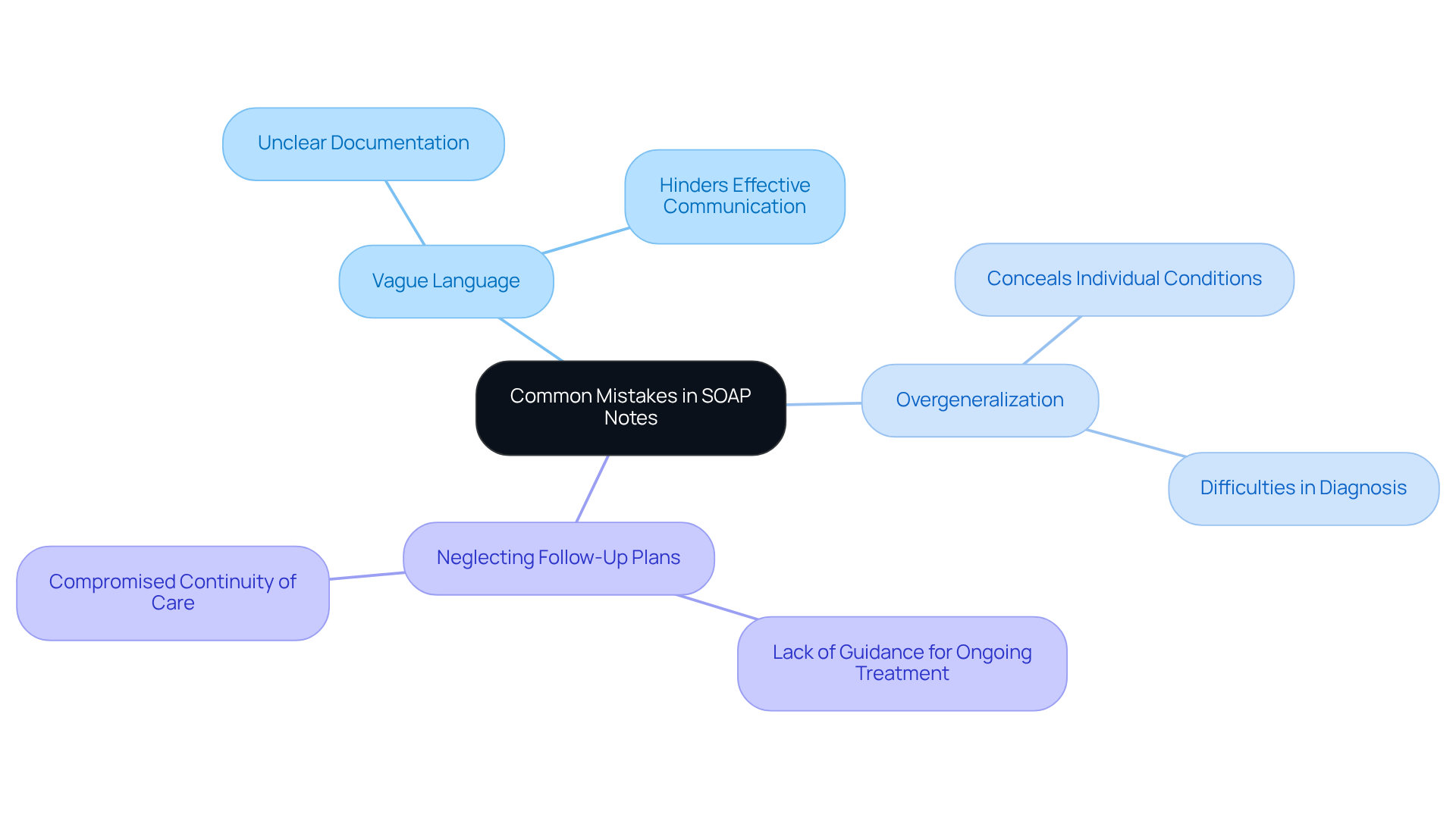
Common Mistakes in SOAP Notes: What to Avoid for Better Care
Common errors in the soap case notes example can significantly impact client care, creating emotional challenges for healthcare providers. It's crucial to recognize key pitfalls that can lead to misunderstandings and compromise patient safety. For instance, vague language can result in unclear documentation, hindering effective communication among providers. Have you ever felt unsure about a colleague's notes? Research shows that this lack of clarity can affect treatment efficacy.
