Overview
This article addresses the emotional challenges faced by EMS providers, particularly in the realm of documentation. Many providers experience stress and frustration due to the administrative burdens that come with their vital work. By enhancing documentation skills through the use of SOAP (Subjective, Objective, Assessment, Plan) notes, we can alleviate some of this pressure.
Mastering the SOAP format not only improves patient care but also fosters better communication among healthcare professionals. It helps to streamline processes, ultimately reducing the administrative load that can lead to burnout. Imagine a workplace where providers feel more supported, leading to better health outcomes for patients and a more fulfilling experience for the providers themselves.
Consider how adopting effective documentation practices can transform your daily routine. What if you could spend less time on paperwork and more time focusing on patient care? By integrating these techniques, you can take a significant step towards enhancing your professional satisfaction.
In conclusion, we encourage you to explore the benefits of SOAP notes further. By investing time in mastering this documentation format, you not only improve your own experience but also contribute positively to the healthcare environment as a whole. Together, we can work towards a more supportive and effective healthcare system.
Introduction
In the high-stakes environment of emergency medical services (EMS), the emotional toll on healthcare providers can be significant. Effective documentation is not just a task; it’s paramount to ensuring quality patient care. The SOAP note format—comprising Subjective, Objective, Assessment, and Plan—serves as a vital tool for EMS providers to communicate critical information clearly and efficiently. Yet, the challenge of managing extensive data while maintaining accuracy can often feel overwhelming, even for the most seasoned professionals.
What if there were ways to enhance these documentation skills, streamline processes, and ultimately improve patient outcomes? This article explores seven compelling examples of SOAP EMS notes that not only showcase best practices but also highlight innovative tools and techniques. Together, we can elevate documentation standards in the field, fostering a more supportive environment for both providers and patients.
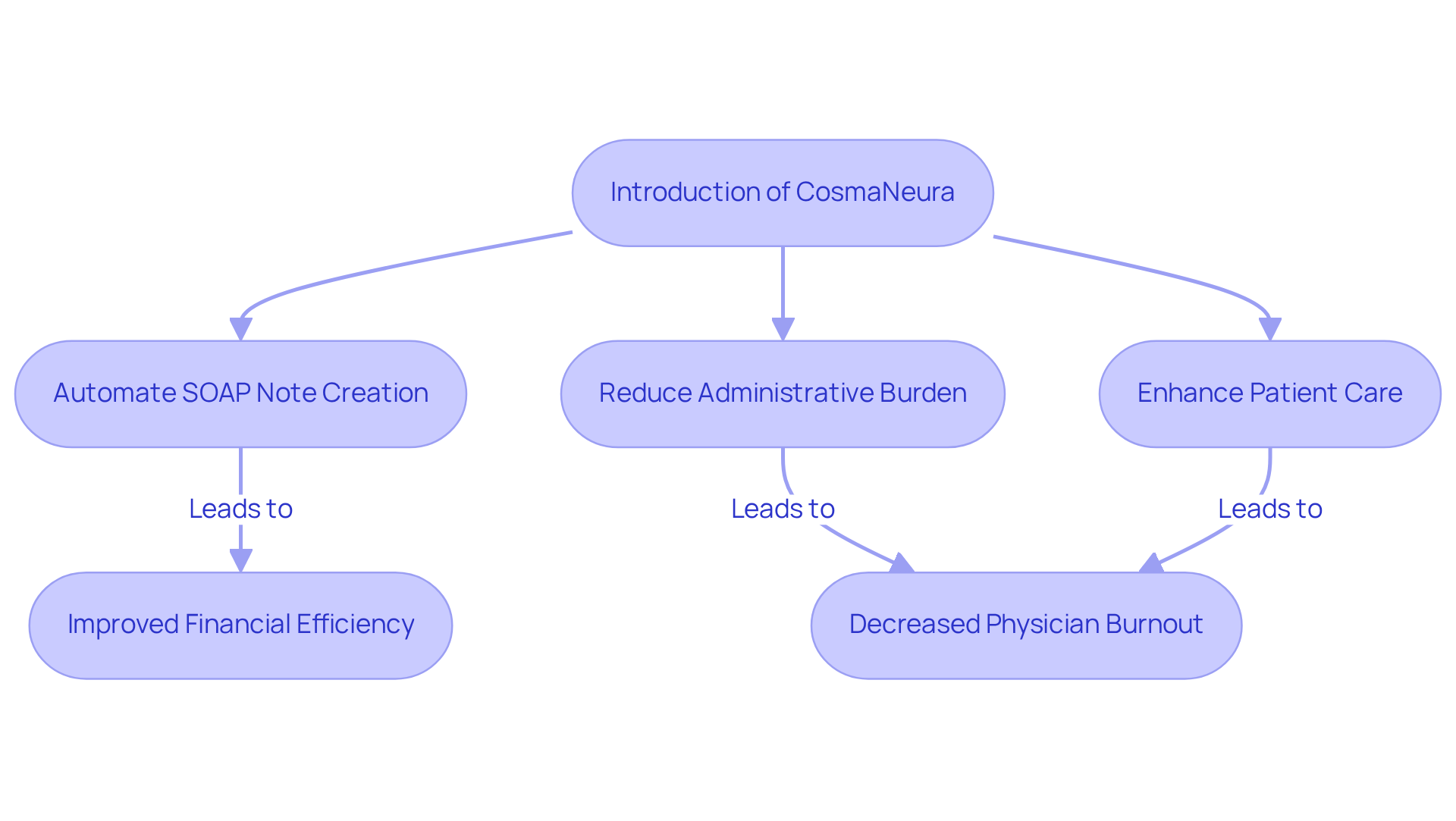
CosmaNeura: AI-Driven SOAP Note Automation for EMS Providers
In the demanding world of healthcare, EMS providers often face overwhelming challenges, particularly with rising costs and financial burdens. CosmaNeura understands these emotional strains and leverages advanced AI technology to automate the creation of a SOAP EMS example. This innovative solution not only saves precious time but also ensures that essential client information is accurately captured, ultimately enhancing financial efficiency.
By alleviating administrative burdens, EMS professionals can focus more on what truly matters: patient care. This shift is crucial in easing physician burnout and fostering meaningful face-to-face interactions. Imagine the difference this could make in your daily practice, allowing you to dedicate more time to your patients and their needs.
At CosmaNeura, we are committed to enhancing clinical experiences while adhering to ethical standards. Join us in this mission to create a more compassionate healthcare environment where providers can thrive, and patient care is prioritized. Together, we can make a in the lives of both healthcare providers and the communities they serve.
