Overview
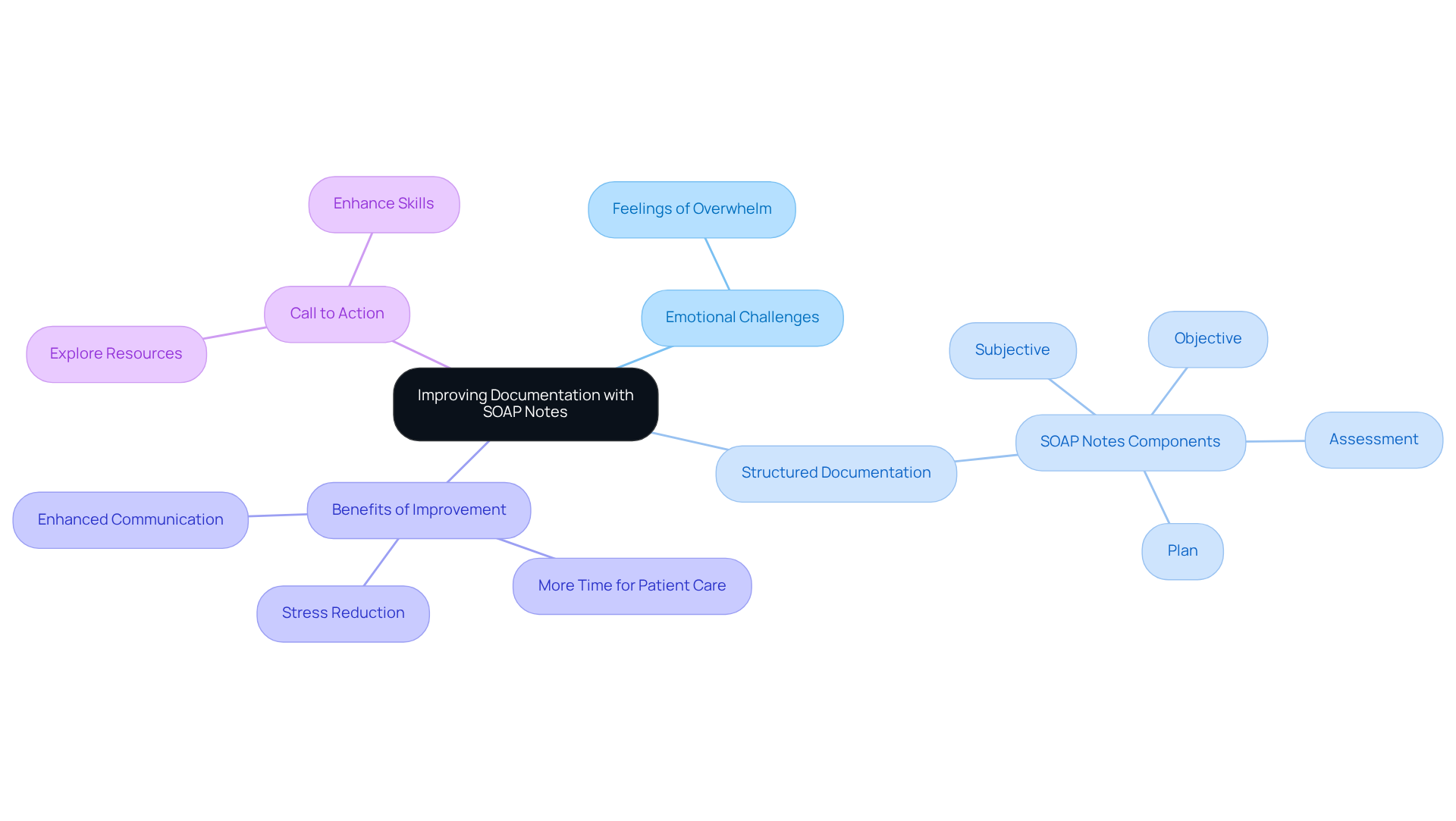
The article titled "7 SOAP Note Problem List Examples for Healthcare Providers" addresses the emotional challenges faced by healthcare professionals in managing documentation. It compassionately presents practical examples and templates for creating effective SOAP notes, recognizing the administrative burdens that can impact patient care. By highlighting how structured SOAP notes enhance communication and streamline documentation processes, it underscores the importance of organized record-keeping in clinical settings.
Are you feeling overwhelmed by the demands of documentation? This article offers solutions that not only improve patient care but also alleviate some of the stress associated with administrative tasks. With various examples and best practices, it illustrates how effective SOAP notes can serve as a supportive tool in your daily practice.
Embracing these structured approaches can lead to significant benefits, such as improved communication with colleagues and better patient outcomes. As you explore these examples, consider how they can be integrated into your workflow to foster a more efficient and compassionate care environment.
Take a moment to reflect on your current documentation practices. Are there areas where you could benefit from a more organized approach? This article encourages you to engage with the provided templates and examples, empowering you to enhance your documentation skills while ensuring that patient care remains at the forefront of your practice.
Introduction
In the fast-paced world of healthcare, the significance of accurate and efficient documentation is profound. SOAP notes are essential communication tools, ensuring that vital patient information is recorded and shared effectively among providers. This article delves into seven exemplary SOAP note problem lists that not only streamline the documentation process but also enhance the quality of care delivered to patients. Yet, as healthcare professionals embrace these structured formats, they often face the emotional burden of maintaining clarity and consistency in their records. What innovative solutions can bridge the gap between thorough documentation and compassionate patient care?
