Overview
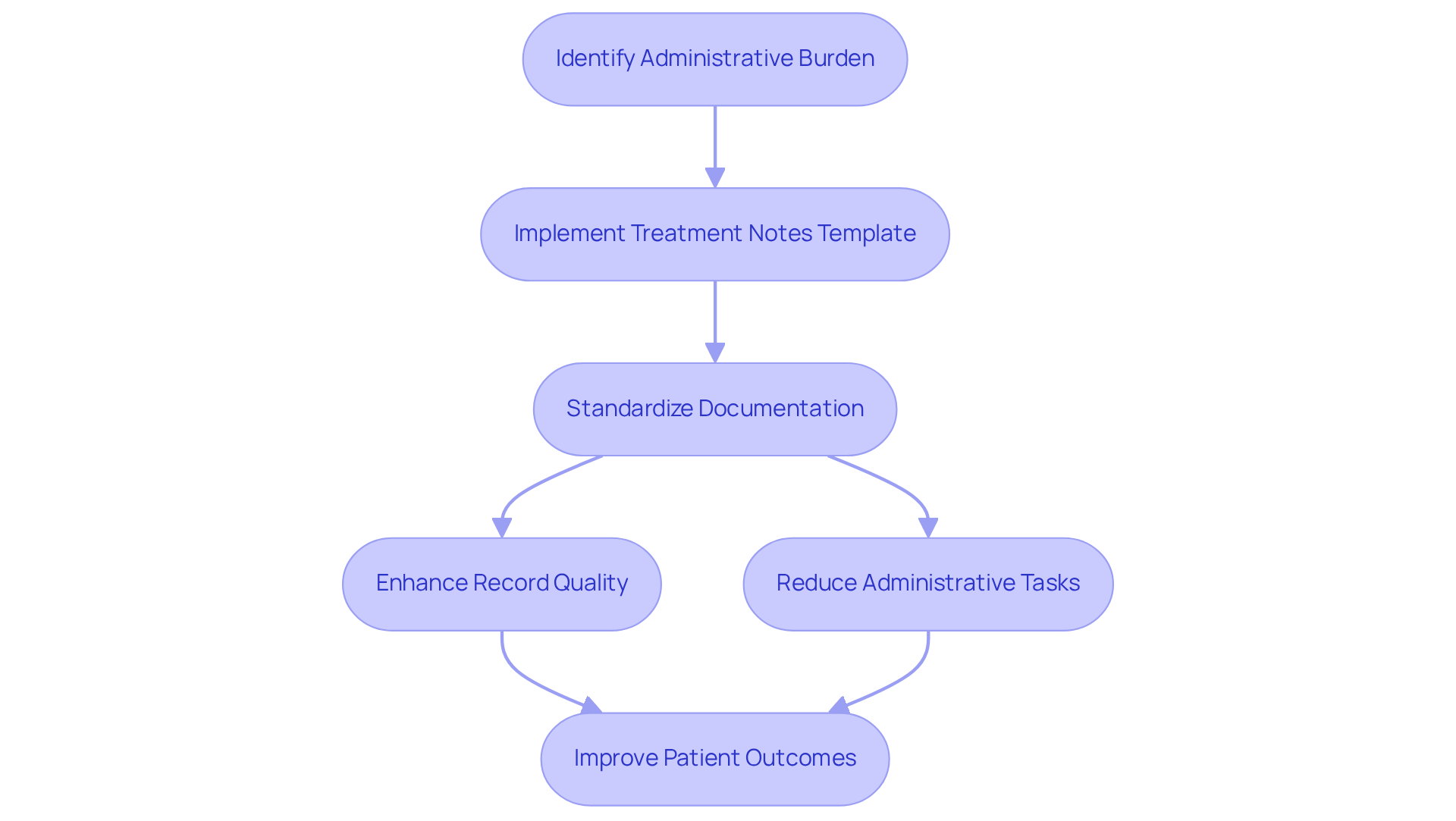
Healthcare providers often face overwhelming emotional challenges as they navigate their demanding roles. The burden of administrative tasks can detract from the quality of patient care, leaving professionals feeling stretched thin. This article offers essential treatment notes templates designed to streamline documentation processes and enhance patient support.
Structured templates, such as SOAP notes and customizable clinical notes, provide a practical solution. These tools not only improve record quality but also foster better communication among providers. By utilizing these templates, healthcare professionals can dedicate more time to what truly matters: supporting their patients.
Imagine the difference it could make if you could reduce the time spent on paperwork. With these templates, you can enhance your efficiency and focus on delivering compassionate care. By embracing these structured approaches, you’re not just improving your workflow; you’re also enriching the patient experience.
We invite you to explore these templates and see how they can transform your practice. Together, we can alleviate some of the pressures you face, allowing you to prioritize patient care above all else.
Introduction
The landscape of healthcare documentation is evolving, and it’s important to recognize the emotional challenges that healthcare providers face. The urgent need for efficiency and accuracy in patient care can feel overwhelming. As providers grapple with the complexities of record-keeping, the introduction of specialized treatment notes templates emerges as a transformative solution. These templates not only streamline documentation processes but also enhance the quality of care delivered to patients.