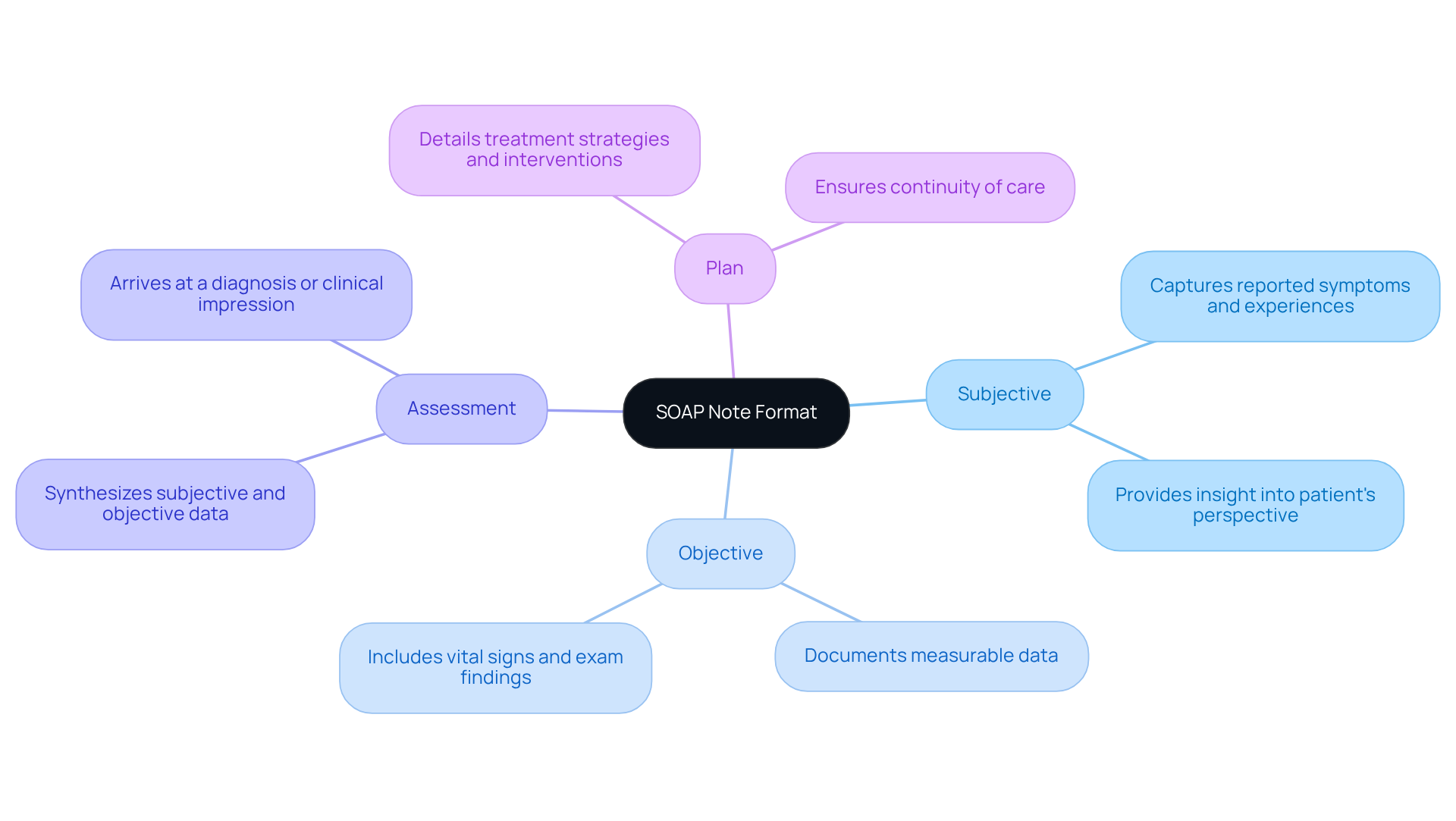
SOAP Note Format: Key Components for Effective EMS Documentation
The SOAP note format is structured around four essential components: Subjective, Objective, Assessment, and Plan. Each of these serves a distinct purpose in effective EMS documentation, and understanding them can significantly ease the burdens faced by healthcare providers.
- Subjective: This section captures the individual's reported symptoms, concerns, and experiences, offering crucial insight into their perspective. For example, an individual might express increased anxiety or difficulty sleeping. Recognizing these feelings is vital for understanding their condition and supporting their needs.
- Objective: Here, measurable data is documented, including vital signs, physical exam findings, and relevant diagnostic information. This objective data forms the foundation for , ensuring that every action taken is informed and precise.
- Assessment: This component synthesizes the subjective and objective information to arrive at a diagnosis or clinical impression. It reflects the clinician's expertise and rationale, ensuring that the assessment is grounded in the documented evidence—something that builds trust and clarity in care.
- Plan: The Plan section details the treatment strategy, encompassing interventions, follow-up actions, and any referrals essential for thorough support. A clear and actionable plan is crucial for continuity of care and effective management of clients, ensuring they feel supported throughout their journey.
Mastering the SOAP EMS example format is essential not only for compliance and efficiency but also for enhancing communication among healthcare providers, which ultimately improves patient outcomes. However, many EMS providers face challenges such as time constraints and data overload, which can hinder effective documentation. Have you ever felt overwhelmed by the sheer volume of information to manage? Consistently examining and refreshing SOAP records can help alleviate these concerns, guaranteeing that the most clinically pertinent information is easily accessible. By doing so, we can foster a more compassionate and effective care environment for everyone involved.
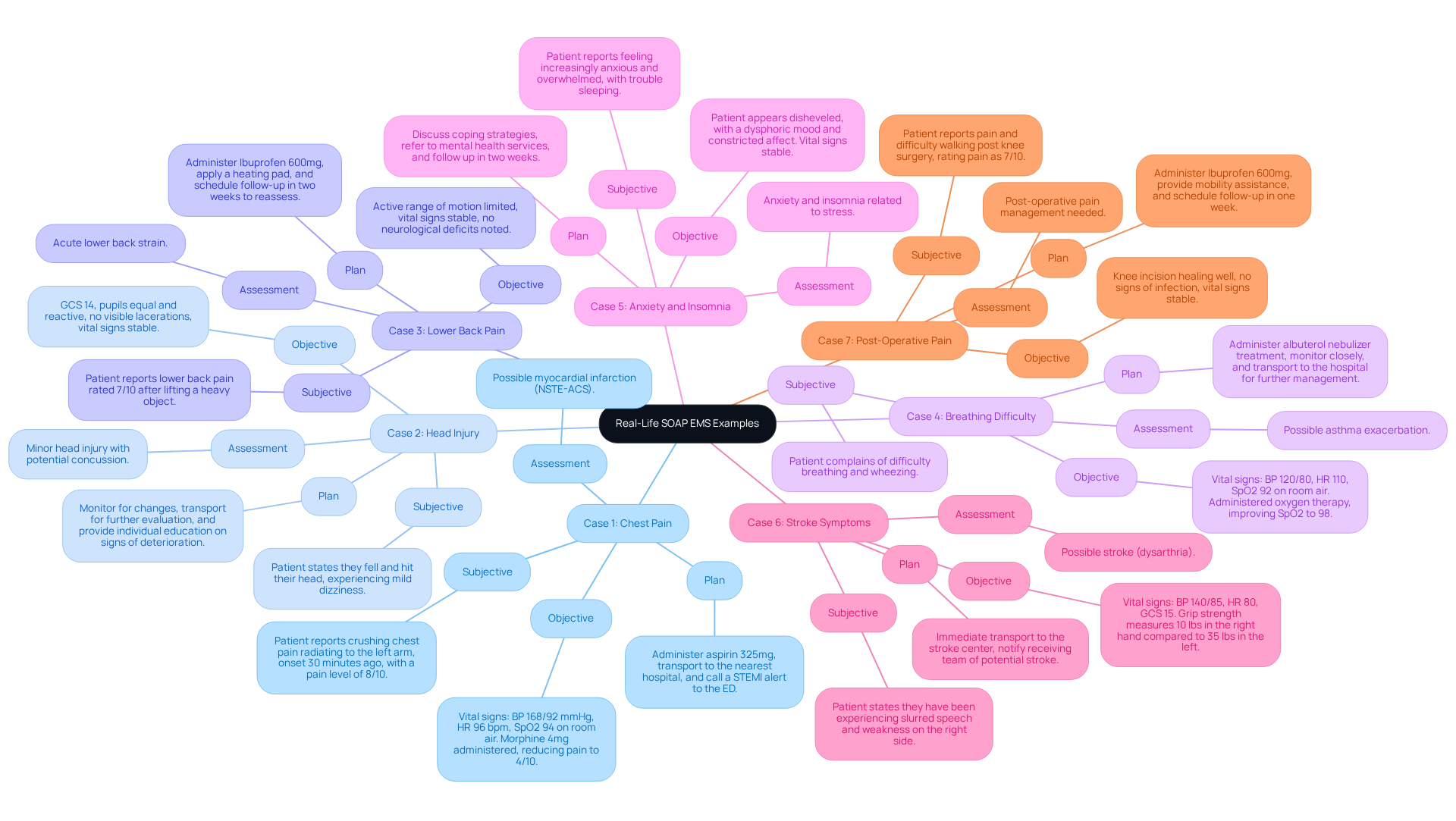
Real-Life SOAP EMS Examples: Practical Applications in Emergency Situations
In the demanding field of emergency medical services (EMS), healthcare providers often face emotional challenges that can impact patient care. Here are several real-life examples of SOAP notes that illustrate practical applications aimed at enhancing patient care through innovative solutions:
- Subjective: "Patient reports crushing chest pain radiating to the left arm, onset 30 minutes ago, with a pain level of 8/10."
