Overview
In the demanding field of speech-language pathology, documentation can often feel like a burden. However, structured and clear documentation is not just a requirement; it is a vital component of effective patient care. This article provides examples of SOAP notes that can enhance your documentation skills, helping you navigate the emotional challenges that come with administrative tasks.
Effective SOAP notes do more than fulfill legal standards; they serve as a bridge for communication among providers and can significantly improve patient outcomes. By illustrating how to craft these notes thoughtfully, we aim to alleviate some of the stress you may face in your practice.
Imagine the peace of mind that comes from knowing your documentation is not only compliant but also contributes positively to your patients' care. The benefits of mastering SOAP notes extend beyond paperwork—they foster a collaborative environment that enhances the overall therapeutic experience.
We encourage you to explore the examples provided and reflect on how you can implement these strategies in your practice. Together, let's prioritize clear and compassionate documentation that truly supports the needs of our patients.
Introduction
In the complex world of speech therapy, the delicate balance between patient care and administrative responsibilities can often feel overwhelming for practitioners. Many find themselves stretched thin, grappling with the demands of both providing quality care and managing paperwork. This article explores the transformative potential of effective SOAP notes. By showcasing ten examples, we aim to illustrate how these structured notes can not only streamline documentation but also elevate the quality of care delivered to clients.
As speech-language pathologists seek clarity and precision in their records, a pressing question emerges: how can these organized notes ease the burden of paperwork while simultaneously promoting better therapeutic outcomes? This exploration is not just about improving efficiency; it’s about nurturing the essential connection between therapist and client, ensuring that every interaction is meaningful and impactful.
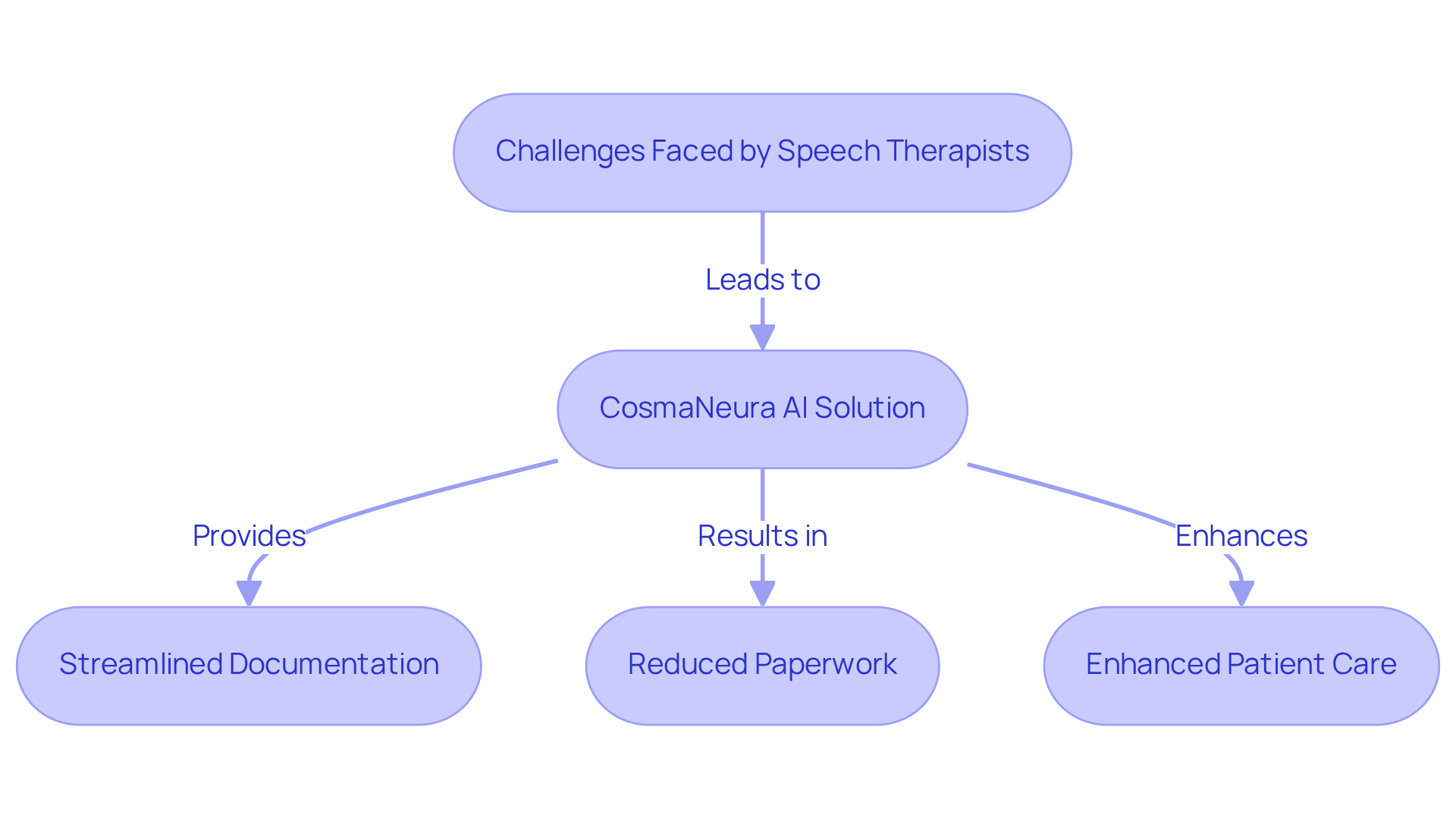
CosmaNeura: AI-Powered SOAP Note Documentation for Speech Therapists
In the demanding world of healthcare, speech therapists often grapple with overwhelming administrative responsibilities. This can lead to stress and detract from the time they could spend with their clients. CosmaNeura understands these challenges and is here to help. By utilizing advanced AI technology, it streamlines the development of SLP soap note examples, allowing therapists to focus on what truly matters—their clients.
