Overview
In the demanding world of healthcare, providers often face emotional challenges that can hinder their ability to deliver optimal patient care. The administrative burdens can feel overwhelming, impacting not only the documentation process but also the quality of interactions with patients. This article offers effective SOAP presentation examples to enhance healthcare documentation, shining a light on the importance of structured notes in improving patient outcomes.
By mastering the components of SOAP notes—Subjective, Objective, Assessment, and Plan—healthcare professionals can streamline their documentation processes. Imagine a scenario where technology and collaboration come together to reduce errors and foster better patient-provider relationships. This is not just a possibility; it is an achievable goal that can transform the way care is delivered.
Consider the benefits of implementing these structured notes:
- Improved clarity
- Enhanced communication
- Ultimately, a more compassionate approach to patient care
As you reflect on your own experiences, think about how these changes could positively impact your practice and your patients.
We encourage you to explore these strategies further. By embracing the principles of effective SOAP documentation, you can alleviate some of the burdens you face and focus more on what truly matters—providing exceptional care to your patients. Together, we can create a more supportive and efficient healthcare environment.
Introduction
In the fast-paced world of healthcare, the ability to document patient interactions effectively is paramount. Many healthcare providers face emotional challenges, feeling overwhelmed by the demands of their roles. SOAP notes, structured to provide a comprehensive overview of patient care, serve as essential tools that can enhance communication among providers and improve patient outcomes. Yet, the administrative burdens can weigh heavily on their ability to focus on what truly matters: patient care.
