Overview
In the demanding world of healthcare, nursing documentation can often feel overwhelming. This article offers compassionate guidance on effective nursing documentation using the SOAP format—Subjective, Objective, Assessment, and Plan. By understanding the emotional challenges faced by healthcare providers, we can appreciate how structured documentation not only enhances communication among team members but also significantly improves patient care.
Clear and organized records are not just a formality; they are crucial for better clinical outcomes and reducing administrative burdens. Imagine the relief of knowing that your documentation supports your team and your patients. This structured approach fosters a nurturing environment where everyone can thrive.
Consider how much easier your day could be with streamlined documentation practices. By adopting the SOAP format, you can alleviate some of the stress that comes with administrative tasks, allowing you to focus more on what truly matters—your patients.
We invite you to embrace these effective documentation strategies. Together, we can create a more supportive and efficient healthcare environment, ensuring that every patient's needs are met with care and compassion.
Introduction
Effective documentation is the backbone of quality patient care. Yet, many healthcare providers face the emotional challenge of navigating the complexities of accurately recording their observations and assessments. The SOAP note format—comprising Subjective, Objective, Assessment, and Plan—offers a structured approach that can help streamline this process, ensuring that vital information is captured clearly and concisely.
However, the burden of administrative tasks can weigh heavily on providers, impacting their ability to focus on patient care. How can healthcare professionals avoid common pitfalls in documentation while enhancing the quality and efficiency of their records? This article explores seven essential tips designed not only to clarify the SOAP note structure but also to empower providers. By improving documentation practices, we can ultimately enrich patient outcomes and foster a more compassionate healthcare environment.
CosmaNeura: Streamline Patient Documentation with AI-Powered Efficiency
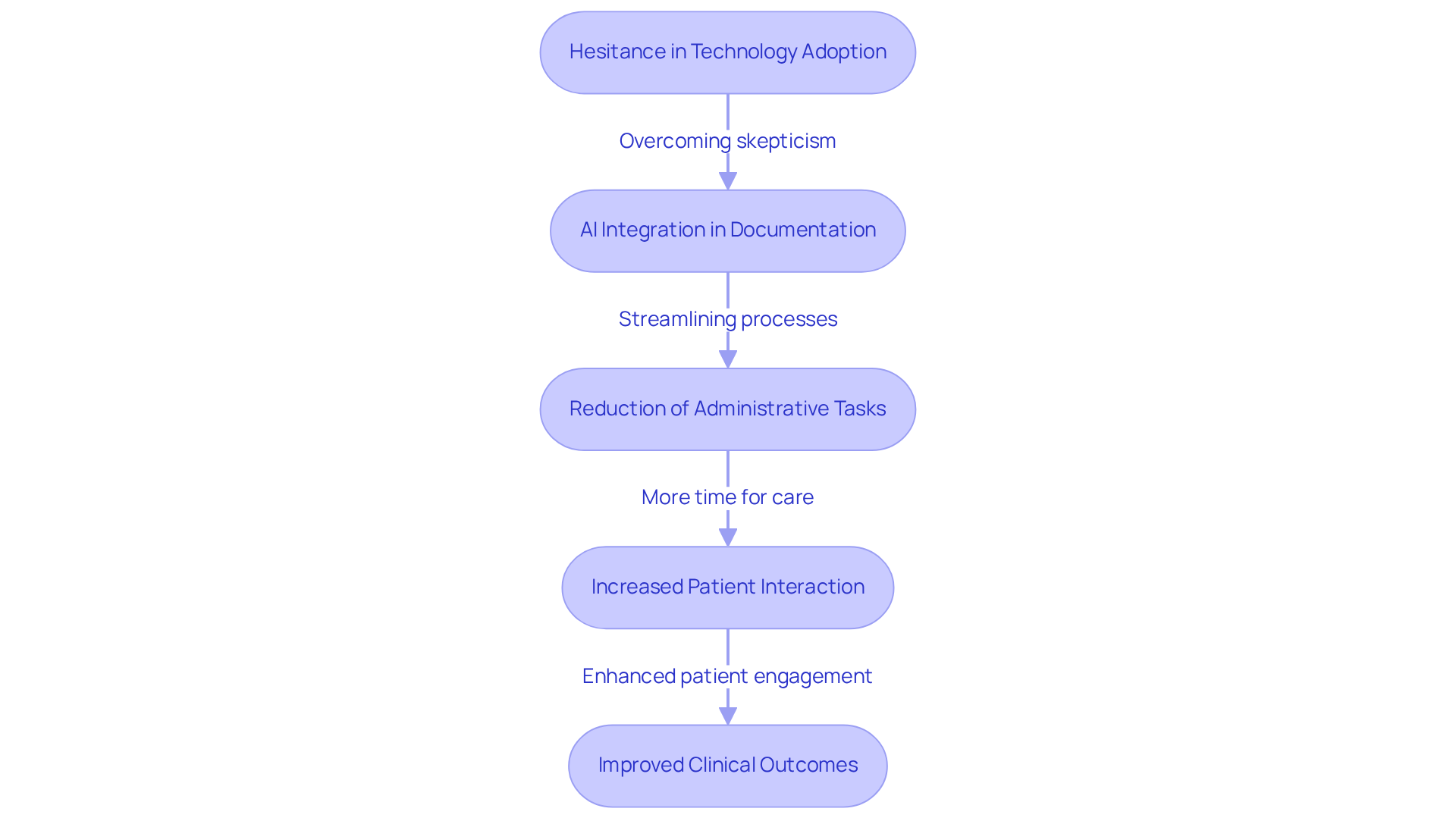
CosmaNeura's AI-driven platform is revolutionizing client records by automating essential administrative tasks. This innovation addresses the common hesitance among healthcare providers, who often face emotional challenges when it comes to adopting new technologies. Many healthcare startups struggle in technology sales conversations, frequently encountering skepticism from physicians concerned about maintaining high-quality care.
By independently managing client intake and triage, healthcare providers can redirect their focus from paperwork to delivering quality care. This shift alleviates burnout and enhances face-to-face interactions, allowing providers to connect more meaningfully with their patients. Not only does this transformation save valuable time, but it also significantly improves the accuracy and availability of records.
