Overview
The article highlights the emotional challenges faced by healthcare providers in their daily practice. It recognizes that the weight of administrative tasks can often overshadow the primary focus of patient care. By providing internal medicine SOAP note examples, it aims to enhance documentation efficiency in healthcare, ultimately alleviating some of this burden.
Structured templates and AI-powered tools emerge as essential solutions, significantly reducing these administrative pressures. This shift allows healthcare providers to concentrate more on what truly matters: their patients. As a result, not only does documentation quality improve, but overall patient outcomes are positively impacted as well.
Imagine a work environment where you can dedicate more time to your patients, fostering deeper connections and better care. This is the promise of embracing efficient documentation practices. We encourage you to explore these tools and templates, and take a step towards transforming your practice for the better.
Introduction
In the complex world of healthcare, many providers find themselves struggling to balance patient care with the weight of administrative tasks. This imbalance can lead to burnout and a reduction in meaningful patient interactions, which is concerning for both clinicians and their patients. This article explores ten innovative internal medicine SOAP note examples designed to ease the documentation burden, ultimately allowing clinicians to focus more on what truly matters—their patients.
As the healthcare landscape continues to evolve, it’s vital for practitioners to consider how these tools can not only lighten their workload but also maintain the high quality of care that patients deserve. How can we ensure that technology serves as a support rather than a hindrance? By examining these examples, we uncover not just practical solutions, but also the essential questions that arise when integrating technology into healthcare documentation. Let’s reflect on the journey ahead and the possibilities that lie within these advancements.
CosmaNeura: Streamline SOAP Note Documentation with AI-Powered Efficiency
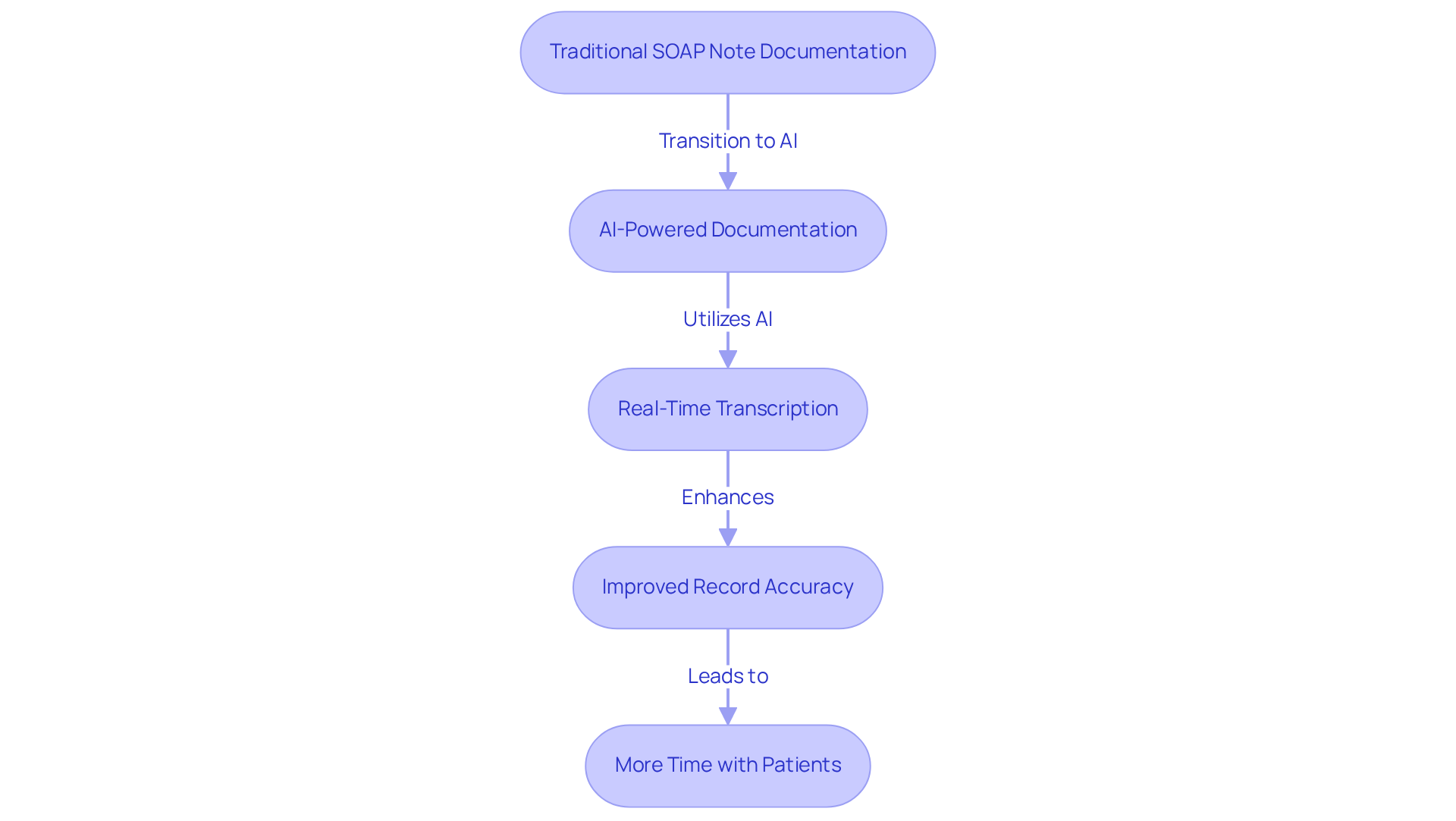
In today's demanding healthcare environment, providers often face overwhelming administrative burdens that can detract from their primary focus—caring for patients. CosmaNeura understands these challenges and utilizes advanced AI technology to transform the recording process for an internal medicine soap note example. By significantly reducing the time healthcare providers allocate to administrative duties, the platform allows clinicians to prioritize quality patient care over paperwork.
Imagine a world where real-time transcription and summarization empower you to spend more time with your patients. This shift not only boosts efficiency but also improves record accuracy, aligning with best practices in clinical environments. Research suggests that AI can decrease the time doctors dedicate to administrative tasks by roughly 20%, freeing up valuable moments for compassionate care.
Moreover, CosmaNeura's commitment to Catholic teachings ensures that ethical considerations in patient care are upheld. This comprehensive approach to healthcare documentation resonates deeply with providers who prioritize moral responsibility. By automating documentation, CosmaNeura creates an internal medicine soap note example that optimizes workflows and promotes a more caring healthcare experience.
Are you ready to embrace a solution that not only enhances your efficiency but also aligns with your values? With CosmaNeura, you can , allowing you to focus on what truly matters—your patients. Join us in creating a more compassionate healthcare environment, where every moment counts.