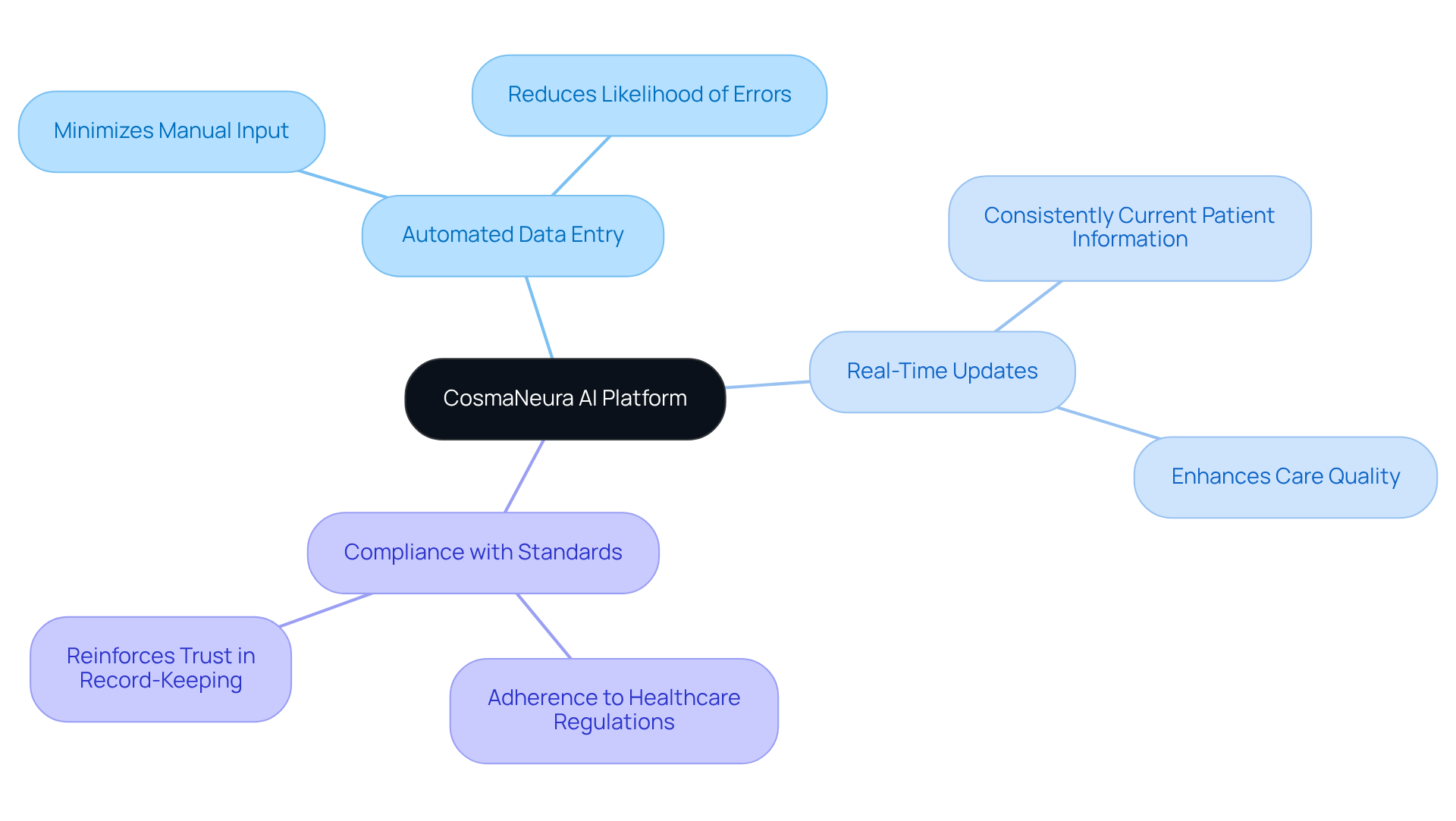
CosmaNeura: Streamline SOAP Note Documentation with AI Efficiency
CosmaNeura's AI platform transforms the creation of a soap note problem list example, allowing healthcare providers to focus on meaningful interactions with individuals instead of being bogged down by administrative duties. By automating the record-keeping process, providers can reclaim precious time and significantly reduce the risk of errors, ensuring that medical files remain accurate and up-to-date. This efficiency not only addresses the common apprehension towards innovation in healthcare—especially among physicians who worry about maintaining quality care—but also streamlines workflows in a sector often hesitant to embrace new technologies. The platform's seamless integration into existing systems further establishes its role as an essential ally for modern healthcare practices.
- Automated Data Entry: Minimizes manual input, thereby reducing the likelihood of errors.
- Real-Time Updates: Guarantees that patient information is consistently current, enhancing care quality.
- Compliance with Standards: Ensures adherence to healthcare regulations and ethical guidelines, reinforcing trust in the record-keeping process.
As Jessica Christie, ND, wisely notes, 'Timely, precise documentation contributes to well-recorded care and should be finalized quickly in accordance with institutional policies.' This underscores how the platform's features enhance , providing a soap note problem list example that fosters a more compassionate approach to care and enables providers to connect more meaningfully with those they serve.