Yet, amidst these advancements, one might wonder: how can healthcare professionals ensure that their documentation practices remain both effective and compassionate? This article delves into ten essential templates that address these concerns, ultimately fostering a more nurturing environment for both providers and patients alike. By embracing these tools, we can support one another in navigating the complexities of healthcare documentation, ensuring that compassion remains at the forefront of our practices.
CosmaNeura: AI-Powered Treatment Notes Automation for Healthcare Providers
CosmaNeura is transforming the way healthcare providers manage treatment notes template through its innovative AI-powered platform. Designed with primary healthcare practitioners in mind, particularly those who uphold Christian principles, CosmaNeura serves as an effective treatment notes template to alleviate the burden of record-keeping. This allows clinicians to dedicate more time to supporting their patients, rather than getting lost in administrative tasks.
Imagine the relief of simplifying record-keeping while adhering to ethical guidelines rooted in Catholic teachings. This approach not only streamlines processes but also ensures that practices uphold the highest standards of moral responsibility. However, many traditional accelerators often overlook the needs of healthcare startups, which can hinder innovation in this vital sector.
Insights from over 40 customer interviews have illuminated these challenges, underscoring the urgent need for solutions that enhance operational efficiency. With 72% of healthcare leaders expressing trust in AI to , the platform significantly boosts operational efficiency. This shift allows providers to focus on what truly matters: delivering compassionate care.
As we look to the future, the integration of AI into healthcare records is projected to reduce clinical record-keeping time by 50% by 2027. This promising development highlights the potential for improved health outcomes and greater patient satisfaction. Let us embrace this change together, fostering a healthcare environment that prioritizes both efficiency and empathy.
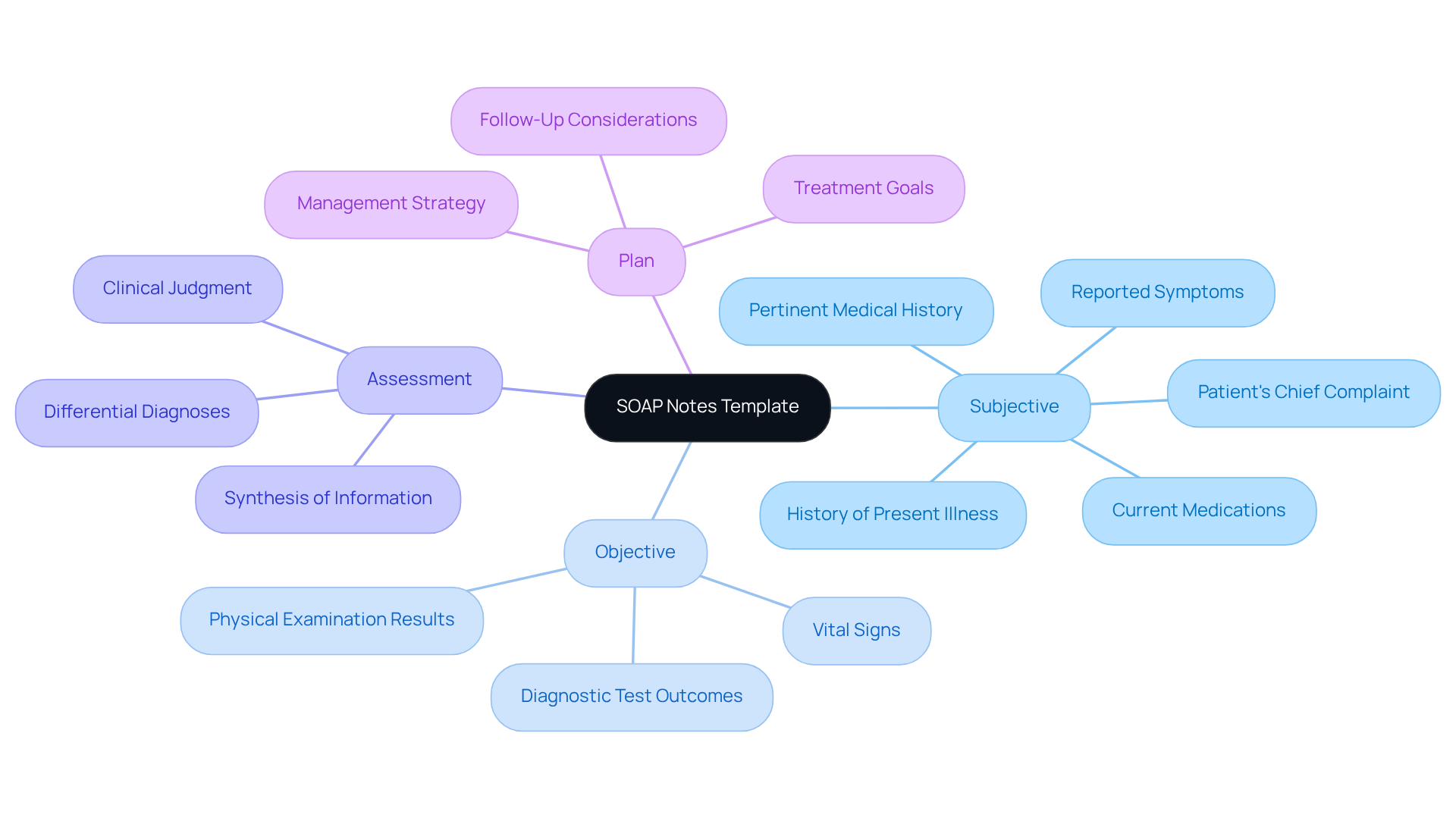
SOAP Notes Template: A Structured Approach to Patient Documentation
The SOAP (Subjective, Objective, Assessment, Plan) notes template is essential for effective clinical documentation. This organized approach helps healthcare providers capture comprehensive client information systematically. Have you ever felt overwhelmed by the amount of information you need to record? The subjective section includes the individual's reported symptoms, while the objective section captures quantifiable data like vital signs and physical examination results. The assessment synthesizes this information into a clinical judgment, and the plan outlines the next steps in treatment.