Heidi Health: Comprehensive SOAP Note Template for Effective Patient Management
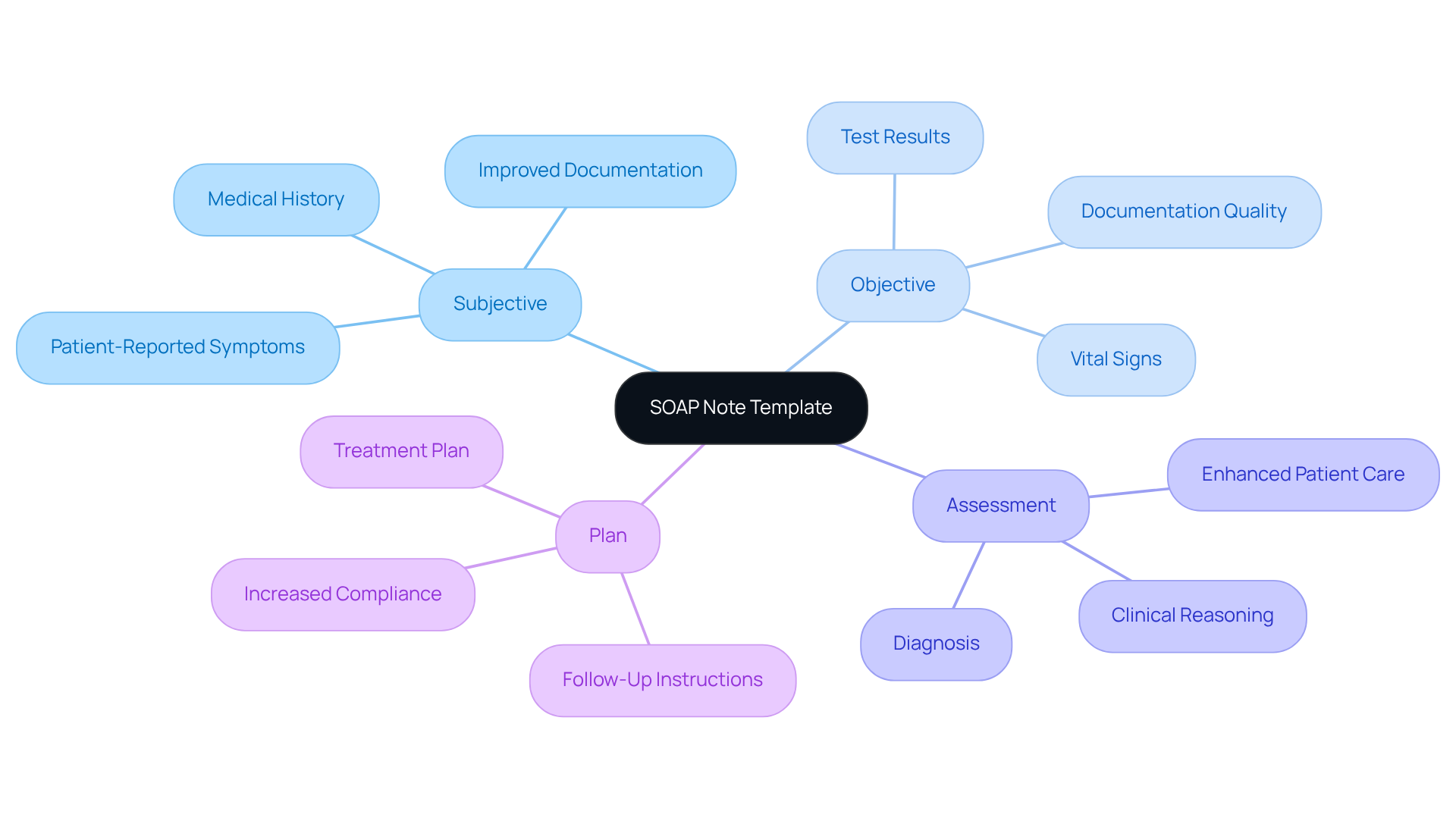
Heidi Health understands the emotional challenges healthcare providers face, especially when it comes to managing administrative tasks that can detract from patient care. That's why we offer an internal medicine soap note example that encompasses the essential sections: Subjective, Objective, Assessment, and Plan. This organized format enables professionals to record interactions with individuals efficiently, much like an internal medicine soap note example that captures all essential information.
Imagine how much easier your day could be with a tool that enhances not only your record-keeping but also the monitoring of progress and treatment results. By employing organized clinical records, such as an internal medicine soap note example, you can improve the quality of your documentation, which greatly aids in better management and care provision. Recent studies show that adopting organized record-keeping methods can boost compliance rates from 38.2% to 87.2%. This emphasizes the significance of structured templates, including an internal medicine soap note example, in clinical practice.
Moreover, professional insights highlight that precise and systematic clinical records, including an internal medicine soap note example, are essential for providing top-notch care. In today’s healthcare environment, using an internal medicine soap note example demonstrates that structured formats are more important than ever. By incorporating generative AI into the record-keeping process, healthcare providers can simplify administrative tasks associated with clinical summaries, such as automating data entry and ensuring uniformity in records.
Dr. Claire Dave stresses that effective records create tangible, quantifiable benefits for both healthcare providers and the practice’s financial outcomes. This reinforces the in improving care for individuals. Embrace the opportunity to enhance your practice and the care you provide by adopting these supportive tools.