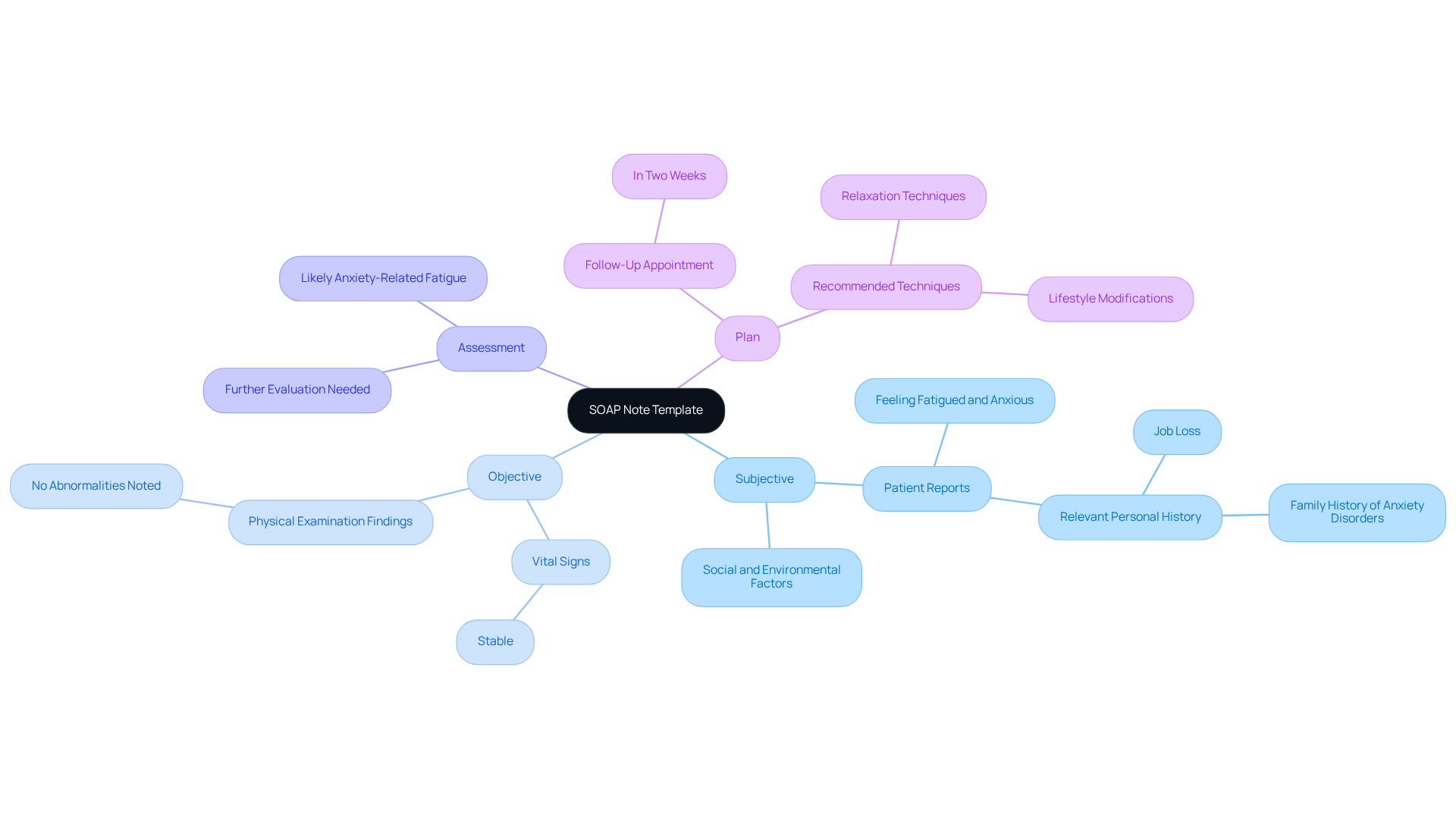
Heidi Health: Comprehensive SOAP Note Template with Examples
Heidi Health understands the emotional challenges healthcare professionals face. The robust SOAP note problem list example they provide includes illustrative examples for each section: Subjective, Objective, Assessment, and Plan. These templates are thoughtfully designed to assist in effectively gathering essential client information, ultimately enhancing the quality of clinical records. By utilizing generative AI, healthcare providers can simplify the documentation process, alleviating administrative burdens and allowing more time to focus on what truly matters—patient care.
- Subjective: Patient reports feeling fatigued and anxious, indicating a potential mental health concern.
- Objective: Vital signs are stable; no abnormalities noted during the physical examination, ensuring a comprehensive assessment of the individual's condition.
- Assessment: The symptoms suggest likely anxiety-related fatigue; further evaluation may be warranted to explore underlying issues.
- Plan: Schedule a follow-up appointment in two weeks to monitor progress; recommend relaxation techniques and lifestyle modifications to alleviate symptoms.
This organized method serves as a soap note problem list example, supporting and fostering continuity of care. It ensures that all pertinent individual information is documented and easily accessible, ultimately enhancing the patient experience. Are you ready to embrace a more efficient approach to documentation? Let’s work together to prioritize care and improve outcomes.