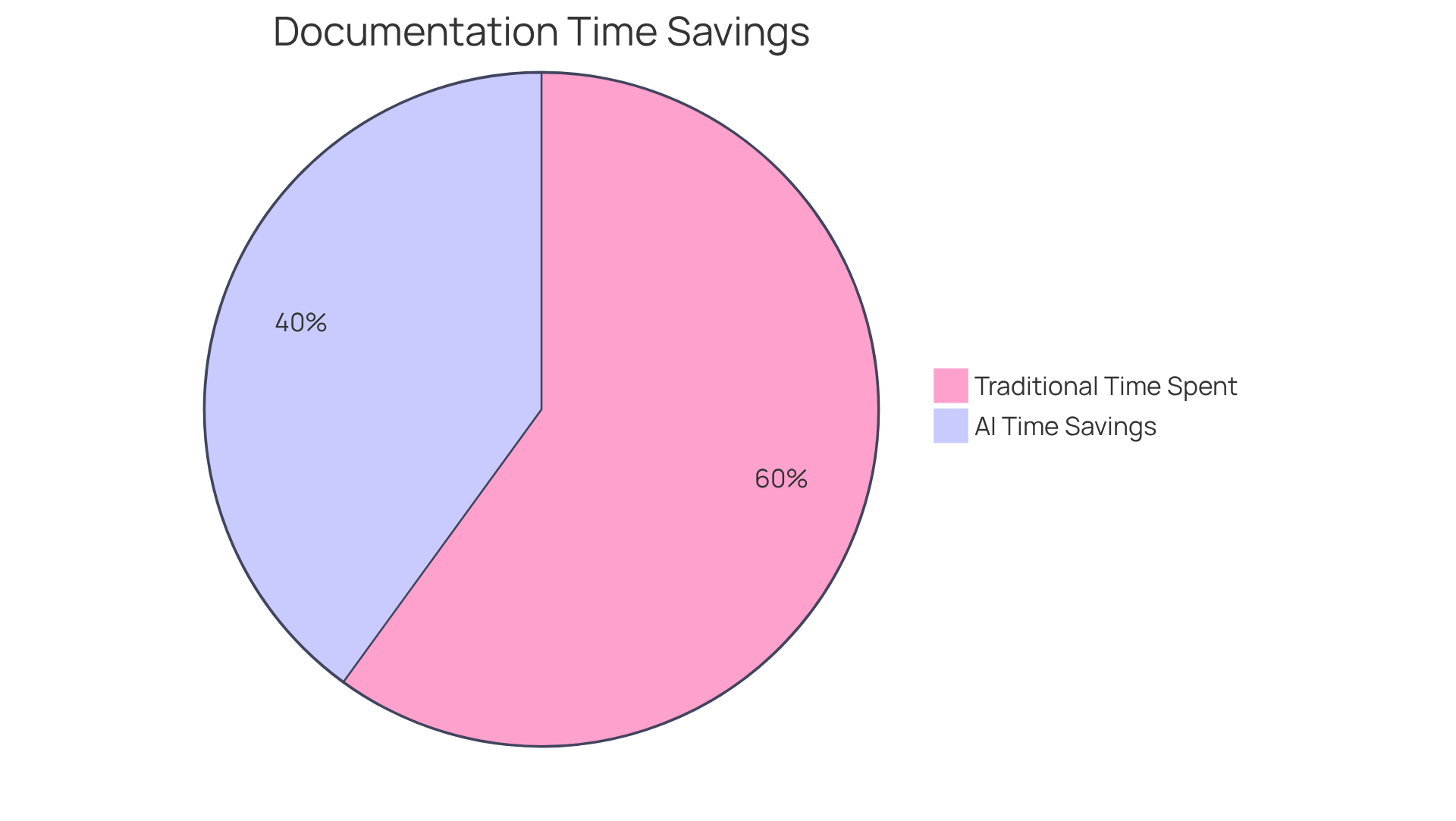
As a result, client interactions are thoroughly documented, leading to better clinical outcomes. Healthcare leaders recognize that AI technologies can reduce documentation time by up to 50%. This enables clinicians to engage more deeply with those they care for. As Craig Lee insightfully notes, 'Establishing trust in AI among users is essential.'
With CosmaNeura, the integration of AI into healthcare practices is a testament to a commitment to operational efficiency and superior care. This ultimately transforms healthcare delivery, enhancing care-centric practices. Imagine a future where healthcare providers can focus on what truly matters—their patients.
Understand the SOAP Note Structure: Subjective, Objective, Assessment, Plan
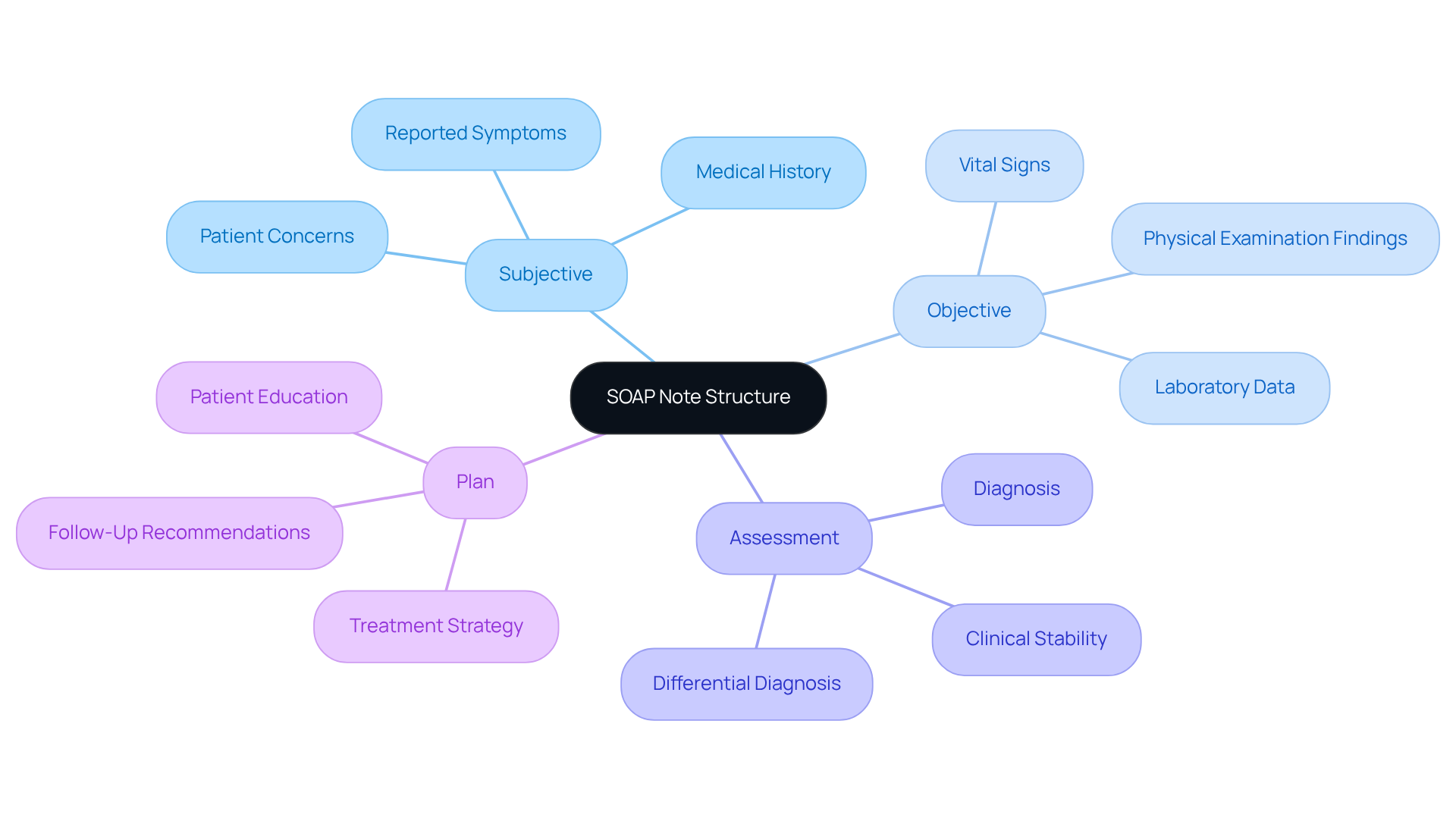
The soap example nursing format is a cornerstone of effective healthcare documentation, comprising four essential components: Subjective, Objective, Assessment, and Plan. The Subjective section captures the individual's reported symptoms, providing insight into their experience and concerns. The Objective section records clinical findings, including vital signs and physical examination results, ensuring a comprehensive view of the individual's condition. The Assessment component combines this information to create a diagnosis, while the Plan outlines the treatment strategy, specifying next steps for care.