Imagine a workday where client intake and record-keeping are automated. CosmaNeura makes this possible, enabling therapists to uphold a high standard of care while significantly cutting down on paperwork, as demonstrated in an SLP soap note example. This innovative solution not only enhances operational efficiency but also alleviates the financial pressures that healthcare organizations face. Ultimately, patient welfare remains at the heart of healthcare delivery.
Are you ready to transform your practice? With CosmaNeura, you can reclaim precious time and direct your energy towards meaningful client interactions. Let's prioritize what truly matters in healthcare together.
Pediatric Articulation Therapy SOAP Note Example: Best Practices
An effective slp soap note example for a pediatric articulation therapy session demonstrates best practices in record-keeping, ultimately supporting the child’s journey. Here’s how it might be structured:
- Subjective: "The child expressed frustration with certain sounds during the session. The parent reports ongoing difficulty with 's' and 'r' sounds at home."
- Objective: "The child produced the 's' sound correctly in 70% of opportunities during structured activities, indicating a measurable level of performance."
- Assessment: "While the child shows notable improvement in articulation, challenges remain with specific phonemes, particularly 's' and 'r'."
- Plan: "Continue with targeted articulation exercises focusing on 's' and 'r' sounds. Arrange a follow-up session in one week to evaluate advancements and modify the therapy plan as necessary."
This structured approach not only ensures clarity but also facilitates effective communication among care providers, enhancing the overall quality of pediatric speech therapy.
Consider the case study of a child named Luke, who struggles with phonemic awareness. It was noted that targeted exercises can significantly aid in improving articulation skills. As Luke's teacher stated, "Effective documentation is crucial for tracking progress and adjusting strategies to meet each child's unique needs." Integrating such insights into an SLP soap note example can further enhance their effectiveness in clinical environments.
Have you thought about how effective documentation can transform the way we support our young learners? By embracing these practices, we can ensure that every child receives the tailored care they deserve.
Adult Voice Therapy SOAP Note Example: Key Components
A SOAP note for an adult voice therapy session can be thoughtfully structured as follows:
- Subjective: "The client shares feelings of hoarseness after a long day of teaching, expressing concern about their voice."
- Objective: "Upon assessment, the voice quality is noted as breathy, with a pitch range of 120-220 Hz, as illustrated in the slp soap note example, indicating potential areas for improvement."
- Assessment: "The client’s vocal fatigue appears to be affecting their teaching effectiveness; it’s clear from the slp soap note example that further vocal exercises are essential for their progress."
- Plan: "We will introduce gentle vocal warm-up exercises and include an slp soap note example during a follow-up in two weeks to assess their development."
This example underscores the significance of attentive observations and personalized plans in voice therapy, fostering a supportive environment for the client's growth.
School-Age Child Stuttering SOAP Note Example: Effective Strategies
An effective SLP soap note example for a school-age child experiencing stuttering can be thoughtfully structured to address both their emotional and speech needs.
- Subjective: "The child expressed feelings of anxiety when asked to speak in class, sharing concerns about potential laughter from peers."
- Objective: "Stuttering was observed in approximately 30% of spoken words during conversations, with notable instances of repetition and prolongation."
- Assessment: "It appears that the child's anxiety significantly impacts the frequency and severity of their stuttering; therefore, additional strategies to address these emotional responses are essential."
- Plan: "Introduce fluency-enhancing techniques such as the Gentle Onset Technique, the Pull-Out Technique, and the Cancellation Technique, which involves pausing after a stutter to alleviate tension and restate the word fluently. Incorporate the Syllable-Timed Speech Technique, known for its effectiveness in reducing stuttering when practiced regularly. Collaborate with the teacher to foster a supportive classroom environment that encourages participation. Additionally, utilize the Light Articulatory Contacts Technique to ease pressure at speech sound touch points for smoother speech. Arrange a follow-up session in one month to evaluate progress and adjust strategies as needed."