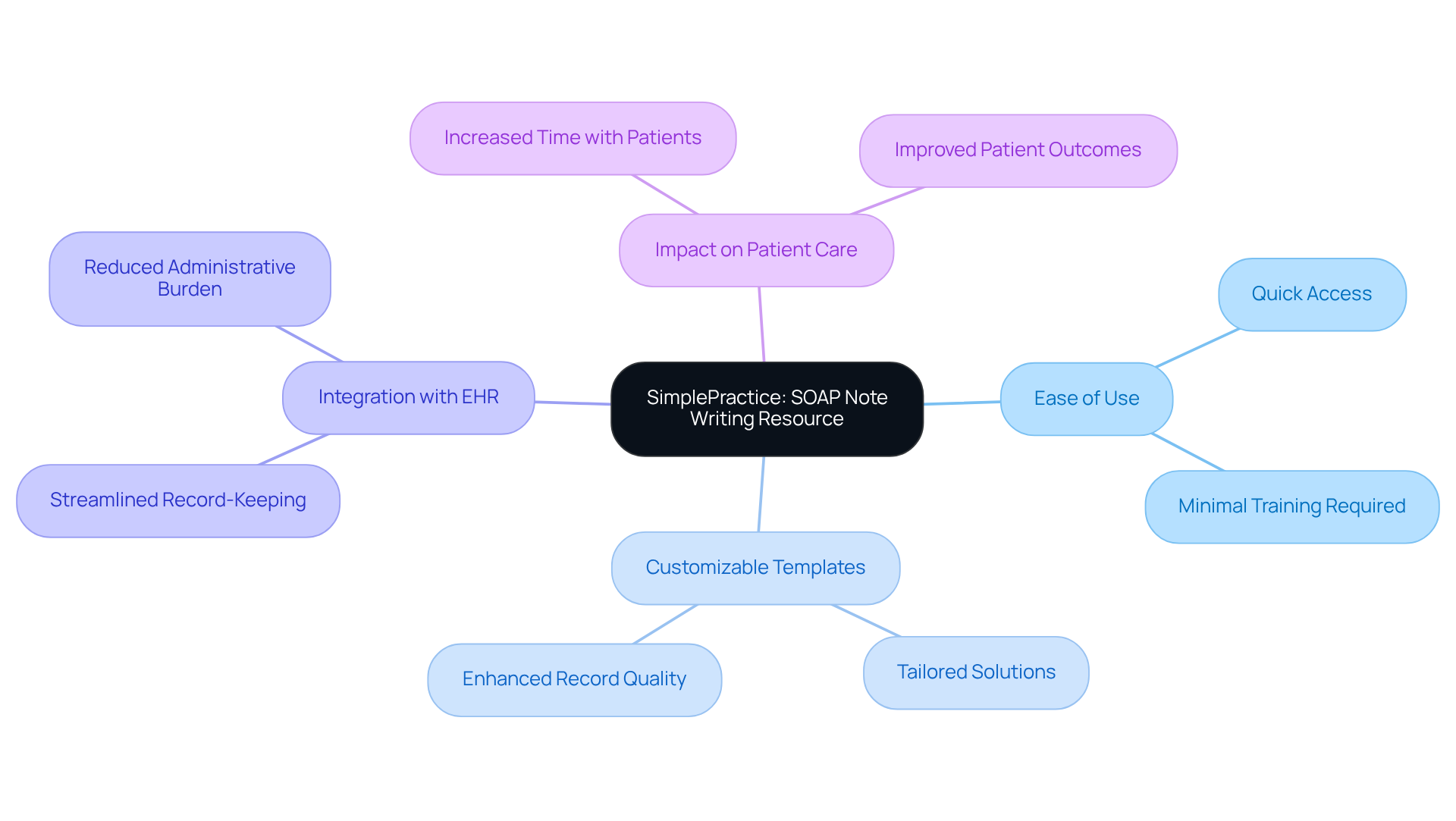
SimplePractice: User-Friendly SOAP Note Writing Resource
SimplePractice offers an intuitive platform for writing a soap note problem list example, making it easier for healthcare providers to document client interactions efficiently. With a user-friendly interface, navigating between sections becomes a breeze, allowing for the timely capture of important information. Given that typical doctor-client interactions last between seven and 17 minutes, this time constraint can often hinder effective communication and client education. By utilizing AI solutions, SimplePractice not only enhances administrative efficiency but also allows healthcare providers to focus more on direct care, addressing the pressing issue of physician burnout. Generative AI can significantly improve time management during these brief interactions, ensuring that healthcare providers can maximize the value of each client encounter.
Benefits:
- Ease of Use: Designed for quick access and minimal training, enabling providers to spend more time with patients.
- Customizable Templates: Tailor the soap note problem list example to meet specific practice needs, thereby enhancing the quality of records.
- Integration with EHR: Seamlessly connects with electronic health records for streamlined record-keeping, reducing the burden of administrative tasks and enhancing overall care delivery.
Healthcare providers using SimplePractice have shared their experiences of significant improvements in documentation efficiency, with many noting a reduction in time spent on paperwork. This shift not only boosts productivity but also contributes to , allowing clinicians to dedicate more time to direct patient care. How might your practice benefit from a tool that understands your needs and helps you focus on what truly matters—your patients?
Physio-pedia: In-Depth Guide to Writing SOAP Notes
Healthcare providers often face emotional challenges as they navigate the complexities of documentation. These administrative burdens can significantly impact patient care, leaving many feeling overwhelmed. It's essential to address these concerns with compassion and understanding.
Physio-pedia offers a comprehensive guide to writing structured documentation, ensuring that each element's purpose is clear and the techniques are optimal. This resource is invaluable for those looking to enhance their documentation skills, ultimately benefiting their patients.
Imagine the relief of improving your documentation process—less stress, more time for patient care, and enhanced communication. By utilizing this guide, you can transform your approach, making documentation a tool for better patient outcomes rather than a burden.
We encourage you to further. Take the first step towards improving your skills and, in turn, enhancing the care you provide. Together, we can make a difference in the lives of those we serve.