Another common issue is overgeneralization. When detailed observations are not provided, it conceals the individual's condition, making it difficult to develop precise diagnoses and treatment strategies. An accurate, reasoned assessment is essential for robust treatment planning, as noted by expert Thomas Lore. Reflecting on your own experiences, how often have you struggled to understand a patient's needs due to insufficient details?
Neglecting follow-up plans is another concern that can hinder continuity of care. Without a , individuals may lack the necessary guidance for their ongoing treatment. Organized training on the SOAP case notes example has shown significant enhancements in the thoroughness and clarity of medical records, which is vital for efficient follow-up. Can you imagine the difference it would make for your patients if every note provided clear next steps?
By identifying and addressing these issues, healthcare providers can enhance the quality of their records, ensuring that their entries serve as trustworthy tools for efficient patient care. Utilizing resources like ICANotes can streamline the note-writing process, allowing for more accurate and efficient documentation. Let's work together to improve our practices and ultimately provide better care for our patients.
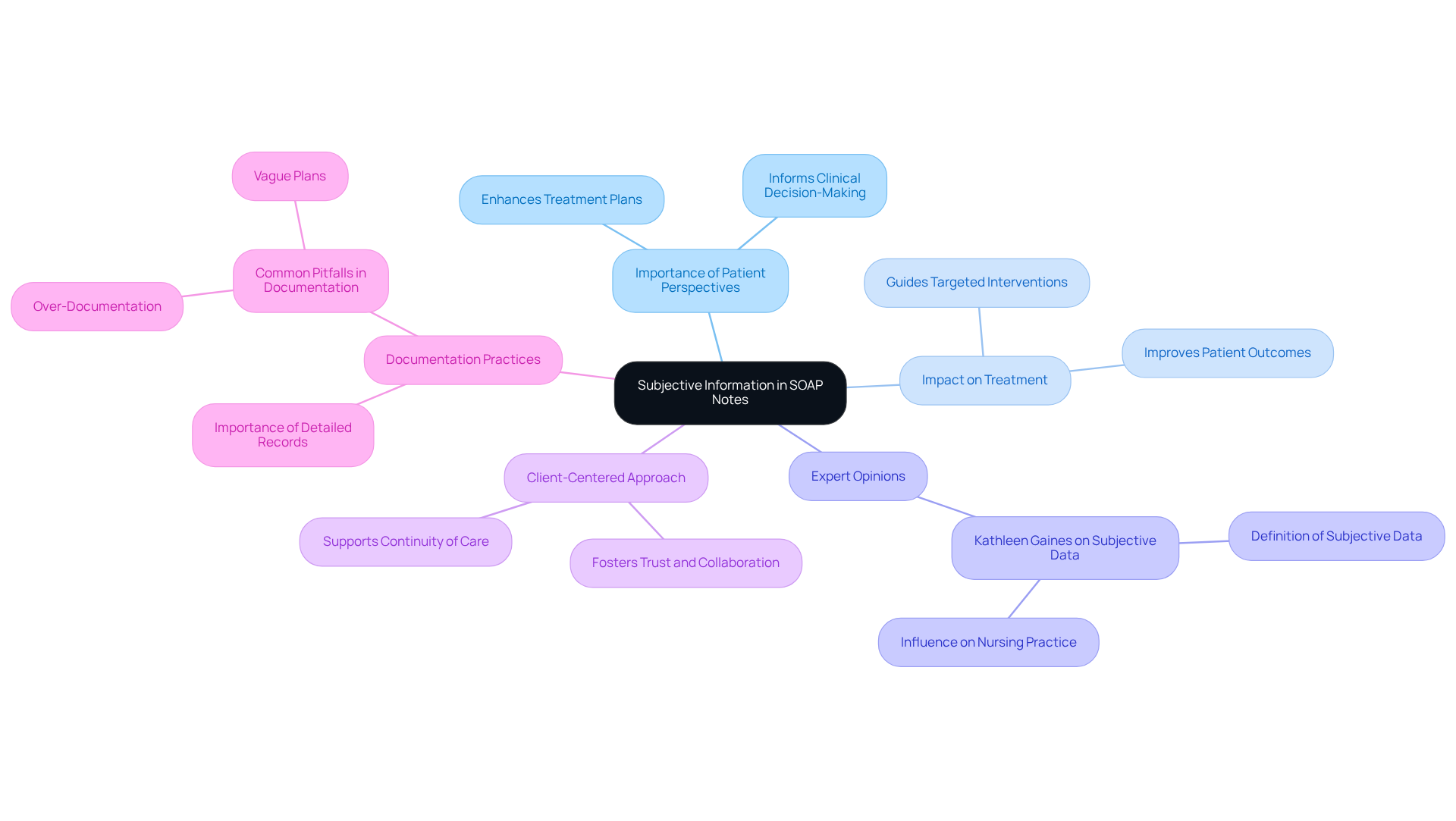
Subjective Information in SOAP Notes: Capturing Patient Perspectives
The subjective part of a SOAP note is vital for capturing the individual's own words regarding their symptoms and concerns. For instance, when someone expresses, "I feel overwhelmed and anxious when I have to go out in public," it provides essential context for the clinician's evaluation. This firsthand account not only informs the treatment plan but also aligns it with the individual's specific needs.