Mentalyc: Tailored SOAP Note Examples for Mental Health Professionals
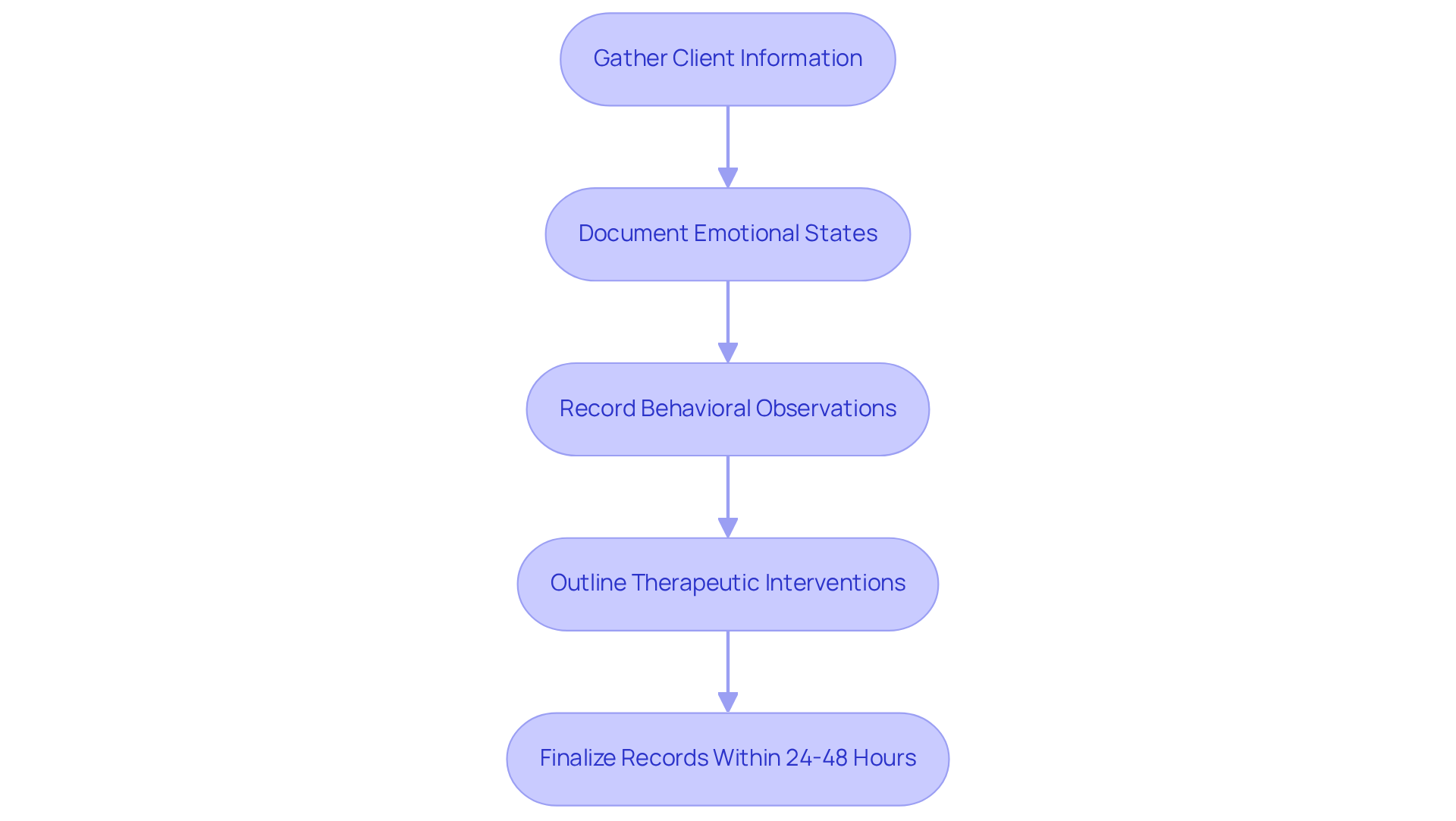
Mentalyc understands the emotional challenges that mental health professionals face, providing a comprehensive array of SOAP note examples tailored specifically for their unique documentation needs. These examples serve as vital resources, enabling clinicians to gather essential client information, such as emotional states, behavioral observations, and therapeutic interventions effectively. By offering context-specific templates, Mentalyc empowers mental health providers to maintain precise and meaningful records, which are crucial for informed treatment planning and enhancing patient engagement.
As Susan Smith, LCSW, wisely points out, 'Aim for records that are succinct yet still thorough in addressing essential components.' This highlights the importance of clarity in written communication, which can significantly impact the quality of care provided. Prompt record-keeping is equally essential; best practices suggest finalizing entries within 24-48 hours of the session to ensure accuracy and relevance.
Tailored documentation not only fosters a deeper understanding of each client's journey but also supports the delivery of high-quality, individualized care. This aligns with the legal and ethical responsibilities inherent in mental health practice. By embracing these practices, mental health professionals can alleviate some administrative burdens, allowing them to focus more on what truly matters—their clients.
SimplePractice: User-Friendly Tools for Writing SOAP Notes
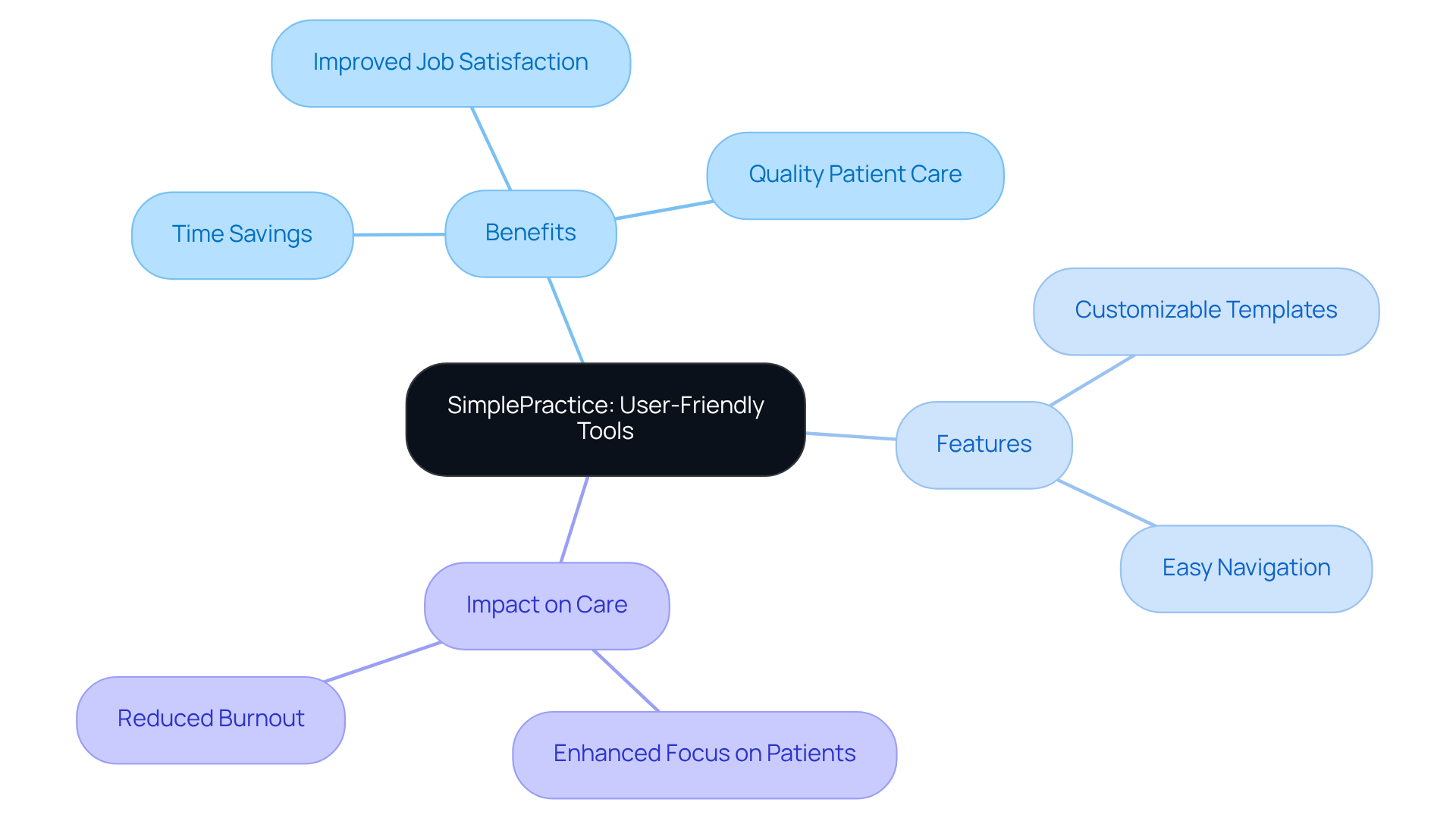
Healthcare providers often face overwhelming emotional challenges due to the administrative burdens they carry. The pressing issue of physician burnout is exacerbated by excessive paperwork, which can detract from the quality of patient care. SimplePractice offers intuitive tools designed to significantly enhance the internal medicine SOAP note example writing process, allowing clinicians to document encounters efficiently while ensuring accuracy and detail.