Social Work Portal: SOAP Notes Guide for Social Workers
The Social Work Portal provides a compassionate guide for creating structured documentation tailored to social work practice. This essential resource highlights the significance of , ensuring that every voice is heard and understood.
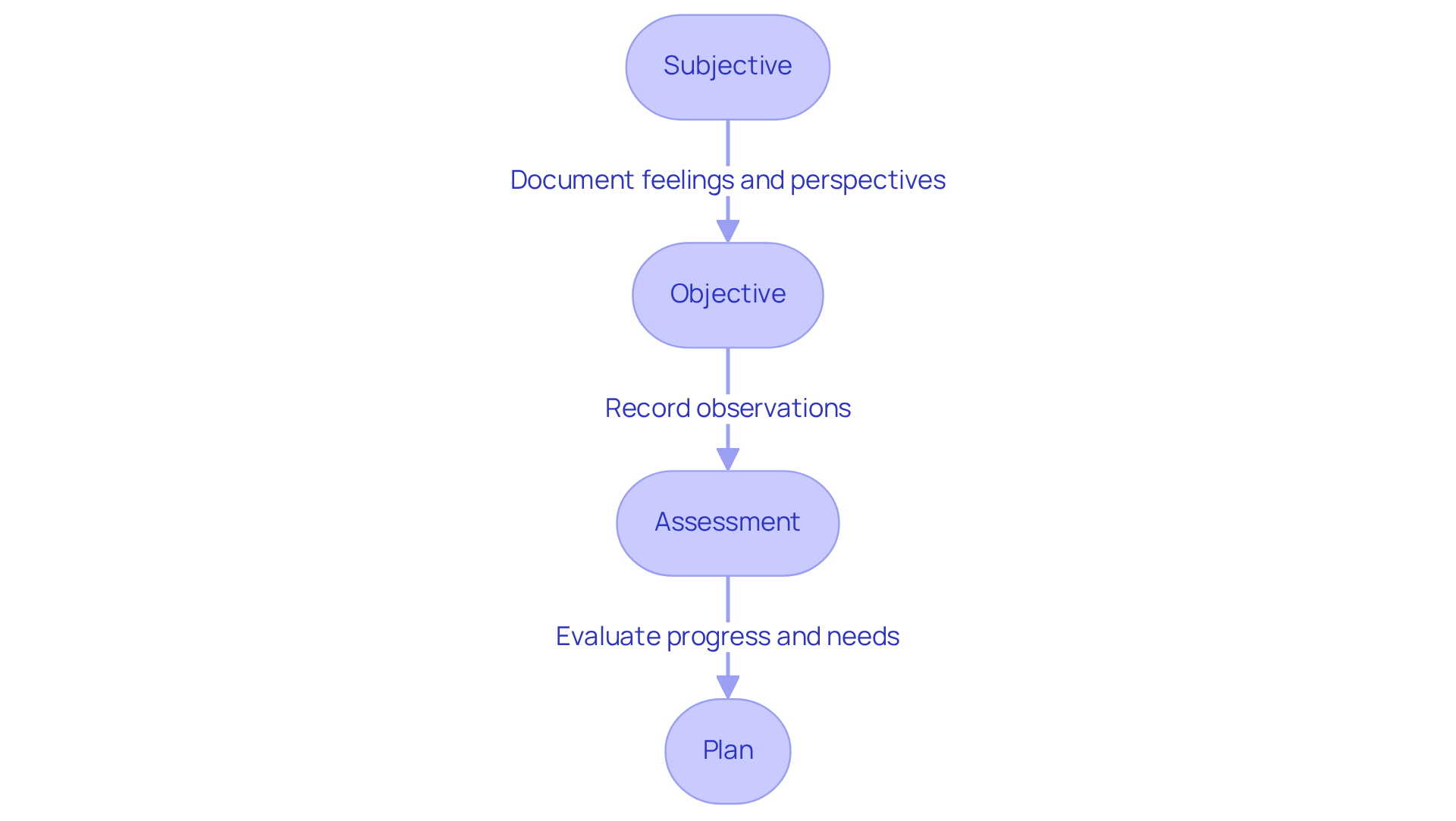
- Subjective: Reflect on the client's feelings and perspectives about their situation. How do they perceive their journey?
- Objective: Document the observations made during sessions. What did you notice that could inform future interactions?
- Assessment: Evaluate the client's progress and needs. Where are they thriving, and where might they need additional support?
- Plan: Outline strategies for future sessions and interventions. How can we best support their growth moving forward?
By focusing on these key components, social workers can enhance their practice, fostering deeper connections with clients while navigating the complexities of their roles.