How can healthcare professionals master the art of SOAP documentation while navigating the complexities of modern medical practice? This article explores seven compelling examples of SOAP presentations that not only illustrate best practices but also highlight the transformative role of technology and collaboration in streamlining documentation processes. By embracing these solutions, providers can alleviate some of their burdens and foster a more nurturing environment for their patients.
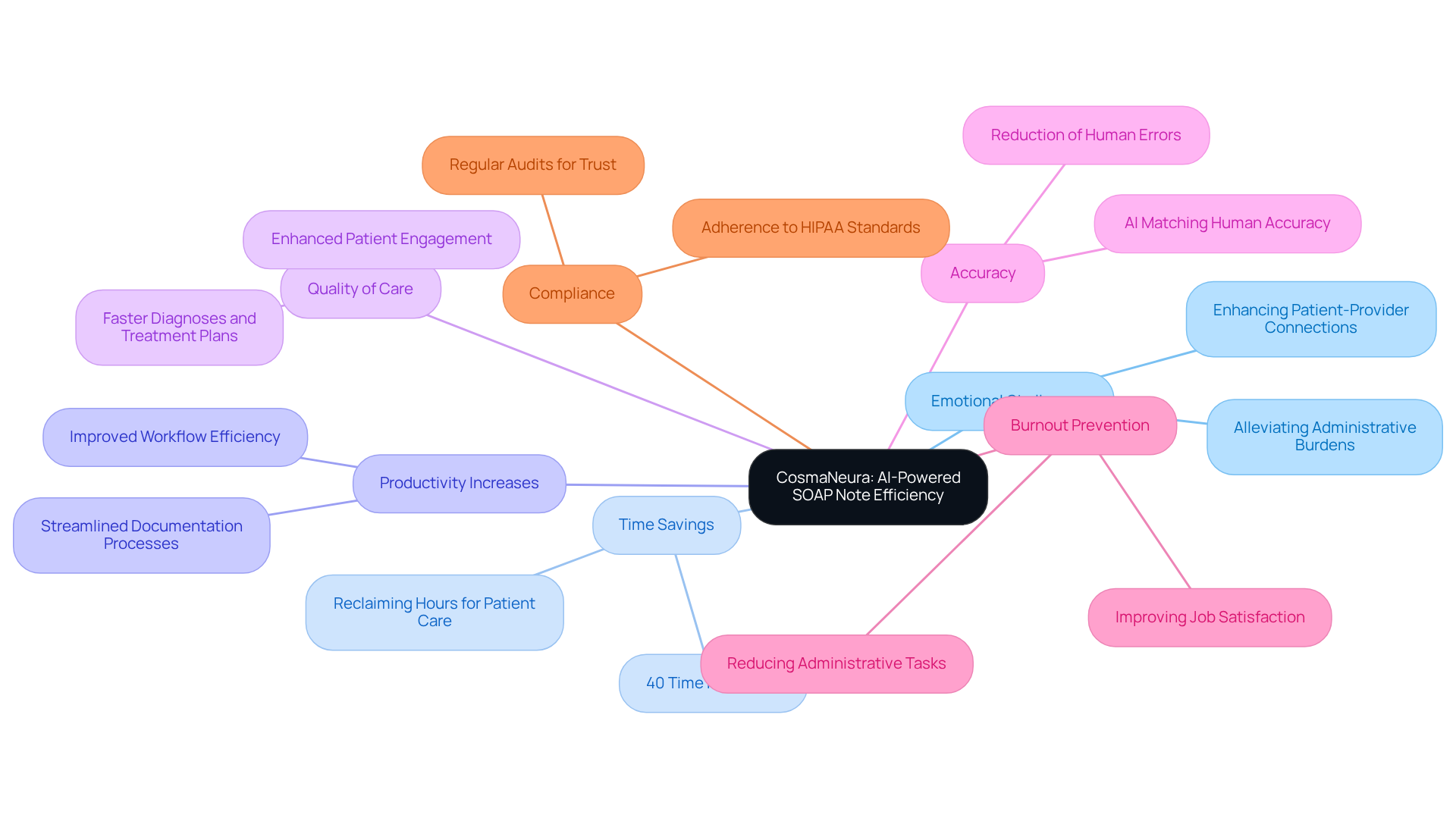
CosmaNeura: Streamline SOAP Note Documentation with AI-Powered Efficiency
Healthcare providers often face overwhelming administrative burdens that can detract from their ability to connect with patients. CosmaNeura's AI platform addresses this emotional challenge by creating a soap presentation example that transforms the development of SOAP notes. Imagine spending more time on meaningful client interactions rather than being bogged down by paperwork. By utilizing advanced algorithms, the platform gathers all relevant individual information with exceptional precision and effectiveness.
This automation significantly —by up to 40%—and reduces human errors. As a result, productivity increases, and the quality of care improves. Such advancements not only optimize workflows but also align with the goal of providing compassionate medical care. With the AI handling administrative tasks, providers can focus on what truly matters: the individuals they serve.
Moreover, the AI's ability to match or exceed human accuracy in generating clinical content is a strong soap presentation example that enhances the reliability of documentation. Think about the peace of mind that comes from knowing your records are accurate and trustworthy. By alleviating these burdens, the platform also helps prevent burnout among medical professionals, allowing for deeper engagement with patients.