This structured documentation, such as an slp soap note example, not only supports tracking the child's progress but also allows for the adjustment of therapeutic strategies to better cater to their needs. As Craig Coleman highlights, "Our role extends beyond merely addressing the technical aspects of the disorder—we are also here to assist clients in processing and managing the emotional and psychological responses that accompany their condition.

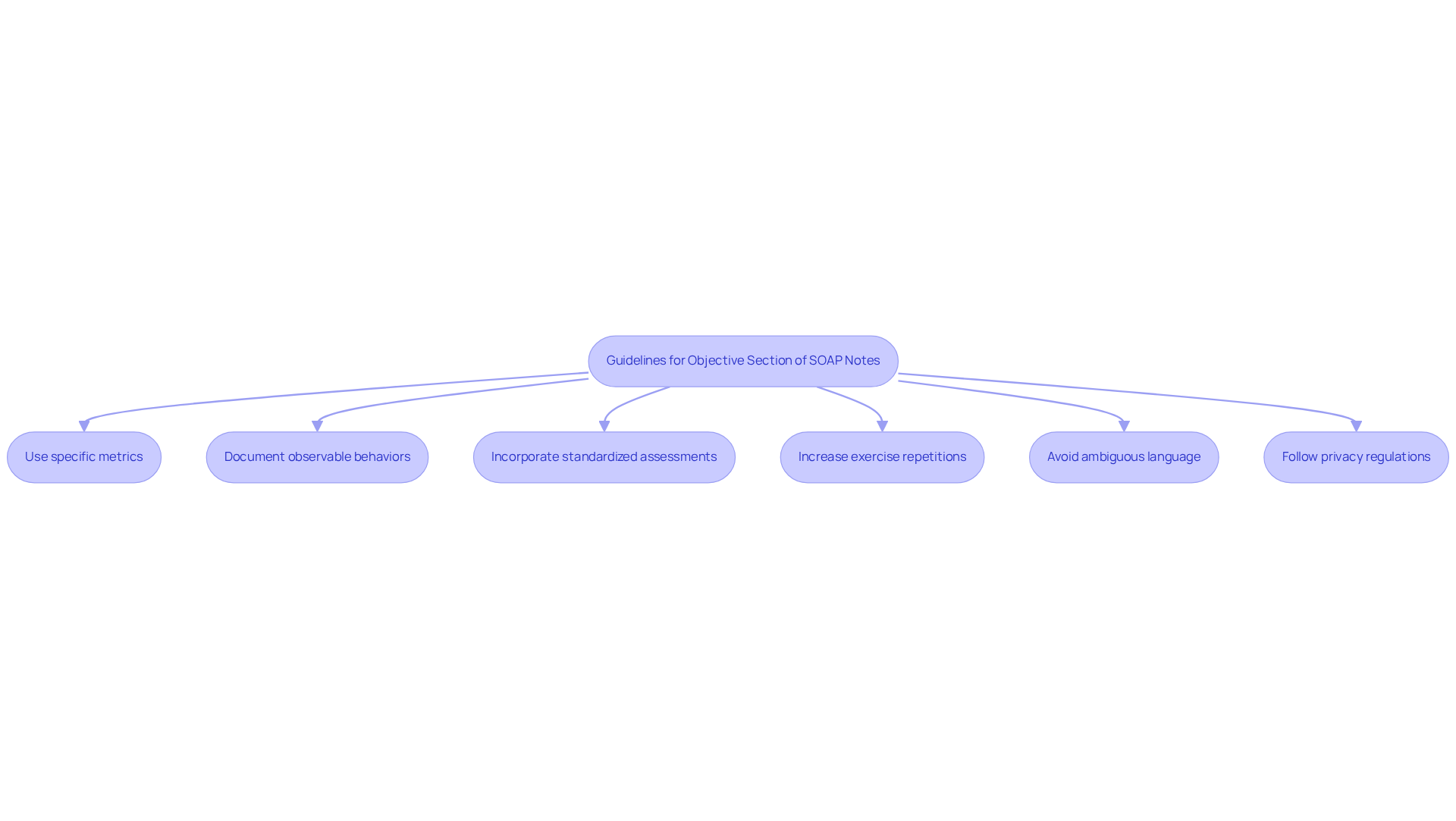
Objective Section of SOAP Notes: Essential Guidelines
The objective section of SLP soap note examples is essential for capturing measurable data and observable facts that guide treatment decisions. It's important to recognize the emotional challenges healthcare providers face in documenting these details. By adhering to the following guidelines, you can enhance the effectiveness of this section:
- Utilize specific metrics, such as the percentage of correct responses, to quantify patient performance.