NCBI: Clinical Significance and Best Practices for SOAP Notes
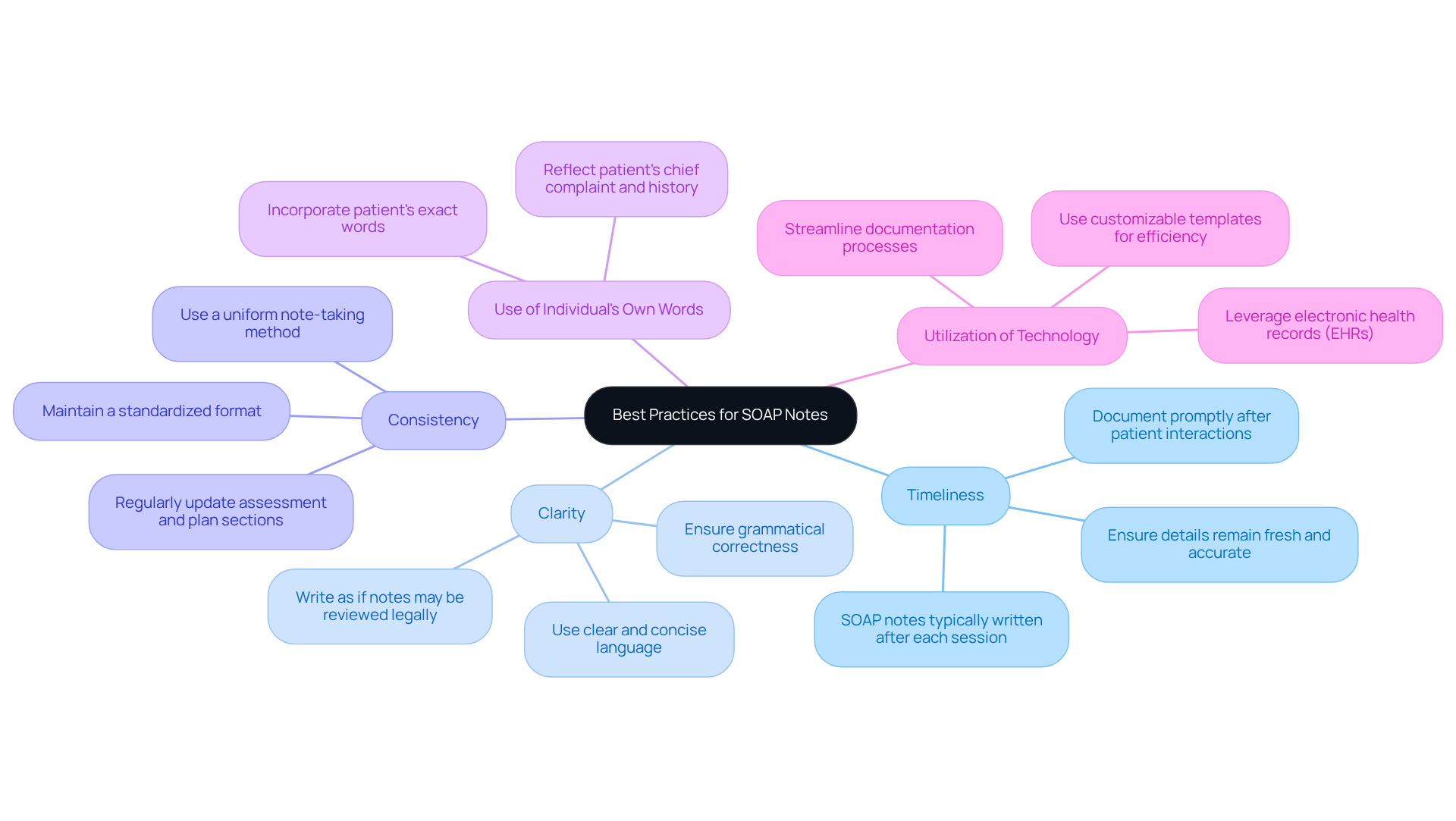
The NCBI highlights the clinical importance of structured documentation, underscoring their function in enhancing communication among healthcare professionals and advancing care for individuals. Best practices for writing SOAP notes include:
- Timeliness: Document notes promptly after patient interactions. This practice is crucial, as it ensures that the details remain fresh and accurate, ultimately .
- Clarity: Use clear and concise language to avoid ambiguity. Remember, written materials should be grammatically correct and composed with the understanding that they may be examined legally or clinically.
- Consistency: Maintain a standardized format for all records. A uniform note-taking method, like the soap note problem list example, enhances the consistency of medical records, making it easier for all providers to understand patient histories.
- Evaluation Result: Content Rewrite Evaluation
Overall Feedback on Use of Provided Context
The rewritten section effectively emphasizes the clinical significance of SOAP notes and integrates best practices for documentation. It accurately reflects the information from the external sources, including relevant statistics and case studies. The structure is clear and aligns well with the needs of healthcare providers, maintaining a focus on actionable insights.
Areas for Improvement
- Timeliness: The rewritten section mentions the importance of documenting notes promptly after patient interactions, which aligns with the external sources. However, it could further highlight the statistic that SOAP records are generally created after each session or patient interaction, reinforcing the importance of prompt record-keeping.
- Clarity: Although the revised segment recommends employing clear and concise language, it could improve by directly mentioning the quote regarding the necessity for written materials to be grammatically correct and composed as if they might be examined legally or clinically. This would enhance the authoritative tone regarding clarity in documentation.
- Consistency: The section highlights upholding a standardized format for all records, which is pertinent. However, it could also include the key point that the uniform note-taking method of SOAP notes, such as the soap note problem list example, improves the consistency of medical records, offering additional support for this best practice.
- Use of Individual's Own Words: The revised section includes the practice of incorporating the individual's exact words, which is beneficial. It could be enhanced by citing the specific point that the subjective section should incorporate the individual's primary concern and pertinent history, ensuring thorough records.
- Regular Updates: The significance of consistently refreshing the assessment and plan sections is noted, but it could be improved by incorporating the statistic that regular updates encourage consistency in records, which is vital for effective patient management.
- Avoid Subjective Statements: The rewritten section advises sticking to observable facts, which is aligned with the external sources. It could be enhanced by clearly citing the guideline to avoid unverifiable subjective statements, which boosts the integrity of the records.