Understanding this structure is crucial for healthcare providers, as it enables systematic documentation of encounters with individuals. Have you ever encountered a situation where clear documentation made all the difference? For instance, a soap example nursing could involve a nurse documenting an individual's complaint of sharp shoulder pain (Subjective), recording a physical examination revealing tenderness (Objective), assessing the condition as a possible rotator cuff injury (Assessment), and recommending a follow-up with physical therapy (Plan). This organized approach not only enhances communication among healthcare professionals but also improves patient outcomes by ensuring that all relevant information is captured and easily retrievable.
Current best practices emphasize clarity and conciseness in SOAP documentation. Experts recommend that efficient record-keeping methods involve using precise language and sustaining a professional tone. As Kunal Sindhu, MD, emphasizes, "The ability to convey medical information accurately, clearly, and succinctly is a key skill all clinicians in training should strive to master." Moreover, the incorporation of generative AI can simplify the record-keeping process, enabling healthcare providers to automate repetitive tasks and concentrate more on interactions with individuals.
Consider the benefits:
- Efficiency: Statistics indicate that the typical duration spent composing annotations has fallen by 11.1%, from 5.4 minutes per entry to 4.8 minutes per entry.
- Quality: By following these principles and utilizing AI tools, such as automated record-keeping software and natural language processing applications, healthcare providers can improve the quality of their records.
- Enhanced Care: Ultimately, this results in enhanced care for individuals.
Moreover, the development of documentation over time illustrates the continuous requirement for efficient communication in interdisciplinary teamwork. This guarantees that all healthcare professionals are synchronized in their methodology to care for individuals. How can you implement these strategies in your practice to foster better collaboration and care?
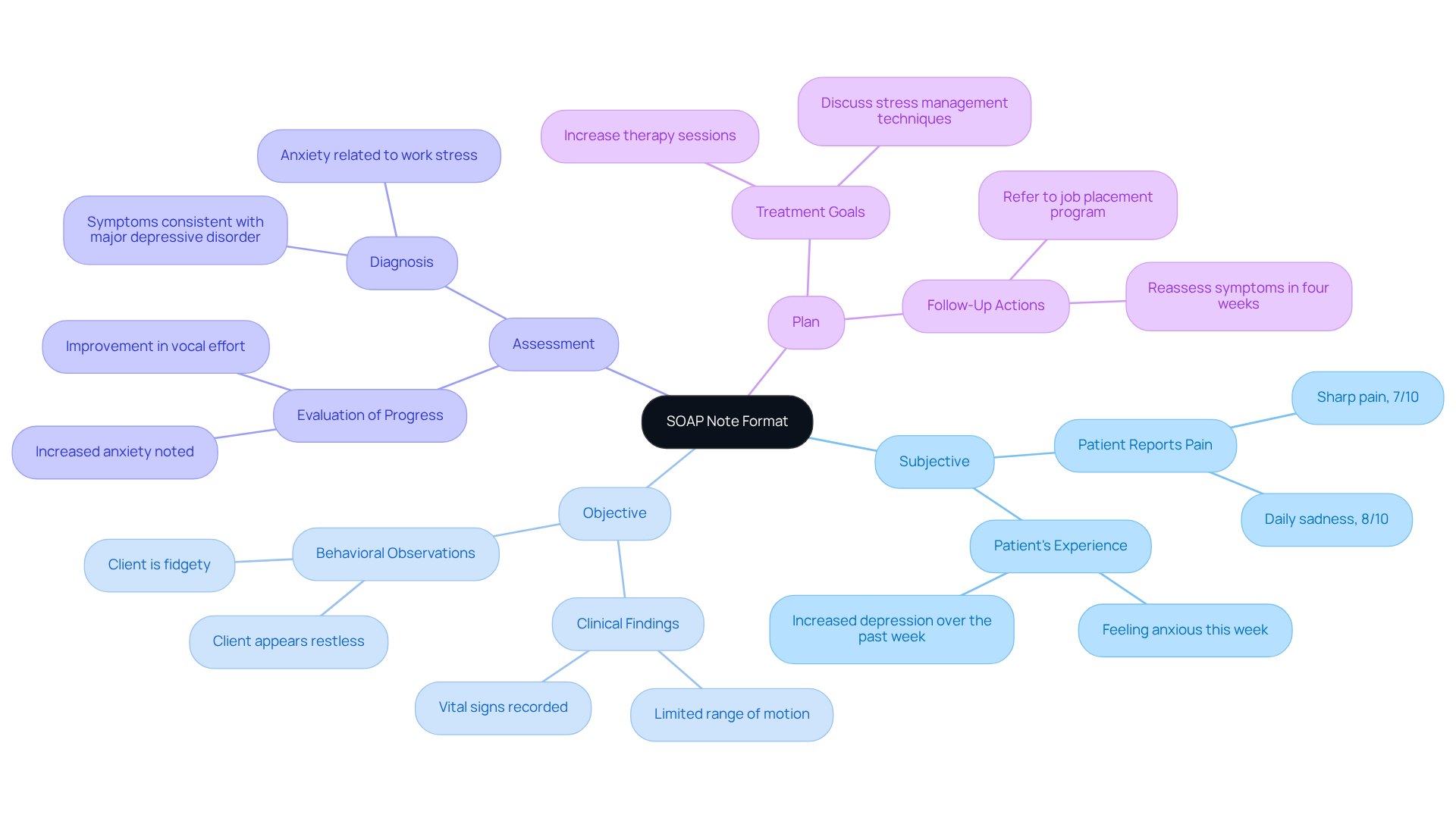
Utilize Real-World SOAP Note Examples for Better Clarity
Navigating the complexities of medical documentation can be emotionally challenging for healthcare providers. Utilizing real-world SOAP example nursing can significantly enhance the clarity of these records. For instance, a personal entry might capture a patient's own words about their discomfort, such as, 'I feel a sharp pain in my lower back that rates a 7 out of 10.' This personal touch helps providers connect with the patient's experience. In contrast, the objective section documents the clinician's findings, like, 'Patient exhibits limited range of motion in the lumbar region, with tenderness noted upon palpation.'