Objective: Vital signs: BP 168/92 mmHg, HR 96 bpm, SpO2 94% on room air. Morphine 4mg administered, reducing pain to 4/10.
Assessment: Possible myocardial infarction (NSTE-ACS).
Plan: Administer aspirin 325mg, transport to the nearest hospital, and call a STEMI alert to the ED. - Subjective: "Patient states they fell and hit their head, experiencing mild dizziness."
Objective: GCS 14, pupils equal and reactive, no visible lacerations, vital signs stable.
Assessment: Minor head injury with potential concussion.
Plan: Monitor for changes, transport for further evaluation, and provide individual education on signs of deterioration. - Subjective: "Patient reports lower back pain rated 7/10 after lifting a heavy object."
Objective: Active range of motion limited, vital signs stable, no neurological deficits noted.
Assessment: Acute lower back strain.
Plan: Administer Ibuprofen 600mg, apply a heating pad, and schedule follow-up in two weeks to reassess. - Subjective: "Patient complains of difficulty breathing and wheezing."
Objective: Vital signs: BP 120/80, HR 110, SpO2 92% on room air. Administered oxygen therapy, improving SpO2 to 98%.
Assessment: Possible asthma exacerbation.
Plan: Administer albuterol nebulizer treatment, monitor closely, and transport to the hospital for further management. - Subjective: "Patient reports feeling increasingly anxious and overwhelmed, with trouble sleeping."
Objective: Patient appears disheveled, with a dysphoric mood and constricted affect. Vital signs stable.
Assessment: Anxiety and insomnia related to stress.
Plan: Discuss coping strategies, refer to mental health services, and follow up in two weeks. - Subjective: "Patient states they have been experiencing slurred speech and weakness on the right side."
Objective: Vital signs: BP 140/85, HR 80, GCS 15. Grip strength measures 10 lbs in the right hand compared to 35 lbs in the left.
Assessment: Possible stroke (dysarthria).
Plan: Immediate transport to the stroke center, notify receiving team of potential stroke. - Subjective: "Patient reports pain and difficulty walking post knee surgery, rating pain as 7/10."
Objective: Knee incision healing well, no signs of infection, vital signs stable.
Assessment: Post-operative pain management needed.
Plan: Administer Ibuprofen 600mg, provide mobility assistance, and schedule follow-up in one week to reassess range of motion and strength.
These examples not only demonstrate how , such as the SOAP EMS example, can improve communication and continuity of treatment in emergency situations but also highlight the importance of addressing the emotional aspects of healthcare delivery. By employing AI-driven speech recognition technology, like that provided by CosmaNeura's Agentic Platform, record-keeping time can decrease by up to 40%. This allows healthcare professionals to focus more on providing compassionate care. Incorporating established templates can further enhance the consistency and quality of EMS reports, ensuring that critical information is captured accurately and efficiently while addressing challenges like physician burnout and resistance to innovation.
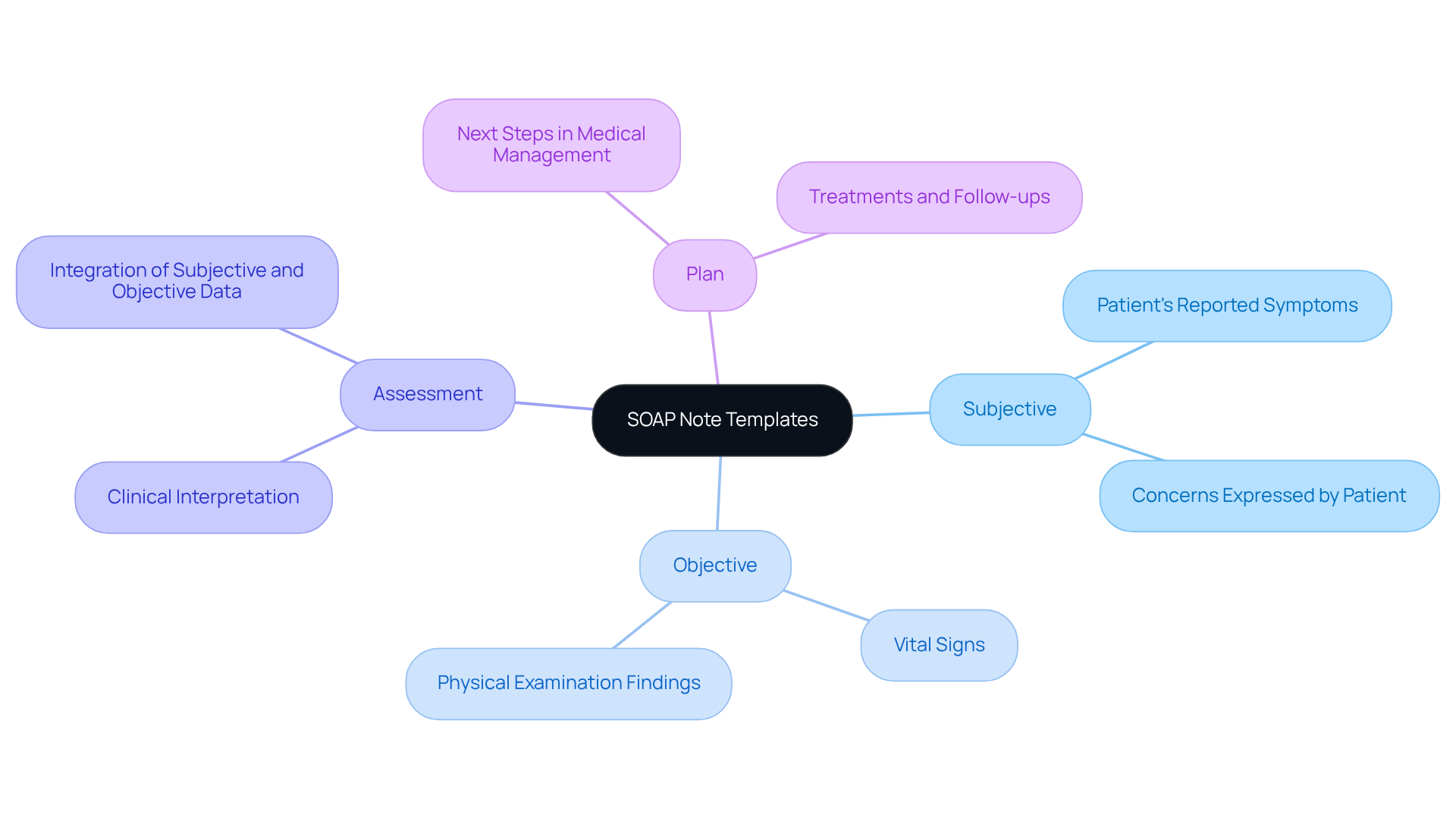
SOAP Note Templates: Streamlining Documentation for EMS Providers
Implementing [SOAP note templates](https://blog.cosmaneura.com/10-essential-np-soap-note-templates-for-efficient-documentation) can greatly alleviate the documentation burdens faced by EMS providers, particularly when enhanced by generative AI technologies. A thoughtfully structured template encompasses the following sections:
- Subjective: Capture the patient's reported symptoms and concerns.