- Utilization of Technology: The mention of leveraging electronic health records (EHRs) is relevant. However, it could be more influential by incorporating the key aspect that EHRs streamline the procedure of obtaining client signatures on clinical documentation, emphasizing the efficiency achieved through technology.
Headway: Therapy-Focused SOAP Note Templates and Examples
Headway recognizes the unique challenges faced by mental health practitioners in maintaining accurate records. Customized templates for progress reports are designed specifically for your needs, streamlining the process of recording client interactions. By capturing essential information in a structured format, you can focus more on what truly matters—your clients. As emphasized by SimplePractice, clarity is paramount; avoiding ambiguous language or unnecessary details ensures that your records are as clear as possible.
- Subjective: Client reports feelings of sadness and isolation, stating, 'I feel like I'm all alone.'
- Objective: Client appears withdrawn, exhibiting minimal eye contact and a flat affect.
- Assessment: Indicators suggest depression; a referral for further evaluation may be warranted.
- Plan: Continue with weekly therapy sessions, focusing on exploring coping strategies and enhancing social support.
Organized clinical records, such as a soap note problem list example, not only enhance transparency in your writing but also align with contemporary trends in mental health practices that emphasize the need for accurate and systematic documentation. Have you considered composing session summaries right after each meeting? This practice guarantees and can significantly improve your workflow. By effectively utilizing these templates, you can enhance communication, ensure continuity of care, and meet compliance standards, ultimately leading to better patient outcomes. However, it's important to recognize that the quality of clinical notes can vary among providers, which might lead to challenges in maintaining consistency in documentation.
Upheal: Telehealth SOAP Note Examples for Remote Care
Upheal offers customized illustrations of clinical notes specifically designed for , enabling healthcare providers to document remote interactions with clarity and precision.
Telehealth SOAP Note Example:
- Subjective: Patient reports increased anxiety during the pandemic, expressing concerns about isolation and stress management.
- Objective: No physical examination was performed; the session was conducted via video, allowing for visual assessment of the individual's demeanor.
- Assessment: Anxiety worsened by current events; the individual may benefit from exploring teletherapy options to address mental health needs.
- Plan: Schedule weekly telehealth sessions to provide ongoing support; offer resources for coping strategies and stress management techniques.
The transition to telehealth has significantly impacted the efficiency of creating a SOAP note problem list example. Providers can now document interactions more swiftly, as the structured format, including a soap note problem list example, allows for quick reference to client concerns and treatment plans. However, challenges persist, especially in capturing detailed interactions with individuals that may be less visible in a virtual environment.
For instance, a clinician may observe, "Patient expressed frustration with technology during the session, which affected communication flow." This highlights the importance of addressing technical issues that can hinder effective record-keeping and care for individuals.
By implementing efficient medical records in remote healthcare environments, providers can ensure thorough documentation that supports both clinical decision-making and patient involvement.
Key Solutions to Enhance Telehealth Documentation:
- Foster open communication about technical challenges.
- Provide training on telehealth tools for both providers and patients.
- Encourage feedback to improve the virtual experience.
In these ways, we can nurture a supportive environment that prioritizes patient care and enhances the telehealth experience.
SonderMind: Mental Health SOAP Note Writing Resources
SonderMind understands the emotional challenges faced by mental health practitioners, particularly when it comes to documentation. The administrative burdens can weigh heavily, impacting the quality of patient care. To alleviate this stress, SonderMind offers a variety of tools specifically designed to .
Our customizable templates serve as a soap note problem list example, catering to various mental health conditions and allowing practitioners to tailor their records to meet specific client needs. How much easier would your documentation be with a personalized approach?
- Examples: Real-world instances serve as practical guides, showcasing effective record-keeping methods, including a soap note problem list example, that enhance clarity and precision. Imagine the confidence you'll gain from knowing you're following best practices.
- Best Practices: Tips for accurately capturing client interactions are essential for maintaining comprehensive records. These records are vital for ongoing treatment and assessment, ensuring that every client receives the care they deserve.
Focusing on customized records not only facilitates effective communication among healthcare providers but also elevates the quality of care provided to clients. By utilizing these resources, mental health experts can ensure their documentation is both effective and aligned with current reporting trends. Integrating SMART objectives into clinical documentation can further enhance treatment planning and outcomes for individuals.
Take the next step towards improving your practice. Explore how these tools can support you in delivering compassionate care, allowing you to focus more on what truly matters—your clients.