- Document observable behaviors, including the frequency of stuttering or other relevant actions, to provide a clear picture of the patient's condition.
- Incorporate results from standardized assessments whenever applicable, as these provide a benchmark for evaluating progress.
- Increase strengthening exercise repetitions to 15 as a specific example of measurable data that can be documented.
- Avoid ambiguous language and assumptions to ensure clarity in records.
- Follow privacy regulations like HIPAA to ensure legal compliance in healthcare records.
This clarity in records not only aids in tracking patient progress but also supports informed decision-making regarding treatment strategies. Experts stress that accurate and quantifiable data are crucial for effective speech therapy records, which serve as an SLP soap note example, ensuring that practitioners can track progress and modify interventions as needed. As Natalia Tague notes, "The subjective section might include that the client says they've been crying every day, that they can't sleep, or that they've lost their appetite," highlighting the importance of clear and measurable documentation.
By focusing on these aspects, you can create a supportive environment that fosters patient growth and well-being. Remember, every detail matters in the pursuit of effective treatment.
Assessment Section of SOAP Notes: Evaluating Patient Progress
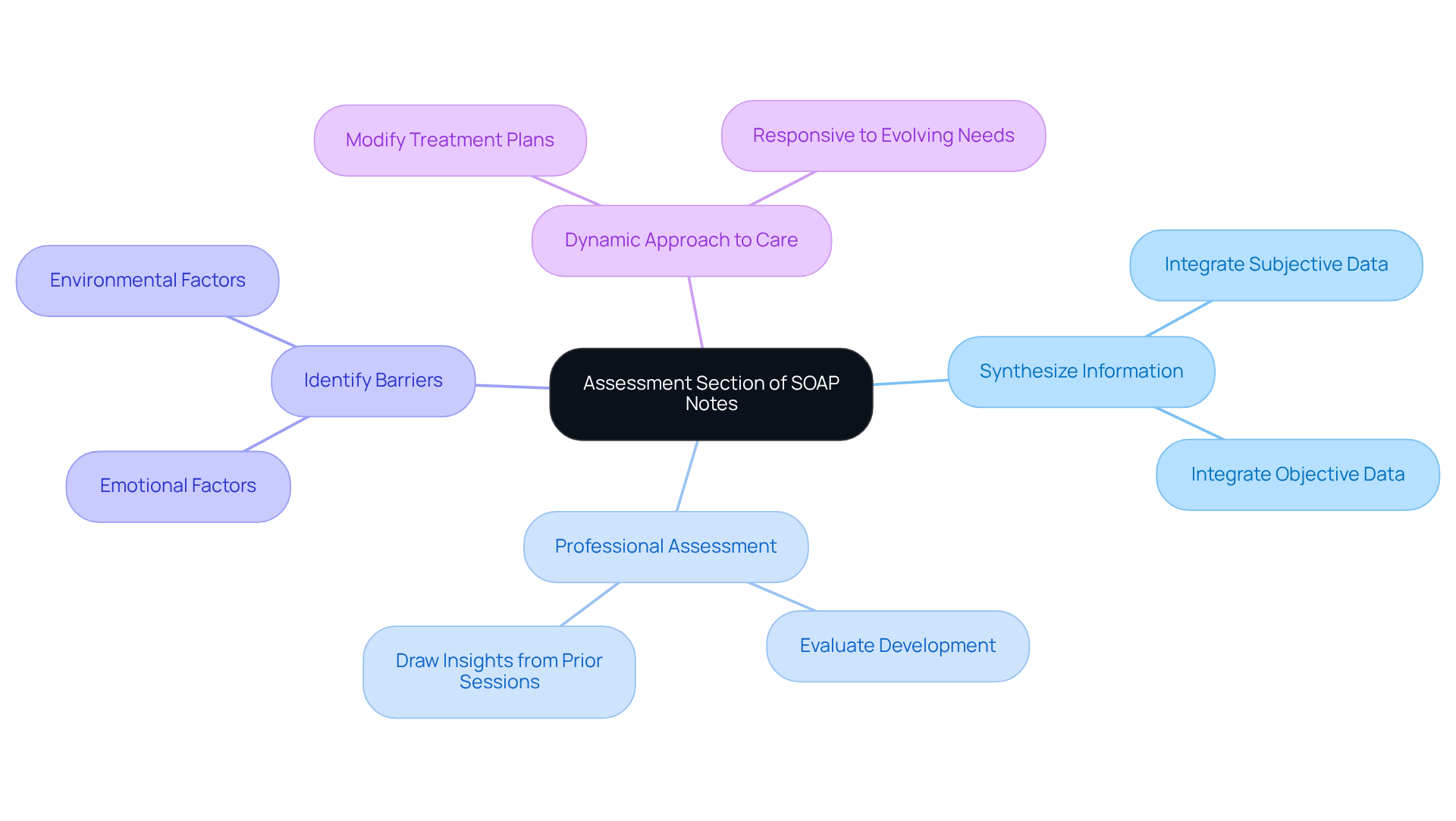
In the assessment section, therapists are called to embrace a compassionate approach:
- Synthesize information from both the subjective and objective sections to create a comprehensive view of the patient's status.