- Objective: Document measurable data such as vital signs and physical examination findings.
- Assessment: Provide a clinical interpretation of the subjective and objective data.
- Plan: Outline the next steps in medical management, including treatments and follow-ups.
By systematically filling in each section, providers can ensure comprehensive information capture while minimizing time spent on paperwork. Have you ever considered how much time could be saved? Research indicates that employing templates can save doctors an average of three minutes per entry, leading to significant time savings across numerous interactions. For example, the average daily charting time was reduced from 30 minutes to 27 minutes when using problem-oriented templates, showcasing a clear efficiency gain.
Healthcare professionals have noted that these templates not only enhance record precision but also elevate overall treatment quality. One physician shared, "Use of evidence-based and problem-oriented templates is associated with improved note quality without significant change in total charting time." Moreover, integrating templates into electronic health records (EHRs) has been shown to reduce under-billed appointments, ensuring that providers capture all necessary billing codes effectively. This standardization is crucial for .
Integrating these workflows using a soap ems example into EMS record-keeping practices not only simplifies workflows but also promotes a more structured approach to client support. This enables providers to allocate more time to direct interactions and less to administrative duties. By utilizing AI in a soap ems example to streamline and improve the record-keeping process, providers can lessen the load of administrative tasks, ultimately enhancing health outcomes and reducing burnout. Providers are encouraged to customize templates to fit their specific workflows, enhancing their effectiveness and usability.
Furthermore, generative AI tools can assist in examining the data collected in these templates, offering insights that can lead to improved care strategies and more effective record-keeping practices. How might your practice change if you had more time to focus on patient care? Embracing these solutions could be a step towards enhancing your ability to provide compassionate care.
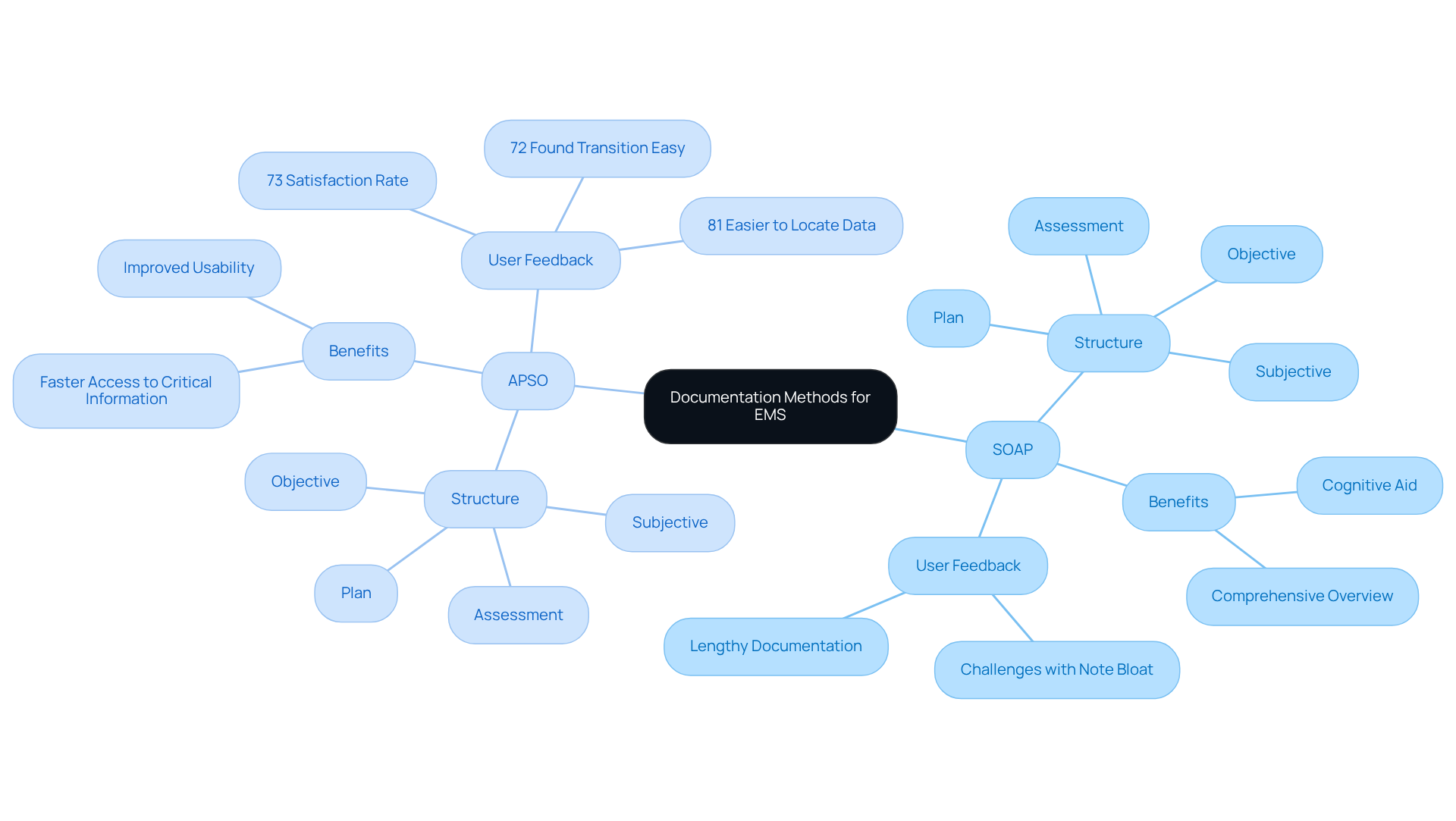
SOAP vs. APSO: Choosing the Right Documentation Method for EMS
The SOAP ems example format (Subjective, Objective, Assessment, Plan) serves as a cornerstone in EMS records, providing a structured approach that promotes a clear chronological flow of information. This organization helps providers easily track client encounters and make informed decisions. Yet, many EMS teams are exploring the (Assessment, Plan, Subjective, Objective), which places the assessment and plan sections at the forefront. This shift can greatly enhance efficiency, especially in fast-paced environments where quick access to critical information is vital.
Choosing the right format for records hinges on the specific needs of the EMS team and the nature of their interactions with individuals. For instance, the SOAP ems example offers a comprehensive overview of a patient’s condition, while APSO allows for immediate access to evaluations and strategies, which can be crucial during emergencies. A study revealed that 73% of providers expressed satisfaction with the APSO format, and 81% found it easier to locate clinically relevant data, underscoring its effectiveness in improving usability and speed in record-keeping.