Integrating subjective information enhances records and promotes deeper insight into the individual's experience. Consider how this perspective can significantly impact treatment outcomes. By addressing the emotional and psychological aspects of care, healthcare providers can offer more comprehensive support. For example, in a case involving a client with heightened anxiety, the therapist noted feelings of being overwhelmed, which guided the introduction of targeted interventions like cognitive restructuring and mindfulness exercises.
Expert opinions reinforce the importance of subjective information in clinical documentation. Kathleen Gaines, a respected authority in nursing, states, 'Subjective data in nursing is the information that individuals, families, and caregivers convey.' This highlights how subjective information, such as reported symptoms, can influence clinical decision-making and treatment effectiveness. By actively listening and documenting individuals' perspectives, clinicians can enhance care quality and ensure treatment plans resonate with lived experiences.
Furthermore, capturing client viewpoints in healthcare records nurtures a client-centered approach, fostering trust and collaboration between providers and clients. This practice not only adheres to record standards but also supports continuity of care, enabling a thorough understanding of the patient's journey through the healthcare system. It's important to recognize that clinical records typically vary from two to four paragraphs in length, underscoring the need for detailed documentation that captures extensive subjective information.
Ultimately, in SOAP case notes is essential for delivering effective, empathetic, and personalized care. However, clinicians should remain mindful of potential pitfalls in documentation, such as over-documentation or vague plans, which can detract from the clarity and usefulness of the records. By focusing on the individual's voice, we can truly enhance the quality of care provided.
Objective Data in SOAP Notes: Documenting Measurable Outcomes
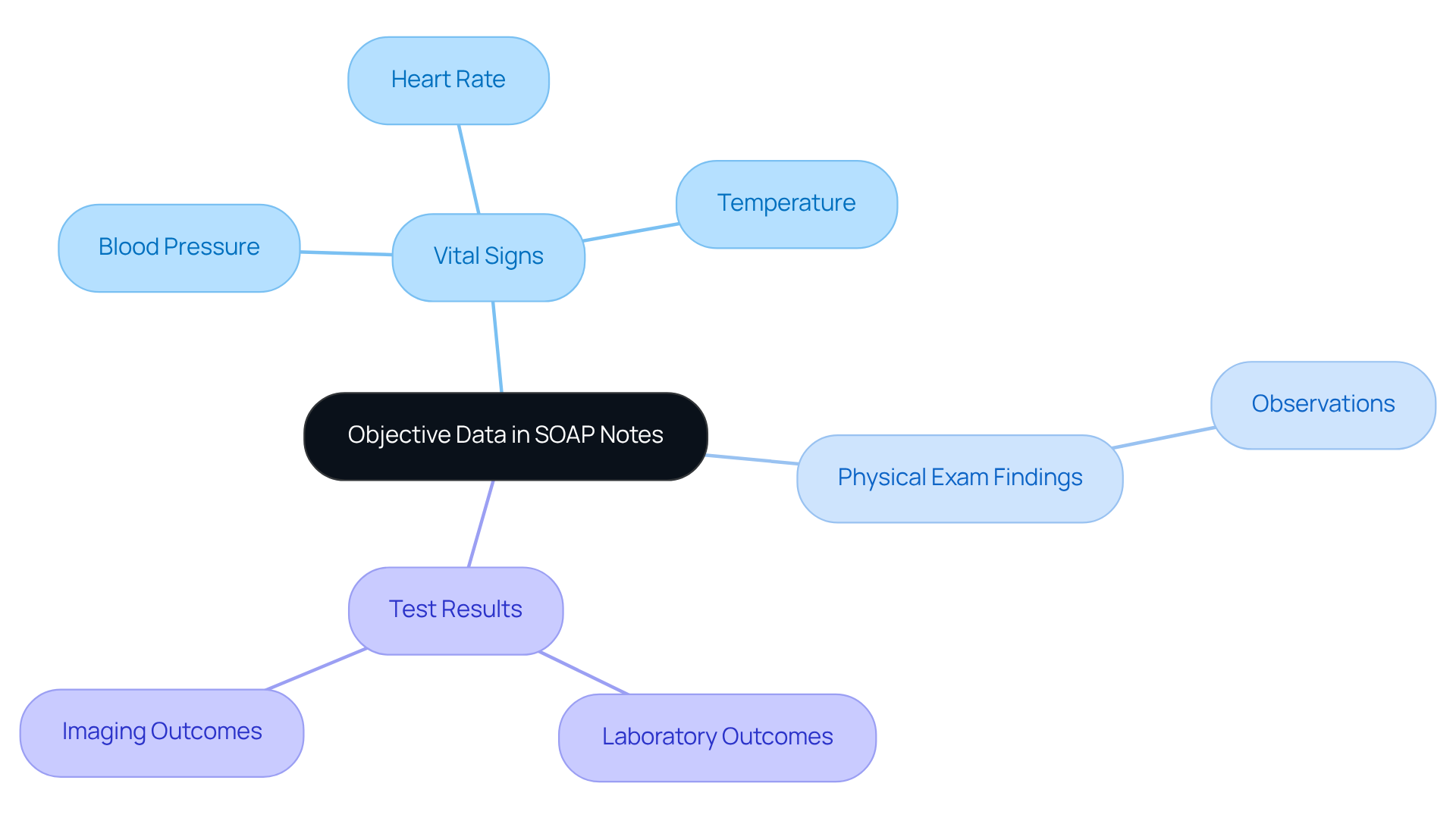
In the objective section, it is essential to include measurable data that can provide clarity and support in patient care. Consider these vital components:
- Vital Signs: Blood pressure, heart rate, temperature.
- Physical Exam Findings: Observations made during the examination.
- Test Results: Laboratory or imaging outcomes pertinent to the individual's condition.
For instance, a clinician might document: "Blood pressure 120/80, heart rate 72 bpm, and no abnormalities noted during the physical exam." This not only supports the clinician's assessment but also serves as a foundation for understanding the patient's needs. Remember, each piece of information contributes to a comprehensive view of the patient's health, allowing for more informed decisions and compassionate care.