Research indicates that using SOAP records can significantly enhance writing quality. In fact, studies show that total scores for record quality improved from a baseline of 21.9 to 61.8 after training interventions (p<0.001). Imagine the difference it could make in your daily practice! Healthcare professionals who adopt this method often report improved communication among providers, ensuring that vital client information is easily accessible and fostering continuity of care.
With over 225,000 healthcare professionals nationwide, their widespread use underscores their effectiveness in promoting structured and clear documentation practices. To further enhance your skills in using SOAP records, consider regularly practicing their composition. This simple step can improve your documentation abilities and ultimately elevate the care you provide to individuals. Remember, every effort you make contributes to better patient outcomes.
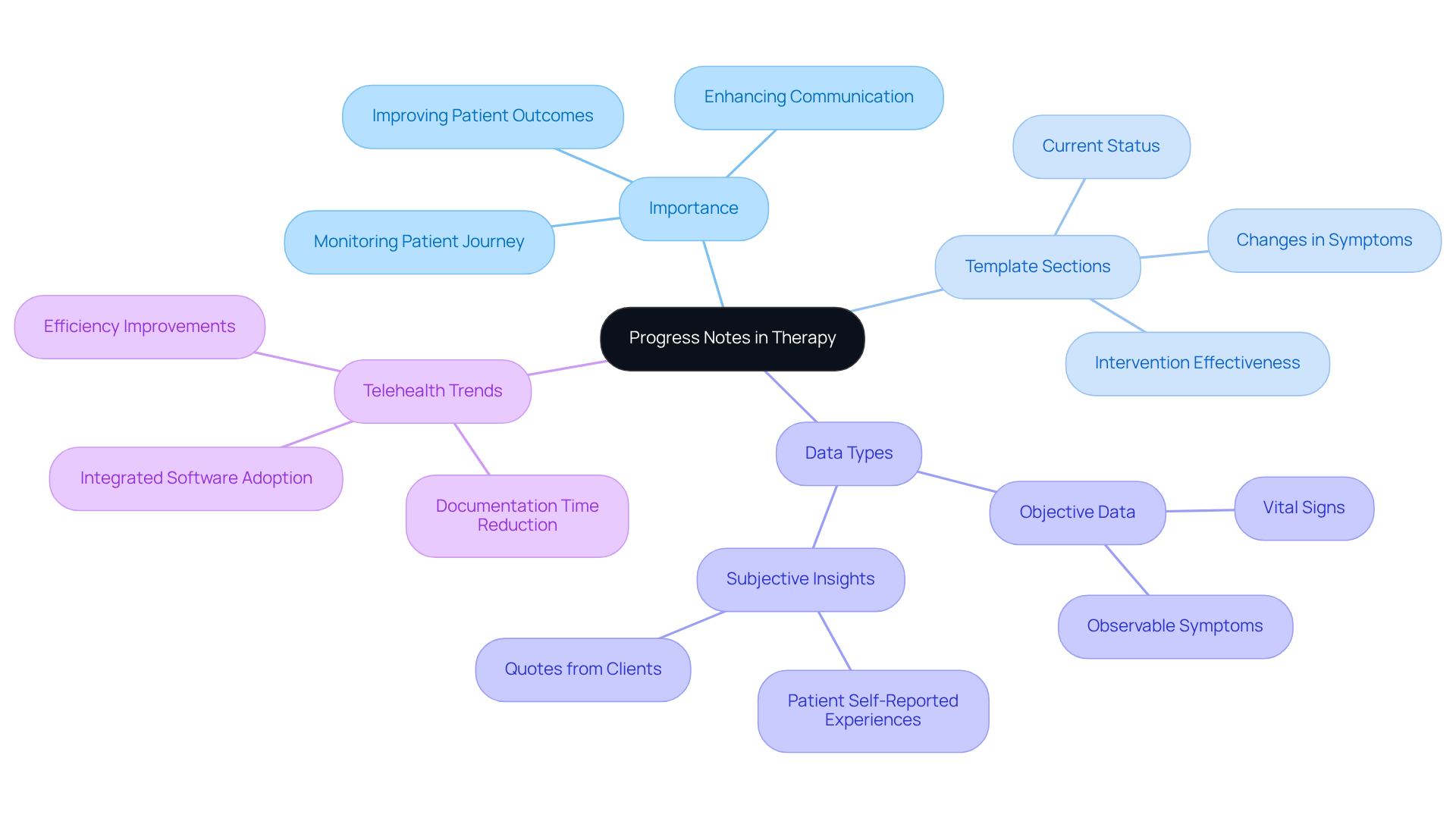
Progress Notes Template: Essential for Monitoring Patient Development
Progress records play a crucial role in monitoring an individual's journey through therapy. Have you ever considered how these records reflect not just data, but the emotional landscape of those in care? A well-organized treatment notes template usually includes sections for documenting the individual's current status, changes in symptoms, and the effectiveness of interventions.