In practice, EMS teams have shared varied preferences for these formats based on their operational demands. One EMS professional remarked, 'In high-pressure situations, having the assessment upfront saves valuable time and helps us focus on immediate patient needs.' This perspective reflects a broader trend among EMS providers who prioritize efficiency and clarity in record-keeping. Furthermore, the issue of 'note bloat' is particularly significant in emergency medicine, where excessive data can obstruct effective communication and decision-making.
Statistics indicate that the transition to APSO has been positively received, with 76% of providers completing the switch within six months of its introduction, and 72% finding the transition easy or very easy. This shift emphasizes the growing recognition of the need for efficient record-keeping methods in emergency medical services. Ultimately, the choice between the SOAP ems example and APSO should be guided by the specific context of healthcare, ensuring that records effectively support optimal clinical decision-making.
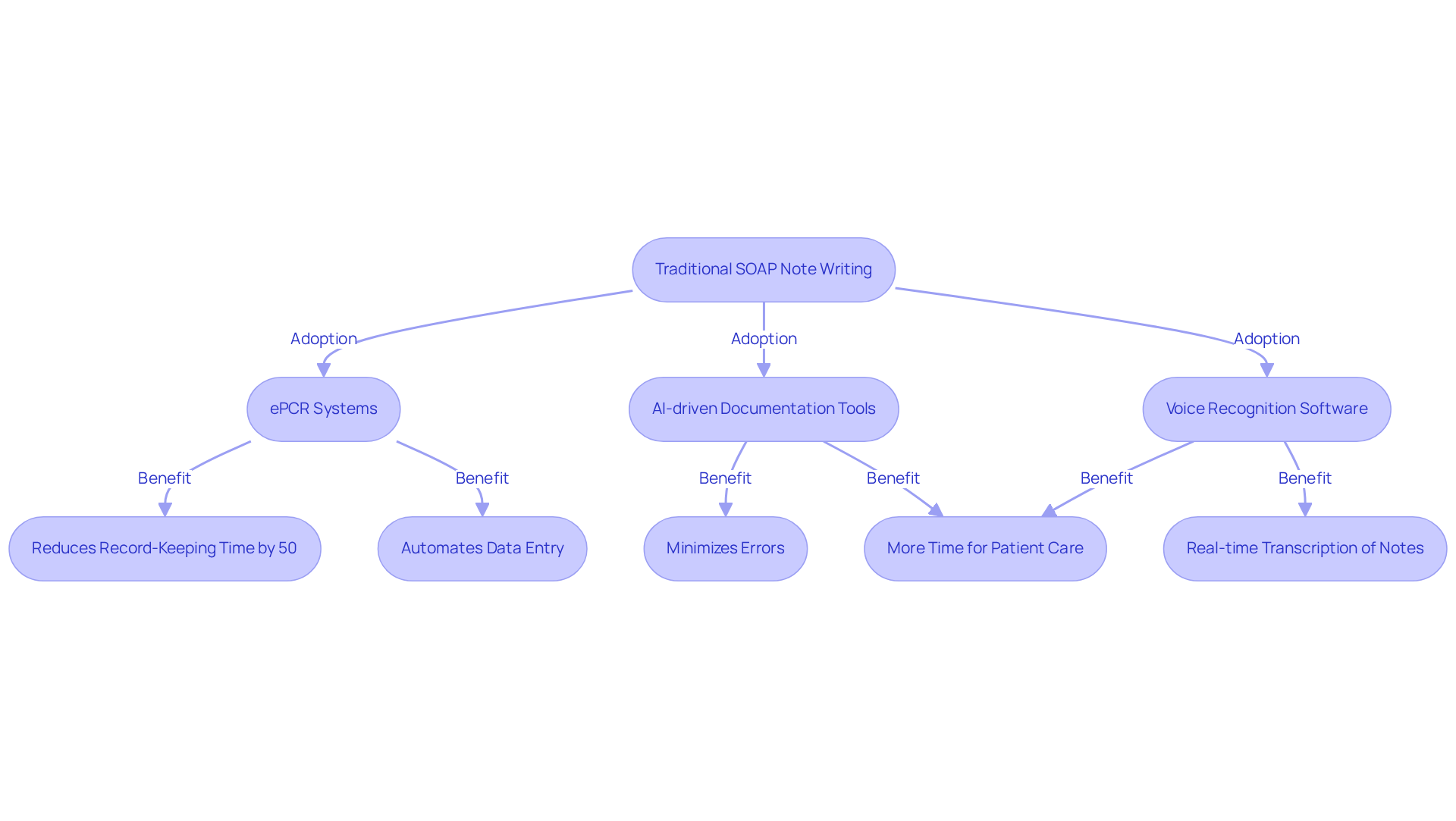
Technology Integration: Enhancing SOAP Note Writing in EMS
In the fast-paced world of healthcare, technology is transforming the way EMS providers write SOAP notes, serving as a SOAP EMS example to address the emotional and administrative challenges they face. It's crucial to recognize how overwhelming these tasks can be, often detracting from the time spent caring for patients. Fortunately, electronic health reporting (ePCR) systems are stepping in to help, automating data entry and ensuring accurate records.
Research shows that ePCR systems can reduce record-keeping time by as much as 50%. This significant improvement allows providers to dedicate more time to supporting their patients, which is what truly matters. Imagine the relief of having tools that streamline workflows while tackling broader healthcare challenges like limited access to services and rising costs.
AI-driven documentation tools, such as voice recognition software, are enhancing the documentation process by enabling real-time transcription of verbal notes into a SOAP EMS example format. This not only minimizes errors but also supports providers in their daily tasks. For instance, Priority Physicians recovered $16,000 in lost clinical time after implementing AI tools like Heidi, showcasing the financial benefits of embracing these innovations.
Dr. Shelagh Fraser's experience further illustrates this point; she reported a remarkable reduction in note-writing time from 2-2.5 hours to around 40 minutes per day with Heidi. Such efficiency gains are not just numbers—they represent more time for patient care and connection.
As leaders in healthcare technology emphasize, these advancements are vital for enabling EMS professionals to focus on what they do best: providing outstanding service. The SOAP EMS example, which was developed to in healthcare environments, continues to be a cornerstone in this evolving landscape of care. By embracing these tools, we can foster a more compassionate and efficient healthcare system for everyone.