With and straightforward navigation, healthcare professionals can prioritize care over tedious record-keeping tasks. This user-friendly interface effectively helps reclaim valuable time that can be redirected towards meaningful interactions with individuals. Imagine the relief of focusing more on delivering quality care rather than being bogged down by administrative duties.
By simplifying the note-taking experience, SimplePractice not only boosts clinician efficiency but also contributes to improved job satisfaction. Providers can feel a renewed sense of purpose, as they are no longer overwhelmed by the weight of administrative tasks. It’s noteworthy that physicians spend approximately 50% of their time on these duties, highlighting the importance of tools like SimplePractice in alleviating this burden.
Consider how much more fulfilling your work could be with the right support. SimplePractice empowers you to focus on what truly matters—your patients. If you’re ready to reclaim your time and enhance your practice, it’s time to explore the benefits of SimplePractice.
Psylio: Specialized SOAP Note Examples for Diverse Therapeutic Practices
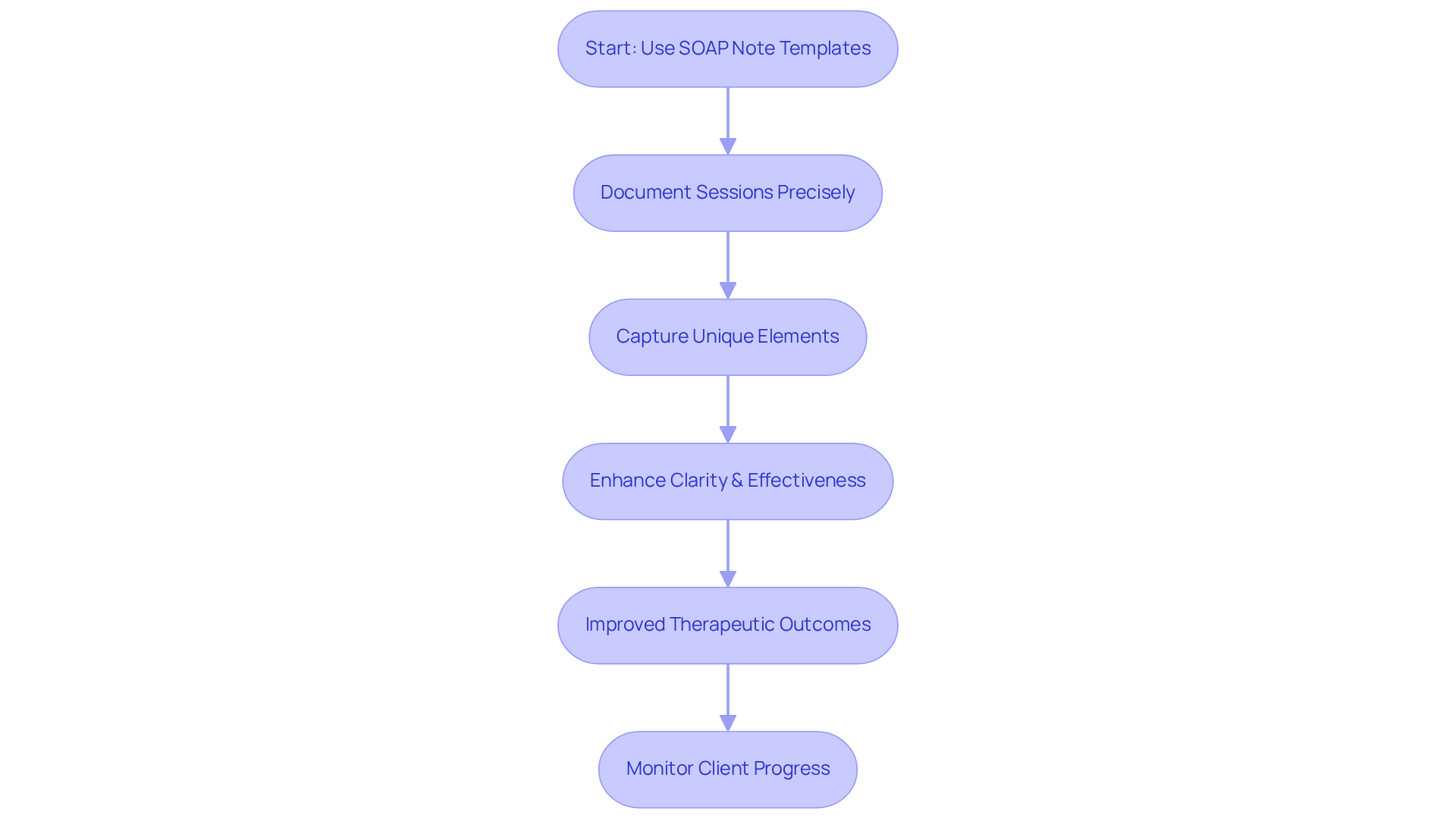
In the demanding world of healthcare, practitioners often face emotional challenges that can impact their ability to provide the best care. Psylio understands these struggles and offers a comprehensive array of specialized SOAP note examples, including an internal medicine soap note example, tailored for diverse therapeutic practices such as psychotherapy, counseling, and holistic health. These context-specific templates empower practitioners to document their sessions with precision, capturing the unique elements of each therapeutic approach.
By concentrating on the subtleties of various modalities, Psylio ensures that clinicians can maintain high record-keeping standards while prioritizing patient care. This customized method not only enhances the clarity and effectiveness of clinical records but also aligns with , which emphasize specificity and relevance in therapeutic settings.
Effective documentation is crucial for compliance and continuity of care. It fosters a deeper understanding of client progress, ultimately leading to improved therapeutic outcomes. Have you considered how including direct quotes from clients in the subjective part of your documentation can capture nuances in their experiences? Monitoring changes in client speech over time can also reveal significant shifts that indicate progress.
However, it is important to acknowledge the potential difficulties of documentation in healthcare. These tasks can be time-consuming and vary in quality among providers. By embracing solutions like Psylio's templates, we can alleviate some of these burdens and focus more on what truly matters—our clients' well-being.