Consistently revising the treatment notes template empowers healthcare professionals to make informed decisions about treatment adjustments. This responsiveness is vital as it with the evolving needs of individuals. Current best practices advocate for including objective data, such as vital signs and observable symptoms, alongside subjective insights like the individual's self-reported experiences. This comprehensive approach fosters better communication among interdisciplinary teams and supports continuity of care, ultimately leading to improved outcomes for individuals.
Did you know that recent trends indicate 67% of telehealth providers have adopted integrated software systems for therapy records and billing? This shift simplifies record-keeping processes, allowing clinicians to focus more on what truly matters: patient support. By prioritizing detailed and timely records, healthcare providers can significantly elevate the quality of care delivered. Together, let’s embrace these practices to ensure that every individual receives the compassionate care they deserve.
Therapy Notes Template: Streamlining Mental Health Documentation
Navigating the complexities of mental health care can often feel overwhelming. For many professionals, the burden of administrative tasks can detract from the vital work of supporting clients. This is where a treatment notes template becomes invaluable. By providing an organized format, it allows for efficient documentation of an individual's mood, therapeutic interventions, and assigned tasks or homework.
Imagine the relief of having a standardized template that captures all pertinent details with ease. This not only reduces the time spent on paperwork but also empowers therapists to focus more on their clients during sessions. Such efficiency can significantly enhance the quality of care provided, ensuring that each client feels truly heard and supported.
Moreover, well-structured therapy records foster better engagement and promote clearer communication among providers. This collaborative approach is essential for ensuring continuity of care, allowing clients to navigate their therapeutic journey with confidence and reassurance. Embracing tools like a treatment notes template can transform the documentation process, making it a supportive ally in the quest for improved mental health outcomes.
Clinical Notes Template: Standardizing Documentation Across Specialties
Healthcare providers often face overwhelming emotional challenges due to administrative burdens that detract from patient care. A treatment notes template offers a structured framework for recording encounters across various specialties, including essential elements such as demographics, medical history, examination findings, and treatment plans. By standardizing records, we can enhance the quality and consistency of medical files, which promotes improved communication and collaboration among multidisciplinary teams.