Regular audits of the AI system are essential to maintain compliance and trust, reinforcing a commitment to ethical practices in healthcare. Let us embrace this technology together, ensuring that healthcare providers can thrive while delivering the compassionate care that patients deserve.
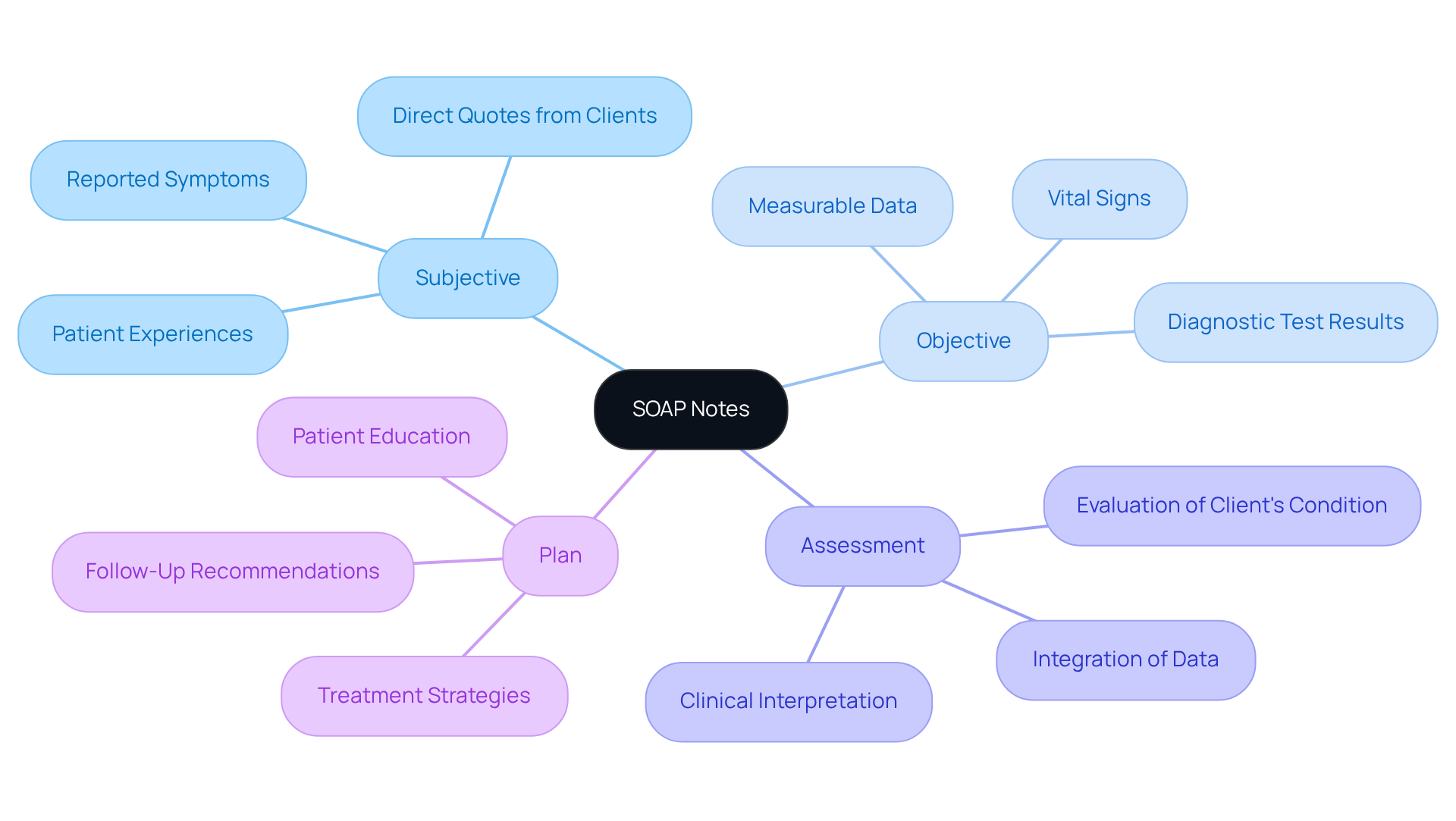
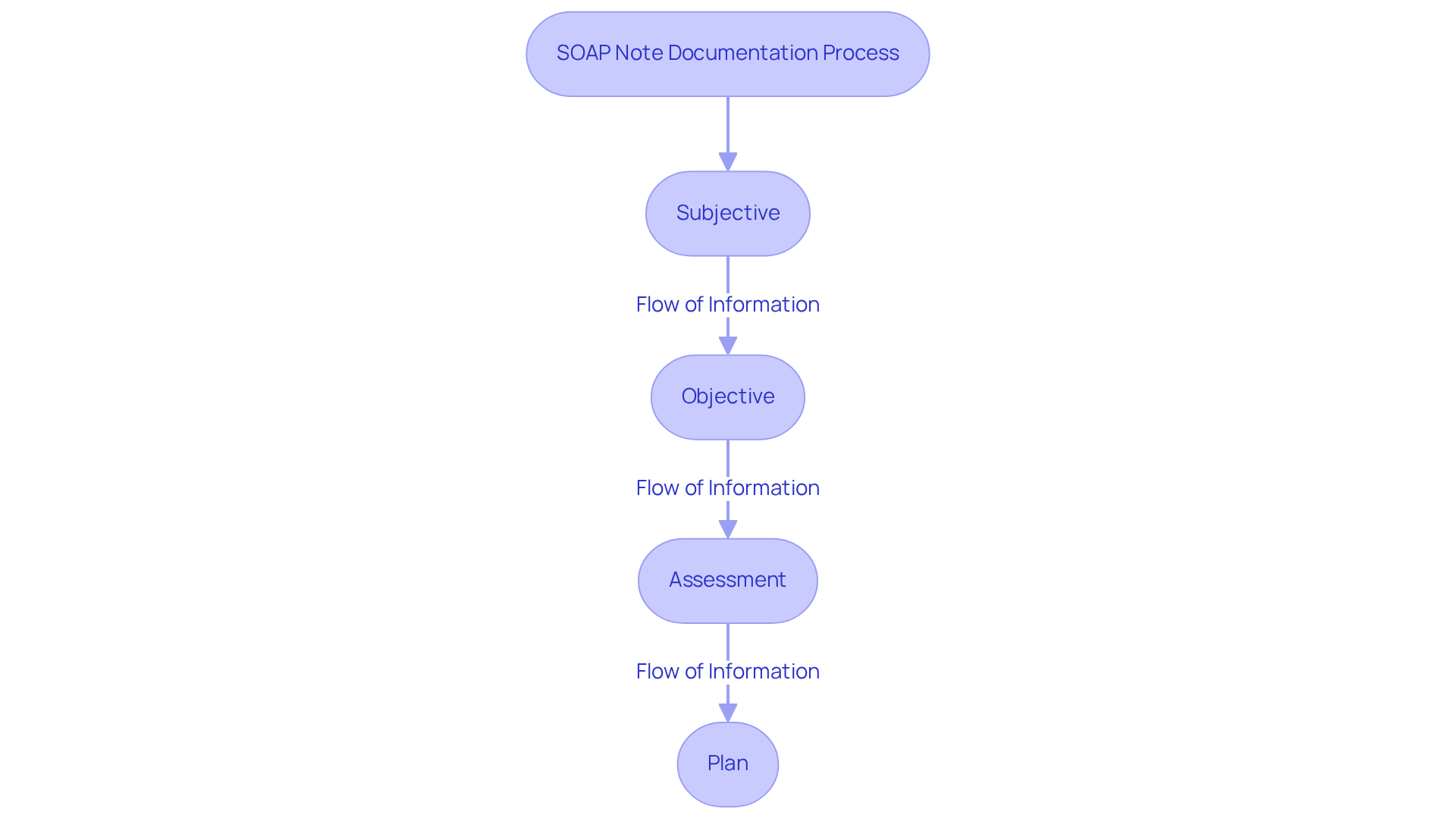
Understanding SOAP Notes: Key Components Every Provider Must Master
An example of a soap presentation illustrates how SOAP notes are structured into four essential components: Subjective, Objective, Assessment, and Plan. These components serve as a vital framework for understanding and addressing the complexities of .
- The Subjective section captures the individual's reported symptoms, feelings, and experiences, providing invaluable context for their condition. Have you ever thought about how these personal insights can shape our understanding of a patient’s journey?
- In contrast, the Objective section presents measurable data, including vital signs and diagnostic test results, which are critical for clinical evaluation.
- The Assessment combines both subjective and objective information to create a clinical interpretation, guiding your understanding of the individual's status. This integration is not just about data; it’s about seeing the whole person.
- Ultimately, the Plan details the subsequent actions in care, including treatment strategies and follow-up recommendations.
Mastering these components is essential for effective communication among medical providers, which can be illustrated by a soap presentation example, ensuring continuity of care and improving outcomes for those receiving treatment.
Research shows that a significant percentage of healthcare providers who excel in these components report enhanced record quality and better patient management. This improvement is not merely procedural; it directly impacts the quality of care patients receive. Moreover, including direct quotes from clients in the Subjective section can offer a more precise account of their experiences, further elevating the quality of SOAP records.