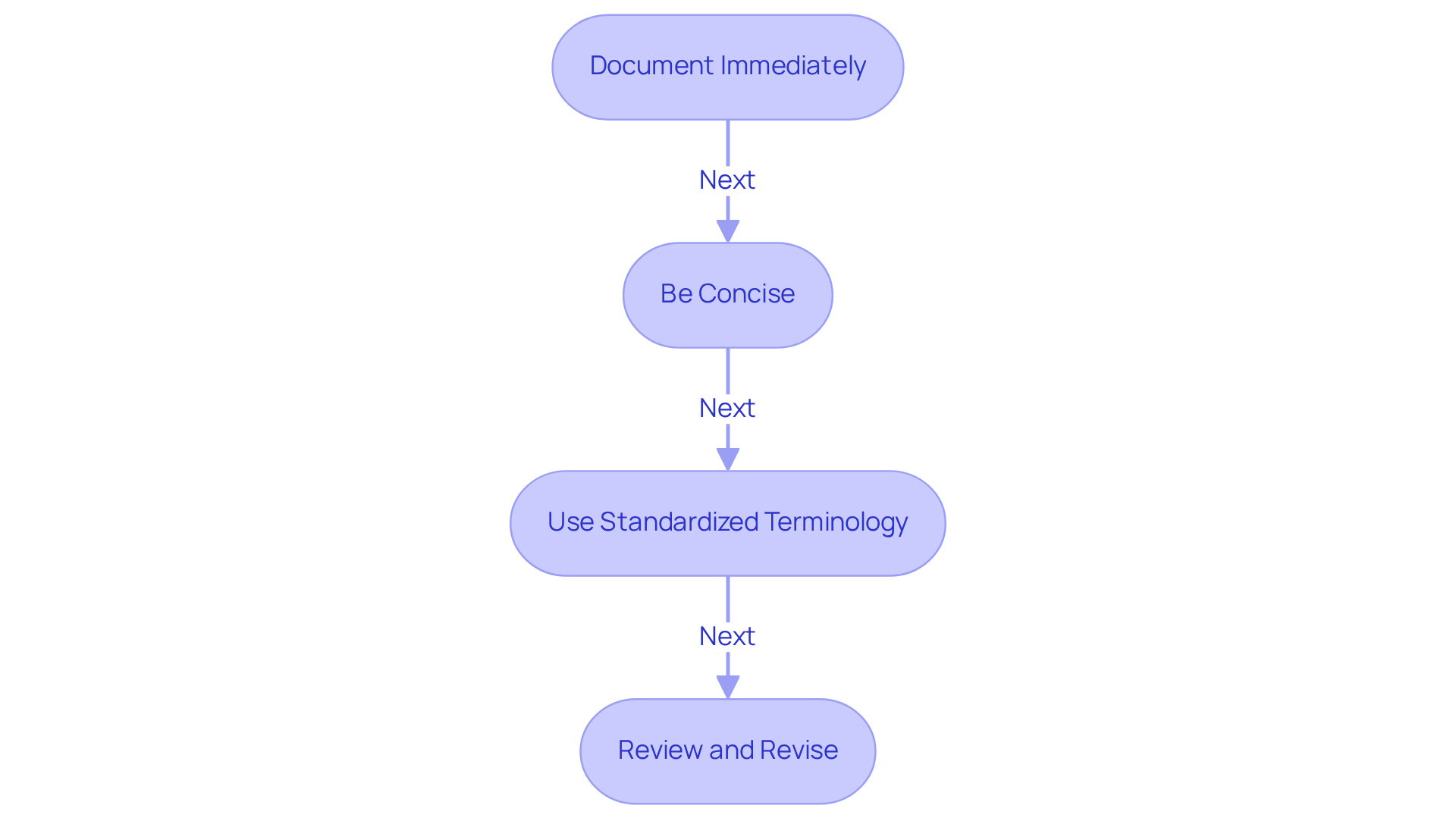
Training Guidelines: Best Practices for Writing SOAP Notes in EMS
To enhance SOAP note writing skills, EMS providers are encouraged to embrace the following best practices, fostering a supportive environment for both themselves and their patients:
- Document Immediately: How often do you find yourself struggling to recall details after a patient encounter? Capturing notes as soon as possible can alleviate this stress. Research shows that implementing a soap ems example for prompt recording significantly improves accuracy, reducing the chances of missed details and enhancing your clinical judgment. With 8,098 views on the , it’s clear how vital this practice is in our field.
- Be Concise: Have you ever felt overwhelmed by unnecessary details? A soap ems example of effective communication is using clear and direct language to convey essential information. By focusing on critical data, you can provide a soap ems example to facilitate better communication among healthcare teams, ensuring everyone is on the same page.
- Use Standardized Terminology: Are you familiar with widely recognized medical terminology and abbreviations? This knowledge not only improves clarity but also serves as a soap ems example, ensuring that your records are understandable to insurers and non-clinical staff. Such familiarity fosters effective interdisciplinary collaboration, ultimately benefiting patient care.
- Review and Revise: How often do you take a moment to evaluate your records? Using a soap ems example, regularly reviewing your documentation for completeness and accuracy is crucial. Implementing a systematic review process can help identify areas for improvement, ensuring compliance with legal and professional standards. As Keith Carlson notes, thorough documentation is vital for legal safeguarding, as records may serve as evidence in court. Additionally, maintaining a record of appointment history, including missed or rescheduled visits, can provide valuable insights into individual engagement and potential health concerns.
By adopting these practices, you not only [enhance your documentation skills](https://blog.cosmaneura.com/10-essential-treatment-notes-templates-for-healthcare-providers) but also contribute to a more compassionate and efficient healthcare environment.
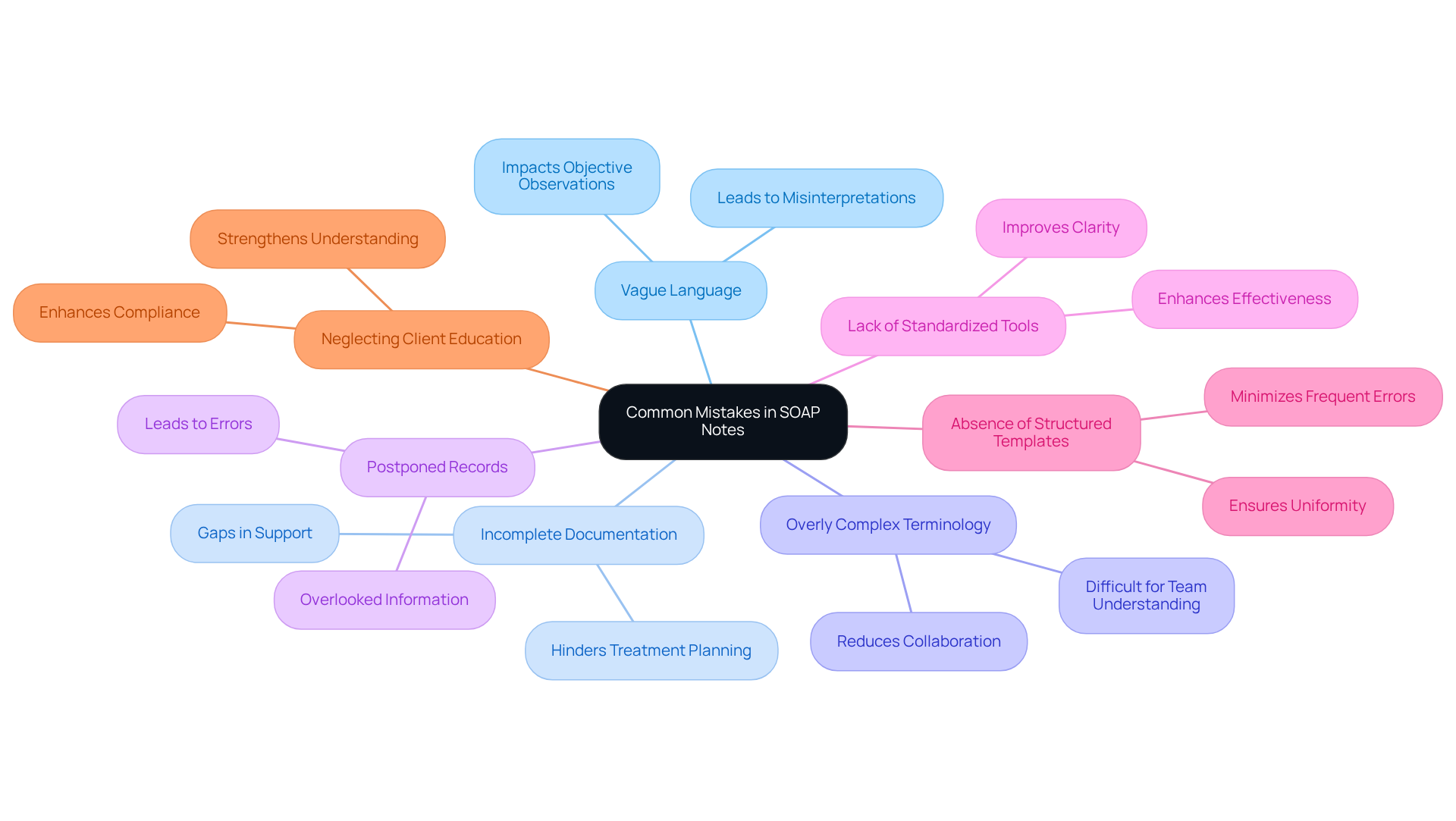
Common Mistakes in SOAP Notes: What EMS Providers Should Avoid
[Common mistakes in the SOAP EMS example notes](https://sprypt.com/blog/common-soap-note-mistakes-and-how-to-avoid-them) can create significant challenges for healthcare providers. These errors not only affect documentation but also impact patient care. Let's explore these common pitfalls and how we can address them together.