- Offer a professional assessment of the individual's development, drawing on insights from prior sessions and current observations.
- Identify any barriers to advancement, such as emotional or environmental factors, and suggest modifications to the treatment plan accordingly.
This section is vital for ensuring that therapy remains responsive to the individual's evolving needs. By fostering a dynamic approach to care, we can significantly enhance therapeutic outcomes. As Van der Kolk (2014) poignantly notes, "traumatic experiences leave lasting traces on our minds, emotions, and biology," which underscores the necessity of careful evaluation in the assessment process.
Moreover, as Irvin D. Yalom wisely states, "Psychotherapy is a cyclical process from isolation into relationship." This highlights the importance of understanding the dynamics of the therapeutic relationship in evaluating patient progress.
Let us reflect on how we can better support our patients through thoughtful assessments that truly resonate with their experiences.
Plan Section of SOAP Notes: Setting Future Therapy Goals
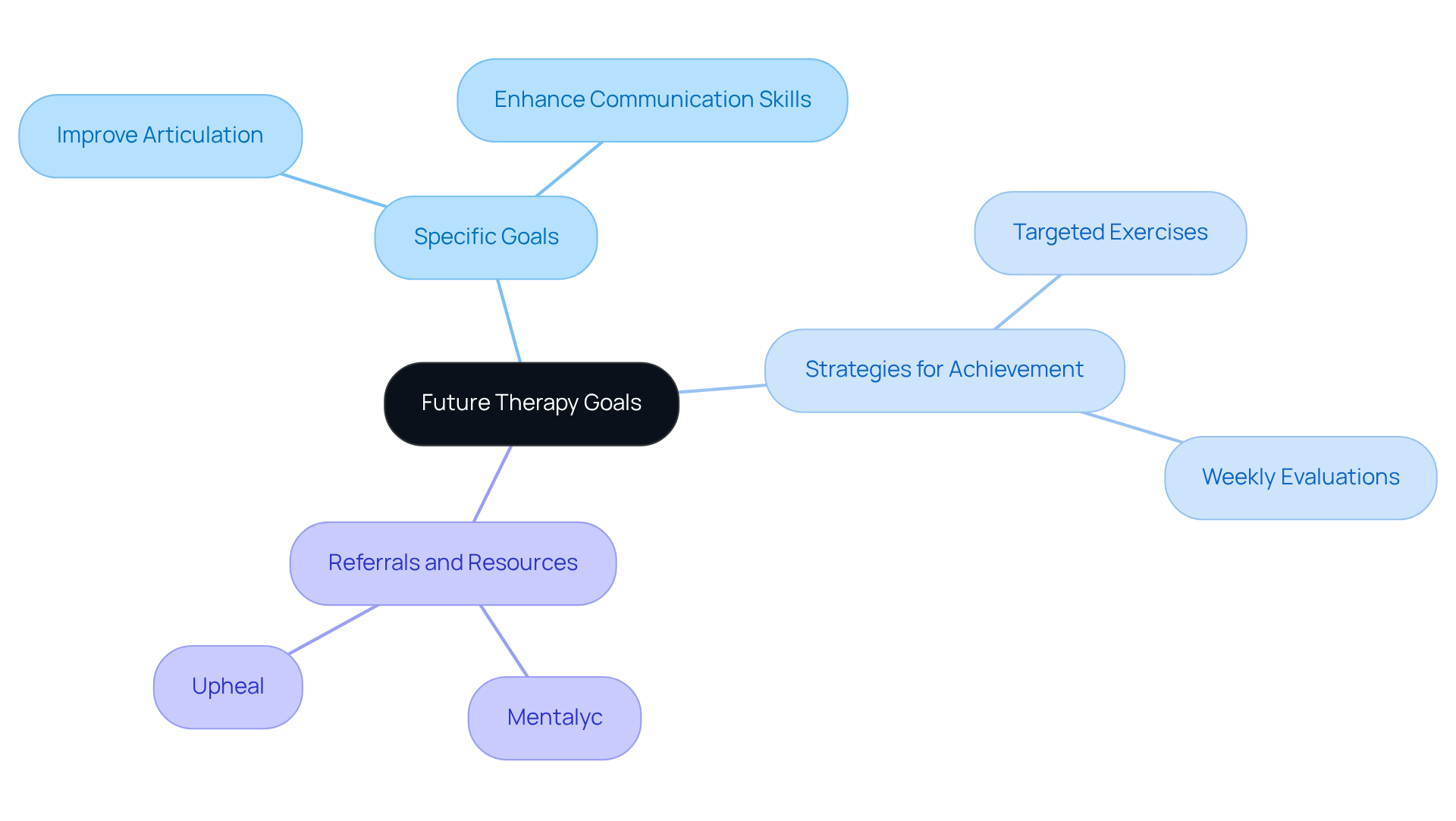
The plan segment of the SLP soap note example plays a vital role in shaping the future of therapy sessions. It is essential to outline the direction with care and clarity.