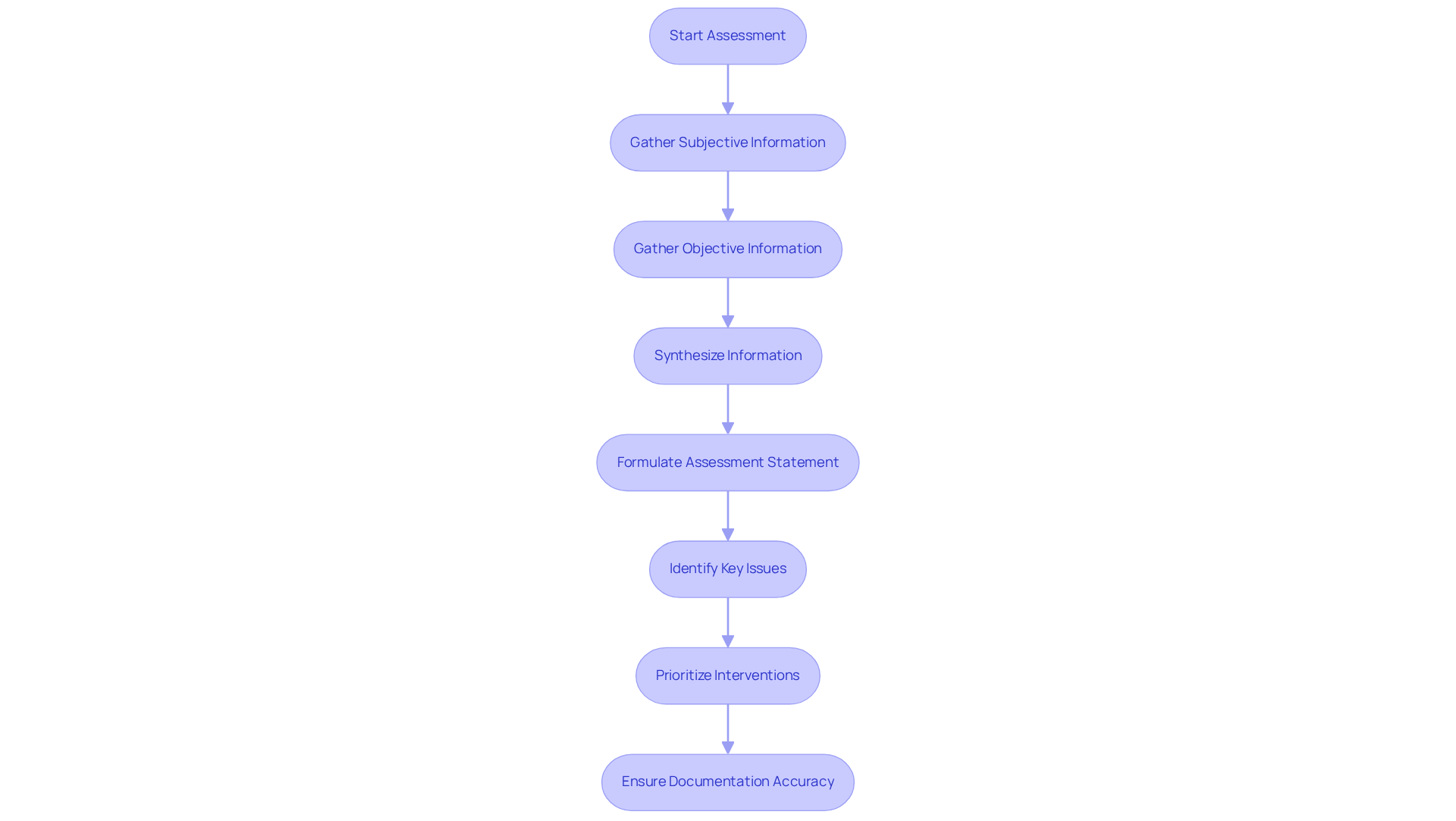
Assessment in SOAP Notes: Synthesizing Patient Information
In the assessment section of SOAP notes, clinicians synthesize information from both the subjective and objective components, forming a comprehensive understanding of the individual's condition. This synthesis is not merely a formality; it is essential for creating an tailored to the individual's unique needs. For example, an assessment statement might read: "The individual exhibits signs of generalized anxiety disorder, as evidenced by reported symptoms and observed behaviors during the session."
Accurate assessments significantly impact treatment outcomes. Have you ever considered how incomplete or erroneous documentation can affect patient care? Research indicates that 36.8% of clinical records are missing vital signatures, and only 27.4% accurately document symptoms. Such deficiencies can lead to miscommunication among healthcare providers and hinder the delivery of optimal care. Moreover, the relationship between evaluation and strategy elements in clinical documentation underscores the importance of comprehensive assessments, as highlighted by a slight correlation discovered in research (r=0.226, p=0.028).
Healthcare experts emphasize that the assessment phase is crucial for effective treatment planning. It allows clinicians to identify the most pressing issues and prioritize interventions accordingly. By ensuring that assessments are precise and thorough, healthcare providers can improve the quality of care offered, ultimately leading to better outcomes for individuals.
As a best practice, clinicians should double-check the assessment component before finalizing the SOAP case notes example to ensure completeness and accuracy.
Key Solutions for Effective Assessments:
- Ensure thorough documentation to prevent miscommunication.