By analyzing a range of SOAP example nursing, healthcare professionals can gain valuable insights into effectively organizing their records. This ensures that both subjective experiences and objective observations are clearly expressed. Such clarity not only streamlines communication among providers but also enhances the overall quality of patient care. Imagine the impact of organized documentation techniques, such as the subjective-objective-assessment-plan format, which is utilized by over 225,000 healthcare professionals across the country.
The structured format, developed in the 1950s by Lawrence Weed, has become an essential tool in clinical practice. However, it’s crucial to acknowledge that the SOAP note model has limitations, including its inability to document changes over time. As specialists have pointed out, 'Identifying the main issue must take place to carry out an effective and efficient diagnosis.' This underscores the necessity for clarity in records.
By incorporating these practical examples and insights, healthcare providers can refine their record-keeping methods. Ultimately, this approach enhances outcomes for those receiving care. How might you implement these strategies in your practice to foster better communication and improve patient care?
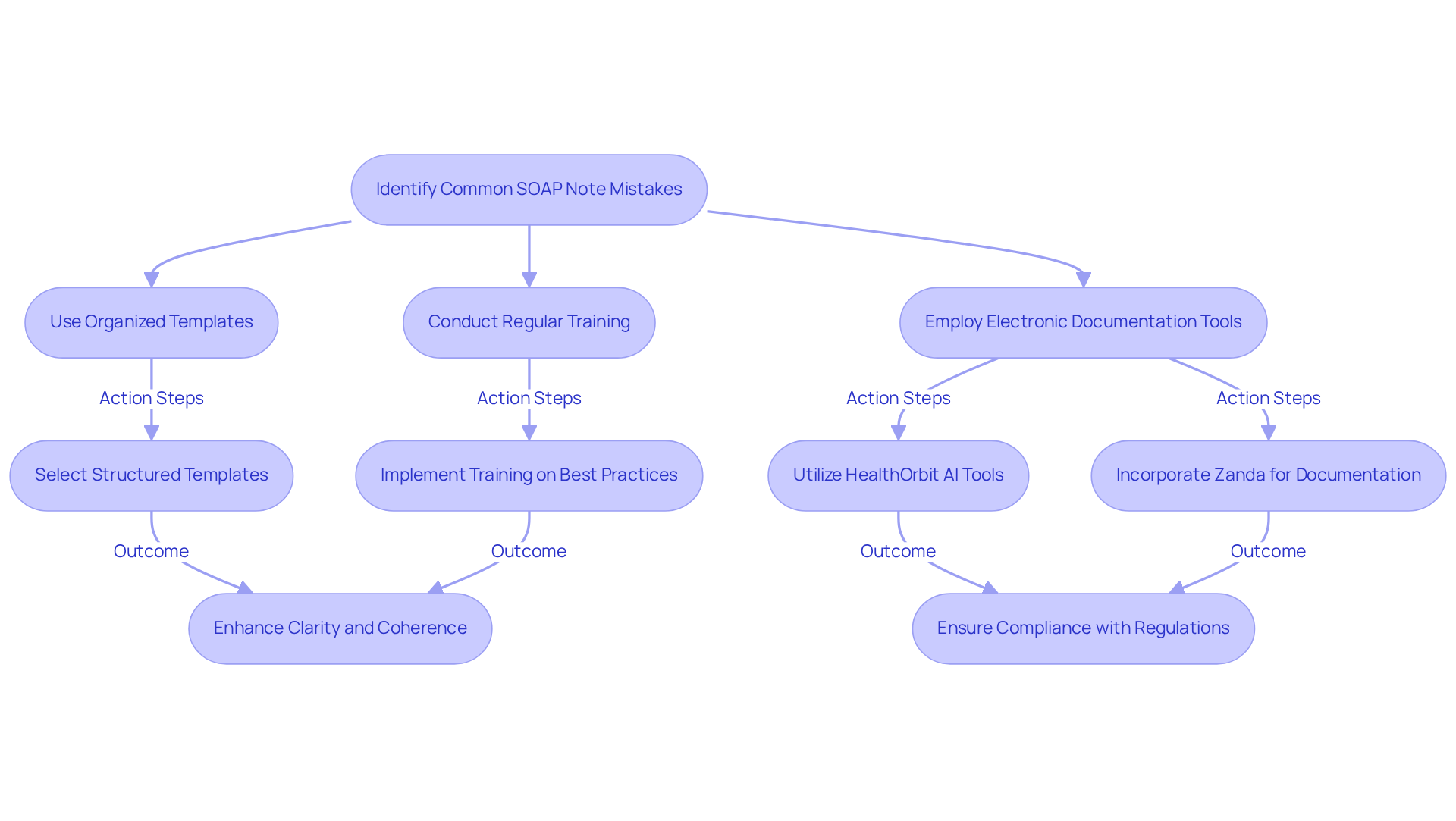
Avoid Common SOAP Note Mistakes: Enhance Accuracy and Clarity
In the demanding world of healthcare, common pitfalls found in the soap example nursing—such as vague language, incomplete information, and the struggle to differentiate between subjective and objective data—can create significant emotional challenges for providers. Have you ever experienced the frustration of ambiguous records leading to miscommunication among your team? Such situations can cause treatment delays or even mistakes, impacting patient care.
By acknowledging these errors, we can take proactive steps to enhance the precision and clarity of our documentation. Utilizing organized templates, such as those offered by HealthOrbit AI, can serve as a soap example nursing to help alleviate these issues by reducing frequent mistakes in medical records. Regular training sessions are equally vital; studies show that they familiarize staff with updated practices and guidelines, fostering a supportive environment for growth.
Moreover, employing electronic documentation tools and practice management software like Zanda encourages the creation of clear, chronological, and comprehensive records. This approach not only enhances outcomes for individuals but also promotes a sense of confidence among healthcare teams. Ultimately, prioritizing precision in clinical documentation fosters improved communication across healthcare groups, ensuring that care is effective and ethically sound.
As Vivek Podder wisely states, "The more concise yet comprehensive a medical record is, the simpler it is for healthcare providers to follow." This highlights the importance of organized records in improving healthcare. Let’s commit to refining our documentation practices together for the benefit of our patients and our teams.