As electronic health records become more prevalent, the digitization of SOAP notes is essential for better accessibility and efficiency in documentation. Embracing these practices can lead to a more compassionate and effective healthcare environment.
Real-World SOAP Note Examples: Best Practices for Effective Documentation
- Example 1: An individual presents with headaches.
Subjective: 'I've been having severe headaches for the past week.'
Objective: Blood pressure 120/80, no neurological deficits.
Assessment: Likely tension headaches.
Plan: Recommend over-the-counter pain relief and follow-up in one week. - Example 2: A diabetic individual reports increased thirst.
Subjective: 'I can't seem to quench my thirst.'
Objective: Blood glucose level 250 mg/dL.
Assessment: Possible hyperglycemia.
Plan: Adjust medication and schedule a follow-up appointment.
Efficient record-keeping methods are essential in healthcare. Have you considered how precise and comprehensive entries can greatly improve health outcomes and patient satisfaction? Research shows that when we capture individual voices in records—like in the 32% of goals-of-care (GOC) records that utilized quotations—we foster a deeper connection with our patients. As Francis Peabody wisely stated, true healing involves genuinely caring for the individual's well-being. This compassion is reflected in .
Optimal methods for a soap presentation example involve ensuring clarity in the subjective section by directly quoting client statements, maintaining objectivity in the assessment, and outlining clear, actionable plans. Moreover, it’s crucial for medical providers to be aware of racial disparities in quotation use, as these can affect the quality of care received by various groups. By embracing these principles, we can enhance the quality of care and build trust with those we serve. Let’s work together to create a more compassionate healthcare environment.