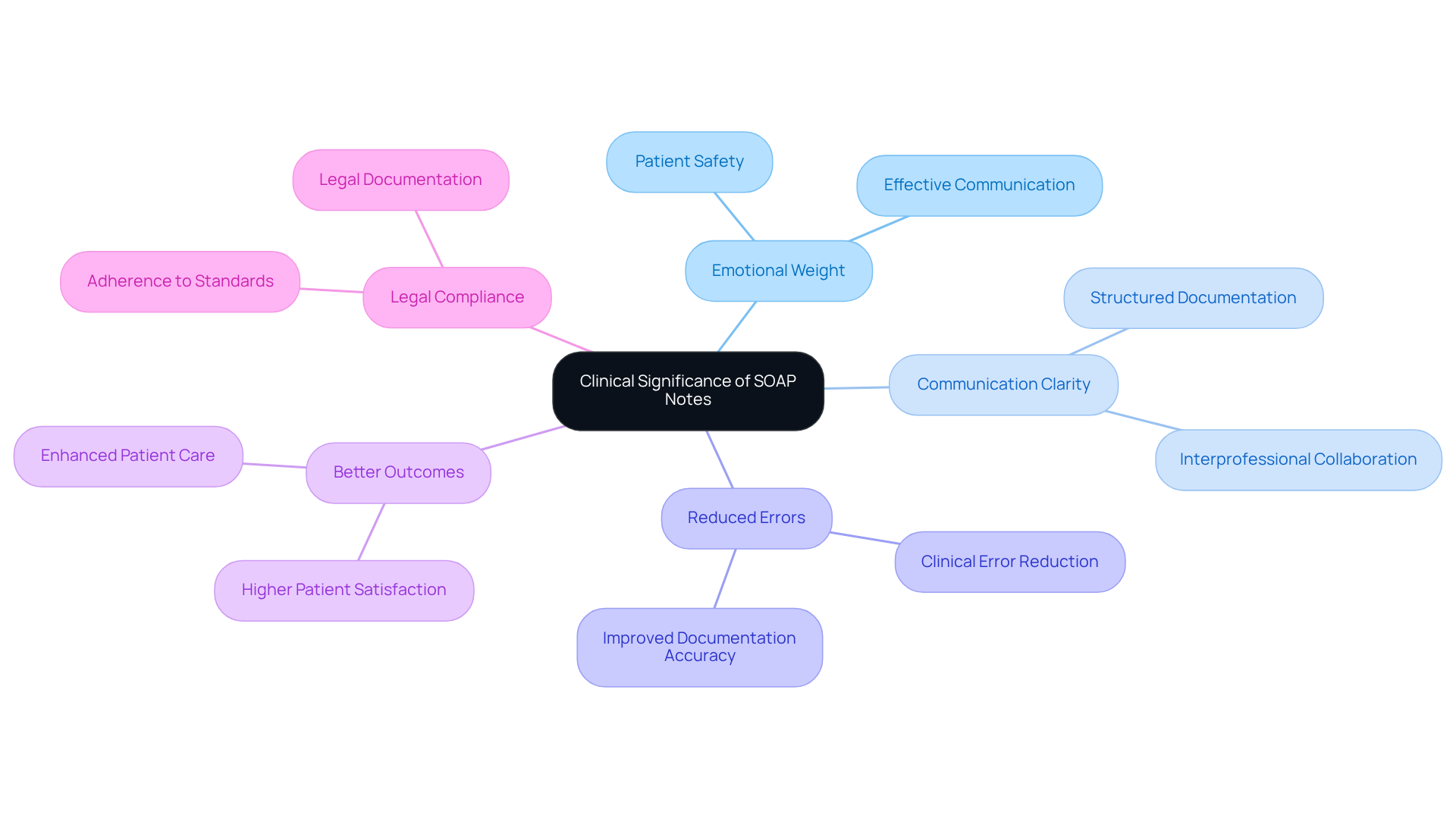
NCBI: Foundational Insights on the Clinical Significance of SOAP Notes
Healthcare professionals often grapple with the emotional weight of ensuring patient safety and effective communication. The clinical importance of structured records shines in their ability to foster clear communication among these dedicated individuals. This organized approach not only ensures that vital client information is accurately documented but also makes it easily retrievable—an essential aspect of delivering efficient care.
Research highlights that structured record frameworks, such as organized formats, significantly enhance communication clarity and reduce clinical errors. These improvements are not just beneficial; they lead to better patient outcomes, which is the ultimate goal of every healthcare provider. Furthermore, adhering to this formatting style supports compliance with legal and regulatory standards, underscoring its vital role in the healthcare environment.
By recognizing the essential function of documentation, clinicians can cultivate a deeper understanding of their impact on delivering high-quality, patient-centered care. How might embracing structured records transform your practice? Together, let's prioritize for the benefit of our patients and ourselves.
CanadianPA: Practical Tips and Examples for Writing Effective SOAP Notes
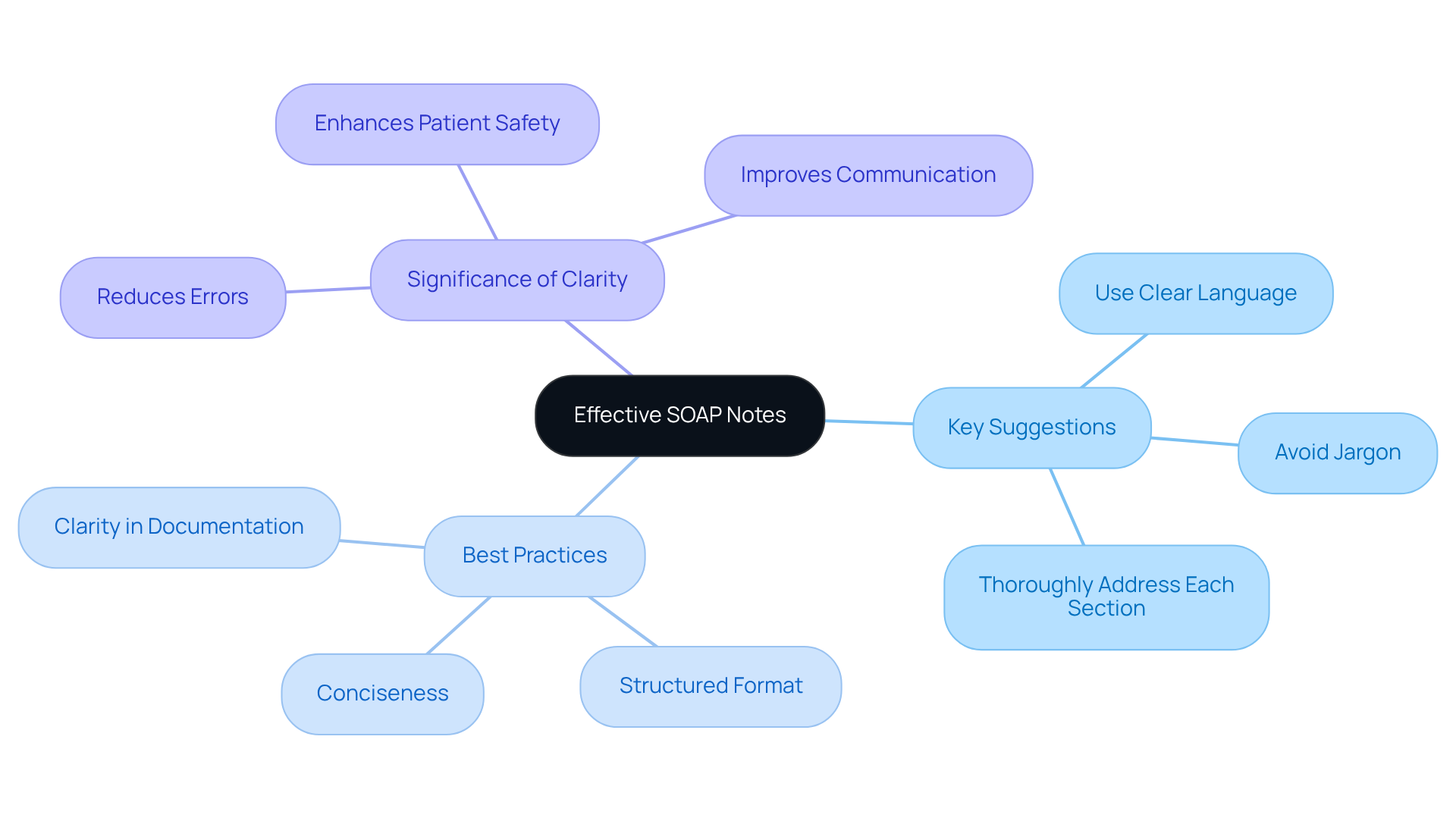
At CanadianPA, we recognize the emotional challenges healthcare providers face in documenting clinical summaries. Effective communication is not just about records; it’s about the care and understanding we offer to individuals. Clarity, brevity, and relevance in documentation are essential, and we’re here to support you in navigating these complexities.
To and ultimately improve outcomes for individuals, consider these key suggestions: utilize standardized terminology, avoid jargon, and ensure that every section of the document is thoroughly addressed. By following these guidelines, you can foster better communication among healthcare providers and provide optimal care.