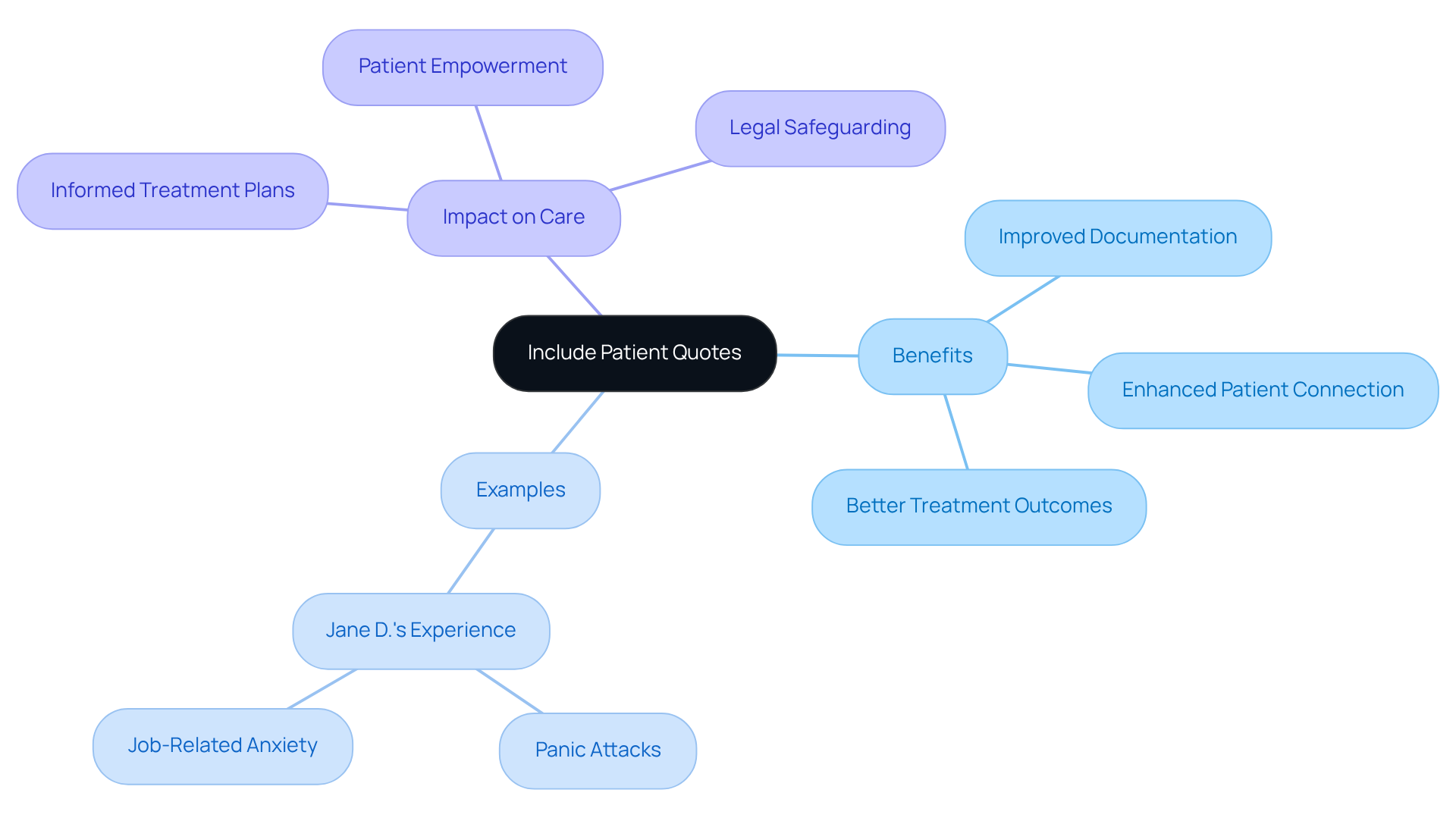
Include Patient Quotes: Capture the Patient's Voice in Documentation
Including direct quotations from individuals into SOAP example nursing records significantly enhances the documentation process. Have you ever considered how capturing an individual's exact words about their symptoms can transform care? For instance, Jane D. shared, 'The panic attacks are getting worse. I had three this week at work. I'm terrified I'll lose my job.' This not only provides essential context for future visits but also informs treatment plans.
This practice acts as a SOAP example nursing by improving the precision of the notes, ensuring that the individual's perspective is clearly represented. It cultivates a deeper connection between the provider and those receiving care, as individuals feel acknowledged and affirmed. Research shows that using a SOAP example nursing approach, which includes individuals' voices in their care records, can lead to enhanced treatment outcomes. When clinicians are better prepared to customize interventions based on expressed concerns and experiences, everyone benefits.
Furthermore, documentation improves clinical clarity by distinguishing subjective from objective information, which is crucial for medication management and risk evaluation. Additionally, clinical records offer legal safeguarding by clearly separating individual statements from clinical observations. This emphasizes the significance of precise record-keeping.
By embracing this compassionate approach to documentation, we can foster a healthcare environment where individuals feel heard and valued. Let’s continue to prioritize the voices of those we serve, enhancing both care and outcomes.
Use Clear and Concise Language: Improve Communication in SOAP Notes
Using clear and concise language in the SOAP example nursing notes is essential for fostering effective communication among healthcare providers. Have you ever felt overwhelmed by complex terminology? By avoiding jargon, all team members can easily understand the materials, enhancing collaboration and ultimately improving patient care.