- Regularly review and update clinical records for accuracy.
- Foster open communication among healthcare providers.
By embracing these practices, we can enhance the care we provide and support our patients more effectively.
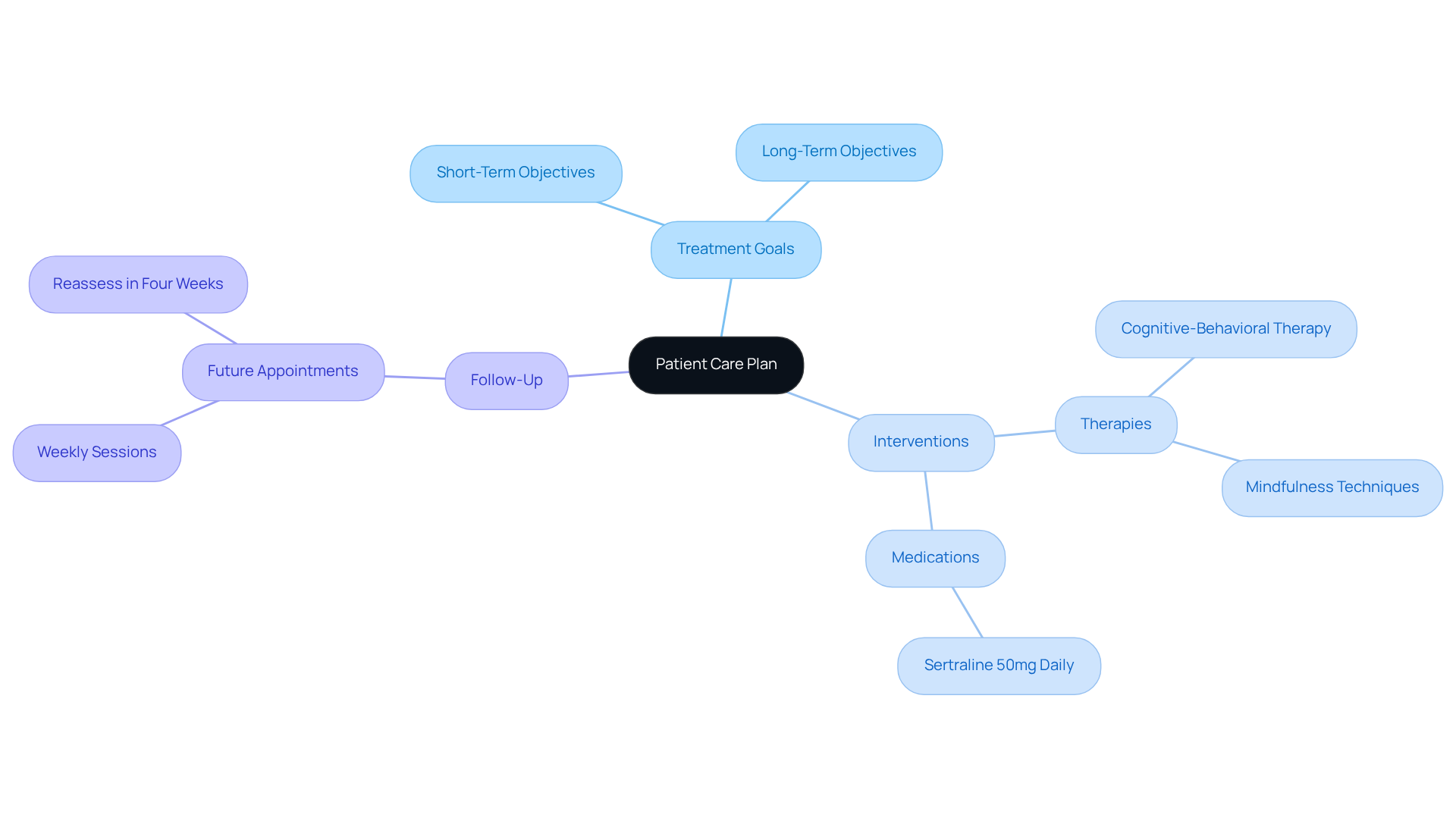
Plan in SOAP Notes: Outlining Next Steps in Patient Care
In this section, we will outline the next steps in your patient's care, focusing on clarity and collaboration:
- Treatment Goals: Establishing both short- and long-term objectives that guide the healing journey.