Research shows that organized records can significantly increase note quality, with scores rising from 64.35 to 77.2 after implementation. This highlights the effectiveness of the in clinical practice and how it can alleviate some of the pressures faced by providers. Additionally, by simplifying the record management process, healthcare professionals can reduce the time spent on administrative tasks like scheduling, billing, and record-keeping. This enables a greater emphasis on client support, ultimately improving outcomes for individuals.
Moreover, this approach addresses the discontent among primary care doctors stemming from excessive administrative loads. It aids adherence to regulatory mandates and ensures that records meet legal criteria, all while enhancing overall service quality. Imagine a work environment where your focus can shift back to patient care, fostering a more fulfilling practice. It’s time to embrace solutions that support you in your vital role, allowing you to connect more deeply with those you serve.
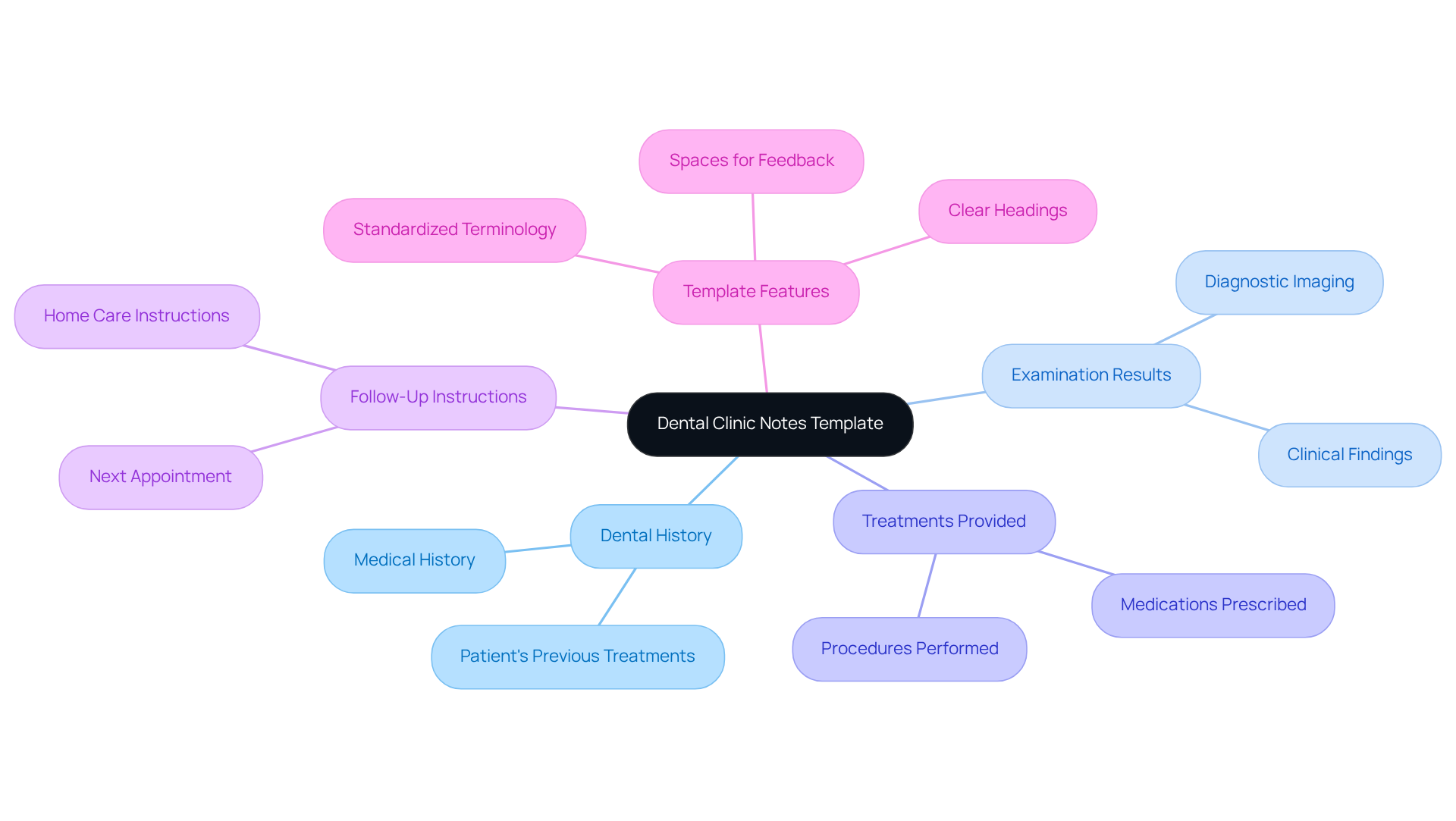
Dental Clinic Notes Template: Essential for Accurate Dental Records
The for the dental clinic is thoughtfully designed to address the essential aspects of dental treatment documentation. It typically features specific sections for capturing an individual's dental history, examination results, treatments provided, and follow-up instructions. By using a structured format, dental professionals can maintain accurate and comprehensive records, which are crucial for ensuring patient safety and supporting effective treatment planning.
Have you ever felt overwhelmed by the administrative demands of your practice? Current best practices emphasize the need for a treatment notes template that thoroughly reflects clinical findings and fosters collaborative care among providers.
As we witness the evolution of trends, the emphasis on digital documentation tools is growing, offering opportunities for real-time updates and improved accessibility. Essential components of an efficient dental clinic documentation template include:
- Clear headings
- Standardized terminology
- Spaces for feedback
These elements not only enhance clarity but also contribute to a deeper understanding of each individual's oral health journey. Remember, each detail matters, and together we can ensure that every patient's experience is as seamless and supportive as possible.
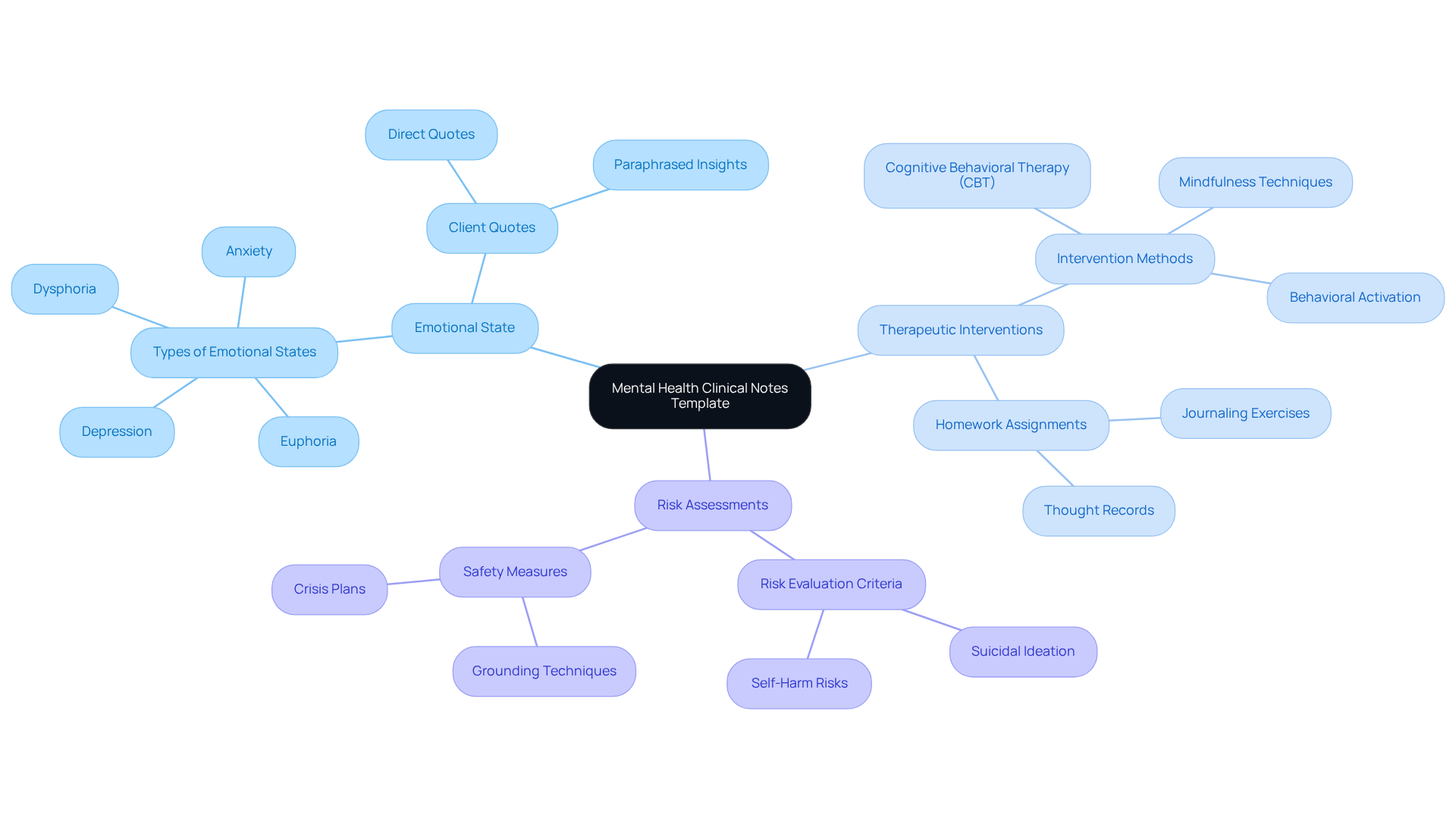