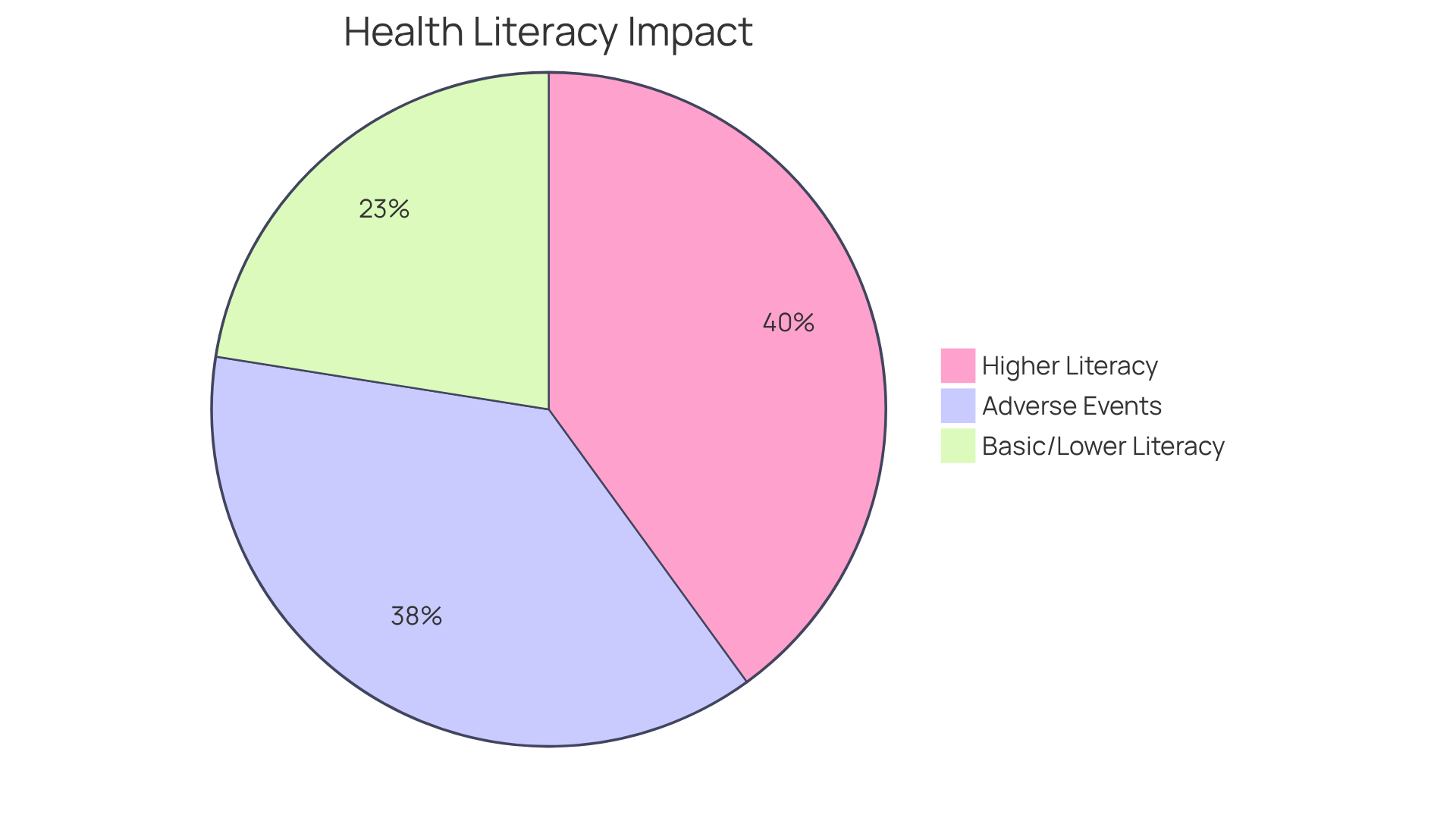
Statistics reveal that 36% of U.S. adults possess basic or lower health literacy. This highlights the urgent need for clear communication in medical records. The Institute of Medicine has reported that preventable errors lead to thousands of deaths annually, often due to miscommunication. Furthermore, the Joint Commission indicates that inadequate communication contributes to over 60% of all hospital adverse events in the USA, underscoring the risks associated with ambiguous records.
Healthcare professionals recognize that using clear language can significantly reduce misunderstandings, which can lead to negative outcomes for patients. By prioritizing clear language in clinical records, healthcare providers can create a SOAP example nursing that ensures their writing is not only effective but also comprehensible. This approach facilitates improved patient involvement and safety, nurturing a supportive healthcare environment. Let's commit to enhancing our communication for the benefit of all.
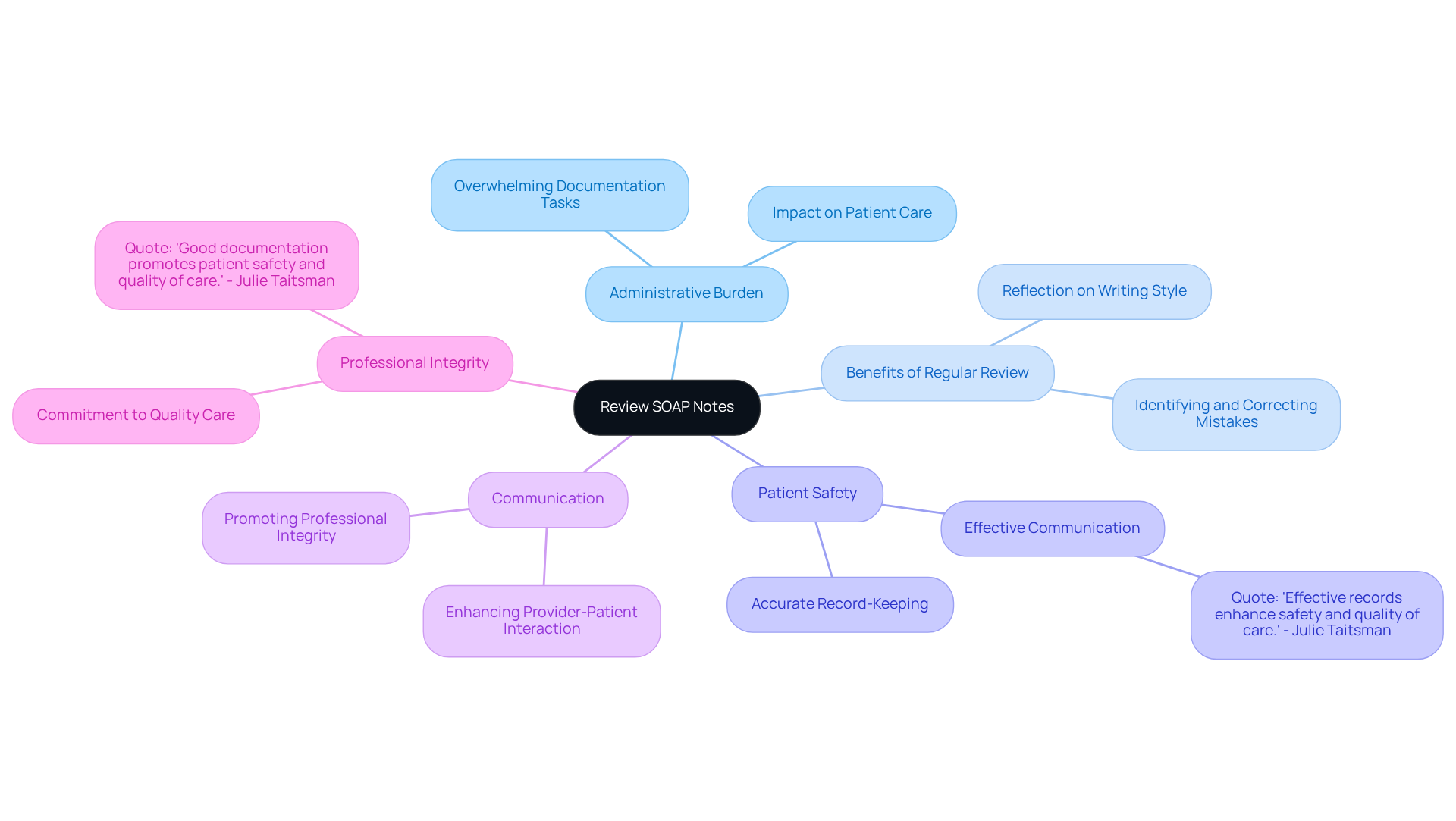
Review and Revise SOAP Notes: Maintain High Documentation Standards
Healthcare providers often face overwhelming administrative burdens that can detract from patient care. Regularly reviewing and revising SOAP example nursing notes is a compassionate practice that not only helps identify and correct mistakes but also encourages providers to reflect on their writing style. This reflection can lead to essential modifications that enhance the quality of care.