Best practices for improving SOAP note clarity include:
- Use of Clear Language: Employ straightforward terminology that accurately conveys the patient's status and treatment plan.
- Conciseness: Aim for brevity without sacrificing essential details. This not only saves time but also reduces the likelihood of misinterpretation.
- Structured Format: Maintain a consistent structure across notes to facilitate easier navigation and understanding.
For instance, instead of stating, "The individual appears to be in mild distress," a clearer approach would be, "The individual reports a pain level of 4 out of 10, indicating mild distress."
The significance of clarity in written records cannot be overstated. Research shows that effective communication in healthcare environments significantly reduces errors and enhances safety for individuals. As one expert aptly noted, "Simplicity is the ultimate sophistication," underscoring that clear and concise documentation fosters better understanding and collaboration among healthcare teams.
By applying these tactics, you can enhance the quality of your documentation. This not only leads to improved outcomes for individuals but also cultivates more efficient communication within the healthcare system. Let’s work together to make a difference in the lives of those we serve.
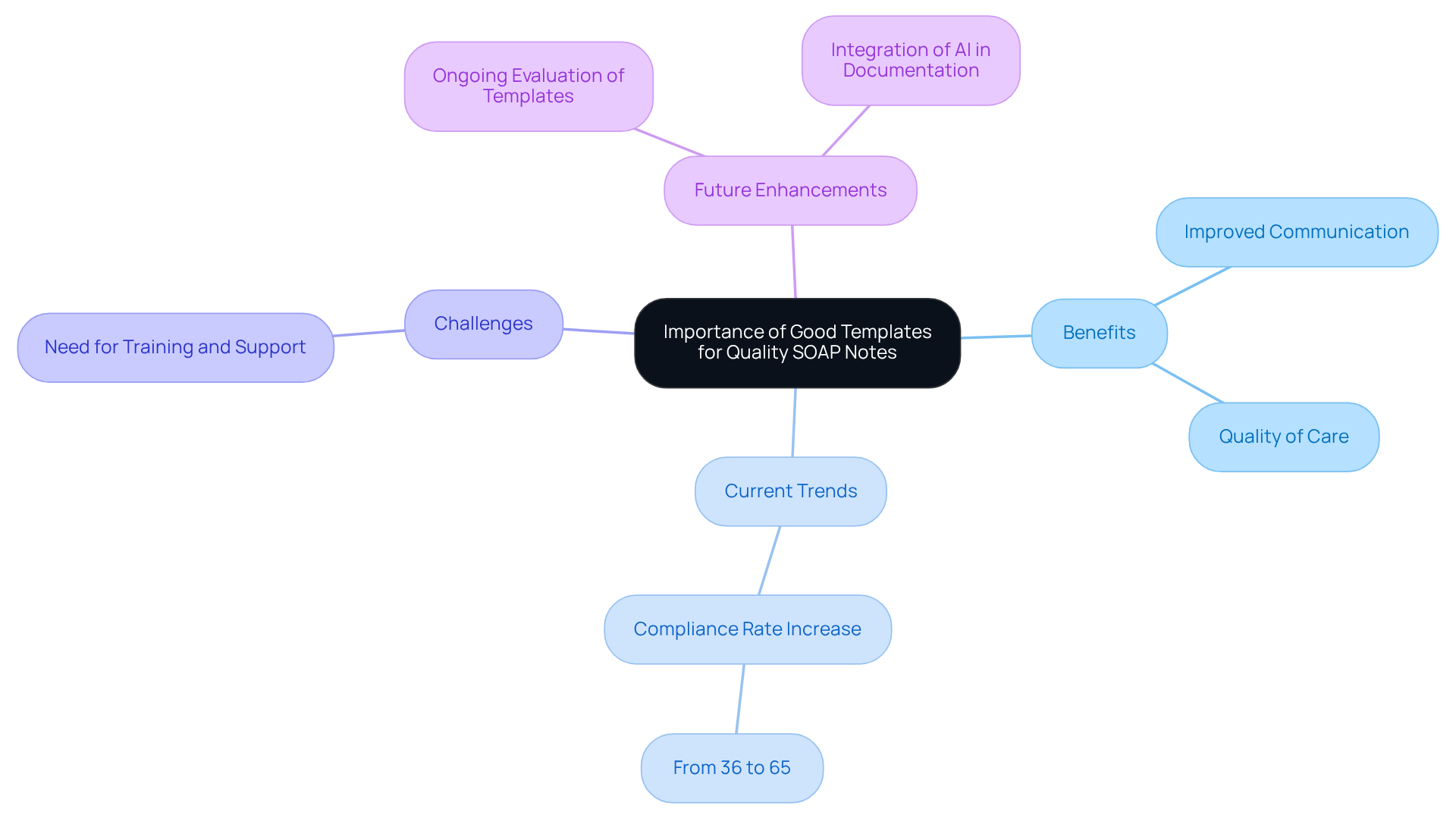
Heidi Health: Importance of Good Templates for Quality SOAP Notes
Heidi Health understands the emotional challenges faced by healthcare providers in today’s demanding environment. The significance of utilizing effective templates, including an internal medicine soap note example, for producing quality clinical documentation cannot be overstated. Well-crafted templates ensure that all pertinent individual information is recorded consistently, which promotes improved communication and continuity of care.