-
Specific Goals: What are the objectives for the next session? Clearly defining goals—such as improving articulation of targeted sounds or enhancing specific communication skills—helps both the therapist and client understand the path forward. It's important for therapists to include a comprehensive yet concise slp soap note example in their entries, ensuring clarity in documentation.
-
Strategies for Achievement: How will these goals be reached? Detailing the methods, including targeted exercises, practice routines, or specific interventions tailored to the client's needs, is crucial. For example, therapists are encouraged to 'Continue with current plan and evaluate each week,' fostering ongoing assessment and adjustment of strategies.
-
Referrals and Resources: Are there additional resources that could support the client's progress? Identifying specialized therapy programs or community resources is key. Many therapists are now embracing AI tools like Mentalyc and Upheal, which alleviate the burden of writing detailed session notes, allowing for increased focus on client care.
This structured approach exemplified in the slp soap note example not only clarifies the objectives for both therapist and patient but also nurtures accountability and focus in the therapeutic process. By ensuring that every session is purpose-driven, therapists can enhance the effectiveness of their interventions and better support their clients' journeys toward achieving their therapy goals. Additionally, capturing significant quotes that reflect clients' emotional experiences or realizations during sessions can provide valuable insights into their progress.
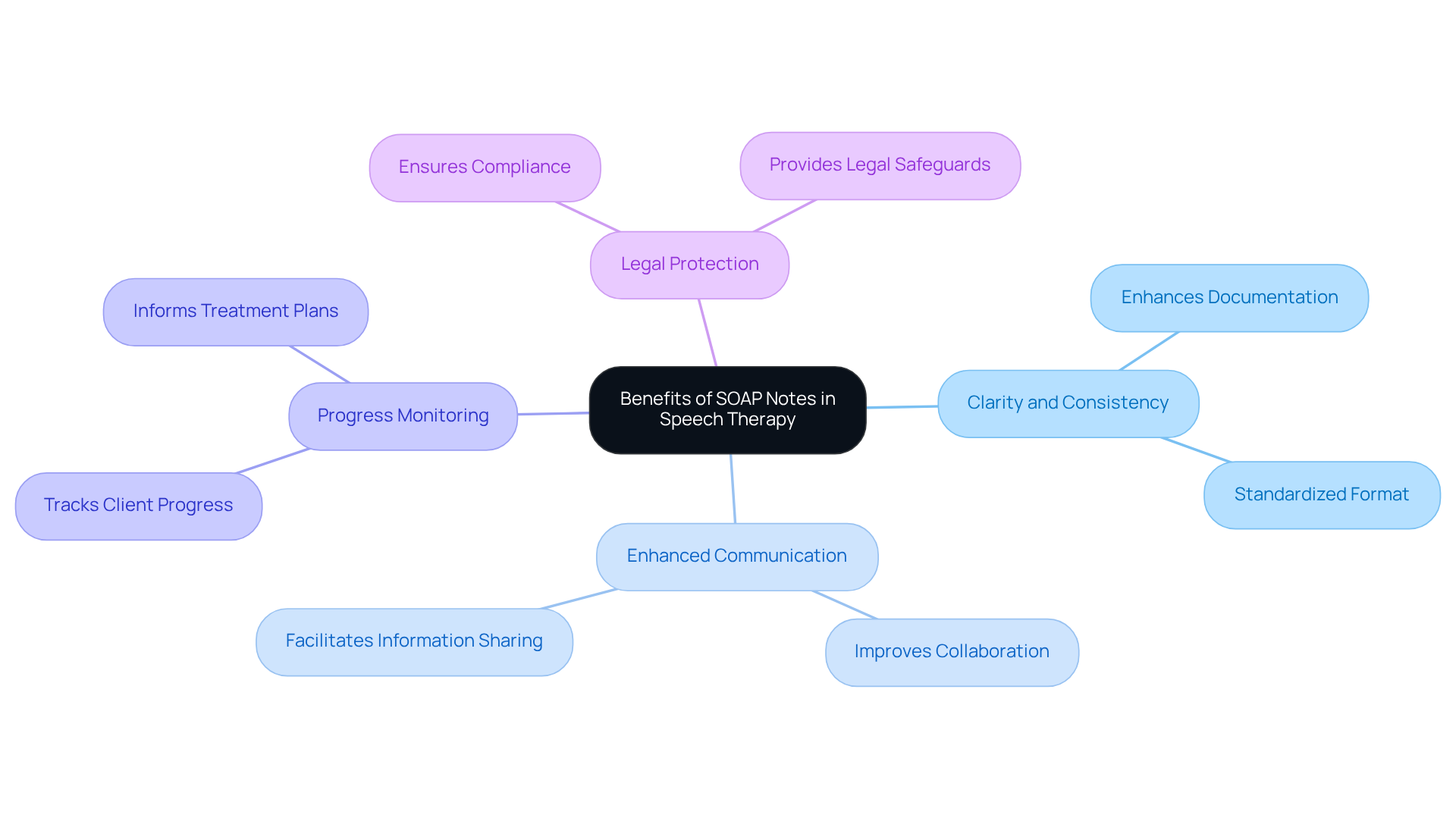
Benefits of SOAP Notes in Speech Therapy: Enhancing Documentation
In the demanding world of speech therapy, healthcare providers often face emotional challenges due to administrative burdens. Using an SLP soap note example can significantly alleviate these pressures, fostering a more compassionate approach to patient care.