Elevated record-keeping standards are crucial for ensuring quality care. Accurate records facilitate effective communication and decision-making, which are vital for patient safety. As Julie Taitsman, Chief Medical Officer for the U.S. Department of Health and Human Services, wisely states, "Effective records enhance safety and quality of care."
Moreover, organized records contribute to superior quality materials, promoting improved data reuse for quality assessment and research objectives. By committing to regular revisions, healthcare providers can enhance their record-keeping practices, ultimately benefiting their patients and reinforcing their professional integrity.
Imagine the impact of consistently high-quality records on your practice. By prioritizing this continuous improvement, you not only elevate your standards but also foster a nurturing environment for your patients. Let's embrace this commitment together for the betterment of healthcare.
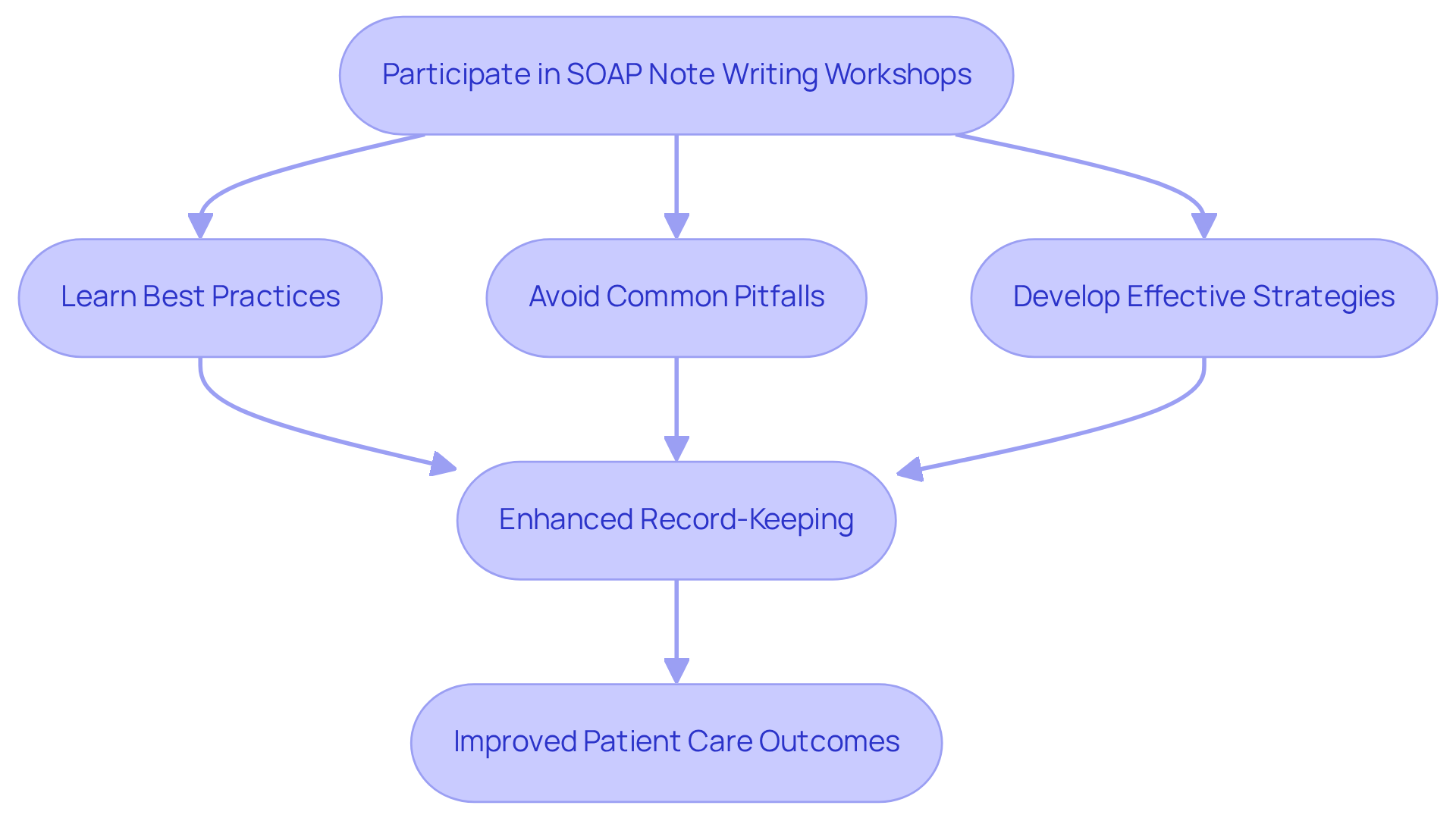
Participate in SOAP Note Writing Workshops: Enhance Your Skills
Participating in soap example nursing writing workshops can significantly alleviate the emotional burdens that healthcare providers face. These workshops focus on best practices, common pitfalls, and effective strategies for crafting comprehensive notes, using a soap example nursing to ultimately foster a supportive environment. By engaging in such training, providers enhance their record-keeping methods and contribute to a culture of ongoing advancement within their practice.
Have you ever felt overwhelmed by the administrative tasks that can detract from patient care? Expert insights reveal that consistent exposure to organized training builds greater confidence and proficiency, leading to improved patient care outcomes. Research shows that structured documentation methods can boost students' confidence and ability to apply these skills in clinical settings. For instance, average scores on pre-tests rise from 85.2% to an impressive 99% on post-tests (p < 0.001).
T.J. Grainger-Rousseau Heun emphasizes that repeated exposure to documentation skills is vital for reinforcing learning and confidence. Furthermore, case studies indicate that learners' performance on written assessments improves significantly, with scores increasing from 3.23 to 3.62 out of 4.
Healthcare providers are encouraged to explore or establish documentation workshops, not just to improve their skills, but to ensure continuous professional growth. By taking this step, you are investing in your own development and enhancing the quality of care you provide. Remember, every effort you make contributes to a brighter future for your practice and the patients you serve.
Leverage AI Tools for Efficient SOAP Note Creation: Enhance Documentation Practices
For healthcare providers, the documentation process can often feel overwhelming. The burden of administrative tasks not only consumes valuable time but can also detract from the quality of patient care. Imagine a solution that alleviates these pressures—this is where AI tools come into play.
Utilizing AI for SOAP example nursing record creation significantly enhances documentation practices by automating repetitive tasks and ensuring high accuracy. CosmaNeura's platform exemplifies this innovation, offering real-time transcription and summarization during interactions with individuals. This capability allows healthcare providers to produce detailed notes with minimal effort, ultimately improving the quality of records.
In fact, methods that have incorporated AI for record-keeping show an impressive 40% decrease in time dedicated to these duties. This means clinicians can focus more on what truly matters: client care. Additionally, AI-driven recording tools promote uniform accuracy across various healthcare settings, minimizing human error and enhancing communication among care teams.
As the healthcare landscape evolves, incorporating a SOAP example nursing approach by embracing AI in record-keeping is not just a passing trend; it is a vital step toward improving operational efficiency and patient outcomes. Let’s explore how these tools can transform your documentation practices and enhance your ability to provide compassionate care.