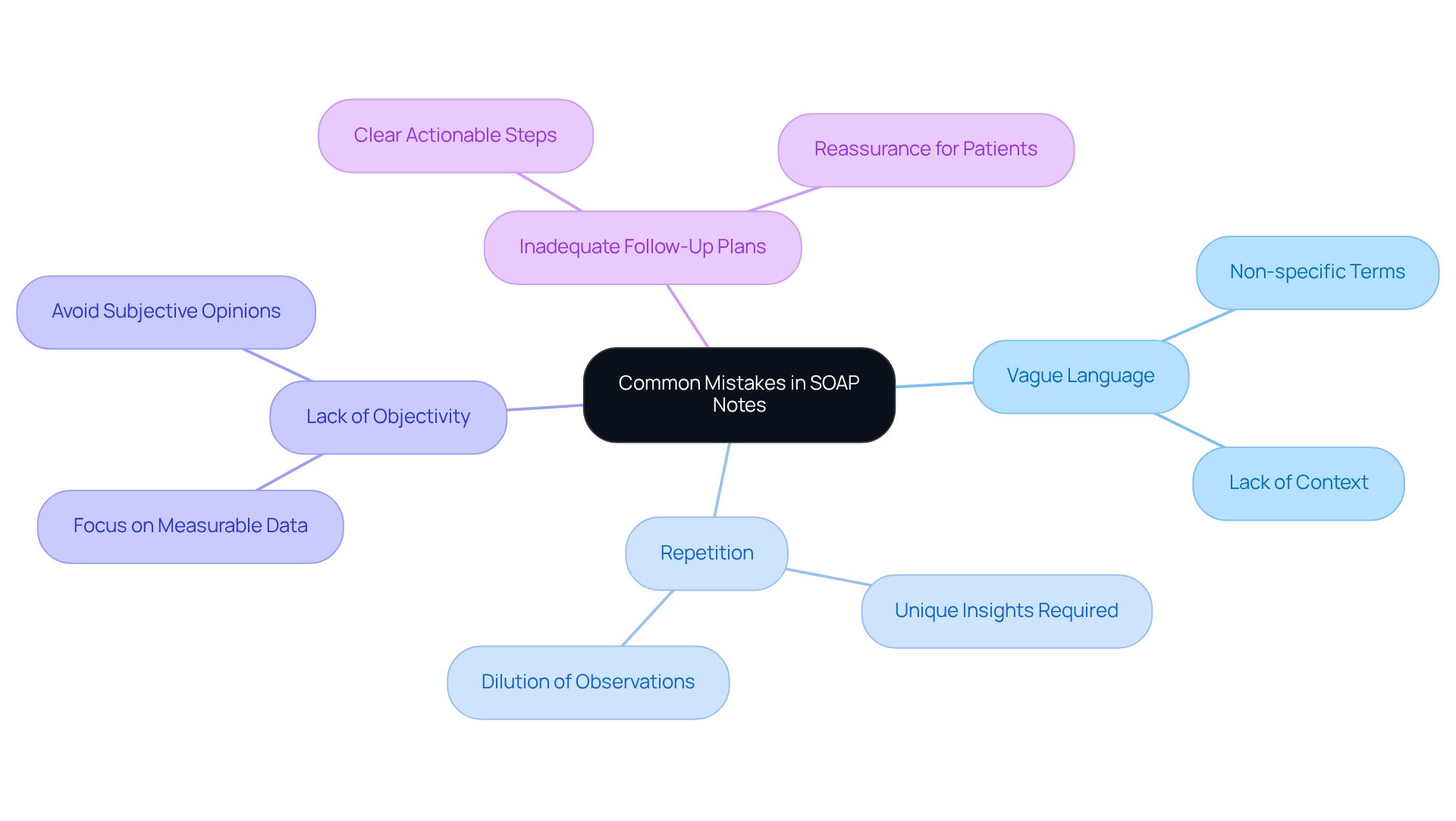
Common Mistakes in SOAP Notes: What Healthcare Providers Should Avoid
- Vague Language: It's important to avoid using non-specific terms like 'feels better' without context. Instead, strive for precision when describing symptoms to ensure clear communication.
- Repetition: Aim to provide unique insights in each part of the SOAP record. Avoid reiterating information across sections, as this can dilute the value of your observations.
- Lack of Objectivity: In the Objective section, focus on measurable data rather than subjective opinions. This ensures that your assessments are grounded in factual evidence, which is vital for effective patient care.
- Inadequate Follow-Up Plans: Always include clear and actionable next steps in the Plan section. This not only guides future actions but also reassures patients that their care is being .