By offering healthcare professionals structured formats, Heidi Health aids in enhancing the accuracy and completeness of the internal medicine soap note example. This ultimately leads to improved quality of care, allowing providers to focus on what truly matters—their patients. Imagine a world where the integration of generative AI into healthcare workflows streamlines the documentation process. Physicians can automate time-consuming administrative tasks, reducing their cognitive load and enabling them to engage more meaningfully with patients. This enhancement significantly enriches the overall patient experience.
Current trends indicate a growing acceptance of standardized templates among healthcare professionals. Compliance rates have increased from 36% to 65% over the study period, reflecting a positive shift. However, it’s essential to acknowledge that challenges remain. Some residents have reported difficulties in adopting these templates, highlighting the need for ongoing training and support.
As we move forward, let’s embrace these tools together, fostering a supportive environment where healthcare providers can thrive. How can we further enhance our practices to ensure that every patient receives the care they deserve? Together, we can tackle these challenges and create a more .
Mentalyc: Common Pitfalls to Avoid in SOAP Note Writing
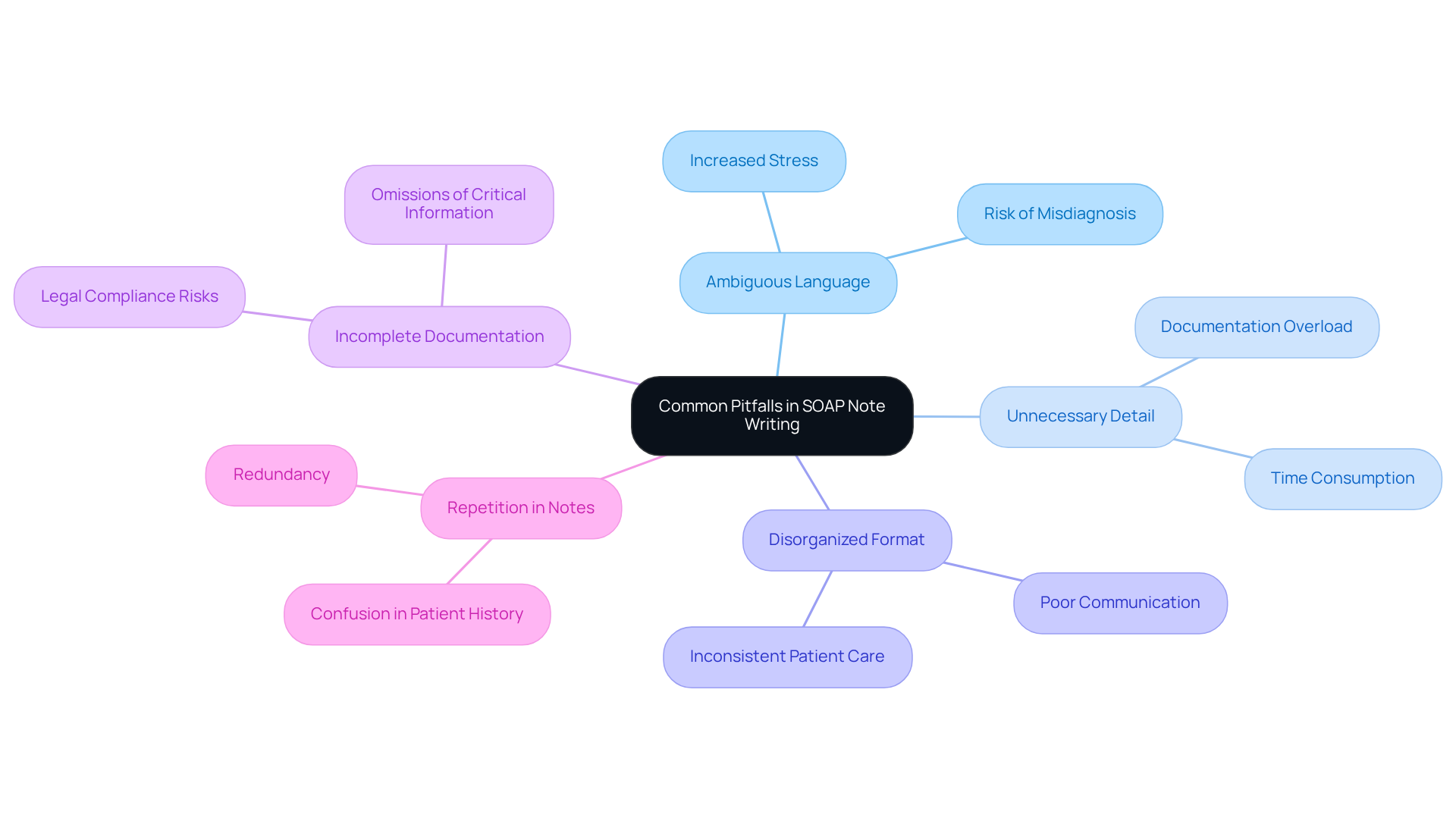
In the demanding world of healthcare, providers often face emotional challenges when it comes to documentation. Mistakes such as ambiguous language, unnecessary detail, and disorganized formats can add to the stress of an already heavy workload. It’s crucial for healthcare professionals to be precise in their documentation, articulating each part of the clinical record clearly.
Imagine utilizing organized tools to prevent omissions in medical records. This practice is vital for upholding clarity and precision, ultimately . Statistics show that ICANotes allows healthcare professionals to generate high-quality documentation in just two to three minutes, significantly improving efficiency and time management.
However, unfinished clinical documentation can lead to missing essential details about symptoms or medical history, which may result in misdiagnosis or unsuitable treatment. By avoiding these common errors and following best practices, healthcare professionals can enhance the clarity and effectiveness of their records. This not only benefits individual patients but also fosters better communication among team members.
Moreover, keeping audit-ready records is critical for compliance and legal protection, underscoring the importance of high-quality clinical entries. Let's work together to improve documentation practices, ensuring that every patient receives the care they deserve.