Know the Legal Implications of SOAP Notes: Safeguard Your Practice
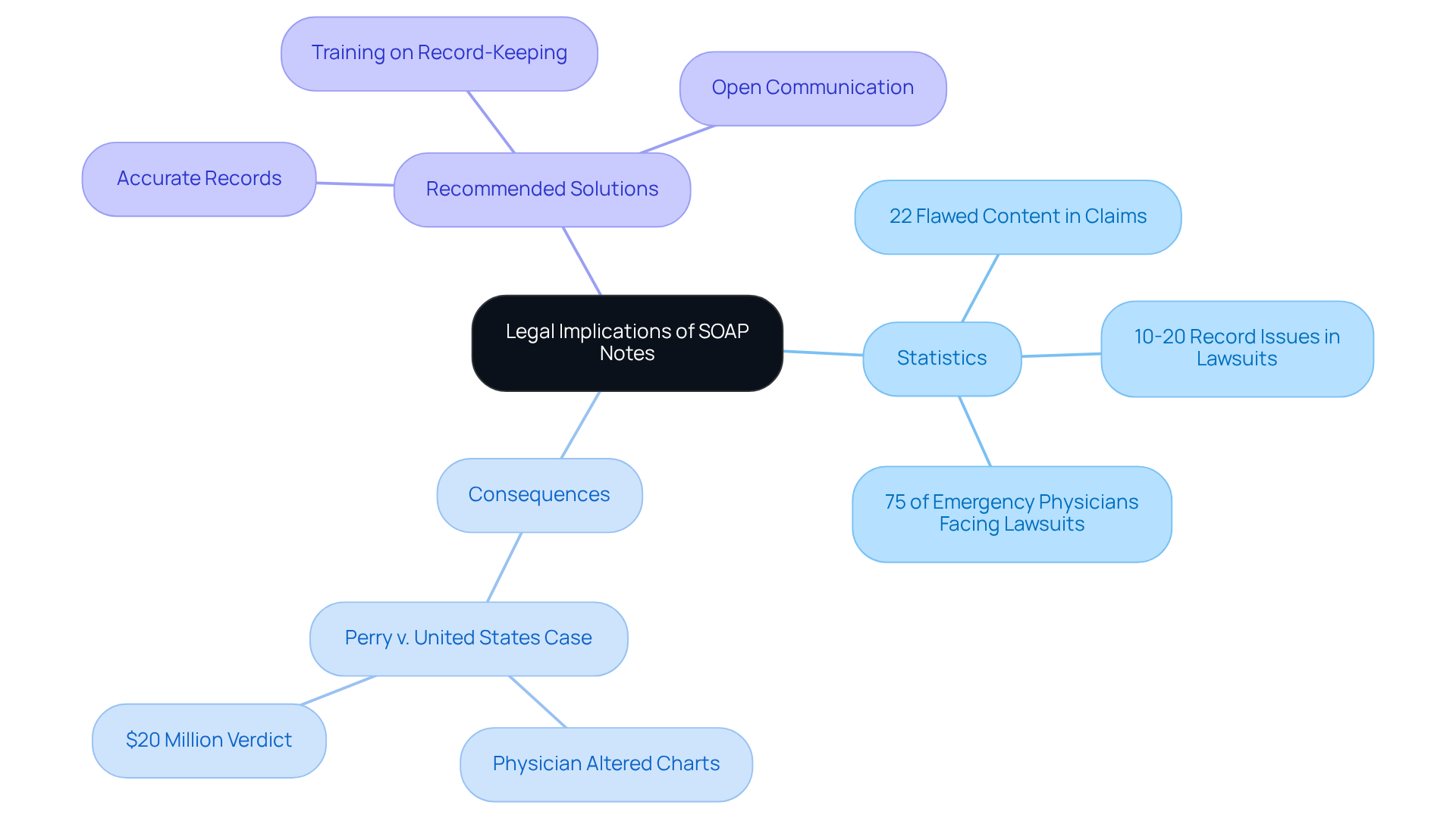
Healthcare providers often grapple with significant emotional challenges, especially when it comes to the legal implications of SOAP notes. These documents can become pivotal evidence in malpractice cases and insurance claims, which can be overwhelming. Did you know that flawed content is involved in 22% of malpractice claims associated with records? Additionally, record issues contribute to 10-20% of malpractice lawsuits. It's a sobering reality that more than 75% of emergency physicians will face a malpractice lawsuit at least once in their careers.
Despite the prevalence of record-keeping mistakes, many physicians receive very little training or guidance on their documentation practices. This highlights a pressing need for accurate record-keeping. By adopting proper practices, providers not only protect themselves from legal consequences but also ensure compliance with regulatory standards, which fosters trust with clients. For instance, maintaining confidentiality and avoiding judgmental language in the SOAP example nursing notes are essential steps in mitigating legal risks.
A significant case, Perry v. United States, illustrates the severe repercussions of record-keeping mistakes. In this instance, a physician modified charts to conceal a patient's fever, which ultimately led to a staggering $20 million verdict. This serves as a powerful reminder of the importance of diligent documentation.
By understanding these implications and regularly reviewing and updating documentation practices, healthcare professionals can safeguard their practices and uphold their professional integrity. Consider implementing the following key solutions:
- Ensure all records are accurate and comprehensive.
- Provide training on effective record-keeping practices.
- Foster an environment where open communication about documentation is encouraged.
These steps not only enhance legal protection but also improve the quality of care provided to patients. Let’s work together to create a supportive environment where healthcare providers can thrive, ensuring that both their legal and professional responsibilities are met with confidence.
Conclusion
Embracing effective documentation practices, especially through the SOAP note structure, is vital for healthcare providers who wish to enhance patient care and ease their workflows. Have you ever felt overwhelmed by administrative tasks? Understanding and utilizing the components of SOAP—Subjective, Objective, Assessment, and Plan—enables clinicians to create comprehensive and clear records that foster better communication and improve clinical outcomes.
Throughout this article, we've explored various strategies, such as:
- the importance of clear language
- incorporating patient quotes
- leveraging AI tools to alleviate administrative burdens
Each of these elements is crucial in refining documentation practices. By focusing on these strategies, healthcare providers can dedicate more time to their patients rather than paperwork. Additionally, avoiding common pitfalls and participating in workshops can further enhance the skills necessary for effective SOAP note writing.
The significance of accurate and thoughtful documentation cannot be overstated. It not only protects healthcare providers legally but also nurtures a culture of trust and quality care. As the healthcare landscape continues to evolve, adopting these best practices will not only improve individual practices but also contribute to the overall advancement of patient-centered care in the industry.
Investing in effective documentation is an investment in the future of healthcare—one that prioritizes clarity, compassion, and quality in every patient interaction. Let’s embrace these changes together. Your commitment to these practices can lead to a brighter, more compassionate future for all patients.