Ethical Considerations in SOAP Notes: Ensuring Compliance and Best Practices
In the demanding world of healthcare, medical providers often face emotional challenges, particularly when it comes to maintaining ethical standards in documentation. Prioritizing confidentiality and obtaining informed consent are not just guidelines; they are essential for fostering trust. How can we ensure that our documentation remains impartial and accurately reflects our interactions with individuals?
Following HIPAA regulations is crucial for protecting individual information and upholding ethical standards. With 99% of medical professionals recognizing the importance of HIPAA compliance, it’s vital to adopt best practices that include:
- Clear documentation of consent
- Use of standardized templates
This not only streamlines the process but also alleviates some of the administrative burdens that can impact patient care.
However, it is concerning that 60% of medical professionals lack confidence in passing a HIPAA audit. This highlights the urgent need for proactive measures. As the OCR director wisely noted, "an ounce of prevention is worth a pound of cure." This underscores the significance of preventive compliance strategies.
Incorporating sophisticated tools, like Medwriter, can serve as a soap presentation example of a game-changer. These tools serve as a soap presentation example by automatically producing SOAP records that accurately reflect individual information while ensuring confidentiality. By focusing on these ethical factors, medical providers can enhance the quality of care they deliver while safeguarding individual rights. Together, let’s embrace these solutions to create a more supportive environment for both providers and patients.
Technology Tools for SOAP Notes: Enhancing Efficiency and Accuracy
- AI-Enhanced Record Tools: Imagine a world where healthcare professionals can spend less time on paperwork and more time caring for their patients. Platforms like CosmaNeura are making this a reality by offering a soap presentation example through the automation of SOAP records. This remarkable efficiency not only reduces the administrative burden but also enhances job satisfaction and professional wellbeing, allowing clinicians to focus on what truly matters—their clients.
- Electronic Health Records (EHR): Have you ever felt overwhelmed by the demands of data entry? Modern EHR systems come equipped with a soap presentation example that is designed to simplify this process, ensuring that your recordings are swift and precise. With the integration of AI capabilities, these systems enhance the consistency and reliability of medical records, as demonstrated in case studies showcasing .
- Mobile Applications: How often do you wish you could document your observations in real time? Tailored mobile apps for healthcare practitioners allow for immediate record-keeping, ensuring that important notes are captured during client interactions. This immediacy not only bolsters the accuracy of records but also fosters better communication among care teams, ultimately benefiting patient care.
- Voice Recognition Software: Have you considered how voice recognition technology could transform your documentation process? Advanced tools that convert speech to text are revolutionizing the way providers document care. By enabling clinicians to dictate records, these tools significantly lighten the administrative load. It's projected that integrating voice technology could save U.S. healthcare providers $12 billion annually by 2027, highlighting its potential to enhance workflow efficiency and reduce clinician burnout. This shift not only improves job satisfaction but also allows you to concentrate more on meaningful patient interactions.
Training and Education: Mastering SOAP Notes for Healthcare Providers
Healthcare providers often face emotional challenges in their roles, particularly when it comes to the demands of accurate record-keeping. The administrative burdens can feel overwhelming, impacting not only their efficiency but also the quality of patient care. Therefore, prioritizing ongoing training in the soap presentation example for recording notes is essential.
Utilizing a variety of methods—such as workshops, online courses, and peer reviews—can significantly and foster the exchange of best practices. Effective training programs, like those offered by ACMSO, focus on core responsibilities and proficiency in electronic health records (EHRs). These programs prepare providers for real-world scenarios, enhancing their confidence in managing patient information.
Moreover, mentorship programs can provide invaluable support to new providers. By offering advice on efficient record-keeping methods, these programs ensure that newcomers are equipped to maintain high standards in patient care. Continuous education is crucial; it not only improves record accuracy but also nurtures a culture of excellence in healthcare delivery.
Consider the benefits of engaging in these training opportunities:
- Improved accuracy in patient records
- Enhanced confidence in using EHRs
- Stronger support networks through mentorship
By investing in their professional development, healthcare providers can create a more compassionate and effective healthcare environment. Let’s embrace ongoing education and support each other in this journey toward excellence.
Telehealth and SOAP Notes: Adapting Documentation for Remote Care
In telehealth environments, modifying SOAP notes to the specifics of remote consultations is crucial for effective record-keeping. Have you considered how the Subjective section can capture comprehensive individual-reported symptoms? Emphasizing detailed narratives that reflect the individual's experience is vital for understanding their unique journey. In the Objective section, providers can include findings from virtual assessments, such as observations made during video consultations or data collected through remote monitoring tools. It is essential to document the Assessment and Plan clearly, as these elements guide follow-up care and ensure continuity in treatment.