- Vague Language: It's essential to avoid using general terms that lack specific information about an individual's condition. Vague language can lead to misinterpretations, particularly in the Objective section, where precise observations are crucial for effective care.
- Incomplete Documentation: Ensure that all sections of the SOAP record are completed. This comprehensive view of the individual's status is vital; omissions can lead to gaps in support and hinder effective treatment planning.
- Overly Complex Terminology: Aim to use language that is easily understood by all members of the healthcare team. This guarantees that everyone engaged in health management can effortlessly comprehend the records, fostering better collaboration.
- Postponed Records: Composing records long after the interaction with the client can result in errors and overlooked information. Prompt record-keeping is essential for preserving the integrity of patient files and ensuring continuity of care.
- Lack of Standardized Tools: Utilizing standardized measurement instruments and scales as a SOAP EMS example to describe symptoms and progress can greatly improve the clarity and effectiveness of SOAP records.
- Absence of Structured Templates: Utilizing organized formats can assist in minimizing frequent errors in SOAP EMS example records. This approach guarantees uniformity and thoroughness in documentation, making it easier for everyone involved.
- Neglecting Client Education: Recording client education within SOAP records strengthens understanding and compliance with treatment strategies. This is vital for efficient client management and ultimately enhances patient outcomes.
By recognizing these common mistakes, we can work towards improving our documentation practices. Together, we can create a more supportive environment that and fosters effective communication within our teams.
Continuity of Care: The Importance of SOAP Notes in EMS
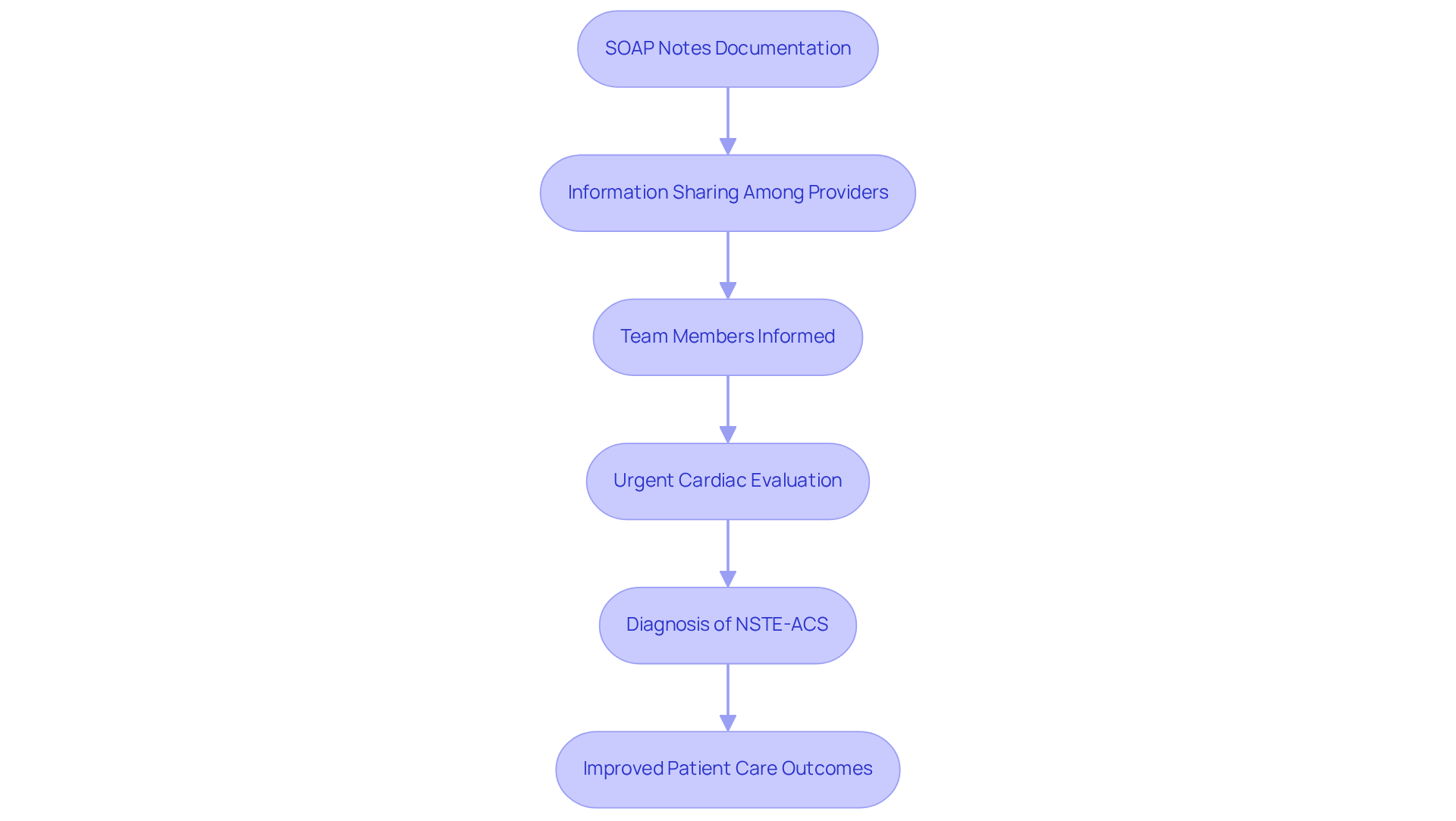
An example of SOAP in EMS shows how these records play a vital role in ensuring continuity of care, serving as organized documentation of encounters that can be easily shared among healthcare providers. This record ensures that all team members are well-informed about the individual's history, , and any changes in condition. Have you ever considered how crucial this information is during a medical emergency? For instance, a case involving a 58-year-old male with central chest pain highlighted how timely and accurate SOAP EMS example notes facilitated urgent cardiac evaluation, ultimately leading to a diagnosis of Non-ST-Elevation Acute Coronary Syndrome (NSTE-ACS).