The benefits of using SOAP notes in speech therapy are numerous:
- They enhance clarity and consistency in documentation, which can be further improved through innovative AI solutions like CosmaNeura's Agentic Platform.
- They promote better communication among healthcare professionals, paving the way for improved collaboration and care for individuals by utilizing an SLP soap note example.
- They facilitate the monitoring of individual progress over time, which serves as an SLP soap note example for creating more tailored treatment plans.
- They provide legal protection and ensure compliance with healthcare regulations, which can be demonstrated through an SLP soap note example, meeting industry standards.
These advantages contribute to a more organized and effective therapeutic process, ultimately enhancing patient care and reducing administrative burdens in healthcare delivery, which can be demonstrated through an SLP soap note example. By embracing these practices, we can create a more supportive environment for both providers and patients alike.
Tips for Writing Effective SOAP Notes: Best Practices for SLPs
An SLP soap note example illustrates how writing effective SOAP notes is essential for SLPs who strive to provide the best care for their clients. To achieve this, consider the following best practices:
- Clarity and conciseness in language are vital. Each note should be easily understandable and actionable, allowing for seamless communication.
- Utilizing standardized terminology promotes consistency, enhancing collaboration among healthcare professionals.
- Documenting immediately after sessions captures details accurately, reducing the risk of forgetting critical information that could impact client care.
- Regularly examining and updating records ensures clarity and thoroughness, including all pertinent details while avoiding superfluous information.
- The organized format of SOAP records not only assists in consistent record-keeping but also aids comprehension among providers.
- Incorporating direct quotes from clients in the Subjective section enriches accuracy and provides deeper context regarding their experiences.
- Lastly, recognizing the significance of SOAP records in facilitating insurance reimbursement and adhering to standards of record-keeping is crucial for maintaining high-quality care.
Embracing these practices serves as an SLP soap note example that not only upholds high standards in clinical records but also profoundly influences the effectiveness of therapy. By offering clear insights into client progress and treatment strategies, SLPs can foster a nurturing environment that supports their clients' journeys.