Providers must also acknowledge the inherent limitations of telehealth, particularly the inability to conduct physical examinations. This necessitates a thoughtful . For example, when evaluating an individual's condition, clinicians may depend more significantly on medical history and reported symptoms, while clearly indicating any limitations in physical assessment. Additionally, specific training on managing telemedicine technology is crucial for medical providers to navigate these challenges effectively.
Despite these challenges, telehealth has been well-received by users, with high satisfaction rates reported, indicating its effectiveness in delivering care. Moreover, telemedicine can provide possible cost-saving benefits for medical systems, making it an appealing choice for both providers and individuals. However, disparities in access to telemedicine for certain patient groups remain a significant concern. How can we work together to create equitable solutions in medical delivery?
By tackling these challenges and adjusting their record-keeping strategies, medical providers can uphold the integrity and precision of their SOAP presentation examples in a remote care setting. Here are some key solutions to consider:
- Modify SOAP notes to reflect remote consultations.
- Emphasize detailed patient narratives in the Subjective section.
- Document virtual assessment findings in the Objective section.
- Clearly outline limitations in physical assessments.
- Seek training on telemedicine technology.
By embracing these strategies, we can continue to provide compassionate and effective care in the evolving landscape of telehealth.
Collaboration in SOAP Notes: Enhancing Teamwork for Better Patient Care
Exchanging SOAP documentation among healthcare team members is essential for maintaining continuity of care. Have you ever considered how collaborative documentation provides a comprehensive view of an individual's progress and treatment strategy? This ensures that all providers are informed and in agreement, fostering a sense of unity in care. Frequent team gatherings focused on reviewing SOAP entries not only enhance communication but also cultivate a cooperative approach to patient care. This teamwork can significantly improve the accuracy of SOAP records, leading to better outcomes for individuals.
In fact, studies reveal that effective collaboration in record-keeping can reclaim several hours each day for clinicians. Imagine the impact if healthcare providers could dedicate more time to patient care rather than administrative tasks. As the saying goes, 'Teamwork divides the task and multiplies the success.' By prioritizing collaboration in the soap presentation example within SOAP documentation practices, medical providers can elevate the quality of care they offer, embodying the compassionate spirit of their profession.
CosmaNeura stands out as the sole company developing AI solutions tailored for the faith-oriented healthcare sector. This unique position allows them to support this collaborative approach, further enhancing the efficiency and effectiveness of the soap presentation example in record keeping. Together, we can create a more .