Mental Health Clinical Notes Template: Tailored for Effective Patient Care
The mental health clinical notes template is thoughtfully crafted to meet the unique needs of mental health providers. This template typically features sections dedicated to capturing an individual's emotional state, therapeutic interventions, and any performed. By utilizing a tailored format, mental health professionals can ensure that all essential details are meticulously documented, which is vital for providing effective and compassionate care.
Including risk evaluations in these records not only enhances safety for individuals but also informs treatment strategies, allowing for a more personalized approach. Furthermore, accurately documenting emotional states is crucial for tracking progress and adjusting therapeutic methods, ultimately leading to improved outcomes for individuals.
The use of customized clinical documentation fosters a deeper understanding of each individual's unique circumstances, enriching the quality of mental health support. How might this structured approach help you in your practice? By embracing these tools, we can collectively enhance the care we provide and support the well-being of those we serve.
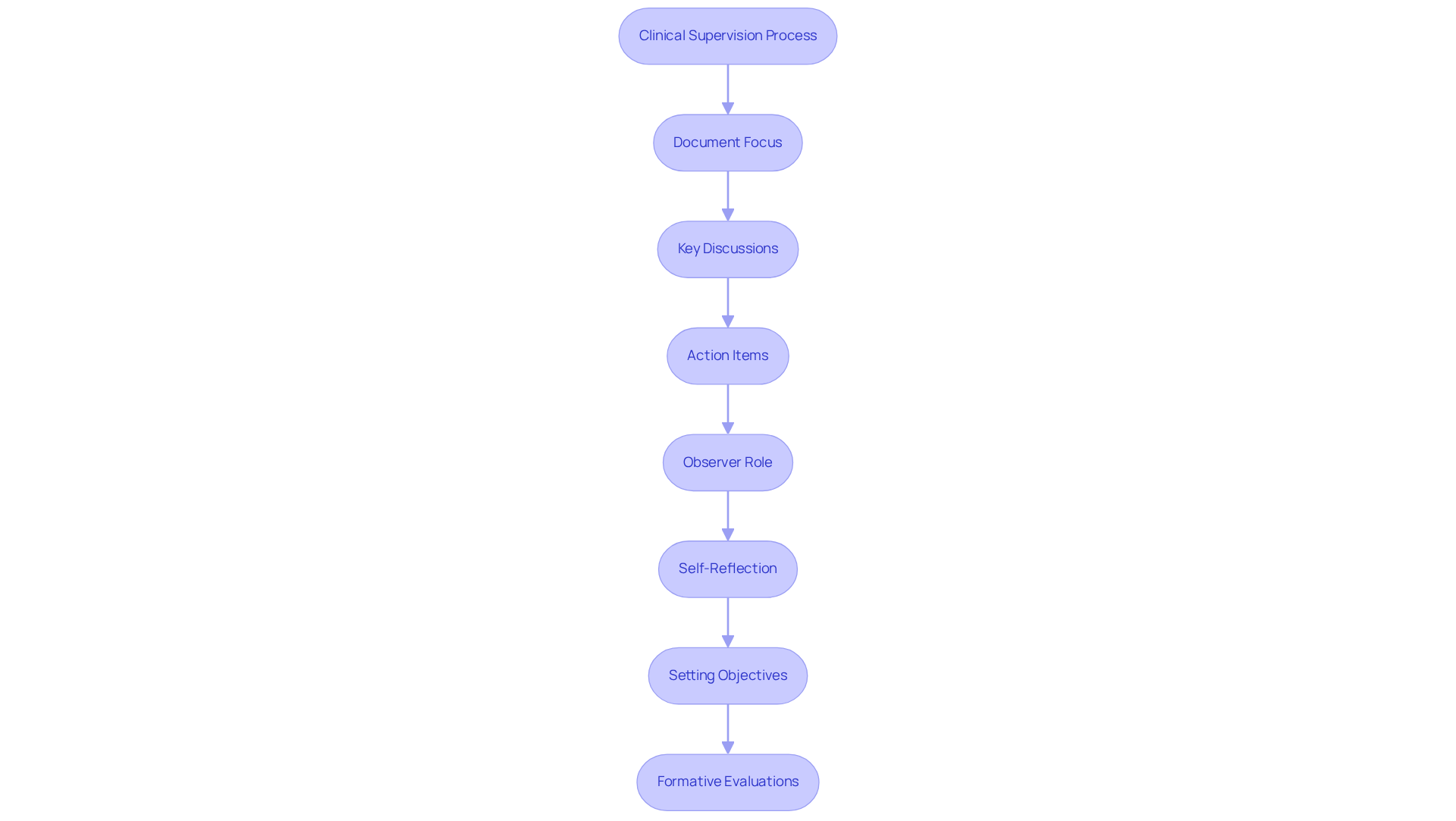
Clinical Supervision Notes Template: Enhancing Provider Training and Oversight
The plays a crucial role in enhancing the training and oversight of healthcare providers. This structured template typically includes sections for documenting the focus of supervision sessions, key discussions, and agreed-upon action items. By maintaining comprehensive supervision notes, organizations ensure that providers receive the necessary support and guidance for their professional growth. This, in turn, improves the quality of care delivered to patients.
Current trends highlight the importance of thorough records in clinical supervision. These records not only enhance accountability but also help identify areas for improvement and foster a culture of ongoing learning within healthcare environments. Effective supervision documentation includes maintaining an observer role during live sessions, allowing supervisors to provide immediate feedback and model best practices.
Moreover, supervisors should encourage self-reflection among supervisees regarding their [cultural biases and attitudes](https://blog.cosmaneura.com/10-examples-of-doctor-notes-for-effective-patient-documentation). This approach fosters a deeper understanding of their professional development. Setting clear objectives for supervision sessions is essential, as it enhances the effectiveness of the supervision process. Formative evaluations that focus on changeable behaviors can offer valuable insights into the ongoing growth of healthcare providers.