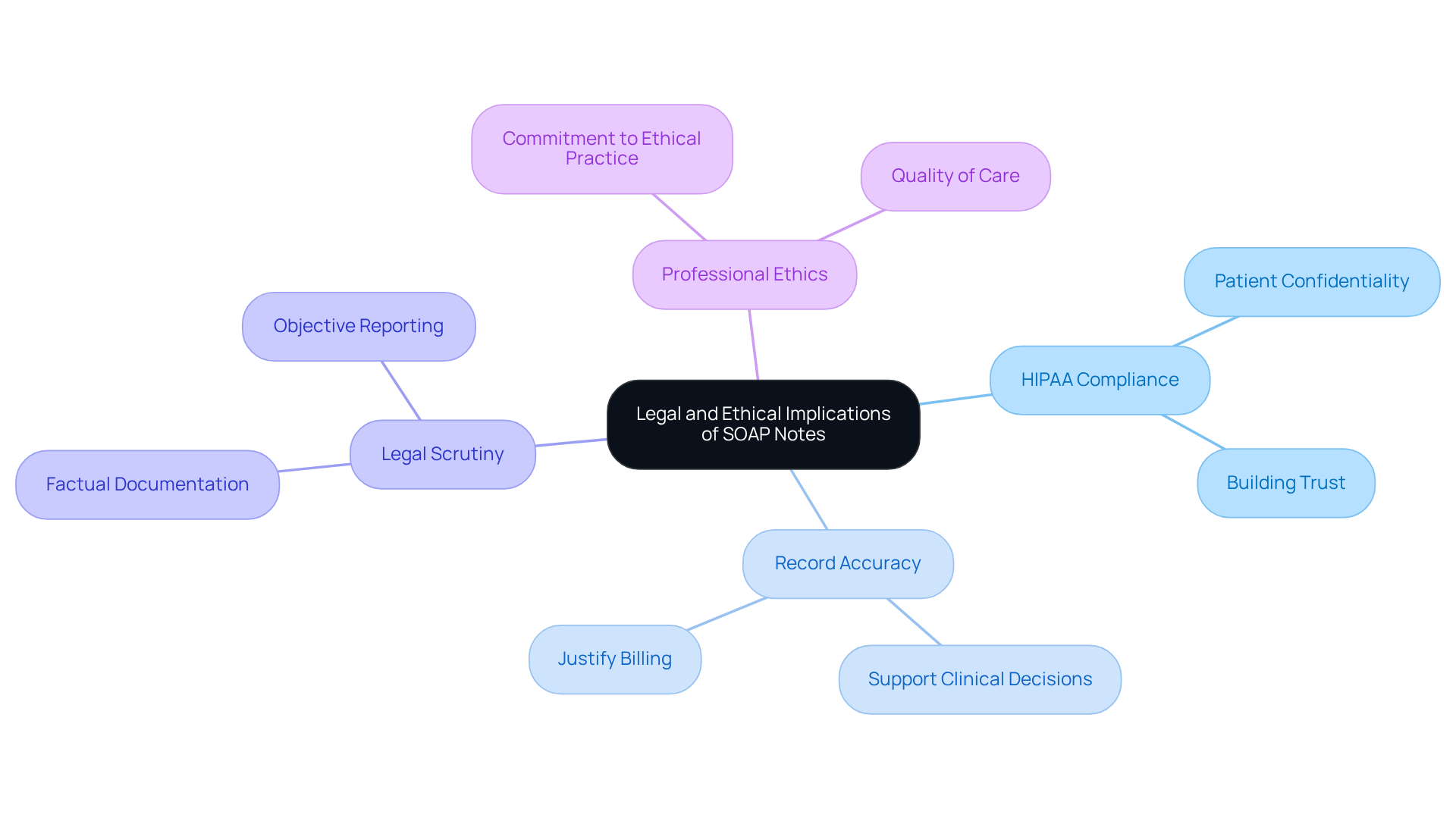
Legal and Ethical Implications of SOAP Notes: What SLPs Need to Know
As speech-language pathologists (SLPs), it's vital to recognize the emotional weight of our responsibilities, especially when it comes to documentation. The legal and ethical implications of writing an SLP soap note example can feel overwhelming, but understanding them is crucial for our practice and our patients.
Firstly, we must ensure compliance with HIPAA regulations to protect our patients' confidentiality. This not only safeguards their privacy but also builds trust in our therapeutic relationships. Additionally, maintaining accurate and thorough records is essential to provide an effective slp soap note example. These records support our clinical decisions and justify billing, ultimately benefiting our patients by ensuring they receive the care they need.
Moreover, we should be mindful of the potential for legal scrutiny. Our documentation must be factual and objective, reflecting our commitment to ethical practice. By embracing these principles, we not only uphold the standards of our profession but also enhance the quality of care we provide.
Reflecting on these implications, how can we further support each other in navigating these challenges? Let’s continue to engage in discussions about best practices and share our experiences to foster a nurturing environment for both ourselves and our patients.
Conclusion
In the realm of speech therapy, effective documentation through SOAP notes transcends mere routine; it is a fundamental aspect that enriches patient care and allows therapists to concentrate on their essential mission—helping clients reach their communication goals. How often do administrative tasks overshadow the passion for helping others? By integrating structured approaches like those illustrated in this article, speech-language pathologists can simplify their documentation processes, alleviating administrative burdens and enhancing the overall quality of care.
This article explores various SLP SOAP note examples, emphasizing best practices across diverse therapeutic contexts, from pediatric articulation to adult voice therapy. Key insights highlight the necessity of clarity in the subjective, objective, assessment, and plan sections, alongside the importance of incorporating measurable data and emotional considerations. Each example serves as a guide, demonstrating how thoughtful documentation can lead to more personalized and effective treatment plans.
The significance of adopting these practices extends beyond individual therapy sessions. By embracing innovative solutions like CosmaNeura's AI-powered documentation tools, speech therapists can boost their efficiency and collaboration, ensuring that patient welfare remains the priority in their practice. As the field continues to evolve, committing to excellence in documentation will be crucial in nurturing a supportive environment for both therapists and clients alike. Let us take these steps together, fostering a brighter future for all.