SimplePractice: Best Practices for Effective SOAP Note Documentation
Effective documentation of clinical notes is not just a task; it’s a vital component of providing high-quality care and complying with healthcare regulations. Timely and precise documentation of individual information is essential, as it directly impacts patient outcomes. Clinicians are encouraged to embrace clear and concise language while following the structured SOAP format, as shown in an internal medicine soap note example—Subjective, Objective, Assessment, and Plan. By consistently revising and refreshing the internal medicine soap note example, we can capture any changes in patient condition, ultimately enhancing the quality of our records.
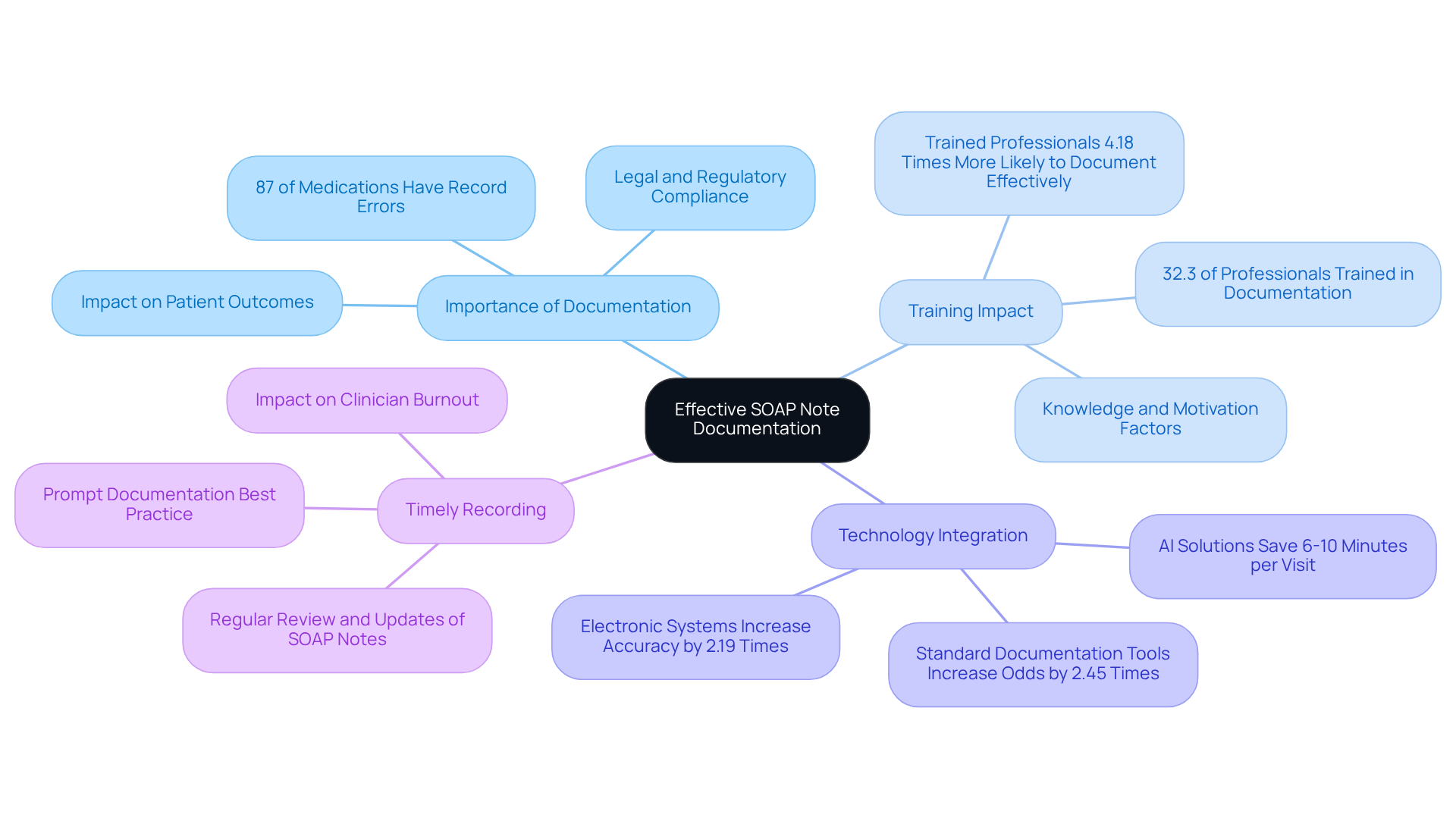
However, many healthcare providers face the emotional burden of ensuring record accuracy, which remains a significant challenge in our field. Did you know that research shows 87% of medications contained record errors in specific areas? This statistic underscores the urgent need for improved practices. Health professionals who have received training are 4.18 times more likely to document routine practices effectively, highlighting the profound impact that education can have on the quality of our records.
Timely recording is not just a best practice; it is a necessity for our patients. An internal medicine soap note example demonstrates how effective record-keeping leads to better treatment outcomes by providing clear and organized files that enhance communication among healthcare providers. For instance, AI-powered solutions can simplify the record-keeping process, allowing clinicians to save 6-10 minutes per visit. This time savings can significantly alleviate burnout and improve job satisfaction. By automating routine paperwork tasks, generative AI enables us to focus more on our patients, ultimately raising the standard of care.
Integrating technology into our record-keeping practices can further elevate accuracy. The use of electronic systems has been shown to increase the likelihood of accurate records by 2.19 times, demonstrating the value of adopting modern tools. By prioritizing timely and precise recording, we can ensure our documentation meets both clinical and regulatory standards, leading to enhanced care for individuals. Furthermore, leveraging generative AI allows us to streamline workflows, reduce administrative burdens, and improve patient experiences, addressing the pressing challenges of labor shortages and increasing demands in healthcare. Together, let’s embrace these solutions to foster a more compassionate and .
Conclusion
The integration of structured SOAP note documentation in healthcare is essential for enhancing patient care and provider efficiency. Many healthcare professionals face emotional challenges due to overwhelming administrative tasks. By utilizing effective templates and AI-powered solutions, clinicians can streamline their documentation processes, allowing for a greater focus on patient interactions rather than administrative burdens. This shift not only improves the accuracy of records but also upholds the ethical standards of care, ensuring that healthcare providers can deliver compassionate and informed treatment to their patients.
Throughout this discussion, various platforms like CosmaNeura, Heidi Health, Mentalyc, SimplePractice, and Psylio have been highlighted for their unique contributions to SOAP note documentation. These tools offer tailored templates, user-friendly interfaces, and AI-driven efficiencies that address the emotional and practical challenges faced by healthcare professionals. Clear communication, adherence to structured formats, and timely documentation are crucial components in improving patient outcomes and compliance with healthcare regulations.
In conclusion, embracing modern documentation practices is not just about improving efficiency; it is about fostering a healthcare environment where providers can thrive and patients receive the highest quality of care. By adopting these innovative solutions, healthcare professionals can alleviate the stress of documentation, enhance their communication, and ultimately focus on what truly matters—the well-being of their patients. It is time to prioritize effective SOAP note strategies and transform the way healthcare is delivered for a more compassionate future.