Additionally, discussions about countertransference and its impact on counseling are vital for ensuring high-quality support. Statistics suggest that supervision should occur at least once every 20-40 hours of clinical practice, serving as a benchmark for effective oversight.
By adopting these practices, healthcare organizations can cultivate skilled professionals who are well-prepared to meet the evolving needs of care. Together, let us commit to nurturing the growth of our healthcare providers, ensuring they feel supported and empowered in their vital roles.
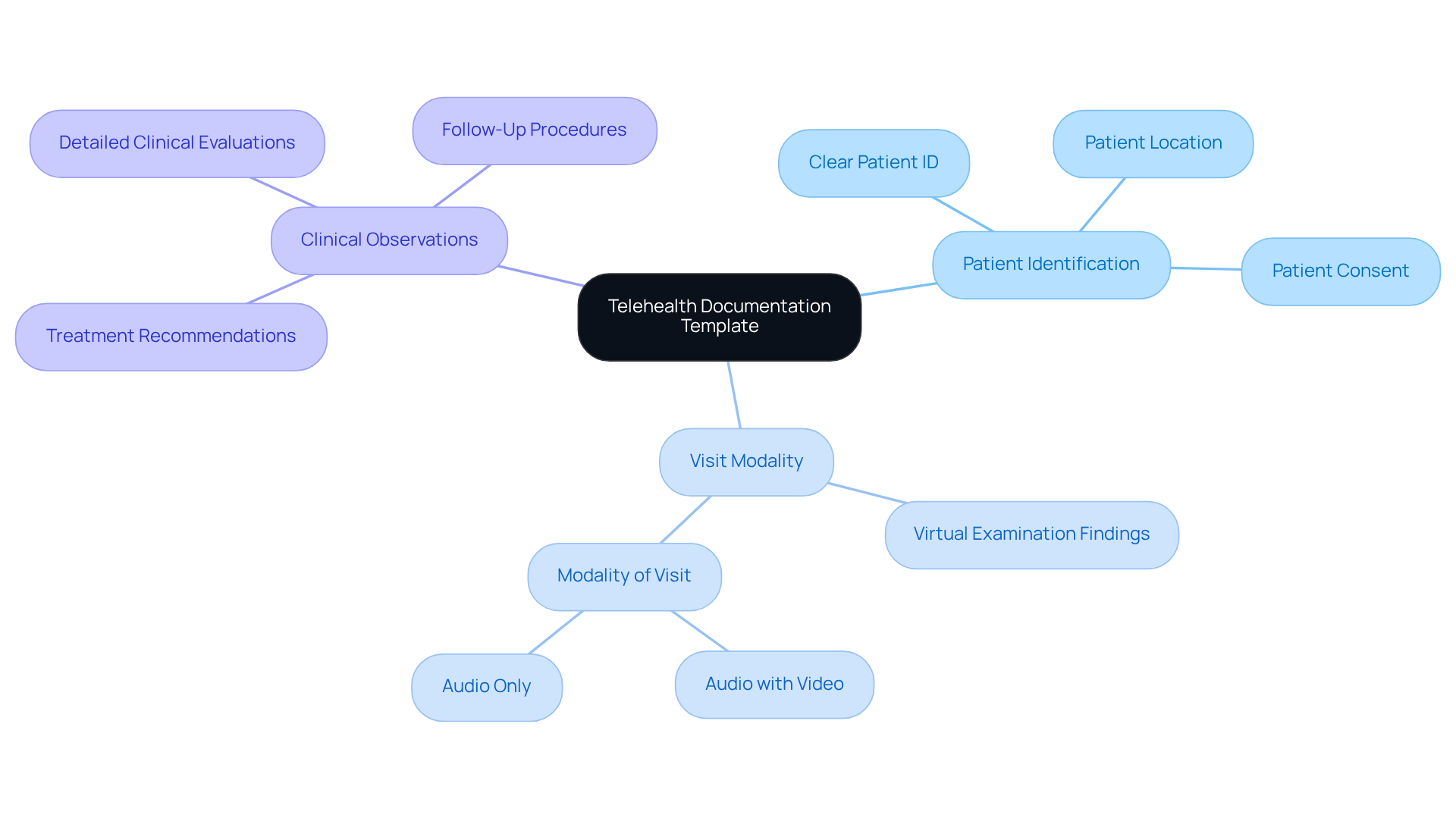
Telehealth Documentation Template: Ensuring Comprehensive Virtual Care Records
A well-crafted treatment notes template is essential for accurately recording all relevant information during virtual consultations. Have you ever felt overwhelmed by the administrative burdens that come with patient care? The treatment notes template should encompass sections for documenting the patient's presenting issues, virtual examination findings, and treatment recommendations. By employing a structured format, healthcare providers can ensure comprehensive records of telehealth interactions, which are vital for continuity of care and adherence to regulatory requirements.
Moreover, generative AI can , such as appointment scheduling and medical record management. Imagine the relief of having these tasks handled efficiently, allowing you to focus more on your patients. Efficient records enhance safety for individuals and simplify billing procedures, ultimately enhancing overall healthcare provision.
Essential components of a successful telehealth recording framework include:
- Clear identification of the individual
- Detailed descriptions of the visit's modality
- Comprehensive observations on clinical evaluations
Organized telehealth records enhance communication among support teams and lead to better outcomes for individuals by ensuring that all pertinent information is easily accessible. Let's work together to improve our documentation practices and provide the best care possible.
Customizable Clinical Notes Template: Adapting Documentation to Provider Needs
Healthcare providers often face emotional challenges in their daily tasks, particularly when it comes to managing documentation. Customizable treatment notes templates offer a solution that allows them to tailor their records to meet specific needs effectively. By incorporating distinct fields customized for different specialties or individual practices, these templates foster a more personalized approach to care.