Such organized records not only enhance communication but also significantly improve healthcare outcomes by enabling quick access to critical information. Imagine the impact this can have on patient care! Studies show that efficient record-keeping methods in EMS can cut consultation durations by more than 26%, allowing providers to focus more on treatment. Moreover, EMS specialists emphasize that clear and concise records, such as the SOAP EMS example, are essential for coordinating assistance and ensuring that all team members are unified in their approach to treatment.
By prioritizing organized records, EMS teams can enhance patient safety and improve overall care quality. Isn't it comforting to know that with effective documentation, we can provide better support to those in need? Let's continue to advocate for the importance of SOAP records in our practice, ensuring that we are all equipped to deliver the best possible care.
Future Trends: The Evolution of SOAP Notes in Emergency Medical Services
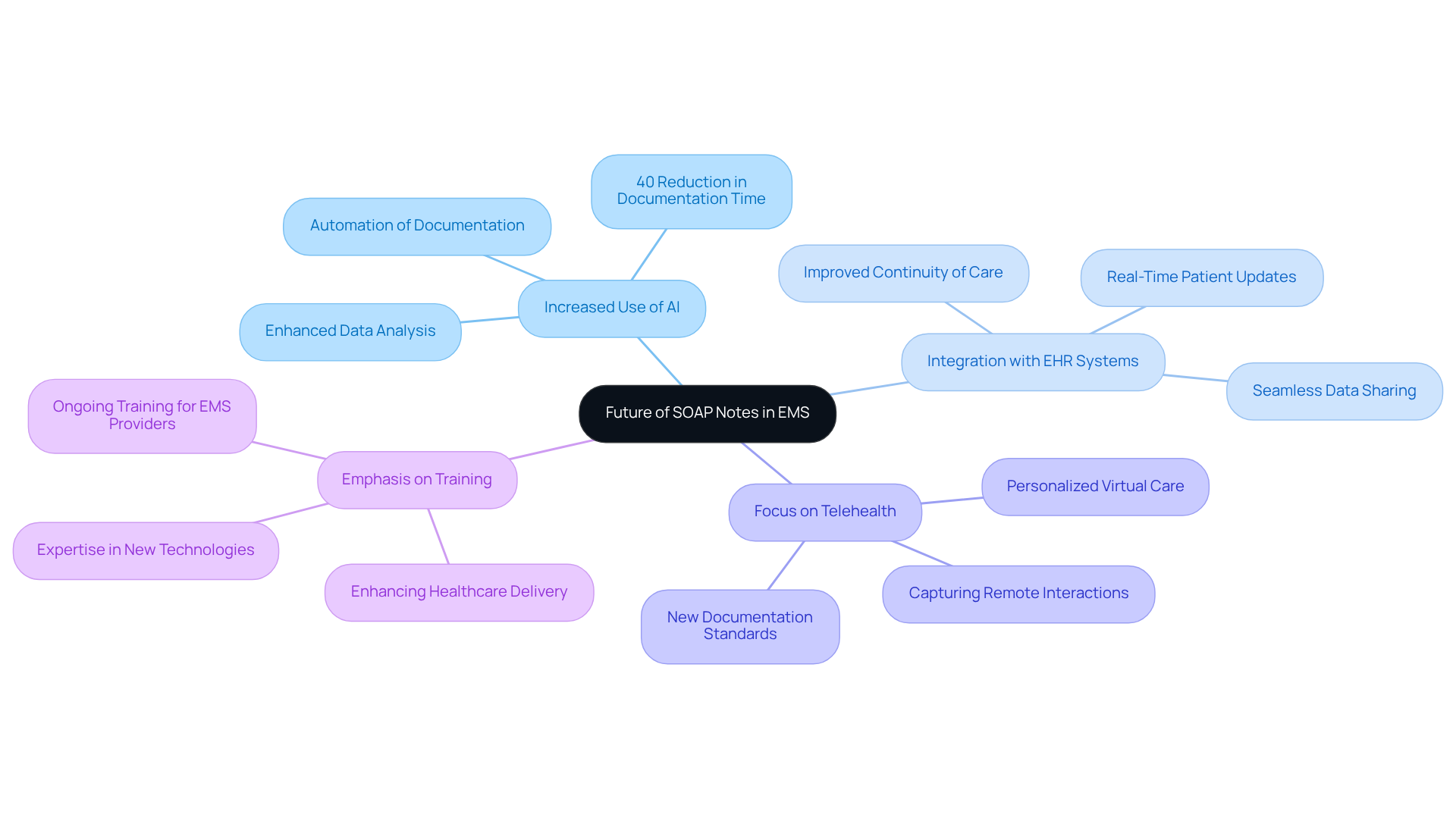
The future of SOAP notes in Emergency Medical Services (EMS), as illustrated by the soap ems example, is on the brink of significant transformation, driven by several key trends that can ease the burdens faced by healthcare providers.
- Increased Use of AI: Imagine a world where record-keeping is streamlined. The incorporation of AI tools is set to revolutionize how notes are taken, automating processes and enhancing data analysis. AI-driven document generators, such as the soap ems example, are already demonstrating improvements in precision and efficiency. Reports suggest that hospitals have experienced as much as a 40% reduction in documentation time after implementing these tools.
- Integration with EHR Systems: As healthcare technology evolves, the integration of SOAP entries with electronic health record (EHR) systems becomes increasingly essential. This development allows for , enabling EMS providers to access and update patient information in real-time. The result? Enhanced continuity of care and improved tracking of individual patients.
- Focus on Telehealth: With the rise of telehealth services, there’s a pressing need for SOAP notes to adapt. Documenting virtual encounters will require new standards that capture the nuances of remote interactions, ensuring that treatment remains thorough and centered on the individual.
- Emphasis on Training: To fully harness these technological advancements, ongoing training for EMS providers is vital. By developing expertise in new recording methods and technologies, providers can effectively utilize AI tools. This, in turn, will enhance healthcare delivery and alleviate administrative burdens.
As we look ahead, the anticipated 270% increase in AI adoption within healthcare over the next four years underscores the importance of evolving the SOAP EMS example. While technology can streamline processes, it’s crucial to maintain the human touch in patient care. Documentation should serve as a tool for enhancing clinical reasoning and communication, ensuring that the heart of healthcare remains focused on the patient. How can we collectively embrace these changes to foster better care? Let's engage in this conversation and support one another in navigating this transformative journey.
Conclusion
The integration of SOAP notes within Emergency Medical Services (EMS) is not just a procedural necessity; it's a vital component in enhancing patient care and alleviating the emotional burdens faced by healthcare providers. By adopting structured formats like the SOAP EMS example, healthcare professionals can streamline their record-keeping processes. This ensures that critical information is captured accurately and efficiently, allowing EMS professionals to focus more on what truly matters—their patients.
Throughout this article, we explored the key components of the SOAP format: Subjective, Objective, Assessment, and Plan. Each section plays a crucial role in emergency situations, and real-life examples illustrated how these elements can be effectively applied. Moreover, we highlighted the importance of technology, including AI-driven tools and standardized templates, in improving the efficiency and accuracy of SOAP note writing. These advancements address common challenges faced by EMS providers, making their work more manageable.
As we navigate the evolving landscape of healthcare, embracing these documentation practices and technological advancements is essential for EMS teams. By prioritizing effective SOAP note writing, providers not only enhance their documentation skills but also contribute to a more compassionate and efficient healthcare system. It is vital for EMS professionals to engage in ongoing training and adapt to new methodologies, ensuring they are equipped to deliver the best possible care in a rapidly changing environment. Together, we can foster a supportive atmosphere that nurtures both providers and patients alike.