- Interventions: Identifying specific therapies or medications that will be utilized to support recovery.
- Follow-Up: Planning the schedule for future appointments or assessments to ensure continuous care.
For example, consider this approach: Continue [cognitive-behavioral therapy](https://cosmaneura.com/newsroom1/tag/Healthcare+Trends) sessions weekly, introduce mindfulness techniques, and reassess in four weeks. This level of clarity not only enhances the treatment plan but also fosters active involvement from the individual, empowering them on their path to well-being.
Medication Management SOAP Note Example: Documenting Pharmacological Care
An effective medication management SOAP note is not just a record; it is a vital component of compassionate pharmacological care. Consider this example:
- Subjective: "Patient reports adherence to medication but continues to experience anxiety."
- Objective: "Patient's blood pressure remains stable at 120/80."
- Assessment: "Current medication may not sufficiently address anxiety symptoms, indicating a need for reevaluation."
- Plan: "Adjust medication dosage and schedule a follow-up appointment in two weeks to assess progress."
This example illustrates the importance of capturing both the individual's subjective experience and the objective clinical response to medications, as seen in a . Have you ever considered how precise documentation can foster effective communication among healthcare providers? It is essential for improving safety for individuals receiving care.
Research shows that nearly 10% of individuals in hospital environments experience medication errors. This statistic highlights the pressing need for meticulous record-keeping. By documenting pharmacological care thoroughly, you can enhance outcomes for individuals, ensuring that treatment aligns with their specific needs and reduces the risk of adverse drug events. Let’s commit to this practice, as it not only supports our patients but also strengthens our role as caregivers.
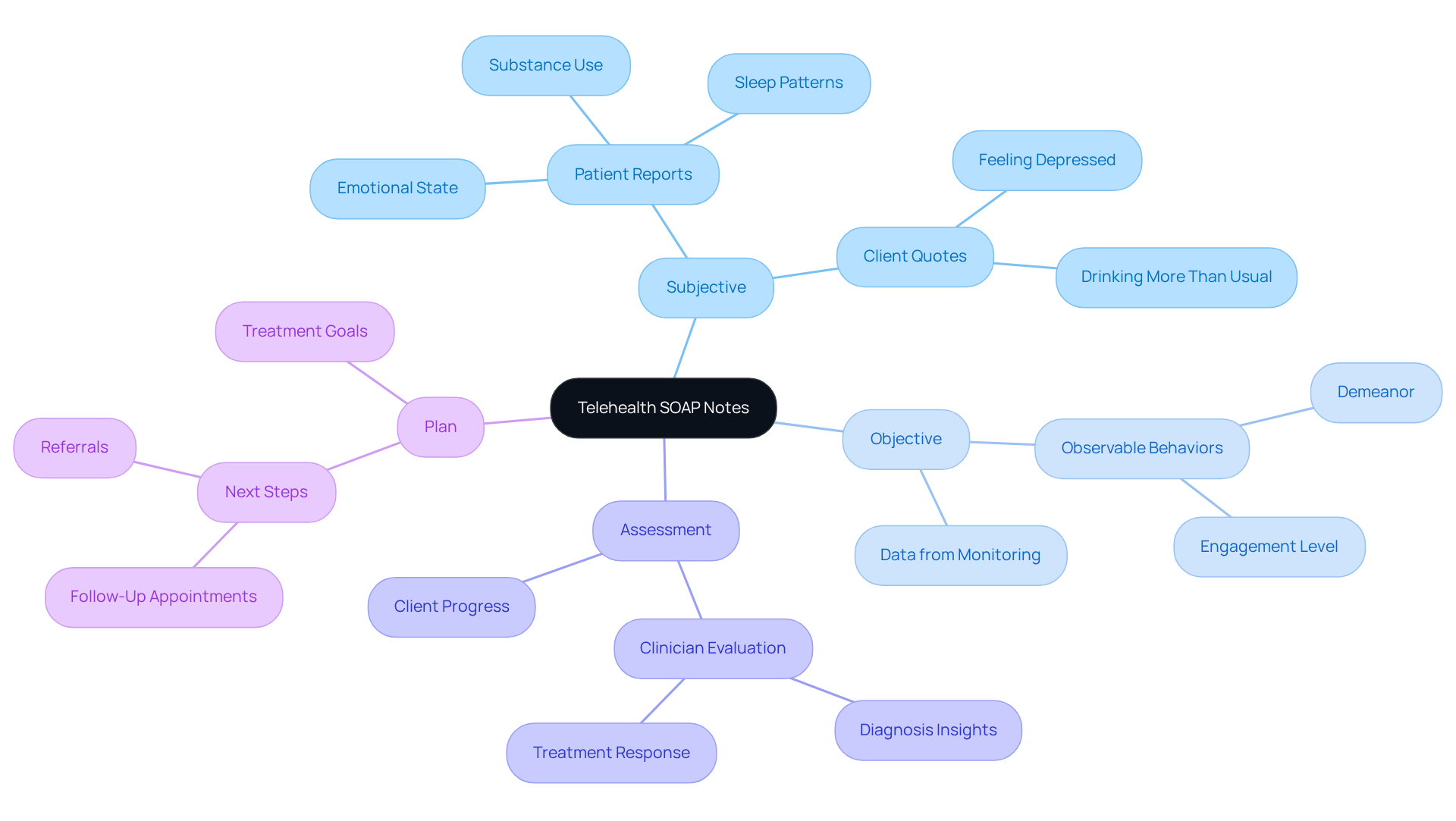
Telehealth SOAP Notes: Adapting Documentation for Remote Care
Documenting telehealth sessions can feel overwhelming, but by using a [SOAP case notes example](https://cosmaneura.com) effectively, this process can be transformed into a tool for clear and compassionate communication. Each section of the SOAP case notes example should be thoughtfully tailored to reflect the unique aspects of remote care.
- Subjective: Capture the patient's verbal reports during the session, emphasizing their feelings and concerns. For instance, an individual might express, "I've been feeling more anxious lately." This insight is crucial for understanding their emotional state.
- Objective: Document observable behaviors during the video consultation, such as the individual's demeanor and level of engagement. Noting signs like fidgeting or difficulty maintaining eye contact can provide valuable context for their experience.