Imagine the relief that comes from knowing that your documentation processes can be significantly enhanced. With such customization, providers can improve both the of their records. This guarantees that all essential information is gathered in a way that aligns with the specific requirements of their practice and the diverse needs of those they serve.
Key features, such as standardized fields for communication and integrated data sharing capabilities, not only streamline workflows but also promote improved communication among care teams. This collaborative environment ultimately leads to better outcomes for individuals, enhancing the overall patient experience. In today's competitive healthcare landscape, prioritizing patient experience is essential for organizational success. Effective documentation plays a crucial role in achieving this goal.
Consider how the treatment notes template can alleviate some of the administrative burdens that impact patient care. By embracing this innovative approach, healthcare providers can focus more on what truly matters—the well-being of their patients. Let's work together to create a more compassionate healthcare experience.
Conclusion
Embracing effective treatment notes templates is not just a procedural change; it’s a vital step for healthcare providers striving to enhance their documentation processes and ultimately improve patient care. Have you ever felt overwhelmed by administrative tasks? By integrating structured frameworks like SOAP, progress notes, and customizable templates, professionals can streamline their record-keeping, allowing more time to focus on delivering compassionate care. The innovative use of AI, particularly through platforms like CosmaNeura, alleviates the administrative burden even further, enabling healthcare workers to prioritize their patients' needs.
Throughout this article, we’ve explored various templates, each tailored to specific aspects of healthcare documentation. From the structured approach of SOAP notes to the personalized nature of customizable templates, these tools not only improve the quality of records but also foster better communication among care teams. Insights from customer interviews and research highlight the growing trust in AI and the significance of adopting these practices to enhance operational efficiency.
As the healthcare landscape continues to evolve, it’s crucial for providers to embrace these documentation solutions. By doing so, they can ensure they meet regulatory requirements while fostering an environment that prioritizes patient experience and outcomes. The call to action is clear: invest in effective treatment notes templates to transform administrative tasks into opportunities for enhanced patient care and support. Together, let’s make a difference in the lives of those we serve.