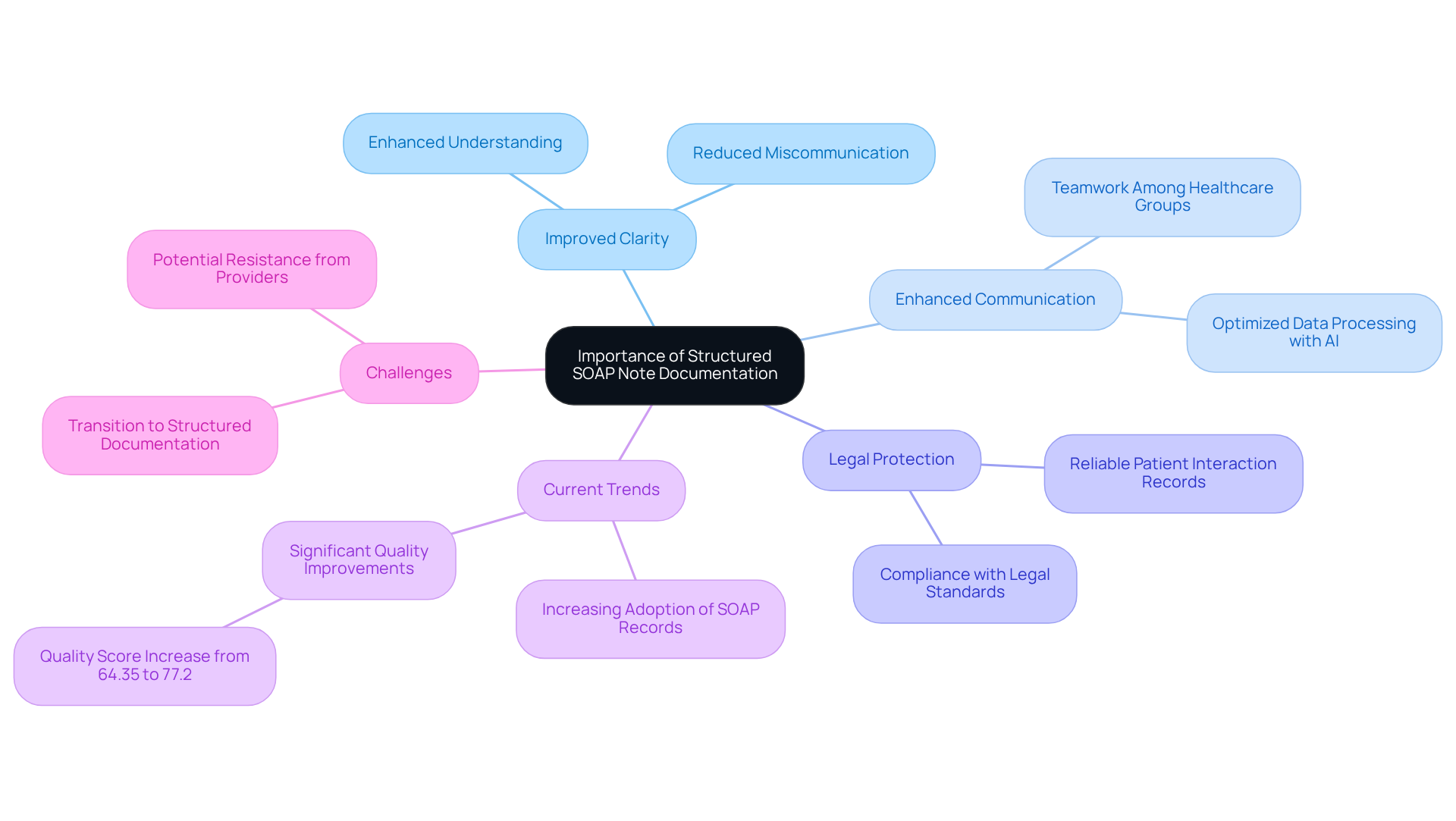
Heidi Health: Importance of Structured SOAP Note Documentation
Heidi Health emphasizes the significance of organized SOAP record documentation in enhancing care and communication among healthcare professionals. This organization not only improves monitoring of individual development but also ensures that essential details are readily available, especially when integrated with like CosmaNeura's Agentic Platform.
Improved Clarity: Clear organization of patient information significantly enhances understanding and reduces the risk of miscommunication.
Enhanced Communication: Organized records foster teamwork among healthcare groups, enabling smooth information exchange and coordinated care. Generative AI technologies further optimize data processing, making communication even more effective.
Legal Protection: These records provide a reliable account of patient interactions, crucial for legal compliance and safeguarding against potential disputes.
Current trends indicate an increasing adoption of organized SOAP records among healthcare professionals, with the soap note problem list example highlighting the need for improved record quality. Research shows that organized documentation can lead to a remarkable enhancement in the quality of clinical records, with average quality scores rising from 64.35 for unorganized records to 77.2 for organized records (p < 0.001). This transformation not only streamlines workflows for providers but also enriches the overall patient experience. Patients feel more understood and cared for when their information is organized and accessible. As Tom Ebbers from Radboud University Medical Center noted, "This study demonstrated that structured and standardized recording led to an increase in the quality of entries in the EHR."
Moreover, the introduction of organized and standardized records in EHRs, including a soap note problem list example, is highly recommended due to the substantial improvement in note quality. However, it is essential for healthcare providers to also consider the potential challenges that may arise during the transition to structured documentation systems. How can we support each other in this journey towards improved patient care?
Conclusion
The integration of structured SOAP note documentation is essential for healthcare providers who strive to improve patient care while managing the complexities of administrative tasks. By embracing efficient tools like those offered by CosmaNeura and Heidi Health, practitioners can alleviate the burdens of documentation, ensuring that their records are both accurate and timely. This transformation not only nurtures meaningful interactions between patients and providers but also enhances the quality of care, allowing practitioners to focus on what truly matters—patient well-being.
Throughout this discussion, various platforms have been highlighted, showcasing their unique features and benefits, such as:
- Automated data entry
- Real-time updates
- Customizable templates
These innovations address the common challenges that healthcare professionals encounter, including time constraints and the risk of errors. Ultimately, they lead to more effective communication and improved patient outcomes. The emphasis on best practices—particularly clarity and consistency in documentation—further underscores the necessity of organized records in clinical settings.
As the healthcare landscape evolves, adopting structured SOAP notes becomes not just a recommendation but a vital necessity for enhancing patient management and care delivery. Are you ready to explore these tools and resources? Taking proactive steps to improve your documentation practices can make a significant difference. By prioritizing efficient record-keeping, we can shift our focus back to the heart of healthcare—compassionate, quality care for every individual.