The Future of SOAP Notes: Trends and Innovations for Healthcare Providers
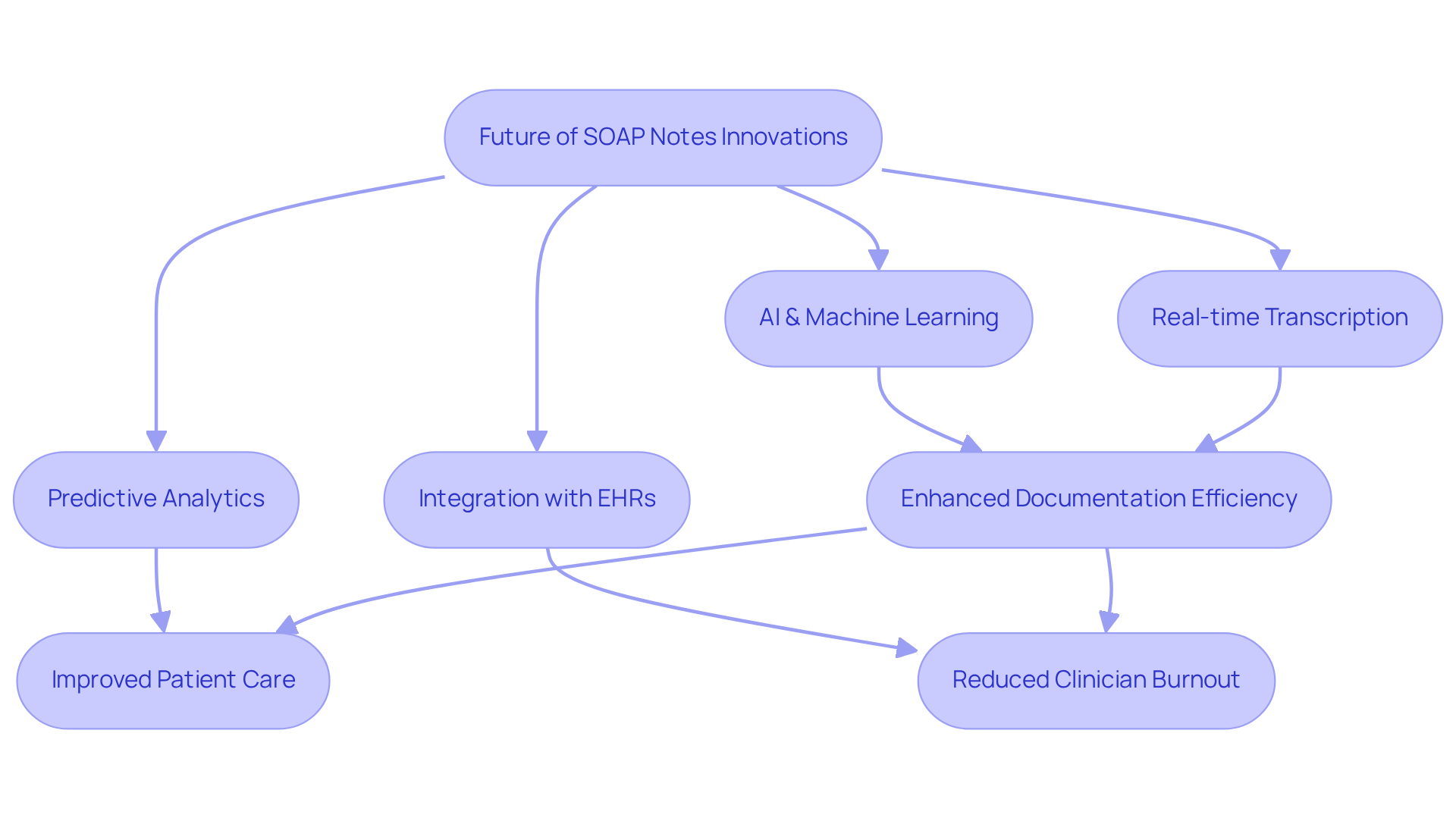
The future of SOAP records is set to undergo a profound transformation, driven by advancements in AI and machine learning. These innovations promise to automate and enhance the documentation process, alleviating some of the burdens healthcare providers face. Imagine real-time transcription and summarization during telehealth sessions—tools like CosmaNeura are already paving the way for immediate and accurate record-keeping.
As we look ahead, predictive analytics will play a vital role in improving outcomes, identifying trends and potential health risks. This proactive approach empowers healthcare providers to manage patient care more effectively. Furthermore, the seamless integration of the SOAP presentation example with electronic health records (EHRs) is expected to enhance workflows and foster better communication among medical teams. The ultimate goal? Improved care and satisfaction for individuals navigating their health journeys.
This shift towards not only boosts documentation efficiency but also has the potential to significantly reduce clinician burnout. By streamlining these processes, healthcare providers can dedicate more time to what truly matters: meaningful interactions with their patients.
How might these advancements change your daily practice? As we embrace these technologies, let’s support one another in this journey towards a more compassionate and efficient healthcare system.
Conclusion
The integration of effective SOAP note documentation in healthcare is vital for enhancing patient care and improving provider efficiency. Have you ever felt overwhelmed by the administrative tasks that take time away from meaningful patient interactions? By utilizing structured approaches and advanced tools, healthcare professionals can streamline their documentation processes while ensuring accuracy and compliance. Emphasizing the importance of both AI technologies and robust training programs, we see how these elements can significantly reduce administrative burdens, allowing providers to focus on what truly matters: compassionate patient care.
Key insights from this article highlight the necessity of mastering the four components of SOAP notes:
- Subjective
- Objective
- Assessment
- Plan
By avoiding common pitfalls and adopting best practices, healthcare providers can enhance the quality of their documentation, which directly correlates with improved patient outcomes. Collaboration and continuous education are essential in fostering a supportive environment for both providers and patients, creating a culture of care and understanding.
As the healthcare landscape evolves, embracing innovative technologies and refining documentation practices will be crucial. Engaging in ongoing training and adapting to new tools can empower healthcare professionals to deliver compassionate care while maintaining high standards of documentation. By prioritizing these strategies, the future of SOAP notes can lead to a more efficient, accurate, and patient-centered healthcare system. Together, let’s commit to fostering an environment where both providers and patients thrive.