- Assessment: Offer a clinician's evaluation based on the remote interaction, synthesizing the subjective and objective data to inform clinical decisions. For example, the evaluation might conclude that the individual is experiencing heightened anxiety, which can guide future interventions.
- Plan: Clearly outline the next steps, including any referrals or follow-up appointments. An effective plan could state, "Refer to a psychiatrist for medication evaluation and schedule a follow-up in one month," ensuring continuity of care.
This structured approach not only enhances the quality of telehealth documentation but also acts as a , ensuring that critical information is accurately recorded. Ultimately, this can improve patient engagement and outcomes. By adapting SOAP notes to the telehealth environment, providers can maintain high standards of care while navigating the challenges of remote interactions. How can you implement these strategies in your practice to foster a more supportive experience for your patients?
Conclusion
Effective documentation through SOAP case notes is not merely a routine task; it is a vital part of delivering quality patient care. Have you ever felt overwhelmed by administrative burdens? By utilizing structured formats and embracing innovative tools like CosmaNeura's AI platform, healthcare providers can streamline their documentation processes. This allows more time for meaningful patient interactions rather than getting lost in paperwork. Such a shift enhances not only the clarity and accuracy of records but also fosters a more compassionate healthcare environment.
Throughout this article, we have shared key insights regarding best practices for writing SOAP notes. Capturing both subjective and objective data is essential, as is conducting thorough assessments and crafting clear plans. Have you ever encountered miscommunication due to vague documentation? Common mistakes in documentation have been highlighted, emphasizing the need for precise language and detailed observations to avoid such pitfalls and ensure continuity of care. By adhering to these guidelines, healthcare professionals can significantly enhance the quality of their documentation.
Ultimately, your commitment to effective SOAP note practices is crucial for improving patient outcomes and fostering trust between providers and clients. As the healthcare landscape continues to evolve, embracing technology and structured documentation methods will empower you to deliver more personalized and effective care. It is time to prioritize these practices—not only for compliance but also to enhance the overall patient experience. Together, let’s make a difference in how we care for our patients.




